Abstract
Objectives
We implemented narrative medicine in clinical practice using the Digital Narrative Medicine (DNM) platform.
Methods
We conducted a preliminary, open, uncontrolled, real-life study in the oncology and radiotherapy departments of Istituto di Ricovero e Cura a Carattere Scientifico National Cancer Institute Regina Elena, Rome, Italy. We recruited adult Italian-speaking patients who then completed the DNM diary from the start of treatment. The primary endpoint was DNM feasibility; secondary endpoints were health care professionals’ opinions about communication, therapeutic alliance, and information collection and patients’ opinions about therapeutic alliance, awareness, and coping ability. We used open- and closed-ended questions (scores 1 to 5) and a structured interview.
Results
Thirty-one patients (67%) used the diary (84% women). Health care professionals’ mean scores for feasibility and utility were ≥4.0. Patients’ utility scores were related to health care professionals’ feedback regarding the narratives. The main advantages for health care professionals were the opportunity to obtain relevant patient data and to strengthen communication and patient relationships (mean scores 4.4–5.0). Both groups strongly encouraged introduction of the diary in clinical practice.
Conclusion
Use of the DNM in oncology patients assisted clinicians with understanding their patients experience.
Keywords: Narrative-based medicine, digital diary, digital narrative medicine, personalized medicine, personalized care, chemotherapy, radiotherapy
Introduction
Understanding the causes of a patient’s doubts and fears may help clinicians to provide more detailed explanations, psychological advice, or to be more attentive to scheduling to improve patients’ awareness, empowerment, and treatment adherence. However, for this, appropriate interaction with each patient is needed. If adequately oriented, narrative medicine may help to improve personal relationships, therapeutic alliance, and promote adherence to treatment while fostering the professional growth of clinicians. This approach may provide clinicians with a deeper knowledge of the patient and help them to obtain information that is difficult for patients to communicate during chemo- or radiotherapy sessions and follow-up visits.
Approximately 30 years ago, narrative medicine was first described as a new approach to improving the patient–clinician relationship. 1 Kleinman introduced the use of narratives as a tool to collect and interpret information on the patient’s experience of illness, not only to enrich knowledge about their physical and psychological condition but also to formulate a correct diagnosis.2–5 Narratives may have therapeutic potential and may be applied in a way that provides health care professionals with information that can be used for diagnosis or the personalization of treatment. Although the Italian Istituto Superiore di Sanità published recommendations in 2014 for the implementation of narrative medicine in the management of rare and chronic degenerative diseases, no standard method is currently available in Italy for the management of oncology patients.
A specific digital platform has been developed to obtain guided narratives from patients during chemotherapy or radiotherapy for solid tumors. 6 The tool was designed to obtain information about barriers to treatment adherence and to facilitate the relationship between health care professionals and patients. Herein, we report a preliminary study aimed to evaluate the feasibility, practicability, and self-assessed utility of the digital narrative medicine approach from the perspective of both patients and health care professionals.
Methods
Patients
Two groups of patients from the Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) National Cancer Institute Regina Elena in Rome, Italy were included, namely, patients with breast or colorectal cancer receiving chemotherapy in the Medical Oncology 1 Department, and patients with a solid tumor receiving radiotherapy in the Radiotherapy Department. These departments could ensure that each patient was followed up by a single health care professional during the study.
All consecutive patients who fulfilled the inclusion criteria (age ≥18 years, Italian speaking, able to use electronic devices, having an E-mail account) and who were admitted for treatment to one of the two departments were invited to take part in this study.
Health care professionals and project team
Health care professionals included in the study were those trained in the application of narrative medicine who were able to follow up participating patients from admission to the end of their treatment, according to common practice; 7 these comprised physicians in the Oncology Department and nurses in the Radiotherapy Department. The entire project team included other professionals involved in the study design and analysis with expertise in the application of narrative medicine in research projects: an oncologist and epidemiologist, an anthropologist, a philosopher (all trained in qualitative research methodology), and two librarians.
Study design and ethical considerations
This was a preliminary, open, uncontrolled study in a real-life setting. The study was approved by the Ethical Committee of IRCCS Regina Elena, Rome, Italy (AMENO study: Registro Sperimentazioni IFO 877/16 – 14/12/2016, and AMENART study: Registro Sperimentazioni IFO 1034/17 – 18/01/2018). Patients gave their written informed consent to participate in the study, to use the digital narrative diary (DNM), and to the confidential data handling procedures for research and assistance according to the Italian Law 193/2006 on Privacy and Safeguarding of Sensitive Data and the General Data Protection Regulation of the European Union 2016/279 (Personal data code protection, Regulation (EU) 2016/679).8,9
This project was performed according to the principles of the Declaration of Helsinki. Patients’ priorities, experiences, and preferences were constantly taken into account during the collection of digital narrative outcomes. Patients were not directly involved in the design of the study but were informed of the outcome of the research in personal communications with health care professionals.
Intervention
The Digital Narrative Medicine (DNMLAB) is a digital platform developed by an innovative non-profit start-up (DNM srl, Rome, Italy). The platform is designed to help implement narrative medicine in clinical practice. This method can provide support to patients in the production of narratives and assist health care professionals in interpretating patients’ narratives. The platform uses a set of narrative prompts created for specific objectives (Table 1). The prompts may be shared with other centers and health providers, contributing to the definition of common tools for the application of digital narrative medicine in different therapeutic fields. The patient accesses the platform via a computer or smartphone and writes their story, guided by prompts that are presented twice a week according to an agreed sequence, in two waves over a period of 3 months. The patient can decide to ignore a prompt and to freely produce the narrative according to their observations. Moreover, the patient can write or record their story. The team project predefines a limit for the length for the response to help patients focus on specific aspects of their experience. With the patient’s consent, the health care provider can share the story with other caregivers directly via the platform and notes that are not visible to the patient can be exchanged among team members.
Table 1.
Digital Narrative Diary: prompts used in the AMENO and AMENART studies
| Narrative prompts | Translation |
|---|---|
| Tutto è cominciato quando … | It all started when … |
| Le cure: come le vivo e cosa ne penso | How I live with and what I think about the treatments |
| Oggi mi sento … – | Today I feel … |
| Le parole che mi aiutano … e le parole che non sopporto … | The words that help me … and the words I can't stand … |
| La mia vita quotidiana … | My daily life … |
| Potrei stare meglio se … | I could feel better if … |
| Volevo raccontarle che … | I want to tell you that … |
| In questo momento i miei pensieri si concentrano su … | Right now my thoughts are focused on … |
| Vorrei … | I would like to … |
| In questo momento, le cure … | Right now, the treatments … |
| Credo che potrebbe essere utile … | I think it might be helpful to … |
| La mia vita adesso … | My life right now … |
| Per me potrebbe essere utile … | For me it could be helpful … |
AMENO, Application of Narrative Medicine in the Chemotherapy Treatment of Oncological Patients; AMENART, Application of Narrative Medicine in Radiotherapy.
The digital diary was provided to both groups of patients concomitantly with the start of their treatment. Health care professionals subsequently reviewed the narrative texts and discussed them with patients during scheduled visits.
Each patient gave their specific consent for the use of their anonymized information in research studies, communication campaigns, and guideline production. DNMLAB cannot be used by patients to communicate emergency conditions. DNMLAB uses encryption and respects the privacy and safety of patient data, according to current health care system regulations.
Endpoints
The main endpoint of this study was feasibility of the DNMLAB platform. The measure of feasibility according to health care professionals was ease of use and time needed to use the platform. Feasibility was assessed by patients in terms of accessibility, ease of use, and satisfaction.
Secondary endpoints were the opinions of health care professionals about improvements in communication, therapeutic alliance, and collection of information that would otherwise be unattainable as well as patients’ opinions regarding the ease in producing a story, effectiveness in terms of being better listened to and better understood, initiation of a therapeutic alliance, and increasing awareness of and coping ability with their disease.
Assessment was performed at the end of the study using questionnaires with open- and closed-ended questions. Answers to closed-ended questions were scored on a 5-point Likert scale, with scores from 1 = complete disagreement to 5 = complete agreement. 10
A structured interview was used to investigate the reasons behind not participating in the project, opinions regarding implementation in clinical practice, and the intentions to make use of the tool in the future (Table 2).
Table 2.
Results from the 15 patient interviews addressing lack of participation in the AMENO and AMENART studies
| 1. Please explain your reasons for not using the digital diary. (more than one option could be selected) | Number of responses |
|---|---|
| a. I had forgotten the E-mail invitation to participate | 1 |
| b. I do not feel comfortable with digital technology | 3 |
| c. I found it difficult to use | 0 |
| d. I had technical difficulties trying to use it | 3 |
| e. I did not feel like talking about myself | 4 |
| f. I do not believe it is really useful | 2 |
| g. I prefer talking about myself during medical visits | 3 |
| h. I did not really understand what it was for | 1 |
| i. I was worried that my privacy was not guaranteed | 1 |
| j. Other reasons (lacking time to dedicate to myself, physical and concentration difficulties, lacking continuity of care with the same doctor). | 4 |
| 2. Which are your intentions regarding diary use in the near future? (more than one option could be selected) | |
| a. I will inform my doctor that I do not intend to use it | 1 |
| b. I would like to receive a new E-mail invitation to participate | 6 |
| c. I will start using it | 2 |
| d. I do not think I have time enough for this project | 1 |
| 3. Do you consider the diary useful in personalizing care? (express your evaluation using a score from 0 to 5) | 3.7 (median score) |
AMENO, Application of Narrative Medicine in the Chemotherapy Treatment of Oncological Patients; AMENART, Application of Narrative Medicine in Radiotherapy.
Statistical analysis
In line with qualitative research methods, the sample size was defined so as to assess the study objectives using descriptive analysis. Numerical data of continuous variables are presented as mean and standard deviation (SD) or median and range. Discrete variables are reported as frequency and percentage. Patients were considered to participate in the study if, after being invited by E-mail, they responded to at least one narrative prompt.
We carried out thematic qualitative analysis of all texts, narratives, open-ended questions, and comments. Texts were analyzed either manually or using Microsoft Word and a word cloud generator, available in DNMLAB. Three health care professionals (AF, EC, BCG) and two additional researchers on the team (the oncologist/epidemiologist [MCC] and the anthropologist [CC]) independently analyzed the texts. Patients’ narratives were analyzed according to Kleinman classification, distinguishing between disease-centered narratives and illness-centered narratives that focused on personal experience with the disease, and sickness-centered narratives focusing on social perception of the patient and disease. 11 Open interpretative coding was used to define the emerging topics. The results were presented to and discussed among the entire research team. We used the SQUIRE reporting guidelines in this study. 12
Results
Forty-six patients were invited to take part in the study (26 receiving chemotherapy and 20 receiving radiotherapy); 31 patients (67%) agreed to participate, 15 (48%) from the Oncology Department and 16 (52%) from the Radiotherapy Department. The median age was 58 years (range 31–79) in patients receiving chemotherapy, and 48 years (range 31–67) in patients receiving radiotherapy; the median age of the total was 52.5 years (range 31–79). Overall, 20 patients (65%) had breast cancer, nine had colorectal cancer (29%) and two (6%) had a different solid tumor. Only five participants were men (Table 3). The results from interviews investigating patients’ lack of participation are reported in Table 2. Patients’ customary use of electronic devices and a predisposition to talk about oneself were the main drivers of participation among patients.
Table 3.
General patient characteristics
| Characteristics | Invited, n | Participants, n (%) |
|---|---|---|
| Population size | 46 | 31 (67) |
| Sex (male/female) | 8/38 | 5/26 (16/84) |
| Age (years), median (range) | ||
| • Chemotherapy | 55 (31–79) | 58 (31–79) |
| • Radiotherapy | 52 (31–73) | 48 (31–67) |
| Cancer site | ||
| • Breast | 28 | 20 (65) |
| • Colon/rectum | 14 | 9 (29) |
| • Other | 4 | 2 (6) |
| Treatment group (health care professionals) | ||
| • Chemotherapy (two oncologists, one nurse) | 26 | 15 (48) |
| • Radiotherapy (five nurses) | 20 | 16 (52) |
| Narrative path: prompts with a reply | 168/202 (83) |
Participating health care professionals comprised two oncologists and six nurses, one from the Oncology Department and five from the Radiotherapy Department (Table 4).
Table 4.
Evaluation of the digital narrative diary by health care professionals
| Likert score, mean (SD) |
||
|---|---|---|
| Health care professionals’ assessment | Oncologists (n = 2) | Nurses (n = 6) |
| Feasibility | ||
| Diary user friendliness | 4.8 (0.4) | 4.6 (0.5) |
| Diary immediacy and comprehensibility | 4.0 (1.2) | 4.6 (0.5) |
| Time management | 4.5 (0.6) | 4.2 (0.4) |
| Optimized clinical examination (length) | 4.5 (1.0) | 4.2 (0.4) |
| Optimized clinical examination (quality) | 4.5 (0.6) | 4.6 (0.5) |
| Utility | ||
| Improved communication | 4.4 (0.9) | 5.0 (0) |
| Improved care relationship | 4.4 (0.9) | 5.0 (0) |
| Deeper knowledge of patient | 5.0 (0) | 4.4 (0.9) |
| Improved therapeutic alliance | 4.2 (0.4) | 4.8 (0.4) |
| Focus on care history | 4.0 (0.7) | 4.8 (0.4) |
Patients’ evaluation of DNMLAB
Final evaluation of the feasibility and utility of the narrative medicine diary was available for 14 patients receiving chemotherapy and for 16 patients receiving radiotherapy. One patient in the chemotherapy group could not complete the final questionnaire owing to occurrence of a stroke event.
All items related to feasibility received a mean score ≥4 by patients receiving chemotherapy as well as by those receiving radiotherapy. Patients receiving chemotherapy mainly related the utility of the platform to increased personalization of treatment. The items addressing a possibility to express one’s point of view and a perception of effectiveness in taking charge had mean scores ≥4 whereas items related to disease awareness and coping with the disease had scores <4. Assessment of platform utility was related not only to treatment personalization but also to improved disease awareness among patients receiving radiotherapy (Table 5).
Table 5.
Evaluation of the digital narrative diary by patients
| Likert score, mean (SD) |
||
|---|---|---|
| Patients’ assessment | Chemotherapy group (n = 14)* | Radiotherapy group (n=16) |
| Feasibility | ||
| Diary user friendliness | 4.5 (0.9) | 4.8 (0.4) |
| Diary immediacy and comprehensibility | 4.6 (0.5) | 4.8 (0.4) |
| Adequacy of one’s own computer skills | 4.4 (0.7) | 4.1 (1.4) |
| Opportunity to express oneself | 4.6 (0.7) | 4.7 (0.6) |
| Opportunity to provide personal information that is otherwise unavailable | 4.4 (0.7) | 4.2 (1.0) |
| Utility | ||
| Possibility to express one’s own point of view | 4.5 (0.7) | 4.4 (0.7) |
| Perception of effectiveness in taking charge | 4.0 (1.1) | 4.4 (0.8) |
| Improved awareness | 3.8 (1.1) | 4.2 (0.9) |
| Improved empowerment and self-confidence | 3.6 (0.8) | 3.9 (1.1) |
| Improved care relationship | 3.9 (0.9) | 4.1 (0.7) |
| Recommendation to introduce it in clinical practice | 4.5 (0.8) | 4.6 (0.6) |
*One patient was unable to complete the questionnaire owing to a stroke during chemotherapy treatment.
Health care professionals’ evaluation of DNMLAB
Among health care professionals, the mean feasibility score was >4 for all items except comprehensibility of the diary among oncologists (score of 4.0) and >4 for all items among nurses. The main advantages for health care professionals were the opportunity to obtain relevant patient data and to strengthen communication and patient relationships (mean scores 4.4–5.0) (Table 4). Interviews showed that, in the opinion of health care professionals, organizational barriers to the long-term implementation of DNMLAB may exist.
Text analysis
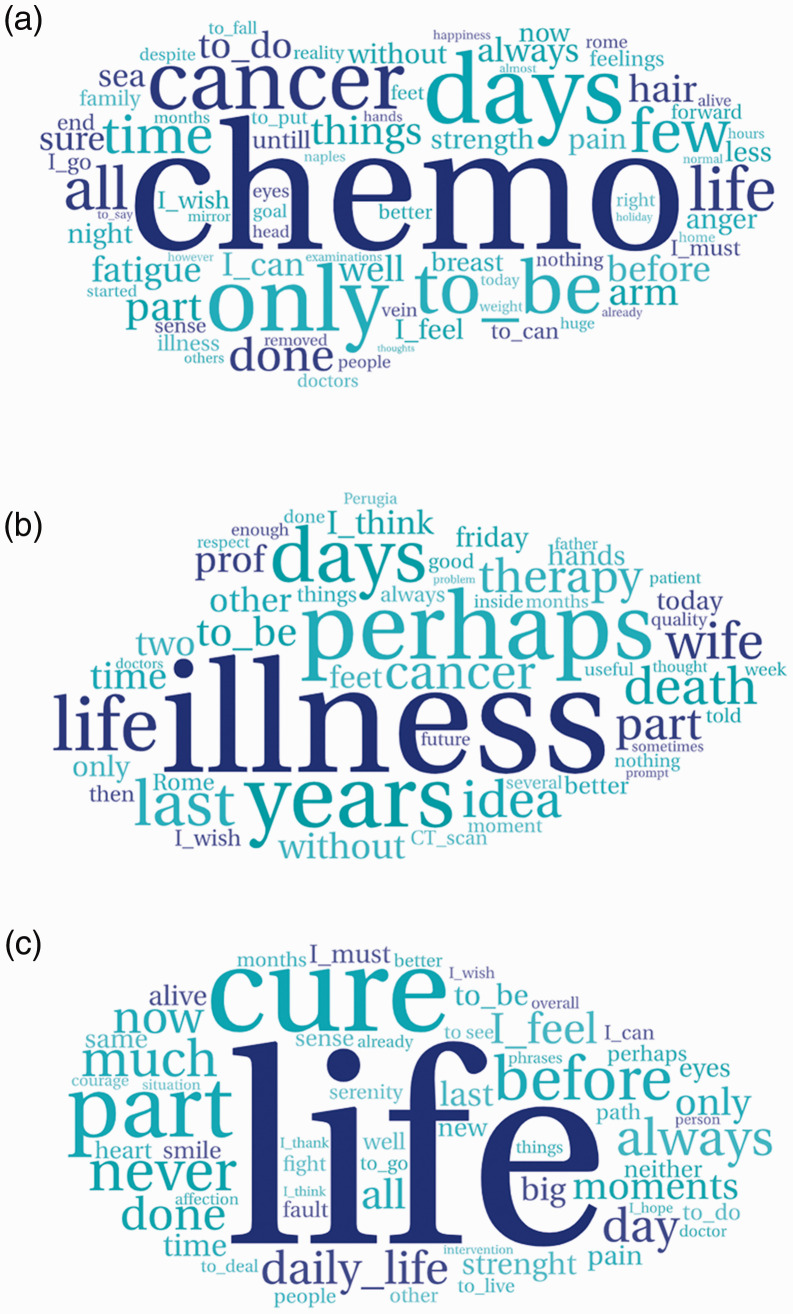
We analyzed all narratives, comments, and texts from the open-ended questions. In accordance with the study aim, health care professionals individually applied their patients’ narratives to clinical practice by integrating them with clinical data in the path of care for each patient. Word clouds were generated and interpreted for each patient (Figure 1). Patients’ narratives were also manually analyzed according to Kleinman classification. 11 As for the guiding narrative prompts, disease-centered prompts were mainly focused on the time and process of diagnosis (“It all started when …”) and on aspects related to chemotherapy or radiotherapy, essentially toxicity. Whereas diagnosis-related aspects were generally described using more technical language, adverse side effects of therapy were often described according to the individual’s experience, providing a deeper, more complex, and unique description of the patient’s physical and psychological status that would not otherwise be obtainable using standardized classification. Examples of such descriptions from our study participants include the following: “I feel like I am wandering in a reality that acts around me but does not affect me closely. I am asleep and I really feel the need to rest. Sleeping until the morning when I have difficulty opening my eyes. An intrusive, heavy, and at the same time almost artificial sleep. With cold sweats regardless of the temperature, and a sense of inadequacy.” Moreover, through patients’ narratives regarding their daily life activities and expectations, clinicians were provided with a suitable tool for developing a tailored and personalized approach to therapy. Clinicians also had the opportunity to redefine their ideas about patients’ real lives: “I found out that during chemotherapy, patients have a much more intense and active daily life than I could imagine.”
Figure 1.
Example word clouds generated from narratives of (a) 31-year-old woman, (b) 58-year-old man, (c) 46-year-old woman.
Furthermore, using the narrative approach, otherwise unobtainable relevant aspects that influenced treatment adherence emerged, as follows. “I had known the patient for several years, but she had never revealed to me that she had a daughter who was severely disabled since birth, for fear of biasing the choice of treatment toward less toxic but less effective drugs.” “The patient described how her cancer was nothing in comparison with the pain of forced separation from her children that had been imposed on her; her only motivation for cure was to be able to reunite with them one day.”
Finally, the need to be considered “normal” when receiving often pitiful or embarrassed looks from others who still consider cancer to be taboo emerged among the sickness-centered themes: “Avoiding those who were likely to pity me, even if without malice, was one of the very first things I did. I can recognize them right away; they have “the poor girl” stamped on their faces.” Word clouds from selected patient diary narratives are shown in Figure 1a to 1c.
Discussion
This preliminary study showed that use of the DNMLAB digital platform in oncology outpatients receiving either chemotherapy or radiotherapy was feasible and considered useful by both patients and health care professionals.
Among patients in both therapy settings, usefulness mainly referred to an improved opportunity to personalize treatment. Scores regarding improving awareness and empowerment in the radiotherapy group (>4) differed from those in the chemotherapy group (<4). According to the narratives, this difference can be attributed to a path guaranteeing continuity of care with the same health care professional during the duration of radiotherapy. These data are noteworthy, particularly when considering that continuity of care with the same clinician is associated with improved patient outcomes. 13 Responses from oncologists indicated that digital narrative medicine could improve the relationship with the patient, understanding of the condition as experienced by the patient, and could optimize time management during scheduled visits. Additionally, oncologists appreciated that the present project was an opportunity for professional growth, mainly owing to the opportunity to deepen their knowledge of illness-related aspects (i.e., toxic side effects in daily life in the patient's own words) and to enhance the multidisciplinary approach. Responses from both oncologists and nurses indicated that the digital narrative medicine enabled them to obtain information that the patient would otherwise be unable to communicate, which could improve the therapeutic alliance and patients’ adherence to treatment.
In this experience, narratives were guided by prompts prepared by specialized professionals to obtain information that is difficult to retrieve during typical chemotherapy or radiotherapy sessions. The digital platform provided patients with a private digital space where personal opinions, desires, fears, and requests could be expressed in a timely manner and without interference, as well as the certainty that the descriptions would be read and given attention. Nevertheless, the narratives were guided to assure that the issues described would be relevant to the cure.
In light of this, the present results further support the notion that narrative medicine may be introduced into clinical practice to complement evidence-based medicine because health care professionals consider it a useful tool for improving patient outcomes.
Apart from the oncological setting, storytelling is central to the management of many clinical conditions like heart failure, cardiovascular disease, and epilepsy, and some authors have reported data concerning the beneficial use of the digital platform DNMLAB.14–16 In the preliminary assessments, the strongest advantages of use of the digital diary reported by health care professionals were the disclosure of relevant patient information that was not otherwise obtainable, optimization of clinical examinations, and improved patient–doctor relationships and doctor-to-doctor communication. 14 Despite this, although narrative medicine has attracted interest over the past few decades, a standard method in oncological clinical practice is still lacking. 17 Several narrative research studies on illness narratives and parallel charts (personal notebooks in which clinicians can write down reflections and feelings) have provided insights for clinical practice and health care service organizations.18,19
Time spent producing narratives is treatment time that does not necessarily create a burden on organizations and caregivers. 20 On the contrary, facilitating treatment adherence and teamwork can substantially reduce time and costs.16,21 However, the introduction of a systematic narrative approach into clinical practice, training to improve narrative skills among physicians, and a change in clinicians’ perspectives toward care are required. 7 In a further qualitative study aimed at exploring the impact of this approach on health care professionals’ perception of their own role, our results showed that the diary was appreciated as a tool for application in narrative-based medicine, and the reading/writing format was considered to be of high quality and suitable for clinical practice. The narrative approach involves personal experience and emotional resonance with health care professionals, leading them to redefine their values in terms of health and disease. This study pointed out that the narrative medicine approach must be viewed in the light of relational systemic theory, taking into account the following aspects: training in narrative medicine itself, the acquisition of professional skills by practitioners, and the organizational development of the institution (i.e., organizational structures but also values and professional work culture). 22
Although this was a preliminary study aiming simply to assess the feasibility of this tool and a specific method, we believe that the results presented here will encourage further investigation to validate this instrument and to propose an organizational pathway for health care institutions. At our institute, we are currently conducting other studies exploring different settings, which include a larger number of patients and health care professionals operating in different roles and disciplines, with the aim to validate use of the digital narrative path in oncological clinical care. It will be necessary to educate participants, and this new method will need to be adopted in clinical practice. In fact, participants consistently reported that although feasible and useful in their personal practice, the digital path is not entirely suitable for the current organization of their institution. 22
A limitation to this study was that there was a small number of participants. This limited the duration of the study, the number of patients that could be included, and prevented testing of the platform throughout the entire study period as well as pathways of care and follow-up.
Conclusion
DNMLAB is a new tool for use in narrative medicine. We proposed a specific approach using the prompts in DNMLAB to produce patient narratives, aimed at retrieving patient information that is otherwise unattainable. The platform was considered feasible and useful by oncology outpatients in different settings and by health care professionals in charge of their treatment.
Acknowledgements
Editorial assistance was provided by Laura Brogelli, PhD, Barbara Bartolini, PhD and Aashni Shah (Polistudium SRL, Milan, Italy). Technical assistance for the word clouds images was provided by Leonardo Lancioni (DNM SRL, Rome, Italy).
Footnotes
Authors’ contributions: MCC and CC performed the study and prepared the article. EC, AF, IB, BGG, PDR, MM, PP, and LB enrolled the patients. AF, EC, BCG, MCC, and CC independently analyzed the texts. VS, FS, and AF edited the bibliographic research and contributed to the discussion. IT assisted in sample collection and statistical analysis. FC and GS revised the manuscript. All the authors have read and approved the final version of this manuscript.
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Editorial assistance was supported with internal funds.
ORCID iD: Maria Cecilia Cercato https://orcid.org/0000-0002-8346-6601
References
- 1.Kleinman A. The Illness Narratives. New York: Basic Book, 1988. [Google Scholar]
- 2.Charon R. Narrative Medicine: Honoring the Stories of Illness. New York: Oxford University Press, 2006. [Google Scholar]
- 3.Marchalik D. The return to literature-making doctors matter in the new era of medicine. Acad Med 2017; 92: 1665–1667. [DOI] [PubMed] [Google Scholar]
- 4.Riggs G. Commentary: Are we ready to embrace the rest of the Flexner report? Acad Med 2010; 85: 1669–1671. [DOI] [PubMed] [Google Scholar]
- 5.Johnston SC. Anticipating and training the physician of the future: the importance of caring in an age of artificial intelligence. Acad Med 2018; 93: 1105–1106. [DOI] [PubMed] [Google Scholar]
- 6.Digital Narrative Medicine. http://digitalnarrativemedicine.com/it/
- 7.Cercato MC. Narrative medicine in the oncological clinical practice: the path from a story-telling intervention to a narrative digital diary. Recenti Prog Med 2018; 109: 324–327. [DOI] [PubMed] [Google Scholar]
- 8.Personal data code protection. Legislat. decree No. 196 of 30 June 2003. published in the Italian official Journal N. 174, July 29, 2003, supplementary N. 123. Available: https://www.camera.it/parlam/leggi/deleghe/Testi/03196dl.htm [Accessed 31 May 2021].
- 9.Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing directive 95/46/EC (General data protection regulation. published in the official Journal of the European Union L 119, May 4, 2016. Available: https://op.europa.eu/it/publication-detail/-/publication/3e485e15-11bd-11e6-ba9a-01aa75ed71a1/language-en [Accessed 31 May 2021].
- 10.Cohen L, Manion L, Morrison K. Research Methods in Education. 5th Edition. London: Routledge Falmer, 2000. [Google Scholar]
- 11.Kleinman A. The illness narratives: Suffering, healing, and the human condition. Acad Med 2017; 92: 1406. 10.1097/ACM.0000000000001864 [DOI] [PubMed] [Google Scholar]
- 12.Ogrinc G, Davies L, Goodman D, et al. SQUIRE 2.0 (Standards for Quality Improvement Reporting Excellence): Revised publication guidelines from a detailed consensus process. BMJ Qual Saf 2016; 25: 986–992. doi: 10.1136/bmjqs-2015-004411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pereira Gray DJ, Sidaway-Lee K, White E, et al. Continuity of care with doctors—a matter of life and death? a systematic review of continuity of care and mortality. BMJ Open 2018; 8: e021161. doi: 10.1136/bmjopen-2017-021161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Volpe M, Testa M. Tales in cardiology. Eur Heart J 2019; 40: 800–802. 10.1093/eurheartj/ehz064 [DOI] [PubMed] [Google Scholar]
- 15.Cenci C, Mecarelli O. Digital narrative medicine for the personalization of epilepsy care pathways. Epilepsy Behav 2020; 111: 107143. doi: 10.1016/j.yebeh.2020.107143 [DOI] [PubMed] [Google Scholar]
- 16.Cenci C, Cercato MC, Mecarelli O. Narrative medicine in the digital time. Scenario, methods, and clinical use in epileptology and oncology. In: Ingrosso M, Pierucci P. (eds), Treatment relationships in the digital era. Canterano, Roma, Italy: Aracne Publisher, 69–88. [Google Scholar]
- 17.Fioretti C, Mazzocco K, Riva S, et al. Research studies on patients' illness experience using the narrative medicine approach: A systematic review. BMJ Open. 2016; 6: e011220. doi: 10.1136/bmjopen-2016-011220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Testa M, Cappuccio A, Latella M, et al. The emotional and social burden of heart failure: Integrating physicians’, patients’, and caregivers’ perspectives through narrative medicine. BMC Cardiovasc Disord 2020; 20: 522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tonini MC, Fiorencis A, Iannacchero R, et al. Narrative Medicine to integrate patients’, caregivers’ and clinicians’ migraine experiences: The DRONE multicentre project. Neurol Sci 2021; 1–12. doi: 10.1007/s10072-021-05227-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van der Wel C. First “more”, then “less”. Arch Intern Med 2012; 172: 465. doi: 10.1001/archinternmed.2011.2252 [DOI] [PubMed] [Google Scholar]
- 21.Wilcock PM, Brown GC, Bateson J, et al. Using patient stories to inspire quality improvements within the NHS modernization agency collaborative programmes. J Clin Nurs 2003; 12: 422–430. [DOI] [PubMed] [Google Scholar]
- 22.Zocher U, Bertazzi I, Colella E, et al. Applicazione della medicina narrativa nella pratica clinica oncologica: l’impatto sull’operatore [Application of narrative medicine in oncological clinical practice: impact on health care professional]. Recenti Prog Med 2020; 111: 154–159. doi: 10.1701/3315.32857 [DOI] [PubMed] [Google Scholar]