Abstract
Background
Biomarkers and clinical indices have been investigated for predicting mortality in patients with coronavirus disease (COVID-19). We explored the prognostic utility of procalcitonin (PCT), presepsin, and the Veterans Health Administration COVID-19 (VACO) index for predicting 30-day-mortality in COVID-19 patients.
Methods
In total, 54 hospitalized COVID-19 patients were enrolled. PCT and presepsin levels were measured using the Elecsys BRAHMS PCT assay (Roche Diagnostics GmbH, Mannheim, Germany) and HISCL Presepsin assay (Sysmex, Kobe, Japan), respectively. The VACO index was calculated based on age, sex, and comorbidities. PCT and presepsin levels and the VACO index were compared using ROC curve, Kaplan–Meier method, and reclassification analysis for the 30-day mortality.
Results
ROC curve analysis was used to measure PCT and presepsin levels and the VACO index to predict 30-day mortality; the optimal cut-off values were 0.138 ng/mL for PCT, 717 pg/mL for presepsin, and 12.1% for the VACO index. On Kaplan–Meier survival analysis, hazard ratios (95% confidence interval) were 15.9 (4.1-61.3) for PCT, 26.3 (6.4-108.0) for presepsin, and 6.0 (1.7-21.1) for the VACO index. On reclassification analysis, PCT and presepsin in addition to the VACO index significantly improved the prognostic value of the index.
Conclusions
This study demonstrated the prognostic utility of measuring PCT and presepsin levels and the VACO index in COVID-19 patients. The biomarkers in addition to the clinical index were more useful than the index alone for predicting clinical outcomes in COVID-19 patients.
Keywords: Procalcitonin, Presepsin, VACO index, Prediction, 30-Day mortality, COVID-19
INTRODUCTION
Coronavirus disease (COVID-19), caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), outbroke in December 2019 in Wuhan, Hubei Province, China and is still a pandemic, despite vaccination programs initiated worldwide [1-6]. In Korea, the first COVID-19 case was traced to Daegu [2-4].
When SARS-CoV-2 is transmitted into cells via the spike protein-biding domain and angiotensin-converting enzyme 2 (ACE2) receptor, it induces ACE2 internalization, cell damage, and lymphocyte death through the release of cytokines (e.g., interferon [IFN]-γ and interleukins [ILs]) and recruitment of inflammatory cells [6]. This in turn causes pro-coagulation, microvascular injury, and hypo-fibrinolysis and releases extracellular histones and neutrophil extracellular traps, resulting in immunothrombosis [6].
According to the WHO, the disease severity of COVID-19 ranges from mild to critical, and critically ill COVID-19 patients present with acute respiratory distress syndrome (ARDS), sepsis, septic shock, or acute thrombosis [7]. The sequential organ failure assessment (SOFA) score is used for assessing sepsis and disease severity of COVID-19 [7, 8]. Recently, the Veterans Health Administration COVID-19 (VACO) index was developed to predict 30-day mortality in COVID-19 patients, using demographic data, including age, sex, and comorbidities, from the Veterans Affairs (VA) national system in the United States [9, 10]. The VACO index does not predict COVID-19 disease severity; rather, it predicts the 30-day-mortality. The VACO index-predicted and observed 30-day mortality showed good calibration in the VA development cohort [9].
Several biomarkers have been investigated for predicting disease progression and the prognosis of COVID-19 [11-14]. Inflammatory biomarkers, such as the erythrocyte sedimentation rate and C-reactive protein, serum ferritin, procalcitonin (PCT), IL-2, IL-6, IL-8, and IL-10 levels, are increased in COVID-19 patients [11-13]. PCT, the pro-peptide of calcitonin, increases during severe infection and is considered a promising diagnostic and prognostic biomarker of sepsis [11, 15, 16]. Increased PCT levels may be associated with disease severity and mortality in COVID-19 patients [11-13, 17-20]. Presepsin, a 13-kDa glycoprotein cleavage N-terminal fragment of CD14, is released into circulation by pro-inflammatory signals during infection and has diagnostic and prognostic values in sepsis [21-24]. In COVID-19, presepsin was suggested as a predictive biomarker for disease severity [24-26].
To our knowledge, no study has compared these biomarkers and the newly proposed clinical index for predicting short-term mortality in COVID-19 patients. We explored the prognostic utility of PCT, presepsin, and the VACO index for predicting 30-day mortality in COVID-19 patients. We also explored whether adding PCT or presepsin to the VACO index would improve the prognostic value of the index or make it obsolete.
MATERIALS AND METHODS
Study population
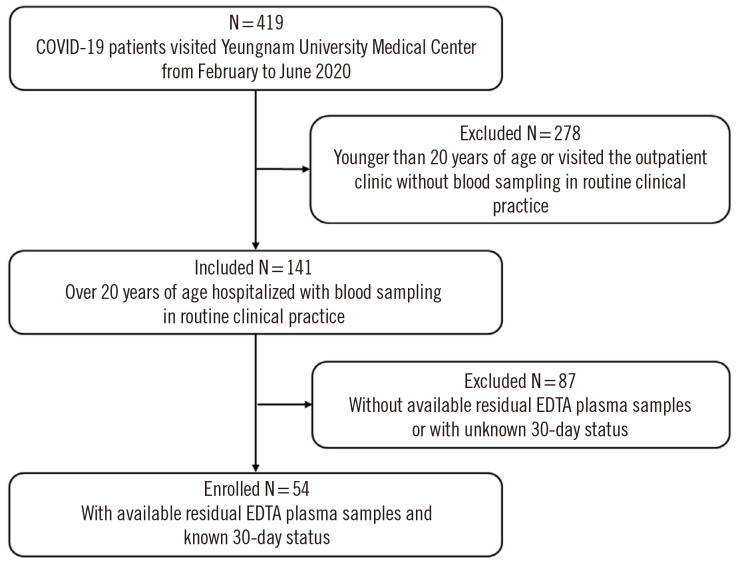
A study population enrollment flowchart is presented in Fig. 1. From February to June 2020, a total of 419 patients with COVID-19 visited Yeungnam University Medical Center (YUMC), Daegu, Korea. We excluded 278 patients who were younger than 20 years or visited the outpatient clinic without blood sampling in routine clinical practice. From 141 hospitalized patients over 20 years of age, we further excluded 87 patients due to the unavailability of residual EDTA plasma samples or unknown 30-day status. Finally, 54 patients were enrolled. No additional intervention or blood sampling was performed. This study with forward residual blood sampling and retrospective medical records review was approved by the institutional review board of YUMC (approval No. 2020-03-093), and written informed consent from the study population was waived.
Fig. 1.
Flowchart for patient enrollment. Abbreviation: COVID-19, coronavirus disease.
In all patients, the diagnosis of COVID-19 was confirmed by real-time reverse transcription-polymerase chain reaction (RT-PCR) [1]. The Allplex 2019-nCoV assay (Seegene, Seoul, Korea), Emergency Use Authorization Real-Time RT-PCR kit was used with nasopharyngeal swabs or sputum, and a positive result was defined as threshold cycle values of ≤40 for all target genes (E, N, RdRP), according to the manufacturer’s instructions [1]. Patients’ medical records were reviewed to obtain demographic, clinical, and laboratory data. The use of ventilator and extracorporeal membrane oxygenation during the hospital stay was assessed. The SOFA score, WHO disease severity, and VACO index were assessed at enrollment [7-10]. WHO disease severity was classified into mild (without viral pneumonia and hypoxia), moderate (pneumonia), severe (severe pneumonia), and critical (ARDS, sepsis, septic shock, acute thrombosis) disease [7]. Sepsis and septic shock were defined according to the Sepsis-3 definitions [8]. Acute thrombosis was defined as acute venous thromboembolism, such as pulmonary embolism, acute coronary syndrome, or acute stroke [7].
PCT and presepsin assays
Residual EDTA plasma samples were aliquoted to avoid repeated freezing and thawing and were stored at –70°C until use. Frozen samples were thawed at room temperature and gently mixed immediately before measuring the PCT and presepsin levels. PCT level was measured using the Elecsys BRAHMS PCT assay (Roche Diagnostics GmbH, Mannheim, Germany) on a cobas e801 module (Roche Diagnostics GmbH) based on a electrochemiluminescence immunoassay. The manufacturer-suggested reference range for PCT was up to 0.046 ng/mL. Presepsin level was measured using the HISCL Presepsin assay (Sysmex, Kobe, Japan) in an HISCL 5000 automated analyzer (Sysmex) based on a delayed one-step sandwich chemiluminescence enzyme immunoassay. The manufacturer-suggested reference range for presepsin was up to 333.0 pg/mL. Both assays were performed according to the manufacturers’ instructions.
VACO index
The VACO index was calculated based on a reported equation [9, 10] consisting of age, sex, Charlson comorbidity index (CCI), and the presence of myocardial infarction (MI) or peripheral vascular disease (PVD).
Coefficientsum=Agecoefficient+Sexcoeffient+CCI_Agecoefficient+MI_PVDcoefficient+Constantcoefficient
Odds ratio (OR)calc=exp(coefficientsum)
Riskpred=ORcalc/(1+ORcalc)
As the age coefficient value is set from the age of 20 years, the VACO index can be applied to COVID-19 patients over the age of 20 years. The age coefficient value ranges from –2.228678713 to 2.018752269, depending on age. The sex coefficient value is zero for females and 0.322291449 for males. CCI is estimated as the sum of the weights of comorbidities, including acquired immunodeficiency syndrome, cancer (non-metastatic, metastatic), cerebrovascular disease, chronic pulmonary disease, congestive heart failure, dementia, diabetes with or without complications, liver disease (mild, moderate, or severe), MI, peptic ulcer disease, PVD, plegia, kidney disease, and rheumatic disease. CCI is graded from 1 to 6 depending on the comorbidity. The CCI coefficient value ranges from zero to 1.395164653, depending on the CCI value for patients under 85 years but is set to 1.529325519 for patients above 85 years. If MI or PVD is present, the coefficient value is 0.267265312, otherwise it is zero. The constant coefficient value is set to –4.216058062. Riskpred is calculated using OR obtained by raising e (the natural number) to the power of the sum of coefficient values. The VACO index is obtained by multiplying the riskpred value by 100 and is expressed as a percentage.
Statistical analysis
Data are presented as number (percentage) or median (interquartile range, IQR). The Shapiro–Wilk test was used to assess the normality of the data distribution. The Mann–Whitney U test was used to compare values of PCT, presepsin, SOFA score, and VACO index between survivors and non-survivors. Fisher’s exact test was used to compare the distribution of WHO disease severity and incidence rates of ARDS, sepsis, septic shock, and acute thrombosis between survivors and non-survivors. In ROC curve analysis, the area under the curve (AUC), optimal cut-off values, sensitivity, and specificities of PCT, presepsin, SOFA score, WHO disease severity, and VACO index for 30-day mortality were estimated. A multimarker approach using PCT, presepsin, and the VACO index above the respective optimal cut-off values for 30-day mortality was analyzed using the ROC curve.
Kaplan–Meier survival analysis was used to estimate the hazard ratio (HR) with 95% confidence interval (CI) for 30-day mortality for PCT, presepsin, SOFA score, WHO disease severity, and VACO index. Sample size for the Kaplan–Meier survival analysis was estimated based on a previous study [27]. The inputs were as follows: analysis time t=1 month, accrual time α=5 months, follow-up time b=1 month, null survival probability was set to S0(t)=0.013, 0.025, or 0.026 based on the overall mortality reported in Korea during the study period and in previous studies [2, 3, 5]. The alternative survival probability was set to S1(t)=0.185 based on the 30-day mortality in this study. Using log-minus-log transformation and a two-sided type I error rate (α) of 0.05 and power (1-β) of 0.8, the sample size was estimated to be 18-21, with an actual power >0.8. Accordingly, a sample size of 54 was considered sufficient for Kaplan–Meier survival analysis.
Reclassification analyses using integrated discrimination improvement (IDI) and net reclassification improvement (NRI) were performed to assess the added value of the multimarker approach over the VACO index [28]. If IDI and NRI were significantly greater than zero, the new prediction model was considered to have improvement over the old model. For the statistical analyses, MedCalcSoftware (version 20.014, MedCalc Software, Ostend, Belgium) and R version 4.1.0 (The R Foundation for Statistical Computing, Vienna, Austria) were used. P<0.05 was considered statistically significant.
RESULTS
The characteristics of the study population are summarized in Table 1. The median age (IQR) was 71.0 years (63.0-79.0), and males accounted for 57.4% (N=31). The median values (IQR) of PCT and presepsin levels were 0.09 ng/mL (0.04-0.31) and 367.0 pg/mL (182.0-859.0), respectively. Moderate and critical WHO disease severity accounted for 27.8% (N=15) and 72.2% (N=39), respectively, with no mild or severe diseases. The median VACO index was 12.1% (5.3-18.0), and the 30-day mortality was 18.5% (N=10).
Table 1.
Characteristics of the study population
| Variable | All patients (N=54) |
|---|---|
| Age (yr) | 71.0 (63.0-79.0) |
| Male, N (%) | 31 (57.4) |
| Comorbidities, N (%) | |
| Hypertension | 28 (51.9) |
| Diabetes mellitus | 19 (35.2) |
| Dyslipidemia | 9 (17.0) |
| Malignancy | 7 (13.0) |
| Neurodegenerative | 7 (13.0) |
| Cerebrovascular disease | 5 (9.3) |
| Cardiovascular disease | 5 (9.3) |
| Heart failure | 4 (7.4) |
| Pulmonary disease | 3 (5.6) |
| Psychiatric disorders | 3 (5.6) |
| Chronic kidney disease | 2 (3.7) |
| Peripheral artery disease | 2 (3.7) |
| Liver disease | 2 (3.7) |
| Rheumatic arthritis | 1 (1.9) |
| Symptoms, N (%) | |
| Fever ( ≥ 37.5°C) | 35 (64.8) |
| Dyspnea | 29 (53.7) |
| General weakness | 24 (44.4) |
| Cough | 21 (38.9) |
| Sputum | 14 (25.9) |
| Fatigue | 11 (20.4) |
| Gastrointestinal symptoms* | 8 (14.8) |
| Chilling | 6 (11.1) |
| Myalgia | 6 (11.1) |
| Headache | 5 (9.3) |
| Sore throat | 4 (7.4) |
| Hemoptysis | 1 (1.9) |
| Rhinorrhea | 1 (1.9) |
| Nasal obstruction | 1 (1.9) |
| Chest pain | 1 (1.9) |
| Dizziness | 1 (1.9) |
| Mental change | 1 (1.9) |
| Limb muscle weakness | 1 (1.9) |
| Symptom duration (day) | 4.0 (0.0-8.0) |
| COVID-19 diagnosis to admission (day) | 0.0 (0.0-3.0) |
| COVID-19 diagnosis to blood sampling (day) | 4.0 (0.0-9.0) |
| Vital signs | |
| Systolic blood pressure (mmHg) | 126.5 (110.0-145.0) |
| Diastolic blood pressure (mmHg) | 75.0 (70.0-81.0) |
| Heart rate (frequency/min) | 83.0 (76.0-92.0) |
| Respiratory rate (frequency/min) | 20.0 (20.0-23.0) |
| Body temperature (°C) | 37.2 (36.9-37.8) |
| O2 saturation (%) | 96.0 (94.0-97.9) |
| Clinical data | |
| Use of ventilator, N (%) | 12 (22.2) |
| Use of ECMO, N (%) | 5 (9.3) |
| Hospital stay (day) | 28.0 (18.0-41.0) |
| In-hospital mortality, N (%) | 14 (25.9) |
| 30-day mortality, N (%) | 10 (18.5) |
| Laboratory data | |
| WBC ( × 109/L) | 6.3 (5.0-7.7) |
| ANC ( × 109/L) | 4.6 (3.2-6.1) |
| Lymphocyte ( × 109/L ) | 1.0 (0.7-1.5) |
| N/L ratio | 4.1 (2.5-8.6) |
| Hb (g/L) | 117.0 (109.0-130.0) |
| Hct (%) | 35.0 (32.8-37.9) |
| P LT ( × 109/L) | 219.0 (157.0-306.0) |
| AST (IU/L) | 30.0 (24.0-42.0) |
| ALT (IU/L) | 25.0 (15.0-43.3) |
| ALP (IU/L) | 72.0 (63.0-85.0) |
| Total bilirubin (umol/L) | 11.9 (8.6-17.1) |
| Direct bilirubin (umol/L) | 3.4 (1.7-6.8) |
| LDH (U/L) | 516.0 (421.0-677.0) |
| BUN (mmol/L) | 5.7 (3.6-8.6) |
| Cr (µmol/L) | 70.7 (53.0-97.2) |
| Lactate (mmol/L) | 2.0 (1.3-2.4) |
| CRP (mg/L) | 31.0 (5.0-125.0) |
| Blood culture positive†, N (%) | 1 (1.9) |
| PCT (ng/mL) | 0.09 (0.04-0.31) |
| Presepsin (pg/mL) | 367.0 (182.0-859.0) |
| Severity assessment | |
| SOFA score | 3.0 (1.0-6.0) |
| SOFA score ≥ 2, N (%) | 39 (72.2) |
| SOFA score: range | 0-14 |
| 0 (4, 7.4%); 1 (11, 20.3%); 2 (8, 14.8%); 3 (8, 14.8%); 4 (7, 13.0%); 5 (2, 3.7%); 6 (2, 3.7%); 7 (2, 3.7%); 8 (1, 1.9%); 9 (3, 5.6%); 11 (4, 5.6%); 12 (2, 1.9%); 14 (2, 3.7%) | |
| WHO disease severity, N (%) | |
| Mild disease | 0 (0.0) |
| Moderate disease (pneumonia) | 15 (27.8) |
| Severe disease (severe pneumonia) | 0 (0.0) |
| Critical disease | 39 (72.2) |
| ARDS‡ | 10 (18.5) |
| Sepsis | 32 (82.1) |
| Septic shock | 6 (15.3) |
| Acute thrombosis§ | 1 (11.1) |
| VACO index (%) | 12.1 (5.3-18.0) |
Data are represented as number (percentage) or median (interquartile range).
*Gastrointestinal symptoms include anorexia, nausea, abdominal pain, abdominal distension, or diarrhea; †Blood culture results were obtained from 35 patients at enrollment; ‡ARDS with sepsis (N=6) and ARDS with septic shock (N=4); §One COVID-19 patient presenting with limb muscle weakness was diagnosed as having acute stroke with sepsis at enrollment.
Abbreviations: COVID-19, coronavirus disease; ECMO, extracorporeal membrane oxygenation; WBC, white blood cell; ANC, absolute neutrophil count; N/L ratio, neutrophil:lymphocyte ratio; Hb, hemoglobin; Hct, hematocrit; PLT, platelets; AST, aspartate aminotransferase; ALT, alanine aminotransferase; ALP, alkaline phosphatase; LDH, lactate dehydrogenase; BUN, blood urea nitrogen; Cr, creatinine; CRP, C-reactive protein; PCT, procalcitonin; SOFA, sequential organ failure assessment; ARDS, acute respiratory distress syndrome; VACO, Veterans Health Administration COVID-19.
A comparison of PCT and presepsin levels, SOFA score, WHO disease severity, and VACO index for predicting the 30-day mortality is presented in Table 2. The median values of PCT, presepsin, and the VACO index differed significantly between survivors and non-survivors (0.06 ng/mL vs. 0.49 ng/mL, 287.0 pg/mL vs. 1,479.0 pg/mL, 10.0% vs. 20.5%; all P<0.05). However, the median value of the SOFA score and rate of critical disease did not differ significantly between the groups (3.0 vs. 8.0, 70.5% vs. 80.0%; all P>0.05).
Table 2.
Comparison of PCT, presepsin, the SOFA score, WHO disease severity, and the VACO index in hospitalized COVID-19 patients according to 30-day mortality
| Variable | Survivors (N=44) | Non-survivors (N=10) | P |
|---|---|---|---|
| PCT (ng/mL) | 0.06 (0.04-0.14) | 0.49 (0.31-2.71) | < 0.001 |
| Presepsin (pg/mL) | 287.0 (173.5-580.0) | 1,479.0 (962.0-2,148.0) | < 0.001 |
| SOFA score | 3.0 (1.0-4.0) | 8.0 (2.0 –11.0) | 0.073 |
| WHO disease severity, N (%) | |||
| Moderate | 13 (29.5) | 2 (20.0) | 0.708 |
| Critical | 31 (70.5) | 8 (80.0) | |
| ARDS | 6 (13.6) | 4 (40.0) | 0.075 |
| Sepsis | 27 (61.4) | 5 (50.0) | 0.513 |
| Septic shock | 3 (6.8) | 3 (30.0) | 0.069 |
| Acute thrombosis | 1 (2.3) | 0 (0.0) | 1.000 |
| VACO index (%) | 10.0 (5.1-16.6) | 20.5 (13.7-20.5) | 0.011 |
Data are represented as number (percentage) or median (interquartile range).
Abbreviations: PCT, procalcitonin; SOFA, sequential organ failure assessment; ARDS, acute respiratory distress syndrome; VACO, Veterans Health Administration COVID-19.
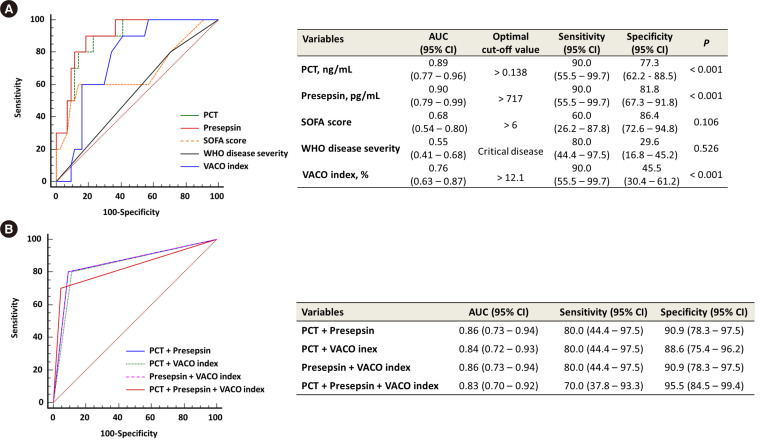
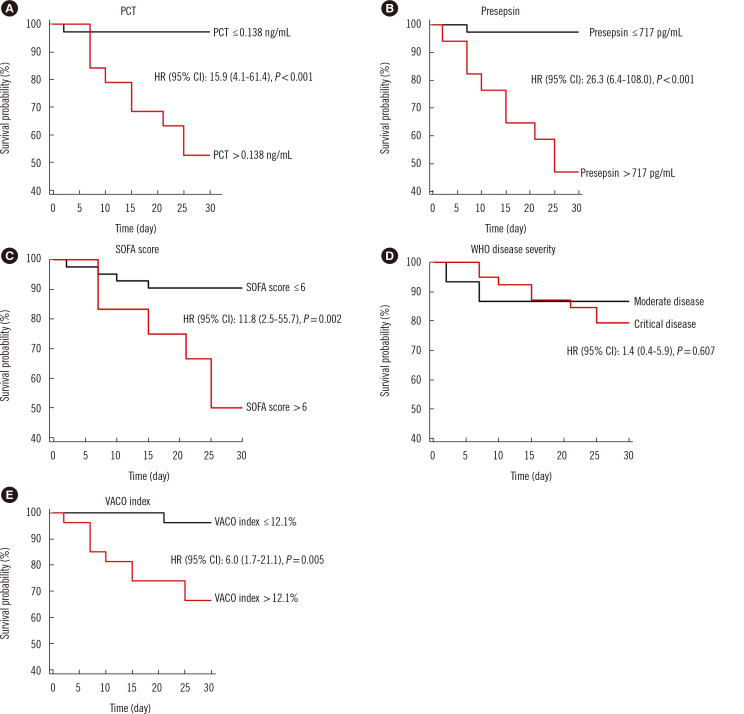
In the ROC curve analysis, PCT and presepsin levels and the VACO index comparably predicted the 30-day mortality (0.89 vs. 0.90 vs. 0.76, all P>0.05); the optimal cut-off values for 30-day mortality were 0.138 ng/mL for PCT, 717 pg/mL for presepsin, and 12.1% for the VACO index (Fig. 2A). The SOFA score and WHO disease severity could not predict 30-day mortality. Compared with each marker or index, the multimarker approach combining PCT, presepsin, and VACO index using the respective optimal cut-off values showed no significant difference for predicting 30-day mortality (Fig. 2B). In the Kaplan–Meier survival analysis, HR (95% CI) for predicting 30-day mortality was 15.9 (4.1-61.3) for PCT, 26.3 (6.4-108.0) for presepsin, 11.8 (2.5-55.7) for the SOFA score, 1.4 (0.4-5.9) for WHO disease severity of critical disease, and 6.0 (1.7-21.1) for the VACO index (Fig. 3).
Fig. 2.
ROC curve analysis of PCT, presepsin, the SOFA score, WHO disease severity, the VACO index, and multimarker approaches for predicting 30-day mortality. (A) PCT, presepsin, the SOFA score, WHO disease severity, and the VACO index. (B) Multimarker approaches using the above optimal cut-off values of PCT, presepsin, and the VACO index. Abbreviations: PCT, procalcitonin; SOFA, sequential organ failure assessment; VACO, Veterans Health Administration COVID-19; AUC, area under the ROC curve; CI, confidence interval.
Fig. 3.
Kaplan–Meier survival curves of PCT, presepsin, the SOFA score, WHO disease severity, and the VACO index for predicting 30-day mortality. (A) PCT. (B) Presepsin. (C) SOFA score. (D) WHO disease severity. (E) VACO index. Abbreviations: PCT, procalcitonin; SOFA, sequential organ failure assessment; VACO, Veterans Health Administration COVID-19; HR, hazard ratio; CI, confidence interval.
In the reclassification analyses, PCT and presepsin in addition to the VACO index significantly increased IDI and NRI compared with that by the VACO index alone (Table 3). IDI and NRI of presepsin in addition to the VACO index were higher than those of PCT and the VACO index.
Table 3.
Reclassification analysis of multimarker approaches using PCT, presepsin, and the VACO index for 30-day mortality
| Approaches | IDI (95% CI) | P | NRI (95% CI) | P |
|---|---|---|---|---|
| PCT+VACO index | 0.28 (0.04-0.52) | 0.022 | 0.39 (–0.02-0.80) | 0.061 |
| Presepsin+VACO index | 0.36 (0.15-0.56) | < 0.001 | 0.47 (0.21-0.73) | < 0.001 |
| PCT+presepsin+VACO index | 0.46 (0.24-0.69) | < 0.001 | 0.64 (0.32-0.95) | < 0.001 |
IDI and NRI values of multimarker approaches using the above optimal cut-off values of PCT, presepsin, and the VACO index were obtained in comparison with VACO index.
Abbreviations: PCT, procalcitonin; VACO; Veterans Health Administration COVID-19; IDI, integrated discrimination improvement; CI, confidence interval; NRI, net reclassification improvement.
DISCUSSION
We explored the prognostic utility of PCT, presepsin, the VACO index, and their combinations for predicting 30-day mortality in hospitalized COVID-19 patients. As COVID-19 patients with pneumonia were mostly hospitalized in YUMC during the study period, the study population included only patients with moderate and critical diseases according to WHO disease severity, with a skewed distribution. Our data showed that the VACO index was significantly higher in non-survivors than in survivors and may be applicable in clinical practice. To our knowledge, no published study has compared the VACO index with other markers in COVID-19. One study reported that a median VACO index of 10.0% and 20.5% in survivors and non-survivors, respectively, indicated high risk and very high risk, respectively. The AUC of the VACO index for 30-day mortality ranged from 0.78 to 0.84 in the VA and Yale New Haven Hospital cohorts [9, 10], consistent with our data. Previous studies reported that the SOFA score and disease severity showed significant differences according to clinical outcome [2, 4, 17]; however, the SOFA score and WHO disease severity did not differ significantly between survivors and non-survivors in our study.
Based on our data, similar to the VACO index, PCT and presepsin levels were significantly higher in non-survivors than in survivors. A PCT level of 0.5 ng/mL is considered the cut-off for sepsis [15, 16]. Although most patients presented with sepsis or septic shock in this study, the median PCT levels in survivors and non-survivors were below 0.5 ng/mL. The prognostic utility of PCT in COVID-19 is arguable, since it is in the normal range in most patients [4, 11, 17]. This may be due to the absence of bacterial infection and downregulation of PCT by IFN-γ released during viral infection [11]. It has been recommended that PCT level should be regularly monitored for detecting secondary bacterial infection in COVID-19 patients [13]. In this study, one patient among the 10 non-survivors had the highest PCT value (8.69 ng/mL), with positive blood culture results, indicating the presence of bacterial infection.
Based on our data, presepsin reflects clinical severity of COVID 19 better than PCT. Unlike PCT, the median level of presepsin in survivors was below the upper reference limit (URL), whereas that in non-survivors was approximately four times the URL. Kocyigit, et al. [24] reported that presepsin and IL-6 levels significantly increased according to COVID-19 disease severity and positively correlated with each other and COVID-19 disease severity. Zaninotto, et al. [25] reported that the median level of presepsin was significantly higher in non-survivors than in survivors (1,047 vs. 417 pg/mL, P<0.05). Monocytes and cytokines, such as IL-6 and tumor necrosis factor α, which are associated with COVID-19 pathogenesis, are involved in the secretion of presepsin and PCT, respectively [6, 12, 16, 22]. Severe COVID-19 infection can cause systemic hyperinflammation, during which the levels of several cytokines, such as monocyte chemoattractant protein 1 and macrophage inflammatory protein 1a, are increased; these may stimulate the production of presepsin more than that of PCT [6]. In previous studies on septic patients, presepsin showed greater diagnostic and prognostic values than PCT [21-23]. Taken together, compared with PCT, presepsin may show better clinical utility in terms of prognosis prediction in critically ill patients.
This study demonstrated a comparable performance of PCT and presepsin to the VACO index in predicting 30-day mortality. Although all combinations of PCT, presepsin, and the VACO index were comparable in predicting 30-day mortality, the AUC of combined PCT and presepsin was slightly higher than that of PCT, presepsin, and the VACO index combined. Our data showed slightly higher AUCs of PCT and presepsin than that of the VACO index, indicating that the biomarkers, even when used alone, can predict 30-day mortality in COVID-19 patients. The AUCs of presepsin and presepsin and the VACO index combined were slightly higher than those of PCT and PCT and the VACO index combined, respectively. This suggests that presepsin may better predict 30-day mortality in COVID-19 patients than PCT. In previous studies, the SOFA score showed the ability to predict in-hospital mortality in COVID-19 patients [29]; however, it did not predict 30-day mortality as did WHO disease severity in our study.
Our study findings showed not only significantly high HRs of PCT, presepsin, and the VACO index above the respective cut-off values but also significantly added values of PCT and presepsin to the VACO index. Presepsin demonstrated significantly higher contribution to the VACO index than PCT. Thus, biomarkers added to the clinical index increase the performance for predicting 30-day mortality in COVID-19 patients. Presepsin may be more useful for predicting 30-day mortality in COVID-19 patients than PCT. Biomarker-based and multimarker approaches using biomarkers and a clinical scoring system (SOFA score) would be useful for predicting the prognosis of sepsis patients [15, 22]. To our knowledge, no published study has suggested a prognostic model measuring PCT or presepsin levels for 30-day mortality in COVID-19 patients. Further studies using larger study populations are needed to incorporate PCT or presepsin into a prognostic model for 30-day mortality in COVID-19 patients.
This study had several limitations. First, although the sample size was sufficient for statistical analysis, this study population was limited to patients with moderate and critical diseases according to WHO disease severity, which may have affected our data. Second, blood sampling and severity assessment were conducted at the time of enrollment, and thus, our data may have been affected by the heterogeneous clinical course of COVID-19 [4, 30]. Third, we only assessed PCT and presepsin levels and the VACO index with regard to 30-day mortality in COVID-19 patients; non-specific prognostic biomarkers, including other hematological and biochemical markers [11, 13], and the prediction of disease severity were not within the scope of this study.
In conclusion, this was the first study to investigate the prognostic utility of PCT, presepsin, the VACO index, and their combinations for predicting 30-day mortality in COVID-19 patients. PCT, presepsin, and the VACO index showed comparable performance in predicting 30-day mortality in hospitalized COVID-19 patients. PCT and presepsin in addition to the VACO index may be a more reliable prognostic approach than using the VACO index alone. Further studies are needed to support our findings and implement the combined use of biomarkers and a clinical index in clinical practice.
ACKNOWLEDGEMENTS
None declared.
Footnotes
AUTHOR CONTRIBUTIONS
Park M designed the study, analyzed the data, and wrote the draft; Hur M conceived the study, analyzed the data, and finalized the draft; Kim HY collected blood samples; Kim H, Lee CH, and Lee, JH, and Nam M discussed the data and reviewed the manuscript. All authors read and approved the final manuscript.
CONFLICT OF INTEREST
None declared.
RESEARCH FUNDING
None declared.
REFERENCES
- 1.Hong KH, Lee SW, Kim TS, Huh HJ, Lee J, Kim SY, et al. Guidelines for laboratory diagnosis of coronavirus disease 2019 (COVID-19) in Korea. Ann Lab Med. 2020;40:351–60. doi: 10.3343/alm.2020.40.5.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim SW, Kim SM, Kim YK, Kim JY, Lee YM, Kim BO, et al. Clinical characteristics and outcomes of COVID-19 cohort patients in Daegu metropolitan city outbreak in 2020. J Korean Med Sci. 2021;36:e12. doi: 10.3346/jkms.2021.36.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee JY, Hong SW, Hyun M, Park JS, Lee JH, Suh YS, et al. Epidemiological and clinical characteristics of coronavirus disease 2019 in Daegu, South Korea. Int J Infect Dis. 2020;98:462–6. doi: 10.1016/j.ijid.2020.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoo EH, Chang SH, Song DY, Lee CH, Cheong GY, Park S, et al. Comprehensive laboratory data analysis to predict the clinical severity of coronavirus disease 2019 in 1,952 patients in Daegu, Korea. Ann Lab Med. 2022;42:24–35. doi: 10.3343/alm.2022.42.1.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Korea Disease Control and Prevention Agency, author. Current status of COVID-19 outbreak and vaccination in Korea (6.30.) [Updated on Nov 2021]. https://www.kdca.go.kr/board/board.es?mid=a20501010000&bid=0015&list_no=713810&cg_code=&act=view&nPage=41.
- 6.Shaw RJ, Bradbury C, Abrams ST, Wang G, Toh CH. COVID-19 and immunothrombosis: emerging understanding and clinical management. Br J Haematol. 2021;194:518–29. doi: 10.1111/bjh.17664. [DOI] [PubMed] [Google Scholar]
- 7.WHO, author. Living guidance for clinical management of COVID-19. [Updated on Nov 2021]. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2.
- 8.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3) JAMA. 2016;315:801–10. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.King JT, Jr, Yoon JS, Rentsch CT, Tate JP, Park LS, Kidwai-Khan F, et al. Development and validation of a 30-day mortality index based on pre-existing medical administrative data from 13,323 COVID-19 patients: the Veterans Health Administration COVID-19 (VACO) Index. PLoS One. 2020;15:e0241825. doi: 10.1371/journal.pone.0241825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.King JT, Jr, Yoon JS, Bredl ZM, Habboushe JP, Walker GA, Rentsch CT, et al. Accuracy of the Veterans Health Administration COVID-19 (VACO) index for predicting short-term mortality among 1307 US academic medical centre inpatients and 427 224 US Medicare patients. J Epidemiol Community Health. 2021:jech-2021-216697. doi: 10.1101/2021.01.01.20249069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bivona G, Agnello L, Ciaccio M. Biomarkers for prognosis and treatment response in COVID-19 patients. Ann Lab Med. 2021;41:540–8. doi: 10.3343/alm.2021.41.6.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ponti G, Maccaferri M, Ruini C, Tomasi A, Ozben T. Biomarkers associated with COVID-19 disease progression. Crit Rev Clin Lab Sci. 2020;57:389–99. doi: 10.1080/10408363.2020.1770685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Henry BM, de Oliveira MHS, Benoit S, Plebani M, Lippi G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chem Lab Med. 2020;58:1021–8. doi: 10.1515/cclm-2020-0369. [DOI] [PubMed] [Google Scholar]
- 14.Welder D, Jeon-Slaughter H, Ashraf B, Choi SH, Chen W, Ibrahim I, et al. Immature platelets as a biomarker for disease severity and mortality in COVID-19 patients. Br J Haematol. 2021;194:530–6. doi: 10.1111/bjh.17656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hur M, Kim H, Lee S, Cristofano F, Magrini L, Marino R, et al. Diagnostic and prognostic utilities of multimarkers approach using procalcitonin, B-type natriuretic peptide, and neutrophil gelatinase-associated lipocalin in critically ill patients with suspected sepsis. BMC Infect Dis. 2014;14:224. doi: 10.1186/1471-2334-14-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vijayan AL, Vanimaya, Ravindran S, Saikant R, Lakshmi S, Kartik R, et al. Procalcitonin: a promising diagnostic marker for sepsis and antibiotic therapy. J Intensive Care. 2017;5:51. doi: 10.1186/s40560-017-0246-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang G, Hu C, Luo L, Fang F, Chen Y, Li J, et al. Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China. J Clin Virol. 2020;127:104364. doi: 10.1016/j.jcv.2020.104364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tjendra Y, Al Mana AF, Espejo AP, Akgun Y, Millan NC, Gomez-Fernandez C, et al. Predicting disease severity and outcome in COVID-19 patients: a review of multiple biomarkers. Arch Pathol Lab Med. 2020;144:1465–74. doi: 10.5858/arpa.2020-0471-SA. [DOI] [PubMed] [Google Scholar]
- 20.Hu R, Han C, Pei S, Yin M, Chen X. Procalcitonin levels in COVID-19 patients. Int J Antimicrob Agents. 2020;56:106051. doi: 10.1016/j.ijantimicag.2020.106051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang HS, Hur M, Yi A, Kim H, Lee S, Kim SN. Prognostic value of presepsin in adult patients with sepsis: systematic review and meta-analysis. PLoS One. 2018;13:e0191486. doi: 10.1371/journal.pone.0191486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim H, Hur M, Moon HW, Yun YM, Di Somma S GREAT Network, author. Multi-marker approach using procalcitonin, presepsin, galectin-3, and soluble suppression of tumorigenicity 2 for the prediction of mortality in sepsis. Ann Intensive Care. 2017;7:27. doi: 10.1186/s13613-017-0252-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Iskandar A, Arthamin MZ, Indriana K, Anshory M, Hur M, Di Somma S, et al. Comparison between presepsin and procalcitonin in early diagnosis of neonatal sepsis. J Matern Fetal Neonatal Med. 2019;32:3903–8. doi: 10.1080/14767058.2018.1475643. [DOI] [PubMed] [Google Scholar]
- 24.Kocyigit A, Sogut O, Durmus E, Kanimdan E, Guler EM, Kaplan O, et al. Circulating furin, IL-6, and presepsin levels and disease severity in SARS-CoV-2-infected patients. Sci Prog. 2021;104:368504211026119. doi: 10.1177/00368504211026119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zaninotto M, Mion MM, Cosma C, Rinaldi D, Plebani M. Presepsin in risk stratification of SARS-CoV-2 patients. Clin Chim Acta. 2020;507:161–3. doi: 10.1016/j.cca.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fukada A, Kitagawa Y, Matsuoka M, Sakai J, Imai K, Tarumoto N, et al. Presepsin as a predictive biomarker of severity in COVID-19: a case series. J Med Virol. 2021;93:99–101. doi: 10.1002/jmv.26164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nagashima K, Noma H, Sato Y, Gosho M. Sample size calculations for single-arm survival studies using transformations of the Kaplan-Meier estimator. Pharm Stat. 2021;20:499–511. doi: 10.1002/pst.2090. [DOI] [PubMed] [Google Scholar]
- 28.Pencina MJ, D'Agostino RB, Sr, D'Agostino RB, Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–72. discussion 207–12. doi: 10.1002/sim.2929. [DOI] [PubMed] [Google Scholar]
- 29.Raschke RA, Agarwal S, Rangan P, Heise CW, Curry SC. Discriminant accuracy of the SOFA score for determining the probable mortality of patients with COVID-19 pneumonia requiring mechanical ventilation. JAMA. 2021;325:1469–70. doi: 10.1001/jama.2021.1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aguilar RB, Hardigan P, Mayi B, Sider D, Piotrkowski J, Mehta JP, et al. Current understanding of COVID-19 clinical course and investigational treatments. Front Med (Lausanne) 2020;7:555301. doi: 10.3389/fmed.2020.555301. [DOI] [PMC free article] [PubMed] [Google Scholar]