Abstract
Background
Recent advances in remote cardiac monitoring technology have created new challenges for clinicians and staff working in device clinics who are left processing large volumes of data. Often, this process is fractured and inefficient, with occurrence of unnecessary alerts that strain staff time and resources.
Objective
The purpose of this survey was to identify challenges allied health professional clinicians and staff encounter when managing a remote monitoring device clinic.
Methods
A 27-item mixed methods survey was developed using a Qualtrics-encrypted, anonymous Web survey tool. Demographic information and questions rating satisfaction level for remote device clinic issues were obtained using a 5-point Likert scale. Three open-ended questions were included that addressed challenges and successes in managing a remote monitoring clinic and served as a method for identifying common themes.
Results
Major themes identified were poor connectivity, staffing issues, and large volume of alerts. Approximately 50% of respondents were either satisfied or unsatisfied with issues surrounding managing remote monitoring device clinics. Strategies for success included optimizing alerts, assigning designated staff, and partnering with third-party platforms.
Conclusion
This survey confirms these issues as an opportunity for industry and digital health leaders to determine best practices for incorporating these technologies into patient care.
Keywords: Cardiac implantable electronic device, Defibrillator, Implantable loop recorder, Pacemaker, Remote cardiac monitoring, Wearable health device
Key Findings.
-
▪
A total of 45 Heart Rhythm Society Allied Health Professionals representing the United States (40), United Kingdom 3, Australia (1), and Egypt (1) participated in a mixed methods survey examining challenges in managing a remote monitoring device clinic.
-
▪
Approximately 50% of respondents were either satisfied or dissatisfied with issues surrounding managing remote monitoring device clinics. Major themes identified were poor connectivity, staffing issues, and large volume of alerts. The counts of estimated percent remote transmission based on the level of frequency were low (0%–24%), mild (45%–49%), moderate (50%–74%), and high (75%–100%), with a median of 40%. Connectivity was a major concern for 88%, and 76% did not use a third-party data management system for importing, monitoring, and reviewing remote reports.
-
▪
Strategies for success included optimizing standard alerts, assigning designated remote monitoring staff, and partnering with third-party platforms.
Background
Recent advances in remote cardiac monitoring technology have created new challenges for clinicians and staff working in device clinics who frequently are left processing large volumes of data. Often, this process is fractured and inefficient, with the occurrence of unnecessary alerts that strain staff time and resources. Most patients with arrhythmias have some form of cardiac implantable electronic device (CIED), such as an implantable loop recorder, pacemaker, or defibrillator, which can be programmed to perform remote monitoring in the patient’s home and then transmit abnormal rhythms and alerts to the clinics. Most of the major manufacturers of CIEDs have their own remote monitoring systems with an accompanying Web site portal for access to reports and alerts. Accessing this information is time-consuming and inefficient. Some clinics have opted to use a third-party digital platform that consolidates all reports and data into a single repository. Another way clinics have reduced staff demand is by tailoring alerts to nonactionable alerts that do not require an intervention, such as arrhythmia detection for patients with known asymptomatic bradycardia or permanent atrial fibrillation (AF). A recent position paper discussed the challenges and possible solutions to the vast amount of digital health data by creating an algorithm that has decision support for the type of alert and to whom it should be triaged, whether it be the physician, nurse practitioner (NP), registered nurse (RN), or other staff.1 Digital health is the use of digital information, data, and communication technologies to collect, share, and analyze health information in order to improve patient health and care delivery. Increasingly, cardiac patients are presenting electronic data from their smart watches and other wearable health devices to providers so that they can screen for and identify possible arrhythmias. This article serves as an impetus for examining our current state of technology and capacity to support remote monitoring device clinics.
The purpose of this research was to survey Heart Rhythm Society (HRS) allied health professionals (AHPs), with the goal of identifying challenges clinicians and staff encounter when managing a remote monitoring device clinic. The specific aims are to (1) identify staffing and workflow patterns; (2) determine how alerts are triaged; (3) evaluate the use of third-party and industry-driven repositories for remote data; and (4) recommend effective strategies for processing remote data.
Methods
A 27-item mixed methods survey was developed using a Qualtrics-encrypted (United States), anonymous Web survey tool that included basic demographic information and specific questions unique to remote monitoring device clinics. Participants were asked to rate their satisfaction level for various aspects of managing remote monitoring device clinics based on a 5-point Likert scale (Table 1). Three open-ended questions were included that addressed challenges and successes in managing a remote monitoring clinic and served as a method for identifying common themes. Content validity was assured, as the survey questions were reviewed by 3 AHP content experts. All HRS AHPs listed on the “Communities” HRS Web portal were invited to participate, including technicians, pharmacists, RNs, advanced practice nurses, and physician assistants (PAs). The survey was deemed exempt by the University of Tennessee Health Science Center Institutional Review Board. The survey and consent disclosure statements were linked to the HRS AHP Communities Web portal and included a message inviting participants to take part in the survey, which was available from June 21, 2021, to August 14, 2021, with an extension and reminder e-mail sent on July 19, 2021. Data were analyzed using descriptive statistics with Microsoft Excel© (Microsoft Corp., Redmond, WA), and internal consistency was analyzed using IBM SPSS Version 27 (IBM Corp., Armonk, NY). Qualitative data were analyzed using thematic analysis.2
Table 1.
Remote monitoring device satisfaction
| Survey questions | Strongly agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Strongly disagree |
|---|---|---|---|---|---|
| You are satisfied with the current patient-to-staff device ratios. | 20.59 | 29.41 | 5.88 | 14.71 | 29.41 |
| Connectivity is a major concern. | 44.12 | 44.12 | 2.94 | 8.82 | 0 |
| You are satisfied with the education patients, staff, and physicians receive from industry regarding remote monitoring systems. | 2.94 | 34.29 | 5.88 | 38.24 | 17.65 |
| Your clinic is adequately staffed to handle a large volume of remote reports. | 23.53 | 26.47 | 2.94 | 17.65 | 29.41 |
| You are satisfied with the present workflow for responding to alerts, patient follow-up, and processing reports. | 20.59 | 20.59 | 11.76 | 23.53 | 23.53 |
| You are satisfied with how your clinic processes alert transmissions after hours. | 29.41 | 14.71 | 8.82 | 29.41 | 17.65 |
| Your staff is knowledgeable about wearable health devices. | 20.59 | 29.41 | 17.65 | 17.65 | 11.76 |
| Your clinic has the technology to process wearable health device data. | 12.12 | 15.15 | 18.18 | 12.12 | 42.42 |
| Your clinic allows for the integration of wearable health device data into the electronic medical record. | 21.21 | 12.12 | 12.12 | 15.15 | 39.39 |
Values are given as percent.
Results
Of the 349 members of the HRS AHP Communities group, a total of 45 (13%) participated in the survey, which was approximately 15–20 minutes in duration and included representation from the United States (40), United Kingdom (3), Australia (1), and Egypt (1). Demographic information showed most were RNs (42.22%), followed by less representation from NPs, PAs, technicians, and others. Eighty percent had more than 10 years of experience, with an age range from 29 to 69 years (Table 2). Patient-to-staff device ratios capable of reprogramming devices and interpreting data ranged from <500:1 (27%); 500–999:1 (36%); 1000–1500:1 (15%); >1500:1 (9%); and not sure (12%).
Table 2.
Demographic information (n = 45)
| Role | |
| RN | 19 (42.22) |
| NP | 14 (31.11) |
| PA | 2 (4.44) |
| Technician | 5 (11.11) |
| Pharmacist | 0 |
| Other | 5 (11.11) |
| Experience (y) | |
| <5 | 2 (4.44) |
| 5–10 | 7 (15.56) |
| >10 | 36 (80) |
| Age (y) | 49 (11.69) |
| Work location | |
| Urbanized area | 43 (95.56) |
| Urbanized cluster | 1 (2.22) |
| Rural | 1 (2.22) |
Categorical variables are given as n (%). Continuous variable is given as mean.
NP = nurse practitioner; PA = physician assistant; RN = registered nurse.
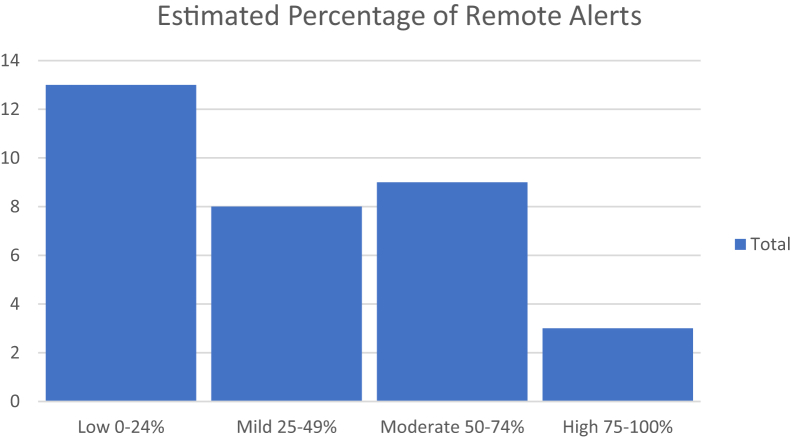
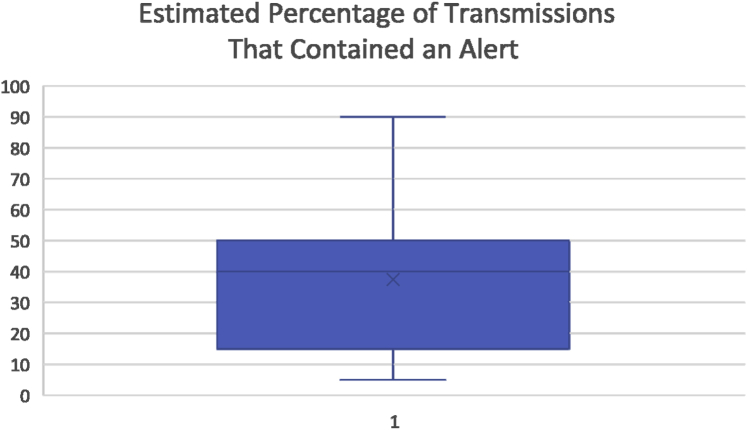
The survey questions were found to be reliable and internally consistent (Cronbach alpha = 0.765). Fifty percent were satisfied with the current patient-to-staff device ratio, but connectivity was a major concern (88%). Approximately half were satisfied with the degree of education that patients, staff, and physicians received from industry representatives with regard to remote monitoring systems. Most clinics (76%) did not use a third-party data management system for importing, monitoring, and reviewing all or most of the CIED reports. Fifty percent were satisfied with the current patient-to-staff device ratio and felt their clinic was adequately staffed to handle a large volume of remote reports. Less (41%) were satisfied with the present workflow for responding to alerts, patient follow-ups, and processing reports. Similarly, 44% were satisfied with how their clinic processed alert transmissions after hours. Fifty percent reported being knowledgeable of wearable health devices, 27% reported their clinic had the technology to process wearable health device data, and 33% of the clinics allowed for the integration of wearable health device data into the electronic medical record (EMR). Respondents were also asked to estimate what percentage of remote transmission their clinic received for alerts. The counts of estimated percent remote transmission were measured and based on the level of frequency as low (0%–24%), mild (45%–49%), moderate (50%–74%), and high (75%–100%) (Figure 1), with a median of 40% (Figure 2).
Figure 1.
Count of reported estimated percentages of remote alerts.
Figure 2.
Estimated percentage of transmissions that contained an alert (25th IQR 15%, 75th IQR 50%). IQR = interquartile range.
Three major themes emerged based on participants being asked to “Describe your biggest challenge in managing patients with remote monitoring” and were identified as follows: connectivity, transmissions, and staffing. Loss of connectivity to remote monitors was identified as a major barrier to managing remote data and included issues such as troubleshooting home monitors, managing disconnections in a timely matter, handling lack of service in rural areas, and addressing inability to tailor alerts without the patient being present in the clinic. The large volume of transmissions was identified as a major barrier and included issues such as dealing with nonclinically actionable alerts not requiring an intervention and unnecessary patient transmissions resulting from nontailored alerts, managing alerts outside clinic hours, and handling lack of uniformity with alert management. Actionable alerts are defined as those requiring initiation or titration of an antiarrhythmic agent or significant device reprogramming, revision, or replacement.3 Staffing was the third major theme and included issues such as lack of CIED-trained staff, lack of staff in general, and keeping staff trained. Data management was noted to be an issue along with a lack of uniformity in billing and a “need for standardization across the country for alert management and billing.” Lack of patient buy-in was also identified as a concern, in that “patients do not want to come into the office for in-clinic checks.”
Two major themes emerged from participants being asked, “What would you consider to be the greatest barrier to having optimal staffing?” These themes were staff training and administrative/financial issues. The low supply of knowledgeable clinicians and staff was identified as a major barrier and included issues such as lack of qualified applicants, lengthy process of training, knowledge regarding electrocardiography, and burnout. Administrative/financial issues included the number of unbillable tasks, difficulty in showing productivity, lack of benchmarks, budget, and workflow. These issues are summarized by the following admission: “The Device Clinic is not viewed as a revenue-generating cost center.”
Three major themes emerged as a result of respondents being instructed to “Describe a process your clinic has adopted that has improved workflow and quality of patient care for patients being remotely monitored.” These were optimizing alert transmissions, increasing remote staffing, and utilizing third-party platforms. Alert transmissions were optimized by creating standardized alert protocols, making postoperative phone calls on how to use a home monitor, and providing “detailed patient education and issuing a remote monitor at time of implant.” Remote monitoring staff were increased using various approaches that including having a full-time remote team working from home, a designated electrophysiology technician, and a dedicated device office person to check insurance and schedules. Training was also emphasized with “Robust, long, on-the-job training for new hires and continued training throughout the year.” Many clinics opted to partner with third-party platforms that interface with the EMR to reduce alerts and manual data entry. Others refined their billing process by billing quarterly and integrating Health Level Seven International (HL7) into the EMR. HL7 is a set of international standards for the transfer of clinical and administrative data between software applications used by various health care providers.4 When asked if clinics had HL7 integration in their EMR, 59% reported yes, 28% reported no, and 12.5% were not sure.
Discussion
Numerous studies have outlined the benefits of remote monitoring for patient care.5,6 These include improved device surveillance and patient clinical management, with a reduction in manpower and more consistent patient follow-up.7, 8, 9 Despite decades of utilization of remote monitoring for CIEDs, there remain significant workflow and staffing barriers to optimal device remote management programs. Patient education, connectivity, and adequate staffing remain themes as opportunities for improvement. Issues related to poor connectivity most likely are multifactorial and related to the type of home monitoring system, patient education, degree of Internet access, and socioeconomic factors. Education for patients regarding the importance of remote monitoring is recommended even before device implantation in the HRS consensus statement; however, patient education remains a barrier to optimal remote monitoring. Staffing also continues to be a question unanswered for adequate staff ratios and skill mix. Another major theme identified was that remote monitoring device clinics were not considered as revenue-generating. This is reflected by the 76% who did not report using a third-party remote monitoring system, which could potentially maximize insurance and Medicare reimbursements.
Results of the survey found that respondents’ estimates of alerts and nonactionable transmissions continue to be a significant workload for device clinics. Although interest in artificial intelligence technology is increasing, there currently remains a need for human device transmission review. One opportunity for further research is defining a best practice for actionable alert programming that is standard among vendors. Ploux et al10 conducted a review of the most common types of remote monitoring systems with an overview of device-specific technical and clinical alerts. They provide programming suggestions and advice for optimizing remote monitoring and alerts for various CIEDs. For implantable cardioverter-defibrillator (ICD) leads, they suggest turning on all ICD lead-related alerts that do not interfere with therapy, enabling the lead noise discrimination algorithm, and routinely monitoring right ventricular lead impedance and R-wave sensing scheduled reports. For ventricular-related alerts, they suggest analyzing all ventricular arrhythmias tracings that are transmitted to identify sources of inappropriate or aborted shock. For atrial arrhythmia–related alerts, they suggest programming the AF detection threshold at their lowest for patients free of AF and increasing the threshold for an AF alert in patients with known AF or high burden. Additional advice and suggestions are made regarding heart failure alerts and patient traveling. The review in general serves as a practical guide for optimizing remote CIED alerts.10
Bluetooth technology and wearable health devices are becoming increasingly familiar to patients as they seek to have control of their own data and be more involved in their health care; however, there remains a digital divide. This survey pointed out that device clinics are largely unprepared to handle these data or have a system by which to enter the data into the EMR.
Study limitations
The main limitation of this survey was the low response rate, which likely is secondary to the short window of time given to take the survey using the HRS AHP Communities Web portal and other coronavirus disease 2019 (COVID-19) pandemic-related issues. Additionally, not all respondents completed all sections of the survey. Other areas that were not addressed and may benefit from future inquiry include international practice issues and the use of industry personnel in US device clinics.
Conclusion
This mixed methods survey highlights the challenges in managing a remote monitoring clinic, suggests possible solutions, and serves as a call to action for societies to assist with guidance. Major themes identified were poor connectivity, staffing issues, and large volume of alerts. Although results were mixed, with approximately 50% of respondents reporting being either satisfied or not satisfied with issues surrounding managing remote monitoring device clinics, some clinics have found solutions through designated staffing, education, standardized remote alerts, third-party platforms, and refined billing processes. The result of the survey confirm these issues as an opportunity for industry and digital health leaders in the electrophysiology arena to determine best practices for incorporating these technologies into patient care and as a call to action for societies to assist with guidance.
Acknowledgments
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosures
The authors have no conflicts to disclose.
Authorship
All authors attest they meet the current ICMJE criteria for authorship.
Ethics Statement
The survey was deemed exempt by the University of Tennessee Health Science Center Institutional Review Board.
Disclaimer
Given her role as Section Editor, Margaret Harvey had no involvement in the peer review of this article and has no access to information regarding its peer review. Full responsibility for the editorial process for this article was delegated to Editors Nazem Akoum and Jeanne E. Poole.
References
- 1.Varma N., Cygankiewicz I., Turakhia M.P., et al. 2021 ISHNE/HRS/EHRA/APHRS collaborative statement on mHealth in arrhythmia management: digital medical tools for heart rhythm professionals: from the International Society for Holter and Noninvasive Electrocardiology/Heart Rhythm Society/European Heart Rhythm Association/Asia Pacific Heart Rhythm Society. Cardiovasc Digit Health J. 2021;2:4–54. doi: 10.1016/j.cvdhj.2020.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garth T., Hayfield N. American Psychological Association; Washington, DC: 2021. Essentials of Thematic Analysis. [Google Scholar]
- 3.Varma N., Love C.J., Michalski J., Epstein A.E. Alert-based ICD follow-up: a model of digitally driven remote patient monitoring. JACC Clin Electrophysiol. 2021;7:976–987. doi: 10.1016/j.jacep.2021.01.008. [DOI] [PubMed] [Google Scholar]
- 4.Health Level Seven International (HL7) HL7 Standards 2021. http://www.hl7.org/implement/standards/index.cfm?ref=nav Available at.
- 5.Varma N., Ricci R.P. Telemedicine and cardiac implants: what is the benefit? Eur Heart J. 2013;34:1885–1895. doi: 10.1093/eurheartj/ehs388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Slotwiner D.J., Varma N., Akar J.G., et al. HRS expert consensus statement on remote interrogation and monitoring for cardiovascular implantable electronic devices. Heart Rhythm. 2015;12:e69–e100. doi: 10.1016/j.hrthm.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 7.Ricci R.P., Morichelli L., D’Onofrio A., et al. Manpower and outpatient clinic workload for remote monitoring of patients with cardiac implantable electronic devices data from the HomeGuide Registry. J Cardiovasc Electrophysiol. 2014;25:1216–1223. doi: 10.1111/jce.12482. [DOI] [PubMed] [Google Scholar]
- 8.Ricci R.P., Morichelli L. Workflow, time, and patient satisfaction from the perspectives of home monitoring. Europace. 2013;15(Suppl 1):i49–i53. doi: 10.1093/europace/eut113. [DOI] [PubMed] [Google Scholar]
- 9.Varma N., Michalski J., Stambler B., Pavri B.B. Superiority of automatic remote monitoring compared with in-person evaluation for scheduled ICD follow-up in the TRUST trial—testing execution of the recommendations. Eur Heart J. 2014;35:1345–1352. doi: 10.1093/eurheartj/ehu066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ploux S., Varma N., Strik M., Lazarus A., Bordachar P. Optimizing implantable cardioverter-defibrillator remote monitoring: a practical guide. JACC Clin Electrophysiol. 2017;3:315–328. doi: 10.1016/j.jacep.2017.02.007. [DOI] [PubMed] [Google Scholar]