Abstract
Introduction
Although immunisation prevents the death of millions of infants and children each year, the vaccination coverage of routine childhood vaccination does not reach its target. The reasons for low vaccination uptake can be related to both demand and supply side determinants. The prevalence of vaccine hesitancy is increasing globally. However, data on vaccine hesitancy in low-income Arabic countries are scarce. To investigate this issue in Yemen, an Arabic low-income country, we aim to examine the link between vaccine hesitancy and the immunisation status of children living in Costal Hadhramout, Yemen, from the perspective of their parents and healthcare providers.
Methods and analysis
We will use a mixed-method research design. The study will be conducted in Costal Hadhramout in three phases. Phase 1 will involve a situational analysis using secondary data from records of the national expanded immunisation programme in Costal Hadhramout to examine the trend for previous years. Phase 2 will be a quantitative study aimed at assessing the prevalence of vaccination status of children aged <2 years and the determinants of parental vaccine hesitancy perception through a validated questionnaire. Lastly, phase 3 will be a qualitative study that explores vaccine hesitancy in Yemen using in-depth interviews and focus group discussions with parents and healthcare providers, respectively.
Ethics and dissemination
The study has been approved by the Research Committee of the Faculty of Medicine, University Kebangsaan Malaysia. The findings will be disseminated via publication in peer-reviewed academic journals, academic conferences and public presentations.
Keywords: public health, community child health, paediatric infectious disease & immunisation
Strengths and limitations of this study.
The strength of the present study protocol is its ability to determine all aspects of child, parental and healthcare factors of vaccine hesitancy among the Yemeni.
Using national data will aid generalisation of the findings to Yemen.
Using mixed methods has the advantage of improving the grey area of socioperspective, facilitators and barriers.
The validated questionnaire used will ensure better data quality.
The inability to meet face to face during the current COVID-19 pandemic poses a limitation. Video or voice calls alone may not fully depict the respondent’s expression and validity of the data captured.
Introduction
During the 20th century, there was a significant increase in life expectancy, attributed mainly to improvements in child survival. Universal child immunisation has been an effective preventive measure for protecting the vulnerable group. Immunisation has prevented millions of deaths related to vaccine-preventable diseases (VPDs) around the world.1 From 2007 to 2010, global third dose diphtheria, tetanus and pertussis (DTP3) coverage increased from 79% to 84% but has been plateauing since 2010. DTP3 coverage varies by region, being only 72% in the WHO African Region while it is 97% in the WHO Western Pacific Region.2
The reasons for low vaccination uptake are often not completely understood and appear to be multifactorial. Inadequate vaccination coverage can be related to both demand and supply side determinants. Most of the reasons for the low uptake of childhood vaccination in developing countries are related to lack of access to vaccination and family factors. Low education, literacy and socioeconomic status are well-known indirect contributors to coverage not being achieved. However, in several developing countries, the weakness of the health system is considered a significant barrier.3 4 Persistent challenges seen related to acceptance of the services that affect vaccine uptake, especially in developing countries.5 6
Vaccine hesitancy is a behavioural phenomenon among both those who accept all vaccines without hesitation and those refuse all vaccines.7 8 Vaccine hesitancy has been recognised as a growing problem of global importance that affects both developing and developed countries. The WHO has defined it as a delay in acceptance or refusal of vaccines despite the availability of vaccine services.9 Recently, vaccine hesitancy prevalence has emerged as a global problem and is evident in poor childhood vaccination coverage. The WHO has identified it as a priority issue and has developed a vaccine hesitancy model framework that emphasises confidence, complacency and convenience.9 The framework was expanded to included confidence, complacency, constraints, risk calculation and collective responsibility. These factors were identified as the psychological antecedents of vaccination.10 These models have been suggested based on research predominantly conducted in well-developed and high-income countries.11 Studies in neighbouring Arab countries have addressed parental vaccine hesitancy as a concerning problem that likely influences the uptake of childhood vaccination.12 13 However, to the best of our knowledge, no published study to date has addressed vaccine hesitancy in Yemen.
Yemen’s issues and challenges regarding child immunisation
Yemen is a low-income Arabic country with poor socioeconomic status and a fragile health system. It has a hard geographic environment, which affects access to essential basic services, and limited financial support for covering costs presents a major challenge.14 Since March 2015, Yemen had been engaged in civil war, which has continued to date. Civil war and internal conflict affect local development in Yemen.15 16 The instability, shortage of services and internal displacement may lead to limited vaccination coverage.17 The Expanded Program of Immunisation (EPI) in Yemen was initiated in 1979 as a part of the Primary Health Care General Directorate in Public Health and Population. It is aimed at preventing morbidity and mortality from VPDs. The target groups are infants, and women of childbearing age.18 Routine immunisation services in Yemen are provided through fixed vaccination posts within health facilities and outreach vaccination strategies and are based on the proximity of the target populations to the health facility. Table 1 shows the standard schedule of routine immunisation of children in Yemen.
Table 1.
Standard schedule of routine immunisation of children in the Republic of Yemen
| Vaccine | Age | |||||
| At birth | 6 weeks | 10 weeks | 14 weeks | 9 months | 18 months | |
| BCG | × | |||||
| OPV | × | × | × | × | × | × |
| Pentavalent (DPT, Hep B, Hib) | × | × | × | |||
| Pneumococcal | × | × | × | |||
| Rotavirus | × | × | ||||
| MR | × | × | ||||
| IPV | × | |||||
DPT, diphtheria, tetanus and pertussis; Hep B, hepatitis B; Hib, haemophilus influenzae type b; IPV, inactivated poliovirus vaccine; MR, measles and rubella; OPV, oral polio vaccine.
According to the last Yemen National Health and Demographic Survey, in 2013, only 42.6% of children aged 12–23 months were fully vaccinated, while 16% did not receive any vaccination. No reported published data are available for comparison on trend. However, vaccines for significant VPDs are publicly available for free.19 The WHO and the UNICEF reported that the 2018 vaccination coverage for Yemen was 65% based on DTP3, which remains below the 90% every country has achieved by 2020.20 From previous studies performed in Yemen, we may conclude that even before the war, vaccination coverage in Yemen had not been meeting an acceptable target, and the percentage of children who are completely unvaccinated has increased. In addition, various Governorates of Yemen have reported that children are unvaccinated or partially vaccinated mainly due to a lack of information and parental motivation.18 21–23
The rationale for this research
Although vaccine hesitancy has been addressed extensively in the literature in the past few years, few studies have explored this issue in low-income countries. Thus, most findings and models developed are based on studies performed in high-income countries.11 Limited studies have addressed the issue of childhood vaccination in Yemen, and most studies have focused on coverage and the reasons for non-vaccination.17 18 22 23 Only one study has addressed the determinants of complete vaccination,21 although it did not address the issue of vaccine hesitancy. Furthermore, all published studies addressing childhood vaccination in Yemen used a quantitative method, which cannot yield in-depth details on the problem when integrated with available qualitative study findings. In addition, all community-based studies performed in Yemen explored the problem from the parents’ perspective only and did not consider that of the healthcare workers, who can provide a bigger picture of the problem.
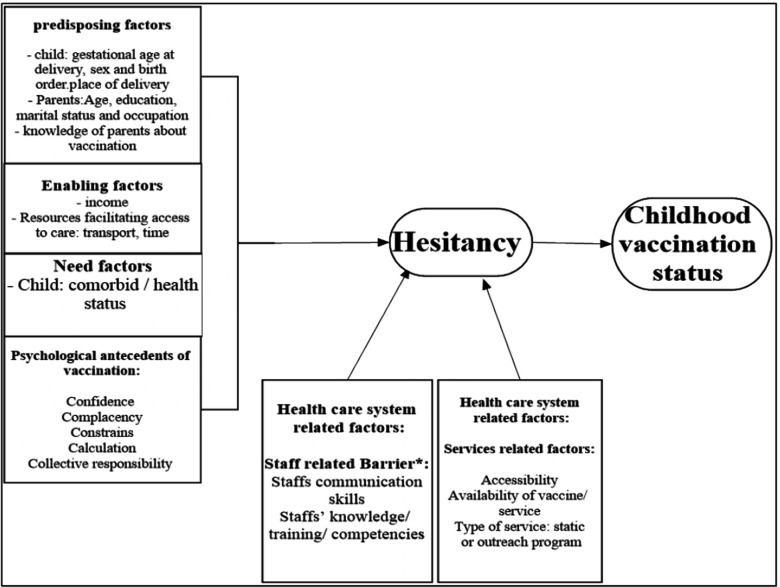
Studying the perspective of parents and healthcare workers on vaccine hesitancy regarding childhood vaccination is vital for improving service delivery and vaccine uptake. In addition, it aids the reduction of the high morbidity and mortality rate among children from VPDs, which are the leading cause of under-five mortality. Therefore, understanding their perceptions is crucial, as they play a vital role in vaccination programmes. Furthermore, exploring their perspectives would be informative for understanding the barriers they face. Accordingly, to bridge the knowledge gap in the literature on vaccine hesitancy and childhood vaccination in Yemen, the present study is a mixed-method study for assessing the determinants of vaccine hesitancy from the perspective of parents and healthcare workers. A conceptual framework (figure 1) illustrates the concept of the present study to bridge the evidence gap in the literature, which must be explored.
Figure 1.
Conceptual framework.
Aims and objectives
This research aims to address the issue of vaccine hesitancy and child immunisation status among children living in Costal Hadhramout, Hadhramout Governorate, Yemen, from the perspective of parents and healthcare providers. The specific research objectives are:
To conduct a situational analysis of routine childhood immunisation EPI data in Costal Hadhramout.
To measure the prevalence of vaccine hesitancy and child immunisation status among children and their mothers living in Costal Hadhramout.
To identify the associated factors and predict the vaccine hesitancy and immunisation status of children living in Costal Hadhramout.
To explore mothers’ reasons for hesitancy regarding childhood vaccination.
To explore the barriers healthcare providers face in achieving immunisation coverage in Costal Hadhramout.
Methods
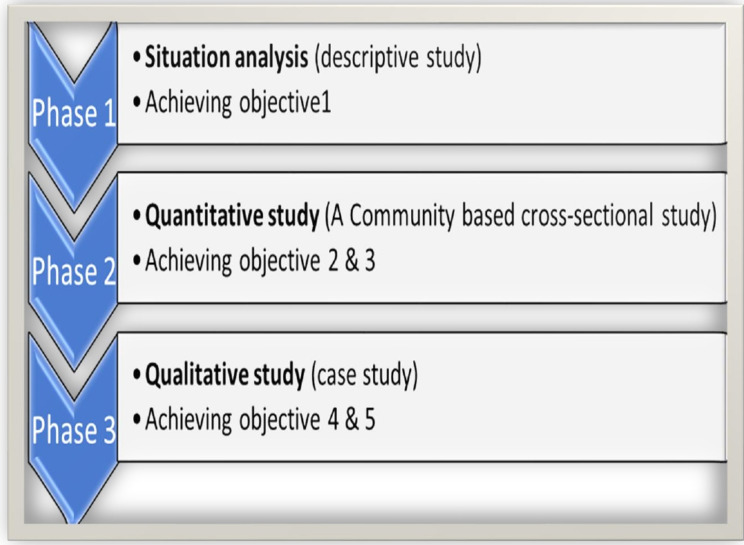
A complementary explanatory sequential mixed-method study design is used. The study will take place in Hadhramout in Yemen, consisting of 30 districts and occupying vast areas of the Arabian Sea coast. Hadhramout is divided administratively into two parts: the valley/desert (Wadi Hadhramout) and the coast (Coastal Hadhramout). Coastal Hadhramout overlooks south to the Arabian Sea and has a coastline of approximately 120 km. The estimated total population of Coastal Hadhramout in 2018 was 893 502 people. The population grows at a rate of 3.08% annually. This research targets the 12 districts of Coastal Hadhramout: Al-Mukalla, rural Al-Mukulla, Gail Bawazeer, Al-Shahr, Al-Dees, Ridh and Gosaiar, Ghail bin Yumin, Doan, Al-dulaia, Yeabeth, Hajer and Broome-Mayfa’a.24 This study will consist of three phases: (1) situation analysis, (2) quantitative study and (3) qualitative study. Figure 2 illustrates the overview of the study phases and their flow.
Figure 2.
An overview of the study phases.
Phase 1: situation analysis
Phase 1 is a retrospective descriptive study. The records from the national immunisation programme for the past 10 years (from January 2011 to December 2020) for the 12 Coastal Hadhramout districts will be reviewed and analysed (secondary data analysis). After permission has been obtained from the general manager of the Coastal Hadhramout Health and Population Affairs Office, data will be extracted from Coastal Hadhramout Health and Population Affairs Office Department of EPI data. First, we will assess the immunisation coverage rate (estimated for each vaccine, and for multidose vaccines, for each dose received (eg, diphtheria-tetanus-pertussis-containing vaccine (DTPCV1, DTPCV2, DTPCV3) in each year (trend analysis, the first outcome of this phase)). The districts will be classified into good or low coverage. The classification will be dependent on the Global Immunisation Vision and Strategy goal: at least 90% national vaccination coverage and at least 80% vaccination coverage in every district or equivalent administrative unit. Therefore, each district with ≥80% coverage will be classified as good coverage while any district with <80% coverage will be considered a low-coverage district. This classification is the second outcome of this phase and will be used for selecting districts in phase 2. Phase1 data collection and analysis began in August 2021 and ended in December 2021.
Phase 2: quantitative study
Phase 2 uses a community-based, cross-sectional study design. The study population is the mothers or caretakers of children aged <2 years in 2021 and living in Coastal Hadhramout. The study will use stratified cluster sampling, combining stratified and cluster sampling methods. First, the 12 Coastal Hadhramout districts will be stratified by immunisation coverage level, that is, good or low as per phase 1. Two districts will be selected randomly from each stratum. Second, a 30-household cluster (estimated by the researcher and may be more based on the absolute number of houses in each cluster) will be chosen from the selected districts proportionally to size. Then, all households in those clusters will be surveyed for an eligible child.
The researcher will prepare the sampling frame used in this study after consultation with the Coastal Hadhramout EPI director-general. Moreover, this sampling frame will be prepared based on the list of household distribution used in the last National Immunisation Days. The clusters in each district will be identified based on this list (every cluster contains approximately 20–30 households). Then, the researcher will select the number of clusters required to cover the sample size in this study from each district proportionally. In this study, an eligible mother or caretaker refers to a mother with a child aged <2 years. The youngest child will be taken for mothers with more than one child aged <2 years. We will exclude non-Yemeni families.
The sample size for this phase is calculated based on estimating proportion (prevalence) using the Kish formula25 and comparing two proportions using the Fleiss formula26 with a CI of 95% and study power of 0.80. The largest sample size derived using both formulae was 767, so this will be the sample size for this phase. The researcher and research assistants (health workers) will collect data from the households in the selected clusters. Four health workers will be trained to collect data from the mothers. During fieldwork, each health worker will work in a team. Each team will be supervised in the field by the researcher or fieldwork supervisor. Respondents will be interviewed using a structured, pretested designed questionnaire related to vaccine hesitancy perception (VHP) after being informed of the purpose of the study and after agreeing to participate in the study.
The VHP questionnaire will be adopted from varies validated questionnaire and adapted to the Yemeni population. The VHP questionnaire will cover the following domains: domain 1: child-related characteristics, for example, age, sex, birth order, place and type of delivery, gestational age at delivery and health status. Domain 2: family-related characteristics, for example, age, education, work, monthly income, residency and number of people living in the family. Domain 3: immunisation-related knowledge. Domain 4: vaccine hesitancy. Domain 5: psychological antecedents of vaccination (confidence, complacency, constraints, calculation, collective responsibility). Domain 6: vaccination status of the child (full, partial or unvaccinated) based on the child’s immunisation card and history of immunisation provided by the mother. Domain 7: availability and accessibility to vaccination service. Domain 8: reasons for the child’s incomplete vaccination or non-vaccination. Table 2 lists the operational definitions of the study variables.
Table 2.
List of independent variables and their definitions in this study
| Independent variable | Definition and analysis |
| I. Child-related variables | |
| Age | Age in months at data collection obtained from the child’s birth certificate, immunisation card or by asking the mother/caretaker. The mean and SD will be calculated. |
| Sex | Male or female. |
| Birth order | The child’s position among their siblings. Categorised as firstborn, 2–3, 4–5 and ≥6.29 |
| Place of delivery | At a health facility or at home.29 30 |
| Type of delivery | Vaginal or caesarean.21 |
| Gestational age at delivery | Full-term or premature. |
| Health status | Well or has a medical problem. |
| II. Family-related variables | |
| Mother’s age (years) | Age in years at data collection. The mean and SD will be calculated. |
| Age at first birth (years) | Mother’s age when she birthed her first child. The mean and SD will be calculated. |
| Mother’s marital status | Married or unmarried (divorced or widowed).21 |
| Mother’s education level | The highest formal education gained. Categorised as illiterate, able to read and write, essential education, secondary education or university and above.31 |
| Mother’s occupation | Employed or homemaker.32 |
| Father’s education level | The highest formal education gained. Categorised as illiterate, able to read and write, essential education, secondary education or university and above. |
| Father’s occupation | Government employee, daily labourer, merchant, unemployed or other. |
| Family size | The total number of persons living in the household.33 |
| Family residency | Permanent place of residence of the child’s family. Categorised as urban or rural.21 34 |
| Monthly family income | Average total income per month in Yemeni riyals (YR). The mean and SD will be calculated. |
| III. Mother/caretaker’s immunisation-related knowledge | |
| Source of information | The source from which the participant learns about vaccination and VPD. Categorised as 0=radio, 1=TV, 2=internet, 3=friends, 4=schools, 5=health personnel, 6=other. |
| Immunisation-related knowledge | The mother’s knowledge on VPDs, the best means of protection against VPDs, the causes of VPDs, number of vaccine doses, and the time of vaccine administration was assessed through five groups of questions containing 38 items. Each item was scored as I=correct, 0=wrong, or 0=don’t’ know the answer. The scale is adapted from a previous study performed in Yemen after permission has been obtained from the author.21 Analysis: the total knowledge score is calculated by summing the participant’s responses. The median of the summative calculation score will be used. We classify it as 0=poor knowledge (less than the median score) or 1=good knowledge (equal and more than the median score). |
| IV. Physiological antecedents of vaccination. These variables will be measured by using the 5C scale 10 | |
| Confidence | Assessed via three items from the 5C scale: (1) I am completely confident that vaccines are safe. (2) Vaccinations are effective. (3) Regarding vaccines, I am confident that public authorities decide in the best interest of the community. Each item is scored on a 7-point Likert scale (1=strongly disagree, 2=moderately disagree, 3=slightly disagree, 4=neutral (neither disagree nor agree), 5=slightly agree, 6=moderately agree, 7=strongly agree). Analysis: the mean score will be calculated by summing the participant’s responses for the three items and dividing it by 3.10 |
| Complacency | Assessed via three items from the 5C scale: (1) Vaccination is unnecessary because VPDs are not common anymore. (2) My immune system is strong, and it also protects me against diseases. (3) VPDs are not so severe that I should be vaccinated. Each item is scored on a 7-point Likert scale as described for the confidence variable. Analysis: the mean score will be calculated by summing the participant’s responses to the three items and dividing it by 3.10 |
| Constraints | Assessed via three items from the 5C scale: (1) Everyday stress prevents me from being vaccinated. (2) For me, it is inconvenient to be vaccinated. (3) Visiting the doctor makes me feel uncomfortable; this keeps me is being vaccinated. Each item is scored on a 7-point Likert scale as described for the confidence variable. Analysis: the mean score will be calculated by summing the participant’s responses to the three items and dividing it by 3.10 |
| Calculation | Assessed via three items from the 5C scale: (1) When I think about being vaccinated, I weigh its benefits and risks to make the best decision possible. (2) For every vaccination, I closely consider whether it is useful for me. (3) I need to understand the topic of vaccination before I get vaccinated fully. Each item is scored on a 7-point Likert scale same as described for the confidence variable. Analysis: the mean score will be calculated by summing the participant’s responses to the three items and dividing it by 3.10 |
| Collective responsibility | Assessed via three items from the 5C scale: (1) When everyone else is vaccinated, I do not have to be vaccinated too. (2) I get vaccinated because I can also protect people with a weaker immune system. (3) Vaccination is a collective action to prevent the spread of diseases. Each item is scored on a 7-point Likert scale as described for the confidence variable. Analysis: the mean score will be calculated by summing the participant’s responses to the three items and dividing it by 3.10 |
| V. Access to vaccination service | |
| Distance | The time taken to reach the nearest health facility. Categorised as 0≤30 min, 1≥30 min. |
| Means of accessing the health facility | Refers to how parents can arrive at the health facility, that is, either by walking or using transport. |
| Availability of vaccine or vaccinator | Refers to whether the vaccines and vaccinator are available at the health facility. |
| Waiting time | Refers to the parents waiting for a long time before their child can be vaccinated. |
VPD, vaccine-preventable diseases.
In this study, the primary dependent variable is the mother’s hesitancy level, which will be assessed using an Arabic version of the Parent Attitudes about Childhood Vaccines questionnaire (PACV) after granted permission from the author.12 27 The PACV questionnaire is divided into three domains: behaviour, safety and efficacy, and general attitude and trust. Fifteen items are grouped under these domains. The PACV uses a numeric score, where items answered with a hesitant response are scored 2 points, items answered with a response of do not know or not sure are scored 1 point and items answered with a non-hesitant response are scored 0 points. The raw score is then converted to a score of 0–100. Accordingly, parents are assigned 1 to indicate a hesitant score ≥50 or 0 as a non-hesitant parent with a score <50.
The second dependent variable in this study is the immunisation (vaccination) status of children aged 12–23 months. The immunisation status is classified as complete (full), incomplete or unimmunised. These classifications are defined according to the Yemini EPI schedule: complete (full) immunisation: A child aged 12–23 months who has received one BCG dose, at least three doses of pentavalent vaccine, at least three doses of pneumococcal vaccine, at least three doses of oral polio vaccine, two doses of rotavirus vaccine and one dose of MR (measles and rubella) vaccine. Incomplete immunisation: a child who has not received all routine EPI vaccines before their first birthday. Unimmunised (unvaccinated): a child who did not receive any of the 13 doses of the recommended vaccines.22
The independent variables in our study are the child and family characteristics: age, sex, birth order, place and type of delivery, gestational age at delivery and health status of the child; parents’ age, education, work, monthly income, residence and number of people living in the family. Immunisation-related knowledge: this variable will be assessed using a scale adapted from a previous study performed in Yemen.21 Psychological antecedents of vaccination: confidence, complacency, constraints, calculation and collective responsibility (5C scale). These variables will be measured using the 5C scale.10 To the best of our knowledge, there is no Arabic version of the 5C scale. Therefore, according to the sample study protocol, the translation and validation of the 5C scale proposed by Betsch et al28 will be used. Availability and accessibility of vaccination service will be assessed using four questions adapted from the literature.21 After permission has been obtained from the author, all mentioned scales will be adapted to suit the local population.
The validity and reliability of the VHP questionnaire will be assessed. The univariate analysis describes frequencies and percentages. The associations between dependent and independent variables will be assessed with bivariate analysis. A p value of <0.05 will determine the significant variables. The effect of different variables on hesitancy and children’s immunisation status will be assessed with multiple logistic regression. The results will be presented as tables and graphs. Data collection and analysis for this phase will begin in January 2022 and should end in May 2022.
Phase 3: qualitative study
The case study will be conducted in Coastal Hadhramout. The study population is the mothers/caretakers who participated in phase 2 and who were identified as hesitant mothers, and the healthcare providers and health leaders involved in the immunisation programme in Coastal Hadhramout. This phase will involve purposive sampling. Mothers/caretakers will be selected from among those who participated in phase 2 and showed good cooperation. Healthcare providers and leaders will be selected from the health facilities that provide immunisation in the selected cluster areas in phase 2.
Data will be collected through in-depth interviews with the mothers/caretakers and from healthcare providers and health leaders via focus group discussions (FGD) (table 3). The in-depth interviews and FGD will be performed until saturation is reached after triangulation. Then, thematic analysis will be performed to analyse the contents of in-depth interviews and FGD. Table 3 lists the key questions. Data collection and analysis for this phase will begin in June 2022 and should end in October 2022.
Table 3.
Critical questions for the qualitative phase
| A. The key question for the in-depth interview with the mothers | B. The critical question for the FGD with the healthcare providers and leaders |
Why do parents refuse or not complete vaccination for their children?
|
What are the barriers to achieving immunisation coverage?
|
FGD, focus group discussions.
Patient and public involvement
The participants, that is, the parents and healthcare providers, will be involved in the study design mainly in phase 2. In this phase, a research team will pilot and test the study tools, which would require contributions from the participants. Furthermore, in phase 3, participants will have the opportunity to present any additional comments during the interview and FGD. Therefore, their priorities, experiences and perception can be taken into consideration.
Ethics and dissemination
The study proposal has been reviewed and approved by the Research Ethics Committee of the Faculty of Medicine, University Kebangsaan Malaysia (project code: FF-2021-051). Permission for conducting the research has been obtained from the Costal Hadhramout health affairs office. The participants will receive a simple and clear explanation of the study’s aim and procedure. Consent will be obtained from all participants. Personal safety risks to the participants or researchers involved in this study are not expected. The participants’ privacy and confidentiality will be assured. The findings will be communicated through publication in peer-reviewed academic journals and disseminated to healthcare professionals, stakeholders, researchers and the public through academic conferences and public presentations.
Supplementary Material
Footnotes
Contributors: SAB: write the research protocol, conduct and report of the work described in the article. RS: provide idea in research protocol planning, review critically information reporting of the work described in the article. HI: review critically information reporting of the work described in the article. ASB-G: review critically information reporting of the work described in the article. SAB and RS: responsible for the overall content as guarantor(s).
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.World Health Organization . World Health Organization vaccination coverage cluster surveys: reference manual. Geneva: World Health Organization, 2018. [Google Scholar]
- 2.VanderEnde K, Gacic-Dobo M, Diallo MS, et al. Global Routine Vaccination Coverage - 2017. MMWR Morb Mortal Wkly Rep 2018;67:1261–4. 10.15585/mmwr.mm6745a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith LE, Amlôt R, Weinman J, et al. A systematic review of factors affecting vaccine uptake in young children. Vaccine 2017;35:6059–69. 10.1016/j.vaccine.2017.09.046 [DOI] [PubMed] [Google Scholar]
- 4.Larson HJ. The biggest pandemic risk? viral misinformation. Nature 2018;562:309–10. 10.1038/d41586-018-07034-4 [DOI] [PubMed] [Google Scholar]
- 5.Cooper S, Okeibunor JC, Wiyeh A, et al. Knowledge advances and gaps on the demand side of vaccination. Lancet Infect Dis 2019;19:13–15. 10.1016/S1473-3099(18)30733-3 [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization . Assessment report of the global vaccine action plan: strategic Advisory group of experts on immunization. Geneva: World Health Organization, 2017. [Google Scholar]
- 7.MacDonald NE, SAGE Working Group on Vaccine Hesitancy . Vaccine hesitancy: definition, scope and determinants. Vaccine 2015;33:4161–4. 10.1016/j.vaccine.2015.04.036 [DOI] [PubMed] [Google Scholar]
- 8.Domek GJ, O'Leary ST, Bull S, et al. Measuring vaccine hesitancy: field testing the who SAGE Working group on vaccine Hesitancy survey tool in Guatemala. Vaccine 2018;36:5273–81. 10.1016/j.vaccine.2018.07.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The SAGE Vaccine Hesitancy Working Group . Report of the SAGE working group on vaccine hesitancy. Geneva, Switzerland: World Health Organization, 2014. [Google Scholar]
- 10.Betsch C, Schmid P, Heinemeier D, et al. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One 2018;13:e0208601. 10.1371/journal.pone.0208601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cooper S, Betsch C, Sambala EZ, et al. Vaccine hesitancy – a potential threat to the achievements of vaccination programmes in Africa. Hum Vaccin Immunother 2018;14:2355–7. 10.1080/21645515.2018.1460987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alsuwaidi AR, Elbarazi I, Al-Hamad S, et al. Vaccine hesitancy and its determinants among Arab parents: a cross-sectional survey in the United Arab Emirates. Hum Vaccin Immunother 2020;16:3163–9. 10.1080/21645515.2020.1753439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alsubaie SS, Gosadi IM, Alsaadi BM, et al. Vaccine hesitancy among Saudi parents and its determinants. Saudi Med J 2019;40:1242–50. 10.15537/smj.2019.12.24653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.El Bcheraoui C, Jumaan AO, Collison ML, et al. Health in Yemen: losing ground in war time. Global Health 2018;14:42. 10.1186/s12992-018-0354-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boley J, Kent E, Grassie S. A conflict overlooked: Yemen in crisis, 2017. [Google Scholar]
- 16.OCHA-Yemen . 2019 humanitarian needs overview: Yemen: United nations office for the coordination of humanitarian Affairs, 2018. [Google Scholar]
- 17.Torbosh A, Al Amad MA, Al Serouri A, et al. The impact of war in Yemen on immunization coverage of children under one year of age: descriptive study. JMIR Public Health Surveill 2019;5:e14461. 10.2196/14461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ba'amer AA. Coverage of and barriers to routine child vaccination in Mukalla district, Hadramout governorate, Yemen. East Mediterr Health J 2010;16:223–7. 10.26719/2010.16.2.223 [DOI] [PubMed] [Google Scholar]
- 19.Ministry of Public Health Population, Central Statistical Organization . Yemen National health and demographic survey. Maryland, USA: MOPHP, CSO, PAPFAM, and ICF International Rockville, 20132015. [Google Scholar]
- 20.Peck M, Gacic-Dobo M, Diallo MS. Global routine vaccination coverage, 2018/Couverture de la vaccination systematique dans le monde, 2018. Weekly Epidemiological Record 2019;94:498–505. [Google Scholar]
- 21.Basaleem HO, Al-Sakkaf KA, Shamsuddin K. Immunization coverage and its determinants among children 12-23 months of age in Aden, Yemen. Saudi Med J 2010;31:1221–6. [PubMed] [Google Scholar]
- 22.Al-Tarbi AM, Bin Ghout AS. Vaccination coverage in Tarim district, Yemen 2017. Am J Epidemiol 2020;4:10–15. [Google Scholar]
- 23.Al-Rabeei NA, Dallak AM, Al-Fosail AA. Immunization coverage among children in Al-Taizyah district, Taiz governorate, Yemen. Indian J Community Health 2014;26:343–8. [Google Scholar]
- 24.Health Affairs Office Hadhramout Governorate . The statistical report for the year 2018 of the health office in Hadhramaut Governorate. 26. Yemen: Republic of Yemen Ministry of Health & Population : Health Affairs Office Hadhramout Governorat, 2018. [Google Scholar]
- 25.Kish L. Survey sampling. New York: John Wiley and Sons, 1965. [Google Scholar]
- 26.Fleiss JL. Statistical methods for rates and proportions. New York: John Wiley and Sons, 1981. [Google Scholar]
- 27.Opel DJ, Taylor JA, Mangione-Smith R, et al. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine 2011;29:6598–605. 10.1016/j.vaccine.2011.06.115 [DOI] [PubMed] [Google Scholar]
- 28.Betsch C, Bach Habersaat K, Deshevoi S, et al. Sample study protocol for adapting and translating the 5C scale to assess the psychological antecedents of vaccination. BMJ Open 2020;10:e034869. 10.1136/bmjopen-2019-034869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Efendi F, Pradiptasiwi DR, Krisnana I, et al. Factors associated with complete immunizations coverage among Indonesian children aged 12–23 months. Child Youth Serv Rev 2020;108:104651. 10.1016/j.childyouth.2019.104651 [DOI] [Google Scholar]
- 30.Mbengue MAS, Sarr M, Faye A, et al. Determinants of complete immunization among senegalese children aged 12–23 months: evidence from the demographic and health survey. BMC Public Health 2017;17:9. 10.1186/s12889-017-4493-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Asif AM, Akbar M, Tahir MR, et al. Role of maternal education and vaccination coverage: evidence from Pakistan demographic and health survey. Asia Pac J Public Health 2019;31:679–88. 10.1177/1010539519889765 [DOI] [PubMed] [Google Scholar]
- 32.Jama AA. Determinants of complete immunization coverage among children aged 11-24 months in Somalia. Int J Pediatr 2020;2020:1–7. 10.1155/2020/5827074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Herliana P, Douiri A. Determinants of immunisation coverage of children aged 12-59 months in Indonesia: a cross-sectional study. BMJ Open 2017;7:14. 10.1136/bmjopen-2016-015790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Geweniger A, Abbas KM. Childhood vaccination coverage and equity impact in Ethiopia by socioeconomic, geographic, maternal, and child characteristics. Vaccine 2020;38:3627–38. 10.1016/j.vaccine.2020.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.