We read with interest the article of Arciola et al. (1) on the presence of icaA and icaD genes in Staphylococcus aureus and S. epidermidis isolates from catheter-associated infections and its correlation with a slime-positive phenotype detected with Congo red agar. These are the organisms most frequently the cause of foreign-body-related infections. The polysaccharide intercellular adhesin (PIA), synthesized by icaADBC-encoded proteins, is essentially involved in S. epidermidis biofilm accumulation (10). PIA has been shown to be a virulence factor of S. epidermidis (15). Recently, the icaADBC genes and PIA/poly-N-succinyl β-1-6-glucosamine (PNSG) were also detected in S. aureus (4, 13), together with evidence for a role of PIA/PNSG in S. aureus infections (13).
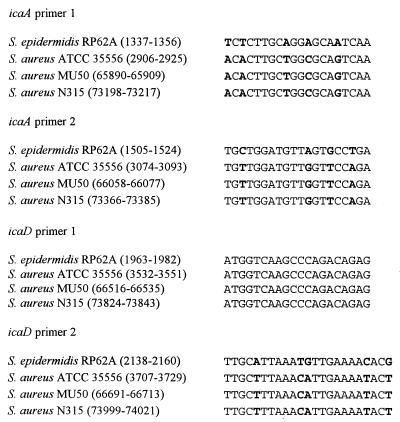
Using PCR, Arciola et al. (1) detected icaA and icaD in only 14 (61%) of 23 S. aureus isolates. These results are in contrast to data reported by others, who found all S. aureus isolates examined to be icaADBC positive (4, 7). Our own data on the prevalence of icaADBC in a collection of clinical S. aureus isolates confirm these latter observations, as all of 80 S. aureus isolates were icaADBC positive by PCR with oligonucleotides specific for icaA of S. aureus (M. A. Horstkotte, J. K.-M. Knobloch, H. Rohde, and D. Mack, unpublished data). A reasonable explanation for this discrepancy is that the primers used by Arciola et al. (1) were based on the icaADBC sequence of S. epidermidis RP62A (GenBank accession no. U43366), in which icaA and icaD display only 76 and 72% identity to the sequence of S. aureus ATCC 35556, respectively (4). Essentially, this leads to mismatches of 4 to 5 bases within three of the four primers used (Fig. 1).
FIG. 1.
Comparison of oligonucleotides specific for S. epidermidis as used by Arciola et al. (1) for icaA and icaD detection with homologous sequences of different S. aureus strains. The primers were derived from the icaADBC sequence data of S. epidermidis RP62A (GenBank accession no. U43366). The homologous sequences of the icaADBC locus of S. aureus ATCC 35556 (GenBank accession no. AF086783), S. aureus Mu50 (localized in section 9/9; DDBJ accession no. AP003366), and S. aureus N315 (localized in section 10/10; DDBJ accession no. AP003138) are aligned. Base mismatches are in boldface.
Arciola et al. (1) also described a close association between icaADBC detection and slime formation as detected with Congo red agar in 14 (61%) of 23 S. aureus strains. Congo red agar was used earlier to detect biofilm (slime) production of S. epidermidis (6, 8), which correlated well with a biofilm-positive phenotype observed in vitro (8, 16). However, in a standard biofilm assay with Trypticase soy broth (Becton Dickinson, Cockeysville, Md.) as the growth medium (2, 3, 11), most icaADBC-positive S. aureus isolates in our collection (78 of 80 isolates) were biofilm negative (Horstkotte et al., unpublished data), which is in accordance with previous reports (4, 7, 13). It does not seem reasonable to propose that Congo red agar be used as a means of screening clinical S. aureus isolates for a biofilm (slime)-positive phenotype and a icaADBC-positive genotype while the correlation of these properties is still uncertain. Moreover, studies that evaluate whether there exists a correlation between a black colony-forming phenotype on Congo red agar and a biofilm-positive phenotype of S. aureus are necessary. This should be explored using several different growth media, as expression of icaADBC depends significantly on environmental factors and regulatory mechanisms apparently differ between S. epidermidis and S. aureus (5, 9, 12, 14).
REFERENCES
- 1.Arciola C R, Baldassarri L, Montanaro L. Presence of icaA and icaDgenes and slime production in a collection of staphylococcal strains from catheter-associated infections. J Clin Microbiol. 2001;39:2151–2156. doi: 10.1128/JCM.39.6.2151-2156.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baldassarri L, Simpson W A, Donelli G, Christensen G D. Variable fixation of staphylococcal slime by different histochemical fixatives. Eur J Clin Microbiol Infect Dis. 1993;12:866–868. doi: 10.1007/BF02000411. [DOI] [PubMed] [Google Scholar]
- 3.Christensen G D, Simpson W A, Younger J J, Baddour L M, Barrett F F, Melton D M, Beachey E H. Adherence of coagulase-negative staphylococci to plastic tissue culture plates: a quantitative model for the adherence of staphylococci to medical devices. J Clin Microbiol. 1985;22:996–1006. doi: 10.1128/jcm.22.6.996-1006.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cramton S E, Gerke C, Schnell N F, Nichols W W, Götz F. The intercellular adhesion (ica) locus is present in Staphylococcus aureusand is required for biofilm formation. Infect Immun. 1999;67:5427–5433. doi: 10.1128/iai.67.10.5427-5433.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cramton S E, Ulrich M, Götz F, Döring G. Anaerobic conditions induce expression of polysaccharide intercellular adhesin in Staphylococcus aureus and Staphylococcus epidermidis. Infect Immun. 2001;69:4079–4085. doi: 10.1128/IAI.69.6.4079-4085.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deighton M A, Capstick J, Borland R. A study of phenotypic variation of Staphylococcus epidermidisusing Congo red agar. Epidemiol Infect. 1992;109:423–432. doi: 10.1017/s095026880005041x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fowler V G, Fey P D, Reller L B, Chamis A L, Corey G R, Rupp M E. The intercellular adhesin locus ica is present in clinical isolates of Staphylococcus aureusfrom bacteremic patients with infected and uninfected prosthetic joints. Med Microbiol Immunol. 2001;189:127–131. doi: 10.1007/s430-001-8018-5. [DOI] [PubMed] [Google Scholar]
- 8.Freeman D J, Falkiner F R, Keane C T. New method for detecting slime production by coagulase negative staphylococci. J Clin Pathol. 1989;42:872–874. doi: 10.1136/jcp.42.8.872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Knobloch J K M, Bartscht K, Sabottke A, Rohde H, Feucht H H, Mack D. Biofilm formation by Staphylococcus epidermidisdepends on functional RsbU, an activator of the sigB operon: differential activation mechanisms due to ethanol and salt stress. J Bacteriol. 2001;183:2624–2633. doi: 10.1128/JB.183.8.2624-2633.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mack D, Bartscht K, Dobinsky S, Horstkotte M A, Kiel K, Knobloch J K M, Schäfer P. Staphylococcal factors involved in adhesion and biofilm formation on biomaterials. In: An Y H, Friedman R J, editors. Handbook for studying bacterial adhesion: principles, methods, and applications. Totowa, N.J: Humana Press; 2000. pp. 307–330. [Google Scholar]
- 11.Mack D, Bartscht K, Fischer C, Rohde H, de Grahl C, Dobinsky S, Horstkotte M A, Kiel K, Knobloch J K M. Genetic and biochemical analysis of Staphylococcus epidermidisbiofilm accumulation. Methods Enzymol. 2001;336:215–239. doi: 10.1016/s0076-6879(01)36592-8. [DOI] [PubMed] [Google Scholar]
- 12.Mack D, Rohde H, Dobinsky S, Riedewald J, Nedelmann M, Knobloch J K M, Elsner H-A, Feucht H H. Identification of three essential regulatory gene loci governing expression of the Staphylococcus epidermidispolysaccharide intercellular adhesin and biofilm formation. Infect Immun. 2000;68:3799–3807. doi: 10.1128/iai.68.7.3799-3807.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McKenney D, Pouliot K L, Wang Y, Murthy V, Ulrich M, Doring G, Lee J C, Goldmann D A, Pier G B. Broadly protective vaccine for Staphylococcus aureusbased on an in vivo-expressed antigen. Science. 1999;284:1523–1527. doi: 10.1126/science.284.5419.1523. [DOI] [PubMed] [Google Scholar]
- 14.Rachid S, Ohlsen K, Wallner U, Hacker J, Hecker M, Ziebuhr W. Alternative transcription factor sigma(B) is involved in regulation of biofilm expression in a Staphylococcus aureusmucosal isolate. J Bacteriol. 2000;182:6824–6826. doi: 10.1128/jb.182.23.6824-6826.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rupp M E, Ulphani J S, Fey P D, Bartscht K, Mack D. Characterization of the importance of polysaccharide intercellular adhesin/hemagglutinin of Staphylococcus epidermidisin the pathogenesis of biomaterial-based infection in a mouse foreign body infection model. Infect Immun. 1999;67:2627–2632. doi: 10.1128/iai.67.5.2627-2632.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ziebuhr W, Heilmann C, Götz F, Meyer P, Wilms K, Straube E, Hacker J. Detection of the intercellular adhesion gene cluster (ica) and phase variation in Staphylococcus epidermidisblood culture strains and mucosal isolates. Infect Immun. 1997;65:890–896. doi: 10.1128/iai.65.3.890-896.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]