Abstract
Objective
To evaluate sialic acid binding Ig-like lectin 1 (SIGLEC1) expression on monocytes by flow cytometry as a type I interferon biomarker in idiopathic inflammatory myopathies (IIM).
Methods
We performed a retrospective analysis of adult and paediatric patients with the diagnosis of IIM. SIGLEC1 expression was assessed by flow cytometry and was compared with Physician Global Assessment or Childhood Myositis Assessment Scale disease activity scores. Mann Whitney U test and receiver operating characteristic curves were used for cross-sectional data analysis (n=96), two-level mixed-effects linear regression model for longitudinal analyses (n=26, 110 visits). Response to treatment was analysed in 14 patients within 12 months, using Wilcoxon test. SIGLEC1 was compared with interferon-stimulated gene 15/MxA status by immunohistochemical staining of muscle biopsies (n=17).
Results
96 patients with adult (a) and juvenile (j) dermatomyositis (DM, n=38), antisynthetase syndrome (AS, n=19), immune-mediated necrotising myopathy (IMNM, n=8), inclusion body myositis (IBM, n=9) and overlap myositis (n=22) were included. SIGLEC1 distinguished significantly between active and inactive disease with an area under the curve of 0.92 (95% CI 0.83 to 1) in DM and correlated with disease activity longitudinally (aDM: standardised beta=0.54, p<0.001; jDM: standardised beta=−0.70, p<0.001). Response to treatment in DM was associated with a decreasing SIGLEC1 (p<0.01, Wilcoxon test). SIGLEC1 was found upregulated in 8 of 19 patients with AS, 2 of 9 patients with IBM but not in IMNM.
Conclusion
SIGLEC1 is a candidate biomarker to assess type I interferon activity in IIM and proved useful for monitoring disease activity and response to treatment in juvenile and adult DM.
Keywords: dermatomyositis, autoantibodies, autoimmunity, polymyositis
Key messages.
What is already known about this subject?
There is an unmet need for type I interferon biomarkers in rheumatic musculoskeletal diseases.
Sialic acid binding Ig-like lectin 1 (SIGLEC1) is part of the type I interferon signature and transcripts are upregulated in various autoimmune diseases (eg, SLE, dermatomyositis).
SIGLEC1 is expressed on the surface of monocytes and thus is easily assessable by flow cytometry.
What does this study add?
An activation of the type I interferon system in idiopathic inflammatory myopathies can be identified by flow cytometry analysing SIGLEC1 expression. SIGLEC1 correlated to disease activity and improvement under therapy in juvenile and adult dermatomyositis.
How might this impact on clinical practice or further developments?
SIGLEC1 expression is a suitable biomarker for monitoring type I interferon activation in rheumatic musculoskeletal diseases, which has clinical implications for patient stratification and treatment decision making especially in the context of interferon inhibitory therapies.
Introduction
Idiopathic inflammatory myopathies are a group of autoimmune diseases that can affect the muscles, skin, lungs, joints and other organs. The EULAR/American College of Rheumatology (ACR) classification of 2017 divides them into dermatomyositis, polymyositis and inclusion body myositis.1 However, increasing knowledge about subentities such as antisynthetase syndrome and immune-mediated necrotising myopathy, and the discovery of new myositis-specific autoantibodies, has led to even more differentiation. Furthermore, the existence of polymyositis has recently been challenged.2–4 Serum creatine kinase is used in clinical practice for diagnosis and monitoring of disease activity despite its shortcomings in subtypes of dermatomyositis.5 6
Studies have pointed out a crucial role of type I interferons in the etiopathogenesis of connective tissue diseases such as systemic lupus erythematosus and idiopathic inflammatory myopathies,7 8 and therefore, have become therapeutic targets of interest.9–12 An upregulation of type I interferon-inducible transcripts was found in peripheral blood, muscle and skin biopsy specimens, particularly in patients with adult and juvenile dermatomyositis, showing a correlation with disease activity in adult and juvenile dermatomyositis.7 13–20 However, type I interferon activation varies individually and is frequently not present. Thus, an easy assessable type I interferon biomarker for patient stratification and disease activity monitoring in routine clinical diagnostics is highly needed.21
Analysing the type I interferon signature in whole blood, SIGLEC1 (sialic acid binding Ig-like lectin 1, CD169), although monocyte restricted, was found to be a highly upregulated transcript in patients with adult and juvenile dermatomyositis, systemic lupus erythematosus and various genetic interferonopathies.13 22–25 However, the whole blood type I interferon signature is influenced by potentially disruptive factors (such as changes in immune blood cell distribution) that prevent optimal longitudinal comparative analysis.26 Moreover, PCR testing and interpretation can be challenging and time-consuming. Hence, a cell-specific approach to analysing type I interferon activity by measuring cell surface expression of SIGLEC1 on monocytes by flow cytometry could be advantageous.26 The utility of SIGLEC1 assessment by flow cytometry has been shown very recently in juvenile dermatomyositis,27 adult and juvenile systemic lupus erythematosus,25 28–31 systemic sclerosis,32 Sjögren’s syndrome,33 genetic interferonopathies34 and viral infections including COVID-19,35 but has not been analysed in adult dermatomyositis and other subtypes of idiopathic inflammatory myopathies.
The aim of this study was to analyse the usefulness of flow cytometric measurement of SIGLEC1 expression on monocytes as a biomarker for type I interferon activity in patients with idiopathic inflammatory myopathies, and to determine if SIGLEC1 expression in blood correlates with disease activity, specific autoantibody profiles, response to treatment and type I interferon activity in skeletal muscle biopsies.
Materials and methods
Study population
Adult and Paediatric Rheumatology of Charité - Universitätsmedizin Berlin’s hospital electronic patient record system was searched (MG and TR) for patients with a diagnosis of dermatomyositis, polymyositis, antisynthetase syndrome, inclusion body myositis, immune-mediated necrotising myopathy or overlap myositis and at least one flow cytometric measurement of SIGLEC1 expression on monocytes during the period between July 2015 and May 2020. Control groups consisted of patients with systemic lupus erythematosus and healthy individuals.
Laboratory measurement of SIGLEC1 and autoantibodies
Blood samples for the analysis of SIGLEC1 (CD169) expression on monocytes, creatine kinase and autoantibody profiles were obtained on an outpatient or inpatient basis as part of routine diagnostics at the Charité - Universitätsmedizin Berlin, and they were analysed at Labor Berlin - Charité Vivantes.
SIGLEC1 expression in whole blood was determined by flow cytometry using a highly standardised quantitative assay (online supplemental eText S1), as described by Stuckrad et al.28 The CD169/SIGLEC-1 assay is an accredited method according to EN ISO 15189. Standardisation procedure of this method is based on a protocol based on a flow cytomtric assay to quantify HLA-DR expression on monocytes.36 The lower limit of quantitation of this assay was 1200 monoclonal antibodies bound per cell (mAb/cell). The reference range for the expression of SIGLEC1 in healthy controls was determined to be less than 2400 mAb/cell.
rmdopen-2021-001934supp001.pdf (15.8MB, pdf)
Screening for IgG antinuclear antibodies (ANA) in human serum was performed as part of the routine diagnostics using the AESKUSLIDES ANA-HEp-2 indirect immunofluorescence assay from AESKU.GROUP (Wendelsheim, Germany). Qualitative determination of ANA (SS-A 52, SS-A 60, SS-B, RNP-70, Sm, RNP/Sm, Scl-70, centromere B and Jo1) in human serum was performed using the ANACombi ELISA from Orgentec (Mainz, Germany). Myositis-specific (anti-NXP2, anti-TIF1γ, anti-MDA5, anti-SRP, anti-Mi2, anti-OJ, anti-EJ, anti-PL7, anti-PL12, anti-Jo1 and anti-SAE) and myositis-associated autoantibodies (anti-Ku, anti-PM75, anti-PM100 and anti-Ro52) were determined in serum using the EUROLINE Autoimmune Inflammatory Myopathies 16 Ag line immunoassay (Euroimmun, Lübeck, Germany). Anti-HMGCR antibodies were determined using QUANTA Flash (Inova Diagnostics, San Diego, California, USA).
Assessment of disease activity
Juvenile patients with idiopathic inflammatory myopathies were routinely evaluated with the Childhood Myositis Assessment Scale (CMAS) by a trained physiotherapist at the time of their visit, as described by Rider et al.37 CMAS is a validated tool to measure muscle strength and endurance in juvenile idiopathic inflammatory myopathies.37 38 Physiotherapists were not informed about laboratory parameters, such as creatine kinase or SIGLEC1 expression. The Physician Global Assessment (PGA), with scores ranging from 0 (no disease activity) to 10 (high disease activity), was used to rate overall disease activity in juveniles and adults. If PGA data was missing in the medical records, it was determined retrospectively by two experienced rheumatologists (US and SLvS) based on all available information except for SIGLEC1 expression. Visit 1 was defined as the date of the patient’s first SIGLEC1 expression measurement at our clinic. We did not investigate an association of SIGLEC1 with clinical manifestations in dermatomyositis and antisynthetase syndrome since the heterogeneity of these diseases resulted in a low number of patients in each subgroup, which may result in false positive findings and invalid conclusions from statistical analysis.
Response to treatment analysis
To assess a clinically meaningful response to treatment in juvenile and adult patients with dermatomyositis we included all patients with (A) active disease (PGA ≥5) on the first visit (B) a follow-up visit in a time frame of 3 to 12 months and (C) reduction of PGA by at least 20% (as proposed by Rider et al39).
Assessment of type I interferon activity in muscle biopsies
Interferon-stimulated gene 15 (ISG15) and myxovirus resistance protein A (MxA) reflect the type I interferon activity40 and their protein expression can be assessed by immunohistochemical (IHC) analysis. Fixation of the muscle was done by standard cryofixation in methylbutane precooled in liquid nitrogen at a temperature of –120°C. The tissue was mounted on tissueTek on a cork plate and was moved in small circles for 60 s in the alcohol. Briefly, 7–8 µm cryosections of skeletal muscle biopsies were stained using MxA (Santa Cruz polyclonal, Mx1/2/3, H-285, sc-50509, 1:100) and ISG15 (Abcam, clone ab14374, 1:50) as the primary antibodies, and IHC analysis was performed using the iVIEW DAB (3,3'-diaminobenzidine) Benchm. Detection Kit 05266157001/760-091 (Ventana Medical Systems, Tucson, Arizona, USA), as previously described.41 42 The kit specifically detects mouse IgG, IgM and rabbit IgG antibodies bound to antigen and the specific antibody is located by a biotin-conjugated secondary antibody. Following this, a streptavidin enzyme (streptavidin-HRP) conjugates with the biotin-bound secondary antibody and visualisation is made possible via hydrogen peroxide substrate and DAB, producing a brown precipitate. Appropriate biotinylated secondary antibodies were used for signal amplification, and visualisation of the reaction product was carried out on a Benchmark XT immunostainer (Ventana) using a standardised procedure. As previously described, MxA and ISG15 staining in the cytoplasm was considered positive except for necrotic or regenerating fibres. Fibres with equivocally faint staining were considered negative.41 42 Appropriate positive and negative controls (tissue reactions) were used where necessary. Additionally, normal muscle or physiological control (eg, staining of arterioles by C5b-9, MHC class I positivity of capillaries) were used as negative control for all reactions. Negative control staining with an irrelevant antibody is presented in online supplemental eFigure S8. Biopsies were included in this study only if performed within 7 days of SIGLEC1 measurement in blood.
Statistical analysis
Quantitative data are presented as mean (range) or median (IQR), and qualitative data are presented as absolute numbers (percentage). The Mann-Whitney U test (MWU) was used to compare groups with non-normally distributed data. Spearman’s rank test was used to evaluate correlations between SIGLEC1 or creatine kinase and disease activity scores (PGA, CMAS). Receiver operating characteristic curves were plotted to compare the capability of SIGLEC1 and creatine kinase to distinguish between active (PGA ≥5) and inactive disease (PGA <5).
Longitudinal data analyses were performed using a two-level mixed-effects linear regression model. Standardised beta coefficients (betaST) were reported to compare the strength of association between the following parameters of interest: (1) CMAS score and SIGLEC1/creatine kinase, respectively, in juvenile dermatomyositis and (2) PGA score and SIGLEC1/creatine kinase, respectively, in adult dermatomyositis. Clinically meaningful response to treatment was analysed using Wilcoxon matched-pairs signed rank test. Linear mixed models analyses were performed with STATA V.12.1, and Graphpad Prism V.9.1.2 was used for all other data analyses and graphs. Values of p<0.05 were considered statistically significant.
Patient and public involvement
Patients and/or the public were not involved in the design, conduct, reporting or dissemination of this research.
Results
Study population
Seventy-four patients with confirmed diagnoses of idiopathic inflammatory myopathies were included (table 1) and 44 patients were excluded due to unclear diagnoses and/or insufficient clinical data. According to the EULAR/ACR criteria for idiopathic inflammatory myopathies,1 82.4%–100% of the patients with adult and juvenile dermatomyositis, antisynthetase syndrome and inclusion body myositis had a probable or definite diagnosis. This was the case for only 62.6% of the patients with immune-mediated necrotising myopathy, however, these diagnoses were conclusive according to clinical and morphological criteria, as discussed at the 224th ENMC International Workshop.43 The ‘overlap’ group consisted of 22 patients with overlap myositis (n=16), mixed connective tissue disease (n=5) and systemic sclerosis (n=1). No patient with isolated polymyositis as an independent entity could be identified in the time frame of 5 years.
Table 1.
Patient characteristics
| Patient characteristics | Adult DM (n=21) |
Juvenile DM (n=17) |
AS (n=19) |
IMNM (adult +juvenile) (n=8) |
IBM (n=9) |
Control 1: Overlap (adult +juvenile) (n=22) |
Control 2: SLE (n=30) |
Control 3: Healthy individuals (n=19) |
| Female, n (%) | 10 (47.6) | 9 (53) | 10 (52.6) | 3 (37.5) | 6 (66.6) | 20 (90.9) | 26 (86.67) | 10 (52.63) |
| Age at diagnosis, years, mean (range) | 52.3 (20–84) | 9 (2–16) | 53.3 (17–77) | 56.9 (6–86) | 67 (52–79) | 39.5 (10–77) | 41.7 (19–70) | ND (18–62) |
| Time since first diagnosis*, n (%) | ||||||||
| <3 months | 10 (47.6) | 7 (41.2) | 6 (31.6) | 4 (50) | 0 | 8 (36.4) | 14 (46.7) | NA |
| 3–12 months | 3 (14.3) | 2 (11.8) | 5 (26.3) | 2 (25) | 1 (11) | 3 (13.7) | 3 (10) | NA |
| >12 months | 8 (38) | 8 (47.1) | 8 (42.1) | 2 (25) | 8 (89) | 11 (50) | 13 (43.3) | NA |
| SIGLEC1 expression, mAb/cell, median (IQR)* | 5876 (1211–10282) | 5272 (1200–12691) | 1580 (1200–3390) | 1246 (1200–1853) | 1949 (1306–4602) | 1661 (1200–6915) | 7947 (3695–11924) | 1200 (1200–1200) |
| CK, U/l, median (IQR)* | 109 (74.5–442.5), NR=1 | 218.5 (116.3–1988), NR=1 | 627 (102.3–2173), NR=1 | 2118 (445.8–4353) | 497 (322.5–988.5), NR=1 | 421 (68–962.3), NR=4 | 62.5 (45.4–97.3) | ND |
| CRP, mg/L, median (IQR)* | 4.95 (0.7–24), NR=1 | 0.8 (0.3–3.3), NR=2 | 5.5 (1.9–29.1), NR=1 | 2.75 (0.68–11.3), NR=2 | 3.3 (1.3–33), NR=1 | 3.0 (0.9–7.4), NR=2 | 2.4 (0.7–17.3) | ND |
| Biopsy-confirmed IIM diagnosis/performed biopsies | 14/15 | 6/7 | 7/9 | 6/7 | 9/9 | 0/10 | NA | NA |
| ‘Definite’ or ‘probable’ IIM as per EULAR/ACR criteria, n (%) | 19 (90.5) | 13 (82.4) | 17 (89.5) | 5 (62.6) | 9 (100%) | NA | NA | NA |
| PGA, mean (range)* | 6 (2–10) | 4.4 (0–8) | 5.4 (2–9) | 4.9 (2–8) | 4.22 (3-6) | 4.5 (3–9), NR=7 | NA | NA |
| CMAS, mean (range)† | NA | 35 (2–52), NR=4 | NA | NA | NA | NA | NA | NA |
| SLEDAI-2k, mean (range)* | NA | NA | NA | NA | NA | NA | 6.6 (0–24) | NA |
| Prednisolone, no of patients (mean in mg/day on visit 1) | 12 (36.1 mg/day) | 9 (8.3 mg/day), NR=1 | 16 (13.3 mg/day) | 4 (13.1 mg/day) | 3 (7.5 mg/day) | 9 (6.9 mg/day), NR=1 | 17 (NR) | NA |
| Other medication*, n (%) | ||||||||
| Hydroxychloroquine/chloroquine | 1 (4.8) | 2 (11.8) | 3 (15.8) | – | – | 3 (13.7) | 10 (33.3) | NA |
| Intravenous immunoglobulin | 2 (9.5) | 2 (11.8) | 1 (5.3) | 1 (12.5) | 1 (11.1) | – | – | NA |
| Methotrexate | 1 (4.8) | 6 (35.3) | 3 (15.8) | 1 (12.5) | 1 (11.1) | 4 (18.2) | 1 (3.3) | NA |
| Rituximab | – | – | 2 (10.5) | – | 1 (11.1) | – | – | NA |
| JAK Inhibitor | 3 (14.3) | – | – | – | – | – | – | NA |
| MMF/CsA/Cyc/AZA | 5 (23.8) | 3 (17.6) | 5 (26.3) | 2 (25) | – | 3 (13.7) | 6 (20) | NA |
| No medication | 8 (38.1) | 7 (41.2) | 3 (15.8) | 4 (50) | 5 (55.6) | 10 (45.5) | 13 (43.3) | 19 (100) |
*On first visit with assessment of SIGLEC1.
†On first visit with assessment of SIGLEC1 and CMAS.
ACR, American College of Rheumatology; AS, antisynthetase syndrome; AZA, azathioprine; CK, creatine kinase; CMAS, Childhood Myositis Assessment Scale; CRP, C reactive protein; CsA, ciclosporin A; Cyc, cyclophosphamide; DM, dermatomyositis; IBM, inclusion body myositis; IIM, idiopathic inflammatory myopathies; IMNM, immune-mediated necrotising myopathy; JAK, Janus Kinase; Mab, monoclonal antibody; MCTD, mixed connective tissue disease; MMF, mycophenolate mofetil; n, absolute value; NA, not applicable; ND, not determined; NR, not reported; PGA, physician global assessment; SIGLEC1, sialic acid binding Ig-like lectin 1; SLE, systemic lupus erythematosus; SLEDAI-2k, Systemic Lupus Erythematosus Disease Activity Index 2000.
SIGLEC1 expression in inflammatory myopathies and control groups
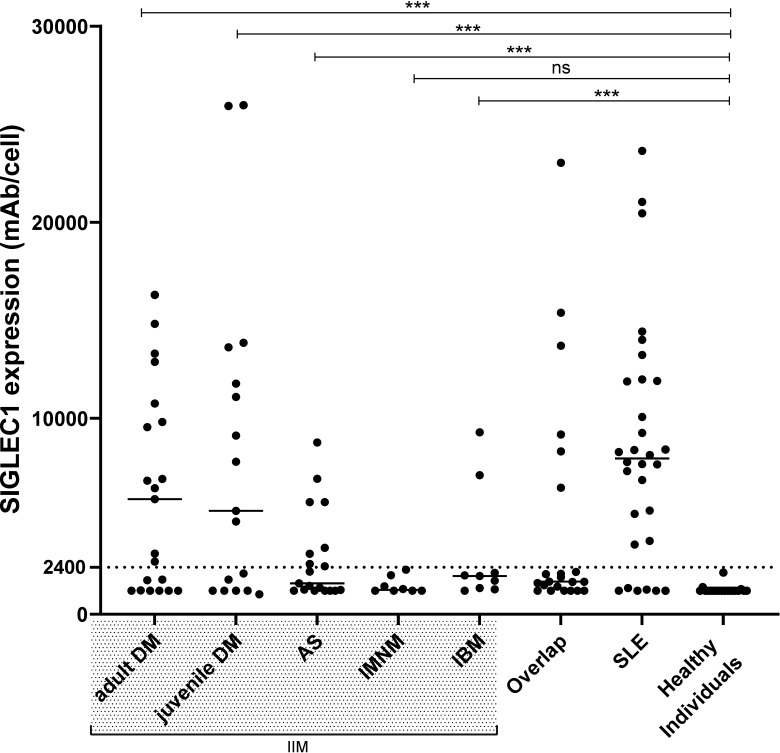
Adult and juvenile dermatomyositis patients expressed high levels of SIGLEC1 (median, 5876 and 5272 mAb/cell) (figure 1 and table 1). SIGLEC1 was upregulated in all newly diagnosed juvenile dermatomyositis patients (n=4, median, 13735 mAb/cell) and in 77.8% (n=7) of the newly diagnosed adult dermatomyositis patients (n=9, median, 9812 mAb/cell). There was no significant difference in SIGLEC1 expression between adult/juvenile dermatomyositis and systemic lupus erythematosus (systemic lupus erythematosus vs adult dermatomyositis: p=0.172; systemic lupus erythematosus vs juvenile dermatomyositis: p=0.485; MWU). Elevated SIGLEC1 expression was observed in two patients with inclusion body myositis (both anti-Ro52+, one anti-U1RNP+ and anti-Ku+). In the overlap group, six patients showed elevated SIGLEC1 levels: four with mixed connective tissue disease (anti-U1RNP+), one with anti-Ku antibodies, and one with overlap to juvenile systemic lupus erythematosus. In patients with systemic lupus erythematosus, SIGLEC1 correlated with the systemic lupus erythematosus disease activity index-2k (r=0.46, p=0.013, Spearman’s r).
Figure 1.
SIGLEC1 expression on monocytes of all patients at first visit. Horizontal bars show median values. Mann-Whitney U test was used to compare patients with the following idiopathic inflammatory myopathies (IIM)—adult (n=21) and juvenile (n=17) dermatomyositis (DM), antisynthetase syndrome (AS, n=18), immune-mediated necrotising myopathy (IMNM, n=8), inclusion body myositis (IBM, n=9)—with healthy individuals (n=19); ***p<0.001; ns, not significant; SIGLEC1, sialic acid binding Ig-like lectin 1; SLE, systemic lupus erythematosus.
SIGLEC1 expression and disease activity
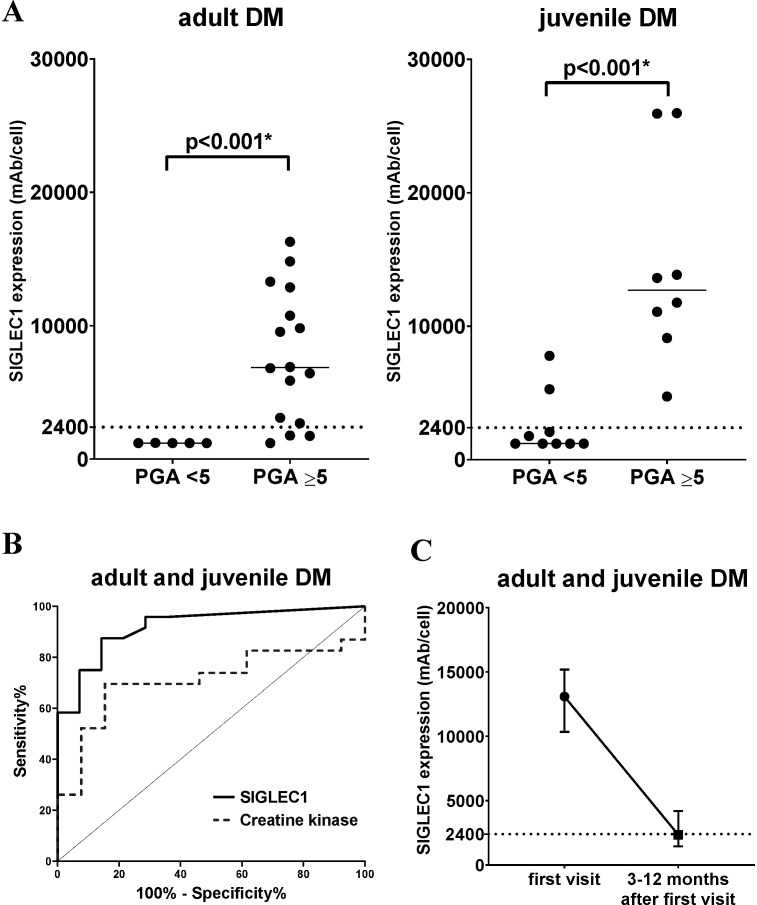
To determine if SIGLEC1 expression is associated with disease activity, each subgroup of idiopathic inflammatory myopathies was divided into two groups by PGA score: PGA<5 (no to moderate disease activity) and PGA≥5 (moderate to severe disease activity) (figures 2 and 3). There was a significant difference between the two groups in adult dermatomyositis (p<0.001, MWU) and juvenile dermatomyositis (p<0.001, MWU). SIGLEC1 levels generally correlated with PGA levels in adult and juvenile dermatomyositis (adult dermatomyositis: r=0.81, p<0.001 and juvenile dermatomyositis: r=0.80, p<0.001; Spearman’s r) (online supplemental eFigure S3). We also analysed the capability of SIGLEC1 and creatine kinase to distinguish between PGA <5 and PGA ≥5 and found a high area under the curve (AUC) for SIGLEC1 in dermatomyositis (AUC=0.92, p<0.001) and both dermatomyositis subgroups (juvenile dermatomyositis: AUC=0.97, p=0.001; adult dermatomyositis: AUC=0.96, p=0.002). The AUC was lower for creatine kinase (dermatomyositis: AUC=0.71; p=0.04; juvenile dermatomyositis: AUC=0.94, p=0.003; adult dermatomyositis: AUC=0.60, p=0.513) (figure 2 and online supplemental eFigure S1). To identify the best cut-off point for SIGLEC1 in dermatomyositis, we applied the Youden-index (J=sensitivity + specificity – 1) and found a lower threshold of 2383 mAb/monocyte (sensitivity 87,5%; specificity 85,71%), with a positive predictive value of 91.3%. In juvenile dermatomyositis, SIGLEC1 correlated with CMAS (r=−0.57, p=0.046; Spearman’s r) in cross-sectional analysis, while creatine kinase showed no significant correlation with CMAS (r=−0.40, p=0.180, Spearman’s r) (online supplemental eFigure S2).
Figure 2.
SIGLEC1 expression in DM patients (A) adult and juvenile DM subgroups (n=21/n=17) are separated by PGA score: PGA <5 (no to moderate disease activity) and PGA ≥5 (moderate to severe disease activity). Horizontal bars show median values; asterisks (*) represent significant results (p<0.05). The Mann-Whitney U test was used to compare groups. (B) Receiver operating characteristic curves for SIGLEC1 and creatine kinase in juvenile and adult DM (n=38). The curves show the ability of each biomarker to distinguish between patients with PGA ≥5 (moderate to severe disease activity) and PGA <5 (no to moderate disease activity): SIGLEC1: AUC=0.92, 95% CI 0.83 to 1; p<0.001; CK: AUC=0.71; 95% CI 0.54 to 0.89; p=0.04 (C) SIGLEC1 expression in adult and juvenile DM patients with a clinically meaningful improvement between the first visit and 3–12 months after the first visit (n=14, p<0.01, Wilcoxon test). The median and IQR for each time point is shown. AUC, area under the curve; DM, dermatomyositis; PGA, physician global assessment; SIGLEC1, sialic acid binding Ig-like lectin 1.
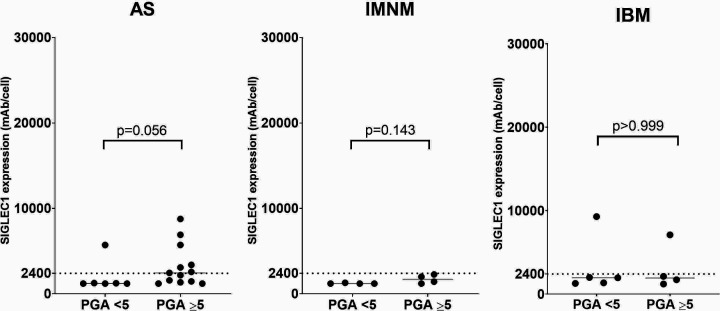
Figure 3.
SIGLEC1 expression versus disease activity in AS, IMNM and IBM subgroups, separated by PGA score: PGA <5 (no to moderate disease activity) and PGA ≥5 (moderate to severe disease activity). Horizontal bars show median values. The Mann-Whitney U test was used to compare groups. AS, antisynthetase syndrome; IBM, inclusion body myositis; IMNM, immune-mediated necrotising myopathy; PGA, Physician Global Assessment; SIGLEC1, sialic acid binding Ig-like lectin 1.
In the longitudinal analyses based on a total of 65 visits by 12 juvenile dermatomyositis patients (SIGLEC1 vs CMAS) and 45 visits by 14 adult dermatomyositis patients (SIGLEC1 vs PGA), SIGLEC1 correlated with disease activity in juvenile (SIGLEC1 vs CMAS: betaST=−0.70, p<0.001) and adult dermatomyositis (SIGLEC1 vs PGA: betaST=0.54, p<0.001) (table 2). The correlations between disease activity and SIGLEC1 were stronger than those between disease activity and creatine kinase in all analyses. The increase or decrease of SIGLEC1 between two consecutive visits was associated with changes in disease activity scores. Results for creatine kinase were not significant. Longitudinal graphs of biomarkers and disease activity are presented in online supplemental eFigure S4 and S5.
Table 2.
Results of longitudinal analyses comparing SIGLEC1 and CK with disease activity scores (CMAS/PGA) for (A) 12 juvenile and (B) 14 adult dermatomyositis patients
| A: Patients with juvenile dermatomyositis | ||
| Do SIGLEC1/CK correlate with CMAS over time? | ||
| CMAS—all values* | n=65 betaST=−0.70; p<0.001 95% CI −0.85 to −0.54 |
n=87 betaST=−0.39; p<0.001 95% CI −0.57 to −0.21 |
| CMAS—visits with complete data (SIGLEC1 and CK)† | n=53 betaST=−0.65; p<0.001 95% CI −0.80 to −0.49 |
n=53 betaST=−0.50; p<0.001 95% CI −0.66 to −0.33 |
| Is the change of SIGLEC1/CK associated with a change in CMAS? Change between visits (∆ Visitt-1 and visitt): | ||
| CMAS—all values* | n=28 betaST=−0.53; p<0.001 95% CI −0.77 to −0.29 |
n=41 betaST=−0.27; p=0.051 95% CI −0.62 to –0.08 |
| CMAS—visits with complete data (SIGLEC1 and CK)† | n=16 betaST=−0.42; p<0.001 95% CI −0.71 to −0.14 |
n=16 betaST=−0.14; p=0.566 95% CI −0.39 to 0.11 |
| B: Patients with adult dermatomyositis | ||
| Do SIGLEC1/CK correlate with PGA over time? | ||
| PGA—all values* | n=45 betaST=0.54; p<0.001 95% CI 0.34 to 0.74 |
n=41 betaST=0.17; p=0.149 95% CI −0.11 to 0.45 |
| PGA—visits with complete data (SIGLEC1 and CK)† | n=41 betaST=0.52; p<0.001 95% CI 0.32 to 0.72 |
n=41 betaST=0.17; p=0.149 95% CI −0.11 to 0.45 |
| Is the change of SIGLEC1/CK associated with a change in PGA? Change between visits (∆ visitt-1 and visitt): | ||
| PGA—all values* | n=31 betaST=0.48; p=0.003 95% CI 0.16 to 0.79 |
n=25 betaST=−0.10; p=0.634 95% CI −0.45 to 0.27 |
| PGA—visits with complete data (SIGLEC1 and CK)† | n=25 betaST=0.60; p=0.001 95% CI 0.29 to 0.91 |
n=25 betaST=−0.10; p=0.634 95% CI −0.45 to 0.27 |
Statistical analysis was performed using a two-level mixed-effects linear regression model.
*SIGLEC1 and CK values were analysed independently of each other.
†Included only those visits where both biomarkers (SIGLEC1 and CK) were assessed (complete-case analysis).
betaST, standardised beta coefficient; CK, creatine kinase; CMAS, Childhood Myositis Assessment Scale; n, number of analysed values; PGA, Physician Global Assessment; SIGLEC1, sialic acid binding Ig-like lectin 1.
Fourteen patients with dermatomyositis (adult, n=6 and juvenile, n=8) fulfilled the inclusion criteria for our response to treatment analysis. Between the two visits, there was a significant reduction of SIGLEC1 expression (median of differences −10059, IQR −6058 to −12152, p<0.01, Wilcoxon test) (figure 2). PGA scores between the respective visits improved by −76.5% (median of differences, IQR −63% to −91%). Medication for the treatment were as followed: Prednisolone (n=14), Methotrexate (n=9), Intravenous Immunoglobulin (n=9), Hydroxychloroquine (n=4), Azathioprine (n=3), Cyclophosphamide (n=2).
No significant correlation between SIGLEC1 and disease activity was detected in patients with antisynthetase syndrome, inclusion body myositis or immune-mediated necrotising myopathy (figure 3 and online supplemental eFigure S3).
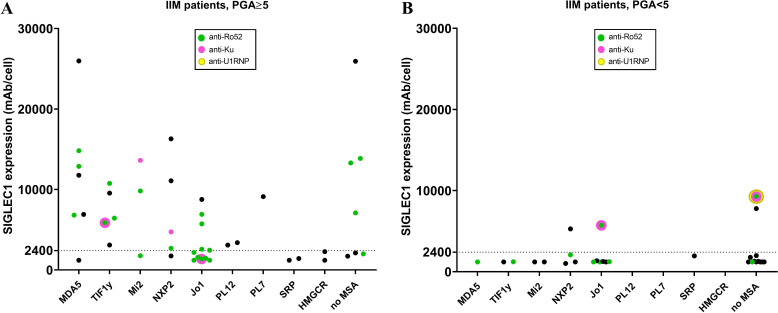
SIGLEC1 expression and myositis-specific autoantibodies
Subgroup analysis of juvenile and adult dermatomyositis patients with moderate to high disease activity (PGA ≥5) revealed elevated SIGLEC1 expression in 5/5 patients with TIF1γ-antibodies, 6/7 with MDA5-antibodies, 4/5 with NXP2-antibodies and 2/3 with Mi2-antibodies. Those with immune-mediated necrotising myopathy-associated antibodies (anti-SRP, anti-HMGCR) had consistently low SIGLEC1 expression (figure 4).
Figure 4.
SIGLEC1 expression and autoantibody status. SIGLEC1 expression of all IIM patients (n=74) at first visit. Each group represents patients with a positivity for the respective myositis-specific autoantibody (MSA) and (A) PGA ≥5 (moderate to severe disease activity) and (B) PGA <5 (no to moderate disease activity); if present, additional myositis associated antibodies (MAA) are marked by different colours and no MAA is resembled by black. IIM, idiopathic inflammatory myopathies; PGA, Physician Global Assessment; SIGLEC1, sialic acid binding Ig-like lectin 1.
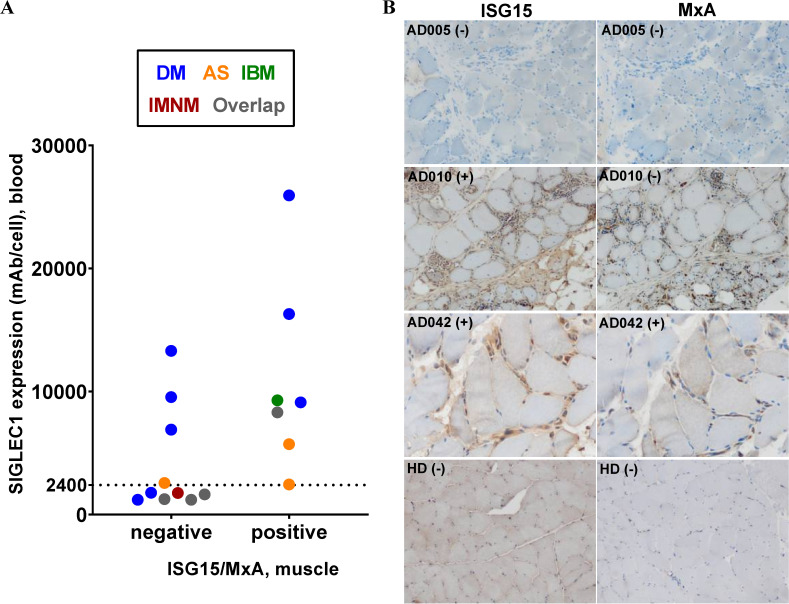
Comparison of SIGLEC1 expression on monocytes with ISG15/MxA status in muscle tissue
Of the 17 muscle samples eligible for IHC staining (inclusion criteria: 7 days or less between SIGLEC1 measurement and muscle biopsy), 7 (41.2%) were positive for ISG15 and/or MxA. The average time between SIGLEC1-measurement and muscle biopsy was 3 days (range: 0–7 days). All muscle biopsy patients that were positive for ISG15/MxA (in staining) had elevated SIGLEC1 expression on monocytes in peripheral blood (figure 5), but one patient with antisynthetase syndrome had only minimal elevation (2449 mAb/cell). Three patients with upregulation of SIGLEC1 expression had a negative ISG15/MxA status and were diagnosed with dermatomyositis: one had anti-TIF1γ antibodies, one did not have any myositis-specific autoantibodies, and one had anti-MDA5+ amyopathic dermatomyositis. One patient with inclusion body myositis who was positive for SIGLEC1 expression on monocytes and in IHC staining in muscle biopsy was also positive for anti-Ku, anti-U1RNP and anti-Ro52 antibodies (online supplemental eTable S1).
Figure 5.
Immunohistochemical staining of type I interferon-inducible proteins (ISG15/MxA) in muscle tissue (A) comparison of SIGLEC1 expression in blood with negative or positive ISG15 and/or MxA status in immunohistochemical muscle biopsy staining (n=17). Colours represent patients with the specified subgroups of IIM and overlap (see legend box). (B) ISG15 and MxA status of three patients and one healthy donor (HD) are shown. Patient AD005 (adult DM, SIGLEC1 in blood 13301 mAb/cell) had negative (−) stains. Patient AD010 (adult IBM, SIGLEC1 in blood 9281 mAb/cell) stained clearly positive (+) for MxA on capillaries and macrophages; regarding the ISG15 status, some macrophages were positive, but myofibers were not. Patient AD042 (adult DM, SIGLEC1 in blood 16295 mAb/cell) was ISG15-positive (more densely stained on sarcolemma than on sarcoplasm) and MxA-positive. AS, antisynthetase syndrome; DM, dermatomyositis; IBM, inclusion body myositis; IMNM, immune-mediated necrotising myopathy; IIM, idiopathic inflammatory myopathies; SIGLEC1, sialic acid binding Ig-like lectin 1.
Discussion
We found that SIGLEC1 expression on monocytes correlated with disease activity in patients with juvenile and adult dermatomyositis. Clinically meaningful improvement under therapy was associated with a significant decrease in SIGLEC1 expression. These results are in line with studies that analysed type I interferon transcripts,13–19 but with the advantage of being easily assessable by flow cytometry. Very recently, Lerkvaleekul et al27 published data of SIGLEC1 in 21 patients with newly diagnosed juvenile dermatomyositis. They found, that SIGLEC1 expression correlated to disease activity and was superior to predict treatment response compared with an ISG score consisting of five genes. Our results validate the findings in juvenile dermatomyositis and by that underline the potential of SIGLEC1 in clinical routine diagnostics.
In our study, SIGLEC1 could distinguish between active and inactive disease in adult and juvenile dermatomyositis patients with a large AUC. In this context, published results in a comment suggest the utility of direct assessment of interferon by using a highly sensitive interferon-alpha single-molecule array (SIMOA) digital ELISA in juvenile dermatomyositis.44 SIMOA technology is of special interest, since direct measurement of interferon alpha using ELISA has been shown to have a low sensitivity in systemic lupus erythematosus.29 A direct comparison of these two type I interferon biomarkers would be highly interesting, as they are both candidates for routine clinical diagnostics.
In this study, expression of SIGLEC1—which is mostly type I interferon regulated34 45—was lower in antisynthetase syndrome than in dermatomyositis. It has been proposed that type II interferons might play a more prominent role in the etiopathogenesis of antisynthetase syndrome.40 46 However, Reed et al found high interferon scores (including IP-10, I-TAC and MCP-1) in patients with antisynthetase syndrome.47 We also identified patients with high expression of SIGLEC1 indicating a type I interferon response. This interesting finding warrants further investigation.
Two of our nine patients with inclusion body myositis exhibited high expression of SIGLEC1: both were positive for anti-Ro and one was also positive for anti-U1RNP autoantibodies, which are known to induce type I interferons.48 Sjoegren’s syndrome could be excluded. One of these anti-U1RNP+ inclusion body myositis patients was also analysed for MxA/ISG15 in muscle tissue and showed an unusual positive staining on myofibers (cf. patient AD010). Data on the role of interferons in inclusion body myositis are inconsistent and need to be clarified.40 49 50 The detection of an activated type I interferon system might have important treatment implications in this debilitating chronic disease.
We did not find evidence of an upregulation of SIGLEC1 expression in immune-mediated necrotising myopathy, which is in line with other current studies analysing type I interferon-regulated transcripts (in muscle).40
Few studies have explored differences in interferon signatures in blood according to myositis-specific autoantibody status.47 We found the highest SIGLEC1 expression in anti-MDA5+ dermatomyositis patients, but could not detect a specific association of SIGLEC1 to certain myositis-specific autoantibodies in dermatomyositis otherwise. Our findings underline, that the autoantibody status alone is not predictive for the detection of a type I interferon activation. Thus, the assessment of myositis-specific autoantibodies in conjunction with the assessment of type I interferon activity might be useful for patient stratification.
The current study has strengths and limitations. A strength is that we could demonstrate that SIGLEC1, as an implemented routine biomarker, was able to validate findings from other studies investigating type I interferon signature with the advantage of being easily assessable by flow cytometry. A limitation is that muscle strength scores equivalent to the CMAS were not available for adult patients. Second, the PGA was performed retrospectively in most cases, which has to be considered when interpreting the data. Since the missing scores were determined by two experienced rheumatologists with access to all clinical data for each visit but blinded to SIGLEC1 expression, we hope that we could reduce a potential bias. Third, although we could show that a clinical meaningful response to therapy was associated with a decrease in SIGLEC1 expression, the clinical benefit of measuring type I interferon biomarkers still needs to be proven by subsequent prospective studies. Another limitation of the study was the low number of patients in the subanalysis of autoantibodies. This problem can only be solved by multicentre collaborations.
In conclusion, analysis of SIGLEC1 expression by flow cytometry enables the individual assessment of type I interferon activity in idiopathic inflammatory myopathies. Present and published data on SIGLEC1 expression in patients with interferon-associated rheumatic and musculoskeletal diseases, interferonopathies and viral infections confirm that SIGLEC1 is an easy-to-use type I interferon biomarker and demonstrate its potential for patient stratification, disease activity monitoring and assessment of treatment response in routine clinical practice.
Footnotes
Twitter: @kruschemartin
Contributors: Conceptualisation and manuscript preparation: MG and TR. Coordination of the study: TR. Acquisition of data: US, TR, SLvS, TK, RB, TB, MK and MG. Data of patients with systemic lupus erythematosus: RB and LZ-P. Data of healthy individuals: NU and CM. Data of immunohistochemical staining: AU and WS. Statistical analysis: JK, MG and TR. Preparation of figures and tables: MG and TR. Interpretation of the data: TR, US, MG, GRB, FH, AU, WS and TK. All authors commented on the manuscript draft and approved the final version of the manuscript. TR is responsible for the overall content as guarantor.
Funding: This research was funded by the German Research Foundation (DFG, Transregio TRR130, Project 15).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Prior approval for this study was obtained from the local ethics committee of the Charité - Universitätsmedizin Berlin (application number: EA2/094/19). Informed consent was not necessary for this retrospective study.
References
- 1.Lundberg IE, Tjärnlund A, Bottai M, et al. 2017 European League against Rheumatism/American College of rheumatology classification criteria for adult and juvenile idiopathic inflammatory myopathies and their major subgroups. Ann Rheum Dis 2017;76:1955–64. 10.1136/annrheumdis-2017-211468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allenbach Y, Benveniste O, Goebel H-H, et al. Integrated classification of inflammatory myopathies. Neuropathol Appl Neurobiol 2017;43:62–81. 10.1111/nan.12380 [DOI] [PubMed] [Google Scholar]
- 3.Mariampillai K, Granger B, Amelin D, et al. Development of a new classification system for idiopathic inflammatory myopathies based on clinical manifestations and myositis-specific autoantibodies. JAMA Neurol 2018;75:1528–37. 10.1001/jamaneurol.2018.2598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tanboon J, Uruha A, Stenzel W, et al. Where are we moving in the classification of idiopathic inflammatory myopathies? Curr Opin Neurol 2020;33:590–603. 10.1097/WCO.0000000000000855 [DOI] [PubMed] [Google Scholar]
- 5.Mathur T, Manadan AM, Thiagarajan S, et al. The utility of serum aldolase in normal creatine kinase dermatomyositis. J Clin Rheumatol 2014;20:47–8. 10.1097/RHU.0000000000000062 [DOI] [PubMed] [Google Scholar]
- 6.Allenbach Y, Uzunhan Y, Toquet S, et al. Different phenotypes in dermatomyositis associated with anti-MDA5 antibody: study of 121 cases. Neurology 2020;95:e70–8. 10.1212/WNL.0000000000009727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gallay L, Mouchiroud G, Chazaud B. Interferon-signature in idiopathic inflammatory myopathies. Curr Opin Rheumatol 2019;31:634–42. 10.1097/BOR.0000000000000653 [DOI] [PubMed] [Google Scholar]
- 8.Rose T, Dörner T. Drivers of the immunopathogenesis in systemic lupus erythematosus. Best Pract Res Clin Rheumatol 2017;31:321–33. 10.1016/j.berh.2017.09.007 [DOI] [PubMed] [Google Scholar]
- 9.Ladislau L, Suárez-Calvet X, Toquet S, et al. Jak inhibitor improves type I interferon induced damage: proof of concept in dermatomyositis. Brain 2018;141:1609–21. 10.1093/brain/awy105 [DOI] [PubMed] [Google Scholar]
- 10.Morand EF, Furie R, Tanaka Y, et al. Trial of Anifrolumab in active systemic lupus erythematosus. N Engl J Med 2020;382:211–21. 10.1056/NEJMoa1912196 [DOI] [PubMed] [Google Scholar]
- 11.Paik JJ, Casciola‐Rosen L, Shin JY, et al. Study of tofacitinib in refractory dermatomyositis: an Open‐Label pilot study of ten patients. Arthritis Rheumatol 2021;73:858–65. 10.1002/art.41602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kurasawa K, Arai S, Namiki Y, et al. Tofacitinib for refractory interstitial lung diseases in anti-melanoma differentiation-associated 5 gene antibody-positive dermatomyositis. Rheumatology 2018;57:2114–9. 10.1093/rheumatology/key188 [DOI] [PubMed] [Google Scholar]
- 13.Huard C, Gullà SV, Bennett DV, et al. Correlation of cutaneous disease activity with type 1 interferon gene signature and interferon β in dermatomyositis. Br J Dermatol 2017;176:1224–30. 10.1111/bjd.15006 [DOI] [PubMed] [Google Scholar]
- 14.Bilgic H, Ytterberg SR, Amin S, et al. Interleukin-6 and type I interferon-regulated genes and chemokines mark disease activity in dermatomyositis. Arthritis Rheum 2009;60:3436–46. 10.1002/art.24936 [DOI] [PubMed] [Google Scholar]
- 15.Greenberg SA, Higgs BW, Morehouse C, et al. Relationship between disease activity and type 1 interferon- and other cytokine-inducible gene expression in blood in dermatomyositis and polymyositis. Genes Immun 2012;13:207–13. 10.1038/gene.2011.61 [DOI] [PubMed] [Google Scholar]
- 16.Baechler EC, Bauer JW, Slattery CA, et al. An interferon signature in the peripheral blood of dermatomyositis patients is associated with disease activity. Mol Med 2007;13:59–68. 10.2119/2006-00085.Baechler [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O'Connor KA, Abbott KA, Sabin B, et al. Mxa gene expression in juvenile dermatomyositis peripheral blood mononuclear cells: association with muscle involvement. Clin Immunol 2006;120:319–25. 10.1016/j.clim.2006.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walsh RJ, Kong SW, Yao Y, et al. Type I interferon-inducible gene expression in blood is present and reflects disease activity in dermatomyositis and polymyositis. Arthritis Rheum 2007;56:3784–92. 10.1002/art.22928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reed AM, Peterson E, Bilgic H, et al. Changes in novel biomarkers of disease activity in juvenile and adult dermatomyositis are sensitive biomarkers of disease course. Arthritis Rheum 2012;64:4078–86. 10.1002/art.34659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greenberg SA. Dermatomyositis and type 1 interferons. Curr Rheumatol Rep 2010;12:198–203. 10.1007/s11926-010-0101-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Benveniste O, Goebel H-H, Stenzel W. Biomarkers in inflammatory Myopathies-An expanded definition. Front Neurol 2019;10:554. 10.3389/fneur.2019.00554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rice GI, Melki I, Frémond M-L, et al. Assessment of type I interferon signaling in pediatric inflammatory disease. J Clin Immunol 2017;37:123–32. 10.1007/s10875-016-0359-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rice GI, Forte GMA, Szynkiewicz M, et al. Assessment of interferon-related biomarkers in Aicardi-Goutières syndrome associated with mutations in TREX1, RNASEH2A, RNASEH2B, RNASEH2C, SAMHD1, and ADAR: a case-control study. Lancet Neurol 2013;12:1159–69. 10.1016/S1474-4422(13)70258-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yao Y, Higgs BW, Morehouse C, et al. Development of potential pharmacodynamic and diagnostic markers for Anti-IFN-α monoclonal antibody trials in systemic lupus erythematosus. Hum Genomics Proteomics 2009;2009. 10.4061/2009/374312. [Epub ahead of print: 17 Nov 2009]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Biesen R, Demir C, Barkhudarova F, et al. Sialic acid-binding Ig-like lectin 1 expression in inflammatory and resident monocytes is a potential biomarker for monitoring disease activity and success of therapy in systemic lupus erythematosus. Arthritis Rheum 2008;58:1136–45. 10.1002/art.23404 [DOI] [PubMed] [Google Scholar]
- 26.Strauß R, Rose T, Flint SM, et al. Type I interferon as a biomarker in autoimmunity and viral infection: a leukocyte subset-specific analysis unveils hidden diagnostic options. J Mol Med 2017;95:753–65. 10.1007/s00109-017-1515-7 [DOI] [PubMed] [Google Scholar]
- 27.Lerkvaleekul B, Veldkamp SR, van der Wal MM, et al. Siglec-1 expression on monocytes is associated with the interferon signature in juvenile dermatomyositis and can predict treatment response. Rheumatology 2021:keab601. 10.1093/rheumatology/keab601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stuckrad SLvon, Klotsche J, Biesen R, et al. SIGLEC1 (CD169) is a sensitive biomarker for the deterioration of the clinical course in childhood systemic lupus erythematosus. Lupus 2020;29:1914–25. 10.1177/0961203320965699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rose T, Grützkau A, Hirseland H, et al. Ifnα and its response proteins, IP-10 and SIGLEC-1, are biomarkers of disease activity in systemic lupus erythematosus. Ann Rheum Dis 2013;72:1639–45. 10.1136/annrheumdis-2012-201586 [DOI] [PubMed] [Google Scholar]
- 30.Aue A, Szelinski F, Weißenberg SY, et al. Elevated STAT1 expression but not phosphorylation in lupus B cells correlates with disease activity and increased plasmablast susceptibility. Rheumatology 2020;59:3435–42. 10.1093/rheumatology/keaa187 [DOI] [PubMed] [Google Scholar]
- 31.Rose T, Grützkau A, Klotsche J, et al. Are interferon-related biomarkers advantageous for monitoring disease activity in systemic lupus erythematosus? A longitudinal benchmark study. Rheumatology 2017;56:1618–26. 10.1093/rheumatology/kex220 [DOI] [PubMed] [Google Scholar]
- 32.York MR, Nagai T, Mangini AJ, et al. A macrophage marker, Siglec-1, is increased on circulating monocytes in patients with systemic sclerosis and induced by type I interferons and Toll-like receptor agonists. Arthritis Rheum 2007;56:1010–20. 10.1002/art.22382 [DOI] [PubMed] [Google Scholar]
- 33.Rose T, Szelinski F, Lisney A, et al. SIGLEC1 is a biomarker of disease activity and indicates extraglandular manifestation in primary Sjögren's syndrome. RMD Open 2016;2:e000292. 10.1136/rmdopen-2016-000292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Orak B, Ngoumou G, Ebstein F, et al. SIGLEC1 (CD169) as a potential diagnostical screening marker for monogenic interferonopathies. Pediatr Allergy Immunol 2021;32:621–5. 10.1111/pai.13400 [DOI] [PubMed] [Google Scholar]
- 35.Doehn J-M, Tabeling C, Biesen R, et al. CD169/SIGLEC1 is expressed on circulating monocytes in COVID-19 and expression levels are associated with disease severity. Infection 2021;49:757–62. 10.1007/s15010-021-01606-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Döcke W-D, Höflich C, Davis KA, et al. Monitoring temporary immunodepression by flow cytometric measurement of monocytic HLA-DR expression: a multicenter standardized study. Clin Chem 2005;51:2341–7. 10.1373/clinchem.2005.052639 [DOI] [PubMed] [Google Scholar]
- 37.Rider LG, Werth VP, Huber AM, et al. Measures of adult and juvenile dermatomyositis, polymyositis, and inclusion body myositis: Physician and Patient/Parent Global Activity, Manual Muscle Testing (MMT), Health Assessment Questionnaire (HAQ)/Childhood Health Assessment Questionnaire (C-HAQ). Arthritis Care Res 2011;63:S118–57. 10.1002/acr.20532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huber AM, Feldman BM, Rennebohm RM, et al. Validation and clinical significance of the childhood myositis assessment scale for assessment of muscle function in the juvenile idiopathic inflammatory myopathies. Arthritis Rheum 2004;50:1595–603. 10.1002/art.20179 [DOI] [PubMed] [Google Scholar]
- 39.Rider LG, Giannini EH, Harris-Love M, et al. Defining clinical improvement in adult and juvenile myositis. J Rheumatol 2003;30:603–17. [PubMed] [Google Scholar]
- 40.Pinal-Fernandez I, Casal-Dominguez M, Derfoul A, et al. Identification of distinctive interferon gene signatures in different types of myositis. Neurology 2019;93:e1193–204. 10.1212/WNL.0000000000008128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Uruha A, Allenbach Y, Charuel J-L, et al. Diagnostic potential of sarcoplasmic myxovirus resistance protein A expression in subsets of dermatomyositis. Neuropathol Appl Neurobiol 2019;45:513–22. 10.1111/nan.12519 [DOI] [PubMed] [Google Scholar]
- 42.Uruha A, Nishikawa A, Tsuburaya RS, et al. Sarcoplasmic MxA expression: a valuable marker of dermatomyositis. Neurology 2017;88:493–500. 10.1212/WNL.0000000000003568 [DOI] [PubMed] [Google Scholar]
- 43.Allenbach Y, Mammen AL, Benveniste O, et al. 224th ENMC International workshop:: Clinico-sero-pathological classification of immune-mediated necrotizing myopathies Zandvoort, the Netherlands, 14-16 October 2016. Neuromuscul Disord 2018;28:87–99. 10.1016/j.nmd.2017.09.016 [DOI] [PubMed] [Google Scholar]
- 44.Melki I, Devilliers H, Gitiaux C, et al. Circulating interferon-α measured with a highly sensitive assay as a biomarker for juvenile inflammatory myositis activity: Comment on the article by Mathian et al. Arthritis Rheumatol 2020;72:195–7. 10.1002/art.41096 [DOI] [PubMed] [Google Scholar]
- 45.Bourgoin P, Biéchelé G, Ait Belkacem I, et al. Role of the interferons in CD64 and CD169 expressions in whole blood: relevance in the balance between viral- or bacterial-oriented immune responses. Immun Inflamm Dis 2020;8:106–23. 10.1002/iid3.289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rigolet M, Hou C, Baba Amer Y, et al. Distinct interferon signatures stratify inflammatory and dysimmune myopathies. RMD Open 2019;5:e000811. 10.1136/rmdopen-2018-000811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Reed AM, Crowson CS, Hein M, et al. Biologic predictors of clinical improvement in rituximab-treated refractory myositis. BMC Musculoskelet Disord 2015;16:257. 10.1186/s12891-015-0710-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Savarese E, Chae O-wha, Trowitzsch S, et al. U1 small nuclear ribonucleoprotein immune complexes induce type I interferon in plasmacytoid dendritic cells through TLR7. Blood 2006;107:3229–34. 10.1182/blood-2005-07-2650 [DOI] [PubMed] [Google Scholar]
- 49.Ekholm L, Vosslamber S, Tjärnlund A, et al. Autoantibody specificities and type I interferon pathway activation in idiopathic inflammatory myopathies. Scand J Immunol 2016;84:100–9. 10.1111/sji.12449 [DOI] [PubMed] [Google Scholar]
- 50.Roos A, Preusse C, Hathazi D, et al. Proteomic profiling unravels a key role of specific macrophage subtypes in sporadic inclusion body myositis. Front Immunol 2019;10:1040. 10.3389/fimmu.2019.01040 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2021-001934supp001.pdf (15.8MB, pdf)
Data Availability Statement
Data are available on reasonable request. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.