Abstract
Aim
This study aimed to assess the timely initiation of Antenatal Care and associated factors among pregnant women attending antenatal care clinics at Bahir Dar city, North West Ethiopia.
Design
Institutional based cross‐sectional study was conducted.
Methods
Data were collected on 804 pregnant women from 20 February to 27 March 2017. Face‐to‐face interview through systematic sampling technique was applied. Binary logistic regression was performed using SPSS software version 21, and the level of significance of association was determined at p‐value <0.05 with a 95%confidence interval.
Results
This study identified 44.2% of pregnant women started their first antenatal care timely. Maternal secondary and above level of education AOR = 7.07 (95% CI: 4.41, 11.35)), age at first pregnancy >18 years AOR = 2.77 (95% CI: 1.39, 5.57) and having information about the correct time of ANC booking AOR = 3.14 (95% CI: 1.67, 5.92) were significantly associated with timely commencement to first antenatal care.
Keywords: antenatal care, Ethiopia, pregnant, timely initiation, women
1. INTRODUCTION
Despite several efforts were made to reveres maternal mortality, it is still a global public health problem. Globally, maternal mortality rate is 216 per 100,000 live births with a large proportion of deaths due to early preventable or treatable pregnancy and childbirth complications, 99% of maternal deaths occur in low‐ and middle‐income countries, in sub‐Saharan African countries alone accounting for 66% (Alkema et al., 2016; World Health Organization (WHO) 2016a, 2016bWorld Health Organization). Ethiopia is one of the Sub‐Saharan African countries with the highest maternal mortality ratio (MMR) which is 412 maternal deaths per 100,000 live births (Central Statistical Agency (CSA) [Ethiopia] and ICF, 2016).
Antenatal care (ANC) is one of the key strategies designed to minimize such devastating conditions through providing health promotion, prevention, detection and treatment care for pregnancy‐related illnesses (World Health Organization (WHO), 2015). Moreover, ANC can reduce both maternal and neonatal mortality by detecting at‐risk pregnancy and initiating appropriate medical and educational interventions towards the risk associated (Federal Ministry of Health (FMOH) [Ethiopia], 2010; World Health Organization (WHO), 2015; World Health Organization (WHO) 2016a, 2016b).
Therefore, timely ANC initiation is crucial for better woman's pregnancy experience and the successes of maternal and neonatal health by early identifying, managing and preventing any problems through supplementation of micronutrients like iron and folic acid, screening of infection (e.g. HIV, Syphilis and hepatitis) and health promotion (Furness et al., 2011; Prathapan et al., 2011; Roth et al., 2011; Ӧzge et al., 2017; World Health Organization (WHO) 2016a, 2016b).
Many maternal and prenatal deaths occur in women who have not received timely, inadequate and no utilization of ANC (Oyerinde, 2013). Early antenatal care attendance during the first three months of gestation plays a major role in detecting and treating complications that occur during pregnancy (Abou‐Zahr and Wardlaw, 2003).
According to the World Health Organization (WHO) Focus antenatal care model recommendation, all pregnant ladies are better to start their first antenatal care (ANC) booking within the first trimester of pregnancy (8–12 weeks) (World Health Organization (WHO) (2002)).
The global existing evidence displays that the prevalence of early booking of antenatal care visits was 43%. There is a high inconsistency between regions, which showed that in developed 85%, in developing below 45% and in sub‐Sahara region less than 25% (Moller et al., 2017). Despite focussed ANC is provided for free in Ethiopia, according to the Ethiopian demographic health survey (EDHS) 2016 report, only 20% of women received their first ANC during the first trimester of pregnancy(Central Statistical Agency (CSA) [Ethiopia] and ICF, 2016). Different literature conducted in Ethiopia also revealed that the prevalence of early booking of ANC visits ranges from 13.2% to 65.6% (Amtatachew et al., 2013; Belayneh et al., 2014; Ewnetu et al., 2015; Feleke et al., 2015; Tolera Gudissa et al., 2015; Yilal, 2015).
Studies conducted in developing countries showed that age of the mother, residence, educational status of the mother, occupation, age at first marriage, age at first pregnancy, parity, planned or wanted pregnancy, information access, advised booking within 12weeks and decision‐making power were factors for early ANC booking (Adekanle & Isawumi, 2008; Ajayi & Osakine, 2013; Amtatachew et al., 2013; Banda et al., 2012; Belayneh et al., 2014; Erica, 2012; Ewnetu et al., 2015; Feleke et al., 2015; Ochako & Girchuhi, 2016; Tolera Gudissa et al., 2015; Yilal, 2015). This study aims to assess the prevalence and factors associated with early antenatal care initiation of mothers in health facilities.
1.1. Study setting
This study was conducted at Bahir Dar City public health institutions, Bahir Dar, North West Ethiopia. Bahir Dar City is the capital city of the Amhara National Regional State, located Northwest at about 565 km far from the capital city of Ethiopia (Addis Ababa). In the city, there are Ten Governmental health centres, one regional referral hospital, One District Hospital owned by the government. In the city, there are 17 urban administrative kebeles and 4 special towns. Based on the 2007 National Census conducted by the Central Statistical Agency of Ethiopia (CSA) projection, the town has a total population of 848,596.
2. METHODS
2.1. Study design and period
An institutional‐based cross‐sectional study was carried out in Bahir Dar City public health institutions from 20 February to 27 March 2017, North West Ethiopia.
2.1.1. Study participants
All pregnant mothers who visited public ANC clinics were included in the study, whereas pregnant mothers who were seriously ill and in labour pain were excluded.
In this study, timely visit of first antenatal care is visiting ANC service before and at 12 complete gestational weeks (World Health Organization (WHO) 2016a, 2016b).
2.2. Sample size determination and techniques
The sample size for the study was calculated by using single population proportion formula with the following assumptions. By assuming a margin of error of 5%, 95% CI (1.96), proportion =47.7% (Belayneh et al., 2014), non‐response rate of 5% and by considering design effect 2, the final sample size was found to be 804.
Generally, a multi‐stage sampling technique was used. Then, seven governmental health institutions were selected out of 12 governmental health institutions randomly by lottery method. The average daily client flow receiving the service in the selected health institutions was taken from the registry book. According to the expected number of women in the specified period of data collection, the sample size was proportionally allocated to those health institutions. Finally, the study participants were selected by using a systematic sampling technique.
2.3. Data collection tools and procedures
The questioner was developed by authors after reviewing different kinds of literature on the topic and validated by professional experts. Data were collected using structured and pre‐tested interviewer‐administered questionnaires through face‐to‐face exit interviews, which consists of a sociodemographic characteristic, obstetric information and other related variables. The data on the timing of the first ANC booking were gathered from women's recall, if the failure to remember, and it was extracted from their medical charts. The questionnaire was first prepared in English and then translated to Amharic (local language) and back to English again by a language expert to maintain consistency. Seven qualified diploma midwife data collectors were selected from other catchments which are not selected for data collection and two midwives having masters' in clinical midwifery were recruited to supervise the data collection process.
2.4. Data quality control
Two consecutive days of training to the data collectors and supervisors on the objectives, relevance of the study, ethical concern and techniques of interviews were given before the actual data collection. Before data collection, Research Ethics Committee approval was taken from the IRB of Bahir Dar University, College of Medicine and health sciences, and informed consent and confidentiality were assured by data collectors to the participants. The Amharic version of the questionnaire was pre‐tested on 40 (5%) pregnant mothers of the sample population in the health institutions not included in the study, and then, the instrument was amended accordingly. The data collection is strictly followed and supervised daily by supervisors along with the principal investigators. Data coding and entry were checked throughout the work. Data cleaning was checked at the end of the data entry.
2.5. Data processing and analysis
All the questionnaires were checked visually, and data cleaning, coding and entry were done by using EPI Info version 7.0 and exported to SPSS version 21.0 software package for analysis. Descriptive and summary statistics like frequency, percentage, mean and standard deviation were carried out. Tables and graphs were also used for data presentation. Bivariate and multivariable logistic regression analyses were used to identify variables associated with timely antenatal care initiation. Variables with a p‐value ≤0.20 in the bivariate logistic regression analysis were selected into the multivariable logistic regression model for controlling the possible effect of confounders. Finally, variables that had an independent association with timely antenatal care initiation were identified based on the adjusted odds ratio (AOR), with 95%CI and p‐value less than 0.05. Ethical clearance was obtained from the institutional review board of Bahir Dar University. A formal letter request of cooperation was written to the Bahir Dar city health office. Written consent was obtained from each study participant. Confidentiality of information and privacy was maintained.
3. RESULTS
3.1. Socio‐demographic characteristics of respondents
All 804 pregnant women were participated making a response rate of 100%. Among the total participants, 82% of the respondents were in the age group of 20‐35years. The mean age of the respondents was 26.3 (SD ±4.9 years). Less than half (47.3%) of participants' educational level was secondary and above. Three hundred and sixty‐three (45.1%) of the respondent travelled 30–60 min to reach the ANC services (Table 1).
TABLE 1.
Socio‐demographic characteristics of pregnant women in Bahir Dar city, North West Ethiopia, 2017(n = 804)
| Variables | Categories | Frequency | Per cent |
|---|---|---|---|
| Age in years | <20 | 102 | 12.7 |
| 20–34 | 659 | 82 | |
| ≥35 | 43 | 5.3 | |
| Residence | Urban | 619 | 77 |
| Rural | 185 | 23 | |
| Ethnic | Amhara | 793 | 98.6 |
| Others a | 11 | 1.4 | |
| Religion | Orthodox | 734 | 91.3 |
| Muslim | 62 | 7.7 | |
| Others a , b , c | 8 | 1.0 | |
| Marital status | Married | 778 | 96.8 |
| Single | 20 | 2.5 | |
| Others c | 6 | 0.7 | |
| Educational status | No formal education | 278 | 34.6 |
| Primary school (1–8) | 146 | 18.1 | |
| Secondary and above | 380 | 47.3 | |
| Occupation | Employed | 163 | 20.3 |
| Self Employed | 54 | 6.7 | |
| Housewife | 523 | 65 | |
| Daily labourer | 64 | 8.0 | |
| Distance in minutes | ≤30 | 266 | 33.1 |
| 30–60 | 363 | 45.1 | |
| >60 | 175 | 21.8 |
Oromo, Tigre.
Catholic, Protestant.
Divorced, Widowed.
3.2. Obstetric characteristics of respondents
Among married women, 450 (57.4%) of respondents' age at first marriage was ≥18 years. More than two‐thirds of their age at first pregnancy was above eighteen years. Fifty hundred twenty‐five (65.7%), of respondents, had parity one and above. The majority (75.5%) of respondents perceived that the correct time of first ANC booking is within 12 weeks of gestation (Table 2).
TABLE 2.
Obstetric characteristics of pregnant women in Bahir Dar city, North West Ethiopia, 2017(n = 804)
| Variables | Categories | Frequency | Per cent |
|---|---|---|---|
| Age at first marriage(N = 784) | <18 | 334 | 42.6 |
| ≥18 | 450 | 57.4 | |
| Age at first pregnancy | ≤18 | 160 | 19.9 |
| >18 | 644 | 80.1 | |
| Parity | Nulliparous | 279 | 34.3 |
| Para one and above | 525 | 65.7 | |
| Planned or wanted pregnancy | Yes | 658 | 81.8 |
| No | 146 | 18.2 | |
| Having information about ANC initiation time | Yes | 651 | 81 |
| No | 153 | 19 | |
| Decision‐making power on ANC initiation time | Yes | 757 | 94.2 |
| No | 47 | 5.8 | |
| Mothers who perceived the right time to start ANC | ≤12 week | 607 | 75.5 |
| >12 week | 197 | 24.5 | |
| Timing of first ANC booking | 0–12 week | 355 | 44.2 |
| 13−27week | 415 | 51.6 | |
| 28−42week | 34 | 4.2 |
3.3. Timing of initial antenatal care visit
This study identified that 44.2% with 95%CI (40.6, 47.8) of respondents were booking their first ANC in a timely within 12weeks of gestation. The rest study participants initiated the first ANC. The mean gestational age of starting the first ANC visit was 15.9 (SD ± 6.03 weeks). The timing of the first ANC booking was ranging from 4 weeks up to 36 weeks of gestational age (Figure 1).
FIGURE 1.
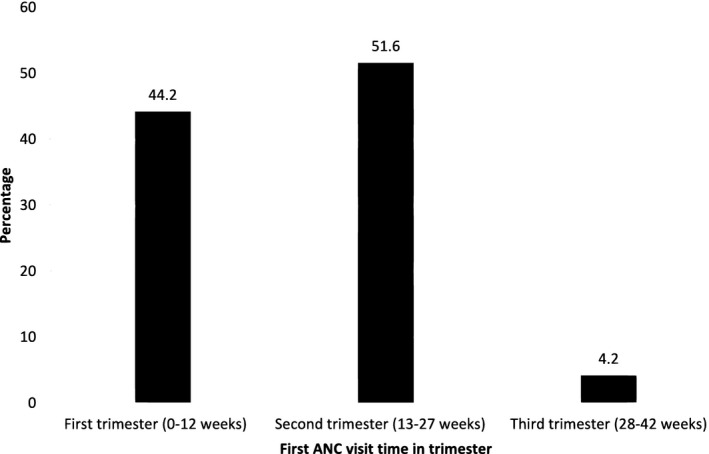
Timing of initial antenatal care visit
3.4. Reasons for late antenatal care initiation
Among respondents who started their first ANC booking late, 18.4% of them reported that do not know the appropriate time, and 2.2% of respondents perceived it as the appropriate time (Figure 2).
FIGURE 2.
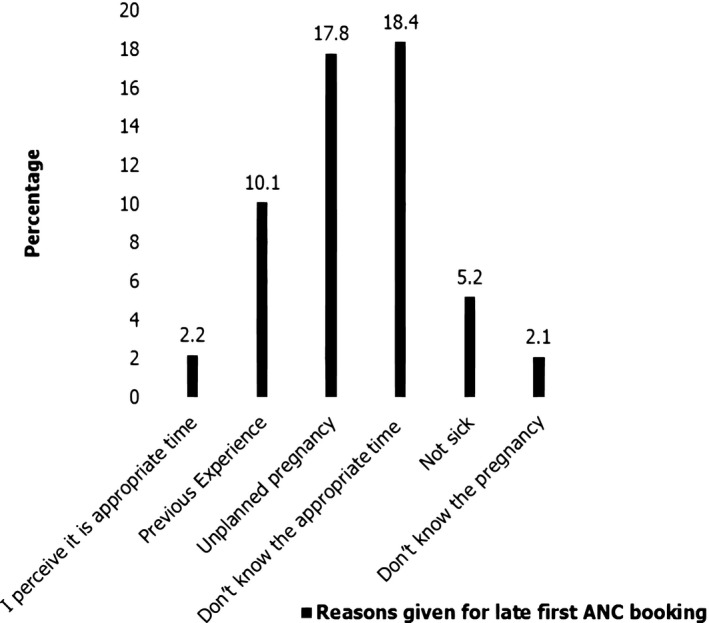
Reasons for late antenatal care initiation
3.5. Factors associated with the timely visit of first antenatal care
Bivariate analysis showed that residence, women educational status, partner educational status, women occupation, age at first pregnancy, having information about the correct time of ANC booking, mothers who perceived the right time to start ANC, having decision‐making power to use ANC and for whom mothers inform their pregnancy at the first time were a candidate variables for multivariable analysis at p‐value less than 0.2. In multivariable analysis, women with a secondary and above level of education (AOR: 7.07, 95% CI: 4.41, 11.35), women's age (>18 years) at first pregnancy (AOR: 2.79, 95% CI: 1.39, 5.57) and having information about the correct time of ANC booking (AOR: 3.14, 95% CI:1.67, 5.92) were significantly associated with timely first ANC booking at p‐value less than 0.05 (Table 3).
TABLE 3.
Association of factors with a timely booking of first ANC in Bahir Dar city, North West, Ethiopia
| Variables | Time at first ANC visit | COR (95%CI) | AOR (95%CI) | |||||
|---|---|---|---|---|---|---|---|---|
| Booked timely | Booked late | |||||||
| Residence | ||||||||
| Urban | 333 | 286 | 8.62 (5.38,13.84) | |||||
| Rural | 22 | 163 | 1 | |||||
| Women educational status | ||||||||
| Secondary and above | 278 | 102 | 12.28 (8.78,17.18) | 7.07 (4.41, 11.35) ** | ||||
| Primary and bellow | 77 | 347 | 1 | 1 | ||||
| Partner educational status | ||||||||
| Secondary and above | 279 | 127 | 22.22 (12.94, 38.16) | |||||
| Primary (1–8) | 55 | 134 | 4.15 (2.31, 7.48) | |||||
| Unable read and write | 17 | 172 | 1 | |||||
| Occupation | ||||||||
| Employed | 140 | 77 | 12.72 (5.77, 28.08) | |||||
| Housewife | 207 | 316 | 4.58 (2.14, 9.82) | |||||
| Daily labour | 8 | 56 | 1 | |||||
| Age at first marriage | ||||||||
| >18 years | 338 | 306 | 9.29 (5.49, 15.72) | 2.77 (1.39, 5.57)* | ||||
| ≤18 years | 17 | 143 | 1 | 1 | ||||
| Having information about ANC initiation time | ||||||||
| Yes | 332 | 319 | 5.88 (3.68, 9.41) | 3.14 (1.67, 5.92)** | ||||
| No | 23 | 130 | 1 | 1 | ||||
| Mothers who perceived the right time to start ANC | ||||||||
| ≤12 week | 279 | 328 | 1.35 (1.02, 1.88) | |||||
| >12 week | 76 | 121 | 1 | |||||
| Decision‐making power to use ANC | ||||||||
| No | 8 | 39 | 1 | |||||
| Yes | 347 | 410 | 0.24 (0.11, 0.53) | |||||
| For whom Mothers inform the pregnancy at the first time | ||||||||
| To husband | 266 | 372 | 1.37 (0.69, 2.74) | |||||
| Her Mother | 76 | 52 | 2.81 (1.32, 5.99) | |||||
| Others a | 13 | 25 | 1 | |||||
*p‐value < 0.005, **p‐value < 0.001.
Sister and friend.
4. DISCUSSION
A large proportion of maternal death worldwide was due to early preventable or treatable pregnancy and childbirth complications (Alkema et al., 2016; World Health Organization (WHO) 2016a, 2016b). Ethiopia is one of the Sub‐Saharan African countries with the highest maternal mortality ratio (Central Statistical Agency (CSA) [Ethiopia] and ICF, 2016). Antenatal care help to ensure the well‐being of the mother and foetus through early detection of risks in pregnancy, prevention of pregnancy and labour complications and ensures the safe delivery of mother and child (Federal Ministry of Health (FMOH) [Ethiopia], 2010; World Health Organization (WHO), 2015; World Health Organization (WHO) 2016a, 2016b).
This study identified only about 44.2% of respondents have started their first ANC booking within the recommended time with 95% CI (40.6, 47.8). This result showed that ANC in the study area did not meet the WHO antenatal care model recommendation, which states that every pregnant woman should start the first ANC visit within the first trimester of pregnancy (World Health Organization (WHO) (2002)). This finding was in line with the finding of previous studies conducted in Gondar, Ethiopia 47.4% (Belayneh et al., 2014). However, the finding of this study was lower than the study conduct in Addis Ababa, Ethiopia 65.6% (Yilal, 2015). This might be since Addis Ababa is the capital city of Ethiopia, women's level of awareness could be better than the study area. Moreover, the possible explanation for this difference, the community in Addis Ababa might have better accessible and available health services than the study area.
On the contrary, the finding in this study was higher when compared with studies from the different areas of African countries, Zimbabwe less than 1% (Erica, 2012) and Zambia 30% (Banda et al., 2012). The possible explanation for this variation might be the presence of socio‐economic differences and socio‐cultural status variations, time gap, availability and accessibility of health services. The finding of this study was higher than the national finding Ethiopian DHS 20% (Central Statistical Agency (CSA) [Ethiopia] and ICF, 2016). The explanation might be due to the time gap. Furthermore, this might be due to a difference in the scope of the study, to the fact that the national study covered more rural areas, and this study was conducted at an institution; therefore, women were more likely to attend ANC earlier than the general population.
Similarly, this finding was also higher than a study done in a different area of Ethiopia, in Ambo town 13.2% (Tolera Gudissa et al., 2015), Arba Minch Town 17.4% (Feleke et al., 2015), Jimma University Specialized Hospital 39.9% (Ewnetu et al., 2015) and Debre Brhan 26.2% (Amtatachew et al., 2013). This inconsistency could be attributed to the time gap, accessibility of health services and improvement in health service delivery. Moreover, the finding might be also justified by the fact that due to the efforts done by the Ethiopian government health policy to strengthen strategies for maternal and child health morbidity and mortality reduction through increasing utilization of maternal health services, particularly increasing ANC utilization (Federal Democratic Republic of Ethiopia [FDRE] & Ministry of Health [MoH], 2015).
Factors that positively affect the timely ANC booking were women's secondary and above level of education, age at first pregnancy and having information about ANC initiation time.
Women with a secondary and above level of education were 7.07 times more likely to be booked earlier than their counterparts. This finding agrees with the studies done in Kenya (Ochako & Girchuhi, 2016), south Nigeria (Adekanle & Isawumi, 2008), Tanzania (Ajayi & Osakine, 2013) and in Ethiopia Gondar (Belayneh et al., 2014), Addis Ababa (Yilal, 2015). The possible explanation could be due to women with a secondary and above level of education might be more likely to be employed, financially independent, and knowledgeable on the necessity of having antenatal care follow‐up during pregnancy, as a result, they might be more likely to realize the importance of early booking their first ANC visit timely. Evidence suggests that educated and knowledgeable mothers are more likely to initiate their first ANC timely (Hagey, 2014).
On the other hand, pregnant mothers who were above eighteen years at the time of first pregnancy were near 2.77 times more likely to be booked their ANC visit within the first trimester of pregnancy than younger women. There is a limited finding concerning the relationship between the timing of first ANC booking and age at their first pregnancy in the previous study, but in this study, age at their first pregnancy with above eighteen years was one of the determinant factors for the timing of initiation of ANC. The explanation could be the fact that awareness and level of decision‐making increases with age and those teenagers might feel shame by their pregnancy.
Additional statistical analysis of this study showed that having information about the correct time of ANC booking was a factor for an early ANC visit. Respondents who had information about the time of ANC initiation were 3.14 times more likely to book their first ANC visit within the recommended time compared to respondents who were not informed. This finding was in line with a previous study conducted in Addis Ababa and Gondar (Belayneh et al., 2014; Yilal, 2015). It might be explained by exposure to information on early initiation of ANC visit, enhances women's level of understanding and increases knowledge on the benefit of timely booking. Therefore, this suggested that proper information and advice on a pattern of ANC utilization is important to book at the recommended time.
5. CONCLUSION
Even though the ANC services are available free to all women, the timely visit of the first ANC was still low in the study area. Maternal education, age at first pregnancy and having information about the correct time of ANC booking were significantly associated with the timely booking of first antenatal care. Thus, encouraging women's education, avoiding teenage pregnancy and creating awareness for the initiation of the first ANC booking within the recommended time are highly advised.
5.1. Limitation
This study was not triangulated with the qualitative method.
CONFLICT OF INTEREST
I attest that this manuscript is the authors' original work and has not been submitted to, nor is under review at, elsewhere and is prepared following the instructions to authors' guideline. All authors have contributed to this manuscript, reviewed and approved the current form of the manuscript to be submitted.
AUTHOR CONTRIBUTIONS
Fentahun Yenealem Byene, Amlaku Mulat Aweke and Getahun Belay Gela inception designed the protocol, data analysis and interpretation. Azimeraw Arega Tesfu and Kihinetu Gelaye Wudineh participate in the data collection, the editorial, and data entry and analysis. The manuscript was drafted by Azimeraw Arega. Finally, the manuscript was revised and approved by all authors.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical clearance was obtained from the institutional review board of Bahir Dar University. A formal letter request of cooperation was written to the Bahir Dar city health office. Written consent was obtained from each study participant. Confidentiality of information and privacy was maintained.
CONSENT FOR PUBLICATION
Not applicable.
ACKNOWLEDGEMENTS
We thank the College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar Ethiopia for granting this research. We would like to extend our thanks to Bahir Dar city Health Office for permitting us to conduct the study and providing the necessary preliminary information. We are also obliged to thank data collectors, study participants and supervisors for their commitment to take part in the study. We also thank APHI for the selection of the abstract of this paper as a poster presentation in the APHI first Annual Conferences and was presented then posted online for readers. The abstract of this paper was posted online and available at: https://www.researchgate.net/publication/343635902_Timely_Initiation_of_First_Antenatal_Care_Visit_and_Its_Associated_Factors_among_Antenatal_Care_Attendees_in_Bahir_Dar_city_Health_Institutions_Northwest_Ethiopia
Tesfu, A. A. , Aweke, A. M. , Gela, G. B. , Wudineh, K. G. , & Beyene, F. Y. (2022). Factors associated with timely initiation of antenatal care among pregnant women in Bahir Dar city, Northwest Ethiopia: Cross‐sectional study. Nursing Open, 9, 1210–1217. 10.1002/nop2.1162
Funding information
Bahir Dar University
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Abou‐Zahr, C. L. , & Wardlaw, T. M. (2003). Antenatal care in developing countries: Promises, achievements, and missed opportunities: An analysis of trends, levels, and differentials, 1990–2001. World Health Organization, 2003, 2. [Google Scholar]
- Adekanle, D. , & Isawumi, A. (2008). Late antenatal care booking and its predictors among pregnant women in South‐Western Nigeria. Online Journal of Health Allied Science, 7(1), 4. [Google Scholar]
- Ajayi, I. , & Osakine, D. (2013). Socio‐demographic factors determining the adequacy of antenatal care among pregnant women visiting Ekiti state primary health centers. Health and Allied Sciences, 12(2), 4. [Google Scholar]
- Alkema, L. , Chou, D. , Hogan, D. , Zhang, S. , Moller, A.‐B. , Gemmill, A. , Fat, D. M. , Boerma, T. , Temmerman, M. , Mathers, C. , & Say, L. (2016). Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario‐based projections to 2030: A systematic analysis by the UN maternal mortality estimation inter‐agency group. Obstetric Anesthesia Digest, 36(4), 191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amtatachew, M. , Bekis, D. , & Digssu, N. (2013). Prevalence and Determinant of early antenatal care visit among pregnant women attending ANC in Debre Berhan health institution. African Journal of Reproductive Health, 17(4), 130. [PubMed] [Google Scholar]
- Banda, T. , Michlo, C. , & Hazemba, A. (2012). Factors associated with late antenatal care utilization in selected rural and urban communities. Medical Journal of Zambia, 39(3). [Google Scholar]
- Belayneh, T. , Adefris, M. , & Andargie, G. (2014). Previous early antenatal service utilization improves timely booking: cross‐sectional study at the university of Gondar hospital, northwest Ethiopia. Journal of Pregnancy, 2014, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Central Statistical Agency (CSA) [Ethiopia] and ICF (2016). Ethiopia demographic and health survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF. [Google Scholar]
- Erica, K. (2012). Timing of first antenatal care visit of factors associated with access to care among antenatal care attendants at chitungwiza municipal clinic Zimbabwe. Medicine.https://catalog.ihsn.org/index.php/citations/53938 [Google Scholar]
- Ewnetu, W. A. , Assegid, S. , Wondafrash, B. , & Ewnetu, H. (2015). Factors associated with late antenatal care initiation in an Ethiopian clinic. Research, 2, 1292. [Google Scholar]
- Federal Democratic Republic of Ethiopia [FDRE] , & Ministry of Health [MoH] (2015). Health Sector Transformation Plan [HSTP]. 2015/16–2019/20. Addis Ababa: Ministry of Health. [Google Scholar]
- Federal Ministry of Health (FMOH) [Ethiopia] (2010). Management protocol on selected obstetrics topics. Addis Ababa, Ethiopia: FMOH. January 2010. [Google Scholar]
- Feleke, J. , Yohannes, D. , & Biziya, A. (2015). Timing of first antenatal care attendance and associated factors among pregnant women in Arbaminch Town. Journal of Environmental and Public Health, 20(15), 7–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furness, D. L. , Dekker, G. A. , & Robert, C. T. (2011). DNA damage and health in pregnancy. Journal of Reproductive Immunology, 89(2), 153–162. 10.1016/j.jri.2011.02.004 [DOI] [PubMed] [Google Scholar]
- Hagey, J. , Rulisa, S. , & Pérez‐Escamilla, R. (2014). Barriers and solutions for timely initiation of antenatal care in Kigali, Rwanda: Health facility professionals’ perspective. Midwifery, 30(1), 96–102. 10.1016/j.midw.2013.01.016 [DOI] [PubMed] [Google Scholar]
- Moller, A.‐B. , Max, P. , Doris, C. , & Lale, S. (2017). Early antenatal care visit: a systematic analysis of regional and global levels and trends of coverage from 1990 to 2013. The Lancet Global Health, 5(10), e977–e983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ochako, R. , & Girchuhi, W. (2016). Pregnancy wantedness, frequency and timing of antenatal care visit among women of childbearing age in Kenya. Reproductive Health, 2(1), 13–51. 10.1186/s12978-016-0168-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oyerinde, K. (2013). Can antenatal care result in significant maternal mortality reduction in developing countries. J Community Med Health Educ, 3(2), 2–3. 10.4172/2161-0711.1000e116 [DOI] [Google Scholar]
- Prathapan, S. , Lindmark, G. , Fonseka, P. , Lokubalasooriya, A. , & Prathapan, R. (2011). How good is the quality of antenatal care in the Colombo district of Sri Lanka in diagnosing and treating anemia? Qual. Primary Care, 19(4), 245–250. [PubMed] [Google Scholar]
- Roth, C. , Magnus, P. , Schjølberg, S. , Stoltenberg, C. , Surén, P. , McKeague, I. W. , Davey Smith, G. , Reichborn‐Kjennerud, T. , & Susser, E. (2011). Folic acid supplements in pregnancy and severe language delay in children. JAMA, 306(14), 1566–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolera Gudissa, D. , Desta, W. , & Abebe, G. M. (2015). Timing of antenatal care booking and associated factors among pregnant women attending Ambo Town health facilities, Central Ethiopia. Journal of Gynecology and Obstetrics, 3(5), 103–106. [Google Scholar]
- Tunçalp, Ӧ. , Pena‐Rosas, J. P. , Lawrie, T. , Bucagu, M. , Oladapo, O. T. , Portela, A. , & Metin Gülmezoglu, A. (2017). WHO recommendations on antenatal care for a positive pregnancy experience‐going beyond survival. BJOG, 124(6), 860–862. 10.1111/1471-0528.14599 [DOI] [PubMed] [Google Scholar]
- WHO, UNICEF, UNFPA, World Bank Group, and United Nations Population Division (2016a). WHO, UNICEF, UNFPA, World Bank Group, and United Nations Population Division Trends in Maternal Mortality: 1990 to 2015 Geneva: World Health Organization, 2015. Population and Development Review, 42(4), 726. 10.1111/padr.12033 [DOI] [Google Scholar]
- World Health Organization (WHO) (2016b). WHO recommendations on antenatal care for a positive pregnancy experience. World Health Organization. [PubMed] [Google Scholar]
- World Health Organization (WHO) (2002). WHO, UNDP, UNFPA, and World Bank: Antenatal Care Randomized Trial: Manual for the Implementation of the new Model. Geneva; 2002. [Google Scholar]
- World Health Organization (WHO) (2015). Strategies towards ending preventable maternal mortality (EPMM). [Google Scholar]
- Yilal, S. (2015). Late initiation of antenatal care and associated factors among antenatal care attendances in 10 selected health centers Addis Ababa. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


