Abstract
Background
The purpose of this study was to evaluate the clinical and radiologic outcomes of reverse total shoulder arthroplasty (RTSA) using a small glenoid baseplate in patients with a small glenoid and to analyze the contributing factors to scapular notching.
Methods
A total of 71 RTSAs performed using a 25-mm baseplate were evaluated at a mean of 37.0 ± 3.3 months. Shoulder function was evaluated using American Shoulder and Elbow Surgeons (ASES) score, visual analog scale (VAS) for pain, Single Assessment Numeric Evaluation (SANE) for satisfaction, and active range of motion. Scapular neck angle (SNA), prosthesis-scapular neck angle (PSNA), peg glenoid rim distance (PGRD), and sphere bone overhang distance (SBOD) were measured to assess the effects on scapular notching.
Results
Shoulder function (ASES: 39.4 ± 13.8 preoperative vs. 76.2 ± 9.5 at last follow-up, p < 0.001), VAS for pain (6.1 ± 1.8 vs. 1.7 ± 1.4, p < 0.001), SANE for satisfaction (7.0 ± 11.8 vs. 83.4 ± 15.3, p < 0.001), and active forward flexion (115.6° ± 40.1° vs. 141.6° ± 17.2°, p < 0.001) were significantly improved. The mean diameter of the inferior glenoid circle was 26.0 ± 3.0 mm and the mean glenoid vault depth was 24.0 ± 4.5 mm. Scapular notching was found in 13 patients (18.3%) and acromial fracture in 2 patients (2.8%). There were no significant differences in preoperative SNA and PSNA at postoperative 3 years between patients with and without scapular notching (101.6° ± 10.5° and 110.8° ± 14.9° vs. 97.3° ± 13.3° and 104.9° ± 12.4°; p = 0.274 and p = 0.142, respectively). PGRD and SBOD were significantly different between patients with scapular notching and without scapular notching (24.8 ± 1.6 mm and 2.6 ± 0.5 mm vs. 21.9 ± 1.9 mm and 5.8 ± 1.9 mm; p < 0.001 and p < 0.001, respectively).
Conclusions
RTSA using a 25-mm baseplate in a Korean population who had relatively small glenoids demonstrated low complication rates and significantly improved clinical outcomes. Scapular notching can be prevented by proper positioning of the baseplate and glenosphere overhang using size-matched glenoid baseplates.
Keywords: Reverse total shoulder arthroplasty, Small glenoid, Size-matched baseplate, Clinical outcomes, Radiologic outcomes
The success of reverse total shoulder arthroplasty (RTSA) has led many surgeons to judge it as a safe and reliable procedure as the last treatment option for various shoulder diseases. Although RTSA has shown good clinical outcomes in the majority of patients, unsatisfactory improvement of symptoms and poor shoulder function after surgery still frequently occur.1) Preoperative factors, including age,2) sex,3,4,5) body mass index (BMI),6) diagnosis,7) and shoulder function,8) have been reported to relate to functional outcomes after RTSA. Intraoperative factors, such as component version,9) offset,10) and center of rotation, have been also associated with clinical outcomes and complications.
The characteristics of the glenoid baseplate is one of the intraoperative factors related to postoperative prognosis. The position of the glenoid baseplate has affected clinical outcomes such as range of motion (ROM) after RTSA.11,12) A mismatch in size between the glenoid and baseplate could cause difficulty in proper glenoid baseplate positioning and fixation especially for a small glenoid with a large baseplate during surgery.13) Generally, it is known that the size of the glenoid is related to ethnicity,14) sex,3,4,5) and height.15) Although a range of glenoid baseplate sizes are required to match individuals, commercially available baseplate sizes are limited.
The purpose of this study was to evaluate the clinical and radiologic outcomes of RTSA with a small glenoid component in patients who had a small glenoid and to analyze the contributing factors to scapular notching. We hypothesized that RTSA using a size-matched glenoid component would show satisfactory clinical outcomes and lower complications in Korean population.
METHODS
This study protocol was approved by the Institutional Review Board of Ewha Womans University Medical Center (No. ECT 13-38A-17), Kyung Hee University Hospital (No. KHUH 2013-10-502), Seoul National University Bundang Hospital (No. E-1309/218-001), Samsung Medical Center (No. 2013-05-063-004), and Hallym University Kangnam Sacred Heart Hospital (No. 2013-05-040). Five surgeons (YGR, JHO, JCY, KCN, and SJS) with an average of 6 years of orthopedic surgery experience assessed the patients and obtained written informed consent from all participants before surgery prospectively.
Patient Selection
We performed a prospective, multicenter case series study and included 87 patients who underwent RTSA using a 25-mm baseplate from December 2013 to January 2015 in five tertiary university hospitals. The surgical indications for RTSA were symptomatic shoulder disorders combined with rotator cuff deficiency that failed to receive the appropriate period of conservative treatment. The inclusion criteria were symptomatic irreparable massive rotator cuff tears and cuff tear arthropathy (CTA) and primary osteoarthritis (OA) with a full-thickness rotator cuff tear. Patients who visited the hospital for comprehensive assessment and follow-up more than 3 years after surgery were included. The exclusion criteria were the diagnosis of sequelae of septic shoulder, fracture, severe glenoid bone loss that needed augmentation, revision arthroplasty, and other arthritis such as rheumatoid arthritis and traumatic OA. Patients who were unable to return for comprehensive assessment and follow-up were excluded.
Surgical Technique and Rehabilitation
Before this prospective study, all surgeons controlled surgical indications and standardized the operation environment and techniques. Comprehensive reverse shoulder system (Zimmer Biomet, Warsaw, IN, USA) was performed in the beach chair position using a deltopectoral approach in all patients. After tenotomy of the subscapularis on the lesser tuberosity, the shoulder was dislocated. The humeral head was resected and the shaft was prepared using sequential reamers. We attempted to place the glenoid baseplate along the inferior margin of the glenoid by palpation. A 25-mm glenoid baseplate was inserted with a 10° inferior tilt with two compression screws in the superior and inferior holes and two locking screws in the anterior and posterior holes. A 2.5-mm inferior glenoid offset was applied and a 36-mm standard glenosphere was used in all patients. The humeral stem was inserted with a 20° retroversion. The subscapularis tendon was sutured using the transosseous technique during the last stage of the procedure when the subscapularis tendon was able to be repaired. All operation procedures were performed similarly by five expert orthopedic surgeons in each hospital (YGR, JHO, JCY, KCN, and SJS).
After surgery, patients were immobilized with an abduction brace for 4 weeks. Progressive passive and active ROM exercises were started at 4 weeks and shoulder muscle strengthening exercises were initiated at 12 weeks postoperatively. Return to physical activities began at 6 months postoperatively. All patients were treated using the same rehabilitation protocol.
Clinical and Radiological Evaluations
Each patient’s demography, including age, sex, affected site, and predominant arm, were assessed. BMI, preoperative diagnosis, and presence of pseudoparalysis were also evaluated. Subscapularis-repaired patients were recorded. American Shoulder and Elbow Surgeons (ASES) score, visual analog scale for pain, Single Assessment Numeric Evaluation score for satisfaction, and active ROM were evaluated preoperatively and postoperatively at 6 weeks, 6 months, 12 months, and annually thereafter. Active forward flexion and external rotation (ER) with the affected arm at the side were measured using a goniometer. Active internal rotation (IR) behind-the-back was measured at the most cephalad vertebral level reached by the tip of the extended thumb. The IR levels were converted into numerical data such as 0 for sacral level, 1 to 5 for L5 to L1, and 6 to 12 for T12 to T6, respectively. Preoperative and postoperative parameters were assessed by five shoulder fellowship-trained orthopedic surgeons (MSK, SWK, SCK, GWL, and YWK) who were not involved in this study.
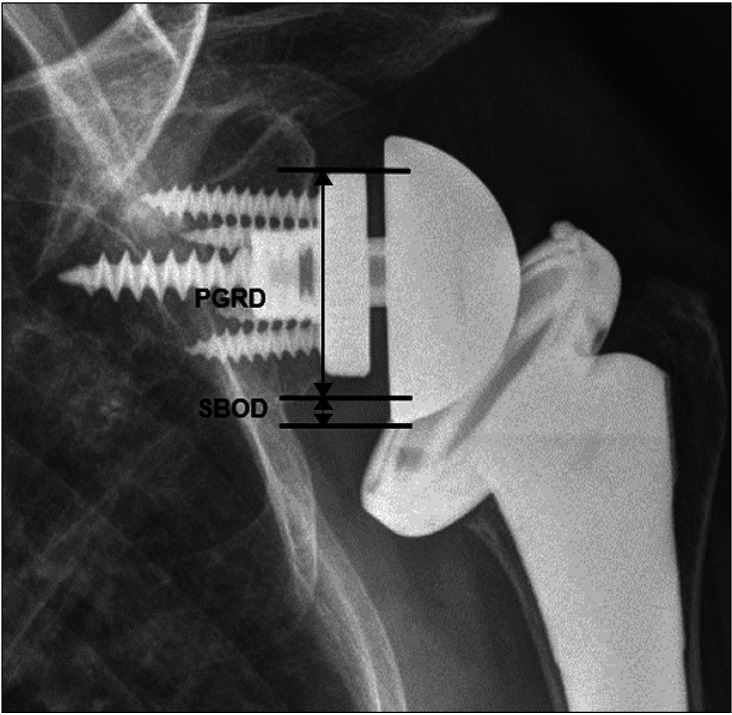
Radiologically, plain radiographs were obtained for all patients, including anteroposterior (AP), axial, and Grashey views. Three-dimensional (3D) computed tomography (CT) was performed preoperatively and at 3 years postoperatively. Using the 3D CT scan, the diameter of the glenoid and glenoid vault depth were measured preoperatively.13,16,17) The glenoid diameter was measured as the diameter of the inferior glenoid circle, which is the best fit circle along with anterior, posterior, and inferior margins of the glenoid on the en face 3D CT. The glenoid vault depth was measured by the perpendicular line from the glenoid surface midpoint to the endosteal wall on the axial CT.16,17) The midpoint of glenoid, which overlaps on the coronal, axial, and sagittal CT, was used as the glenoid surface for measuring vault depth. Preoperative scapular neck angle (SNA) and the postoperative prosthesis-scapular neck angle (PSNA) were assessed on the Grashey view at the final follow-up visit (Fig. 1).18) The SNA and PSNA are measured by the intersection of line AB and line BC. Point A is the most superior and lateral glenoid rim, and point B is the most inferior and lateral glenoid rim. Point C is medial to point B along with scapular neck. We evaluated the location of the baseplate peg according to whether the peg was inside the glenoid vault without anterior or posterior cortex penetration or with any cortex penetration on axial CT and whether it was centered or superior in position compared to the glenoid center on coronal CT (Fig. 2).17) The center was taken at the coronal cut using scout navigation based on axial cut in 3D CT. The peg glenoid rim distance (PGRD) and sphere bone overhang distance (SBOD) were assessed on the postoperative Grashey view at the final follow-up visit (Fig. 3).18,19)
Fig. 1. (A) Preoperative scapular neck angle (SNA) on the Grashey view. (B) Postoperative prosthesis-scapular neck angle (PSNA) on the Grashey view.
Fig. 2. Variable peg positions in the glenoid on axial and coronal computed tomography views at postoperative 3 years. The baseplate peg was inside the vault and center position (A), in the vault and superior position (B), and out of the vault and center position (C).
Fig. 3. Peg glenoid rim distance (PGRD) is the distance between the topmost point of a peg and the lowest point of the glenoid on the Grashey view. Sphere bone overhang distance (SBOD) is the distance between the lowest point of the glenoid and the lowest point of the glenosphere on the Grashey view.
Scapular notching was classified according to the Nerot-Sirveaux grading classification using a plain AP view at the last follow-up.20) Patients were divided into two groups based on the presence of scapular notching at the final follow-up to analyze the contributing factors for the occurrence of scapular notching. Preoperative magnetic resonance imaging was used to classify the subscapularis tendon tear based on the Lafosse classification.21) The preoperative and postoperative radiological evaluation was interpreted by a blinded musculoskeletal radiologist who was not involved in this study (JYH).
Statistical Analysis
All statistical analyses were conducted using IBM SPSS ver. 25.0 (IBM Corp., Armonk, NY, USA). Summary statistics are reported as means with standard deviations for continuous variables and the number of subjects with percentages for categorical variables. For continuous variables, Student t-test was used to compare mean differences between the two groups. For categorical variables, the chi-square test or Fisher’s exact test was used to test the proportion differences between the two groups. The statistical significance was set at p < 0.05.
RESULTS
Of the 87 patients, 12 patients were lost to follow-up, 3 patients had incomplete data due to complications (2 patients had revision surgeries due to infections; 1 patient had traumatic clavicle fracture) and 1 patient was deceased. Finally, 71 patients with RTSA were enrolled in this study. The average follow-up period was 37.0 ± 3.3 months (range, 36–51 months) after RTSA.
Preoperative patient demographic data are summarized in Table 1. The most common diagnosis was CTA and 26 patients (36.6%) demonstrated pseudoparalysis preoperatively. Shoulder function and ROM, except for active ER and IR, improved at the last follow-up (Table 2). The ASES score significantly improved by 93.4% (p < 0.001). Intraoperative subscapularis tendon repair was performed in 57 (80.3%) of total patients and did not show a significant difference in IR at the last follow-up (p = 0.067).
Table 1. Preoperative Patient Demographics.
| Characteristic | Patient (n = 71) | |
|---|---|---|
| Age (yr) | 72.0 ± 6.9 | |
| Sex (male : female) | 12:59 | |
| Body mass index (kg/m2) | 24.3 ± 3.3 | |
| Involved shoulder (right : left) | 52:19 | |
| Involvement of dominant side | 54 (76.1) | |
| Diagnosis (%) | ||
| Irreparable rotator cuff tear | 20 (28.2) | |
| Cuff tear arthropathy | 43 (60.6) | |
| OA with FTRCT | 8 (11.3) | |
| Pseudoparalysis | 26 (36.6) | |
| Subscapularis state before surgery | ||
| Less than Lafosse classification II | 45 | |
| More than Lafosse classification III | 26 | |
| Subscapularis repair | 57 (80.3) | |
Values are presented as mean ± standard deviation or number (%).
OA: osteoarthritis, FTRCT: full-thickness rotator cuff tear.
Table 2. Preoperative and Postoperative 3-Year Clinical Outcomes.
| Variable | Preoperative | Postoperative 3 yr | p-value |
|---|---|---|---|
| ASES score* | 39.4 ± 13.8 | 76.2 ± 9.5 | < 0.001 |
| VAS for pain* | 6.1 ± 1.8 | 1.7 ± 1.4 | < 0.001 |
| SANE for satisfaction* | 7.0 ± 11.8 | 83.4 ± 15.3 | < 0.001 |
| Active FF (°)* | 115.6 ± 40.1 | 141.6 ± 17.2 | < 0.001 |
| Active ER (°) | 48.6 ± 20.1 | 49.2 ± 16.9 | 0.808 |
| Active IR | 4.9 ± 2.8 | 5.0 ± 1.9 | 0.829 |
Values are presented as mean ± standard deviation.
ASES: American Shoulder and Elbow Surgeons, VAS: visual analog scale, SANE: Single Assessment Numeric Evaluation, FF: forward flexion, ER: external rotation, IR: internal rotation.
*Statistically significant difference.
The mean diameter of the inferior glenoid circle was 26.0 ± 3.0 mm (range, 20.9–37.5 mm) with 28.7 ± 2.9 mm in men and 25.3 ± 2.6 mm in women. The mean glenoid vault depth was 24.0 ± 4.5 mm (range, 10.9–36.1 mm) with 26.9 ± 4.5 mm in men and 23.3 ± 4.2 mm in women. The diameter of the glenoid inferior circle and glenoid vault depth were significantly different between men and women (p < 0.001 and p = 0.004, respectively). The baseplate pegs were located inside the glenoid vault in 55 patients (77.5%) and outside of the glenoid vault in 16 patients (22.5%). Among the patients whose pegs were inside the vault, 32 patients (58.2%) were positioned in the center, 21 patients (38.2%) in the superior, and 2 patients (3.6%) in the inferior. Among those whose pegs were out of the vault, pegs positioned in the center and anterior cortex penetration were found in 14 patients (87.5%), while posterior cortex penetration was found in 2 patients (12.5%). The mean preoperative SNA was 97.8° ± 12.1° and postoperative PSNA was 105.8° ± 12.7°. This finding significantly increased at the last follow-up (p < 0.001). The mean PGRD was 22.4 ± 2.2 mm and mean SBOD was 5.2 ± 2.2 mm.
Scapular notching occurred in 13 patients (18.3%). It was grade 1 in 9 patients (12.6%), grade 2 in 3 patients (4.2%), and grade 3 in 1 patient (1.4%). A comparison of clinical and radiologic outcomes between patients with and without notching are summarized in Table 3. No significant differences were found in the shoulder function and active ROM between patients with and without scapular notching at the last follow-up. There were no significant differences in preoperative SNA (p = 0.274) and postoperative PSNA (p = 0.142) between patients with and without scapular notching. However, PGRD was significantly longer and SBOD was shorter in patients with scapular notching (p < 0.001).
Table 3. Comparison of Preoperative and Postoperative Clinical and Radiologic Outcomes between Patients with Notching and without Notching.
| Variable | Notching | Without notching | p-value | |
|---|---|---|---|---|
| ASES score | ||||
| Preoperative | 35.6 ± 14.2 | 40.3 ± 13.6 | 0.278 | |
| Postoperative 3 yr | 72.0 ± 9.1 | 77.1 ± 9.5 | 0.081 | |
| p-value | < 0.001 | < 0.001 | ||
| VAS for pain | ||||
| Preoperative | 6.4 ± 1.8 | 6.0 ± 1.8 | 0.507 | |
| Postoperative 3 yr | 1.9 ± 1.0 | 1.4 ± 1.3 | 0.184 | |
| p-value | < 0.001 | < 0.001 | ||
| SANE for satisfaction | ||||
| Preoperative | 8.46 ± 15.7 | 6.72 ± 10.8 | 0.634 | |
| Postoperative 3 yr | 76.9 ± 25.6 | 84.8 ± 11.7 | 0.092 | |
| p-value | < 0.001 | < 0.001 | ||
| Active FF (°) | ||||
| Preoperative | 116.2 ± 37.3 | 115.5 ± 41.0 | 0.959 | |
| Postoperative 3 yr | 138.5 ± 14.1 | 143.2 ± 17.0 | 0.355 | |
| p-value | 0.048 | < 0.001 | ||
| Active ER (°) | ||||
| Preoperative | 49.6 ± 25.9 | 48.4 ± 18.8 | 0.841 | |
| Postoperative 3 yr | 50.8 ± 18.0 | 49.6 ± 15.6 | 0.808 | |
| p-value | 0.845 | 0.694 | ||
| Active IR (°) | ||||
| Preoperative | 4.5 ± 1.3 | 5.1 ± 2.9 | 0.453 | |
| Postoperative 3 yr | 4.6 ± 0.9 | 5.1 ± 2.0 | 0.372 | |
| p-value | 0.656 | 0.912 | ||
| Preoperative SNA (°) | 101.6 ± 10.5 | 97.3 ± 13.3 | 0.274 | |
| Postoperative 3 yr PSNA (°) | 110.8 ± 14.9 | 104.9 ± 12.4 | 0.142 | |
| p-value | 0.002 | < 0.001 | ||
| PGRD (mm)* | 24.8 ± 1.6 | 21.9 ± 1.9 | < 0.001 | |
| SBOD (mm)* | 2.6 ± 0.5 | 5.8 ± 1.9 | < 0.001 | |
Values are presented as mean ± standard deviation.
ASES: American Shoulder and Elbow Surgeons, VAS: visual analog scale, SANE: Single Assessment Numeric Evaluation, FF: forward flexion, ER: external rotation, IR: internal rotation, SNA: scapular neck angle, PSNA: prosthesis-scapular neck angle, PGRD: peg rim glenoid distance, SBOD: sphere bone overhang distance.
*Significantly different between the two groups.
Besides scapular notching, the only other postoperative complication was an acromial fracture in 2 patients (2.8%). Instability, baseplate failure, implant loosening, neurologic deficit, or intraoperative glenoid fractures were not found.
DISCUSSION
Satisfactory short-term clinical outcomes, including improved shoulder function and ROM restoration, were obtained after RTSA using 25-mm baseplates in patients with small glenoids. The rate of scapular notching was low and no baseplate-related complications occurred. The development of scapular notching was closely related to the overhang of the glenosphere in this study.
During the RTSA procedure, the insertion of the baseplate and the glenosphere is considered to be one of the most challenging procedures. With regard to the baseplate size, it is difficult to insert the baseplate when using a standard 29-mm size baseplate relative to a small glenoid without the likelihood of causing complications during the operation.13) Moon et al.22) investigated the glenoid size in a Korean population using CT scans and found that the AP diameter averaged 26.1 ± 2.4 mm and the superoinferior diameter was 31.2 ± 2.3 mm. Similar results were obtained in our study using the mean diameter of the inferior glenoid circle measured on CT scans. However, the mean glenoid width in Caucasians has been reported to be 28 ± 4.9 mm, which is much larger than that found in Asian populations.14) There have been several reported clinical and radiological complications resulting from the size mismatch between the glenoid and the baseplate.13) In this study, we used a 25-mm baseplate (a size that not only matched individuals with a small glenoid but also improved the surgical field of view with less invasiveness) and increased size matched implant-bone contact area. No complications related to the baseplate, including baseplate loosening, fracture, or disengagement of the glenosphere from the baseplate, were found.
For a small glenoid, it is very important that the baseplate is placed inside the glenoid vault for a solid fixation and to avoid complications. In a study by Ji et al.,13) when a large baseplate was inserted into a small glenoid, there was a chance to redrill the central peg holes because initial fixation was not positioned at the center of the glenoid due to the limited surgical field of view, which was one of the causes of glenoid fractures. In addition, firm fixation of compression screws in the baseplate was possible in only 60% of patients due to the relatively small anterior or posterior glenoid bone stock.13) In this situation, glenoid wear may result in a decreased contact surface area and bony support to the baseplate, which may weaken the initial stability of the glenoid component fixation. In our study, 77.5% of the baseplates were successfully inserted inside the glenoid vault and firm fixation of the baseplate was achieved. Therefore, our study demonstrated no major complications related to the glenoid baseplate and glenosphere when using a size-matched baseplate.
A biomechanical study proved that a 25-mm baseplate showed less micromotion and greater impingement-free ROM than a 29-mm baseplate.23) The length of the superior, anterior, and posterior screws were longer and the remaining glenoid bone stock was larger when a 25-mm baseplate was used compared to a 29-mm baseplate. These support the use of a small baseplate on a small glenoid, which allows for sufficient bone stock and increases stability.
Several studies demonstrated that overhang reduces the development of scapular notching.24,25) Using a large baseplate for a small glenoid requires more reaming to achieve adequate inferior tilt and insufficient bone stock for initial correct positioning results in insufficient overhang and inferior tilt than a small baseplate. Ji et al.13) reported that scapular notching was found in 30% of patients who used a 29-mm baseplate along with a 36-mm glenosphere despite placing the baseplate in the inferior position with a 10° inferior tilt on the glenoid. Scapular notching occurred in 18.3% of patients enrolled in our study. It is assumed that the low occurrence of scapular notching compared to other studies is due to the increased overhang and appropriate positioning using 25-mm baseplates. In addition, the humeral stem design also has an effect on the occurrence of scapular notching. Athwal and Faber25) showed scapular notching in 46% of patients who used a 25-mm baseplate and 36-mm glenosphere BIO-RSA (Aequlais Reversed; Tornier, Bloomington, MN, USA). However, they used an inlay type humeral stem with 155° inclination. This medialized humeral stem might cause a higher incidence of scapular notching even with a small glenoid baseplate. A postoperative increase in PSNA has also been reported to be associated with scapular notching.18) However, increased PSNA after RTSA had no relationship in the prevention of scapular notching in our study. Even if the same PSNA is shown, the positional relationship of the inferior tilt of the arm, scapular neck, and glenoid component can be reflected differently. This implies that the PSNA increase alone is not associated with scapular notching. Many other factors such as the optimization of the bone-component contact surface, stable fixation, and component position could influence scapular notching.24,26) A PGRD of more than 22 mm has yielded a sensitivity of 82% and a specificity of 79% for scapular notching.18) Previous studies revealed that increased PGRD and decreased SBOD were associated with scapular notching.19,26) Our study also demonstrated that PGRD and SBOD were significantly different between patients with and without scapular notching. By using a size-matched baseplate, the glenoid component could be easily positioned in the appropriate location to increase overhang and reduce the occurrence of scapular notching.
The relationship between scapular notching and clinical outcomes is still a topic of debate. Scapular notching is known to decrease clinical outcomes and lead to mechanical implant failure.18,20,27) Mollon et al.27) reported that patients with scapular notching had significantly lower postoperative active ROM and deteriorated shoulder function than patients without scapular notching at a mean follow-up of 38 months. Several studies reported worse clinical outcomes of scapular notching at longer follow-ups.18,20) On the other hand, some authors demonstrated that scapular notching was not related to clinical outcomes.7,28) Wall et al.7) reported that scapular notching occurred in 50.1% of enrolled patients; however, no differences were found in functional scores and active ROM at the mean follow-up of 39.9 months. In our study, no significant effects of scapular notching on clinical outcomes were found at the mean follow-up of 37 months. Functional outcomes and postoperative active ROM improved regardless of the occurrence of notching. Further long-term follow-up is needed to investigate the effects of scapular notching after RTSA.
This study has several limitations. First, this study is not a comparative study with regard to different baseplate sizes. A comparative study between small- and large-sized baseplates is necessary to investigate whether different outcomes exist. However, we described the differences in the clinical outcomes by indirectly comparing with a previous study that contained a large baseplate component. Second, our interests are only restricted to a small glenoid population. The effects of the glenoid size on clinical and radiological outcomes in a large glenoid population need to be investigated. Third, inhomogenous patient groups such as CTA and OA could affect clinical and radiological outcomes. Fourth, the complication rates and functional outcomes after RTSA might be influenced by the follow-up period. A long-term follow-up is needed to evaluate complications and clinical outcomes with size-matched baseplates. Fifth, a multicenter study can produce several biases, including assessments of clinical outcomes, radiologic evaluations, surgeon-dependent technical factors, and rehabilitation despite standardization of the protocol. Finally, we performed the study using a single implant design. To generalize the results of our study, further evaluation using other implant designs is necessary.
RTSA using a 25-mm baseplate in a Korean population who had relatively small glenoids demonstrated low complication rates and significantly improved clinical outcomes. A firm fixation of the baseplate in the appropriate position increased baseplate stability by using size-matched baseplates. Scapular notching can be prevented by proper positioning of the baseplate and glenosphere overhang using size-matched glenoid baseplates.
ACKNOWLEDGEMENTS
We appreciate Sang Woo Kim, MD (Department of Orthopaedic Surgery, Seoul National University Bundang Hospital), Su Cheol Kim, MD (Department of Orthopaedic Surgery, Samsung Medical Center), Geun Woo Lee (Department of Orthopaedic Surgery, Hallym University Kangnam Sacred Heart Hospital), Young Wan Ko (Department of Orthopaedic Surgery, Kyung Hee University Hospital), Ji Young Hwang, MD (Department of Radiology, Ewha Womans University Seoul Hospital) for preoperative and postoperative parameter assessment.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Carducci MP, Zimmer ZR, Jawa A. Predictors of unsatisfactory patient outcomes in primary reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2019;28(11):2113–2120. doi: 10.1016/j.jse.2019.04.009. [DOI] [PubMed] [Google Scholar]
- 2.Hartzler RU, Steen BM, Hussey MM, et al. Reverse shoulder arthroplasty for massive rotator cuff tear: risk factors for poor functional improvement. J Shoulder Elbow Surg. 2015;24(11):1698–1706. doi: 10.1016/j.jse.2015.04.015. [DOI] [PubMed] [Google Scholar]
- 3.Wong SE, Pitcher AA, Ding DY, et al. The effect of patient gender on outcomes after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26(11):1889–1896. doi: 10.1016/j.jse.2017.07.013. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz DG, Cottrell BJ, Teusink MJ, et al. Factors that predict postoperative motion in patients treated with reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(9):1289–1295. doi: 10.1016/j.jse.2013.12.032. [DOI] [PubMed] [Google Scholar]
- 5.Piponov HI, Savin D, Shah N, et al. Glenoid version and size: does gender, ethnicity, or body size play a role? Int Orthop. 2016;40(11):2347–2353. doi: 10.1007/s00264-016-3201-8. [DOI] [PubMed] [Google Scholar]
- 6.Beck JD, Irgit KS, Andreychik CM, Maloney PJ, Tang X, Harter GD. Reverse total shoulder arthroplasty in obese patients. J Hand Surg Am. 2013;38(5):965–970. doi: 10.1016/j.jhsa.2013.02.025. [DOI] [PubMed] [Google Scholar]
- 7.Wall B, Nove-Josserand L, O’Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89(7):1476–1485. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]
- 8.Jeon YS, Rhee YG. Factors associated with poor active anterior elevation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2018;27(5):786–793. doi: 10.1016/j.jse.2017.10.027. [DOI] [PubMed] [Google Scholar]
- 9.Favre P, Sussmann PS, Gerber C. The effect of component positioning on intrinsic stability of the reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2010;19(4):550–556. doi: 10.1016/j.jse.2009.11.044. [DOI] [PubMed] [Google Scholar]
- 10.Gutierrez S, Greiwe RM, Frankle MA, Siegal S, Lee WE., 3rd Biomechanical comparison of component position and hardware failure in the reverse shoulder prosthesis. J Shoulder Elbow Surg. 2007;16(3 Suppl):S9–S12. doi: 10.1016/j.jse.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 11.Li X, Knutson Z, Choi D, et al. Effects of glenosphere positioning on impingement-free internal and external rotation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22(6):807–813. doi: 10.1016/j.jse.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 12.Gutierrez S, Levy JC, Frankle MA, et al. Evaluation of abduction range of motion and avoidance of inferior scapular impingement in a reverse shoulder model. J Shoulder Elbow Surg. 2008;17(4):608–615. doi: 10.1016/j.jse.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 13.Ji JH, Jeong JY, Song HS, et al. Early clinical results of reverse total shoulder arthroplasty in the Korean population. J Shoulder Elbow Surg. 2013;22(8):1102–1107. doi: 10.1016/j.jse.2012.07.019. [DOI] [PubMed] [Google Scholar]
- 14.Cabezas AF, Krebes K, Hussey MM, et al. Morphologic variability of the shoulder between the populations of North American and East Asian. Clin Orthop Surg. 2016;8(3):280–287. doi: 10.4055/cios.2016.8.3.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cabezas AF, Gutierrez S, Teusink MJ, et al. Kinematic impact of size on the existing glenohumeral joint in patients undergoing reverse shoulder arthroplasty. Clin Biomech (Bristol Avon) 2014;29(6):622–628. doi: 10.1016/j.clinbiomech.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 16.Poon PC, Ting FS. A 2-dimensional glenoid vault method for measuring glenoid version on computed tomography. J Shoulder Elbow Surg. 2012;21(3):329–335. doi: 10.1016/j.jse.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 17.Oh JH, Lee S, Rhee SM, Jeong HJ, Yoo JC. Rationale for small glenoid baseplate: position of central cage within glenoid vault (Exactech® Equinoxe® reverse system) Clin Shoulder Elb. 2019;22(1):24–28. doi: 10.5397/cise.2019.22.1.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Simovitch RW, Zumstein MA, Lohri E, Helmy N, Gerber C. Predictors of scapular notching in patients managed with the Delta III reverse total shoulder replacement. J Bone Joint Surg Am. 2007;89(3):588–600. doi: 10.2106/JBJS.F.00226. [DOI] [PubMed] [Google Scholar]
- 19.Duethman NC, Aibinder WR, Nguyen NT, Sanchez-Sotelo J. The influence of glenoid component position on scapular notching: a detailed radiographic analysis at midterm follow-up. JSES Int. 2020;4(1):144–150. doi: 10.1016/j.jses.2019.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff: results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86(3):388–395. doi: 10.1302/0301-620x.86b3.14024. [DOI] [PubMed] [Google Scholar]
- 21.Lafosse L, Jost B, Reiland Y, Audebert S, Toussaint B, Gobezie R. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am. 2007;89(6):1184–1193. doi: 10.2106/JBJS.F.00007. [DOI] [PubMed] [Google Scholar]
- 22.Moon YR, Ha SH, Noh KH. Normal glenoid size of the korean in 7th and 8th decades. Clin Shoulder Elbow. 2008;11(1):37–40. [Google Scholar]
- 23.Chae SW, Kim SY, Lee H, Yon JR, Lee J, Han SH. Effect of baseplate size on primary glenoid stability and impingement-free range of motion in reverse shoulder arthroplasty. BMC Musculoskelet Disord. 2014;15:417. doi: 10.1186/1471-2474-15-417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Wilde LF, Poncet D, Middernacht B, Ekelund A. Prosthetic overhang is the most effective way to prevent scapular conflict in a reverse total shoulder prosthesis. Acta Orthop. 2010;81(6):719–726. doi: 10.3109/17453674.2010.538354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Athwal GS, Faber KJ. Outcomes of reverse shoulder arthroplasty using a mini 25-mm glenoid baseplate. Int Orthop. 2016;40(1):109–113. doi: 10.1007/s00264-015-2945-x. [DOI] [PubMed] [Google Scholar]
- 26.Choi CH, Kim SG, Lee JJ, Kwack BH. Comparison of clinical and radiological results according to glenosphere position in reverse total shoulder arthroplasty: a short-term follow-up study. Clin Orthop Surg. 2017;9(1):83–90. doi: 10.4055/cios.2017.9.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mollon B, Mahure SA, Roche CP, Zuckerman JD. Impact of scapular notching on clinical outcomes after reverse total shoulder arthroplasty: an analysis of 476 shoulders. J Shoulder Elbow Surg. 2017;26(7):1253–1261. doi: 10.1016/j.jse.2016.11.043. [DOI] [PubMed] [Google Scholar]
- 28.Sadoghi P, Leithner A, Vavken P, et al. Infraglenoidal scapular notching in reverse total shoulder replacement: a prospective series of 60 cases and systematic review of the literature. BMC Musculoskelet Disord. 2011;12:101. doi: 10.1186/1471-2474-12-101. [DOI] [PMC free article] [PubMed] [Google Scholar]