Abstract
Aim
This current study examined the mediation roles of burnout and job stress in the association between fear of COVID‐19 and mental health among emergency nurses.
Design
Cross‐sectional survey.
Methods
A total of 516 emergency nurses with a mean age of 41.18 (SD = 8.24), mostly females (76.16%) and married (78.9%) responded to measures on fear of COVID‐19, burnout, job stress and mental health between 15 September and 7 November 2020.
Results
There was a significantly direct effect between (a) fear of COVID‐19 and mental health, (b) fear of COVID‐19 and mediators (burnout and job stress) and (c) mediators (burnout and job stress) and mental health. Also, there was a significantly indirect effect between fear of COVID‐19 and mental health through job stress, burnout or both.
Conclusions
Fear of COVID‐19 directly and indirectly influenced the mental health of emergency nurses. Therefore, hospital authorities should provide sufficient resources to allay the fears of nurses during this COVID‐19 pandemic period.
Keywords: burnout, fear of COVID‐19, job stress, mediation, mental health, nurse
1. INTRODUCTION
The emergence of COVID‐19 and its enervating effects on lifestyle (Balanzá–Martínez et al., 2020; Lippi et al., 2020; Van Lancker & Parolin, 2020), health (Ahorsu, Imani, et al., 2020; Ahorsu, Lin & Pakpour et al., 2020; Fazeli et al., 2020) and economies around the world (Gössling et al., 2020; Nicola et al., 2020) are very disturbing. With the increasing COVID‐19 cases (over 234 million), severities and fatalities (over 4.8 million) worldwide as of 5th October 2021 (World Health Organisation, 2021), emergency department (especially if they oversee the treatment of COVID‐19 cases) staff members may get overwhelmed by the influx of COVID‐19 cases which directly increases their workload. This is especially a challenging issue among emergency nurses as they have to triage all patients including COVID‐19 cases within a limited time period. This consequently increases their job stress as they have to deal with triaging and treating different cases with limited personal protective equipment (PPEs) and within a limited time period (Al Thobaity & Alshammari, 2020; Shoja et al., 2020; Wang et al., 2020).
2. BACKGROUND
Recent studies have indicated that frontline workers which include emergency nurses have increased job stress as they have added tasks and new protocols which must be strictly adhered to due to the COVID‐19 pandemic (Al Thobaity & Alshammari, 2020; Shoja et al., 2020; Wang et al., 2020). Other studies which reported reduced non‐COVID‐19 case visits to the emergency department indicated that the workload remained unchanged or increased due to changes and special extra tasks that needs to be performed by the emergency nurses (Shoja et al., 2020; Sung et al., 2020; Zhan et al., 2020). An increased workload/job stress may have cascading adverse effects on relationships, appropriate service delivery and overall job performance among nurses (Cui et al., 2021; Gualano et al., 2021; Zare et al., 2021). The situation may even be worse when most nurses fear COVID‐19 due to the limited PPEs, and other uncertainties surrounding COVID‐19, and unavailability of a cure or definite treatment (Al Thobaity & Alshammari, 2020; Çınar et al., 2021; Zare et al., 2021).
One of the most challenging aspects of COVID‐19 is the indefinite transmission medium which includes but not limited to respiratory droplets during close face‐to‐face spread by asymptomatic, presymptomatic and symptomatic carriers (Wiersinga et al., 2020). This situation is especially challenging for the emergency staff members because they are charged with overseeing the treatment of COVID‐19 cases and more specifically emergency nurses as they have to attend to trauma‐related and other life‐death cases that have unknown COVID‐19 status. This increases their chance of contracting COVID‐19 and hence increasing their fear of COVID‐19. The fear of COVID‐19 combined with limited PPEs and inadequate information among the nurses may hinder effective delivery of quality services to patients as the nurses may have decreased job satisfaction, increased psychological distress, performance, and increased organizational and professional turnover intentions (Al Thobaity & Alshammari, 2020; De los Santos & Labrague, 2021; Labrague & de Los Santos, 2021; Rajabimajd et al., 2021; Shoja et al., 2020; Yayla & Eskici İlgin, 2021). Apart from the poor delivery of quality services, job stress in tandem with fear of contracting COVID‐19 may cause burnout and mental health challenges among the nurses (Hu et al., 2020; Zare et al., 2021).
Burnout, syndrome of three feelings (emotional exhaustion, depersonalization and low personal accomplishment; Maslach et al., 2018), among nurses is mostly due to factors such as excessive workload, low rewards and poor relationships with colleagues (Dall'Ora et al., 2020) which unfortunately may further lead to other mental health challenges if not properly dealt with (Hu et al., 2020; Shoja et al., 2020). That is, with the increasing COVID‐19 cases in the hospital, inadequate resources and support structures to cope with the influx of cases, nurses may be prone to burnout (physical and emotional exhaustion, depersonalization, and low personal accomplishment). The continuous burnout among nurses may deteriorate their health and specifically their mental health which may affect their performance at work (Hamed et al., 2020; Zeng et al., 2020). That is, burnout has strongly been associated with reduced job performance, poor quality of care, poor patient safety, adverse events, patient negative experience, medical errors, infections, patient falls and intention to leave (Al Sabei et al., 2020; Dall'Ora et al., 2020; Kwon et al., 2021) This leaves a huge financial burden and serious administrative challenges for the health authorities (managers and directors). For instance, the estimated financial cost for burnout‐related turnover among US physicians and nurses was $17 and $14 billion, respectively, per annum (National Taskforce for Humanity in Healthcare, 2018). In other reports, the financial burden of burnour and/or mental health among nurses or healthcare workers are in several billions dollars per anum (Kline & Lewis, 2019; Medibank, 2011; Perry et al., 2015; Torjesen, 2018). Yet, no known study has examined the mediating roles of burnout and job stress in the association between fear of COVID‐19 and mental health.
2.1. Research question
Hence, and considering current COVID‐19 situation, this current study aimed to examine the mediation roles of burnout and job stress in the association between fear of COVID‐19 and mental health (see Figure 1). The findings will be beneficial to hospital authorities and health professionals themselves by providing information on how to handle their workplace challenges and their mental health appropriately. It will also serve as a background for future clinical studies among health professionals during this COVID‐19 pandemic period.
FIGURE 1.
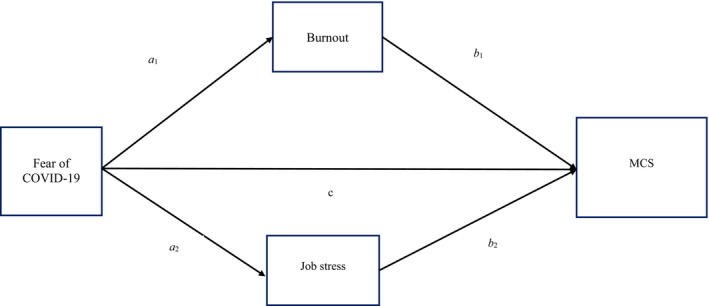
Mediation model with burnout and Job stress as proposed mediators of the effect of fear of COVID‐19 on emergency nursing staff's mental health. Note: Age, sex, years of experience and marital status were adjusted for the model. MCS, mental component summary
3. THE STUDY
3.1. Design
This study used the cross‐sectional design and with the help of a survey to gather the needed data from emergency nursing staff.
3.2. Method
3.2.1. Participants and procedure
This study recruited 516 emergency nursing staff between 15 September and 7 November 2020 from 18 hospitals in Qazvin (Iran) using a list of nursing staffs who were working at emergency departments as prepared by Treatment Affairs (Qazvin, Iran). An online questionnaire was sent by SMS to 800 staff members and 516 (response rate of 64.5%) of them agreed to participate in the study. Inclusion criteria were as follows: educated in nursing, working at emergency department and provided online consent form for participation.
3.2.2. Measures
Fear of COVID‐19
The emergency nurses' fear of COIVD‐19 was assessed using the fear of COVID‐19 scale. This scale was developed by Ahorsu, Lin, Imani, et al. (2020). It is made up of seven items which are rated on a five‐point Likert‐type scale response format (strongly agree = 5 to strongly disagree = 1). The total score which was generated by adding all the responses ranged from 7 to 35. Hence, higher scores indicated greater fear of COVID‐19. The Persian version was used for this study with an acceptable internal consistency (α = 0.82; Ahorsu, Lin, Imani, et al., 2020).
Job stress
The emergency nurses' occupational stress was assessed using the occupational stress inventory (revised) which was developed by Osipow (1998). It is made up of six subscales (role overload, role insufficiency, role ambiguity, role boundary, responsibility and physical environment) with 10 items per each subscale. It is rated on a five‐point Likert‐type scale response format (1 = never, 2 = occasionally, 3 = sometimes, 4 = usually and 5 = most of the time) with a higher subscale score depicting a greater level of role stressor. The Persian version was used for this study with an acceptable internal consistency (α = 0.83; Sharifian et al., 2006).
Burnout
The nurses' burnout was assessed using the Maslach Burnout Inventory Human Services Survey for Medical Professionals, fourth edition (MBI‐HSS MP, 4th Ed.) developed by Maslach et al. (2018). It is made up of 22 items with frequency rating choices of Never (0), A few times a year or less (1), Once a month or less (2), A few times a month (3), Once a week (4), A few times a week (5) or Every day (6) that covers 3 areas (Emotional Exhaustion, EE; Depersonalization, DP; and low sense of Personal Accomplishment, PA). Hence, three MBI scale scores were calculated and interpreted separately for each nurse. The Persian version of MBI showed acceptable Cronbach's alpha coefficients (0.71–0.85) from a previous study Moalemi et al. (2018). Moreover, the Cronbach's alpha coefficients of MBI calculated using the present study's data were acceptable with the range between 0.73 and 0.83.
Mental health
The nurses' mental health was assessed using the 12‐Item Short Form Health Survey (SF‐12) developed by Ware Jr et al. (1996). Specifically, this study used the Mental Component Summary (MCS) of the scale. The Persian version was used for this study with acceptable Cronbach's alpha coefficient of above 0.82 (Montazeri et al., 2011; Pakpour et al., 2011).
3.3. Data analysis
The demographic information of the participants was presented using descriptive statistics, including mean (SD) and frequency (percentage). Then, Pearson's correlation was applied to examine the bivariate correlations among the studied variables. After the confirmation of the associations (as shown by the Pearson correlation) among the studied variables, structural equation modelling using full information maximum likelihood estimator was used to examine the proposed mediation model (Figure 1). More specifically, fear of COVID‐19 was the independent variable, job stress and burnout were the mediators, and mental health was the outcome variable. Age, sex, years of clinical experience and marital status were adjusted for the mediation model. Moreover, bootstrapping method with a total of 5,000 resamples was used to examine the mediation effect.
Several fit indices, including comparative fit index (CFI) (Bentler, 1990), Tucker–Lewis index (TLI) (Tucker & Lewis, 1973), standardized root mean square residual (SRMR) and root mean square error of approximation (RMSEA) (Joreskog & Sorbom, 1981), were used to examine whether the mediation model is supported. Values of CFI and TLI > 0.9 together with SRMR and RMSEA < 0.08 indicate a supported mediation model (Hyland et al., 2014). The sample size was also calculated using the proposed mediation model. The mediation model contains 23 degrees of freedom, with the set‐up of type I error at 0.05, power at 0.9, null RMSEA at 0 and alternative RMSEA at 0.05, the desired sample size for the mediation model is around 480 (Preacher & Coffman, 2006). All statistical analyses were conducted using SPSS version 25 and Amos version 24.
4. RESULTS
A total of 516 emergency nurses with a mean age of 41.18 (SD = 8.24) years were used for this study. They were mostly females (n = 393; 76.16%), married (n = 407; 78.9%) with an average of 12.46 (SD = 10.35) years of working experience. These statistics is almost comparable to 2,500 nurses working in Qazvin province of whom 1,998 (79.92%) are females with a mean age of 37.56 years. Further details on the demographic information were shown in Table 1.
TABLE 1.
Participants characteristics (N = 516)
| Mean ± SD or n (%) | |
|---|---|
| Age (year) | 41.18 ± 8.24 |
| Gender (female) | 393 (76.16%) |
| Years of experience | 12.46 ± 10.35 |
| <5 | 159 (30.8%) |
| 5–9 | 107 (20.7%) |
| ≥10 | 250 (48.4%) |
| Marital status | |
| Single | 88 (17.1%) |
| Married | 407 (78.9%) |
| Divorced/widowed | 21 (4.1%) |
Table 2 shows the Pearson r correlation matrix between fear of COVID‐19, job stress, medical professionals' burnout (emotional exhaustion, depersonalization and low sense of personal accomplishment) and mental health. All the correlation coefficients (r = 0.12–0.68) were significant (p < .05).
TABLE 2.
Pearson's correlation matrix of the variables of interest
| Variables | Fear of COVID−19 | Job stress | EE | PA | DP | MCS |
|---|---|---|---|---|---|---|
| Fear of COVID−19 a | — | 0.269** | 0.242** | −0.295** | 0.231** | −0.271** |
| Job stress b | — | 0.118** | −0.188** | 0.125** | −0.477** | |
| EE c | — | −0.534** | 0.682** | −0.174** | ||
| PA c | — | −0.578* | 0.194** | |||
| DP c | — | −0.121** | ||||
| MCS d | — | |||||
| Mean ± SD | 21.45 ± 6.13 | 163.39 ± 68.80 | 4.30 ± 1.26 | 4.73 ± 1.29 | 2.24 ± 1.49 | 40.08 ± 30.60 |
Abbreviations: DP, depersonalization; EE, emotional exhaustion; PA, personal accomplishment.
*p‐value < .05; **p‐value < .01.
Assessed using Fear of COVID‐19 Scale (FCV‐19S).
Assessed using Osipow occupational stress inventory.
Assessed using Maslach Burnout Inventory Human Services Survey for Medical Professionals (MBI‐HSS MP).
Assessed using the 12‐Item Short Form Health Survey (SF‐12).
Table 3 shows that there was a significant direct effect of fear of COVID‐19 on burnout (β = 0.311, 95% CI = 0.031–0.07), job stress (β = 2.69, 95% CI = 2.024–4.075) and mental health (β = 0.131, 95% CI = −1.101–−0.171); a significant direct effect of burnout on mental health (β = −0.80, 95% CI = −4.175–−0.667); and a significant direct effect of job stress on mental health (β = −0.430; 95% CI = −0.238–−0.161). Also, burnout (β = −0.085, 95% CI = −0.192–−0.054), job stress (β = −0.116, 95% CI = −0.844–−0.373) and job stress and burnout (sequential mediators; β = −0.140, 95% CI = −1.010–−0.472) were found to be significant mediators in the association between fear of COVID‐19 and mental health. In all, there was a significant total effect of fear of COVID‐19 on mental health of emergency nurses (β = −0.271, 95% CI = −1.801–−0.931). Moreover, the entire mediation model is supported by the satisfactory fit indices: χ2 = 70.307, df = 23; p < .001; CFI = 0.982, TLI = 0.961, SRMR = 0.0440, RMSEA = 0.064, 90% CI = [0.034, 0.095].
TABLE 3.
Direct, indirect and total effects in the structural equation model testing relations among emergency nurses
| Path | B (SE) | β | 95% CI | |
|---|---|---|---|---|
| LL | UL | |||
| Direct effects | ||||
| Fear of COVID−19→Burnout | 0.051 (0.010) | 0.311*** | 0.031 | 0.070 |
| Fear of COVID−19→Job stress | 2.970 (0.518) | 0.269*** | 2.024 | 4.075 |
| Fear of COVID−19→MCS | −0.652 (0.200) | −0.131*** | −1.101 | −0.171 |
| Burnout→MCS | −2.421 (0.893) | −0.80** | −4.175 | −0.667 |
| Job stress→MCS | −0.194 (0.019) | −0.430*** | −0.238 | −0.161 |
| Indirect effects | ||||
| Fear of COVID−19→ Burnout→MCS | −0.123 (0.035) | −0.085** | −0.192 | −0.054 |
| Fear of COVID−19→Job Stress→MCS | −0.576 (0.112) | −0.116*** | −0.844 | −0.373 |
| Fear of COVID−19→Job Stress, Burnout →MCS | −0.699 (0.128) | −0.140*** | −1.010 | −0.472 |
| Total effects | ||||
| Fear of COVID−19→MCS | −1.351 (0.220) | −0.271*** | −1.801 | −0.931 |
Age, sex, years of experience, and marital status were included as control variables in the structural equation model.
Abbreviations: B, unstandardized path coefficient; 95% CI, 95% confidence interval of unstandardized path coefficient; LL, lower limit of 95% CI; MCS, mental component summary; SE, standard error; β, standardized path coefficient; UL, upper limit of 95% CI.
*p < .05; ** p < .01; *** p < .001.
5. DISCUSSION
This cross‐sectional survey study examined the mediation roles of burnout and job stress in the association between fear of COVID‐19 and mental health. The correlation results revealed that fear of COVID‐19 related positively to job stress, emotional exhaustion and depersonalization but related negatively to personal accomplishment and mental health with small effect size for all these relationships (Cohen, 1988, 1992) which is similar to previous studies (Ahorsu, Imani, et al., 2020; Ahorsu, Lin, & Pakpour, 2020; Hu et al., 2020). This indicates that when emergency nurses' fear of COVID‐19 increases their stress at the workplace, emotional exhaustion and depersonalization symptoms may also increase and vice versa. However, when nurses' fear of COVID‐19 increases, their sense of personal accomplishment and mental health decreases and vice versa. The positive relationships between job stress, emotional exhaustion and depersonalization indicate that when nurses' stress on the job increases their burnout (emotional exhaustion and depersonalization) symptoms also increase (and vice versa). The negative relationships between job stress, sense of personal accomplishment and mental health indicate that when nurses' stress on the job increases, sense of personal accomplishment and mental health decrease and vice versa. The negative relationships between burnout (emotional exhaustion and depersonalization) symptoms and mental health indicate that the higher the nurses' experience burnout symptoms the poorer their mental health. The positive relationship between sense of personal accomplishment and mental health indicates that as nurses' sense of personal accomplishment increases their mental health also increase and vice versa. Similarly, previous studies have reported an association between fear of COVID‐19, mental health, burnout and stress (Ahorsu, Imani, et al., 2020; Ahorsu, Lin, & Pakpour, 2020; Hu et al., 2020).
These interrelationships (fear of COVID‐19, job stress, burnout and mental health) were further explained by the mediation analysis. The mediation results indicated that there were direct significant associations between (a) fear of COVID‐19 and mental health, (b) fear of COVID‐19 and mediators (job stress and burnout) and (c) mediators (job stress and burnout) and mental health. These findings strengthen the earlier relationships observed between the variables. That is, fear of an infectious disease such as COVID‐19 may significantly influence nurses' burnout, job stress or both which may influence their mental health as reported in previous studies (Ahorsu, Imani, et al., 2020; Ahorsu, Lin, & Pakpour, 2020; Hu et al., 2020; Shoja et al., 2020). Additionally, the mediating effects observed indicated an indirect effect of fear of COVID‐19 on mental health through burnout, job stress and job stress‐burnout with the strongest mediator effect being for the sequential job stress‐burnout, job stress and finally burnout. This indicates that fear of COVID‐19 indirectly influences the mental health of emergency nurses through job stress, burnout or both. In other words, fear of COVID‐19 significantly influenced emergency nurses' burnout and job stress positively which then influenced their mental health negatively. Hence, fear of COVID‐19, directly and indirectly, influences the mental health of emergency nurses.
These findings are very important as emergency nurses are mostly at the frontline of health services attending to all kinds of conditions including COVID‐19. This importance is against the backdrop that their burnout and compromised mental health situation may affect their job performance (e.g. quality of care, poor patient safety, adverse events, patient negative experience and medical errors) and, consequently, detrimental to their patients' life (Al Thobaity & Alshammari, 2020; De los Santos & Labrague, 2021; Labrague & de Los Santos, 2021; Shoja et al., 2020; Yayla & Eskici İlgin, 2021). Furthermore, the financial implications associated with the consequences of burnout and/or mental illness (absenteeism, sickness presenteeism, job performance, medical errors, turnover intention and job satisfaction) among nurses alone are significant enough to threaten the smooth running of the health service (Kline & Lewis, 2019; Medibank, 2011; National Taskforce for Humanity in Healthcare, 2018; Perry et al., 2015; Torjesen, 2018). This present study has provided significant evidence that fear of COVID‐19 may influence these negative events. Hence, hospital authorities (e.g. administrators and medical directors) should endeavour to provide adequate PPEs and other necessary resources needed to allay the fears of nurses in treating all kinds of patients during this COVID‐19 (or other infectious condition) pandemic period.
5.1. Limitation
This study had limitations. Only emergency nurses were used in this study; hence, the findings may be extended to nurses at the frontline of infectious diseases such as COVID‐19 but not necessarily to other departmental staffs in a hospital. Also, as different countries implemented different policies in managing COVID‐19, there may be the need replication of this study in order to holistically ascertain how the variables used in this study relate to other countries. This study used a cross‐sectional design which limits the cause and effect relationships between the variables and so readers should be cautious in overextending the findings of this study. In addition, self‐report measures were used in this study for gathering the data; hence, there may be biases such as social desirability. However, the use of appropriate administering procedures and the robustness of the psychometric properties for these measures suggest that the data are valid and trustworthy to an appreciable degree.
5.2. Conclusion
This cross‐sectional survey study revealed that fear of COVID‐19 may, directly and indirectly (through burnout, job stress or both), influence the mental health of emergency nurses negatively. This is a very important finding not only because of COVID‐19 but that it also pertains to the mental health of nurses and the life of patients they are treating. This finding suggests that fear of COVID‐19 and other fatal infectious condition for that matter influences the mental health of nurses. Hence, hospital authorities such as administrators and medical directors should provide enough resources to allay the fears of nurses in their line of duty during this COVID‐19 pandemic period. Replication of this study may be needed to ascertain how the variables used in this study differed from other countries.
CONFLICT OF INTERESTS
None.
ETHICAL STATEMENT
All participants provided written informed consent before study participation. The study protocol was approved by the Ethics Committee of Qazvin University of Medical Sciences (n. IR.QUMS.REC.1399.351) and conformed to the requirements of the Declaration of Helsinki. Approval from the participating institutions was also obtained. The data of the participants were kept confidential and used for academic research only.
ACKNOWLEDGEMENTS
The authors wish to thank all the participants who took part in this study.
Ahorsu, D. K. , Lin, C.‐Y. , Marznaki, Z. H. , & Pakpour, A. H. (2022). The association between fear of COVID‐19 and mental health: The mediating roles of burnout and job stress among emergency nursing staff. Nursing Open, 9, 1147–1154. 10.1002/nop2.1154
Funding information
None
DATA AVAILABILITY STATEMENT
The authors elect not to share data. Research data are not shared for ethical and confidentiality reasons.
REFERENCES
- Ahorsu, D. K. , Imani, V. , Lin, C.‐Y. , Timpka, T. , Broström, A. , Updegraff, J. A. , Årestedt, K. , Griffiths, M. D. , & Pakpour, A. H. (2020). Associations between fear of COVID‐19, mental health, and preventive behaviours across pregnant women and husbands: An actor‐partner interdependence modelling. International Journal of Mental Health and Addiction, 1–15. 10.1007/s11469-020-00340-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahorsu, D. K. , Lin, C.‐Y. , Imani, V. , Saffari, M. , Griffiths, M. D. , & Pakpour, A. H. (2020). The Fear of COVID‐19 Scale: Development and Initial Validation. International Journal of Mental Health and Addiction, 1–9, 10.1007/s11469-020-00270-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahorsu, D. K. , Lin, C.‐Y. , & Pakpour, A. H. (2020). The association between health status and insomnia, mental health, and preventive behaviors: The mediating role of fear of COVID‐19. Gerontology and Geriatric Medicine, 6, 2333721420966081. 10.1177/2333721420966081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Sabei, S. D. , Labrague, L. J. , Miner Ross, A. , Karkada, S. , Albashayreh, A. , Al Masroori, F. , & Al Hashmi, N. (2020). Nursing work environment, turnover intention, job burnout, and quality of care: The moderating role of job satisfaction. Journal of Nursing Scholarship, 52(1), 95–104. 10.1111/jnu.12528 [DOI] [PubMed] [Google Scholar]
- Al Thobaity, A. , & Alshammari, F. (2020). Nurses on the Frontline against the COVID‐19 Pandemic: An Integrative Review. Dubai Medical Journal, 3(3), 87–92. 10.1159/000509361 [DOI] [Google Scholar]
- Balanzá–Martínez, V. , Atienza–Carbonell, B. , Kapczinski, F. , & De Boni, R. B. (2020). Lifestyle behaviours during the COVID‐19–time to connect. Acta Psychiatrica Scandinavica, 141, 399–400. 10.1111/acps.13177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler, P. M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238–246. 10.1037/0033-2909.107.2.238 [DOI] [PubMed] [Google Scholar]
- Çınar, D. , Kılıç Akça, N. , Zorba Bahçeli, P. , & Bağ, Y. (2021). Perceived stress and affecting factors related to COVID‐19 pandemic of emergency nurses in Turkey. Journal of Nursing Management, 29, 1916–1923. 10.1111/jonm.13329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Routledge. [Google Scholar]
- Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155–159. 10.1037/0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- Cui, S. , Jiang, Y. , Shi, Q. , Zhang, L. , Kong, D. , Qian, M. , & Chu, J. (2021). Impact of COVID‐19 on anxiety, stress, and coping styles in nurses in emergency departments and fever clinics: A cross‐sectional survey. Risk Management and Healthcare Policy, 14, 585–594. 10.2147/RMHP.S289782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dall’Ora, C. , Ball, J. , Reinius, M. , & Griffiths, P. (2020). Burnout in nursing: A theoretical review. Human Resources for Health, 18(1), 41. 10.1186/s12960-020-00469-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De los Santos, J. A. A. , & Labrague, L. J. (2021). The impact of fear of COVID‐19 on job stress, and turnover intentions of frontline nurses in the community: A cross‐sectional study in the Philippines. Traumatology, 27(1), 52–59. 10.1037/trm0000294 [DOI] [Google Scholar]
- Fazeli, S. , Mohammadi Zeidi, I. , Lin, C.‐Y. , Namdar, P. , Griffiths, M. D. , Ahorsu, D. K. , & Pakpour, A. H. (2020). Depression, anxiety, and stress mediate the associations between internet gaming disorder, insomnia, and quality of life during the COVID‐19 outbreak. Addictive Behaviors Reports, 12, 100307. 10.1016/j.abrep.2020.100307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gössling, S. , Scott, D. , & Hall, C. M. (2020). Pandemics, tourism and global change: A rapid assessment of COVID‐19. Journal of Sustainable Tourism, 29(1), 1–20. 10.1080/09669582.2020.1758708 [DOI] [Google Scholar]
- Gualano, M. R. , Sinigaglia, T. , Lo Moro, G. , Rousset, S. , Cremona, A. , Bert, F. , & Siliquini, R. (2021). The burden of burnout among healthcare professionals of intensive care units and emergency departments during the COVID‐19 pandemic: A systematic review. International Journal of Environmental Research and Public Health, 18(15), 8172. 10.3390/ijerph18158172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamed, R. A. , Abd Elaziz, S. Y. , & Ahmed, A. S. (2020). Prevalence and predictors of burnout syndrome, post‐traumatic stress disorder, depression, and anxiety in nursing staff in various departments. Middle East Current Psychiatry, 27(1), 36. 10.1186/s43045-020-00044-x [DOI] [Google Scholar]
- Hu, D. , Kong, Y. , Li, W. , Han, Q. , Zhang, X. , Zhu, L. X. , Wan, S. W. , Liu, Z. , Shen, Q. U. , Yang, J. , He, H.‐G. , & Zhu, J. (2020). Frontline nurses' burnout, anxiety, depression, and fear statuses and their associated factors during the COVID‐19 outbreak in Wuhan, China: A large‐scale cross‐sectional study. EClinicalMedicine, 24, 100424. 10.1016/j.eclinm.2020.100424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland, P. , Shevlin, M. , Adamson, G. , & Boduszek, D. (2014). The organization of irrational beliefs in posttraumatic stress symptomology: Testing the predictions of REBT theory using structural equation modelling. Journal of Clinical Psychology, 70(1), 48–59. 10.1002/jclp.22009 [DOI] [PubMed] [Google Scholar]
- Joreskog, K. , & Sorbom, D. (1981). LISREL V: Analysis of linear structural relationships hy the method of maximum likelihood. National Educational Resources. [Google Scholar]
- Kline, R. , & Lewis, D. (2019). The price of fear: Estimating the financial cost of bullying and harassment to the NHS in England. Public Money & Management, 39(3), 166–174. 10.1080/09540962.2018.1535044 [DOI] [Google Scholar]
- Kwon, C. Y. , Lee, B. , Kwon, O. J. , Kim, M. S. , Sim, K. L. , & Choi, Y. H. (2021). Emotional labor, burnout, medical error, and turnover intention among South Korean nursing staff in a University hospital setting. International Journal of Environmental Research and Public Health, 18(19), 10111. 10.3390/ijerph181910111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrague, L. J. , & de Los Santos, J. A. A. (2021). Fear of Covid‐19, psychological distress, work satisfaction and turnover intention among frontline nurses. Journal of Nursing Management, 29(3), 395–403. 10.1111/jonm.13168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippi, G. , Henry, B. M. , & Sanchis‐Gomar, F. (2020). Physical inactivity and cardiovascular disease at the time of coronavirus disease 2019 (COVID‐19). European Journal of Preventive Cardiology, 27(9), 906–908. 10.1177/2047487320916823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslach, C. , Jackson, S. , & Leiter, M. (2018). Maslach burnout inventory manual, 4th ed. Mind Garden Inc. [Google Scholar]
- Medibank . (2011). Sick at Work: The cost of presenteeism to your business and the economy. In Economic Modelling of the Cost of Presenteeism in Australia: 2011 Update (Medibank, KPMG Econtech). http://www.medibank.com.au/Client/Documents/Pdfs/sick_at_work.pdf [Google Scholar]
- Moalemi, S. , Kavosi, Z. , Beygi, N. , Deghan, A. , Karimi, A. , & Parvizi, M. M. (2018). Evaluation of the Persian Version of Maslach Burnout Inventory‐Human Services Survey among Iranian nurses: Validity and reliability. Galen Medical Journal, 7, e995. 10.22086/gmj.v0i0.995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montazeri, A. , Vahdaninia, M. , Mousavi, S. J. , Asadi‐Lari, M. , Omidvari, S. , & Tavousi, M. (2011). The 12‐item medical outcomes study short form health survey version 2.0 (SF‐12v2): A population‐based validation study from Tehran, Iran. Health and Quality of Life Outcomes, 9, 12. 10.1186/1477-7525-9-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Taskforce for Humanity in Healthcare (2018). The business case for humanity in healthcare. https://www.vocera.com/public/pdf/NTHBusinessCase_final003.pdf
- Nicola, M. , Alsafi, Z. , Sohrabi, C. , Kerwan, A. , Al‐Jabir, A. , Iosifidis, C. , Agha, M. , & Agha, R. (2020). The socio‐economic implications of the coronavirus pandemic (COVID‐19): A review. International Journal of Surgery, 78, 185–193. 10.1016/j.ijsu.2020.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osipow, S. H. (1998). Occupational Stress Inventory‐Revised Edition (OSI‐R): Professional manual. Psychological Assessment Resources Inc. [Google Scholar]
- Pakpour, A. H. , Nourozi, S. , Molsted, S. , Harrison, A. P. , Nourozi, K. , & Fridlund, B. (2011). Validity and reliability of short form‐12 questionnaire in Iranian hemodialysis patients. Iranian Journal of Kidney Disease, 5(3), 175–181. [PubMed] [Google Scholar]
- Perry, L. , Lamont, S. , Brunero, S. , Gallagher, R. , & Duffield, C. (2015). The mental health of nurses in acute teaching hospital settings: A cross‐sectional survey. BMC Nursing, 14(1), 1–8. 10.1186/s12912-015-0068-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher, K. J. , & Coffman, D. L. (2006). Computing power and minimum sample size for RMSEA [Computer software]. http://quantpsy.org/ [Google Scholar]
- Rajabimajd, N. , Alimoradi, Z. , & Griffiths, M. D. (2021). Impact of COVID‐19‐related fear and anxiety on job attributes: A systematic review. Asian Journal of Social Health and Behavior, 4(2), 51–55. 10.4103/shb.shb_24_21 [DOI] [Google Scholar]
- Sharifian, S. A. , Aminian, O. , Kiyani, M. , Barouni, S. H. , & Amiri, F. (2006). The evaluation of the degree of occupational stress and factors influencing it in forensic physicians working in Legal Medicine Organization in Tehran ‐ Autumn of 2005. Scientific Journal of Forensic Medicine, 12(3), 144–150. [Google Scholar]
- Shoja, E. , Aghamohammadi, V. , Bazyar, H. , Moghaddam, H. R. , Nasiri, K. , Dashti, M. , Choupani, A. , Garaee, M. , Aliasgharzadeh, S. , & Asgari, A. (2020). Covid‐19 effects on the workload of Iranian healthcare workers. BMC Public Health, 20(1), 1636. 10.1186/s12889-020-09743-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung, C.‐W. , Lu, T.‐C. , Fang, C.‐C. , Huang, C.‐H. , Chen, W.‐J. , Chen, S.‐C. , & Tsai, C.‐L. (2020). Impact of COVID‐19 pandemic on emergency department services acuity and possible collateral damage. Resuscitation, 153, 185–186. 10.1016/j.resuscitation.2020.06.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torjesen, I. (2018). Bullying and harassment cost NHS over £2bn a year, study suggests. BMJ, 363, k4463. 10.1136/bmj.k4463 [DOI] [PubMed] [Google Scholar]
- Tucker, L. R. , & Lewis, C. (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38(1), 1–10. 10.1007/BF02291170 [DOI] [Google Scholar]
- Van Lancker, W. , & Parolin, Z. (2020). COVID‐19, school closures, and child poverty: A social crisis in the making. The Lancet Public Health, 5(5), e243–e244. 10.1016/S2468-2667(20)30084-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, J. , Zong, L. , Zhang, J. , Sun, H. , Harold Walline, J. , Sun, P. , Xu, S. , Li, Y. , Wang, C. , Liu, J. , Li, F. , Xu, J. , Li, Y. I. , Yu, X. , & Zhu, H. (2020). Identifying the effects of an upgraded ‘fever clinic’ on COVID‐19 control and the workload of emergency department: Retrospective study in a tertiary hospital in China. British Medical Journal Open, 10(8), e039177. 10.1136/bmjopen-2020-039177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware, J. E. Jr , Kosinski, M. , & Keller, S. D. (1996). A 12‐Item Short‐Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34(3), 220–233. 10.1097/00005650-199603000-00003 [DOI] [PubMed] [Google Scholar]
- Wiersinga, W. J. , Rhodes, A. , Cheng, A. C. , Peacock, S. J. , & Prescott, H. C. (2020). Pathophysiology, transmission, diagnosis, and treatment of Coronavirus disease 2019 (COVID‐19): A review. JAMA, 324(8), 782–793. 10.1001/jama.2020.12839 [DOI] [PubMed] [Google Scholar]
- World Health Organisation . (2021). COVID‐19 Weekly Epidemiological Update on COVID‐19—5 October 2021. https://www.who.int/publications/m/item/weekly‐epidemiological‐update‐on‐covid‐19‐‐‐5‐october‐2021 [Google Scholar]
- Zare, S. , Kazemi, R. , Izadi, A. , & Smith, A. (2021). Beyond the outbreak of COVID‐19: Factors affecting burnout in nurses in Iran. Annals of Global Health, 87(1), 51. 10.5334/aogh.3190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yayla, A. , & Eskici İlgin, V. (2021). The relationship of nurses' psychological well‐being with their coronaphobia and work‐life balance during the COVID‐19 pandemic: A cross‐sectional study. Journal of clinical nursing, 30(21‐22), 3153–3162. 10.1111/jocn.15783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng, L.‐N. , Zhang, J.‐W. , Zong, Q.‐Q. , Chan, S.‐C. , Browne, G. , Ungvari, G. S. , Chen, L.‐G. , & Xiang, Y.‐T. (2020). Prevalence of burnout in mental health nurses in China: A meta‐analysis of observational studies. Archives of Psychiatric Nursing, 34(3), 141–148. 10.1016/j.apnu.2020.03.006 [DOI] [PubMed] [Google Scholar]
- Zhan, Y. , Ma, S. , Jian, X. , Cao, Y. , & Zhan, X. (2020). The current situation and influencing factors of job stress among frontline nurses assisting in Wuhan in fighting COVID‐19. Frontiers in Public Health, 8, 579866. 10.3389/fpubh.2020.579866 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors elect not to share data. Research data are not shared for ethical and confidentiality reasons.


