Abstract
Study Design
Survey.
Introduction
AO Spine Research Objectives and Common Data Elements for Degenerative Cervical Myelopathy (AO Spine RECODE-DCM) is an international initiative that aims to accelerate knowledge discovery and improve outcomes by developing a consensus framework for research. This includes defining the top research priorities, an index term and a minimum data set (core outcome set and core data elements set – core outcome set (COS)/core data elements (CDE)).
Objective
To describe how perspectives were gathered and report the detailed sampling characteristics.
Methods
A two-stage, electronic survey was used to gather and seek initial consensus. Perspectives were sought from spinal surgeons, other healthcare professionals and people with degenerative cervical myelopathy (DCM). Participants were allocated to one of two parallel streams: (1) priority setting or (2) minimum dataset. An email campaign was developed to advertise the survey to relevant global stakeholder individuals and organisations. People with DCM were recruited using the international DCM charity Myelopathy.org and its social media channels. A network of global partners was recruited to act as project ambassadors. Data from Google Analytics, MailChimp and Calibrum helped optimise survey dissemination.
Results
Survey engagement was high amongst the three stakeholder groups: 208 people with DCM, 389 spinal surgeons and 157 other healthcare professionals. Individuals from 76 different countries participated; the United States, United Kingdom and Canada were the most common countries of participants.
Conclusion
AO Spine RECODE-DCM recruited a diverse and sufficient number of participants for an international PSP and COS/CDE process. Whilst PSP and COS/CDE have been undertaken in other fields, to our knowledge, this is the first time they have been combined in one process.
Keywords: spinal cord diseases, cervical vertebrae, spondylosis, spinal osteophytosis, surveys and questionnaires
Introduction
Degenerative cervical myelopathy (DCM) is a syndrome of chronic symptomatic spinal cord compression secondary to a range of degenerative pathology in the cervical spine. 1 It is the most common cause of adult spinal cord impairment worldwide,1-3 has a large number of debilitating symptoms4,5 and amongst the worst quality of life of any chronic disease.6,7 Unfortunately, past translational research efforts have been hindered by lack of public awareness and lack of recognition by governmental and non-governmental funders of research. This has been compounded by the lack of standardisation of clinical assessment tools, a lack of preclinical research using translationally relevant models of DCM, a lack of high quality prospective clinical research studies with an excess reliance on small single-centre case series and inadequate synergy between researchers due to the lack of collaborative investigative initiatives.8-11
AO Spine Research Objectives and Common Data Elements for Degenerative Cervical Myelopathy (RECODE-DCM) is an international initiative designed to improve the efficiency of DCM research. 12 A number of objectives are encompassed within the project: the definition of the top DCM research priorities; establishment of a minimum dataset; and agreement of a single index term for the condition. Research priority definition follows James Lind Alliance Priority Setting Partnership (PSP) methodology. The minimum dataset incorporates two separate components, a core outcome set (COS) to include critical outcomes of the disease and a core data element (CDE) set, to include the additional data that should be reported to interpret outcomes. The initiative also aims to encourage international collaboration between all DCM stakeholders: clinicians, researchers, people living with DCM 13 and people supporting those living with DCM.
Degenerative cervical myelopathy stakeholders comprise a diverse group, most obviously people living with DCM, their supporters and spinal surgeons, who are the final common pathway in the management of DCM. 2 However, appropriate clinical suspicion by non-specialists and prompt referral on to specialists is fundamental to effective DCM care. 14 General practitioners, emergency department clinicians, neurologists, physiotherapists, osteopaths and a range of other healthcare professionals are therefore key DCM stakeholders. These latter perspectives have been underrepresented in DCM research to date, and whilst AO Spine and Myelopathy.org represent a large and international community of surgeons and people with DCM respectively, no such community of interested ‘other healthcare professionals’ exists. Achieving a broad and diverse perspective is fundamental to meeting the objectives of AO Spine RECODE-DCM.
The objective of this article is to describe the methods used to achieve a global perspective and the resultant sampling characteristics underpinning the recommendations of AO Spine RECODE-DCM.
Methods
Leadership Team
An international group of DCM stakeholders including spinal surgeons, other healthcare professionals, people with DCM and supporters of people with DCM comprise the AO Spine RECODE-DCM steering committee (SC), with responsibility for the project. A small group comprising an AO Spine Research Manager, a representative from the James Lind Alliance and three clinician-researchers comprise the study management group (MG), which is responsible for day-to-day operations. Global partners were recruited as an extended study group, forming an expert panel of advisors and collaborators. The global partners formed a network of local ambassadors throughout the world for study advertisement and dissemination.
Survey Development
Surveys were developed and piloted by the management group before steering committee piloting and discussion at a series of online meetings, to reach a final consensus.
The first part of the survey was designed to provide background to AO Spine RECODE-DCM, including an educational video and hyperlinks to the project website. The first question divided participants into three stakeholder groups: people with DCM and their supporters, spinal surgeons and other healthcare professionals. The first page of the survey was a registration form capturing basic participant data: age, sex, country of residence, full name, email address and informed consent. For healthcare professionals, the registration form also included questions capturing profession, speciality, job title, hospital/university affiliation, number of people with DCM treated each year, years working with people with DCM and desire to be involved in future DCM research initiatives.
The survey captured a number of additional data points from people with DCM: year of diagnosis, history of surgery, history of physiotherapy, additional DCM treatments, self-reported modified Japanese Orthopaedic Association (mJOA) score, self-rated pain score, previous involvement in DCM research and employment status. For supporters, the same data about the person with DCM were captured, in addition to supporter employment status and involvement of the supporter in previous DCM research.
Following completion of the registration page, participants were randomised to either the PSP or COS/CDE stream, before being presented with further information pertaining to the specific stream. These two processes were split to reduce the length of the survey for each participant but enable a single recruitment process.
For the PSP steam, participants were invited to enter as free text what they thought were the most important DCM research questions within each of the 4 categories of diagnosis, treatment, long-term care and follow-up and other. For a random subset of participants, an identical page followed in which a word-cloud appeared for each category. Word clouds were developed by piloting the PSP questions on approximately 60 individuals from all stakeholder groups. Participant entries from the first page were carried forward, allowing addition of further ideas stimulated by the word clouds.
For the COS stream, a large number of possible outcome variables were developed from previous systematic reviews9,10,15 and interviews.16,17 These were revised into a long list of unique outcomes or data elements by the MG, with approval by the SC. Outcomes were divided into 4 core domains 18 to structure the survey: physiological, life impact, adverse events and resource use (Table 1). These domains were further subdivided into subdomains.
Table 1.
Proposed outcomes presented to participants in the round 1 COS/CDE survey.
| Physiological | Life Impact | Adverse Events | Resource Use |
|---|---|---|---|
| Subdomain: pain | Subdomain: function | Subdomain: complications | Subdomain: financial |
| Arm pain | Falls | Medication side effects | Employment status |
| Finger/hand pain | Mobility | Readmission to hospital | Length of treatment |
| Lower limb pain | Ability to drive | Revision surgery | Cost of care |
| Neck pain | Altered sex life | Dysphagia | Financial problems |
| Headache | Retribution | Dysphonia | Quality of life |
| Muscle spasm/shaking | Insomnia | C5 nerve palsy | |
| Pain control | Fatigue | Other new radiculopathy | |
| Subdomain: other symptoms | Relationship problems | Spinal cord injury | |
| Restless legs | Helplessness | Epidural haematoma | |
| Urinary incontinence | Subdomain: quality of life | CSF leak | |
| Difficulty passing urine | Anticipatory anxiety | Dural tear | |
| Faecal incontinence | Frustration | Wound infection | |
| Nocturia | Variability | Spinal fusion | |
| Arm weakness | Dependence | Failure of spinal fusion | |
| Leg weakness | Stigma | Death | |
| Balance | Isolation | ||
| Manual dexterity | Problems with mental health | ||
| Finger strength | Acceptance of symptoms | ||
| Grip strength | Vitality | ||
| Breathlessness | |||
| Numbness | |||
| Paraesthesia | |||
| Sweating/temperature dysregulation | |||
| Subdomain: radiology | |||
| Cervical spine alignment | |||
| Adjacent segment degeneration | |||
| Adequate decompression | |||
| Cord signal change |
Note: COS: core outcome set; CDE: core data elements; CSF: cerebrospinal fluid.
An identical process was undertaken for the CDE survey. The potential core data elements presented to participants in the round 1 survey were mental health, obesity, diabetes, smoking status, other neurological diseases, other diseases, performance status, age, biological sex, ethnicity, medication, illness coping/resilience, welfare support, family history of DCM, length of symptoms, rate of progression, presence of myelopathy, number of previous surgeries, definition of DCM, levels of spinal cord compression, pathology causing spinal cord compression, presence of spinal cord signal change, amount of spinal cord compression, structured non-operative management, nerve root injection, operation type, operated levels, instrumentation, operative approach, intraoperative neurophysiology, post-operative collar and post-operative rehabilitation/physiotherapy.
Surveylet (Calibrum International, Virginia, US) was used for the round 1 survey. Both PSP and COS/CDE streams were built into the same software, with individuals randomised to one stream of the survey only. The SC agreed on a pre-defined sampling aim of 25% spinal surgeons, 25% other healthcare professionals and 50% people with DCM.
Survey Piloting
All members of the SC and MG completed the survey in a pilot-run. Technical issues such as typographical errors, problems with hyperlinks, video playback and navigation buttons within the survey were identified and corrected before a further round of piloting. Piloting was repeated until all SC and MG members approved the final survey.
Global Contact Directory
An international contact directory was compiled of DCM stakeholder individuals and organisations. A team of medical student researchers was recruited and trained to assist with directory development. All 53 countries with DCM research output over the past 20 years 8 were the initial focus of the directory. Students were each assigned several countries. Within each country, students compiled a list of names and contact email addresses for stakeholder individuals such as neurosurgeons, orthopaedic surgeons, neurologists, general practitioners and physiotherapists. Students also included contact details for stakeholder organisations such as medical charities, universities, medical colleges, hospitals and medical journals. The directory was compiled manually; no commercial datasets were acquired. In total, 1010 organisations and 3889 individuals were included. An estimated 90% of individuals in the directory were spinal or neurological surgeons. A small number of organisations agreed to disseminate the survey to their members.
Email Campaign
An email campaign targeted at stakeholders in the contact directory was executed using MailChimp (Georgia, US). Emails provided a concise introduction to AO Spine RECODE-DCM and explained that we had identified the individual as someone who may be interested in participating. Email style was alternated between emails with colourful infographics and an embedded introductory video and emails consisting of simple plain text. Real-time analytic data were utilised to optimise email advertisements. Unique emails were sent to individuals and organisations. Recipients were offered the opportunity to opt-out via a link in every email. All emails included a contact email address. Stakeholders who did not wish to participate contacted our research manager requesting to be removed from subsequent emails.
Interim analysis of respondent demographics identified underrepresentation of the other healthcare professional group. An additional global contact directory consisting of 1511 other healthcare professional stakeholders was therefore developed.
Dissemination and Recruitment
A total of 5 emails were sent to the global contact directory, each separated by approximately 1 week; 3 emails were sent to the directory of organisations, each separated by approximately 2 weeks; 2 emails were sent to the directory of other healthcare professionals, separated by approximately 2 months. These mailing intervals were selected based on email performance data. The aim was to maximise response rate whilst avoiding overwhelming respondents.
Myelopathy.org is an international DCM charity with an online community of thousands of people with DCM. The charity website and its social media channels were utilised to target people with DCM and their supporters. Social media posts were utilised to solicit stakeholder views in survey design, including word cloud development, and to recruit people with DCM to complete the survey. AO Spine is the largest international community of spinal healthcare professionals. The organisation was utilised to advertise the study via its website and social media outlets. AO Spine RECODE-DCM also has a designated page on the AO Spine website (https://aospine.aofoundation.org/research/recode-dcm). Advertisements were also published in newsletters and online by organisations, including the World Federation of Neurosurgical Societies and the European Association of Neurosurgical Societies.
A study website was established (https://recode-dcm.com/). The website hosts background information about DCM and the AO Spine RECODE-DCM project, regular progress updates, study protocols, participant information sheets, privacy, consent and GDPR statements. It also formed a key method of dissemination and recruitment.
Analytics
Urchin Tracking Module (UTM) survey links were sent to each organisation. This enabled each organisation to receive a unique hyperlink, which was tracked in AO Spine RECODE-DCM Google Analytics account. UTMs were also utilised for each dissemination strategy targeted at individuals. UTMs, therefore, enabled evaluation of the study recruitment strategies.
Results
Engagement
In total, 208 people or supporters of people with DCM, 389 spinal surgeons and 157 other healthcare professionals participated.
Definition of Survey Endpoints
For the PSP, the survey endpoint was defined when saturation of uncertainties was achieved. This was identified by analysis of submitted uncertainties until no new uncertainties had been suggested in the preceding month. The survey was terminated at saturation, despite not meeting pre-defined sampling criteria. The PSP survey was live for 12 weeks, with PSP/COS randomisation paused for the final 6 weeks to direct all participants into the PSP stream.
The COS/CDE survey responses involved ranking a list of possible outcomes; hence, the concept of saturation did not apply. The survey was open for 9 months in total, with all participants initially randomised to the PSP or COS/CDE streams for 6 weeks, all directed to the PSP for 6 weeks period, before all being directed to the COS/CDE stream after the PSP closed in August 2019. The SC agreed to close the COS/CDE survey on February 20, 2020 as responses had fallen to negligible levels.
Sampling Characteristics
For the PSP and COS/CDE, the mean ages of people with DCM were 57.1 and 56.6 years, with a male representation of 36.8% and 25.7%, respectively. The United States (37.9% and 28.6%) and the United Kingdom (31.6% and 35.2%) were the most common countries of participants (Table 2). Mean mJOA scores were 11.7 and 12.0, with 81.1% and 75.2% of participants having undergone surgery and 64.2% and 62.8% of participants having undergone physiotherapy for the PSP and COS/CDE streams, respectively. For spinal surgeons, the mean number of years managing DCM patients was 13.9 and 13.2 years for the PSP and COS/CDE stream, with an average of 25-50 patients managed yearly for both streams. For the other healthcare professionals group, the mean number of years managing DCM patients was 14.5 and 13.3 years for the PSP and COS/CDE stream, with an average of 0–25 patients managed yearly for both streams.
Table 2.
Survey Participant Demographics.
| Demographic | PSP, n (%) | COS/CDE, n (%) |
|---|---|---|
| Person with DCM | n = 95 | n = 113 |
| Age | 57.1 +/−11.0 | 56.6 +/−9.4 |
| Male | 35 (36.8) | 29 (25.7) |
| Country of residence | ||
| United States | 36 (37.9) | 30 (28.6) |
| United Kingdom | 30 (31.6) | 37 (35.2) |
| Uganda | 6 (6.3) | 11 (10.5) |
| Ecuador | 5 (5.3) | 3 (2.9) |
| Ukraine | 2 (2.1) | 7 (6.7) |
| United Arab Emirates | 2 (2.1) | 7 (6.7) |
| Norway | 2 (2.1) | 1 (1.0) |
| India | 2 (2.1) | 0 |
| Lesotho | 1 (1.1) | 0 |
| Netherlands | 1 (1.1) | 2 (1.9) |
| Other | 8 (8.8) | 5 (5.0) |
| Years since diagnosis | 4.9 +/− 4.7 | 5.7 +/− 6.6 |
| Surgery | ||
| Yes | 77 (81.1) | 85 (75.2) |
| Physiotherapy | ||
| Yes | 61 (64.2) | 71 (62.8) |
| mJOA score | 11.7 +/−2.9 | 12.0 +/− 2.6) |
| Pain score | 5.6 +/−2.5 | 5.6 +/− 2.2 |
| Employment | ||
| Full-time employment | 17 (17.9) | 24 (21.2) |
| Part-time employment | 8 (8.4) | 17 (15.0) |
| Unemployed | 7 (7.4) | 8 (7.1) |
| Unable to work | 30 (31.6) | 38 (33.6) |
| Retired | 33 (34.7) | 26 (23.0) |
| Spinal surgeons | n = 231 | n = 158 |
| Age | 44.5 +/− 9.5 | 44.6 +/−10.2 |
| Male | 224 (97.0) | 152 (96.2) |
| Country of practice | ||
| United States | 22 (9.5) | 16 (10.1) |
| India | 20 (8.7) | 17 (10.8) |
| United Kingdom | 17 (17.4) | 16 (10.1) |
| Canada | 14 (6.1) | 7 (4.4) |
| Japan | 14 (6.1) | 8 (5.1) |
| Italy | 11 (4.8) | 11 (7.0) |
| Australia | 10 (4.3) | 7 (4.4) |
| Germany | 8 (3.5) | 6 (3.8) |
| Portugal | 6 (2.6) | 1 (.6) |
| Greece | 6 (2.6) | 3 (1.9) |
| Uganda | 6 (2.6) | 0 (0) |
| South Korea | 6 (2.6) | 2 (1.3) |
| Ukraine | 6 (2.6) | 1 (.6) |
| Other | 85 (36.8) | 63 (39.9) |
| Training speciality | ||
| Neurosurgery | 140 (60.6) | 89 (56.3) |
| Orthopaedics | 91 (39.4) | 69 (43.7) |
| Years managing DCM | 13.9 +/− 11.0 | 13.2 +/−8.5 |
| DCM patients per year | ||
| 0–25 | 43 (18.6) | 37 (23.4) |
| 25–50 | 79 (34.2) | 51 (32.3) |
| 50–100 | 66 (28.6) | 39 (24.7) |
| 100+ | 43 (18.6) | 31 (19.6) |
| Other healthcare professionals | n = 96 | n = 61 |
| Age | 45.5 +/− 12.4 | 42.9 +/−10.2 |
| Male | 54 (56.3) | 38 (62.3) |
| Country of practice | ||
| United States | 16 (16.7) | 6 (10.0) |
| Canada | 16 (16.7) | 15 (25.0) |
| United Kingdom | 9 (9.4) | 7 (11.7) |
| Ireland | 6 (6.3) | 2 (3.3) |
| Italy | 5 (5.2) | 2 (3.3) |
| Australia | 3 (3.1) | 8 (13.2) |
| Switzerland | 3 (3.1) | 3 (5.0) |
| Germany | 3 (3.1) | 0 (0) |
| United Arab Emirates | 3 (3.1) | 3 (5.0) |
| Other | 32 (33.3) | 13 (21.3) |
| Profession | ||
| Family doctor/General practitioner | 9 (9.4) | 2 (3.3) |
| Neurologist | 18 (18.8) | 7 (11.5) |
| Other allied health professional | 13 (13.5) | 9 (14.8) |
| Other medical/surgical doctor | 26 (27.1) | 17 (27.9) |
| Physiotherapist | 11 (11.5) | 19 (31.1) |
| Researcher | 18 (18.8) | 5 (8.2) |
| Specialist nurse | 1 (1.0) | 2 (3.3) |
| Years managing DCM | 14.5 +/− 10.6 | 13.3 +/− 9.3 |
| DCM patients per year | ||
| 0-25 | 56 (58.3) | 34 (55.7) |
| 25-50 | 20 (20.8) | 16 (26.2) |
| 50-100 | 12 (12.5) | 9 (14.8) |
| 100+ | 8 (8.3) | 2 (3.3) |
Note: DCM: degenerative cervical myelopathy; COS: core outcome set; CDE: core data elements; mJOA: modified Japanese Orthopaedic Association.
Global Reach
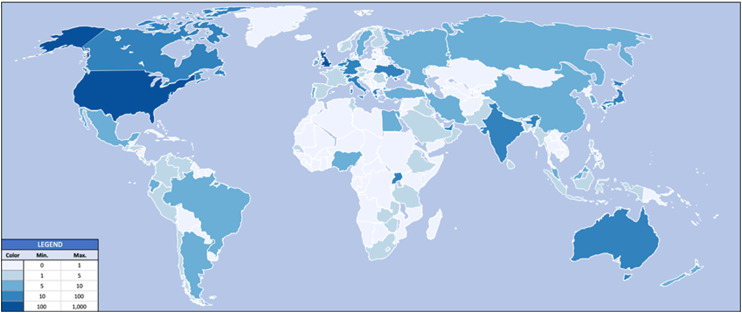
Individuals from 76 countries from 6 continents participated in the round 1 surveys, with the United Kingdom and United States the largest contributors (Figure 1).
Figure 1.
AO Spine RECODE-DCM participants. The darker the colour, the greater the number of participants from that country. Countries shaded in white had zero participants.
Dissemination Strategies
Three separate email campaigns targeted: (1) a mixed group of healthcare professionals consisting largely of surgeons, (2) DCM-relevant organisations and (3) a group of non-surgical other healthcare professionals (Table 3). Overall campaign performance exceeded the MailChimp average open rate of 26.9% and click rate of 3.3%. Engagement from the mixed group of healthcare professionals, consisting largely of surgeons, was greater than that of the two other groups. Emails were opened by individuals from across the globe (Table 4).
Table 3.
Email Campaign Engagement.
| Individuals [% (n)] | Organisations [% (n)] | Other healthcare professionals [% (n)] | ||||
|---|---|---|---|---|---|---|
| Opens | Clicks | Opens | Clicks | Opens | Clicks | |
| One | 38.8 (1509) | 5.4 (209) | 33.8 (329) | 5.9 (57) | 28.4 (426) | 1.5 (23) |
| Two | 35.8 (1384) | 4.0 (155) | 31.0 (300) | 5.2 (50) | 35.0 (515) | 1.4 (20) |
| Three | 39.4 (1521) | 2.0 (77) | 38.8 (372) | 7.8 (75) | ||
| Four | 29.0 (1110) | 2.4 (91) | ||||
| Five | 34.7 (1320) | 5.0 (191) | ||||
Table 4.
Top locations by email opens.
| Top Locations by Email Opens [country] | ||||||
|---|---|---|---|---|---|---|
| Individuals [% (n)] | Organisations [% (n)] | Other healthcare professionals [% (n)] | ||||
| One | United States | 38.5 (1041) | United States | 34.6 (383) | United States | 66.8 (661) |
| United Kingdom | 20.8 (562) | Australia | 12.7 (140) | United Kingdom | 9.9 (98) | |
| China | 8.4 (226) | United Kingdom | 6.4 (71) | Canada | 3.8 (38) | |
| Japan | 3.6 (98) | France | 4.6 (51) | Australia | 2.9 (29) | |
| India | 2.3 (61) | Switzerland | 3.2 (35) | Netherlands | 2.3 (23) | |
| Two | United States | 40.7 (857) | United States | 34.8 (302) | United States | 46.6 (316) |
| China | 12.0 (252) | Ukraine | 13.7 (119) | United Kingdom | 9.9 (67) | |
| United Kingdom | 11.4 (241) | Switzerland | 6.8 (59) | Netherlands | 5.6 (38) | |
| Japan | 6.1 (129) | New Zealand | 5.4 (47) | Australia | 4.1 (28) | |
| Italy | 3.0 (64) | United Kingdom | 5.4 (47) | Belgium | 3.7 (25) | |
| Three | United States | 33.2 (1183) | United States | 21.0 (642) | ||
| United Kingdom | 21.1 (778) | Canada | 12.6 (385) | |||
| China | 8.1 (299) | Switzerland | 12.2 (373) | |||
| Japan | 4.4 (162) | United Kingdom | 10.5 (320) | |||
| Canada | 3.5 (127) | Netherlands | 6.6 (202) | |||
| Four | United States | 44.3 (713) | ||||
| United Kingdom | 9.6 (155) | |||||
| China | 9.6 (154) | |||||
| Japan | 7.1 (115) | |||||
| Canada | 3.0 (48) | |||||
| Five | United States | 40.2 (1080) | ||||
| United Kingdom | 17.6 (472) | |||||
| China | 7.3 (195) | |||||
| Japan | 5.9 (158) | |||||
| United Arab Emirates | 3.7 (99) | |||||
Google Analytics
Over the period the survey was live (May 16, 2019 to February 20, 2020), there were at total of 4767 users of the AO Spine RECODE-DCM website, 79.8% of which were first-time users. In total, there were 8376 sessions and 12593 page views. There were 1.8 sessions per user and 1.5 page views per session; 51.6% of users were female (Table 5). Users from 105 different countries visited the website, with the most users from the United States, the United Kingdom and Canada. The most common sources of website users were direct site visitors (23.1%) and users recruited via the MailChimp email campaign to individuals (19.2%).
Table 5.
AO Spine RECODE-DCM Google Analytics Data.
| Demographic | Percentage (Number) |
|---|---|
| Age (n = 1288) | |
| 18–24 | 5.2 (69) |
| 25–34 | 25.2 (322) |
| 35–44 | 23.9 (315) |
| 45–54 | 19.3 (255) |
| 55–64 | 14.6 (192) |
| 65+ | 11.8 (156) |
| Gender (n = 1301) | |
| Male | 48.4 (634) |
| Female | 51.6 (676) |
| Country (n = 4767) | |
| United States | 28.6 (1377) |
| United Kingdom | 22.7 (1093) |
| Canada | 5.8 (277) |
| Australia | 2.6 (126) |
| Netherlands | 2.6 (125) |
| India | 2.6 (123) |
| Ireland | 2.5 (119) |
| Japan | 2.3 (112) |
| France | 2.2 (106) |
| Switzerland | 1.9 (90) |
| Device (n = 4767) | |
| Desktop | 57.8 (2756) |
| Mobile | 37.1 (1766) |
| Tablet | 5.1 (245) |
| Source | n = 4767 |
| Direct | 23.1 (1501) |
| MailChimp individuals | 19.2 (1249) |
| Link in survey | 9.2 (597) |
| AO spine | 6.2 (404) |
| Myelopathy.org | 6.1 (393) |
| 5.0 (327) | |
| Facebook mobile | 3.9 (250) |
| AO SPINE RECODE-DCM Organisations | 1.5 (100) |
| Student reps | 1.3 (82) |
| MailChimp other healthcare professionals | .9 (57) |
Discussion
Although challenging to implement, the AO Spine RECODE-DCM survey methodology has successfully engaged a global multi-disciplinary cohort of DCM stakeholders, with representation of surgeons, non-surgical healthcare professionals and people with or supporting those with DCM.
Key Demographics
The mean age of people with DCM who participated was in the mid-late 50s, similar to international trial cohorts,19,20 providing reassurance of a representative sample. However, the gender composition was around 70% female, in contrast to male-dominance in trial data, but consistent with previous online DCM surveys, where it has been postulated that this may be due to greater engagement of females with online health initiatives.7,21 The mean age of around 45 for spinal surgeons suggests a large number of experienced consultant/attending surgeons were included; the gender composition of 96% male for the spinal surgeon group roughly matches the gender composition of the speciality.22-25 As expected, although spinal surgeons and other healthcare professionals report similar years of managing people with DCM, the modal number of patients managed per year was much higher for spinal surgeons than other healthcare professionals, perhaps reflecting the predominance of surgeons in the management of DCM 2 and heterogeneity in non-surgical service provision for people with DCM. 26
Large Representation of Surgeons
The SC had agreed a target representation of 25% surgeons, 25% other healthcare professionals and 50% people with DCM and their supporters. In reality, a much greater representation of surgeons of 51.6% was achieved. Targeted efforts directed at non-surgical stakeholder groups were unable to fully redress this. This is not surprising given that DCM is a condition typically managed by surgeons19,20,27 and surgery has dominated the DCM research literature over the past 20 years. 8 Nonetheless, other healthcare professionals and people with DCM and their supporters were represented, making up 27.6% and 20.8% of participants, respectively. Given the desired representation of stakeholders amongst the MG and SC and evidence of information saturation within the survey, this was considered sufficient.
Challenges in Engaging Non-surgical Healthcare Professionals
The difficulty in recruiting healthcare professionals other than spinal surgeons was anticipated. Firstly, this represents a diverse group of professionals, without a single representative body, but also aligns with a poor awareness of DCM linked to significant delays in diagnosis.2,28-30 DCM is currently poorly represented in medical curricula 31 and is referred to by a wide range of different terms,32,33 and the vast majority of research over the past 20 years has been conducted by surgeons. 8
Raising awareness was subsequently identified as the number one research priority for DCM by AO Spine RECODE-DCM. 34 Retaining and growing these perspectives is likely to remain an integral part of supporting progress in DCM. It is hoped therefore that AO Spine RECODE-DCM represents a foundation from which to build upon.
Value of Research Databases
The central tenet of RECODE-DCM is the need for greater standardisation and collaboration in DCM research. 35 A global contact database of all DCM stakeholders may be an effective method of communication. This is born out in our database forming the single most effective source of website traffic, after direct visitors. Our database was developed by identifying individuals and organisations whom we had reason to believe were DCM stakeholders. The success of this initiative is reflected in our email, open and click rates being significantly higher than the MailChimp industry average. Whilst a small number of individuals unsubscribed or contacted our research manager to explain they could not participate for various reasons, we experienced no major complaints from individuals who felt they were not stakeholders. In the long term, an open, online opt-in database of DCM stakeholders will help improve sensitivity and inclusiveness of stakeholder recruitment in future work and aid international collaboration.
Limitations and Reflections
Participant randomisation to PSP and COS/CDE was probably unhelpful. Due to the recruitment rates and an earlier date of the PSP consensus meeting necessitating an earlier end date of the PSP survey, the COS/CDE was temporarily closed to focus on the PSP recruitment. Further participants who had completed the COS/CDE were subsequently invited to submit research uncertainties. Whilst the decision to split these streams was taken to reduce participant attrition, it appeared that the difficulty in engaging a large and diverse community meant that this would have been better kept as one survey, or as sequential surveys.
Organisations were also harder to engage than individuals. Only 2% (100/4767) of AO Spine RECODE-DCM website traffic was directed from third parties. Willingness to assist was often significantly delayed by the necessity for approval by internal reviews and authorisation processes. Therefore, developing relationships and contacting organisations well in advance is an important lesson for future projects.
Developing a global contact directory of all possible stakeholders was an overwhelming task. Focusing our contact directory on the 53 countries with any DCM research output over the past 20 years 8 risked excluding new or under-represented stakeholder voices. Nonetheless, we are reassured by analytics data showing that individuals from 105 different countries visited the project website, with individuals from 76 countries participating. This suggests engagement from individuals not previously involved in DCM research – a key objective of the inclusive, collaborative ethos of RECODE-DCM.
Website traffic was significantly higher than total survey responses, with 4767 website users delivering 754 complete survey responses. Engagement of those stakeholders who visited the website but did not participate in the survey, especially those from countries not previously involved in DCM research, is a focus for future work in developing the AO Spine RECODE-DCM network. The concordance of analytics data from the project website with the final survey data, for example, the UK, US and Canada being the common countries in both datasets, suggests that our analytics data is a good predictor of our survey population.
Conclusions
In a short space of time, AO Spine RECODE-DCM recruited a diverse range of stakeholders, sufficient to inform the PSP and COS/CDE process. Whilst PSP and COS/CDE have been undertaken in other fields, to our knowledge this is the first time they have been combined in one process. The project has laid foundations for an ongoing global, multidisciplinary DCM research collaborative.
Footnotes
Declaration of Conflict of Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The research priorities were organised and funded by AO Spine through the AO Spine Knowledge Forum Spinal Cord Injury, a focused group of international Spinal Cord Injury experts. AO Spine is a clinical division of the AO Foundation, which is an independent medically guided not-for-profit organisation. Study support was provided directly through the AO Spine Research Department.AM is funded by a National Institute for Health Research (NIHR) Clinician Scientists Fellowship award (NIHR CS-2017-17-010) and further supported by the NIHR Biomedical Research Centre (BRC) at University Hospitals Bristol and Weston NHS Foundation Trust and the University of Bristol (BRC-1215-20011). MRNK is supported by the National Institute for Health Research (NIHR) Brain Injury MedTech Co-operative based at Cambridge University Hospitals NHS Foundation Trust and University of Cambridge, and BMD a NIHR Clinical Doctoral Research Fellowship. The views expressed in this publication are those of the authors and not necessarily those of the NIHR.
ORCID iDs
Oliver Mowforth https://orcid.org/0000-0001-6788-745X
George Pickering https://orcid.org/0000-0002-2652-0288
Yuri Hirayama https://orcid.org/0000-0003-2366-2915
Max Butler https://orcid.org/0000-0002-2536-0534
Keerthi Senthil https://orcid.org/0000-0002-8564-3210
Jefferson R. Wilson https://orcid.org/0000-0001-5965-0305
Michael G. Fehlings https://orcid.org/0000-0002-5722-6364
References
- 1.Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG. Degenerative cervical myelopathy. Spine. 2015;40(12):E675-E693. doi: 10.1097/BRS.0000000000000913. [DOI] [PubMed] [Google Scholar]
- 2.Davies BM, Mowforth OD, Smith EK, Kotter MR. Degenerative cervical myelopathy. BMJ. 2018;360:k186. doi: 10.1136/bmj.k186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Badhiwala JH, Ahuja CS, Akbar MA, et al. Degenerative cervical myelopathy-update and future directions. Nat Rev Neurol. 2020;16(2):108-124. doi: 10.1038/s41582-019-0303-0. [DOI] [PubMed] [Google Scholar]
- 4.Davies BM, Munro CF, Kotter MR. A novel insight into the challenges of diagnosing degenerative cervical myelopathy using web-based symptom checkers. J Med Internet Res. 2018;21:e10868. (forthcoming/in press). doi: 10.2196/10868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nouri A, Cheng JS, Davies B, Kotter M, Schaller K, Tessitore E. Degenerative cervical myelopathy: A brief review of past perspectives, present developments, and future directions. J Clin Med. 2020;9(2):535. doi: 10.3390/jcm9020535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oh T, Lafage R, Lafage V, et al. Comparing quality of life in cervical spondylotic myelopathy with other chronic debilitating diseases using the sf-36 survey. World Neurosurg. 2017;106:699-706. doi: 10.1016/j.wneu.2016.12.124.Published Comparing quality of life in cervical spondylotic myelopathy with other chronic debilitating diseases using the sf-36 surveyonline January 5 [DOI] [PubMed] [Google Scholar]
- 7.Mowforth OD, Davies BM, Kotter MR. Quality of life among informal caregivers of patients with degenerative cervical myelopathy: Cross-sectional questionnaire study. Interact J Med Res. 2019;8(4):e12381. doi: 10.2196/12381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mowforth OD, Davies BM, Goh S, O’Neill CP, Kotter MRN. Research inefficiency in degenerative cervical myelopathy: Findings of a systematic review on research activity over the past 20 years. Global Spine J. 2020;10(4):476-485. doi: 10.1177/2192568219847439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davies BM, McHugh M, Elgheriani A, et al. The reporting of study and population characteristics in degenerative cervical myelopathy: A systematic review. PloS One. 2017;12(3):e0172564. doi: 10.1371/journal.pone.0172564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davies BM, McHugh M, Elgheriani A, et al. Reported outcome measures in degenerative cervical myelopathy: A systematic review. PloS One. 2016;11(8):e0157263. doi: 10.1371/journal.pone.0157263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khan DZ, Khan MS, Kotter MR, Davies BM. Tackling research inefficiency in degenerative cervical myelopathy: Illustrative review. JMIR Res Protoc. 2020;9(6):e15922. doi: 10.2196/15922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davies BM, Khan DZ, Mowforth OD, et al. RE-CODE DCM (REsearch objectives and common data elements for degenerative cervical myelopathy): A consensus process to improve research efficiency in dcm, through establishment of a standardized dataset for clinical research and the definition of the research priorities. Global Spine J. 2019;9(suppl l):65S-76S. doi: 10.1177/2192568219832855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boerger TF, Davies BM, Sadler I, Sarewitz E, Kotter MRN. Patient, sufferer, victim, casualty or person with cervical myelopathy: Let us decide our identifier. Integr Healthc J. 2020;2(1):e000023. doi: 10.1136/ihj-2019-000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hilton B, Tempest-Mitchell J, Davies B, Kotter M. Route to diagnosis of degenerative cervical myelopathy in a UK healthcare system: A retrospective cohort study. BMJ Open. 2019;9(5):e027000. doi: 10.1136/bmjopen-2018-027000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tetreault L, Lange SF, Chotai S, et al. A systematic review of definitions for neurological complications and disease progression in patients treated surgically for degenerative cervical myelopathy. Spine. 1976;44(18):1318-1331. doi: 10.1097/BRS.0000000000003066.2019 [DOI] [PubMed] [Google Scholar]
- 16.Davies BM, Munro C, Khan DZ, et al. Outcomes of degenerative cervical myelopathy from the perspective of persons living with the condition: Findings of a semistructured interview process with partnered internet survey. Global Spine J. 2020;18:2192568220953811. doi: 10.1177/2192568220953811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khan DZ, Fitzpatrick SM, Hilton B, et al. Prevailing outcome themes reported by people with degenerative cervical myelopathy: Focus group study. JMIR Form Res. 2021;5(2):e18732. doi: 10.2196/18732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boers M, Kirwan JR, Wells G, et al. Developing core outcome measurement sets for clinical trials: OMERACT filter 2.0. J Clin Epidemiol. 2014;67(7):745-753. doi: 10.1016/j.jclinepi.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 19.Fehlings MG, Wilson JR, Kopjar B, et al. Efficacy and safety of surgical decompression in patients with cervical spondylotic myelopathy: Results of the AOSpine North America prospective multi-center study. J Bone Joint Surg Am. 2013;95(18):1651-1658. doi: 10.2106/JBJS.L.00589. [DOI] [PubMed] [Google Scholar]
- 20.Fehlings MG, Ibrahim A, Tetreault L, et al. A global perspective on the outcomes of surgical decompression in patients with cervical spondylotic myelopathy: Results from the prospective multicenter AOSpine international study on 479 patients. Spine. 2015;40(17):1322-1328. doi: 10.1097/BRS.0000000000000988. [DOI] [PubMed] [Google Scholar]
- 21.Mowforth OD, Davies BM, Kotter MR. The use of smart technology in an online community of patients with degenerative cervical myelopathy. JMIR Form Res. 2019;3(2):e11364. doi: 10.2196/11364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Benzil DL, Abosch A, et al. The future of neurosurgery: A white paper on the recruitment and retention of women in neurosurgery. J Neurosurg. 2008;109(3):378-386. doi: 10.3171/JNS/2008/109/9/0378. [DOI] [PubMed] [Google Scholar]
- 23.Royal College of Surgeons of England . Statistics; 2021. https://www.rcseng.ac.uk/careers-in-surgery/women-in-surgery/statistics/. Accessed April 26, 2021. [Google Scholar]
- 24.Post AF, Dai JB, Li AY, et al. Workforce analysis of spine surgeons involved with neurological and orthopedic surgery residency training. World Neurosurg. 2019;122:e147-e155. doi: 10.1016/j.wneu.2018.09.152. [DOI] [PubMed] [Google Scholar]
- 25.Hiller KP, Boulos A, Tran MM, Cruz AI. What are the rates and trends of women authors in three high-impact orthopaedic journals from 2006-2017?. Clin Orthop Relat Res. 2020;478(7):1553-1560. doi: 10.1097/CORR.0000000000001043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Butler MB, Mowforth OD, Badran A, et al. Provision and perception of physiotherapy in the nonoperative management of degenerative cervical myelopathy (DCM): A cross-sectional questionnaire of people living with DCM. Global Spine J. 2020;1:2192568220961357. doi: 10.1177/2192568220961357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fehlings MG, Tetreault LA, Riew KD, et al. A clinical practice guideline for the management of patients with degenerative cervical myelopathy: Recommendations for patients with mild, moderate, and severe disease and nonmyelopathic patients with evidence of cord compression. Global Spine J. 2017;7(suppl l):70S-83S. doi: 10.1177/2192568217701914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pope DH, Mowforth OD, Davies BM, Kotter MRN. Diagnostic delays lead to greater disability in degenerative cervical myelopathy and represent a health inequality. Spine. 2020;45:368-377. doi: 10.1097/BRS.0000000000003305. [DOI] [PubMed] [Google Scholar]
- 29.Behrbalk E, Salame K, Regev GJ, Keynan O, Boszczyk B, Lidar Z. Delayed diagnosis of cervical spondylotic myelopathy by primary care physicians. Neurosurg Focus. 2013;35(1):E1. doi: 10.3171/2013.3.FOCUS1374. [DOI] [PubMed] [Google Scholar]
- 30.Mowforth O, Davies B, Stewart M, et al. Current provision of myelopathy education in medical schools in the UK: Protocol for a national medical student survey. BMJ Open. 2020;10(8):e035563. doi: 10.1136/bmjopen-2019-035563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Waqar M, Wilcock J, Garner J, Davies B, Kotter M. Quantitative analysis of medical students' and physicians' knowledge of degenerative cervical myelopathy. BMJ Open. 2020;10(1):e028455. doi: 10.1136/bmjopen-2018-028455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Khan DZ, Khan MS, Kotter MR, Davies BM. Tackling research inefficiency in degenerative cervical myelopathy: Illustrative review. JMIR Res Protoc. 2020;9(6):e15922. doi: 10.2196/15922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khan DZ, Davies BM, Kotter MRN. Spinal research-a field in need of standardization. J Rheumatol. 2020;47(4):633-634. doi: 10.3899/jrheum.191225. [DOI] [PubMed] [Google Scholar]
- 34.Davies BM, Khan DZ, Mowforth OD, et al. RE-CODE DCM (REsearch objectives and common data elements for degenerative cervical myelopathy): A consensus process to improve research efficiency in DCM, through establishment of a standardized dataset for clinical research and the definition of the research priorities. Global Spine J. 2019;9(suppl l):65S-76S. doi: 10.1177/2192568219832855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mowforth OD, Starkey ML, Kotter MR, Davies BM. Letter to the Editor. The need for research prioritization in cervical myelopathy. J Neurosurg Spine. 2020;32:777-779. doi: 10.3171/2019.11.SPINE191300. [DOI] [PubMed] [Google Scholar]