Abstract
Introduction
The burden of chronic breathlessness on individuals, family, society and health systems is significant, and set to increase exponentially with population ageing, complex multimorbidity and coronavirus disease 2019 (COVID-19)-related disability. Breathlessness support services are effective; however, reach and access are limited. Delivering online breathlessness interventions may build capacity and resilience within health systems to tackle chronic breathlessness through supported self-management. The aim of this study was to explore accessibility and willingness of patients with chronic breathlessness to use an internet-based breathlessness self-management intervention (SELF-BREATHE).
Methods
Semi-structured telephone interviews were conducted with adults living with advanced malignant and non-malignant disease and chronic breathlessness (July to November 2020). Interviews were analysed using conventional and summative content analysis.
Results
25 patients (COPD: n=13; lung cancer: n=8; interstitial lung disease (ILD): n=3; bronchiectasis: n=1) were interviewed: 17 male, median (range) age 70 (47–86) years and Medical Research Council dyspnoea score 3 (2–5). 21 patients had internet access. Participants described greater use, acceptance and normalisation of the internet since the advent of the COVID-19 pandemic. They described multifaceted internet use: functional, self-investment (improving health and wellbeing) and social. The concept of SELF-BREATHE was highly valued, and most participants with internet access were willing to use it. In addition to technical limitations, personal choice and perceived value of the internet were important factors that underpinned readiness to use online resources.
Conclusion
These findings suggest that patients living with chronic breathlessness that have access to the internet would have the potential to benefit from the online SELF-BREATHE intervention, if given the opportunity.
Short abstract
These findings suggest that patients living with chronic breathlessness that have access to the internet would have the potential to benefit from the online SELF-BREATHE intervention, if given the opportunity https://bit.ly/3tdJYru
Introduction
Breathlessness is a common symptom that has devastating impact on many people with cardiovascular disease, chronic lung disease and cancer, resulting in anxiety and social isolation for patients and their carers [1]. Over 2 million people with chronic disease experience breathlessness each year in the UK. This includes up to 98% of the over 1 million people in the UK diagnosed with chronic progressive lung disease [2], over 50% of the 200 000+ with incurable cancer and 50% of the 2 million with chronic heart failure [3]. In addition, breathlessness is prevalent in people living with renal and liver failure, neurological conditions, HIV/AIDS, many autoimmune diseases and multimorbidity [4].
Clinical management of breathlessness is challenging; optimal management of the underlying disease is always the first step. However, there is an inconsistent relationship between pathology and breathlessness perception [5, 6], and disease management alone does not guarantee symptom control. Breathlessness generally increases as disease progresses, often becoming chronic (i.e. persistent despite optimal pharmacological treatment of the underlying disease) [7]. Chronic breathlessness often results in emergency department (ED) attendance, re-attendances and hospitalisation. A significant proportion of these ED presentations are due to acute-on-chronic breathlessness crisis (sudden and uncontrollable increase in breathlessness) [8], some of which are potentially avoidable if patients have self-management strategies/management plans in place [8].
There is good evidence for face-to-face delivered, non-pharmacological, self-management interventions for chronic breathlessness in advanced disease, commonly referred to as breathlessness support services [9]. These are recommended by international COPD [10] and oncology clinical guidelines [11]. Despite this, the National Health Service (NHS) (UK) and most health systems globally do not provide breathlessness support services widely. Access is largely limited to the research setting.
Prior to the coronavirus disease 2019 (COVID-19) global pandemic, the burden of chronic breathlessness on individuals, family, society and health systems was significant, and set to increase exponentially with an ageing population with complex multimorbidity. This has been further amplified by the ongoing legacy of high symptom burden and disability as a consequence of the COVID-19 pandemic. Emerging data suggest that >40% of COVID-19 survivors have persistent (chronic) breathlessness [12, 13]. Considering the ongoing healthcare crisis resulting from COVID-19, a proactive and innovative approach is required to build capacity and resilience within the health systems to tackle chronic breathlessness. The evidence supports breathlessness support services for effective self-management; however, implementation of clinic-based services is challenging. This type of short-term, symptom-focused psychoeducational intervention is particularly well suited to being delivered as a web-based intervention.
A systematic review and meta-analysis of internet-based interventions targeting health behaviour in non-communicable disease (n=43 236) showed significant improvements in risk-related behaviour, such as physical activity (effective size 0.24: 95% CI 0.09–0.38), dietary behaviour (effect size 0.20: 95% CI 0.02–0.37) and alcohol consumption (effect size 0.14: 95% CI 0.00–0.27) [14]. Evidence-based digital interventions have the potential to discretely impact on self-management [15] and demonstrate positive trends towards cost-effectiveness [16]. Although limited, digital COPD self-management interventions [17] and pulmonary tele-rehabilitation [18] have demonstrated preliminary positive outcomes. Currently, there is no transdiagnostic online, self-management intervention for people living with chronic breathlessness described in the literature.
The aim of this study was to explore areas of uncertainty, regarding internet accessibility and willingness of patients with chronic breathlessness to use an internet-based breathlessness self-management intervention (SELF-BREATHE).
Methods
Study design
This research is grounded in a pragmatist research paradigm. Pragmatism is oriented towards solving practical problems in real world settings. It recognises that knowledge is understood through human experience and becomes meaningful when coupled with action. Pragmatism encourages experimentation and reflection, and therefore is appropriate for use in the development of interventions such as SELF-BREATHE [19]. Semi-structured qualitative interviews were conducted with patients with advanced malignant and non-malignant disease and chronic breathlessness reported in line with the COREQ (consolidated framework for reporting qualitative research) guidance [20].
Ethical approval
Ethical and local research and development approval was obtained prior to commencing this research (REC reference number: 20/LO/0160). The study was registered on www.clinicaltrials.gov (NCT 04466020).
Setting
Semi-structured qualitative interviews were conducted over the telephone with patients at their place of residence between July 1 and November 1, 2020.
Participants
Inclusion criteria
Adult patients >18 years of age
Chronic breathlessness on exertion and or rest (Medical Research Council (MRC) dyspnoea score >2) [7, 21]
Advanced disease such as cancer, COPD, chronic heart failure or interstitial lung disease (ILD), where the underlying disease was deemed to be optimally medically managed by the referring clinician
Exclusion criteria
Breathlessness of unknown cause
A primary clinical diagnosis of chronic hyperventilation syndrome
Unable to speak English
Not capable of providing informed consent
Sampling strategy
Patients with chronic breathlessness were purposively sampled to give maximum variation in: diagnosis (malignant: 10–12; non-malignant: 10–12) breathlessness severity (MRC 2–3: 10–12; MRC 3–5: 10–12), age (≤70 years: 10–12; ≥71 years: 10–12) and sex (male: 10–12; female 10–12).
Recruitment
Patients were recruited from King's College Hospital NHS Foundation Trust (Denmark Hill and Princess Royal sites) through Respiratory Medicine, Oncology, Physiotherapy and Pulmonary Rehabilitation services, which included virtual clinics offered in response to the COVID-19 pandemic.
Clinicians checked the eligibility of patients during routine consultations. If eligible, clinical staff asked the patient for permission to pass their contact details to the study principal investigator (PI) (C.C. Reilly) who provided them with a copy (paper via the post or electronic via e-mail) of the patient information sheet. Thereafter, the PI or researcher (A.R.) contacted the patient after 72 hours (minimum) to discuss the patient information sheet with them and answer any questions regarding the study. If the patient was happy to participate, an interview was scheduled at a time convenient for the participant. Prior to the interview, the researcher asked the participant to verbally consent and sign and date the consent form. The consent process was audio recorded. Participants returned the signed consent form using a pre-paid self-addressed return envelope to the research team.
Sample size
Recruitment continued until theoretical saturation was indicated (i.e. no new codes or themes relevant to the study aim emerged). This was determined by preliminary analysis of detailed reflective notes taken immediately after interviews and constant comparison of new data with existing findings [22]. We anticipated this would occur after recruitment of ∼20–25 participants.
Interview content
Interviews followed a semi-structured interview schedule guided by relevant literature, the views of relevant professionals and study patient and public involvement (PPI) representatives. The topic guide explored: whether individuals had internet access, whether they were internet users (self-defined), perceived value of the internet, reasons for using or not using the internet, patients’ experiences (good and bad) of using online services, e.g. shopping, frequency and modes of accessing the internet, and confidence in using the internet.
Participants were introduced to the concept of SELF-BREATHE: an online resource where individuals with chronic breathlessness could log on and learn about chronic breathlessness. In addition to being provided with non-drug treatments, e.g. breathing exercises, pacing and exercises to increase fitness, with the overall aim to provide individuals with self-management skills that may help them improve their breathlessness.
Participants were asked about their view on the concept of SELF-BREATHE, what would encourage them to use SELF-BREATHE and what might we need to consider (good and bad) when planning and developing SELF-BREATHE.
Interviews were scheduled to last ∼60 minutes and conducted by a researcher (A.R., C.R.) with experience in qualitative palliative care research. Participants were not known to the interviewer prior to interview. Participants were asked if there were other people present in the room during the interview.
Patient characteristics such as age, ethnicity, MRC dyspnoea score, living situation, modes of accessing the internet and confidence in using the internet, as summarised in table 1, were obtained via direct questioning prior to conducting the semi-structured interviews.
TABLE 1.
Patient characteristics, internet access, use and willingness to use an online supportive breathlessness intervention (SELF-BREATHE)
| All | Internet users | Non-internet users | |
| Participants (n) | 25 | 21 | 4 |
| Age years# | 70 (47–86) | 67 (47–84) | 84 (70–86) |
| Age category years | |||
| 41–50 | 1 (4%) | 1 (5%) | - |
| 51–60 | 6 (24%) | 6 (24%) | - |
| 61–70 | 7 (28%) | 7 (28%) | 1 (25%) |
| 71–80 | 6 (24%) | 6 (24%) | - |
| 81–90 | 5 (20%) | 5 (20%) | 3 (75%) |
| MRC dyspnoea score# | 3 (2–5) | 3 (2–4) | 4 (4–5) |
| MRC dyspnoea category | |||
| MRC 2 | 6 (24%) | 6 (29%) | - |
| MRC 3 | 11 (44%) | 11 (52%) | - |
| MRC 4 | 7 (28%) | 4 (19%) | 3 (75%) |
| MRC 5 | 1 (4%) | 1 (25%) | |
| Sex (male: female) | 15:10 | 13: 8 | 2: 2 |
| Ethnicity | |||
| White | 21 (84%) | 17 (81%) | 4 (100%) |
| Asian or Asian British | 2 (8%) | 2 (9.5%) | 0 (0%) |
| Black, African, Caribbean or Black British | 2 (8%) | 2 (9.5%) | 0 (0%) |
| Primary diagnosis | |||
| COPD | 13 (52%) | 10 (48%) | 3 (75%) |
| Lung cancer | 8 (32%) | 7 (33%) | 1(25%) |
| Interstitial lung disease | 3 (12%) | 3 (14%) | 0 (0%) |
| Bronchiectasis | 1 (4%) | 1 (5%) | 0 (0%) |
| Smoking status | |||
| Nonsmoker | 3 (12%) | 3 (14%) | 0 (0%) |
| Ex-smoker | 19 (76%) | 17 (81%) | 2 (50%) |
| Current smoker | 3 (12%) | 1 (5%) | 2 (50%) |
| Living situation | |||
| Alone | 14 (56%) | 13 (62%) | 1 (25%) |
| Living with significant other/family | 11 (44%) | 8 (38%) | 3 (75%) |
| Support provided by a carer | |||
| Yes | 5 (20%) | 2 (9.5%) | 3 (75%) |
| No | 20 (80%) | 19 (90.5%) | 1 (25%) |
| Internet access | |||
| Yes | 21 (84%) | 21 (100%) | 0 (0%) |
| No | 4 (16%) | 4 (100%) | |
| Mode of accessing the internet | |||
| None | 4 (16%) | 0 (0%) | 4 (100%) |
| One | 7 (28%) | 7 (33%) | 0 (0%) |
| Two or more | 14 (56%) | 14 (67%) | 0 (0%) |
| Confidence in using the internet | |||
| No | 5 (20%) | 1 (5%) | 4 (100%) |
| Low | 6 (24%) | 6 (28%) | 0 (0%) |
| High | 14 (56%) | 14 (67%) | 0 (0%) |
| Would you use SELF-BREATHE? | |||
| No | 4 (16%) | 0 (0%) | 4 (100%) |
| Unsure | 1 (4%) | 1 (5%) | 0 (0%) |
| Yes, with help setting up | 4 (16%) | 4 (19%) | 0 (0%) |
| Yes, definitely | 16 (64%) | 16 (76%) | 0 (0%) |
Data expressed as n (%) unless otherwise indicated. MRC: Medical Research Council. #: denotes data expressed as median (range).
Analysis
The interview audio-recordings were transcribed verbatim, with care taken to use pseudonyms and anonymise patient or staff identifiable references. A reflexive diary was completed to reflect upon the flow of the interview, contextual factors, participant responses and personal reflections. A combination of conventional and summative content analysis was conducted supported by Microsoft Word and Excel software [23]. Initial conventional content analysis was inductive and commenced with immersion in the data. Reading each transcript word by word, codes were derived to capture key thoughts and concepts. Codes were refined and sorted into categories or meaningful clusters. Initial coding was conducted by the primary researcher (C.R.), who has experience of conducting and analysing qualitative interviews. Coding was supported by the qualitative lead for the project (K.B.), who conducted line-by-line coding on extracts of a sample of interviews, and any discrepancies were discussed and resolved by discussion with the wider research team as required. Findings were discussed with the broader research team on development of the initial coding frame, following refinement and on completion of the analysis. A secondary summative approach was employed to describe patterns in views. An iterative and concurrent process of recruitment and analysis was used with constant comparison of categories and their properties. Analysis was guided by the underpinning pragmatist epistemology with a focus on understanding experiences to identify and overcome potential problems and inform development of the intervention [23].
Results
Participants
25 patients (COPD: 13, lung cancer: 8, ILD: 3, bronchiectasis: 1) were interviewed: 17 males, with a median (range) age 70 (47– 86) years and MRC dyspnoea score of 3 (2–5). Of these, 21 (84%) patients had access to the internet and 14 (67%) had two or more modes of accessing the internet, most commonly a personal computer and smart phone. Of the 21 patients with internet access, 20 (95%) reported that they would use an internet-based breathlessness self-management intervention, if available (table 1). The four non-internet users were older and living with more severe breathlessness (table 1).
Findings
Participants talked generally about the internet and how their usage had increased since the advent of the COVID-19 pandemic, social distancing and during government-enforced restrictions (shielding). They described how the internet shaped their activities, their reasons for using the internet or not, and their views on accessing a breathlessness support service online. Each theme is described below with example quotes from the interviews.
COVID-19
For many of those interviewed, the COVID-19 pandemic appeared to have increased the acceptability, use and normalisation of the internet within their social network. It served to bridge the social void created during government-enforced restrictions and social distancing, especially social media and communication tools (e.g. Facebook, Zoom), and helped individuals to retain a connection to the outside world.
I had to shield, it's [the internet] sort of, been a lifeline because it's just me and the dogs, and the dogs have got fed up of talking to me [laughter]. It's been a life saver, just to feel connected to the outside world.
COPD, female, 51–60 years, MRC dyspnoea score: 4
Individuals described the rapid process of learning and familiarisation with online communication tools, often supported by younger family members, and how vital these had become to retain a social existence.
Everyone is talking about Zoom, as if it's this thing we have had forever, and I hadn't even heard of Zoom six months ago. I thought Zoom was a 1970s ice lolly. Now everyone just goes, Oh, I'll Zoom you.
COPD, male, 51–60 years, MRC dyspnoea score: 3
COVID-19 and lockdown has driven lots to use the internet. You know, the grandchildren are teaching grandparents, ‘This is how to use your phone”, and because people are having to buy things online, I think it wouldn't be that long before there wouldn't be anyone left who doesn't know how to use a mobile phone or computer.
COPD, female, 61–70 years, MRC dyspnoea score: 3
The COVID-19 pandemic highlighted the importance of human interactions, and patients reflected on the effect lockdown and government-enforced restrictions has had on their physical and mental health.
I've spent a while sitting in, isolating because of COPD, diabetes, the weight and all that. I got paranoid.
COPD, male, 51–60 years, MRC dyspnoea score: 3
Many were left fearful of leaving the home and contracting COVID-19, or left suffering from the pulmonary sequelae of recovery from COVID-19 in the context of their concurrent chronic conditions.
I have been shielding because of my lung and kidney disease. I did have to go to the hospital (during COVID) and I was a bundle of nerves…I didn't really want to go… I am petrified of getting COVID.
COPD, female, 61–70 years, MRC dyspnoea score: 4
Since COVID, my breathlessness has really deteriorated.
COPD, female, 51–60 years, MRC dyspnoea score: 4
Without the physical presence of others, many participants found comfort and companionship by using the internet, social media and online communication platforms to connect with people and communities.
With COVID, I haven't got any social interaction. I've been shielding for 16 weeks so, it [internet use] has increased. I suppose online meetings do help, as a substitute.
Lung cancer, male, 61–70 years, MRC dyspnoea score: 4
Multifaceted internet use
Patients living with chronic breathlessness described multifaceted internet use: functional, self-investment and social.
Functional (task specific, e.g. shopping, online banking)
Internet use was described as fostering positive feelings of achievement and empowerment when attaining new practical skills.
I watch a lot of YouTube videos, instructional videos, like I've learnt how to do my gas and water pressure since lockdown happened. I tried to get hold of a plumber with my housing association, which is very difficult anyway. I'm a 59-year-old bloke. I should be able to do that bloody sort of stuff, so I watched a video and learned how to do it.
COPD, male, 51–60 years, MRC dyspnoea score: 3
Participants also described other functional benefits of using the internet day to day.
I rarely leave the house, so I do all my shopping, my Christmas shopping online…I research things, if I get a new medication, I always check it (online).
COPD, female, 51–60 years, MRC dyspnoea score: 3
They took comfort in still being able to keep up-to-date with their medications, and the news, to do their shopping and to keep track of expenditure, despite the isolation.
Online banking, I find it helpful to know how much you can spend, because we are pensioners and obviously, we have to keep an eye on our expenditure. So that's a great asset. I can't get out to get the paper every day, so I read the paper every morning, virtually.
ILD, male, 71–80 years, MRC dyspnoea score: 3
Self-investment (improving health and wellbeing)
Participants also described benefits to their health and wellbeing afforded by utilising the internet. For some this included participating in formal workshops and seminars.
Since the lockdown Zoom has become really popular with so many people. I did a Zoom the other day where they wanted to speak to people with mental health issues and lockdown, how it's affecting them. I did my first Zoom. It was like “gosh” that was so helpful.
COPD, female, 51–60 years, MRC dyspnoea score: 4
For others the focus was more on access to online therapeutic resources to support mental health and wellbeing.
Meditation, little self-healing things that you get on there (online), just to calm you down. I do get these panic attacks; I suffer from depression as well, so I try not to get myself too low.
COPD, female, 61–70 years, MRC dyspnoea score: 3
Being able to see others through video conferencing helped to support relationship building and socialisation in the absence of in-person contact.
That thing did the other day, the face-to-face thing on the computer, that was good. You can see who you are talking too, it's easier than talking over the phone, because you see who you are talking to. It makes it much easier, and I think you get more out of it. I thought that was quite good. I have never done it before, but it was good. The hospital sends you a link, you click on it, and everyone pops up.
Bronchiectasis, male, 51–60 years, MRC dyspnoea score: 3
Social (enabling social interactions with friends and family, maintaining self-identity, e.g. cultural, religious)
Participants also described the different ways that the internet and online content enabled them to meet their social and cultural needs. For some, this included social media and online games.
I go on Facebook, every day. I go and watch videos on there's like singing and dancing, they're entertaining. We [family] now play games every week, now on Zoom.
COPD, female, 81–90 years, MRC dyspnoea score: 3
While for others, accessing cultural and religious content online helped them to feel connected to their community and their faith.
I come from Cyprus, so I put on some Greek music. Nothing too complicated, I watch a bit if Greek songs and little clips of videos.
COPD, female, 61–70 years, MRC dyspnoea score: 3
I don't have any (social interactions) at the moment. Since lockdown, I am stuck at home…It's [using the internet] the only activity I am doing at the moment, in the evening time I use if for two or three hours. I like listening to the Koran online…, it's in the cache, when I open YouTube all the videos which I have seen before are there, even those from the last two, three months …so it's not difficult for me.
COPD, male, 41–50 years, MRC dyspnoea score: 4
Decisions regarding using the internet
When discussing internet use, individuality, personal choice and perceived value of the internet were important subthemes that emerged. Despite the physical isolation of recent months, some people preferred not to use the internet for socialisation, nor to seek medical help or support.
No good talking to me about the internet, I wouldn't even know how to turn it on. I am 86. I've grown with old fashioned sort if things. I get very cross when they say go to WWW…. You know? I know my children are all internet and all the rest of it, I don't really want to learn… I'm 86 for crying out loud… as long as I can see my children, I am happy.
Lung cancer, female, 81–90 years, MRC dyspnoea score: 4
For some, learning the skills to navigate online web pages proved too much of a barrier for them to engage with online resources such as SELF-BREATHE.
My granddaughter tried to teach me, and I went on [accessed the internet] on my own. I got stuck on the lottery numbers, and I said to her, “no you keep it [the tablet]”. I haven't got the patience for a computer or anything. When my granddaughter tried to teach me, I turned round and said, “you keep the computer. I'll stick to the phone and writing letters”.
COPD, female, 61–70 years, MRC dyspnoea score: 4
While some were content not to engage with online resources, others described feelings of regret for not engaging with the internet. They could see the benefits and opportunities that having access to the internet would offer people living with chronic breathlessness.
Well for the likes of me, I know nothing about computers, I really don't. Myself personally I think that it's [SELF-BREATHE] it's a bloody good idea, I really do. It's just that I can't use the computer myself, but because there's a lot of people that are computer literate, I think it is a really good idea…I'm so glad people like you are taking the time to try and help people like me.
Lung cancer, male, 71–80 years, MRC dyspnoea score: 2
Confidence was a very real barrier to engaging with online self-help interventions. Patients who rated themselves as having low or no confidence in using the internet reflected on their own personal experiences and described the importance of having support with gaining the skills necessary to access the internet.
I think if you don't know how to use computers, that would be the challenge, but I think if people are taught how to use them (computers), that would be probably helpful, but to try and go into it cold for the likes of me (no confidence using the internet) I wouldn't stand a chance, but if there were someone talking me through it, of what to do, I think probably that would help.
Lung cancer, male, 71–80 years, MRC dyspnoea: score 2
They described solutions based on their own experience to overcome such challenges that fostered a sense of achievement and increase confidence, which they believe to be an important factor in whether an individual chooses to use an online health intervention.
Ignorance is bliss at the moment, with me. I am not very brave with these things until they force me into it, then I get on with it. If I was shown probably how to do it, if they had the patience to sit down and show me, then yes, I can manage it [log on to SELF-BREATHE]. I mean, it's like the phones. First of all, I was only making calls, and then the grandchildren said, “You've got to do this, you got to do that”, and gradually I learned. I can now even transfer money online on my phone.
Lung cancer, female, 71–80 years, MRC dyspnoea score: 2
Views on the SELF-BREATHE online intervention
The SELF-BREATHE intervention was viewed as a novel concept, and patients viewed it as valuable, as they felt it would address an unmet need.
I would welcome it, definitely. There is a gap there for it [SELF-BREATHE]. I not aware of anything like this. There is a gap out there, I have been looking and it's not there. I have spoken to my lung specialist, and he wasn't aware of anything.
Lung cancer, male, 61–70 years, MRC dyspnoea score: 3
A perceived advantage of SELF-BREATHE included availability and convenience with the online delivery removing some of the additional stress associated with attending in-person appointments.
You can do it yourself and you can do it at your convenience. It doesn't involve having to go somewhere on a freezing cold November and the rain is starting. You can do it at home. You and do it at your convenience. It takes some of the grief out of having to go somewhere.
COPD, male, 51–60 years, MRC dyspnoea score: 3
Others described this more in terms of essential access requirements, as they were unable to leave the home.
Some people won't be able to go out of the house, so being able to access the website [SELF-BREATHE] at home, is good, as they can't leave the house.
COPD, female, 51–60 years, MRC dyspnoea score: 4
In addition, the added convenience of being able to return to the material as required was viewed as a benefit to improve uptake and completion.
For example, if you go to physio, they tell you how to do things and then by the time you get home you've forgotten it. Whereas, if you've got a video, you can always fall back on it and make sure you are doing it correctly.
ILD, male, 71–80 years, MRC dyspnoea score: 3
The online nature of the resource was also described as affording patients time to absorb material, without feeling rushed or that they were over-burdening a service for non-urgent care.
When you go to the doctors you get like seven minutes, the seven minutes finish and I have forgotten, you know what I mean. If you had something on the internet, you could watch it over and over an explain it, you know what I mean, so you can understand it.
ILD, male, 51–60 years, MRC dyspnoea score: 3
There was an acknowledgement by patients that self-management is important in the management of chronic breathlessness, to enable them to live as well as possible with their condition.
Everyone's got to do something to help themselves, that's what I truly believe, a lot of people don't want to help themselves. The whole process of getting better is that you have to do some work, you have to put some work in to feel the benefit. The doctor what will they do? He'll listen, he might give you a couple of pills. Ideally, you've still got to do something, you've got to put in some effort into it to make it actually work.
COPD, female, 51–60 years, MRC dyspnoea score: 4
SELF-BREATHE was seen as tool to foster a sense of knowledge, ownership and responsibility with regard to their condition, with less reliance on professionals to take the lead. This was valued by patients.
I think people should have a hand in their illness, rather than just going to the doctors, collect pills, come home, and take pills. If we were given more information about any illness, then we would take control.
COPD, female, 51–60 years, MRC dyspnoea score: 3
Importantly, technological or internet-related challenges were seen to be only some of the barriers to uptake and usage of SELF-BREATHE, with self-motivation another key determinant in its success.
I think the main thing is to motivate people…I think motivation is the hardest thing. It's just so easy to sit down and do nothing, but it [doing nothing] harms you.
COPD, female, 61–70 years, MRC dyspnoea score: 2
People need encouragement, more than anything. I think, with this sort of thing [SELF-BREATHE], it's too easy to give up.
Bronchiectasis, male, 51–60 years, MRC dyspnoea score: 3
The increased reliance on the internet as a result of the COVID-19 pandemic was identified as a potential barrier to the uptake of SELF-BREATHE, as people may be reaching a saturation point with regards to their own and/or society's dependence on the internet to substitute human interaction.
My initial thought is [on SELF-BREATHE], right now, I've had enough of being online. I want to see people. I want the interaction. I think it's nice to have human contact, maybe it's because I'm on my own a lot. Yes, it's good to have human contact. We need to talk. Not just this internet business.
COPD, female, 61–70 years, MRC dyspnoea score: 3
Branding and the endorsement of the SELF-BREATHE intervention and an affiliation with a NHS organisation was important, viewed as a quality assurance marker of the content and advice provided. This reinforced the need for robust methodological studies to explore the acceptability in the effectiveness of any digital health interventions.
I say to you and I stress, if it was a proper site from yourselves [the hospital], I would use, but if it wasn't, no I am sorry, I'd shut it down.
Lung cancer, male, 71–80 years, MRC dyspnoea score: 4
Discussion
Key findings
The COVID-19 pandemic has increased the acceptability, use and normalisation of the internet within society, especially social media platforms and communication tools (e.g. Facebook, Zoom). Using the internet for social interactions helped patients to feel empowered and connected, which was especially important during government-enforced restrictions. These positive experiences changed patients' perspective on the functionality and personal value of the internet. For patients living with chronic breathlessness that have access to the internet, 95% would use an internet-based breathlessness self-management intervention (SELF-BREATHE), if given the opportunity.
Relevance of findings
Widespread internet connectivity is available to at least 55% of the global population. There are over 5 billion mobile phone users, and the availability of thousands of mobile health applications has provided unprecedented access to online health and wellbeing supportive tools/interventions [24]. In the UK, the internet user penetration rate in 2020 was 95.5%, which is expected to increase to 97.5% by 2025 [25].
Prevalence data for internet accessibility and use is lacking for patients with chronic disease. Current data suggest that ∼70% of patients with chronic respiratory disease attending pulmonary rehabilitation in the UK have internet access [26, 27] with 60% willing to use tele-rehabilitation, in keeping with our findings. The high use of the internet and willingness to use SELF-BREATHE in our study was influenced by the COVID-19 pandemic. Global data suggests that internet use and in particular the use of video communication applications have increased exponentially during the COVID-19 pandemic [24], also reflected within our findings.
The COVID-19 pandemic and subsequent government-enforced restrictions have had some negative impacts on the physical and mental health of many, especially those living with chronic respiratory disease [28–30]. However, for some, the internet provided physical, mental and social support, with participants in this study describing the internet as “a lifeline” during the COVID-19 pandemic. Our data demonstrated the potential value of the internet in delivering physical, mental and social interventions for individuals that are geographically isolated, unable to leave the home, or where in-person services are unavailable. Moreover, it is important that online interventions such as SELF-BREATHE complement and supplement the established clinical services, where digital interventions are part of a “treatment ladder” of breathlessness interventions [31].
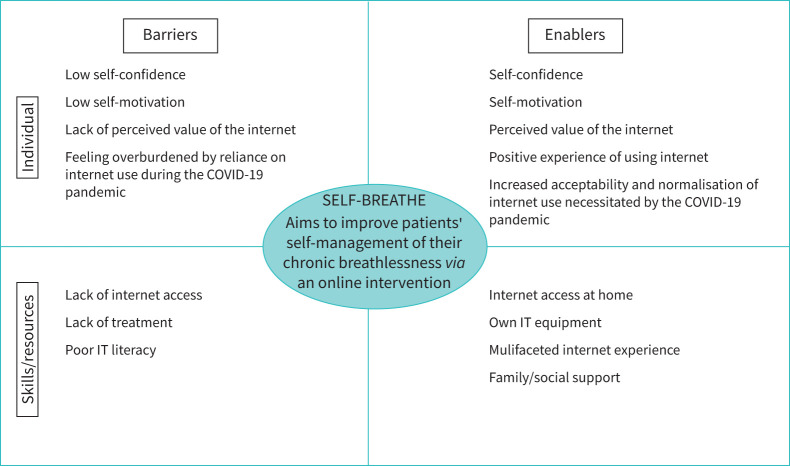
This is the first paper to explore internet use and the potential willingness of patients living with advanced malignant and non-malignant disease and chronic breathlessness. It provides data to understand their experiences, needs, barriers and enablers to the development and use of an online digital intervention for chronic breathlessness (SELF-BREATHE) (figure 1). These data support the development of an online self-management intervention to support patients living with chronic breathlessness. Future research needs to explore: 1) the feasibility and acceptability of SELF-BREATHE; and 2) the clinical effectiveness and cost-effectiveness of SELF-BREATHE.
FIGURE 1.
Barriers and enablers to the use of an online digital intervention for chronic breathlessness (SELF-BREATHE). IT: information technology.
The COVID-19 pandemic led to rapid growth in digital healthcare interventions [32]. These make efficient use of clinician time and can promote patient self-management and empowerment but can introduce inequality due to costs and digital capability (hardware ownership, literacy, etc.). Patient choice and preference should guide use, and communication to understand each person's goals, motivations and challenges remains important.
A potential advantage of SELF-BREATHE is that it could improve access and reach of non-pharmacological self-management intervention for people living with chronic breathlessness in the absence of face-to-face delivered breathlessness services. The costs associated with SELF-BREATHE are potentially low, which is an important predictor of implementation of SELF-BREATHE, if proved to be clinically effective. A limitation of SELF-BREATHE, like any self-management intervention, is that it depended on self-motivation to make positive lifestyle changes.
Access to SELF-BREATHE is dependent on the ability of the individual to gain access to the internet. A proportion of patients without internet access expressed feelings of regret for not engaging with the internet. Those with low confidence or who lacked the necessary IT skills highlighted the importance of having friends or family to support access to online health interventions. This poses the question as to whether health and social care staff or volunteer services, e.g. www.citizensonline.org.uk, can provide access to the internet by highlighting Wi-Fi hubs in the community and providing training and support to those wishing to access online services.
The development and evaluation of any online health intervention requires an iterative and inclusive process, with patients, clinicians and digital health experts, to ensure that such intervention reflects patient healthcare needs and incorporates evolving digital technologies. Behavioural research indicates that actively engaging participants improves health outcomes [33] through factors such as improved autonomy [34], empowerment and mastery [35]. Our data highlighted that providing clear associations between a digital platform such as SELF-BREATHE and “expert” healthcare professionals and/or healthcare organisations was important to satisfy the desire for accountability. This view was reinforced by research that suggests a key factor in promoting engagement with digital health interventions is clear endorsement by respected clinicians or expert organisations [36, 37].
For patients that have access to the internet who are willing and motivated to use a breathlessness self-management intervention, SELF-BREATHE provides a potential option to support those living with chronic breathlessness. However, it must be acknowledged that the non – internet users (n =4, 16% of the sample), were older (median 84 versus 67) and had higher dyspnoea values (4–5) than internet users, highlighting that SELF-BREATHE or any similar digital intervention may not reach all those living with chronic breathlessness. In the absence of face-to-face delivered breathlessness supportive services, a digital solution directly addresses this unmet need at scale and lower cost. To tackle the burden of chronic breathlessness on individuals, society and health services, there is a need for investment in both digital and face-to-face clinical and cost-effective breathlessness supportive interventions.
Effective self-management requires patients to change certain behaviours. An individual's inclination to change behaviour depends on the extent to which they are motivated to change [38]. Our findings are reflective of that of Tadas et al. [39], who highlight that motivation for action is driven by both individual factors and persuasive features of technology. In this study, we identified personal choice, sense of personal responsibility, perceived value of the internet, confidence, emotions, external influences such as friends, family and branding, and NHS endorsement as key factors in influencing whether individuals would use SELF-BREATHE.
We acknowledge that the study involved a small sample of the target population living in southeast London, where cultural, socioeconomic and geographical location (i.e. the availability and quality of internet provision in rural or remote locations) factors are important to consider when developing, testing and implementing digital health interventions.
Conclusion
Patients with advanced disease living with chronic breathlessness with access to the internet are willing to use an online supportive breathlessness intervention (SELF-BREATHE). Moreover, SELF- BREATHE was viewed as a positive step forward to addressing the lack of services and interventions available to manage chronic breathlessness. Future research needs to explore: 1) the feasibility and acceptability of SELF-BREATHE; and 2) the clinical effectiveness and cost-effectiveness of SELF-BREATHE.
Footnotes
Provenance: Submitted article, peer reviewed.
Conflict of interest: An NIHR Clinical Lectureship (ICA-CL-2018-04-ST2-001) supports C.C. Reilly, which funds all aspects of this research. In addition, and unrelated to the present research, they declare funding to their institution from “King's Together: Multi and Interdisciplinary research scheme” (GBP 19 000) and from Royal Brompton Hospital–King's Health Partnership Transformation (GBP 75 000). K. Bristowe declares research grants to their institution from the National Institute for Health Research, Medical Research Council, Health Education England, European Commission and Marie Curie, in the 36 months prior to manuscript submission. A. Roach declares no competing interests. M. Maddocks declares a National Institute for Health Research (NIHR) Career Development Fellowship (CDF-2017–10-009), and an infrastructure grant from the NIHR Applied Research Collaboration South London (NIHR ARC South London) at King's College Hospital NHS Foundation Trust, in the 36 months prior to manuscript submission. I.J. Higginson declares research grants from the National Institute for Health Research, UK Research & Innovation, Cicely Saunders International and Marie Curie, in the 36 months prior to manuscript submission.
Support statement: A National Institute for Health Research (NIHR) Clinical Lectureship (ICA-CL-2018–04-ST2–001) supports C.C. Reilly. M. Maddocks is supported by an NIHR Career Development Fellowship (CDF-2017–10–009). M. Maddocks and I.J. Higginson are supported by the NIHR Applied Research Collaboration South London. This publication presents independent research funded by the NIHR. The views expressed in this publication are those of the authors, and not necessarily those of the National Health Service, NIHR or the Dept of Health and Social Care. Funding information for this article has been deposited with the Crossref Funder Registry.
References
- 1.Bausewein C, Booth S, Gysels M,et al. Understanding breathlessness: cross-sectional comparison of symptom burden and palliative care needs in chronic obstructive pulmonary disease and cancer. J Palliat Med 2010; 13: 1109–1118. doi: 10.1089/jpm.2010.0068 [DOI] [PubMed] [Google Scholar]
- 2.B ritish Lung Foundation . Chronic obstructive pulmonary disease (COPD). 2021. statistics.blf.org.uk/copd
- 3.Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage 2006; 31: 58–69. doi: 10.1016/j.jpainsymman.2005.06.007 [DOI] [PubMed] [Google Scholar]
- 4.Kane PM, Vinen K, Murtagh FE. Palliative care for advanced renal disease: a summary of the evidence and future direction. Palliat Med 2013; 27: 817–821. doi: 10.1177/0269216313491796 [DOI] [PubMed] [Google Scholar]
- 5.Reilly CC, Jolley CJ, Elston C,et al. Blunted perception of neural respiratory drive and breathlessness in patients with cystic fibrosis. ERJ Open Res 2016; 2: 00057-2015. doi: 10.1183/23120541.00057-2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Booth S, Chin C, Spathis A. The brain and breathlessness: understanding and disseminating a palliative care approach. Palliat Med 2015; 29: 396–398. doi: 10.1177/0269216315579836 [DOI] [PubMed] [Google Scholar]
- 7.Johnson MJ, Yorke J, Hansen-Flaschen J,et al. Chronic breathlessness: re-thinking the symptom. Eur Respir J 2018; 51: 1702326. doi: 10.1183/13993003.02326-2017 [DOI] [PubMed] [Google Scholar]
- 8.Hutchinson A, Pickering A, Williams P,et al. Breathlessness and presentation to the emergency department: a survey and clinical record review. BMC Pulm Med 2017; 17: 53. doi: 10.1186/s12890-017-0396-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brighton LJ, Miller S, Farquhar M,et al. Holistic services for people with advanced disease and chronic breathlessness: a systematic review and meta-analysis. Thorax 2019; 74: 270–281. doi: 10.1136/thoraxjnl-2018-211589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Global Initiative for Chronic Obstructive Lung Disease (GOLD). Pocket guide to COPD diagnosis, management, and prevention. 2017 Report. https://goldcopd.org/wp-content/uploads/2016/12/wms-GOLD-2017-Pocket-Guide.pdf
- 11.Ferrell BR, Temel JS, Temin S,et al. Integration of palliative care into standard oncology care: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 2017; 35: 96–112. doi: 10.1200/JCO.2016.70.1474 [DOI] [PubMed] [Google Scholar]
- 12.D'Cruz RF, Waller MD, Perrin F,et al. Chest radiography is a poor predictor of respiratory symptoms and functional impairment in survivors of severe COVID-19 pneumonia. ERJ Open Res 2021; 7: 00655-2020. doi: 10.1183/23120541.00655-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cares-Marambio K, Montenegro-Jiménez Y,Torres-Castro R,et al. Prevalence of potential respiratory symptoms in survivors of hospital admission after coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis. Chron Respir Dis 2021; 18: 14799731211002240. doi: 10.1177/14799731211002240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Webb TL, Joseph J, Yardley L,et al. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res 2010; 12: e4. doi: 10.2196/jmir.1376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tighe SA, Ball K, Kensing F,et al. Toward a digital platform for the self-management of noncommunicable disease: systematic review of platform-like interventions. J Med Internet Res 2020; 22: e16774. doi: 10.2196/16774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Athilingam P, Jenkins B. Mobile phone apps to support heart failure self-care management: integrative review. JMIR Cardio 2018; 2: e10057. doi: 10.2196/10057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nguyen HQ, Donesky D, Reinke LF,et al. Internet-based dyspnea self-management support for patients with chronic obstructive pulmonary disease. J Pain Symptom Manage 2013; 46: 43–55. doi: 10.1016/j.jpainsymman.2012.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hansen H, Bieler T, Beyer N,et al. Supervised pulmonary tele-rehabilitation versus pulmonary rehabilitation in severe COPD: a randomised multicentre trial. Thorax 2020; 75: 413–421. doi: 10.1136/thoraxjnl-2019-214246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Long KM, McDermott F, Meadows GN. Being pragmatic about healthcare complexity: our experiences applying complexity theory and pragmatism to health services research. BMC Med 2018; 16: 94. doi: 10.1186/s12916-018-1087-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007; 19: 349–357. doi: 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 21.Higginson IJ, Bausewein C, Reilly CC,et al. An integrated palliative and respiratory care service for patients with advanced disease and refractory breathlessness: a randomised controlled trial. Lancet Respir Med 2014; 2: 979–987. doi: 10.1016/S2213-2600(14)70226-7 [DOI] [PubMed] [Google Scholar]
- 22.Given LM. The Sage Encyclopedia of Qualitative Research Methods. Los Angeles, CA, Sage Publications, 2008. [Google Scholar]
- 23.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005; 15: 1277–1288. doi: 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 24.statista. Global digital population as of January 2021. www.statista.com
- 25.statista. Internet usage in the United Kingdom (UK). www.statista.com
- 26.Polgar O, Aljishi M, Barker RE,et al. Digital habits of PR service-users: implications for home-based interventions during the COVID-19 pandemic. Chron Respir Dis 2020; 17: 1479973120936685. doi: 10.1177/1479973120936685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Seidman Z, McNamara R, Wootton S,et al. People attending pulmonary rehabilitation demonstrate a substantial engagement with technology and willingness to use telerehabilitation: a survey. J Physiother 2017; 63: 175–181. doi: 10.1016/j.jphys.2017.05.010 [DOI] [PubMed] [Google Scholar]
- 28.Philip K, Cumella A, Farrington-Douglas J,et al. Respiratory patient experience of measures to reduce risk of COVID-19: findings from a descriptive cross-sectional UK wide survey. BMJ Open 2020; 10: e040951. doi: 10.1136/bmjopen-2020-040951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Philip KEJ, Polkey MI, Hopkinson NS,et al. Social isolation, loneliness and physical performance in older-adults: fixed effects analyses of a cohort study. Sci Rep 2020; 10: 13908. doi: 10.1038/s41598-020-70483-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hume E, Armstrong M, Manifield J,et al. Impact of COVID-19 shielding on physical activity and quality of life in patients with COPD. Breathe 2020; 16: 200231. doi: 10.1183/20734735.0231-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Booth S, Johnson MJ. Improving the quality of life of people with advanced respiratory disease and severe breathlessness. Breathe 2019; 15: 198–215. doi: 10.1183/20734735.0200-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peek N, Sujan M, Scott P. Digital health and care in pandemic times: impact of COVID-19. BMJ Health Care Inform 2020; 27: e100166. doi: 10.1136/bmjhci-2020-100166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med 2012; 27: 520–526. doi: 10.1007/s11606-011-1931-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clark RA, Conway A, Poulsen V,et al. Alternative models of cardiac rehabilitation: a systematic review. Eur J Prev Cardiol 2015; 22: 35–74. doi: 10.1177/2047487313501093 [DOI] [PubMed] [Google Scholar]
- 35.Lupton D. The digitally engaged patient: self-monitoring and self-care in the digital health era. Soc Theory Health 2013; 11: 256–270. doi: 10.1057/sth.2013.10 [DOI] [Google Scholar]
- 36.O'Connor S, Hanlon P, O'Donnell CA,et al. Understanding factors affecting patient and public engagement and recruitment to digital health interventions: a systematic review of qualitative studies. BMC Med Inform Decis Mak 2016; 16: 120. doi: 10.1186/s12911-016-0359-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yardley L, Spring BJ, Riper H,et al. Understanding and promoting effective engagement with digital behavior change interventions. Am J Prev Med 2016; 51: 833–842. doi: 10.1016/j.amepre.2016.06.015 [DOI] [PubMed] [Google Scholar]
- 38.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000; 55: 68–78. doi: 10.1037/0003-066X.55.1.68 [DOI] [PubMed] [Google Scholar]
- 39.Tadas S, Coyle D. Barriers to and facilitators of technology in cardiac rehabilitation and self-management: systematic qualitative grounded theory review. J Med Internet Res 2020; 22: e18025. doi: 10.2196/18025 [DOI] [PMC free article] [PubMed] [Google Scholar]