Abstract
Purpose
To evaluate an outbreak of endophthalmitis caused by Fusarium oxysporum after cataract surgery.
Methods
In the present study, we conducted a retrospective review of the medical records of cases of endophthalmitis that developed after cataract surgery. All eyes underwent phacoemulsification and intraocular lens implantation (PEA + IOL) at a single eye clinic on the same date. Symptoms of endophthalmitis occurred 21.5 ± 3.4 days after the cataract surgery.
Results
Nine eyes of 9 patients with fungal endophthalmitis (5 males and 4 females) were enrolled in the current study. The mean age of the patients was 63.4 ± 8.5 years. Soon after the diagnosis of endophthalmitis, pars plana vitrectomy (PPV) had been performed in all the eyes. However, because there was no response to the first PPV plus antibacterial drug therapy, we performed repeat PPV for all the eyes, combined with IOL removal and antifungal therapy (natamycin eye drops plus oral voriconazole or fosfluconazole). After the antifungal drug therapy, no recurrence of endophthalmitis was observed in any of the operated eyes, and good visual outcomes were obtained. Fusarium oxysporum was identified by culture and sequencing analysis.
Conclusion
Early diagnosis and appropriate, adequate treatment are needed for successful management of fungal endophthalmitis.
Keywords: Endophthalmitis, Fungal infection, Cataract surgery
1. Introduction
Infectious endophthalmitis is one of the serious complications of ophthalmic surgery, including cataract surgery.1 According to a recent estimate, endophthalmitis as a complication of cataract surgery occurs at an incidence of 0.07%–0.082%.2,3 In the majority of cases, postoperative endophthalmitis is caused by bacterial, and fungal endophthalmitis is rather rare.4
Visual outcomes in cases of fungal endophthalmitis are generally poor, because no standard management protocol has been established. Previous reports have indicated that Aspergillus species are the most commonly isolated causative organisms in cases of postoperative endophthalmitis; while Fusarium species have been identified in cases of fungal keratitis, reports of endophthalmitis caused by Fusarium species are rare.
An outbreak of endophthalmitis caused by Fusarium oxysporum was previously reported by Buchta et al.5 The visual outcomes in that case series were poor, mainly due to the delay in the initiation of antifungal therapy. In the present study of outbreak of Fusarium oxysporum endophthalmitis after cataract surgery, we started the patients on antifungal therapy even before Fusarium oxysporum was identified as the causative strain. As a result, the visual acuity outcomes were better as compared to those in the aforementioned previous report. The aim of the current study was to evaluate the visual outcomes in patients with Fusarium oxysporum endophthalmitis.
2. Methods
The present study was a single-center interventional study in a case series. The medical records of patients with Fusarium oxysporum endophthalmitis were retrospectively reviewed. Approval of the study protocol was obtained from the institutional review board (IRB). The study adhered to the tenets of the declaration of Helsinki.
Vitreous and IOL samples from all patients were investigated by direct microscopy and culture. Confirmation of the strain was performed by sequencing analysis at Chiba University Medical Mycology Research Center.
The minimum inhibitory concentrations (MIC) of antifungal drugs were determined by the Clinical and Laboratory Standards Institute (CLSI) broth microdilution method (M38-A2 document) for each strain as previously described.6
3. Results
Postoperative endophthalmitis was diagnosed in nine patients, all of whom had undergone uncomplicated phacoemulsification and intraocular lens implantation (PEA + IOL) in the affected eye on the same day at the same eye clinic. For prophylactic intracameral antibiotic injection, 0.5% moxifloxacin eye drop had been diluted to 50mL saline preoperatively and all the patients got the intracameral antibiotic injection from the same bottle at the end of the surgery. The baseline characteristics of the patients are shown in Table 1. Five types of IOL had been used in the patients.
Table 1.
Clinical characteristics of the patients with endophthalmitis.IV: intravenous, PO: per os.
| Case | Sex | Age | Right /Left |
IOL type | 1st VA | Interval cataract surgery to 1st PPV(day) | Interval 1st to following PPV(day) | Intravitreal antimicrovial/antibiotics at following PPV | Vitreous condensation | Culture | Final VA | Fosfluconazole IV (days) ※1 | Voriconazole PO 300mg/day (days) | IOL implant (interval from following PPV) | Following period (days) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 61 | L | ZXV300 | 0.8 | 18 | 11 | Fosfluconazole (20μg/mL) | (−) | negative | 1.2 | 5 | (−) | (+69) | 484 |
| 2 | F | 64 | R | ZXR00 | 0.3 | 18 | 9 | vancomycin+ ceftazidime |
(+) | negative | 0.9 | 10 | 15 | (+91) | 484 |
| 3 | M | 50 | L | ZXR00 | 0.03 | 18 | 20 | Fosfluconazole (20μg/mL) | (+) | negative | 0.7 | 8 | 8 | (−) | 470 |
| 4 | M | 74 | R | W60 | 0.4 | 24 | 24 | (−) | (+) | Fusarium. Oxysporum (hydatoid) | 1.2 | 10 | 184 | (+205) | 467 |
| 5 | F | 60 | L | ZCB00 | 0.7 | 21 | 27 | (−) | (+) | negative | 0.7 | 5 | 20 | (+198) | 463 |
| 6 | M | 66 | L | TFNT00 | 0.03 | 28 | 21 | (−) | (−) | Fusarium. Oxysporum (lens capsule) | 1 | 5 | 6 | (+90) | 459 |
| 7 | M | 77 | R | ZXR00 | 0.03 | 21 | 31 | (−) | (+) | negative | 1 | (−) | 19 | (+145) | 459 |
| 8 | F | 55 | R | TFNT50 | 0.4 | 24 | 31 | voriconazole (20μg/mL) | (+) | negative | 0.9 | (−) | 4 ※2 | (+156) | 459 |
| 9 | M | 77 | R | ZCB00 | 0.2 | 24 | N/A | N/A | (+) | N/A | N/A | N/A | N/A | (−) | 459 |
※1: Intravenous fosfluconazole therapy was performed with 800mg/day for the first two days, and with 400mg/day after that.
※2: In Case 8, the side effect of voriconazole was occurred 4 days after started oral voriconazole therapy. Instead, oral itraconazole therapy was performed for 13 days after that.
The mean age of the patients was 63.4 ± 8.5 years old (4 females and 5 males). The average interval from the cataract surgery to the onset of endophthalmitis was 21.5 ± 3.4 days. The patients presented with blurred vision (8 of 9 eyes), moderate iritis (all 9 eyes, 100%), biofilm on the surface of IOL (6 eyes, 67%), and hypopyon (3 eyes, 33%), with relatively mild eye redness.
All of the patients had undergone the first pars plana vitrectomy (PPV) to treat the endophthalmitis after the cataract surgery at the previous eye clinic. Considering the possibility of bacterial endophthalmitis, all the patients were treated by instillation of vancomycin and ceftazidime drops, without IOL removal. Intraocular 0.02 mg/mL vancomycin and 0.04 mg/mL ceftazidime were administered during vitrectomy in the balanced salt solution. However, as none of the eyes showed any apparent responses to the first PPV combined with antibiotic therapy, we performed a second PPV combined with antifungal drug therapy and IOL removal in all the patients, except one patient with chronic obstructive pulmonary disease who dropped out of the study because of poor general physical condition (Table 1, Case 9). Three patients received intravitreal antifungal therapy during the PPV and all the patients received topical administration of natamycin eye drops and oral voriconazole (VFEND®) or intravenous fosfluconazole (PRODIF®) treatment for 2–3 weeks postoperatively. Only one patient (Case 4) showed recurrence of the inflammation after the PPV with IOL removal. But soon after resuming oral voriconazole therapy, the inflammation disappeared. The final best corrected visual acuity was 1.2. Intrascleral IOL fixation has already been performed for 7 eyes and good visual acuity has been maintained (Table 1).
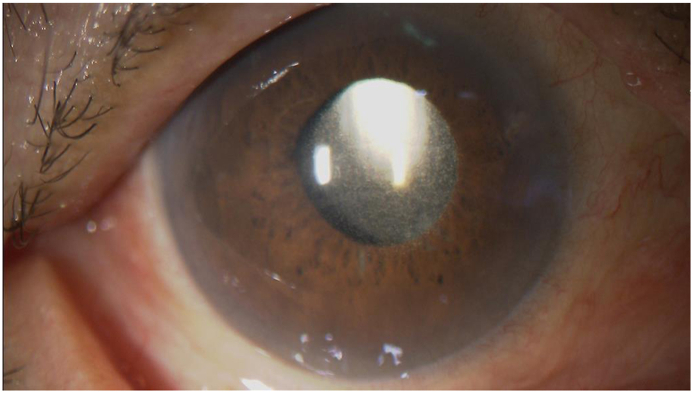
Fig. 1 shows a 74-year-old male patient with endophthalmitis in the right eye (Table 1, Case 4). He had undergone the first PPV 24 days after the cataract surgery at the previous eye clinic. However, recurrent endophthalmitis was observed and the patient was referred to our hospital. At his first visit to our hospital, the visual acuity in his right eye was 0.2. Slit-lamp examination showed biofilm formation on the surface of the IOL and the presence of angle hypopyon (Fig. 1A and B). During the re-PPV with IOL removal at our hospital, the biofilm was also observed to have spread to the vitreous cavity (Fig. 2A and B). IOL implantation was performed 205 days after re-PPV. The best corrected visual acuity was 1.2 at the final visit.
Fig. 1.
Slit lamp examination in patients with endophthalmitis.
Case 4 showed a relatively mild inflammation in the anterior chamber with mild redness and no pain 24 days after the first PPV. A slit-lamp examination revealed a biofilm on the surface of IOL (A). Moreover, angle hypopyon was observed in Case 4 (B).PPV: pars plana vitrectomy, IOL: intraocular lens.
Fig. 2.
Wide-angle fundus viewing during the second PPV.
Vitreous condensation was observed in the vitreous cavity during the second PPV in Case 4 (A). We removed it as much as possible, in addition to the IOL (B). PPV: pars plana vitrectomy, IOL: intraocular lens.
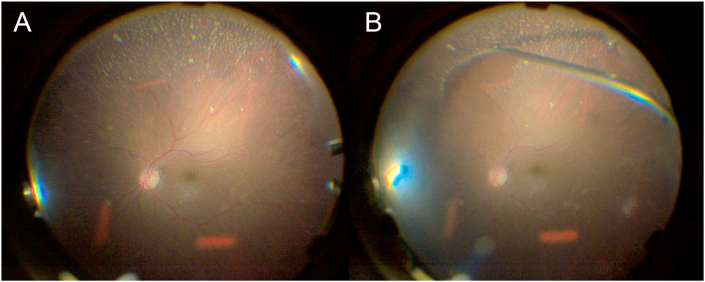
Fusarium oxysporum was isolated from one vitreous and one IOL sample (Fig. 3). MICs of antifungal drugs of two Fusarium Oxysporum strains revealed the same profile (Table 2): the identified strains were resistant to micafungin (MIC >16 mg/l), caspofungin (MIC >16 mg/l), flucytosine (MIC >64 mg/l), fluconazole (MIC >64 mg/l), itraconazole (MIC >8 mg/l) and voriconazole (MIC >8 mg/l), respectively, while they were sensitive to amphotericin B (MIC = 2 mg/l) and miconazole (MIC = 8 mg/l). In addition, the MIC of voriconazole was 2 mg/l when we changed the standard of MIC from IC100 to IC 50.
Fig. 3.
Fusarium oxysporum isolated from Case4
The fungus body, microconidia of single-celled and 2-celled oval shape. It was detected from hydatoid of case 4.
Table 2.
MICs of antifungal drugs of Fusarium Oxysporum strains determined by CLSI M38-A2 method.
| Anti-fungal drug | MIC (MEC) |
|---|---|
| micafungin | >16 |
| caspofungin | >16 |
| amphotericin B | 2 |
| flucytosine | >64 |
| fluconazole | >64 |
| itraconazole | >8 |
| voriconazole | >8 |
| miconazole | 4 |
MIC: Minimum inhibitory concentrations.
4. Discussion
4.1. Early intervention
Fusarium species are known as plant pathogens and mycotoxin producers.7 Fusarium oxysporum and Fusarium solani are the most common Fusarium species isolated from the eye. While cases of contact lens-related keratitis caused by Fusarium species are known, outbreaks of endophthalmitis caused by Fusarium species have rarely been reported.8 However, there are some reports of endophthalmitis caused by Fusarium species resulting in severe vision loss after cataract surgery.5,9 Buchta et al. reported that enucleation had to be performed in 10% of cases, and that the final visual acuity was 6/60 or worse in 85% of the patients. Late-onset fungal endophthalmitis after cataract surgery has been reported to be related to poor visual outcomes.10, 11, 12 However, even in an outbreak of early-onset endophthalmitis caused by Fusarium species reported by Cakir M et al.,13 the final visual acuity of the patients was poor (between light perception and 0.2), suggesting that proper management of fungal infection in the acute phase poses a challenge.
As compared to these reports, our current study demonstrated better visual outcomes, presumably because of correct diagnosis of the microorganism and early intervention. We suspected fungal infection based on the late-onset endophthalmitis which was refractory to intravitreal injection of antibacterial drugs during the first PPV surgery. Vancomycin is considered to be effective against gram-positive bacteria, while ceftazidime is a broad-spectrum antibiotic.14 Topical administration of vancomycin and ceftazidime is usually used to treat bacterial endophthalmitis, however in the present study, recurrence of endophthalmitis was observed in all the eyes within 20 days after the first PPV (Table 1). Second, topical administration of steroid exacerbated the inflammation in the patients with fungal endophthalmitis. In all patients, antibiotic eye drops and steroid eye drops had been used after the first PPV. We reinforced the topical steroid administration at the first visit of the patients to our hospital and confirmed exacerbation of inflammation in the anterior chamber and vitreous. Therefore, even before the causative pathogen was identified, we started the patients on antifungal therapy, earlier than in other reports, and as a result, obtained better visual acuity outcomes than in previous reports.
In the previous clinic, all the endophthalmitis patients underwent intracameral antibiotic injection, which were prepared before the surgery from the same bottle. As Cakir et al. reported,13 it was possible that the prepared solution might carry Fusarium in our cases with endophthalmitis, however the microbiologic investigation was not performed in the current study.
4.2. IOL and capsular removal
IOL removal was performed in all the patients in the current study, lending support to the idea that IOL explantation plays a critical role in the treatment of fungal endophthalmitis. Previous case reports have suggested that mycotic infection is localized to the capsular bag and IOL surface.15 In the present research, Fusarium oxysporum was isolated from the explanted IOL in one patient (Case 6). In all the eyes, the inflammation resolved completely after PPV combined with IOL removal and antifungal therapy.
Vinekar et al. previously reported six patients with postoperative fungal endophthalmitis who were refractory to conventional managements.16 They concluded that no recurrences were observed after final PPV with IOL removal, suggesting the effectiveness of IOL removal in managing postoperative fungal endophthalmitis.
Fungal endophthalmitis is often observed in clusters, often caused by contamination of the intraocular irrigating solution,17 IOLs,4,18,19 and ventilation systems.20 Fusarium species have been reported to cause biofilm formation around soft contact lenses.21 However, even though a few case series of fungal endophthalmitis after cataract surgery have been reported, biofilm formation has not yet been precisely evaluated to date. In the current study, we could not find the source of infection, however, the fungal infection was localized to the capsular bag and IOL surface, with formation of a biofilm, as shown in Fig. 1A. Thus, IOL removal combined with antifungal treatment led to successful resolution of Fusarium endophthalmitis in the current case series.
4.3. Antifungal drug selection
We fortunately succeeded in managing Fusarium oxysporum endophthalmitis by initiating antifungal drug therapy even before Fusarium oxysporum was identified as the causative organism. The Fusarium oxysporum strain identified in our study was resistant to most antifungal drugs, except amphotericin B and miconazole. However, when we used the IC 50 rather than the IC 100 standard, we found that the strain was sensitive to voriconazole.
Oral voriconazole was administered in 7 patients and intravitreal voriconazole in 1 patient, and 2 patients received intravitreal fosfluconazole. Local instillation of natamycin eye drops as antifungal therapy (4 times per day) was continued for at least 3 weeks in all patients. Topical natamycin and voriconazole cannot typically achieve high intraocular concentration for killing fungi. Intracameral antifungal treatment is only a part of therapy for exogenous fungal endophthalmitis, especially in patients associated with keratitis.
Previous reports suggested systemic voriconazole administration is effective to manage fungal keratitis and endophthalmitis.22,23 Therefore, systemic voriconazole administration was selected as an antifungal agent in the current case series although the MIC data suggested that the isolates were resistant to voriconazole but were sensitive to amphotericin B and miconazole. Considering the results of the MIC determinations, oral voriconazole therapy might have been insufficient for controlling the Fusarium oxysporum infection. If the MIC data were obtained at an earlier stage, drug selection might be more rational.
In conclusion, we successfully treated cases of Fusarium oxysporum endophthalmitis by vitrectomy combined with antifungal drug treatment. IOL removal might also be effective to manage Fusarium oxysporum endophthalmitis. The successful treatment is highly associated with removal of IOL/capsule, PPV, and intravitreal antifungal agents with/without systemic antifungal agents. Topical antibiotics could not be the important factors in treatment of endophthalmitis, unless it combined with keratitis. Since successful management is dependent on early diagnosis by identification of the causative fungal species, early intervention might be essential for good visual outcomes.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The following authors have no financial disclosures.
Acknowledgements
None.
References
- 1.Sunaric-Megevand G., Pournaras C.J. Current approach to postoperative endophthalmitis. Br J Ophthalmology. 1997;81(11):1006–1015. doi: 10.1136/bjo.81.11.1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wong T.Y., Chee S.P. The epidemiology of acute endophthalmitis after cataract surgery in an Asian population. Ophthalmology. 2004;111(4):699–705. doi: 10.1016/j.ophtha.2003.07.014. [DOI] [PubMed] [Google Scholar]
- 3.Aaberg T.M., Jr., Flynn H.W., Jr., Schiffman J., Newton J. Nosocomial acute-onset postoperative endophthalmitis survey. A 10-year review of incidence and outcomes. Ophthalmology. 1998;105(6):1004–1010. doi: 10.1016/S0161-6420(98)96000-6. [DOI] [PubMed] [Google Scholar]
- 4.Pettit T.H., Olson R.J., Foos R.Y., Martin W.J. Fungal endophthalmitis following intraocular lens implantation. A surgical epidemic. Arch Ophthalmol. 1980;98(6):1025–1039. doi: 10.1001/archopht.1980.01020031015002. [DOI] [PubMed] [Google Scholar]
- 5.Buchta V., Feuermannová A., Vasa M., et al. Outbreak of fungal endophthalmitis due to Fusarium oxysporum following cataract surgery. Mycopathologia. 2014;177(1-2):115–121. doi: 10.1007/s11046-013-9721-5. [DOI] [PubMed] [Google Scholar]
- 6.Kikuchi K., Watanabe A., Ito J., et al. Antifungal susceptibility of Aspergillus fumigatus clinical isolates collected from various areas in Japan. J Infect Chemother. 2014;20(5):336–338. doi: 10.1016/j.jiac.2014.01.003. https://pubmed.ncbi.nlm.nih.gov/24751235/ [DOI] [PubMed] [Google Scholar]
- 7.Magen N. Mycotoxin contamination of food in Europe: early detection an prevention strategies. Mycopathologia. 2006;162(3):245–253. doi: 10.1007/s11046-006-0057-2. [DOI] [PubMed] [Google Scholar]
- 8.Patel A., Hammersmith K. Contact lens-related microbial keratitis: recent outbreaks. Curr Opin Ophthalmol. 2008;19(4):302–306. doi: 10.1097/ICU.0b013e3283045e74. [DOI] [PubMed] [Google Scholar]
- 9.Gungel H., Eren H.M., Pinarci E.Y., et al. An outbreak of Fusarium solani endophthalmitis after cataract surgery in an eye training and research hospital in Istanbul. Mycoses. 2011;54(6):767–774. doi: 10.1111/j.1439-0507. [DOI] [PubMed] [Google Scholar]
- 10.Oxford K.W., Abbott R.L., Fung W.E., Ellis D.S. Aspergillus endophthalmitis after sutureless cataract surgery. Am J Ophthalmol. 1995;120(4):534–535. doi: 10.1016/s0002-9394(14. [DOI] [PubMed] [Google Scholar]
- 11.Hofling-Lima A.L., Freitas D., Fischman O., et al. Exophiala jeanselmei causing late endophthalmitis after cataract surgery. Am J Ophthalmol. 1999;128(4):512–514. doi: 10.1016/s0002-9394(99)00192-0. [DOI] [PubMed] [Google Scholar]
- 12.Hofling-Lima A.L., Freitas D., Oet al Fischman. Exophiala jeanselmei causing late endophthalmitis after cataract surgery. Am J Ophthalmol. 1999;128(4):512–514. doi: 10.1016/s0002-9394(99)00192-0. [DOI] [PubMed] [Google Scholar]
- 13.Cakir M., Imamoglu S., Cekic O., et al. An outbreak of early-onset endophthalmitis caused by Fusarium species following cataract surgery. Curr Eye Res. 2009;34(11):988–995. doi: 10.3109/02713680903254822. [DOI] [PubMed] [Google Scholar]
- 14.Kodati S., Eller A.W., Kowalski R.P. The susceptibility of bacterial endophthalmitis isolates to vancomycin, ceftazidime, and Amikacin: a 23 Year-review. Ophthalmol Retina. 2017;1(3):206–209. doi: 10.1016/j.oret.2016.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cusumano A., Busin M., Spitznas M. Mycotic infection of the capsular bag in postoperative endophthalmitis. J Cataract Refract Surg. 1991;17(4):503–505. doi: 10.1016/s0886-3350(13)80859-0. [DOI] [PubMed] [Google Scholar]
- 16.Vinekar A. Indian J Ophthalmol. 2014;62(2):136–140. doi: 10.4103/0301-4738.128588. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4005226/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stern W.H., Tamura E., Jacobs R.A., et al. Epidemic postsurgical Candida parapsilosis endophthalmitis. Clinical findings and management of 15 consecutive cases. Ophthalmology. 1985;92(12):1701–1709. doi: 10.1016/s0161-6420(85)34095-2. [DOI] [PubMed] [Google Scholar]
- 18.Theodre FH Etiology and diagnosis of fungal postoperative endophthalmitis. Ophthalmology. 1978;85(4):327–340. doi: 10.1016/s0161-6420(78)35661-x. [DOI] [PubMed] [Google Scholar]
- 19.O'Day D.M. Fungal endophthalmitis caused by Paecilomyces lilacinus after intraocular lens implantation. Am J Ophthalmol. 1977;83(1):130–131. doi: 10.1016/0002-9394(77)90206-9. [DOI] [PubMed] [Google Scholar]
- 20.Fridkin S.K., Kremer F.B., Bland L.A., et al. Acremonium kiliense endophthalmitis that occurred after cataract extraction in an ambulatory surgical center and was traced to an environmental reservoir. Clin Infect Dis. 1996;22(2):222–227. doi: 10.1093/clinids/22.2.222. [DOI] [PubMed] [Google Scholar]
- 21.Mukherjee P.K., Chandra J., Yu Changping, et al. Characterization of fusarium keratitis outbreak isolates: contribution of biofilms to antimicrobial resistance and pathogenesis. Invest Ophthalmol Vis Sci. 2012 Jul 3;53(8):4450–4457. doi: 10.1167/iovs.12-9848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hariprasad S.M., Mieler W.F., Lin T.K., Graybill J.R. Voriconazole in the treatment of fungal eye infections: a review of current literature. Br J Ophthalmol. 2008;92(7):871–878. doi: 10.1136/bjo.2007.136515. [DOI] [PubMed] [Google Scholar]
- 23.Troke P., Obenga G., Gaujoux T., et al. The efficacy of voriconazole in 24 ocular Fusarium infections. Infection. 2013;41(1):15–20. doi: 10.1007/s15010-012-0273-2. [DOI] [PubMed] [Google Scholar]