ABSTRACT
Objective:
The objective of this scoping review was to map and describe the available evidence reporting out-of-pocket expenses related to aging in place for older people with frailty and their caregivers.
Introduction:
As the global population ages, there has been increasing attention on supporting older people to live at home in the community as they experience health and functional changes. Older people with frailty often require a variety of supports and services to live in the community, yet the out-of-pockets costs associated with these resources are often not accounted for in health and social care literature.
Inclusion criteria:
Sources that reported on the financial expenses incurred by older people (60 years or older) with frailty living in the community, or on the expenses incurred by their family and friend caregivers, were eligible for inclusion in the review.
Methods:
We searched for published and unpublished (ie, policy papers, theses, and dissertations) studies written in English or French between 2001 and 2019. The following databases were searched: CINAHL, MEDLINE, Scopus, Embase, PsycINFO, Sociological Abstracts, and Public Affairs Index. We also searched for gray literature in a selection of websites and digital repositories. JBI scoping review methodology was used, and we consulted with a patient and family advisory group to support the relevance of the review.
Results:
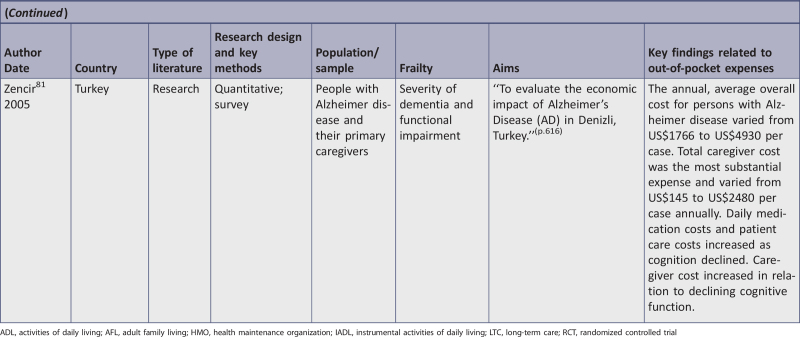
A total of 42 sources were included in the review, including two policy papers and 40 research papers. The majority of the papers were from the United States (n = 18), with others from Canada (n = 6), the United Kingdom (n = 3), Japan (n = 2), and one each from Australia, Brazil, China, Denmark, Israel, Italy, The Netherlands, Poland, Portugal, Singapore, South Korea, Taiwan, and Turkey. The included research studies used various research designs, including cross-sectional (n = 18), qualitative (n = 15), randomized controlled trials (n = 2), longitudinal (n = 2), cost effectiveness (n = 1), quasi-experimental (n = 1), and mixed methods (n = 1). The included sources used the term “frailty” inconsistently and used various methods to demonstrate frailty. Categories of out-of-pocket expenses found in the literature included home care, medication, cleaning and laundry, food, transportation, medical equipment, respite, assistive devices, home modifications, and insurance. Five sources reported on out-of-pocket expenses associated with people who were frail and had dementia, and seven reported on the out-of-pocket expenses for caregivers of people with frailty. While seven articles reported on specific programs, there was very little consistency in how out-of-pocket expenses were used as outcome measures. Several studies used measures of combined out-of-pocket expenses, but there was no standard approach to reporting aggregate out-of-pocket expenses.
Conclusions:
Contextual factors are important to the experiences of out-of-pocket spending for older people with frailty. There is a need to develop a standardized approach to measuring out-of-pocket expenses in order to support further synthesis of the literature. We suggest a measure of out-of-pocket spending as a percentage of family income. The review supports education for health care providers to assess the out-of-pocket spending of community-dwelling older people with frailty and their caregivers. Health care providers should also be aware of the local policies and resources that are available to help older people with frailty address their out-of-pocket spending.
Keywords: aging in place, frailty, older adult, out-of-pocket expenses, scoping review
Introduction
Improving the care of older people experiencing health and functional changes has become a priority for health care systems globally.1 The proportion of the population over 65 years of age is growing; it is estimated that by 2050 there will be 1.5 billion older people in the world, an increase from 703 million in 2019.2 Generally, people are living longer and more often have chronic health conditions than in the past.1,3 With these demographic changes, there has been concern among policy-makers that health care costs will grow.4 Supporting older people to live in the community as they experience health and functional changes has been promoted as a means to avoid preventable hospitalizations incurred due to insufficient support, and to limit health care costs associated with long-term care (LTC).5-8 The increasing interest in supporting older people to live in their homes in the community – often referred to as aging in place – as they experience health and functional changes also aligns with literature reporting on the preferences of older people, which demonstrates that they generally prefer to remain at home for as long as possible.9-11
There has been a growing imperative in health care literature to understanding the unique situation of older people who have multiple chronic conditions that contribute to functional impairment (ie, those considered frail). Frailty is associated with reduced function, a loss of independence, and need for support, as well as continual decline over time.12-14 To support this population to remain living in the community, a range of supports are needed, many of which are associated with out-of-pocket expenses – that is, expenses paid by older people and their caregivers without reimbursement.15 In addition to the health challenges associated with frailty, individuals and their families may experience unanticipated financial burden.16 Financial considerations contribute to decisions to move to LTC for older people.17 The costs to enable an older person to live at home may eventually be comparable to the costs of LTC, or financial concerns combined with other factors, such as safety or caregiver strain, may make living at home impossible.17 While it is essential to consider the sustainability of the health care system as the population ages, it is also important to consider how efforts to support older people in the community contribute to financial burden for them and their family caregivers.18
Frailty
Frailty is increasingly recognized as a physiological condition that impacts the health and quality of life of many older adults.8,13,14 While there is still considerable disagreement in the literature about the operational definition of frailty, it is generally used to refer to people experiencing a loss of capacity to recover after illness, in addition to a higher risk of poor outcomes such as falls, functional decline, mortality, and hospitalization.8,14,19-21 There is a growing body of literature reporting on how people living with frailty use health care services and community supports, which suggests that those who are frail have higher health and social care costs than those who are not frail.15,22,23 Frailty prevalence estimates vary significantly; a systematic review conducted in 2012 found that rates of frailty prevalence ranged from 4% to almost 60% of older people aged 65 years and older.24 Rates varied mainly due to two notable factors: i) the particular characteristics of the population, and ii) the definition of frailty used in the studies. Baseline data from a Canadian longitudinal study found frailty prevalence to be 10.6% in participants over 75 years, with more cases among women and increasing occurrence with age.25 A recent meta-analysis reported frailty prevalence rates in community-dwelling people 65 years or older in China as 5.9% to 17.4%.26 We included studies reporting on people over the age of 60 years experiencing frailty because it is the most inclusive age cut-off used to define older adults in the literature.
Out-of-pocket expenses
For this review, out-of-pocket expenses are defined as financial expenses incurred by older adults or family and friend caregivers to enable frail older people to live well in their homes in the community. Out-of-pocket expenses associated with living well at home include a broad array of services and supports that are related to medical conditions or functional impairment, but are not paid or reimbursed by public health care systems or covered by health insurance. For example, expenses may include assistive devices or over-the-counter medications to address symptoms of health conditions, services such as property maintenance, or essential home modifications to ensure safety when individuals experience functional decline. Literature reporting on the impact of out-of-pocket expenses for people experiencing specific health conditions (eg, cancer, chronic obstructive pulmonary disease, diabetes) also suggests that out-of-pocket spending related to their health conditions impacts their ability to afford basic living expenses such as food and shelter.27-29 For older people with frailty, who have multiple health conditions that affect their functional abilities, medical and non-medical out-of-pocket expenses are a particularly important issue. Older people are often on fixed incomes, and those experiencing frailty may have few opportunities to engage in paid work.1 Significant out-of-pocket expenses combined with limited income can contribute to financial insecurity in older people, which in turn can contribute to medication non-adherence, disrupted access to health care, and inability to leave unsafe living environments.1,27,30
While there has been a concerted effort by many health and social care leaders to support older people with frailty to live in the community to reduce unnecessary costs associated with LTC,1,18 the individual-level expenses required to enable living well at home are often not explicitly addressed. In 2010, Johnson and Mommaerts predicted that out-of-pocket spending by older people in the United States would increase over the subsequent 30 years, contributing to significant financial strain.31
A preliminary search of PROSPERO, MEDLINE, the Cochrane Database of Systematic Reviews, and JBI Database of Systematic Reviews and Implementation Reports was conducted and no planned or in-progress systematic or scoping reviews examining the out-of-pocket expenses to support frail older people in the community were identified. While there have been reviews that address the costs associated with supporting older people with frailty in the community, these reviews have approached the subject from the perspective of the health care system and society,32 and have not considered out-of-pocket expenses borne by individuals and caregivers. Looman and colleagues conducted a review of literature reporting on preventive and integrated care for older people with frailty in the community and reported cost effectiveness from societal and health care perspectives.33 Apóstolo and colleagues published a systematic review of the effectiveness of interventions to limit the progression of frailty, and included an analysis of health care costs.34 Lastly, a review by Young and colleagues compared the health care costs of functionally dependent older adults in the community with health care costs of providing care to this population in LTC.35 However, none of these studies examined the out-of-pocket costs assumed by individuals with frailty and their caregivers. A fourth review explored the economic costs associated with caregiving, and included findings related to out-of-pocket expenses.16 This scoping review did not discuss the out-of-pocket expenses of caregivers or include information on the out-of-pocket expenses incurred by older people with frailty themselves.16
The objective of this scoping review was to map and describe the available evidence reporting out-of-pocket expenses related to aging in place for older people with frailty and their caregivers. An understanding of this literature is important as further synthesis of the available literature can shape policy and practice to better support older people with frailty to continue living in their homes.
Review question
What is the evidence on out-of-pocket expenses associated with aging in place for older people with frailty, and their family and friend caregivers?
Inclusion criteria
Participants
This scoping review considered all research studies and policy papers that included older people experiencing frailty living in community settings, as well as sources that included family and friend caregivers of older people with frailty. Studies that included participants aged 60 years and older, with multiple chronic conditions and functional impairment were included. While our protocol stated we would include studies that employed a measure of frailty, we ultimately decided to broaden our inclusion criteria to studies that described their population as frail or included an older population with multiple chronic conditions and functional impairment,36 because the term “frailty” is not consistently defined or applied in the literature.8
Concept
This review considered studies that reported on the financial, out-of-pocket expenses incurred by older people living with frailty in the community or by their family and friend caregivers. Out-of-pocket expenses are those that are paid by individuals, and do not include expenses paid by public funding or by third parties such as insurance companies. We only included actual expenses, and did not include studies that estimated financial implications, such as lost income due to unpaid caregiving responsibilities.
Context
This review considered studies that focused on older people living in the community and excluded studies reporting on older people living in LTC or assisted living facilities. Studies conducted in all countries were eligible for inclusion.
Types of sources
For this scoping review, we included published and unpublished original research and policy papers that explored issues related to out-of-pocket spending by frail older adults or their caregivers.
Methods
This review was conducted in accordance with the JBI methodology for scoping reviews,37 and included input from people with lived experience supporting older people with frailty through two patient and caregiver engagement groups.38,39 The involvement of stakeholders in scoping reviews aims to provide grounding for the study and foster discussion about potential implications. The patient and caregiver advisory groups in this project contributed to developing the research questions and inclusion criteria, identified keyword synonyms to include in the search, supported the identification of gaps in the body of literature, and generated new ideas about implications of the review.
Search strategy
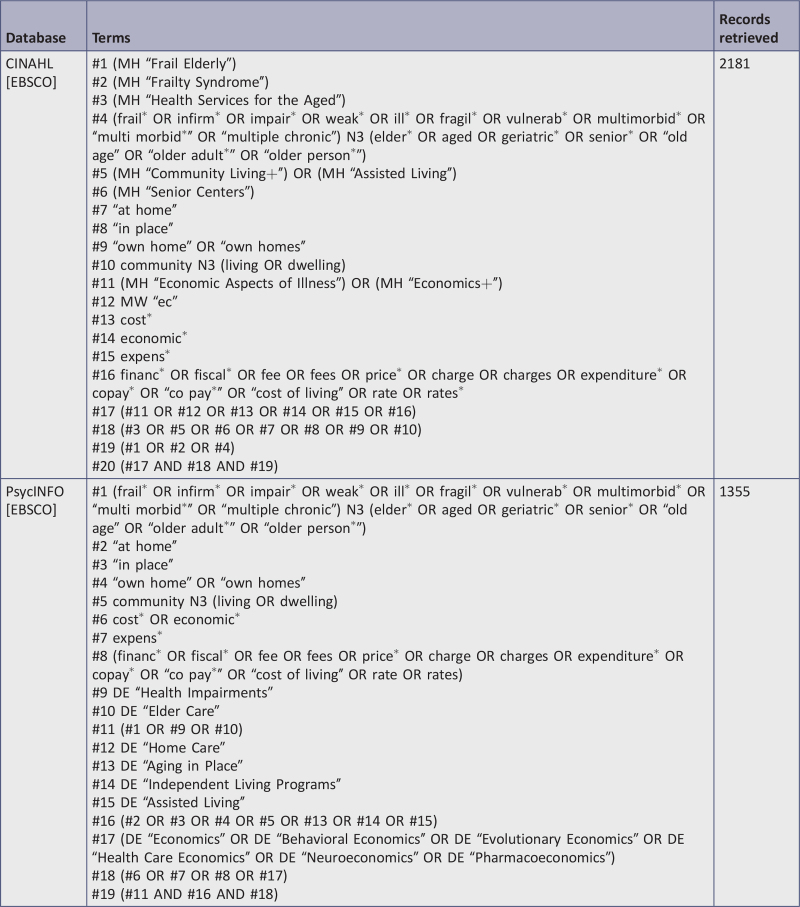
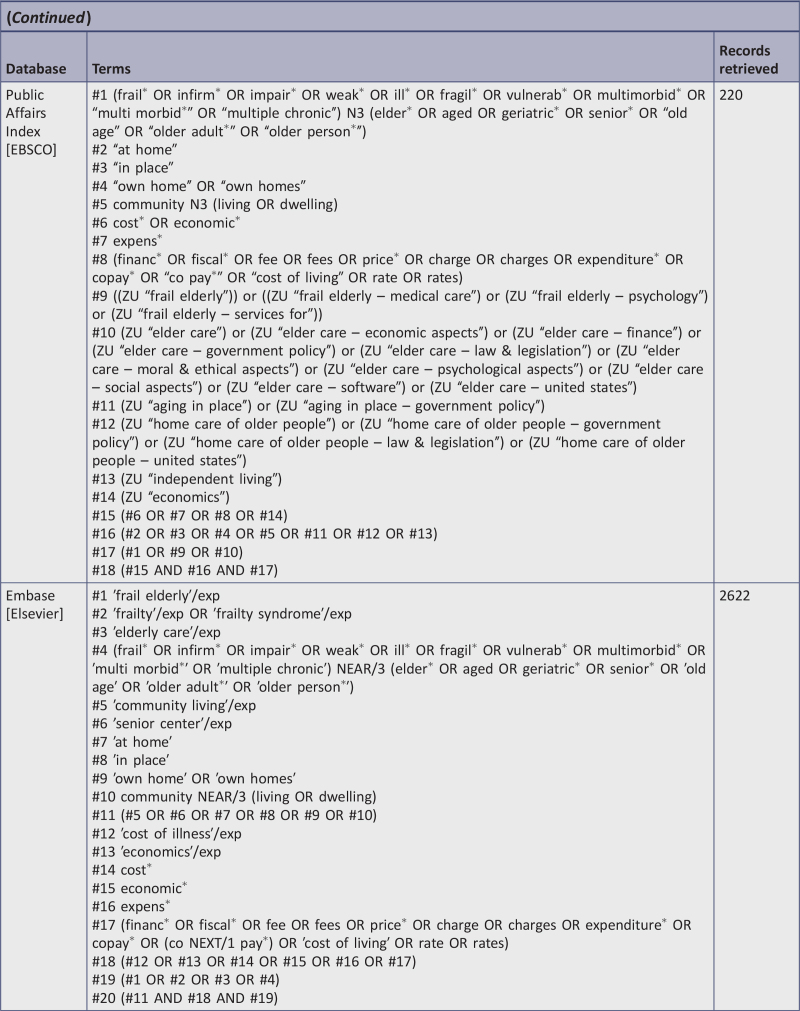
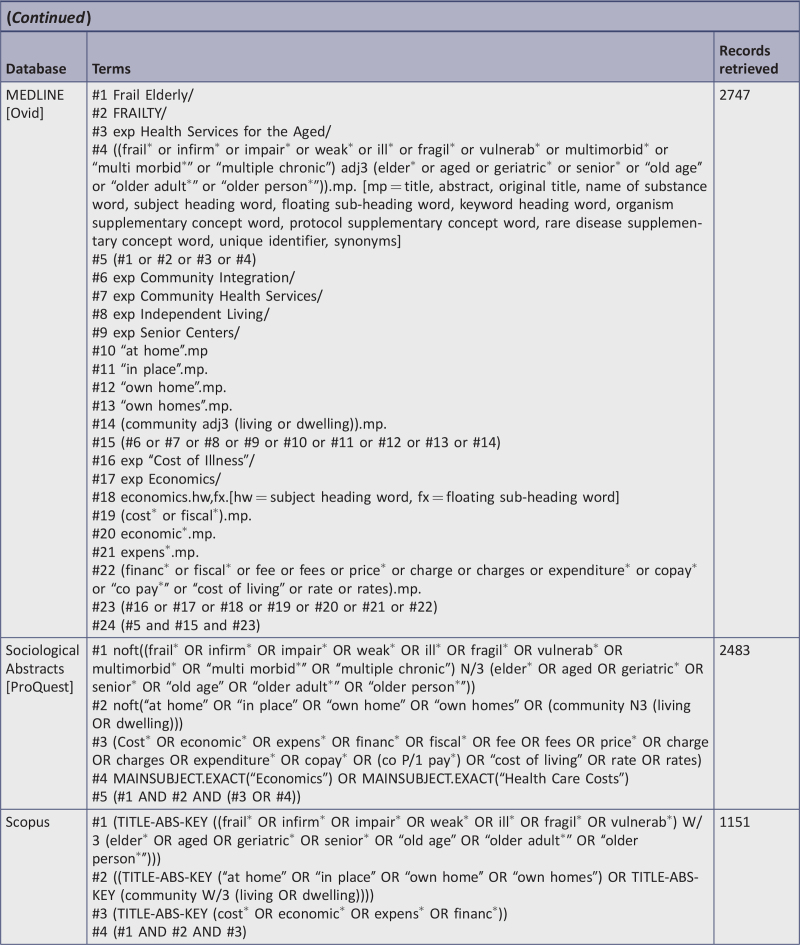
The search strategy aimed to find both published and unpublished literature (ie, policy papers, theses, and dissertations). A three-step search strategy was used to identify published literature. An initial limited search of MEDLINE (Ovid), CINAHL (EBSCO), and Embase (Elsevier) was undertaken followed by an analysis of the text words contained in the title and abstract, and of the index terms used to describe the article. A second systematic search using all identified keywords and index terms was then undertaken across all included published literature databases on September 27, 2019. Third, reference lists of included literature were hand searched for additional relevant studies. The search strategy is included as Appendix I.
The databases searched for published literature include: CINAHL (EBSCO), MEDLINE (Ovid), Scopus, Embase (Elsevier), APA PsycINFO (EBSCO), Sociological Abstracts (ProQuest), and Public Affairs Index (EBSCO). MEDLINE (Ovid) replaced PubMed (listed in the protocol) because the final search strategy included two lines that incorporate adjacency searching, which PubMed does not support.
Due to limited resources, only literature published in English or French was considered for inclusion in this review. We restricted our review to studies conducted after 2001 when a seminal definition of frailty was published21; this is a deviation from the protocol.
The search for gray literature was completed on September 27, 2019, and targeted the following websites and digital repositories: Agency for Healthcare Research and Quality, Alzheimer's Association: Alzheimer's Disease and Dementia (US), Alzheimer Society of Canada, Alzheimer's Society (UK), American Nurses Association, Canadian Nurses Association, centers for health evidence, conference proceedings, digital dissertations, DiVA (dissertations and other publications in full text from Nordic Universities), EPPI-Centre, Google Scholar, GrayLIT Network, Gray Literature Bulletin (North West Health Library and Information Services, Liverpool, UK), Gray Literature Report (via New York Academy of Medicine website), Gray Source: a Selection of Web-based Resources in Gray Literature, Index to Theses, Institute for Health and Social Care Research, National Information Center on Health Services Research and Health Care Technology, National Library of Medicine, Netting the Evidence, Networked Digital Library of Theses and Dissertations, New York Academy of Medicine Gray Literature Report NLM Gateway, Policy Hub, Primary Care Clinical Practice Guidelines, ProQuest Dissertations and Theses Databases, PsycExtra, Public Health Agency of Canada, SIGLE (System for Information on Grey Literature in Europe), and TRIP (Turning Research into Practice).
Study selection
After the search was completed, all citations were uploaded to Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia) and duplicates removed. Two reviewers (from among EM, RG, RMM, JP, MM, LEW, EO, and KJ) independently screened the title and abstract of each citation, and selected studies that met the inclusion criteria. The full-text articles were retrieved and uploaded into Covidence. These studies were then assessed independently by two reviewers (from among those listed above) to determine if they met the study inclusion criteria. Any disagreements between the two independent reviewers at each review stage were resolved by consensus or with a third reviewer. Quality appraisal of selected studies was not conducted, as the standard procedure and aim of scoping reviews is to provide an overview of the literature.37
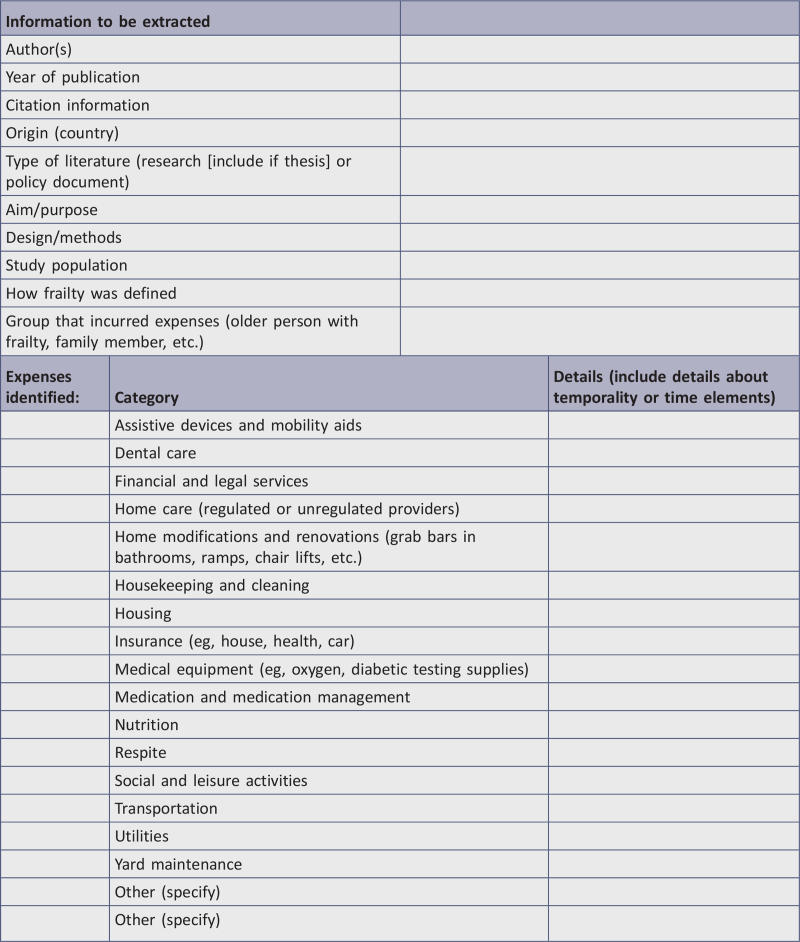
Data extraction
Following the JBI scoping review methodology,37 data were extracted from included papers by two independent reviewers (from among EM, RG, RMM, JP, MM, LEW, EO, and KJ) using a data extraction tool (Appendix II) developed by the reviewers and refined following a piloting with a small number of studies, and subsequently applied to all included studies. Categories of out-of-pocket expenses were refined throughout the data extraction process to ensure all extracted data were accounted for. Any disagreements that arose between the reviewers were resolved through discussion or with a third reviewer.
Data analysis and presentation
Results are reported graphically with tables when possible. The narrative that accompanies the tables further describes the body of literature. The findings of the review are reported in four sections that were determined once the relevant sources were identified to reflect the objectives of the review. The sections are: i) categories of out-of-pocket expenses, ii) measures of combined out-of-pocket expenses, iii) out-of-pocket expenses for select populations, iv) out-of-pocket expenses as outcomes in the evaluation of policies, programs, and services.
Results
Study inclusion
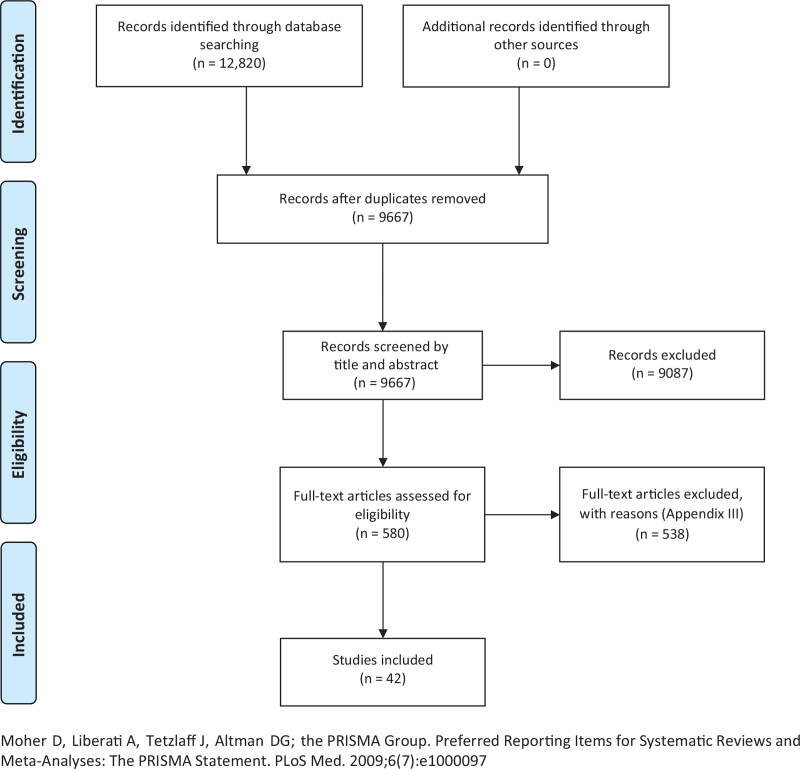
A total of 12,820 titles were identified and uploaded to Covidence for screening. Of these, 3153 were duplicates. At the title and abstract phase, 9667 studies were screened, with 9087 studies found ineligible. There were 580 full-text studies assessed for eligibility through full-text screening, and 538 were excluded (see Figure 1).
Figure 1.
Search results and source selection and inclusion process
Reasons for exclusion were as follows: not a research study or policy document (173), not reporting on out-of-pocket expenses (139), not including an older population that was frail (193), written in a language other than English or French (17), and not set in the community (10). Six citations were not available as full text through our libraries or after contacting the authors. Detailed information on the reason for exclusion of each article can be found in Appendix III. The resulting 42 articles were included in the review. An examination of the reference lists of the included papers did not result in any further literature for inclusion.
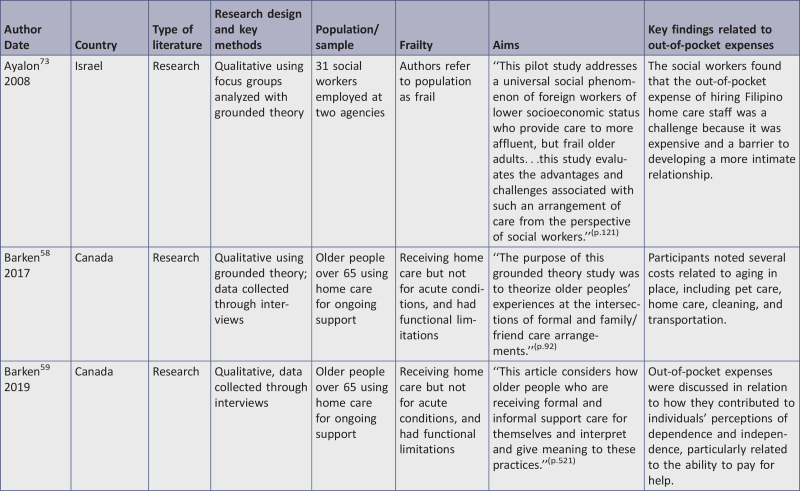
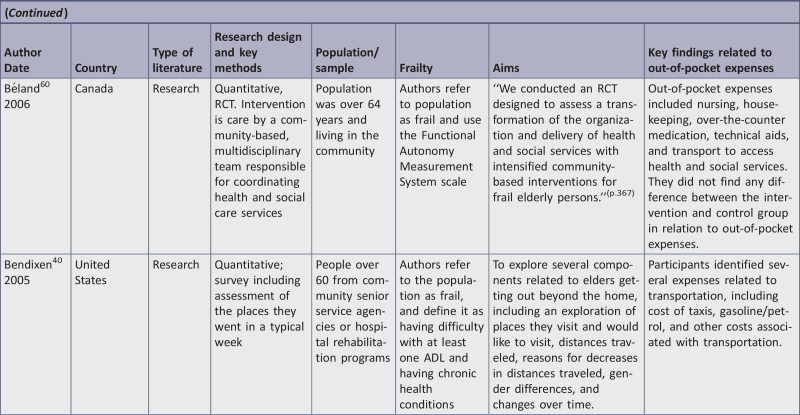
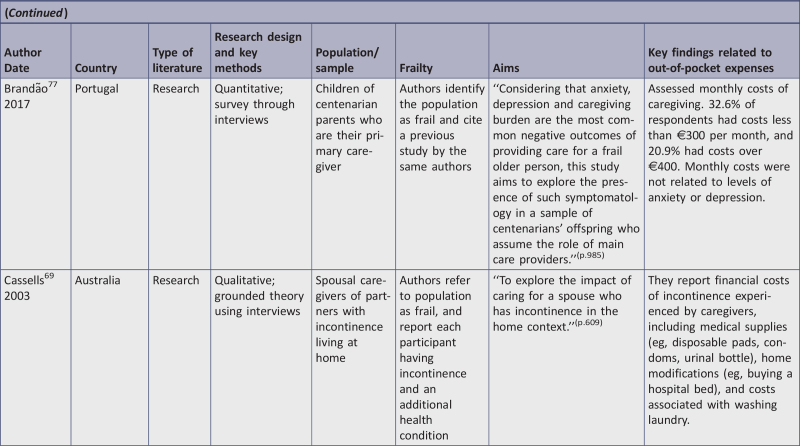
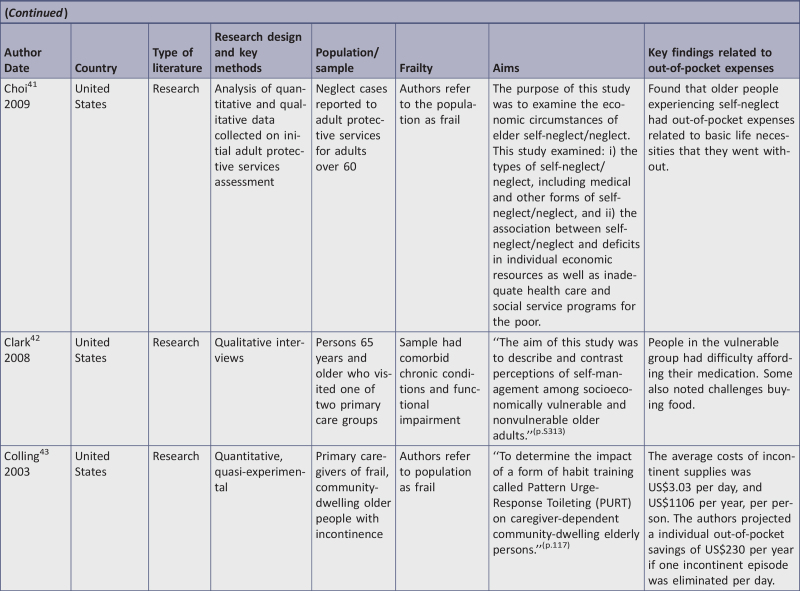
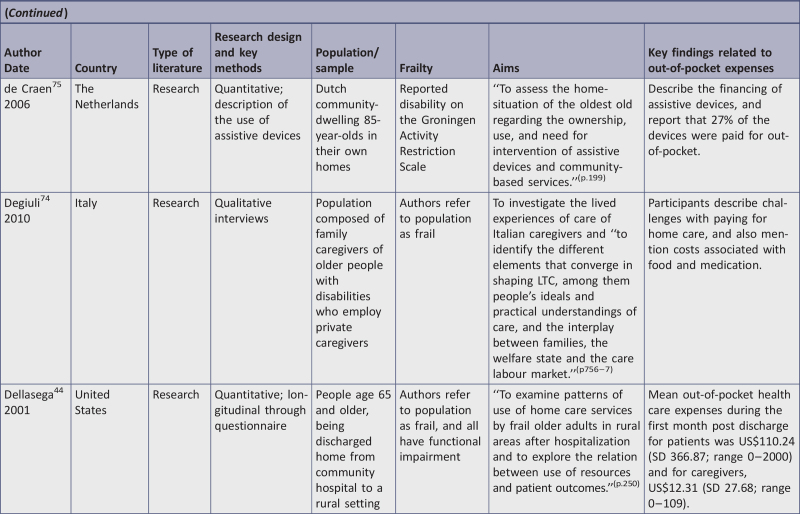
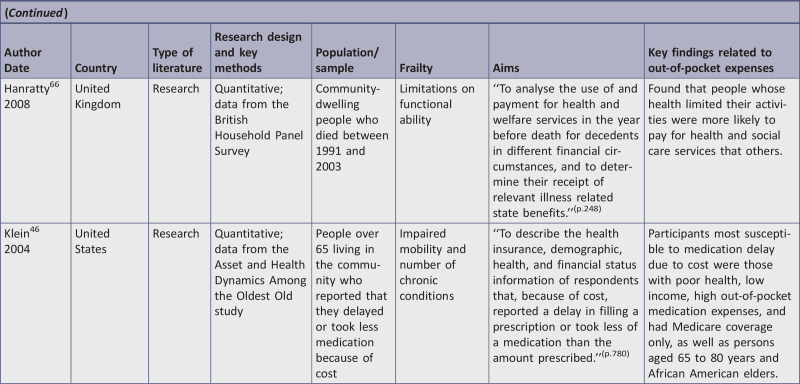
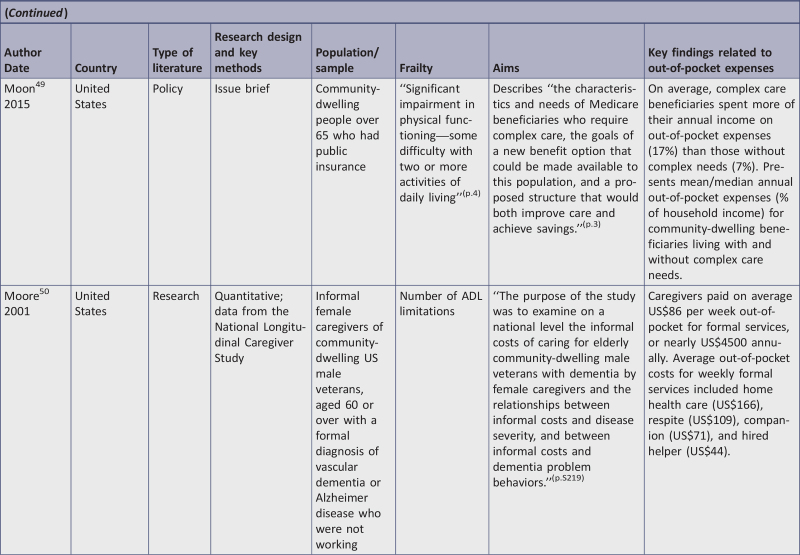
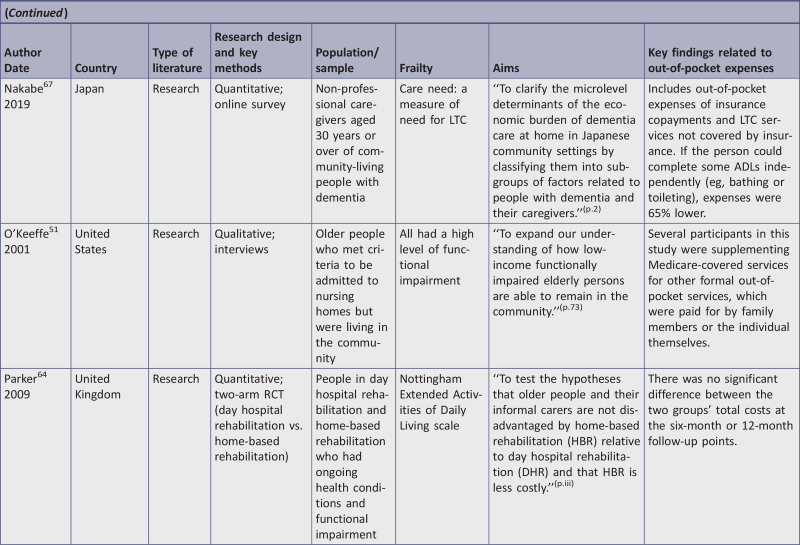
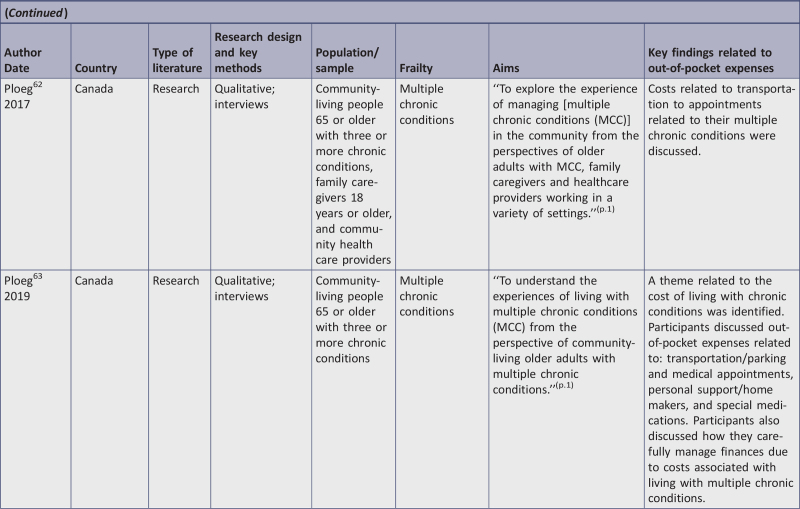
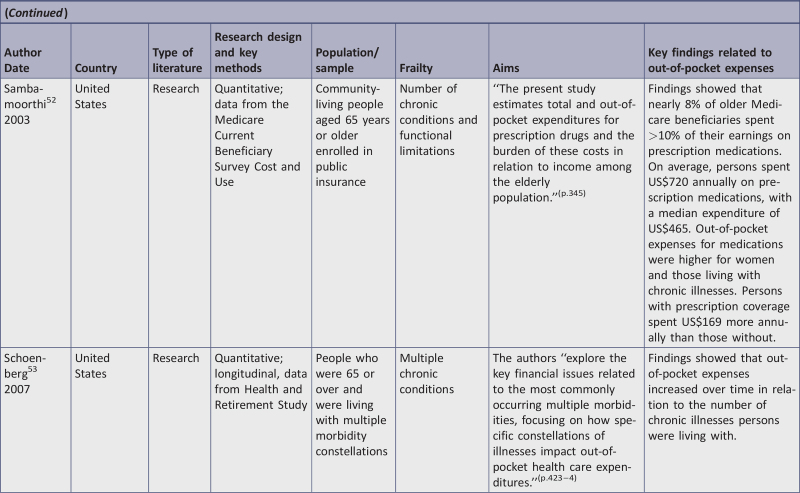
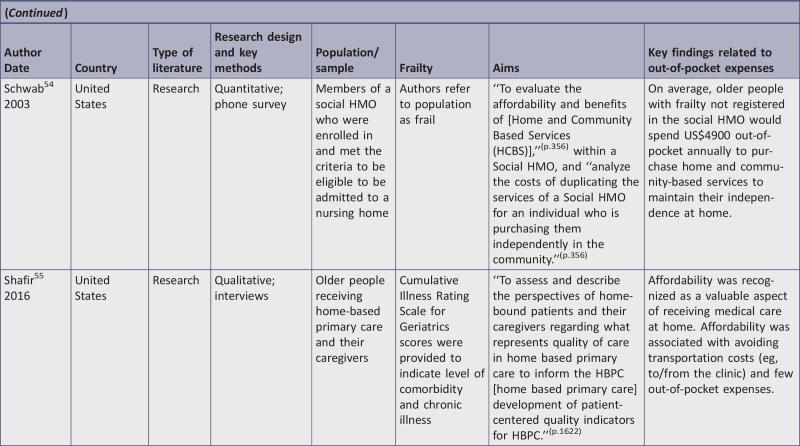
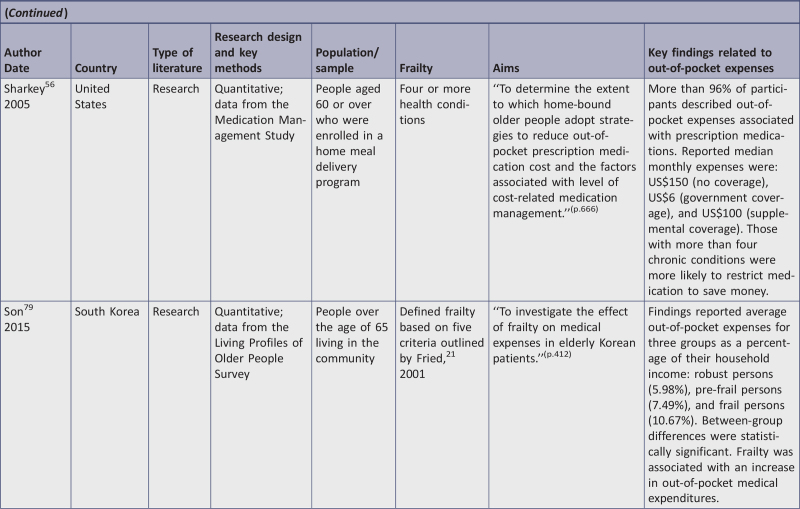
Characteristics of included studies
The characteristics of the included sources are presented in Appendix IV. The majority of the papers were from the United States (n = 18).40-57 Others were from Canada (n = 6),58-63 the United Kingdom (n = 3),64-66 Japan (n = 2),67,68 and one apiece from Australia,69 Brazil,70 China,71 Denmark,72 Israel,73 Italy,74 The Netherlands,75 Poland,76 Portugal,77 Singapore,78 South Korea,79 Taiwan,80 and Turkey.81 Studies were published across the date range included (2001 to 2019); there did not appear to be any trends in studying this issue over time. Most sources included costs incurred by individuals and their caregivers, but seven reported costs only for caregivers.50,61,67-69,77,78 Forty articles were journal articles reporting research findings and two were policy papers.49,72 The included research studies used various research designs, including cross-sectional (n = 18),40,45,46,48,50,52,54,56,57,66-68,70,71,75,77,79,81 qualitative (n = 15),42,47,51,55,58,59,61-63,69,73,74,76,78,80 randomized controlled trials (RCTs; n = 2),60,64 longitudinal (n = 2),44,53 cost effectiveness (n = 1),65 quasi-experimental (n = 1),43 and mixed methods (n = 1).41
Review findings
The results of this scoping review are discussed under the follow sections: i) categories of out-of-pocket expenses, ii) measures of combined out-of-pocket expenses, iii) out-of-pocket expenses for select populations, and iv) out-of-pocket expenses as outcomes in the evaluation of policies, programs, and services.
Categories of out-of-pocket expenses
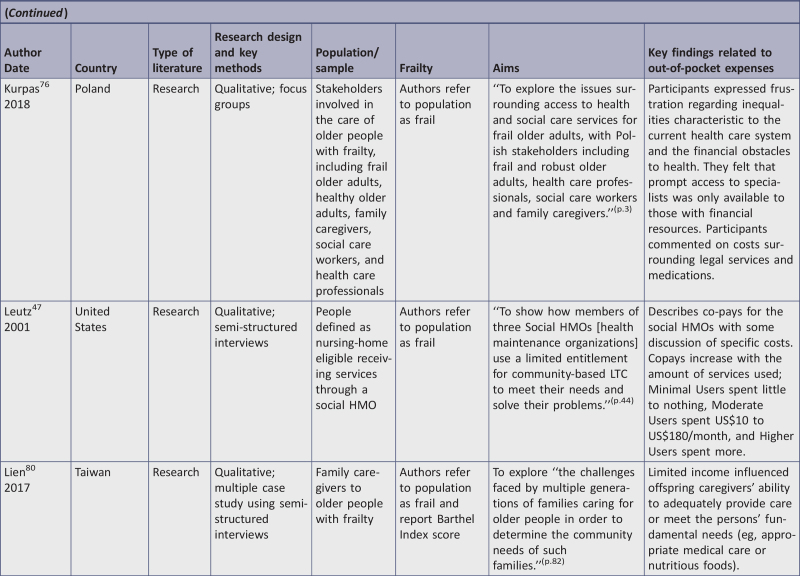
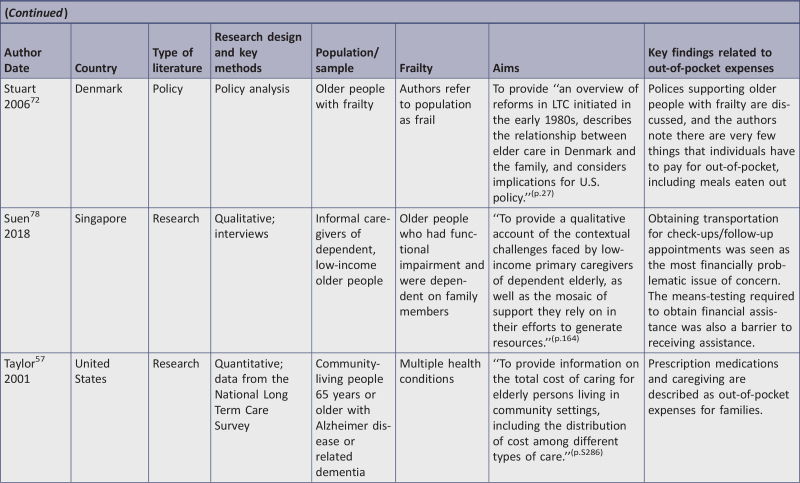
We categorized the expenses that each source identified, and summarized the findings in Table 1. The categories were developed by consensus of the review team. The most common category of out-of-pocket expense discussed was home care provided by regulated or unregulated providers (n = 16), followed by medication and medication management (n = 12), cleaning and laundry (n = 10), food and meal preparation (n = 9), transportation (n = 8), medical equipment and assistive devices (n = 8), respite care (n = 6), home modifications and renovations (n = 5), and insurance (n = 5). Other out-of-pocket expenses that were identified by one or two sources included dental care,53 emergency response systems,47 yard maintenance,47 doctors’ visits,53 financial transfers to family members,71 pet care,58 vacations,74 hair care,50 health care specialists,70 financial and legal services,76 and care planning services.68
Table 1.
Categories of out-of-pocket expenses related to aging in place for frail older people
| Author | Home care | Medication | Cleaning and laundry | Food | Transportation | Medical equipment and assistive devices | Respite | Home modifications | Insurance | Other |
| Ayalon et al. 200873 | X | |||||||||
| Barken 201758 | X | X | X | Pet care | ||||||
| Barken 201959 | X | |||||||||
| Beland et al. 200660 | X | X | X | X | X | |||||
| Bendixen et al. 200540 | X | |||||||||
| Cassells and Watt 200369 | X | X | ||||||||
| Choi et al. 200941 | X | X | X | X | Utilities | |||||
| Clark et al. 200842 | X | X | ||||||||
| Colling et al. 200343 | X | |||||||||
| de Craen et al. 200675 | X | X | ||||||||
| Degiuli 201074 | X | Vacations | ||||||||
| Dosman and Keating 200561 | X | X | X | |||||||
| Flood et al. 200565 | ||||||||||
| Freedman and Spillman 201445 | X | |||||||||
| Hanratty et al. 200866 | X | X | ||||||||
| Klein et al. 200446 | X | |||||||||
| Kurpas et al. 201876 | X | Financial and legal services | ||||||||
| Leutz et al. 200147 | X | X | X | Yard maintenance; emergency response systems | ||||||
| Lien and Huang 201780 | X | X | ||||||||
| Liu et al. 201771 | Financial transfers to children | |||||||||
| Moore et al. 200150 | X | X | X | Hair care | ||||||
| Nakabe et al. 201967 | X | |||||||||
| O’Keefe et al. 200151 | X | X | X | X | ||||||
| Ploeg et al. 201762 | X | |||||||||
| Ploeg et al. 201963 | X | X | X | X | ||||||
| Sambamoorthi et al. 200352 | X | |||||||||
| Schoenberg et al. 200753 | X | X | X | Doctor or dental visits | ||||||
| Schwab et al. 200354 | X | X | X | X | X | X | ||||
| Shafir et al. 201655 | X | Physician access | ||||||||
| Sharkey et al. 200556 | X | |||||||||
| Stuart and Hansen 200672 | X | X | ||||||||
| Taylor et al. 200157 | X | |||||||||
| Veras et al. 200870 | X | X | X | X | X | X | X | X | Health care specialists | |
| Washio et al. 201268 | X | X | X | X | X | X | Care plan services | |||
| Zencir et al. 200581 | X | |||||||||
| Total | 16 | 12 | 10 | 9 | 8 | 8 | 6 | 5 | 5 |
Home care
Several studies had an explicit focus on the costs associated with home care for older people with frailty, such as the expenses associated with hiring regulated and unregulated care providers to perform various activities of daily living (ADLs). Two studies discussed the costs associated with hiring unregulated migrant home care workers to provide care for older people.73,74 Both studies indicated that unregulated migrant home care workers were often hired because they cost less than other home care services. However, the expense of their employment impacted the experience of out-of-pocket spending for caregivers forced to balance the costs of care with the desired quality of care. In Israel, Ayalon and colleagues reported from the perspective of social workers who suggested that families found out-of-pocket costs to hire private care providers contributed to the challenges of caring for older people.73 In Italy, Degiuli reported findings from interviews with family caregivers of older people and discussed expenses associated with hiring migrant nurses and unregulated care providers. Some study participants felt they could not afford “good care,”74(p.764) suggesting that good care would require spending more to have care providers come more often.
Freedman and Spillman examined the out-of-pocket costs associated with home care for people receiving public insurance benefits (Medicare and Medicaid) in the United States.45 They examined the average number of home care hours used by people requiring various levels of assistance and found that those with higher assistance needs not only received more home care but also paid higher amounts in out-of-pocket expenses, such as copayments and added services, than those with lower assistance needs.
Two papers by Barken conducted in Canada reported on a qualitative study of 34 older people receiving home care.58,59 One paper focused on how older people receiving home care balanced the expectations of family to be involved in their care with the role of care providers, and found that paying out-of-pocket for services lessened negative feelings associated with being a burden on family caregivers.58 The other paper explored how older people receiving home care experience independence and dependence, and found that paying out-of-pocket for services contributed to feelings of independence.59
Medication
Costs associated with medication and medication management were also a focus of many of the included sources. Sambamoorthi et al. examined the financial burden of prescription drugs for older people who were enrolled in a publicly funded insurance program in the United States (ie, Medicare and Medicaid), including an analysis of both total and out-of-pocket expenses.52 They gathered data on out-of-pocket expenses, including copayments, deductibles, and other charges, and found that higher out-of-pocket costs were related to higher levels of functional impairment, lower levels of self-reported health, more comorbid medical conditions, and female gender.
The out-of-pocket costs of medications and medication management were a particular concern when individuals had limited financial resources.41,42,46,56,76 Drawing from a national database in the United States, Klein and colleagues examined the characteristics of older people who delayed taking a prescribed medication due to cost.46 They found that people who had more medical illnesses, ADL limitations, or higher levels of mobility impairment were more likely to report delaying medication use due to cost. Similarly, Choi and colleagues examined the experiences of older people with frailty who were also experiencing neglect or self-neglect, and found that they sometimes did not purchase important medication and therefore did not follow the prescribed treatment, and noted costs as one of the reasons.41
Sharkey and colleagues also explored issues around individuals restricting medication use due to costs.56 They collected data on strategies undertaken to decrease medication costs from a sample of homebound older people receiving home-delivered meals in one US state (North Carolina), and found that 96% of respondents had out-of-pocket medication expenses, including copayments, co-insurance, and costs not covered by insurance. The authors reported monthly out-of-pocket spending by level of insurance; those with no drug coverage had a median monthly out-of-pocket medication cost of US$150, those with government coverage had costs of US$6, and those with supplemental drug coverage had costs of US$100. They also found that 20% of the total sample restricted medication use due to cost.
Clark and colleagues examined people who were socioeconomically disadvantaged, and found many had high copayments for medication that contributed to difficultly making payments.42 However, few participants in the study reported missing medications due to costs, unlike other research reported here. Ploeg and colleagues also found that the costs of medication affected the ability of older adults with multimorbidity to pay for other essentials, and had to be weighed against spending on other necessities.63 A study by Kurpas and colleagues exploring the experiences of older people with frailty in Poland accessing health care found that the high costs of medication in relation to available resources meant that many older people did not follow their prescribed treatment plan.76
Cleaning and laundry
Housekeeping, laundry, and cleaning were expenses frequently not covered by other programs and services.47,50,51,54,58,60,61,63,69,72 One study conducted in Canada reported that a woman with the financial means to easily pay for such services preferred to pay for them out-of-pocket rather than add to the burden of her family members.58 Other sources noted out-of-pocket costs for laundry services associated with incontinence,69 reported actual costs paid for cleaning,54 and included housekeeping costs in measures of combined out-of-pocket expenses.50,60
Food
Several identified sources noted meal delivery services requiring out-of-pocket costs.51,54,66,68,75 Two studies reported that other costs impacted the ability of people with frailty to pay for food.41,42 A policy paper from Denmark suggested that the costs associated with eating out at restaurants were one of the few out-of-pocket costs borne by people with frailty in that country.72 Only one study included the cost of food in a measure of combined out-of-pocket expenses.70
Transportation
Transportation expenses included the cost of taxis, public transportation, gasoline/petrol and car insurance, ambulance costs, and paying friends or family members to provide transportation. Bendixen and colleagues examined the experiences of older people with frailty getting out of their homes and included an exploration of related out-of-pocket costs.40 The authors drew on data from initial interviews with older people participating in a national longitudinal study in the United States. As part of their analysis, the authors reported the frequency that participants wanted to go somewhere but could not due to financial considerations such as the cost of taxis, gasoline/petrol, or other transportation costs. Seven percent of participants who wanted to go somewhere but could not cited transportation costs as the barrier.
Shafir and colleagues explored the experience of home-based primary care for homebound older people in the United States.55 A key theme that emerged was related to how the program impacted the costs of accessing medical care. Participants suggested that expenses related to transportation to medical appointments could be prohibitive, and that the home-based primary care program, covered by publicly funded insurance, eased the cost burden of accessing health care elsewhere. Ploeg and colleagues explored the experience of managing multiple chronic conditions for older people living in a Canadian community.62 They conducted interviews to gather the perspective of older people, caregivers, and health care providers. Participants noted that older people with multimorbidity, particularly those living in rural areas, had challenges accessing transportation to attend medical appointments. This was in a context where the participants attended frequent appointments due to their multiple health conditions, thus needed transportation often. Expenses related to transportation, along with expenses such as medication, were noted to impact decisions about how to spend limited resources, and impacted health and quality of life.63
Medical equipment and assistive devices
Medical equipment (eg, home oxygen delivery equipment, diabetic testing supplies, incontinence supplies) and assistive devices (eg, mobility aids) were also reported as out-of-pocket expenses. Two studies looked at out-of-pocket expenses related to incontinence specifically and noted the cost of supplies, such as incontinence pads, disposable pads, disposable diapers, disposable bed pads, and disposable gloves.43,69 Choi and colleagues noted that individuals experiencing neglect often went without cost-prohibitive medical supplies.41 Out-of-pocket costs for assistive devices included expenses such as purchasing mobility aids (eg, canes, walkers) and hearing and vision aids. de Craen and colleagues described the use of assistive devices by older people in The Netherlands.75 They found that devices used to support both mobility (43%) and personal care (27%) were often paid for out-of-pocket. Other sources included medical equipment and assistive devices as part of a combined measure of out-of-pocket expenses,60,70 reported actual costs of medical supplies,54 and identified expenses for medical supplies not covered by LTC insurance.68
Respite
Six studies included out-of-pocket expenses for respite care of older people experiencing frailty.50,51,53,54,68,70 Such expenses included adult day centers,51,54,70 short stays in residential care facilities,68,70 and other unspecified respite care.50,53,54
Home modifications
The sources that reported findings related to out-of-pocket expenses for home modifications described renovations or other significant changes to the home that enabled older people with frailty to adapt to changes in function. A study by Lien and Huang asked adult children of older people experiencing frailty in Taiwan about challenges in providing care.80 They found that the costs of adapting a home were often prohibitive and contributed to unsafe living circumstances for frail older people.80 Other studies included out-of-pocket expenses related to home modifications as part of combined measures of out-of-pocket expenses,70 expenses associated with providing an adult family living service,61 and the cost of services not covered by LTC insurance.68 Choi and colleagues noted that costs associated with home repairs (eg, leaking pipes, leaking roofs, broken toilets) sometimes precluded completing the repairs.41
Insurance
Two studies from Japan examined out-of-pocket expenses in the context of a country with a national LTC insurance program. Along with identifying expenses that were not covered by insurance, the studies reported expenses such as insurance copayments.67,68 Washio et al. found that caregivers reported being heavily burdened had higher insurance copayments than those with lower levels of burden.68 Nakabe et al. examined out-of-pocket expenses for caregivers of people with dementia by level of care need and found that copayments were related to care-need level, with caregivers of people with higher needs having higher costs.67 Insurance was also noted as an expense for adult family living programs61 and for people using social health management organizations.47 One study included insurance costs in measures of combined out-of-pocket expenses.70
Intergenerational financial transfer
One study conducted in China focused explicitly on intergenerational financial transfers. Liu and colleagues examined intergenerational informal support and financial transfers between older people and their children.71 Through a national survey, data were collected from almost 1700 older people with frailty.
Measures of combined out-of-pocket expenses
Several of the included sources used combined measures that were total spending amounts related to periods of time or types of expenses. Measures of combined out-of-pocket expenses included monthly out-of-pocket medical expenses,79 monthly caregiving costs,77 out-of-pocket spending on health care,44 privately paid expenses,82 out-of-pocket expenses over two weeks,60 expenses paid by individuals for health and social services in the 12 months preceding death,66 annual personal assistance expenditure,48 annual out-of-pocket spending,49 and out-of-pocket expenses over the past two years.53
Out-of-pocket expenses for select populations
Within the included studies, out-of-pocket expenses for two sub-populations were particularly common: people with dementia who were frail and caregivers of people who were frail.
Out-of-pocket expenses for people with Alzheimer disease and other dementias
Five of the included studies were focused on people with Alzheimer disease or other dementias. Taylor and colleagues reported on the total costs of care for older people with Alzheimer disease and related dementias living in the community, according to a national survey in the United States.57 They included an analysis of the out-of-pocket prescription drug costs for this population and found that while most costs were higher for people with more severe dementia, out-of-pocket prescription costs were not higher for people with more severe dementia. In contrast, Zencir and colleagues examined costs associated with Alzheimer disease through data collected from 42 people with Alzheimer disease and their caregivers in Turkey.81 While their analysis focused on total costs that included both direct and indirect costs, they also noted that out-of-pocket costs for medications increased with the severity of Alzheimer disease.
Nakabe and Huang examined the economic burden of dementia in Japan.67 They specifically collected data about out-of-pocket costs that were not reimbursed by the LTC insurance program. They found that out-of-pocket expenses were related to caregivers’ income, the functional ability of the people with dementia, and the age of the people with dementia. For people with dementia with the highest care needs, the average daily costs of care were estimated to be US$352, compared to US$95 for those at the lowest care-need level. A study by Moore and colleagues examined experiences of female caregivers of male veterans with dementia, and categorized data based on the number of limitations in completing ADLs experienced by the older person with dementia.50 The study found that caregivers of people with more limitations faced higher out-of-pocket expenses. For example, caregivers of people with more than seven limitations reported paying for an average of 19.8 hours of home health care, which resulted in average costs of US$164 per month. Veras and colleagues examined the out-of-pocket expenses of caregivers of people with dementia in Brazil.70 They found that expenditures varied by severity of disease and the number of other chronic diseases present.
Out-of-pocket expenses for caregivers
Seven studies examined out-of-pocket expenses for family and friend caregivers of older people with frailty. Two studies explored perspectives of caregivers and highlighted areas where caregivers spent significant amounts on the care of older people with frailty, and may benefit from further publicly funded support. Suen and Thang explored the experience of low-income caregivers of dependent older people in Singapore.78 They noted that while there were government subsidies that kept medical costs low, there were gaps in resources available to support transportation needs. They also identified administrative costs for caregivers, such as paying fees related to having medical certificates sent to necessary authorities. Veras and colleagues conducted a study in Brazil that examined out-of-pocket costs for family caregivers of older people with dementia.70 The authors found that, on average, caregivers spent 66% of the family's income on costs associated with caring for the person with dementia.
Washio examined factors that contributed to caregiver burden among caregivers of older people receiving regular hemodialysis treatment in Japan.68 While many of the services received were paid for by Japan's LTC insurance program, the study measured out-of-pocket costs, including copayments, of the insurance program.
Lien and Huang described the experiences of caregiving for intergenerational family members of older people in Taiwan.80 They found that some families struggled with the costs of supporting frail older relatives, noting costs associated with nutritious food, medical care, and home care. Similarly, Degiuli explored the experiences of caregivers of frail older people and noted expenses related to groceries, utilities, and home care.74 Moore and colleagues used a national database in the United States to examine the costs incurred by female caregivers of older male veterans with dementia.50 They found that, on average, caregivers paid more for care when the person with dementia had higher care needs.
In their study examining sources of strain and distress among caregivers of people older than 100 years in Portugal, Brandão and colleagues examined the relationship between monthly out-of-pocket costs and burden.77 The study reported monthly costs of caregiving, but did not report details on how the money was spent.
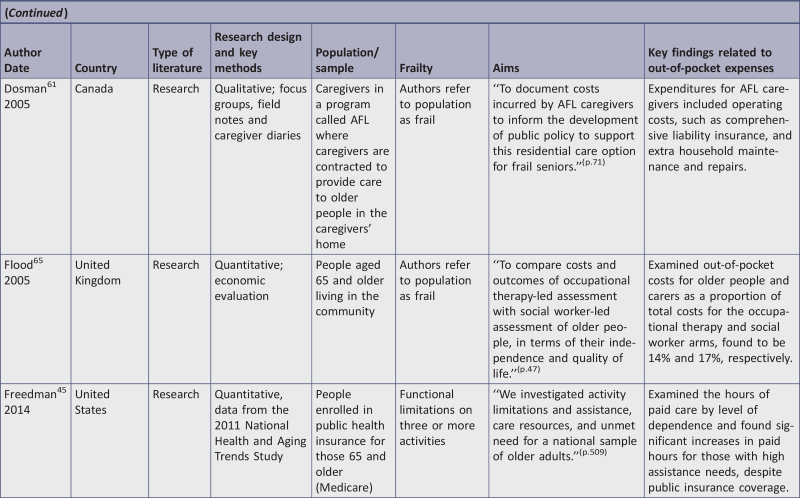
Out-of-pocket expenses as outcomes in the evaluation of policies, programs, and services
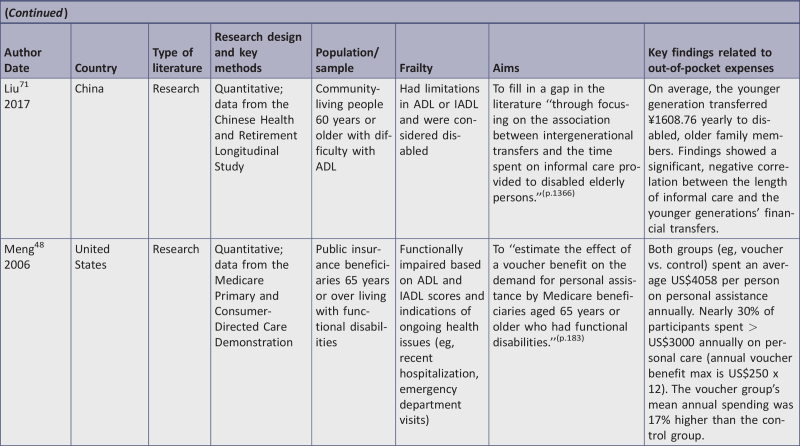
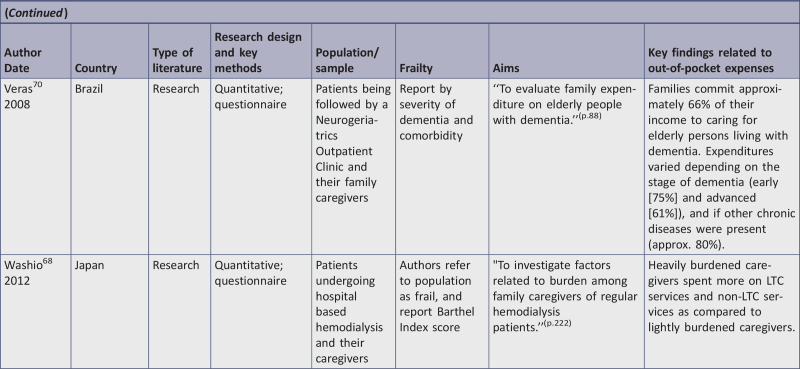
Another key area of the findings was related to the influence of various interventions on out-of-pocket expenses for older people living with frailty in the community. A summary of these sources can be found in Table 2.
Table 2.
Summary of sources that discussed out-of-pocket expenses as outcomes in evaluating policies, programs, and services related to aging in place for frail older people
| Author Country |
Intervention (program/service/policy) | Brief description | Method of evaluation | Findings related to out-of-pocket expenses |
| Béland et al.60 Canada |
Community-based multidisciplinary teams | Provision of community-based multidisciplinary integrated care | RCT | No difference was found for out-of-pocket expenditures between control and intervention groups |
| Dosman and Keating61 Canada |
Program | Provision of high-level care for individuals in a home-like environment | Focus groups | Costs incurred for caregivers included insurance payments, safety equipment, and maintenance/repair expenses |
| Flood et al.65 UK |
Program | Community assessments provided by social workers and occupational therapists | Cost comparison | Costs for participants assessed by social workers were higher; however, the difference was significant only to caregivers |
| Leutz et al.47 US |
Social HMO program | Provision of community-based care services | Qualitative interviews | Some people were found to have expenses beyond program coverage (eg, home care, yard work) Described additional out-of-pocket payments associated with the program that varied according to need |
| Meng et al.48 US |
Voucher program | Vouchers used to reimburse personal assistance expenditures | Quantitative survey data | Intervention group had higher expenditures, and those with higher functional impairment had higher service usage |
| Moon et al.49 US |
Policy | Description of financial implications of older adults’ complex health needs | Policy analysis | Older people with complex needs have higher out-of-pocket expenses Describes proposed complex care option for Medicare |
| Parker and Hill82 UK |
Program | Home-based and day hospital rehabilitation | RCT | Cost analysis found no significant difference between total costs of intervention and control groups |
| Schwab et al.54 US |
Social HMO program | Provision of community-based care services | Gathering actual costs | Average annual estimated costs of services were found to be US$4900 out-of-pocket No comparison with group who received social HMO |
| Stuart and Hansen72 Denmark |
Policy | Description of care services for older people with frailty in Denmark | Policy analysis | Description of how public services and family caregivers cooperate to provide care Note that some out-of-pocket expenses occurred; however, overall sources provided adequate support |
HMO, health maintenance organization; RCT, randomized controlled trial.
While this review was open to policy papers that described the impact of policies on the out-of-pocket expenses of older people with frailty, we only identified two such sources. They provided information on how policies impact the experiences of people with frailty. Stuart and Hansen provided a description of LTC services for older people with frailty in Denmark.72 They described how public services and family caregivers work together to provide care for older people with frailty to meet their complex health and social needs, and described the various policies that supported this situation. They noted that older people at times paid out-of-pocket for household cleaning and meals (if they ate outside the home) but generally, public and family resources provided adequate support for them.
The second policy paper was an issue brief by Moon and colleagues that addressed the financial implications of complex health needs of older people in the United States, and proposed a benefit option as part of the Medicare public insurance program to cover home and community services associated with living in the community.49 The authors noted that older people with complex needs have higher out-of-pocket expenses than those with less complex needs. The next step, according to the authors, is to examine the financial implications of implementing such a program.
Of the seven research studies that reported on the evaluation of programs and services programs, three were conducted in the United States and included discussion of the costs borne by older people with frailty and their caregivers beyond what was covered by publicly funded insurance (ie, Medicare and Medicaid).47,48,54 Two included studies examined social health maintenance organizations (HMOs), which provided community-based LTC.47,54 Leutz and colleagues described the experiences of older people using such a program, noting that some people had expenses for services above and beyond what were covered by the program, such as home care, transportation, and yard work.47 They also described the out-of-pocket costs associated with being part of the social HMO whereby members of the program paid a monthly premium that varied according to their need, as well as copayments for specific services. Schwab and colleagues examined costs associated with a specific social HMO.54 These authors calculated what it would cost to pay out-of-pocket for each of the services the program offered. The actual costs reported were obtained by surveying service and supply providers in the community, and reflect an average of several responses. They found that the services would cost an average of $4900 out-of-pocket per year, but did not include a comparison to the cost of delivering the service. Also in the United States, Meng and colleagues evaluated the effect of a voucher program on the out-of-pocket expenditures for personal assistance of older people in the community.48 The study reported on an RCT of a voucher program that reimbursed personal assistance expenditures. The study found that the intervention group had higher expenditures, and that persons with more functional impairment had higher service use than those without.
Two research studies from the United Kingdom examined programs provided by health care professionals that supported older people with frailty in the community. Flood and colleagues compared the costs and outcomes of community assessments led by social workers and occupational therapists.65 The authors found that costs for participants being assessed by social workers were higher, although the difference was only significant for costs incurred by caregivers. Parker and colleagues conducted an RCT to determine the effectiveness of home-based rehabilitation compared to day hospital rehabilitation for older people, and included a cost minimization analysis of total costs of care after six and 12 months.64 The cost minimization analysis found no statistically significant differences in the total costs between the intervention and control groups.
In Canada, Béland and colleagues reported on an RCT aimed to determine the effectiveness of an intervention comprised of community-based multidisciplinary teams providing integrated community care to older people with frailty.60 The authors analyzed the effect of the intervention on out-of-pocket expenditures including “nursing, homemaker, over-the-counter medication, technical aids, and transport to access health and social services.”(p.370) They found that there were no differences in out-of-pocket expenditure between the control and intervention groups. Also from a Candian context, Dosman and Keating studied the experience of caregivers in an adult family living program.61 Adult family living programs, also called adult foster care, offer people who are in need of high levels of care a home-like environment in the community where they receive accommodation, food, and other care from a paid caregiver in the caregiver's home. The authors asked people filling the role of caregiver in the program what types of costs they incurred, and found that insurance payments, safety equipment, and maintenance and repair expenses were important to participants.
Discussion
The purpose of this scoping review was to map and describe the evidence on out-of-pocket expenses incurred by older people with frailty, and their caregivers, to support aging in place. We categorized the types of expenses that have been studied and identified unique expenses that individuals may face. We found that people with dementia and caregivers were subgroups that were often explored in relation to out-of-pocket spending for aging in place. The body of literature had few studies that could be compared in terms of research design or outcome measures, so there is limited opportunity for further qualitative or quantitative systematic reviews.
Literature reporting on the out-of-pocket expenses associated with living in the community for people with frailty and their caregivers largely focused on support for the functional changes the person was experiencing, such as home care, housekeeping, transportation, and meal preparation. However, there were also various expenses identified that have not been regularly recognized in health and social care literature, such as dental care, yard maintenance, pet care, hair care, and legal services. Such services and supports contribute to the ability of people with frailty to maintain their safety and dignity as they experience health and functional changes. None of the included studies explicitly examined costs associated with maintaining meaningful leisure activities for people with frailty. Activities such as participating in social gatherings or maintaining hobbies may also be associated with out-of-pocket expenses, and are important for ensuring quality of life for people with frailty.83,84
The review revealed that the policy context was particularly important to the experiences of older adults with frailty and their caregivers with out-of-pocket expenses. While we sought to include policy documents in order to better understand how policies impacted out-of-pocket expenses, only two such documents were ultimately included. There were, however, notable differences between countries in how individuals experienced out-of-pocket expenses that were directly related to the policy context of the country. For example, there is an LTC insurance program in Japan that covers some costs for people with frailty in the community, reflecting the high proportion of older people in that country. There were also several studies conducted in the United States that referenced the public insurance programs (ie, Medicare and Medicaid), and this literature often reported on out-of-pocket expenses not covered by the programs.
Few studies used out-of-pocket expenses as outcomes in the evaluation of health care interventions to support older people with frailty. This was surprising as cost effectiveness is an important consideration in the implementation of such programs. This finding may reflect the focus on health care and societal costs in cost-effectiveness studies. The findings suggest that out-of-pocket spending is important to the experiences of many older people experiencing frailty and their caregivers. Individuals balance various types of costs and benefits when considering where to live. Developing a more robust understanding of out-of-pocket costs for aging in place will support the evolution of health and social care systems that are reflective of the population needs. In future intervention research, it will be important to include out-of-pocket expenses in cost analyses.
The review also revealed that there is no consistent measure of out-of-pocket expenses used in the literature on older people with frailty. While there were several measures of combined out-of-pocket expenses, there was very little overlap in these measures. A standardized approach to measurement would support comparisons across studies, populations, and interventions, as well as provide an opportunity for further systematic review and meta-analysis. The UN Sustainable Development Goals have an indicator related to out-of-pocket spending on health care as a proportion of total income.85 It may be useful to report out-of-pocket spending for older people with frailty in a similar manner. In this review, Veras and colleagues reported out-of-pocket expenses as a percentage of the family's monthly income,70 and Moon and colleagues reported yearly out-of-pocket spending by income.49 These may be important methods to consider for a standardized approach to reporting out-of-pocket expenses.
While we expected the review to identify many studies that included established definitions of frailty, this was not the case. We adopted a broad definition of frailty so we could incorporate evidence from diverse disciplinary and methodological perspectives, and could discuss how various definitions were used in literature reporting on out-of-pocket expenses. Of the included studies, two used an established operational definition of frailty; both Son and colleagues79 and Brandão and colleagues77 used the phenotype model.21 However, most studies that used the term “frail” to describe their population did not refer to a published definition of frailty. This review therefore further reinforces the need for clarification of the term “frailty” in the literature.
Conclusions
The literature demonstrates that out-of-pocket expenses are an important consideration for older people with frailty, and affect their ability to stay in their homes and communities. These expenses have implications for their health and well-being. While many sources noted out-of-pocket expenses related to home care, a variety of sources of expenses were ultimately noted, including those specific to health experiences (eg, medical supplies, medication), and those related to the particular living situation of individuals (eg, transportation, yard maintenance). The experience of out-of-pocket spending varied across countries. Caregivers of older people with frailty experience the effects of out-of-pocket expenses, and older people with dementia have unique needs impacting out-of-pocket expenses.
The review was limited by the inclusion of articles only written in English and French due to finite resources and an inability to translate literature. Limiting our search to sources published after 2001, when a seminal definition of frailty was published, may have unnecessarily limited our findings.
Implications for research
More research is needed on the contextual factors that impact the experiences of out-of-pocket costs for older people, notably the micro-, meso- and macro-level policy context. There is also a need for consensus around reliability, and consistently measuring out-of-pocket expenses so that there can be meaningful comparisons across research studies, populations, and contexts.
Implications for practice
This review supports the need for nurses and other health care providers to ask about out-of-pocket expenses when working with older people experiencing frailty. It is important for providers to be aware of the contextual factors that contribute to out-of-pocket spending, such as local policies, and also to stay abreast of resources to support people with frailty and their caregivers with out-of-pocket expenses.
Funding
We received financial support for this review from CIHR SPOR PIHCI Network Knowledge Synthesis Grant, the Government of Nova Scotia, Department of Health and Wellness, and School of Occupational Therapy, Dalhousie University. We are also grateful for support from the Aging, Community and Health Research Unit at McMaster University. The funders did not have any input into the review.
Appendix I: Search strategy
Searches run September 27, 2019
Appendix II: Data extraction instrument
Reviewer: _______________________________________________
Date: ___________________________________________________
Appendix III: Studies ineligible following full-text review
Reason for exclusion: Not a research study or policy document (n = 173)
Anon. Home care may lead to cost-efficient management of frail elderly patients. Dis Manag Advis. 2006;12(10):118–19.
Anon. One million older people face brunt of care with little support from health or social services. J Nurs Manag. 2002;10(1):57–8.
Armentano R, Kun L. Multidisciplinary, holistic and patient specific approach to follow up elderly adults. Health Technol (Berl). 2014;4(2):95–100.
Bauer JM, Sousa-Poza A. Impacts of informal caregiving on caregiver employment, health, and family. J Popul Ageing. 2015;8(3):113–45.
Bell H. In the comfort of home. Minn Med. 2013;96(1):24–9.
Bennett JA, Flaherty-Robb MK. Issues affecting the health of older citizens: meeting the challenge. Online J Issues Nurs. 2003;8(2):9.
Bibgy C. Ageing people with a lifelong disability: challenges for the aged care and disability sectors. J Intellect Dev Disabil. 2002;27(4):231–41.
Bjornsdottir K. From the state to the family: reconfiguring the responsibility for long-term nursing care at home. Nurs Inq. 2002;9(1):3–11.
Bloom S, Sulick B, Hansen JC. Picking up the PACE: the affordable care act can grow and expand a proven model of care. Generations. 2011;35(1):53–5.
Boling PA, Leff B. Comprehensive longitudinal health care in the home for high-cost beneficiaries: a critical strategy for population health management. J Am Geriatr Soc. 2014;62(10):1974–6.
Bossard M, Arbuz G. [Home care, a choice for the elderly and his family?] Soins Gerontol. 2003;(39):18–22. French.
Bottomley JM. Energy assistance programs; keeping older adults housed and warm. Top Geriatr Rehabil. 2001;17(1):71–81.
Branca S, Bennati E, Ferlito L, Spallina G, Cardillo E, Malaguarnera M, et al. The health-care in the extreme longevity. Arch Gerontol Geriatr. 2009;49(1):32–4.
Brennan M. Impairment of both vision and hearing among older adults: prevalence and impact on quality of life. Generations. 2003;27(1):52.
Brookman A, Kimbrel D. Families and elder care in the twenty-first century. Future Child. 2011;21(2):117–40.
Buntin MB, Huskamp H. What is known about the economics of end-of-life care for Medicare beneficiaries? Gerontologist. 2002;42:40–8.
Cagle JG, Munn JC. Long-distance caregiving: a systematic review of the literature. J Gerontol Soc Work. 2012;55(8):682–707.
Canadian Mortgage and Housing Corporation. A home for life: Edmonton initiative offers a blueprint for houses that work for every stage of life. Canada: CMHC, 2017.
Carey T, Kilkenny E, Shea DO, Lee H, Sinnott K. What price choice-cost of facilitating the preference of frail older people. Where should money be spent? Age Ageing. 2017;46:iii13.
Carpenter BD, Mak W. Caregiving couples. Generations. 2007;31(3):47–53.
Ceci C, Purkis ME. Means without ends: justifying supportive home care for frail older people in Canada, 1990–2010. Soc Health Illn. 2011;33(7):1066–80.
Cheek P, Nikpour L, Nowlin HD. Aging well with smart technology. Nurs Adm Q. 2005;29(4):329–38.
Chien-Wen T, Phillips RL, Green LA, Fryer GE, Dovey SM. What physicians need to know about seniors and limited prescription benefits, and why. Am Fam Physician. 2002;66(2):212.
Clegg A, Grout G, Buswell J, Lewis D, Barnes M, Naxarko L, et al. What has been your experience of the impact of the Community Care Act and reimbursement, and how can we ensure that it is applied in ways that meet patients’ needs? Nurs Older People. 2004;16(9):40–1.
Connolly S. Housing tenure and older people. Rev Clin Gerontol. 2012;22(4):286–92.
Conwell Y, Sirey JA, Snowden M. Aging services network providers: partners in mental health care for seniors. Am J Geriatr Psychiatry. 2010;18(3):S23–4.
Cook L, Wood A, Burns E. Care closer to home: an evidence-based approach for straitened times. Br J Hosp Med. 2018;79(10):546–7.
Counsell SR. Integrating medical and social services with GRACE. Generations. 2011;35(1):56–9.
Criddle RA, Flicker L. Helping older people to remain in their own homes. Med J Aust. 2001;174(6):266–7.
Cudennec T, Rogez E. [Caring for the caregivers, an essential key for home care]. Soins Gerontol. 2006;(59):13. French.
Currie CT. Health and social care of older people: could policy generalise good practice? J Intergr Care. 2010;18(6):19–26.
Dancy Jr J, Ralston PA. Health promotion and black elders: subgroup of greatest need. Res Aging. 2002;24(2):218–42.
Davis K, Willink A, Schoen C. Integrated care organizations: Medicare financing for care at home. Am J Manag Care. 2016;22(11):764–8.
Dawson WD, Nash M. Aging with serious mental illness: one state's response. Generations. 2018;42(3):63–70.
De Jonge E, Taler G. Is there a doctor in the house? Caring. 2002;21(8):26–9.
Dilks S, Emblin K, Nash, Jefferies S. Pharmacy at home: Service for frail older patients demonstrates medicines risk reduction and admission avoidance. Clinical Pharmacist. 2016;8(7):2016.
Dix J. Paying for care – the Japanese model. Work Older People. 2005;9(1):24–6.
Dolan TA. Access to care for older Americans. N Y State Dent J. 2010;76(5):34–7.
Doling J, Ronald R. Meeting the income needs of older people in East Asia: using housing equity. Ageing Soc. 2012;32(3):471–90.
Droz JP. Rules allowing the reimbursement of cares of elderly cancer patients in France. Crit Rev Oncog. 2003;48(2):145–9.
Dyer CB, Pickens S, Burnett J. Vulnerable elders: when it is no longer safe to live alone. J Am Med Assoc. 2007;298(12):1448–50.
Ebrahim S. New beginning for care for elderly people? Proposals for intermediate care are reinventing workhouse wards. BMJ. 2001;323(7308):337–9.
Economist, The. Till death do us part: a new market for floating hotels [internet]. The Economist. 2004 Oct 30 [cited 2021 Oct 5]. Available from: https://www.economist.com/business/2004/10/28/till-death-us-do-part.
Edwards-Tate L. Clearing up misconceptions and imperceptions of privately paid home care. Caring. 2011;30(4):36–9.
Elon RD. Reforming the care of our elders: reflections on the role of reimbursement. J Am Med Dir Assoc. 2003;4(2):117–20.
Evans M. Home-care demands rise: medicaid key to helping seniors remain in abodes. Mod Healthc. 2006;36(28):17.
Fange AM, Oswald F, Clemson L. Aging in place in late life: theory, methodology and intervention. J Ageing Res. 2012;2012:547562.
Farag I, Sherrington C, Ferreira M, Howard K. A systematic review of the unit costs of allied health and community services used by older people in Australia. BMC Health Serv Res. 2013;13(69).
Fazzi R, Harlow L. The incredible future of home care and hospice. Caring. 2007;26(3):36–45.
Feikema M. Housing and social care for the elderly in central Europe. Czech Sociol Rev. 2014;50(6):1012–14.
Firman J, Nathan S, Alwin R. Meeting the needs of economically disadvantaged older adults: a holistic approach to economic casework. Generations. 2009;33(3):74–80.
Fortinsky RH, Robinson JT. Targeting function at home in older adults: how to promote and disseminate promising models of care? J Am Geriatr Soc. 2018;66(3):433–5.
Francis SA, Barnett N, Denham M. Switching of prescription drugs to over-the-counter status. Is it a good thing for the elderly? Drugs Aging. 2005;22(5):361–70.
Gable M. Communication helps seniors age in place. Teamwork is vital in keeping satisfaction high, cost low. Health Prog. 2009;90(6):29–31.
Garfinkel D. Overview of current and future research and clinical directions for drug discontinuation: psychological, traditional and professional obstacles to deprescribing. Eur J Hosp Pharm. 2017;24(1):16–20.
Garrett SL, O’Brien JG, Miles TP. Letter to the editor: Quality of care for vulnerable older patients. Ann Intern Med. 2006;144(3):219–20.
Giarchi GG. Older people ‘on the edge’ in the countrysides of Europe. Soc Policy Adm. 2006;40(6):705–21.
Giovannoli L. Home care: changes and concerns. Caring. 2006;31(8):30–3.
Gitlin LN. Conducting research on home environments: lessons learned and new directions. Gerontologist. 2003;43(5):628–37.
Gitlin LN, Szanton SL, Hodgson NA. It's complicated-but doable: the right supports can enable elders with complex conditions to successfully age in community. Generations. 2013;37(4):51–61.
Golden AG, Tewary S, Dang S, Roos BA. Care management's challenges and opportunities to reduce the rapid rehospitalization of frail community-dwelling older adults. Gerontologist. 2010;50(4):451–8.
Gonyea JG, Melekis K. Women's housing challenges in later life: the importance of a gender lens. Generations. 2017;41(4):45–53.
Gonzalez L. A focus on the Program of the All-Inclusive Care for the Elderly (PACE). J Aging Soc Policy. 2017;29(5):475–90.
Goodacre K, McCreadie C, Flanagan S, Lansley P. Enabling older people to stay at home: the costs of substituting and supplementing care with assistive technology. Br J Occup Ther. 2008;71(4):130–40.
Gottlieb AS, Caro FG. Extending the effectiveness of home care for elders through low-cost assistive equipment. Policy Brief (Cent Home Care Policy Res). 2001;(6):1–6.
Grundy E. Ageing and vulnerable elderly people: European perspectives. Ageing Soc. 2006;26:105–34.
Guillard G. The elderly person at home and his relation to money. Soins Gerontol. 2003;(39):37–9.
Haas LB. Caring for community-dwelling older adults with diabetes: perspectives from health care providers and caregivers. Diabetes Spectr. 2006;19(4):240–4.
Haggis C, Sims-Gould J, Winters M, Mckay H. I’d rather stay: documentary video for multi-stakeholder discussions on the barriers and facilitators to growing old in your neighborhood [internet]. Canadian Association on Gerontology; 2014 [cited 2021 Oct 5]. Available from https://cagacg.ca/wp-content/uploads/2014/11/CAG2014_Program.pdf.
Halamandaris VJ. Aging with health and dignity. Caring. 2004;23(10):6–27.
Halamandaris VJ. Doing the right thing for our nation's elderly, infirm, and disabled. Caring. 2011;30(4):48.
Hallberg IR, Kristensson J. Preventive home care of frail older people: a review of recent case management studies. J Clin Nurs. 2004;13(6B):112–20.
Hansen JC. Community and in-home models. Am J Nurs. 2008;108(9 Suppl):69–72.
Henderson EJ, Caplan GA. Home sweet home? Community care for older people in Australia. J Am Med Dir Assoc. 2008;9(2):88–94.
Hebert R. Home care: from adequate funding to integration of services. Healthc Pap. 2009;10(1):58–83.
Hernandez M. Assisted living in all of its guises. Generations. 2005;29(4):16–23.
Heumann LF. Assisted living for lower-income and frail older persons from the housing and built environment perspective. J Hous Elderly. 2004;18(3/4):165–78.
Hood FJ. Medicare's home health prospective payment system. South Med J. 2001;94(10):986–9.
Hostetter M, Klein S, McCarthy D. Aging gracefully: the PACE approach to caring for frail elders in the community. New York, NY: Common Wealth Fund, 2016. 12 p.
Hurley D. Accurately attributing reduced hospital admissions to medications optimisation? Pharmacoepidemiol Drug Saf. 2018;27:8.
Iverson RJ. The silent crisis: women and the need for long-term care insurance. Part 2. Caring. 2003;22(11):32–6.
Jaber R, Starr R. “Please help me” – a caregiver's stress. J Am Geratr Soc. 2015;63:S28.
Johnson RW. Housing costs and financial challenges for low-income older adults. Washington, DC; Urban Institute, 2015. p. 16.
Johnson RW, Mommaerts C. Will health care costs bankrupt aging boomers? Washington, DC; Urban Institute, 2010. p. 46.
Kane RL, Kane RA. HCBS: the next thirty years. Generations. 2012;36(1):131–4.
Kang J-M, Yeo BK, Cho S-J, Cho S-E, Yun S, Kim J, et al. Healthcare-seeking behaviors of patients with in Incheon City: a preliminary study. Intr Psychogeriatr. 2015;27:S81–5.
Keefe J, Glendinning C, Fancey P. Financial payments for family carers: policy approaches and debates. In: Martin-Matthews A, Phillips JE, editors. Aging and caring at the intersection of work and home life: blurring the boundaries. New York: Taylor and Francis Group; 2008. p. 185–206.
Keister D, Shvetzoff S. Allowing the elderly to age in place. In Portland, OR, a Catholic-sponsored PACE site provides community-based health care services. Health Prog. 2004;85(6):50–3.
Kim EHW, Cook, PJ. The continuing importance of children in relieving elder poverty: evidence from Korea. Ageing Soc. 2011;31(6):953–76.
Kim KI, Gollamudi SS, Steinhubl S. Digital technology to enable aging in place. Exp Gerontol. 2017;88:25–31.
Kinosian B, Edes T. Home based primary care for frail, homebound veterans as a model for independence at home. J Am Geriatr Soc. 2010;58:S116.
Kinosian B, Edes T, Davis D, Makineni R, Intrator O. Independence at home (IAH) criteria successfully targets frail, costly veterans. J Am Geriatr Soc. 2015;63:S128.
Kinosian B, Meyer S, Yudin J, Danish A, Touzel S. Elder partnership for all-inclusive care (Elder-PAC): 5-year follow-up of integrating care for frail, community elders, linking home based primary care with an area agency on aging (AAA) as an independence at home (IAH) model. J Am Geriatr Soc. 2010;58:S6.
Knijn T, Verhagen S. Contested professionalism: payments for care and the quality of home care. Adm Soc. 2007;39(4):451–75.
La Martina D. Aging in place home renovations: are they worth the costs? [internet]. 2015 [cited 2021 Sep 15]. Available from: https://www.thinkadvisor.com/2015/05/04/aging-in-place-are-home-renovations-worth-the-costs/.
Lamorthe C. How much does it cost to keep a dependent person at home? Soins Gerontol. 2004;(46):5–7.
LaPorte M. Quality, funding issues hit home care. Provider. 2009;35(8):22–32.
Lecovich E, Doron I. Migrant workers in eldercare in Israel: social and legal aspects. Eur J Soc Work. 2012;15(1):29–44.
Leng Leng T, Wei-Jun, JY. Introduction of special issues of journal of cross cultural gerontology on elder-care issues in Southeast and East Asia. J Cross Cult Gerontol. 2018;33(2):137–42.
Libson N. The sad state of affordable housing for older people. Generations. 2005. 29(4):9–15.
Limpawattana P, Chindaprasirt J. Caregiver burden of older adults: a southeast Asia aspect. In: Thurgood A and Schuldt K, editors. Caregivers: challenges, practices and cultural influences. New York, Nova Science Publishers, Inc. 2020. p.195–206.
Lloyd-Sherlock P. Identifying vulnerable older people: insights from Thailand. Ageing Soc. 2006;26:81–103.
Lyn MJ, Johnson FS. Just for us: in-home care for frail elderly and disabled individuals with low incomes. N C Med J. 2011;72(3):205–6.
Mahoney KJ, Simon-Rusinowitz L, Simone K, Zgoda K. Cash and counseling: a promising option for consumer direction of home- and community-based services and supports. Care Manag J. 2006;7(4):199–204.
Marrelli TM. Prospective payment in home care: an overview. Geriatr Nurs. 2001;22(4):217–8.
Mason A, Weatherly H, Spilsbury K, Golder S, Arksey H, Adamson J, et al. The effectiveness and cost-effectiveness of respite for caregivers of frail older people. J Am Geriatr Soc. 2007;55(2):290–9.
Mason DJ. Long-term care: investing in models that work. JAMA. 2017;318(16):1529–30.
Masotti P, Fick R, Johnson-Masotti A, MacLeod S. The aging population and natural occurring retirement communities (NORCs); local government, healthy aging, and healthy-NORCs. Alaska Med. 2007;42(2):85–8.
Maxwell C, Rothman R, Simmons S, Wolever R, Given B, Miller R, et al. Development of a frailty-focused communication aid for older adults. Palliat Med. 2018;32(1):155.
McCann P. Explaining about…building to last. Work Older People. 2008;12(2):9–11.
McGuire LC, Anderson LA, Talley RC, Crews JE. Supportive care needs of Americans: a major issue for women as both recipients and providers. J Womens Health (Larchmt). 2007;6:784–9.
Mechkat C, Bouldin B. What sort of architecture should there be for a society weakened by old-age? or older people's spaciality between medico-social establishments and living space for all. Gerontol Soc. 2006;119(4):39–73.
Meucci MR. Home modifications: access, funding and effectiveness. National Institute of Health; 2014.
Meyer MH, Roseamelia C. Emerging issues for older couples: protecting income and assets, right to intimacy, and end-of-life decisions. Generations. 2007;31(3):66–71.
Michel J-P, Robine J-M, Herrmann F. Tomorow, who will take care of the elderly? The oldest old support ratio. Bull Acad Natl Med. 2010;194:793–804.
Ming-Sheng W, Chi-Fang W, Wang MS, Wu CF. Assisting caregivers with frail elderly in alleviating financial hardships. Soc Work Public Health. 2018;33(6):396–406.
Miskelly FG. Assistive technology in elderly care. Age Ageing. 2001;30(6):455–8.
Mithers C. How to plan for your parent's future. Ladies Home J. 2008;25(11):62–6.
Mohammad TS. The elderly and family change in Asia with a focus in Iran: a sociological assessment. J Comp Fam Stud. 2006;37(4):583-XI,610.
Montgomery RJV, Rowe JM, Kosloski K. Chapter 16: Family caregiving. In: Blackburn JA, Dulmus CN, editors. Handbook of gerontology: evidenced-based approaches to theory, practice and policy. Hobeken, NJ:John Wiley and Sons Inc, 2007. p. 426–54.
Moore DJ, Appleby J, Meyer J, Myatt J, Oliver D, Ritchie-Campbell J. Frail older people improve their care. Pave the way for better elderly care. Health Serv J. 2014;124(6400):26–9.
Moraitou M, Pateli A, Fotiou S. Smart health caring home: a systematic review of smart home care for elders and chronic disease patients. Adv Exp Med Biol. 2017;989:255–64.
Nelson A, Powell-Cope G, Gavin-Dreschnack D, Quigley P, Bulat T, Baptiste AS, et al. Technology to promote safe mobility in the elderly. Nurs Clin North Am. 2004;39(3):649–71.
Nishita CM, Pynoos J. Retrofitting homes and buildings: improving sites for long-term-care delivery. Generations. 2005;29(4):52–7.
Norlander L. The future of advance care planning. Home Health Care Manag Pract. 2003;15(2):136–9.
Northridge ME, Levick N. Preventing falls at home: transforming unsafe spaces into healthy places for older people. Generations. 2003;26(4):42–7.
Ohwa M, Chen LM. Balancing long-term care in Japan. J Gerontol Soc Work. 2012;55(7):659–72.
O’Toole RE. Integrating contributory elder-care benefits with voluntary long-term care insurance programs. Empl Benefits J. 2002;27(4):13–6.
Overend L, Gawith J, Carruthers L. ‘Expensive’ ultra-long acting insulin: is it cost effective in elderly patients with brittle diabetes? Diabet Med. 2016;33:187–8.
Pan CX, Chai E, Farber J. Myths of the high medical cost of old age and dying. Int J Health Serv. 2008;38(2):253–75.
Papaioannou ESC, Raiha I, Kivela SL. Self-neglect of the elderly. An overview. Eur J Gen Pract. 2012;18(3):187–90.
Parikh RB, Montgomery A, Lynn J. The Older Americans Act at 50 – community-based care in a value-driven era. N Engl J Med. 2015;373(5):399–401.
Park K-S. Consecrating or desecrating filial piety?: Korean elder care and the politics of family support. Dev Soc. 2013;42(2):287–308.
Pedlar D, Lockhart W, Macintosh S. Canada's veterans independence program: a pioneer of “aging at home”. Healthc Pap. 2009;10(1):72–7.
Petter Askheim O. Developments in Direct Payments. Ageing Soc. 2007;27:167–9.
Pierce CA. Home health care. Program of all-inclusive care for the elderly in 2002. Geriatr Nurs. 2002;23(3):173–4.
Pochagina O. The aging of the population in the PRC: sociocultural and sociopsychological aspects. Far East Aff. 2003;31(2):79–95.
Podgorski C, King DA. Losing function, staying connected: family dynamics in provision of care for people with dementia. Generations. 2009;33(1):24–9.
Ponte C. [Nurses, patients and families. 6/8 – dependency and physical, financial and material aides]. Soins Gerontol. 2009;(77):43–4. French.
Poskute V, Greve B. Long-term care in Denmark and Lithuania – a most dissimilar case. Soc Policy Adm. 2017;51(4):659–75.
Potter JF. Aging in America: essential considerations in shaping senior care policy. Aging Health. 2010;6(3):289–99.
Pynoos J, Christy M. The cost and financing of home modifications in the United States. J Disabil Policy Stud. 2003;14(2):68–73.
Pynoos J, Steinman BA, Do Nguyen AQ, Bressette M. Assessing and adapting the home environment to reduce falls and meet the changing capacity of older adults. J Hous Elderly. 2012;26(1–3):137–55.
Rappe E, Rajaniemi J, Topo P. Dementia friendly housing-actors and affordances. Paper presented at: The 24th Nordic Congress of Gerontology 2–4 May, 2018; Oslo, Norway.
Robben SHM, Perry M, Olde R, Marcel GM, Heinen MM, Melis RJF. Care-related goals of community-dwelling frail older adults. J Am Geriatr Soc. 2011;59(8):1552–4.
Robinson H. A guide for making housing decisions: housing options for older adults. Washington, DC: National Association of Area Agencies on Aging; n.d. p. 28.
Rodwin VG, Gusmano MK. Growing older in world cities. New York, London, Paris and Tokyo. Vanderbilt University Press; 2006. p. 376–89.
Schulz R, Martire LM. Family caregiving of persons with dementia: prevalence, health effects, and support strategies. Am J Geriatr Psychiatry. 2004;12(3):240–9.
Schwarz B. Assisted living: sobering realities. New York, NY: Haworth Press Inc; 2001. p. 148.
Serpa MJ, Duque S, Velho S, Braco Forte C, Barrona J, Sequeira M, et al. Impact of social determinants in oral health in older patients admitted in a medical ward of a general hospital. Eur Geriatr Med. 2015;6:S30–1.
Shaw C, McNamara R, Abrams K, Cannings-John R, Hood K, Longo M, et al. Systematic review of respite care in the frail elderly. Health Technol Assess. 2009;13(37):1–246.
Siddiqi SN, Zdenek RO, Gorman EJ. Age-friendly banking: policy, products, and services for financial capability. In: Morrow-Howell N, Sherraden M, editors. Financial capability and asset holding in later life: a life course perspective. Oxford University Press; 2015. p. 195–217.
Skinner K. Nursing interventions to assist in decreasing stress in caregivers of Alzheimer's patients. ABNF J. 2009;20(1):22–4.
Sloan JP. Joining up care around the individual – lessons from Vancouver. J Integr Care. 2014;22(2):32–8.
Spalding K, Watkins J, Williams AP. Self-managed care programs in Canada: a report to Health Canada. Canada: Health Canada, 2006. p. 66.
Spiers P. Supporting older people: care needs and care fees. Br J Community Nurs. 2006;11(2):56–8.
Street D. Women, pension, income, and the cost of caring. Association Paper, Southern Sociological Society (SSS). 2001.
Stone RI. The aging services system – when it's 64. Generations. 2014;38(2):101–6.
Swartz K. Sharing the financial responsibility of caring for patients. JAMA. 2011;306(7):760–1.
Travis SS, Hsueh-Fen SK, Acton GJ. Helping family members manage medication administration hassles. J Psychosoc Nurs Ment Health Serv. 2005;43(11):13–5.
Treadwell HM, Northridge ME. Oral health is the measure of a just society. J Health Care Poor Underserved. 2007;18(1):12–20.
Vara MJ. Long-term care for elder women in Spain: advances and limitations. J Aging Soc Policy. 2014;26(4):347–69.
Vass A. Elderly patients to receive cash to speed up hospital discharge. BMJ. 2002;325(7357):179.
Vladeck F. The next generation of senior services: responding to health reform. Care Manag J. 2012;13(1):37–41.
Warner M, Cohen D. Elderly people's services. Home truths. Health Serv J. 2004;114(5930):28–9.
Washio M, Arai Y, Yamasaki R, Ide S, Kuwahara Y, Tokunaga S, et al. Long-term care insurance, caregivers’ depression and risk of institutionalization/hospitalization of the frail elderly. IMJ. 2005;12(2):99–103.
Wellman NS, Kamp B. Federal food and nutrition assistance programs for older people. Generations. 2004;28(3):78–85.
White A. Care in old age. Br J Community Nurs. 2017;22(1):690.
White C. State funding of elderly care in England has fallen by 40% in five years. BMJ. 2015;350:h3253.
Williams AP, Lum JM, Deber R, Montgomery R, Kuluski K, Peckham A, et al. Aging at home: integrating community-based care for older persons. Healthc Pap. 2009;10(1):8–21.
Wynia K, Spoorenberg SLW, Uittenbroek RJ, Jager M, Kremer HPH, Reijneveld SA. Long-term advantages of person-centred and integrated care: results from a longitudinal study on Embrace. Int J Integr Care. 2018;18:1–2.
Yaggy SD, Michener JL, Yaggy D, Champagne MT, Silberberg M, Lyn M, et al. Just for us: an academic medical center-community partnership to maintain the health of a frail low-income senior population. Gerontologist. 2006;46(2):271–6.
Yarkony L. Abolishing the companionship exemption: good intentions but harmful results. Caring. 2013;32(7):4–7.
Reason for exclusion: Did not report costs incurred by frail older people or their caregivers (n = 139)
Adekpedjou R, Stacey D, Briere N, Freitas A, Garvelink MM, Turcotte S, et al. “Please listen to me”: a cross-sectional study of experiences of seniors and their caregivers making housing decisions. PLoS One. 2018;13(8):e0202975.
Aggar C, Ronaldson S, Cameron ID. Reactions to caregiving during an intervention targeting frailty in community living older people. BMC Geriatr. 2012;12:66.
Aggar C, Ronaldson S, Cameron I. Reactions to caregiving in frailty research. Arch Gerontol Geriatr. 2011;53(2):e138-e143.
Aggar C, Ronaldson S, Cameron ID. Residential respite care is associated with family carers experiencing financial strain. Australas J Ageing. 2014;33(2):93–8.
Alders P, Schut FT. Trends in ageing and ageing-in-place and future market for institutional care: scenarios and policy implications. Health Econ Policy Law. 2018:1–18.
Al-Janabi H, Coast J, Flynn TN. What do people value when they provide unpaid care for an older person? A meta-ethnography with interview follow-up. Soc Sci Med. 2008;67(1):111–21.
Alkema GE, Enguidanos SM, Wilber KH, Trufasiu M, Simmons WJ, Frey D. The role of consultant pharmacists in reducing medication problems among older adults receiving medicaid waiver services. Consult Pharm. 2009;24(2):121–33.
Ament BHL, de Vugt ME, Koomen FMK, Jansen MWJ, Verhey FRJ, Kempen GIJM. Resources as a protective factor for negative outcomes of frailty in elderly people. Gerontology. 2012;58(5):391–7.
Anguelov N, Frank A. The effects of housing costs on nursing home diversion. J Soc Serv Res. 2020;46(1):133–47.
Aronson J. Elderly people's accounts of home care rationing: missing voices in long-term care policy debates. Ageing Soc. 2002;22(pt 4):399–418.
Avila-Funes JA, Paniagua-Santos DL, Escobar-Rivera V, Navarrete-Reyes AP, Aguilar-Navarro S, Amieva H. Association between employee benefits and frailty in community-dwelling older adults. Geriatr Gerontol Int. 2016;16(5):606–11.
Barlow J, Singh D, Bayer S, Curry R. A systematic review of the benefits of home telecare for frail elderly people and those with long-term conditions. J Telemed Telecare. 2007;(4):172–9.
Boehlen FH, Herzog W, Schellberg D, Maatouk I, Saum KU, Brenner H, et al. Self-perceived coping resources of middle-aged and older adults – results of a large population-based study. Aging Ment Health. 2017;21(12):1303–9.
Bots-VantSpijker PC, Bruers JJ, Bots CP, Vanobbergen JN, De Visschere LM, de Baat C, et al. Opinions of dentists on the barriers in providing oral health to community-dwelling frail older people: a questionnaire survey. Gerodontology. 2016;33(2):268–74.
Buhr GT, Kuchibhatla M, Clipp EC. Caregivers’ reasons for nursing home placement: clues for improving discussions with families prior to the transition. Gerontologist. 2006;46(1):52–61.
Butler A, Gallagher D, Gillespie P, Crosby L, Ryan D, Lacey L, et al. Frailty: a costly phenomenon in caring for elders with cognitive impairment. Int J Geriatr Psychiatry. 2016;31(2):161–8.
Casado BL, van Vulpen KS, Davis SL. Unmet needs for home and community-based services among frail older Americans and their caregivers. J Aging Health. 2011;23(3):529–53.
Challis D, Hughes J. Frail old people at the margins of care: some recent research findings. Br J Psychiarty. 2002;180:126–30.
Chapman SA, Keating N, Eales J. Client-centred, community-based care for frail seniors. Health Soc Care Community. 2003;11(3):25361.
Clarkson P, Hughes J, Challis D. The potential impact of changes in public funding for residential and nursing-home care in the United Kingdom: the residential allowance. Ageing Soc. 2005;25(2):159–80.
Couturier P. [Activity monitoring in the medical management of frail elderly people]. Gerontol Soc. 2005;113(2):13–23. French.
Covinsky KE, Eng C, Lui LY, Sands LP, Sehgal AR, Walter LC, et al. Reduced employment in caregivers of frail elders: impact of ethnicity, patient clinic characteristics, and caregiver characteristics. J Gerontol A Biol Sci Med Sci. 2001;56(11):M707–13.
Cucinotta D, Savorani G, Piscaglia F, Galletti L, Petazzoni E, Bolondi L. The chronically ill elderly patients discharged from the hospital: interim report from a controlled study of home care attendance. Arch Gerontol Geriatr. 2004;38(Suppl):103–8.
Davey JA. Older people and transport: coping without a car. Ageing Soc. 2007;27:49–65.
Davey A, Savla J, Sundstrom G, Zarit SH, Malmberg BO. How equitable is Sweden's changing care-mis? Linking individual and regional characteristics over time. Ageing Soc. 2007;27:511–32.
Dembe AE, Partridge JS, Dugan E, Piktialis DS. Employees’ satisfaction with employer-sponsored elder-care programs. Int J Workplace Health Manag. 2011;4(3):216–27.
Doherty JB, DeWeaver KL. Critical incidents in the lives of elders with a disability: factors leading to institutional placement. J Gerontol Soc Work. 2002;38(4):39–51.
Drummond SL. Supporting Canadian caregivers current and future policy directions. Masters Abstr Int. 2010;AAIMR85482.
Chapin R, Dobbs-Kepper D. Aging in place in assisted living: philosophy versus policy. Gerontologist. 2001;41(1):43–50.
Borg C, Hallberg IR, Blomqvist K. Life satisfaction among older people (65+) with reduced self-care capacity: the relationship to social, health and financial aspects. J Clin Nurs. 2006;15(5):607–18.
Dubois M, Dubuc N, Caron CD, Raiche M, Hebert R. Is there agreement between Canadian older adults and their primary informal caregivers on behaviour towards institutionalisation? Health Soc Care Community. 2009;17(6):610–8.
Edes T, Kinosian B, Vuckovic NH, Nichols LO, Becker MM, Hossain M. Better access, quality and cost for clinically complex veterans with home-based primary care. J Am Geriatr Soc. 2014;62(10):1954–61.
Eloniemi-Sulkava U, Saarenheimo M, Laakkonen M-L, Pietila M, Kautiainen H, Tilvis RS, et al. Family care as collaboration: effectiveness of a multicomponent support program for elderly couples with dementia. Randomized controlled intervention study. J Am Geriatri Soc. 2009;57(12):2200–8.
Fabris F, Moaschi M, Aimonino N, Ponzetto M, Maero B, Tibaldi V, et al. Home care for demented subjects: new models of care and home-care allowance. Arch Geront Geriatr. 2004;38:155–62.
Fernandez-Carro C. Ageing at home, co-residence or institutionalisation? Preferred care and residential arrangements of older adult in Spain. Ageing Soc. 2016;36(3):586–612.
Fersch B. Expectations towards home care re-ablement in Danish municipalities. Int J Sociol Soc Policy. 2015;35(3/4):126–40.
Fisher HM, Raphael TG. Managed long-term care: care integration through care coordination. J Aging Health. 2003;15(1):223–45.
French DJ, Sargent-Cox K, Luszcz MA. Correlates of subjective health across the aging lifespan: understanding self-rated health in the oldest old. J Aging Health. 2012;24(8):1449–69.
Frick KD, Scanlon DP, Bandeen-Roche K, Kasper JD, Simonsick EM, Sullivan EM. Influenza vaccination by race among disabled community dwelling older women. J Health Care Poor Underserved. 2004;15(2):220–36.
Garceau M, Vincent C, Robichaud L. Research note: telesurveillance as a tool supporting the social participation of the elderly at home. Can J Aging. 2007;26(1):59–72.
Gianopoulos C, Bolda E, Baldwin M, Olsen L. What works? Maine's statewide uniform assessment and home care planning system tells all. Gerontologist. 2001;41(3):309–11.
Grioux D, Tetreault S, Langlois L. Evaluation del’aptitude d’une personne agee atteinte de deficts cognitifs a ferer sa personne et ses biens: identification des outils disponibles. Can J Aging. 2013;32(4):375–91.
Giroux D, Tetreault S, Langlois L. Assessment of the ability of an elderly person with cognitive deficits to manage their person and their property: Identification of available tools. Can J Aging. 2013;32(4):375–91. French.
Goodacre K, McCreadie C, Flanagan S, Lansley P. Enabling older people to stay at home: how adaptable are existing properties? Br J Occup Ther. 2007;70(1):5–15.
Graham CL, Ivey SL, Neuhasser L. From hospital to home: assessing the transitional care needs of vulnerable seniors. Gerontologist. 2009;49(1):23–33.
Graybill EM, McMeekin P, Wildman J. Can aging in place be cost effective? A systematic review. PLoS One. 2014;9(7):e102705.
Greenfield JC. The long-term costs of caring: how caring for an aging parent impacts wealth trajectories of caregivers. Diss Abstr Int. 2014;74:8-A(E).
Grimmer K, Kay D, Foot J, Pastakia K. Consumer views about aging-in-place. Clin Interv Aging. 2015;10:1803–11.
Gulbrandsen L, Langsether A. Family transactions in the Norwegian housing market. Hous Theory Soc. 2003:20(3):137–52.
Guralnik JM, Alecxih L, Branch LG, Wiener JM. Medical and long-term care costs when older persons become more dependent. Am J Public Health. 2002;92(8):1244–5.
Gussekloo J, Poot A, Achterberg WP, Maas H. Independent living with multimorbidity? Your GP is ready for it! Eur Geriatr Med. 2014;5:S40.
Habermann S, Cooper C, Katona C, Linvingston G. Predictors of entering 24-h care for people Alzheimer's disease: results from the LASER-AD study. Int J Geriatr Psychiatry. 2009;24(11):1291–8.
Hebert R, Dubuc N, Buteau M, Desrosiers J, Bravo G, Trottier L, et al. Resources and costs associated with disabilities of elderly people living at home and in institutions. Can J Aging. 2001;20(1):1–21.
Hoeck S, Francois G, Geerts J, Van der Heyden J, Vandewoude M, Van Hal G. Health-care and home-care utilization among frail elderly persons in Belgium. Eur J Public Health. 2012;22(5):671–7.
Huffman AK, Jackson HE. Retiree out-of-pocket healthcare spending: a study of consumer expectations and policy implications. Am J Law Med. 2013;39:62–133.
Jenkyn KB, Hoch JS, Speechley M. How much are we willing to pay to prevent a fall? Cost-effectiveness of a multifactorial falls prevention program for community-dwelling older adults. Can J Aging. 2012;31(2):121–37.
Johannesen A, Petersen J, Avlund K. Satisfaction in everyday life for frail 85-year old adults: a Danish population study. Scand J Occup Ther. 2004;11(1):3–11.
Keijer U, Molin G, Sandstrom G. Old people living at home with acquired cognitive impairment supported by assistive technology. Cost-benefit studies. Assist technol Res Ser. 2007;20:233–7.
Kietzman KG, Wallace SP, Durazo EM, Torres JM, Choi AS, Benjamin AE, et al. A portrait of older Californians with disabilities who rely on public services to remain independent. Home Health Care Serv Q. 2012;31(4):317–36.
Kita M, Ito K. The caregiving process of the family unit caring for a frail older family member at home: a grounded theory study. Int J Older People Nurs. 2013;8(2):149–58.
Klesges LM, Pahor M, Shorr RI, Wan JY, Williamson JD, Guralnik JM. Financial difficulty in acquiring food among elderly disabled women: results from the Women's Health and Aging Study. Am J Public Health. 2001;91(1):68–75.
Kronborg C, Vass M, Lauridsen J, Avlund K. Cost effectiveness of preventive home visits to the elderly: economic evaluation alongside randomized controlled study. Eur J Health Econ. 2006;7(4):238–46.
Kyongweon L, Raiz L. The home-delivered meals program: a promising intervention for suburban older adults living alone. Care Manag J. 2015;16(4):195–202.
Langa KM, Chernew ME, Kabeto MU, Herzog AR, Ofstedal MB, Willis RJ, et al. National estimates of the quantity and cost of informal caregiving for the elderly with dementia. J Gen Intern Med. 2001;16(11):770–8.
Langa KM, Fultz NH, Saint S, Kabeto MU, Regula HA. Informal caregiving time and costs for urinary incontinence in older individuals in the United States. J Am Geriatr Soc. 2002;50(4):733–7.
Langa KM, Vijan S, Hayward RA, Chernew ME, Blaum CS, Kabeto MU, et al. Informal caregiving for diabetes and diabetic complications among elderly Americans. J Gerontol B Psychol Sci Soc Sci. 2002;57(3):S177–86.
Lapierre TA, Keating N. Characteristics and contributions of non-kin carers of older people: a closer look at friends and neighbours. Ageing Soc. 2013;33(8):1442–68.
Lecovich E. Caregiving burden, community services and quality of life of primary caregivers of frail elderly persons. J Appl Gerontol. 2008;27(3):309–30.
Lee JC, Hasnain-Wynia R, Lau DT. Delay in seeing a doctor due to cost: disparity between older adults with and without disabilities in the United States. Health Serv Res. 2012;47(2):698–720.
Lewin GF, Alfonso HS, Alan JJ. Evidence for the long term cost effectiveness of home care reablement programs. Clin Interv Aging. 2013;8:1273–81.
Li Y. Private long-term care insurance and patterns of care use among older adults. Diss Abstr Int. 2008;68(9-A):3985.
Lin C-S. Telecare projects in Taiwan. Gerontechnology. 2010;9(3):400–7.
Lin S-H. Community-dwelling older adults: services, cost, and changes. Diss Abstr Int. 2016;77:4-B(E).
Kehusmaa S, Autti-Ramo I, Helenius H, Rissanen P. Does informal care reduce public care expenditure on elderly care? Estimates based on Finland's Age Study. BMC Health Serv Res. 2013;13:317.
Litwin H, Sapir EV. Perceived income adequacy among older adults in 12 countries: findings from the survey of health, ageing, and retirement in Europe. Gerontologist. 2009;49(3):397–406.
Liu LJ, Fu YF, Qu L, Wang Y. Home health care needs and willingness to pay for home health care among the empty-nest elderly in Shanghai, China. Int J Gerontol. 2014;8(1):31–6.
Mackenzie R, Sakel M. Teleneurology: ethics of devolving responsibilities from clinicians to families and/or carers. Br J Neurosci Nurs. 2011;7(2):490–3.
Magnusson L, Hanson E. Supporting frail older people and their family carers at home using information and communication technology: cost analysis. J Adv Nurs. 2005;51(6):645–57.
Mann WC, Belchior P, Tomita MR, Kemp BJ. Barriers to the use of traditional telephones by older adults with chronic health conditions. OTJR (Thorofare N J). 2005;25(4):160–6.
Maqsood F, Flatt JD, Albert SM, Maqsood S, Nizamuddin M. Correlates of self-reported depressive symptoms: a study of older persons of Punjab, Pakistan. J Cross Cult Gerontol. 2013;28(1):65–74.
Markle-Reid M. Frail elderly home care clients: the effects and expense of adding nursing health promotion and preventive care to personal support services [PhD]. Ontario, Canada: McMaster University, 2003.
Markle-Reid M, Brown G, Weir R, Gafni A, Roberts J, Henderson SR. The effectiveness and efficiency of home-based nursing health promotion for older people: a review of the literature. Med Care Res Rev. 2006;63(5):531–69.
Markle-Reid M, Weir R, Browne G, Roberts J, Gafni A, Henderson S. Health promotion for frail older home care clients. J Advan Nurs. 2006;54(3):381–95.
Marshall A, Nazroo J, Tampubolon G, Vanhoutte B. Cohort differences in the levels and trajectories of frailty among older people in England. J Epidemiol Community Health. 2015;69(4):316–21.
Matsubayashi K, Wada T, Ishine M, Sakamoto R, Okumiya K, Ishikawa M, et al. Community-based geriatric assessment and preventive intervention lowered medical expenses for the elderly. J Am Geriatr Soc. 2013;58(4):791–3.
Mattke S, Klautzer L, Mengistu T, Garrett J, Hu J, Wu H. Health and well-being in the home: a global analysis of needs, expectations and priorities for home health care technology. California: RAND Coorporation, 2010. 59 p.
McDaid D, Forsman A, Matosevic T, Park A-L. Independence and mental wellbeing (including social and emotional wellbeing) for older people: review 2 barrier and facilitators to improve or protect the mental wellbeing and/or independence of older people. National Institute for Health and Care Excellence, London 2015.
McFadden ES, Lucio J. Aging in (privatized) places: subsidized housing policy and seniors. J Hous Elderly. 2014;28(3):268–87.
McGoldrick C, Barrett GA, Cook I. Befriending and re-ablement service: a better alternative in an age of austerity. Int J Sociol Soc Policy. 2017;37:51–68.
Melis RJ, van Eijken MI, van Achterberg T, Teerenstra S, Vernooij-Dassen MJ, van de Lisdonk EH, et al. The effect on caregiver burden of a problem-based home visiting programme for frail older people. Age Ageing. 2009;38(5):542–7.
Mello J de Almeida, Macq J, Van Durme T, Ces S, Spurytte N, Van Audenhove C, et al. The determinants of informal caregivers’ burden in the care of frail older persons: a dynamic and role-related perspective. Aging Ment Health. 2017;21(8):838–43.
Michell G, Salmon JR, Polivka L, Soberon-Ferrer H. The relative benefits and cost of Medicaid home- and community-based services in Florida. Gerontologist. 2006; 46(4):483–94.
Millen BE, Ohls JC, Ponza M, McCool AC. The elder nutrition program: an effective national framework for preventive nutrition interventions. J Am Diet Assoc. 2002;102(2):234–40.
Morgan DG, Sernchuk KM, Stewart NJ, D’Arcy C. Rural families caring for a relative with dementia: barriers to use of formal services. Soc Sci Med. 2002;55(7):1129–42.
Messecar DC, Archbold PG, Stewart BJ, Kirschling J. Home environmental modification strategies used by caregivers of elders. Res Nurs Health. 2002;25(5):357–70.
Newman S. The living conditions of elderly Americans. Gerontologist. 2003;43(1):99–109.
Oura A, Mori M, Izumi H, Washio M. Depression in family caregivers of the frail elderly in Sapporo, Japan: a cross-sectional study. Sapporo Igaku Zasshi. 2010;79(1–6):21–274.
Pace C, Vella S, Dziegielewski SF. Long-term care of older adults in Malta: influencing factors and their social impacts amid the international financial crisis. J Soc Serv Res. 2016;42(2):263–79.
Pande A, Laditka SB, Laditka JN, Davis DR. Aging in place? Evidence that a state Medicaid waiver program helps frail older persons avoid institutionalization. Home Health Care Ser Q. 2007;26(3):39–60.
Paraponaris A, Davin B, Verger P. Formal and informal care for disabled elderly living in the community: an appraisal of French care composition and costs. Eur J Health Econ. 2012;13(3):327–36.
Payette H, Boutier V, Coulombe C, Gray-Donald K. Benefits of nutritional supplementation in free-living, frail, undernourished elderly people: a prospective randomized community trial. J Am Diet Assoc. 2002;102(8):1088–95.
Penning MJ. Hydra revisited: substituting formal for self- and informal in-home care among older adults with disabilities. Gerontologist. 2002;42(1):4–16.
Phillips VL, Atherly A. Prescription drug costs for dually eligible people in a medicaid home- and community-based services program. J Am Geriatr Soc. 2002;50(7):1283–8.
Piette JD, Rosland AM, Silveira M, Kabeto M, Langa KM. The case for involving adult children outside of the household in the self-management support of older adults with chronic illness. Chronic Illn. 2010;6(1):34–45.
Rantz M, Popejoy LL, Galambos C, Phillips LJ, Lane KR, Marek KD, et al. The continued success of registered nurse care coordination in a state evaluation of aging in place in senior housing. Nurs Outlook. 2014;62(4):237–46.
Rantz M, Lane K, Phillips LJ, Despins LA, Galambos C, Alexander GL, et al. Enhanced registered nurse care coordination with sensor technology: impact on length of stay and cost in aging in place housing. Nurs Outlook. 2015;63(6):650–5.
Rawlins JM, Spencer M. Daughters and wives as informal care givers of the chronically ill elderly in Trinidad. J Comp Fam Stud. 2002;33(1):125–37.
Renaut S, Ogg J, Petite S, Chamahian A. Home environments and adaptations in the context of ageing. Ageing Soc. 2015;35(6):1278–303.
Roelands M, Van Oost P, Buysse A, Depoorter A. Awareness among community-dwelling elderly of assistive devices for mobility and self-care and attitudes toward their use. Soc Sci Med. 2002;54(9):1441–51.
Rogero-Garcia J, Rosenberg MW. Paid and unpaid support received by co-resident informal caregivers attending to community-dwelling older adults in Spain. Eur J Ageing. 2011;8(2):95–107.
Ruiz-Arregui L, Avila-Funes JA, Amieva H, Borges-Yanez SA, Villa-Romero A, Aguilar-Navarro S, et al. The Coyoacan Cohort Study: design, methodology, and participants’ characteristics of a Mexican study on nutritional and psychosocial markers of frailty. J Frailty Aging. 2013;2(2):68–76.
Ryburn B, Wells Y, Foreman P. Enabling independence: restorative approaches to home care provision for frail older adults. Health Soc Care Community. 2009;17(3):225–34.
Sacks D, Das D, Romanick R, Caron M, Morano C, Fahs MC. The value of daily money management: an analysis of outcomes and costs. J Evid Based Soc Work. 2012;9(5):498–511.
Samuel LJ, Szanton SL, Weiss CO, Thorpe Jr. RJ, Semba RD, Fried LP. Financial strain is associated with malnutrition risk in community-dwelling older women. Epidemiol Res Int. 2012;2012:696518.
Sanchez-Garcia S, Sanchez-Arenas R, Garcia-Pena C, Rosas-Carrasco O, Avila-Funes JA, Ruiz-Arregui L, et al. Frailty among community-dwelling elderly Mexican people: prevalence and association with sociodemographic characteristics, health state and the use of health services. Geritr Gerontol Int. 2014;14(2):395–402.
Scribner B, Lynn J, Walker V, Morgan L, Montgomery A, Blair E, et al. Creating a nationwide nonpartisan initiative for family caregivers in political party platforms. J Am Geriatr Soc. 2017;65(6):1126–31.
Scuvee-Moreau J, Kurz X, Dresse A. The economic impact of dementia in Belgium: results of the National Dementia Economic Study (NADES). Acta Neuol Belg. 2002;102(3):104–13.
Sharkey JR. Longitudinal examination of homebound older adults who experience heightened food insufficiency: effect of diabetes status and implications for service provision. Gerontologist. 2005;45(6):773–82.
Stadnyk RL, Lashewicz B. Care work versus career work: sibling conflict over getting priorities right. Work. 2011;40(1):15–9.
Swinkels JC, Suanet B, Deeg DJH, Broese Van Groenou MI. Trends in the informal and formal home-care use of older adults in the Netherlands between 1992 and 2012. Ageing Soc. 2016;36(9):1870–90.
Takahashi NY. Deciding to seek help among family members caring for veterans with diabetes mellitus and co-morbid illnesses. Dis Abstr Int. 2016;77(6-A9E).
Teerawichitchainan B, Knodel J. Long-term care needs in the context of poverty and population aging: the case of older persons in Myanmar. J Cross Cult Gerontol. 2018;33(2):143–62.
Tomata Y, Watanabe T, Sugiyama K, Zhang S, Sugawara Y, Tsuji I. Effects of a community-based program for oral health and nutrition on cost-effectiveness by preventing disability in Japanese frail elderly: a quasi-experimental study using propensity score matching. J Am Med Dir Assoc. 2017;18(8):678–85.
Upchurch GA, Menon MP, Levin KS, Catellier DJ, Conlisk EA. Prescription assistance for older adults with limited income: client and program characteristics. J Pharm Technol. 2001;17(1):6–12.
Valluru R, Yudin J, Patterson CL, Kubisiak J, Boling P, Taler G, et al. Integrated home- and community-based services improve community survival among independence at home medicare beneficiaries without increasing medicaid costs. J Am Geriatr Soc. 2019;67(7):1495–501.
Van Dijk HM, Cramm JM, Van Exel J, Nieboer AP. The ideal neighbourhood for ageing in place as perceived by frail and non-frail community-dwelling older people. Ageing Soc. 2015;35(8):1771–95.
Van Houtvan CH, Oddone EZ, Weinberger M. Informal and formal care infrastructure and perceived need for caregiver training for frail US veterans referred to home and community-based services. Chronic Illn. 2010;6(1):57–66.
Vlachantoni A, Shaw RJ, Evandrou M, Falkingham J. The determinants of receiving social care in later life in England. Ageing Soc. 2015;35(2):321–45.
Walter-Ginzburg A, Guralnik JM, Blumstein T, Gindin J, Modan B. Assistance with personal care activities among the old-old in Israel: a national epidemiological study. J Am Geriatr Soc. 2001;49(9):1176–84.
Washio M, Arai Y, Oura A, Miyabayashi I, Onimaru M, Mori M. Family caregiver burden and public long-term care insurance system in Japan. Int Med J. 2012;19(3):229–33.
Waters TM, Almagor O, Finkel S, Harter K, Bartolozzi PR, Mitzen P, et al. Understanding costs of home and community based services. Manag Care Q. 2001;9(1):45–53.
Wenger GC. Childlessness at the end of life: evidence from rural Wales. Ageing Soc. 2009;29(8):1243–59.
Wilkins CH, Wilkins KL, Meisel M, Depke M, Williams J, Edwards, DF. Dementia undiagnosed in poor older adults with functional impairment. J Am Geriatr Soc. 2007;55(11):1771–6.
Williams AP, Challis D, Deber R, Watkins J, Kuluski K, Lum JM, et al. Balancing institutional and community-based care: why some older persons can age successfully at home while others require residential long-term care. Healthc Q. 2009;12(2):95–105.
Williams SW, Dilworth-Anderson P. Systems of social support in families who care for dependent African American elders. Gerontologist. 2002;42(2):224–36.
Williams SW, Dilworth-Anderson P, Goodwin PY. Caregiver role strain: the contribution of multiple roles and available resources in African-American women. Aging Ment Health. 2003;7(2):103–12.
Wu B, Carter MW, Goins RT, Cheng C. Emerging services for community-based long-term care in urban China: a systematic analysis of Shanghai's community-based agencies. J Aging Soc Policy. 2005;17(4):37–60.
You E, Dunt DR, Doyle C. Case managed community aged care: what is the evidence for effects on service use and costs? J Aging Health. 2013;25(7):1204–42.
Young HM, McCormick WM, Vitaliano PP. Attitudes toward community-based services among Japanese American families. Gerontologist. 2002;42(6):814–25.
Reason for exclusion: Did not include an older population that was frail (n = 193)
Abayomi O, Akinhanmi AO, Adelufosi AO. Psychiatric morbidity and subjective burden among carers of outpatients of a psychogeriatric clinic in Southwestern Nigeria. J Cross Cult Gerontol. 2015;30(4):349–50.
Abhishek G, Uday M, Singh Shivendra K, Manish MK, Chandra TS, Kumar SV. Screening depression among elderly in a city of southeast Asia. J Clin Diagn Res. 2015;9(9):2015.
Aguila E, Lopez-Ortega M, Angst S. Do income supplemental programs for older adults’ help reduce primary caregiver burden? Evidence from Mexico. J Cross Cult Gerontol. 2019;34(4):385–402.
Alakeson V. International development in self-directed care. Issue Brief (Commonw Fund). 2010;78:1–11.
Alkema GE. Bringing the pieces together: person-centeredness is key to transforming policy and services. Generations. 2016;40(4):94–100.
Allen SM, Foster A, Berg K. Receiving help at home: the interplay of human and technological assistance. J Gerontol B Psychol Sci Soc Sci. 2001;56(6):S374–82.
Alsinglawi B, Liu T, Nguyen QV, Gunawardana U, Maeder A, Simoff S. Passive RFID localisation framework in smart homes healthcare settings. Stud Health Technol Inform. 2016;231:1–8.
Angel RJ, Frisco M, Angel JL, Chiriboga DA. Financial strain and health among elderly Mexican-origin individuals. J Health Soc Behav. 2003;44(4):536–51.
Arnaud-Battandier F, Malvy D, Jeandel C, Schmitt C, Aussage P, Beaufrre B, et al. Use of oral supplements in malnourished elderly patients living in the community: a pharmaco-economic study. Clin Nutr. 2004;23(5):1096–103.
Aparasu R, Mort J, Brandt H. Psychotropic medication expenditures for community-dwelling elderly persons. Psychiatr Serv. 2003;54(5):739–42.
Aronson J. Frail and disabled users of home care: confident consumers or disentitled citizens? Can J Aging. 2002;21(1):11–25.
Ashby, K, Ozanne-Smith J, Fox B. Investigating the over-representation of older persons in do-it-yourself home maintenance injury and barriers to prevention. Injury Prevention. 2007;13(5):328–33.
Averill JB. Priorities for action in a rural older adults study. Fam Community Health. 2012;35(4):358–72.
Averill JB. Voices from the Gila: health care issues for rural elders in south-western New Mexico. J Adv Nurs. 2002;40(6):654–62.
Balla S, Simoncini M, Giacometti I, Magnano A, Leotta D, Pernigotti LM. The daily center care on impact of family burden. Arch Gerontol Geriatr. 2007;44:55–9.
Barker JC. Neighbors, friends and other nonkin caregivers of community-living dependent elders. J Gerontol B Psychol Sci Soc Sci. 2002;57(3):S158–167.
Battisto DG. Environmental influences on aging in place [PhD]. University of Michigan: ProQuest Pub, 2004.
Benjamin AE, Matthias RE, Magnano A, Leotta D, Pernigotti LM. Retention of paid related caregivers: who stays and who leaves home care careers? Gerontologist. 2008;48:104–13.
Bercaw LE. No place like home? Housing suitability for older adults who are ageing in place [PhD]. Brandeis University: ProQuest Publication, 2017.
Beverly CJ, Mcatee R, Costello J, Chernoff R, Casteel J. Needs assessment of rural communities: a focus on older adults. J Community Health. 2005;30(3):197–212.
Bisdee D, Daly T, Price D. Behind closed doors: older couples and the gendered management of household money. Soc Policy Soc. 2013;12(1):163–74.
Bittman M, Hill T, Thomson C. The impact of caring on informal carers’ employment, income and earnings: a longitudinal approach. Aust J Soc Issues. 2007;42(2):255–72,136.
Boggatz T, Farid T, Mohammedin A, Dijkstra A, Lohrmann C, Dassen T. Socio-demographic factors related to functional limitations and care dependency among older Egyptians. J Adv Nurs. 2010;66(5):1047–58.
Botsis T, Hartvigsen G. Current status and future perspectives in telecare for elderly people suffering from chronic diseases. J Telemed Telecare. 2008;14(4):195–203.
Bowling A, Gabriel Z. Lay theories of quality of life in older age. Ageing Soc. 2007;27(6):827–48.
Brackertz N. The impact of financial counselling on alleviating financial stress in low income households: a national Australian empirical study. Soc Policy Soc. 2014;13(3):389–407.
Brannelly T, Matthews B. When practical help is valued so much by older people, why do professionals fail to recognize its value? J Integr Care. 2010;18(2):33–40.
Browne CV, Mokuau N, Ka’opua LS, Kim BJ, Higuchi P, Braun KL. Listening to the voices of native Hawaiian elders and ‘Ohana caregivers: discussions on aging, health, and care preferences. J Cross Cult Gerontol. 2014;29(2):131–51.
Bush HM, Dickens NE, Henry RG, Durham L, Sallee N, Skelton J, et al. Oral health status of older adults in Kentucky: results from the Kentucky Elder Oral Health Survey. Spec Care Dentist. 2010;30(5):185–92.
Butler SS. Older women doing home care: exploitation or ideal job? J Gerontol Soc Work. 2013;56(4):299–317.
Butterworth P, Pymont C, Rodgers B, Windsor TD, Anstey KJ. Factors that explain the poorer mental health of caregivers: results from a community survey of older Australians. Aust N Z J Psychiatry. 2010;44(7):616–24.
Callan A, O'Shea E. Willingness to pay for telecare programmes to support independent living: results from a contingent valuation study. Soc Sci Med. 2015;124:94–102.
Cameron ID, Kurrle S, Quine S, Sambrook P, March L, Stocks J, et al. Increasing adherence with the use of hip protectors for older people living in the community. Osteoporos Int. 2011;22(2):617–26.
Canham SL, Battersby L, Fang ML, Wada M, Barnes R, Sixsmith A. Senior services that support housing first in metro Vancouver. J Gerontol Soc Work. 2018;61(1):104–25.
Cao MJ, Guo XL, Yu H, Chen LY, McDonald TA. Chinese community-dwelling elders’ needs: promoting ageing in place. Int Nurs Rev. 2014;61(3):327–35.
Carretero S, Stewart J, Centeno C. Information and communication technologies for informal carers and paid assistants: benefits from micro-, meso- and macro-levels. Eur J Ageing. 2015;12(2):163–73.
Chan L-S, Chou K-L. Poverty in old age: evidence from Hong Kong. Ageing Soc. 2018;38(1):37–55.
Chen HL. Welfare and long-term care in the East and West. Int J Sociol Soc Policy. 2010;30(3/4):167–81.
Cho S-H. Older people's willingness to use home care nursing services. J Adv Nurs. 2005;51(2):166–73.
Cline RR, Gupta K, Singh RL, Schommer JC. Older adults’ drug benefit beliefs: a focus group study. J Manag Care Pharm. 2005;11(1):77–85.
Cohen MA, Miller J, Weinrobe M. Patterns of informal and formal caregiving among elders with private long-term care insurance. Gerontologist. 2001;41(2):180–7.
Comas-Herrera A, Wittenberg R, Costa-Font J, Gori C, Di Maio A, Patxot C, et al. Future long-term care expenditure in Germany, Spain, Italy and the United Kingdom. Ageing Soc. 2006;26(2):285–302.
Cooney TM, Dykstra PA. Family obligations and support behavior: a United States-Netherlands comparison. Ageing Soc. 2011;31(6):1026–50.
Cotter N, Monahan E, McAvoy H, Goodman P. Coping with the cold – exploring relationships between cold housing, health and social wellbeing in a sample of older people in Ireland. Qual Ageing Older Adults. 2012;13(1):38–47.
Cox C. Who is responsible for the care of the elderly? A comparison of policies in the United States, the United Kingdom, and Israel. Soc Thought. 2001;20(3/4):33–45.
Crosby J, McAdams R, Adams A. Prescription drug expenditures among the community-dwelling elderly population: evidence from the 2000 Medical Expenditure Panel Survey. J Pharmaceut Finance Econ Policy. 2005;14(2):25–37.
Dallaire B, McCubbin M, Provost M, Carpentier N, Clement M. [Paths and life situations of seniors with serious mental disabilities: psychosocial perspectives]. Can J Aging. 2010;29(2):267–79. French.
Dante M. Exploring the lived experiences of seniors aging in place [PhD]. Minnesota: Walden University, 2015.
Davis MP, Srivastava M. Demographics, assessment and management of pain in the elderly. Drugs Aging. 2003;20(1):23–57.
De Oliveira DC, Hlebec V. Predictors of satisfaction with life in family carers: evidence from the third European quality of life survey 1. Teorija in Praksa. 2016;53(2):503–23,567–8.
Dong X, Chang ES, Wong E, Wong B, Skarupski KA, Simon MA. Assessing the health needs of Chinese older adults: findings from a community-based participatory research study in Chicago's Chinatown. J Aging Res. 2010;2010:124246.
Doyle M, Timonen V. Breaking the mould: new trajectories in the domiciliary care of older people in Ireland. Int J Soc Welf. 2008;17(4):324–32.
Drewnowski A, Shultz JM. Impact of aging on eating behaviors, food choices, nutrition and health status. J Nutr Health Aging. 2001;5(2):75–9.
Ducharme F, Perodeau G, Paquer M, Legault A, Trudeau D. [Ambulatory shift and family care at home]. Can J Public Health. 2004;95(1):64–8. French.
Duncan KA, Shooshtari S, Roger K, Fast J, Han J. Care-related out-of-pocket expenditures in Canada. J Financ Couns Planning. 2016;27(2):277–96.
Ehrler F, Lovis C. Supporting elderly homecare with smartwatches: advantages and drawbacks. Stud Health Technol Inform. 2014;205:667–71.
Ekstam L, Fange AM, Carlsson G. Negotiating control: from recognizing a need to making a decision to apply for a housing adaptation. J Hous Elderly. 2016;30(4):345–59.
Evans N, Imelda JD, Allotey P, Reidpath DD, Pool R. Social support and care arrangements of older people living alone in rural Malaysia. Ageing Soc. 2018;38(10):2061–81.
Federman AD, Adams AS, Ross-Degnan D, Soumerai SB, Ayanian JZ. Supplemental insurance and use of effective cardiovascular drugs among elderly Medicare beneficiaries with coronary heart disease. JAMA. 2001;286(14):1732–9.
Financial Consumer Agency of Canada. Progress report: Canada's national research plan on financial literacy 2016–2018 [internet]. 2018. Available from: https://www.canada.ca/en/financial-consumer-agency/programs/research/progress-report-national-research-plan-2016-2018.html.
Floyd M, Platz L, French SL. Late-life issues: a survey of residents in a retirement-age community. J Ment Health Aging. 2004;10(2):117–30.
Foster L, Brown R, Phillips B, Lepidus Carlson B. Easing the burden of caregiving: the impact of consumer direction of primary informal caregivers in Arkansas. Gerontologist. 2005;45(4):474–85.
Friedman SM, Steinwachs DM, Temkin-Greener H, Mukamel DB. Informal caregivers and the risk of nursing home admission among individuals enrolled in the program of all-inclusive care for the elderly. Gerontologist. 2006;46(4):456–63.
Fritz RL. The influence of culture on older adults’ adoption of smart home monitoring: a qualitative descriptive study. Diss Abstr Int. 2016;77(3-B(E)).
Fritz RL, Corbett CL, Vandermause R, Cook D. The influence of culture on older adults’ adoption of smart home monitoring: a qualitative descriptive study. Gerontechnology. 2016;14(3):146–56.
Fruhauf CA, Jarrott SE, Allen KR. Grandchildren's perceptions of caring for grandparents. J Family Iss. 2006;27(7):887–911.
Fu YY, Chui EW, Law CK, Zhao ZY, Lou VWQ. An exploration of older Hong Kong residents’ willingness to make copayments toward vouchers for community care. J Aging Soc Policy. 2019;31(4):358–77.
Gandy R, Bell A, McClelland B, Roe B. Evaluating the delivery, impact, costs and benefits of an active lives programme for older people living in the community. Prim Health Care Res Dev. 2017;18(2):122–34.
Gerstenecker A, Eakin A, Triebel K, Martin R, Swenson-Dravis D, Petersen RC, et al. Age and education corrected older adult normative data for a short form version of the financial capacity instrument. Psychol Assess. 2016;28(6):737–49.
Ghesquiere AR, Bazelais KN, Berman J, Greenburg RL, Kaplan D, Bruce ML. Associations between recent bereavement and psychological and financial burden in homebound older adults. Omega. 2016;73(4):326–39.
Giunta N, Chow J, Scharlach AE, Dal Santo TS. Racial and ethnic differences in family caregiving in California. J Hum Behav Soc Environ. 2004;9(4):85–109.
Golant SM. Low-income elderly homeowners in very old dwellings: the need for public policy debate. J Aging Soc Policy. 2008;20(1):1–28.
Goswami S, Deshmukh PR. How “elderly staying alone” cope up with their age and deteriorating health: a qualitative exploration from rural Wardha, Central India. Indian J Palliat Care. 2018;24(4):465–71.
Graham CL, Scharlach AE, Price Wolf J. The impact of the “village” model on health, well-being, service access, and social engagements of older adults. Health Educ Behav. 2014;41(1):91S-97S.
Green-Lapierre RJ, Williams PL, Glanville NT, Norris D, Hunter HC, Watt CG. Learning from “knocks in life”: food insecurity among low-income lone senior women. J Aging Res. 2012;2012:450630.
Haikio L, Anttonen A. Local welfare governance structuring informal carers’ dual position. Int J Sociol Soc Policy. 2011;31(3/4):185–96.
Hall SE, Hendrie DV. A prospective study of the costs of falls in older adults living in the community. Aust N Z J Public Health. 2003;27(3):343–51.
Han SD, Boyle PA, James BD, Yu L, Bennett DA. Poorer financial and health literacy among community-dwelling older adults with mild cognitive impairment. J Aging Health. 2015;27(6):1105–17.
Hanson J, Percival J. The housing and support needs of visually impaired adults living in England today. Br J Vis Impair. 2005;23(3):102–7.
Harrington Meyer M. Changing social security in the US: rising insecurity? Soc Policy Soc. 2013;12(1):135–46.
Hartman M, Catlin A, Lassman D, Cylus J, Heffler S. U.S. health spending by age, selected years through 2004. Health Aff (Millwood). 2008;27(1):w1-w12.
Hayward L, Davies S, Robb R, Denton M, Auton G. Publicly funded and family-friend care in the case of long-term illness: the role of the spouse. Can J Aging. 2004;23(Suppl 1):S39-S48.
Holliday HV, Jenstad LM, Grosjean G, Purves B. “You can lead a horse to water…” focus group perspectives on initiating and supporting hearing health challenges in older adults. Am J Audiol. 2015;24(3):360–76.
Holroyd E. Developing a cultural model of caregiving obligations for elderly Chinese wives. West J Nurs Res. 2005;27(4):437–56.
Hong SI, Hasche L, Lee MJ. Service use barriers differentiating care-givers’ service use patterns. Ageing Soc. 2011;31(8):1307–29.
Horn A. Medical care for the homeless elderly. Care Manag J. 2008;9(1):25–30.
Horton K, Dickinson A. The role of culture and diversity in the prevention of falls among older Chinese people. Can J Aging. 2011;30(1):57–66.
Howell-White S, Gaboda D, Scotto Rosato N, Lucas JA. Creating needs-based tiered models for assisted living reimbursement. Gerontologist. 2006;46(3):334–43.
Hsu HC, Ting YS, Jiang TW, Chien MC, Chien CH. Autonomy and acceptance of long-term care. Educ Gerontol. 2009:35(11):949–62.
Jiang Q, Cohen NL, Marra MV, Woolf K, Gilbride J, Francis SL. Community priorities for healthy eating in older adults. J Nutr Gerontol Geriatr. 2017;36(2–3):75–91.
Jutkowitz E, Gitlin LN, Pizzi L, Lee E, Dennis MP. Cost effectiveness of a home-based intervention that helps functionally vulnerable older adults age in place at home. J Aging Res. 2012;2012:680265.
Kabel A. Fighting for wellness: strategies of mid-to-older women living with cancer. J Cross Cult Gerontol. 2015;30(1):107–17.
Kairuz T, Bye L, Birdsall R, Deng T, Man L, Ross A, et al. Identifying compliance issues with prescription medicines among older people: a pilot study. Drugs Aging. 2008;25(2):153–62.
Kao HF, Acton GJ. Conceptualization and psychometric properties of the Caregiver Burden Scale in Taiwan. Issues Ment Health Nurs. 2006;27(8):853–866.
Karatas K, Duyan V. Difficulties that elderly people encounter and their life satisfaction. Soc Behav Pers. 2008;36(8):1073–83.
Khan, HTA, Leeson GW, Findlay H. Attitudes towards bearing the cost of care in later life across the world. Illn Crises Loss. 2013;21(1):49–69.
Kietzman KG, Benjamin AE, Matthias RE. Whose choice? Self-determination and the motivations of paid family and friend caregivers. J Comp Fam Stud. 2013;44(4):519–40.
Kietzman KG, Durazo EM, Torres JM, Choi AS, Wallace SP. Independence at risk: older Californians with disabilities struggle to remain at home as public supports shrink. Policy Brief UCLA Cent Health Policy Res. 2011;(PB2011–10):1–8.
Kim E, Gellis ZD, Bradway C, Kenaley B. Key determinants to using telehealth technology to service medically ill and depressed homebound older adults. J Gerontol Soc Work. 2019;62(4):451–74.
Kim H, Traphagan JW. From socially weak to potential consumer: changing discourses on elder status in South Korea. Care Manag J. 2009;10(1):32–9.
Lagergren M, Kurube N, Saito Y. Cost trends in long term care in Japan and Sweden over the period 2000 to 2010. J Popul Ageing. 2017;10(3):207–27.
Laher N, Kumar N, Um S, Mckenzie K. Thriving in the city: what does it cost to have a healthy retirement? Toronto: Wellesley Institute, 2018. 20 p.
Lan P-C. Subcontracting filial piety: elder care in ethnic Chinese immigrant families in California. J Fam Issues. 2002;23(7):812–35.
Lan T-Y, Wu S-C, Chang W-C, Chen C-Y. Home environmental problems and physical function in Taiwanese older adults. Arch Gerontol Geriatr. 2009;49(3):335–38.
Langa KM, Fendrick AM, Chernew ME, Kabeto MU, Paisley KL, Hayman JA. Out-of-pocket health-care expenditures among older Americans with cancer. Value Health. 2004;7(2):186–94.
Leduc F. Management of care at home. Soins Gerontol. 2004;(50):29–32.
Lee C, Porteous J. Experiences of family caregiving among middle-aged Australian women. Fem Psychol. 2002;12(1):79–96.
Lehning A, Kim K, Smith R, Choi M. Does economic vulnerability moderate the association between transportation mode and social activity restrictions in later life? Ageing Soc. 2017;38(10).
Leopold T, Raab M, Engelhardt H. The transition to parent care: costs, commitments, and caregiver selection among children. J Marriage Fam. 2014;76(2):300–18.
Li X, Shen JJ, Lu J, Wang Y, Sun M, Li C, et al. Household catastrophic medical expenses in eastern China: determinants and policy implications. BMC Health Serv Res. 2013;13:506.
Lima-Costa MF, Peixoto SV, Malta DC, Szwarcwald CL, Mambrini JVM. Informal and paid care for Brazilian older adults (National Health Survey, 2013). Rev Saude Publica. 2017;51:6s.
Liu J, Lu N, Lou VWQ. Care tasks in the stress process for family caregivers in urban China. Clin Gerontol. 2017;40(5):437–56.
Liu M, Gao M, Bern-klug M. Economic stress among adult-child caregivers of the oldest old in China: the importance of contextual factors. J Cross Cult Gerontol. 2013;28(4):465–79.
Liu M, Gao R, Pusari N. Using participatory action research to provide health promotion for disadvantage elders in Shaanxi province, China. Public Health Nurs. 2006;23(4):332–8.
Livadiotakis G, Gutman G, Hollander MJ. Rationing home care resources: how discharged seniors cope. Home Health Care Serv Q. 2003;22(2):31–42.
Lloyd JL, Wellman NS. Older Americans Act nutrition programs: a community-based nutrition program helping older adults remain at home. J Nutr Gerontol Geriatr. 2015;34(2):90–109.
Locher JL, Ritchie CS, Robinson CO, Roth DL, West DS, Burgio KL. A multidimensional approach to understanding under-eating in homebound older adults: the importance of social factors. Gerontologist. 2008;48(2):223–34.
Lofqvist C, Nygren C, Szeman Z, Iwarsson S. Assistive devices among very old people in five European countries. Scand J Occup Ther. 2005;12(4):181–92.
Loh CP, Shapiro A. Willingness to pay for home- and community-based services for seniors in Florida. Home Health Care Serv Q. 2013;32(1):17–34.
Longino CF Jr, Perzynski AT, Stoller EP. Pandora's briefcase: unpacking the retirement migration decision. Res Aging. 2002;24(1):29–49.
Lowenstein A, Daatland SO. Filial norms and family support in a comparative cross-national context: evidence from the OASIS study. Ageing Soc. 2003;26:203–23.
Lyon D, Glucksmann M. Comparative configurations of care work across Europe. Soc. 2008;42(1):101–18.
McWilliam CL, Ward-Griffin C, Sweetland D, Sutherland C, O’Halloran L. The experience of empowerment in in-home services delivery. Home Health Care Serv Q. 2001;20(4):49–71.
Medrano A. CCTs for female heads of households and market citizenship at state-level in Mexico. Soc Policy Soc. 2016;15(3):495–507.
Messer M. Poor, old and in need of care: a qualitative study about the consequences for home care and participation. Ger Med Sci. 2019;17:Doc08.
Michin H, Harrington D. The effects of caregiving resources on perceived health among caregivers. Health Soc Work. 2016;41(3):155–63.
Misplon S, Pacolet J, Hedebouw G. Care time and costs of care for elderly persons with dementia. Arch Public Health. 2004;62(3–4):143–56.
Moran N, Glendinning C, Wilberforce M, Stevens M, Netten A, Jones K, et al. Older people's experiences of cash-for-care schemes: evidence from the English individual budget pilot projects. Ageing Soc. 2013;33(5):826–51.
Nakagawa Y, Yamada R, Nasu S. Characteristics of care-givers and care recipients influencing the impact of paid care services on family care-giver burdens. Ageing Soc. 2014;34(8):1314–34.
Naughton C, Drennan J. Exploring the boundaries between interpersonal and financial institution mistreatment of older people through a social ecology framework. Ageing Soc. 2016;36(4):694–715.
Nelms L, Johnson V, Teshuva K, Foreman P, Stanley J. Social and health factors affecting community service use by vulnerable older people. Austral Social Work. 2009;62(4):507–524.
Nepal B, Brown L, Ranmuthugala G, Percival R. A comparison of the lifetime economic prospects of women informal carers and non-carers, Australia, 2007. Aus J Soc Issues. 2011;46(1):91–108.
Neubauer S, Holle R, Menn P, Grossfeld-Schmitz M, Graesel E. Measurement of informal care time in a study of patients with dementia. Int Psychogeriatr. 2008;20(6):1160–76.
New York City Department for the Aging. The changing needs of New York City's elderly. Care Manag J. 2007;8(3):127–40.
Nortey ST, Aryeetey GC, Aikins M, Amendah D, Nonvignon J. Economic burden of family caregiving for elderly population in southern Ghana: the case of a peri-urban district. Int J Equity Health. 2017;16(1):16.
O’Leary ME. Caring here, caring there Boston-based immigrant caregivers as agents of the globalization of eldercare. Diss Abstr Int. 2017;78(5A(E)).
Penders YWH, Riejens J, Albers G, Croezen S, Van den Block L. Differences in out-of-pocket costs of healthcare in the last year of life of older people in 13 European countries. Palliat Med. 2017;31(1):42–52.
Penhale B. Ethical dilemmas in charging for care: contrasting the views of social work and legal professionals. J Interprof Care. 2002;16(3):235–47.
Perks T, Haan M. The dwelling-type choices of older Canadians and future housing demand: an investigation using the Aging and Social Support Survey (GSS16). Can J Aging. 2010;29(3):445–63.
Pickard L, Brimblecombe N, King D, Knapp M. ‘Replacement care’ for working carers? A longitudinal study in England, 2013–15. Soc Policy Adm. 2018;52(3):690–709.
Pradhan MAH, Mathbor GM. Elder vulnerability in receiving home care services: evidence from Bangladesh. Social Dev Issues. 2017;39(2):44–61.
Price D, Bisdee D, Daly T, Livsey L, Higgs P. Financial planning for social care in later life: the ‘shadow’ of fourth age dependency. Ageing Soc. 2014;34(3):388–410.
Quashie N, Zimmer Z. Residential proximity of nearest child and older adults’ receipts of informal support transfers in Barbados. Ageing Soc. 2013;33(2):320–41.
Rainville C, Skufca L, Mehegan L. Family caregivers cost survey: what they spend & what they sacrifice. Washington, DC;AARP Research, 2016. 56 p.
Rantz MJ, Phillips L, Aud M, Popejoy L, Marek KD, Zaniletti, et al. Evaluation of aging in place model with home care services and registered nurse care coordination in senior housing. Nurs Outlook. 2011;59(1):37–46.
Rhee YJ, Degenholtz HB, Howard B, Lo Sasso AT, Emanuel LL. Estimating the quantity and economic value of family caregiving for community-dwelling older persons in the last year of life. J Am Geriatr Soc. 2009;57(9):1654–9.
Rigaud AS, Fagnani F, Bayle C, Latour F, Traykov L, Forette F. Patients with Alzheimer's Disease living at home in France: costs and consequences of the disease. J Geriatr Psychiatry Neurol. 2003;16(3):140–5.
Riikonen M, Makela K, Perala S. Safety and monitoring technologies for the homes of people with dementia. Gerontchnology. 2010;9(1):32–45.
Robinson, Buckwalter, Reed. Response by Robinson, Buckwalter and Reed. West J Nurs Res. 2005;27(2):145–7.
Rojo-Perez F, Fernandez-Mayoralas Fernandez G, Pozo Rivera E, Abuin R, Manuel J. Ageing in place: predictors of the residential satisfaction of elderly. Soc Indic Res. 2001;54(2):173–208.
Rosenthal CJ, Martin-Matthews A, Keefe JM. Care management and care provision for older relatives amongst employed informal care-givers. Ageing Soc. 2007;27(5):755–78.
Sheehan NW, Oakes CE. Bringing assisted living services into congregate housing: housing directors’ perspectives. J Aging Soc Policy. 2006;18(1):65–86.
Sheridan MJ, Burley J, Hendricks DE, Rose T. ‘Caring for one's own’: variation in the lived experience of African-American caregivers of elders. J Ethn Cult Divers Soc Work. 2014;23(1):1–19.
Shin J. The residential choices of ethnic elders in affordable housing: changing intergenerational relationships and the pursuit of residential independence. J Hous Elderly. 2014;28(2):221–42.
Sims-Gould J, Martin-Matthews A, Gignac AM. Episodic crises in the provision of care to elderly relatives. J Appl Gerontol. 2008;27(2):123–40.
Snowdon J, Halliday G. A study of severe domestic squalor: 173 cases referred to an old age psychiatry service. Int Psychogeriatr. 2011;23(2):308–14.
Stoddart H, Whitley E, Harvey I, Sharp D. What determines the use of home care services by elderly people? Health Soc Care Community. 2002;10(5):348–60.
Subasic K. Planning for the future a grounded theory of study of well older adults decision making regarding home modification [PhD]. Florida: ProQuest Pub Nova Southeastern University, 2014.
Szanton SL. Stress, poverty, frailty and mortality in older women [PhD]. Washington, DC: Johns Hopkins University, 2007.
Szeman Z. Family strategies in Hungary: the role of undocumented migrants in eldercare. J Popul Ageing. 2012;5(2):97–118.
Takagi E, Silverstein M. Purchasing piety? Coresidence of married children with their older parents in Japan. Demography. 2011;48(4):1559–79.
Teo P. Health care for older persons in Singapore: integrating state and community provisions with individual support. J Aging Soc Policy. 2004;16(1):43–67.
Thanh NX, Lindholm L. Has Vietnam health care fund for the poor policy favored the elderly poor? BMC Health Serv Res. 2012;12(333).
Tinker A, Lansley P. Introducing assistive technology into the existing homes of older people: feasibility, acceptability, costs and outcomes. J Telemed Telecare. 2005;11(Suppl 1):1–3.
Toohey AM, Rock MJ. Disruptive solidarity or solidarity disrupted? A dialogical narrative analysis of economically vulnerable older adults’ efforts to age in place with pets. Public Health Ethics. 2019;12(1):15–29.
Townsend AL, Ishler KJ, Shapiro BM, Pitorak EF, Matthews CR. Levels, types, and predictors of family caregiver strain during hospice home care for an older adult. J Soc Work End Life Palliat Care. 2010;6(1–2):51–72.
Vamstad J. Exit, voice and indifference – older people as consumers of Swedish home care services. Ageing Soc. 2016;36(10):2163–81.
Van Hoi L, Thi Kin Tien N, Van Tien N, Van Dung D, Thi Kin Chuc N, Goran Sahlen K, et al. Willingness to use and pay for options of care for community-dwelling older people in rural Vietnam. BMC Health Serv Res. 2012;12:36.
Van Houtven CH, Norton EC. Informal care and health care use of older adults. J Health Econ. 2004;23(6):1159–80.
Verbrugge LM, Chan A. Giving help in return: family reciprocity by older Singaporeans. Ageing Soc. 2008;28(1):5–34.
Vuorialho A, Karinen P, Sorri M. Counselling of hearing aid users is highly cost-effective. Eur Arch Otorhinolaryngol. 2006;263(1):988–95.
Wallace SP, Benjamin AE, Villa VM, Pourat N. California budget cuts fray the long-term care safety net. Policy Brief UCLA Cent Health Policy Res. 2009;(PB2009–8):1–8.
Wallace SP, Padilla-Frausto DI, Smith SE. Economic need among older Latinos: applying the Elder Economic Security Standard Index. J Cross Cult Gerontol. 2013;28(3):239–50.
Wallace SP, Smith SE. Half a million older Californians living alone unable to make ends meet. California: UCLA Center for Health Policy Research, 2009. 6 p.
Wang PS, Patrick AR, Dormuth C, Maclure M, Avorn J, Canning CF, et al. Impact of drug cost sharing on service use and adverse clinical outcomes in elderly receiving antidepressants. J Ment Health Policy Econ. 2010;13(1):37–44.
Wanless D, Mitchell BA, Wister AV. Social determinants of health for older women in Canada: does rural-urban residency matter? Can J Aging. 2010;29(2):233–47.
Wasserfallen J, Bourgeois R, Bula C, Yersin B, Buclin T, Wasserfallen JB, et al. Composition and cost of drugs stored at home by elderly patients. Ann Pharmacother. 2003;37(5):731–7.
Watt MH, Perera B, Ostbye T, Ranabahu S, Rajapakse H, Maselko J. Care-giving expectations and challenges among elders and their adult children in Southern Sri Lanka. Ageing Soc. 2014;34(5):838–58.
Weaver RH, Roberto KA. Home and community-based service used by vulnerable older adults. Gerontologist. 2017;57(3):540–51.
Weeks LE, LeBlanc K. Housing concerns of vulnerable older Canadians. Can J Aging. 2010;29(3):333–47.
Whittier S, Scharlach AE, Dal Santo TE. Availability of caregiver support services: implications for implementation of the National Family Caregiver Support Program. J Aging Soc Policy. 2005;17(1):45–62.
Wiener JM, Tilly J, Alecxih LMB. Home and community-based services in seven states. Health Care Financ Rev. 2002;23(3):89–114.
Wilhelmson K, Andersson C, Waern M, Allebeck P. Elderly people's perspectives on quality of life. Ageing Soc. 2005;25:585–600.
Wilkinson-Meyers L, Brown P, McLean C, Kerse N. Met and unmet need for personal assistance among community dwelling New Zealanders 75 years and over. Health Soc Care Community. 2014;22(3):317–27.
Williams AM, Forbes DA, Mitchell J, Essar M, Corbett B. The influence of income on the experience of informal caregiving: policy implications. Health Care Women Int. 2003;24(4):280–91.
Wilson E, Thalanany M, Shepstone L, Charlesworth G, Poland F, Harvey I, et al. Befriending carers of people with dementia: a cost utility analysis. Int J Geriatr Psychiatry. 2009;24(6):610–23.
Wind B, Dewilde C. Home-ownership and housing wealth of elderly divorcees in ten European countries. Ageing Soc. 2018;38(2):267–95.
Windle GS, Burholt V, Edwards RT. Housing related difficulties, housing tenure and variations in health status: evidence from older people in Wales. Health Place. 2006;12(3):267–78.
Winterton R, Warburton J, Oppenheimer M. The future for meals on wheels? Reviewing innovative approaches to meal provision for ageing populations. Int J Soc Welf. 2013;22(2):141–51.
Witvorapong N. The relationship between upstream intergenerational transfers and wealth of older adults: evidence from Thailand. J Popul Res. 2015;32:215–42.
Woolham J, Daly G, Sparks T, Ritters K, Steils N. Do direct payments improve outcomes for older people who receive social care? Differences in outcome between people aged 75+ who have a managed personal budget or direct payment. Ageing Soc. 2017;37(5):961–84.
Yuen HK, Gibson RW, Yau MK, Mitcham MD. Actions and personal attributes of community-dwelling older adults to maintain independence. Phys Occup Ther Geriatr. 2007;25(3):35–53.
Yusif S, Soar J, Hafeez-Baig A. Older people, assistive technologies, and the barriers to adoption: a systematic review. Int J Med Inform. 2016;94:112–16.
Reason for exclusion: Language of publication (not English or French) (n = 17)
Aksoydan E. [Are developing countries reading for ageing populations? An examination on the socio-demographic, economic and health status of elderly in Turkey.] Turk Geriatri Derg. 2009;12(2):102–9. Turkish.
Alonso Lopez F. [Adaptive behaviour of persons with functional limitation: housing adaptations in Spain]. Rev Esp Geriatr Gerontol. 2018;53(5):285–92. Spanish.
Fischer T. [Residence for the elderly with nursing care needs. “under no circumstances into a nursing home”!]. Pflege Z. 2012;65(3):148–51. German.
Foulk MA. [Elder care systems and practices in the U.S.A.]. Nihon Ronen Igakkai Zasshi. 2000;37(7):515–18. Japanese.
Gil Montoya JA, Subira Pifarre C. [Domiciliary assistance dental programs: a current demand]. Atencion Primaria. 2004;34(7):368–73. Spanish.
Heusinger J. [Self-determination and organisation of care in domestic care arrangements]. Z Gerontol Geriatr. 2006;39(6):418–22. German.
Homan M, Matsuda S. [An analysis of meidcal expenses of outpatient service for the elderat one health insurace society in Fukuoka prefecture—focused on medical service and concentration of medical expenses]. J UOEH. 2001;23(3):285–95. Japanese.
Ken K, Okuno J, Fukasaku T, Tomura S, Yanagi H. [Factors affecting burden of caregivers for the elderly of Han Chinese and the Korean minority living in a community in northeast China]. Nihon Koshu Eisei Zasshi. 2010;57(9):816–24. Japanese.
Kort HSM. [Technology for longevity: Predictors for use of technology]. Medicina. 2016;49:24–6. Portuguese.
Lamura G, Mnich E, Wojszel B, Nolan M, Krevers B, Mestheneos L, et al. [The experience of family carers of older people in the use of support services in Europe: selected findings from the EUROFAMCARE project]. Z Gerontol Geriatr. 2006;39(6):429–42. German.
Lee E, Kim J. [Economic effect of home health care services for community-dwelling vulnerable populations]. J Korean Acad Nurs. 2016;46(4):52–571. Korean.
Matus-Lopez M. [Trends and reforms in long-term care policies for the elderly]. Cad Saude Publica. 2015;31(12):2475–81. Portuguese.
Meira EC, Goncalves LHT, Zavier JO. [Oral reports by caregivers for ill and frail elderly relatives, in regard to risk factors for intrafamily violence]. Ciencia, Cuidado e Saude. 2007;6(2):171–80. Spanish.
Otto U, Tarnutzer S, Brettenhofer M. [Telemedicine for the elderly-opportunities are increasing, critical factors have to be tackled!] Ther Umsch. 2015;72(9):577–9. German.
Toida M, Takemura S. [Cost-benefit analysis of community based rehabilitation program using willingness to pay measured by the contingent valuation method]. Nihon Ronen Igakkai Zasshi. 2002;49(1):29–40. Japanese.
Verbeek-Oudijk D, Eggink E. [The upper-limits of deinstitutionalization not yet reached]. Tijdschr Gerontol Geriatr. 2014;45(4):188–96. German.
Vilaplana Prieto C, Jimenez-Martin S, Garcia Gomez P. [Trade off between formal and informal care in Europe]. Gac Sanit. 2011;25 Suppl 2:115–24. Spanish.
Reason for exclusion: Not set in the community (n = 10)
Chen L. The decision to institutionalize among nursing home residents and their children in Shanghai [PhD]. Diss Abstr Int. 2014;74(12-A(E)).
Giguere AMC, Farmanova E, Holroyd-Leduc JM, Straus SE, Urquhart R, Carnovale V, et al. Key stakeholders’ views on the quality of care and services available to frail seniors in Canada. BMC Geriatr. 2018;18(1):290.
Guan X, Zhan HJ, Liu, G. Institutional and individual autonomy: investigating predictors of attitudes toward institutional care in China. Int J Aging Hum Dev. 2007;64(1):83–107.
Hawes C, Phillips CD, Holan S, Sherman M, Hutchinson LL. Assisted living in rural America: results from a national survey. J Rural Health. 2005;21(2):131–9.
Huang J, Tung CM. The effects of outpatient co-payment policy on healthcare usage by the elderly in Taiwan. Arch Gerontol Geriatr. 2006;43(1):101–16.
Hughes J, Challis D. Frail older people – margins of care. Rev Clin Gerontol. 2004;14(2):155–64.
Lahtinen A, Leppilahti J, Vahanikkila H, Harmainen S, Koistinen P, Rissanen P, et al. Costs after hip fracture in independently living patients: a randomised comparison of three rehabilitation modalities. Clin Rehabil. 2017;31(5):672–85.
Shankar KN, Hirschman KB, Hanlon AL, Naylor MD. Burden in caregivers of cognitively impaired elderly adults at time of hospitalization: a cross-sectional analysis. J Am Geriatr Soc. 2014;62(2):276–84.
Stone LJ, Clements JA. The effects of nursing home placement on the perceived levels of caregiver burden. J Gerontol Soc Work. 2009;52(3):193–214.
Wai AAP, Fook VFS, Jayachandran M, Biswas J, Nugent C, Mulvenna M, et al. Smart wireless continence management system for persons with dementia. Telemed J E Health. 2008;14(8):825–32.
Reason for exclusion: Full text not available (n = 6)
Cohen M, Miller J. The impact of private long-term care insurance on claimants: formal and informal care in the community. Policy Brief (Cent Home Care Policy Res). 2002;(11):1–4.
Health Policy Tracking Service, a service of Thomson Reuters Accelus, & Seiler LW. Long-term care: home- and community-based services. Issue Brief Health Policy Tracking Serv. 2012:1–32.
Kogan M. Remodeling or moving? Aging in place can cost an arm and a leg. Selling to Seniors. 2006;6(6):6.
Lindy CN, The lived experiences of employed adults with dependent adult caregiving responsibilities [PhD]. Texas: Texas Woman's University, 2006.
Mclaughlin LA. Factors that contribute to stress among Japanese-American and Caucasian-American family caregivers of frail elders. Diss Abstr Int. 2003;63(11-A):4094.
Valluzzi JL. Health care expenditures of community-dwelling adults with disabilities [PhD]. Washington, DC: George Washington University, 2011.
Appendix IV: Characteristics of included studies
Footnotes
RMM is an associate editor of JBI Evidence Synthesis and was not involved in the editorial processing of this manuscript. The other authors declare no conflict of interest.
References
- 1.World Health Organization. World report on ageing and health 2015 [internet]. World Health Organization; 2015 [cited 2021 Oct 5]. Available from: https://apps.who.int/iris/handle/10665/186463. [Google Scholar]
- 2.United Nations. World population ageing 2019. New York; 2020; 64 p. [Google Scholar]
- 3.Canadian Institute for Health Information. Health care in Canada 2011: a focus on seniors and aging [internet]. 2011 [cited 2021 Oct 5]. Available from: https://www.homecareontario.ca/docs/default-source/publications-mo/hcic_2011_seniors_report_en.pdf. [Google Scholar]
- 4.Williams GA, Cylus J, Roubal T, Ong P, Barber S. Sustainable health financing with an ageing population: will population ageing lead to uncontrolled health expenditure growth? [internet]. The economics of healthy and active ageing series. Copenhagen (Denmark): European observatory on health systems and policies; 2019 [cited 2020 Jul 28]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK550604/. [PubMed] [Google Scholar]
- 5.He W, Goodkind D, Kowal P; US Bureau of the Census. An aging world: 2015. United States Census Bureau; 2016. [Google Scholar]
- 6.Canadian Institute for Health Information. Seniors and the health care system: what is the impact of multiple chronic conditions? [internet]. 2011 [cited 2021 Oct 5]. Available from: https://secure.cihi.ca/free_products/air-chronic_disease_aib_en.pdf. [Google Scholar]
- 7.Blomqvist A, Busby C. Paying for the boomers: long-term care and intergenerational equity [internet]. Rochester, NY: Social Science Research Network; 2014 [cited 2018 Mar 4]. Available from: https://papers.ssrn.com/abstract=2498537. [Google Scholar]
- 8.Morley JE, Vellas B, Abellan van Kan G, Anker SD, Bauer JM, Bernabei R, et al. Frailty consensus: a call to action. J Am Med Dir Assoc 2013;14 (6):392–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bjornsdottir K. ‘Holding on to life’: an ethnographic study of living well at home in old age. Nurs Inq 2018;25 (2):e12228. [DOI] [PubMed] [Google Scholar]
- 10.Puts MTE, Shekary N, Widdershoven G, Heldens J, Lips P, Deeg DJH. What does quality of life mean to older frail and non-frail community-dwelling adults in the Netherlands? Qual Life Res 2007;16 (2):263–277. [DOI] [PubMed] [Google Scholar]
- 11.Canadian Home Care Association. Portraits of home care in Canada. Ottawa: Canadian Home Care Association; 2013. [Google Scholar]
- 12.Aliberti MJR, Cenzer IS, Smith AK, Lee SJ, Yaffe K, Covinsky KE. Assessing risk for adverse outcomes in older adults: the need to include both physical frailty and cognition. J Am Geriatr Soc 2019;67 (3):477–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harrison JK, Clegg A, Conroy SP, Young J. Managing frailty as a long-term condition. Age Ageing 2015;44 (5):732–735. [DOI] [PubMed] [Google Scholar]
- 14.Muscedere J, Andrew MK, Bagshaw SM, Estabrooks C, Hogan D, Holroyd-Leduc J, et al. Screening for frailty in Canada's health care system: a time for action. Can J Aging Rev Can Vieil 2016;35 (03):281–297. [DOI] [PubMed] [Google Scholar]
- 15.Andrew MK, Dupuis-Blanchard S, Maxwell C, Giguere A, Keefe J, Rockwood K, et al. Social and societal implications of frailty, including impact on Canadian healthcare systems. J Frailty Aging 2018;7 (4):217–223. [DOI] [PubMed] [Google Scholar]
- 16.Keating NC, Fast JE, Lero DS, Lucas SJ, Eales J. A taxonomy of the economic costs of family care to adults. J Econ Ageing 2014;3: ((Suppl C)): 11–20. [Google Scholar]
- 17.Roy N, Dubé R, Després C, Freitas A, Légaré F. Choosing between staying at home or moving: a systematic review of factors influencing housing decisions among frail older adults. PLoS One 2018;13 (1):e0189266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dalmer NK. A logic of choice: problematizing the documentary reality of Canadian aging in place policies. J Aging Stud 2019;48:40–49. [DOI] [PubMed] [Google Scholar]
- 19.Saum K-U, Dieffenbach AK, Müller H, Holleczek B, Hauer K, Brenner H. Frailty prevalence and 10-year survival in community-dwelling older adults: results from the ESTHER cohort study. Eur J Epidemiol 2014;29 (3):171–179. [DOI] [PubMed] [Google Scholar]
- 20.Song X, Mitnitski A, Rockwood K. Prevalence and 10-year outcomes of frailty in older adults in relation to deficit accumulation. J Am Geriatr Soc 2010;58 (4):681–687. [DOI] [PubMed] [Google Scholar]
- 21.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults. J Gerontol A Biol Sci Med Sci 2001;56 (3):M146–M157. [DOI] [PubMed] [Google Scholar]
- 22.Bock J-O, König H-H, Brenner H, Haefeli WE, Quinzler R, Matschinger H, et al. Associations of frailty with health care costs – results of the ESTHER cohort study. BMC Health Serv Res 2016;16:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ensrud KE, Kats AM, Schousboe JT, Taylor BC, Cawthon PM, Hillier TA, et al. Frailty phenotype and healthcare costs and utilization in older women. J Am Geriatr Soc 2018;66 (7):1276–1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc 2012;60 (8):1487–1492. [DOI] [PubMed] [Google Scholar]
- 25.Kanters DM, Griffith LE, Hogan DB, Richardson J, Patterson C, Raina P. Assessing the measurement properties of a Frailty Index across the age spectrum in the Canadian Longitudinal Study on Aging. J Epidemiol Community Health 2017;71 (8):794–799. [DOI] [PubMed] [Google Scholar]
- 26.He B, Ma Y, Wang C, Jiang M, Geng C, Chang X, et al. Prevalence and risk factors for frailty among community-dwelling older people in China: a systematic review and meta-analysis. J Nutr Health Aging 2019;23 (5):442–450. [DOI] [PubMed] [Google Scholar]
- 27.Piette JD, Heisler M, Wagner TH. Problems paying out-of-pocket medication costs among older adults with diabetes. Diabetes Care 2004;27 (2):384–391. [DOI] [PubMed] [Google Scholar]
- 28.Essue B, Kelly P, Roberts M, Leeder S, Jan S. We can’t afford my chronic illness! The out-of-pocket burden associated with managing chronic obstructive pulmonary disease in western Sydney, Australia. J Health Serv Res Policy 2011;16 (4):226–231. [DOI] [PubMed] [Google Scholar]
- 29.Pisu M, Azuero A, McNees P, Burkhardt J, Benz R, Meneses K. The out of pocket cost of breast cancer survivors: a review. J Cancer Surviv 2010;4 (3):202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goldsmith LJ, Kolhatkar A, Popowich D, Holbrook AM, Morgan SG, Law MR. Understanding the patient experience of cost-related non-adherence to prescription medications through typology development and application. Soc Sci Med 2017;194:51–59. [DOI] [PubMed] [Google Scholar]
- 31.Johnson RW, Mommaerts C. Will health care costs bankrupt aging boomers? [internet] 2010 [cited 2021 Oct 5]. Available from: https://www.urban.org/sites/default/files/publication/28361/412026-Will-Health-Care-Costs-Bankrupt-Aging-Boomers-.PDF. [Google Scholar]
- 32.Gomersall JS, Jadotte YT, Xue Y, Lockwood S, Riddle D, Preda A. Conducting systematic reviews of economic evaluations. Int J Evid Based Healthc 2015;13 (3):170. [DOI] [PubMed] [Google Scholar]
- 33.Looman WM, Huijsman R, Fabbricotti IN. The (cost-)effectiveness of preventive, integrated care for community-dwelling frail older people:a systematic review. Health Soc Care Community 2019;27 (1):1–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Apóstolo J, Cooke R, Bobrowicz-Campos E, Santana S, Marcucci M, Cano A, et al. Effectiveness of the interventions in preventing the progression of pre-frailty and frailty in older adults: a systematic review protocol [internet]. PROSPERO; 2018 [cited 2021 Oct 5]. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=35492. [DOI] [PubMed] [Google Scholar]
- 35.Young C, Hall AM, Gonçalves-Bradley DC, Quinn TJ, Hooft L, van Munster BC, et al. Home or foster home care versus institutional long-term care for functionally dependent older people. Cochrane Database Syst Rev 2017; (4):CD009844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Regional Health Council. Frailty in elderly people: clinical practice guidelines [internet]. Florence, Italy: Regione Toscana, Consiglio Sanitario Regionale; 2013 [cited 2020 Jun 19]. Available from: https://www.guidelinecentral.com/summaries/frailty-in-elderly-people/#section-424. [Google Scholar]
- 37.Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc 2015;13 (3):141–146. [DOI] [PubMed] [Google Scholar]
- 38.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8 (1):19–32. [Google Scholar]
- 39.Government of Canada; Canadian Institutes of Health Research. Patient engagement - CIHR [internet]. 2012 [cited 2019 Nov 7]. Available from: http://www.cihr-irsc.gc.ca/e/45851.html. [Google Scholar]
- 40.Bendixen RM, Mann WC, Tomita M. The relationship of home range to functional status and cognitive status of frail elders. Phys Occup Ther Geriatr 2005;23 (2–3):43–62. [Google Scholar]
- 41.Choi NG, Kim J, Asseff J. Self-neglect and neglect of vulnerable older adults: reexamination of etiology. J Gerontol Soc Work 2009;52 (2):171–187. [DOI] [PubMed] [Google Scholar]
- 42.Clark DO, Frankel RM, Morgan DL, Ricketts G, Bair MJ, Nyland KA, et al. The meaning and significance of self-management among socioeconomically vulnerable older adults. J Gerontol B Psychol Sci Soc Sci 2008;63 (5):S312–S319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Colling J, Owen TR, McCreedy M, Newman D. The effects of a continence program on frail community-dwelling elderly persons. Urol Nurs 2003;23 (2):117–131. [PubMed] [Google Scholar]
- 44.Dellasega CA, Fisher KM. Posthospital home care for frail older adults in rural locations. J Community Health Nurs 2001;18 (4):247–260. [DOI] [PubMed] [Google Scholar]
- 45.Freedman VA, Spillman BC. Disability and care needs among older Americans. Milbank Q 2014;92 (3):509–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Klein D, Turvey C, Wallace R. Elders who delay medication because of cost: health insurance, demographic, health, and financial correlates. Gerontologist 2004;44 (6):779–787. [DOI] [PubMed] [Google Scholar]
- 47.Leutz WN, Capitman J, Green CA. A limited entitlement for community care: how members use services. J Aging Soc Policy 2001;12 (3):43–64. [DOI] [PubMed] [Google Scholar]
- 48.Meng H, Friedman B, Dick AW, Wamsley BR, Eggert GM, Mukamel D. Effect of a voucher benefit on the demand for paid personal assistance. Gerontologist 2006;46 (2):183–192. [DOI] [PubMed] [Google Scholar]
- 49.Moon M, Hollin IL, Nicholas LH, Schoen C, Davis K. Serving older adults with complex care needs: a new benefit option for Medicare. Issue Brief (Commonw Fund) 2015;23:1–11. [PubMed] [Google Scholar]
- 50.Moore MJ, Zhu CW, Clipp EC. Informal costs of dementia care: estimates from the National Longitudinal Caregiver Study. J Gerontol B Psychol Sci Soc Sci 2001;56 (4):S219–S228. [DOI] [PubMed] [Google Scholar]
- 51.O’Keeffe J, Long SK, Liu K, Kerr M. How do they manage? Disabled elderly persons in the community who are not receiving Medicaid long-term care services. Home Health Care Serv Q 2001;20 (4):73–90. [DOI] [PubMed] [Google Scholar]
- 52.Sambamoorthi U, Shea D, Crystal S. Total and out-of-pocket expenditures for prescription drugs among older persons. Gerontologist 2003;43 (3):345–359. [DOI] [PubMed] [Google Scholar]
- 53.Schoenberg NE, Kim H, Edwards W, Fleming ST. Burden of common multiple-morbidity constellations on out-of-pocket medical expenditures among older adults. Gerontologist 2007;47 (4):423–437. [DOI] [PubMed] [Google Scholar]
- 54.Schwab TC, Leung K, Gelb E, Meng Y, Cohn J. Home- and community-based alternatives to nursing homes: services and costs to maintain nursing home eligible individuals at home. J Aging Health 2003;15 (2):353–370. [DOI] [PubMed] [Google Scholar]
- 55.Shafir A, Garrigues SK, Schenker Y, Leff B, Neil J, Ritchie C. Homebound patient and caregiver perceptions of quality of care in home-based primary care: a qualitative study. J Am Geriatr Soc 2016;64 (8):1622–1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sharkey JR, Ory MG, Browne BA. Determinants of self-management strategies to reduce out-of-pocket prescription medication expense in homebound older people. J Am Geriatr Soc 2005;53 (4):666–674. [DOI] [PubMed] [Google Scholar]
- 57.Taylor DH, Schenkman M, Zhou J, Sloan FA. The relative effect of Alzheimer's disease and related dementias, disability, and comorbidities on cost of care for elderly persons. J Gerontol - Ser B Psychol Sci Soc Sci 2001;56 (5):S285–S293. [DOI] [PubMed] [Google Scholar]
- 58.Barken R. Reconciling tensions: needing formal and family/friend care but feeling like a burden. Can J Aging 2017;36 (1):81–96. [DOI] [PubMed] [Google Scholar]
- 59.Barken R. ‘Independence’ among older people receiving support at home: the meaning of daily care practices. Ageing Soc 2019;39 (3):518–540. [Google Scholar]
- 60.Béland F, Bergman H, Lebel P, Clarfield AM, Tousignant P, Contandriopoulos A-P, et al. A system of integrated care for older persons with disabilities in Canada: results from a randomized controlled trial. J Gerontol Ser A 2006;61 (4):367–373. [DOI] [PubMed] [Google Scholar]
- 61.Dosman D, Keating N. Cheaper for whom? Costs experienced by formal caregivers in adult family living programs. J Aging Soc Policy 2005;17 (2):67–83. [DOI] [PubMed] [Google Scholar]
- 62.Ploeg J, Matthew-Maich N, Fraser K, Dufour S, McAiney C, Kaasalainen S, et al. Managing multiple chronic conditions in the community: a Canadian qualitative study of the experiences of older adults, family caregivers and healthcare providers. BMC Geriatr 2017;17 (1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ploeg J, Canesi M, Fraser KD, McAiney C, Kaasalainen S, Markle-Reid M, et al. Experiences of community-dwelling older adults living with multiple chronic conditions: a qualitative study. BMJ Open 2019;9 (3): [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Parker SG, Oliver P, Pennington M, Bond J, Jagger C, Enderby PM, et al. Rehabilitation of older patients: day hospital compared with rehabilitation at home. A randomised controlled trial. Health Technol Assess 2009;13 (39):ix–168. [DOI] [PubMed] [Google Scholar]
- 65.Flood C, Mugford M, Stewart S, Harvey I, Poland F, Lloyd-Smith W. Occupational therapy compared with social work assessment for older people. An economic evaluation alongside the CAMELOT randomised controlled trial. Age Ageing 2005;34 (1):47–52. [DOI] [PubMed] [Google Scholar]
- 66.Hanratty B, Jacoby A, Whitehead M. Socioeconomic differences in service use, payment and receipt of illness-related benefits in the last year of life: findings from the British Household Panel Survey. Palliat Med 2008;22 (3):248–255. [DOI] [PubMed] [Google Scholar]
- 67.Nakabe T, Sasaki N, Uematsu H, Kunisawa S, Wimo A, Imanaka Y. Classification tree model of the personal economic burden of dementia care by related factors of both people with dementia and caregivers in Japan: a cross-sectional online survey. BMJ Open 2019;9 (7):e026733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Washio M, Yoshida H, Ura N, Ohnishi H, Togashi N, Sakauchi F, et al. Burden among family caregivers of patients on chronic hemodialysis in Northern Japan. Int Med J 2012;19 (3):221–223. [Google Scholar]
- 69.Cassells C, Watt E. The impact of incontinence on older spousal caregivers. J Adv Nurs 2003;42 (6):607–616. [DOI] [PubMed] [Google Scholar]
- 70.Veras RP, Caldas CP, Dantas SB, Sancho LG, Sicsú B, Motta LB. Demented elderly people living at home in Rio de Janeiro, Brazil: evaluation of expenditure on care. Psychogeriatrics 2008;8 (2):88–95. [Google Scholar]
- 71.Liu X, Lu B, Feng Z. Intergenerational transfers and informal care for disabled elderly persons in China: evidence from CHARLS. Health Soc Care Community 2017;25 (4):1364–1374. [DOI] [PubMed] [Google Scholar]
- 72.Stuart M, Hansen EB. Danish home care policy and the family: implications for the United States. J Aging Soc Policy 2006;18 (3–4):27–42. [DOI] [PubMed] [Google Scholar]
- 73.Ayalon L, Kaniel M, Rosenberg L. Social workers’ perspectives on care arrangements between vulnerable elders and foreign home care workers: lessons from Israeli/Filipino caregiving arrangements. Home Health Care Serv Q 2008;27 (2):121–142. [DOI] [PubMed] [Google Scholar]
- 74.Degiuli F. The burden of long-term care: how Italian family care-givers become employers. Ageing Soc 2010;30 (5):755–777. [Google Scholar]
- 75.de Craen AJM, Westendorp RGJ, Willems CG, Buskens ICM, Gussekloo J. Assistive devices and community-based services among 85-year-old community-dwelling elderly in The Netherlands: ownership, use, and need for intervention. Disabil Rehabil Assist Technol 2006;1 (3):199–203. [DOI] [PubMed] [Google Scholar]
- 76.Kurpas D, Gwyther H, Szwamel K, Shaw RL, D’Avanzo B, Holland CA, et al. Patient-centred access to health care: a framework analysis of the care interface for frail older adults. BMC Geriatr 2018;18 (1):273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Brandão D, Ribeiro O, Oliveira M, Paúl C. Caring for a centenarian parent: an exploratory study on role strains and psychological distress. Scand J Caring Sci 2017;31 (4):984–994. [DOI] [PubMed] [Google Scholar]
- 78.Suen J, Thang LL. Contextual challenges and the mosaic of support: understanding the vulnerabilities of low-income informal caregivers of dependent elders in Singapore. J Cross-Cult Gerontol 2018;33 (2):163–181. [DOI] [PubMed] [Google Scholar]
- 79.Son JH, Kim SY, Won CW, Choi HR, Kim BS, Park MS. Physical frailty predicts medical expenses in community-dwelling, elderly patients: three-year prospective findings from living profiles of older people surveys in Korea. Eur Geriatr Med 2015;6 (5):412–416. [Google Scholar]
- 80.Lien Y-F, Huang H-M. Challenges in intergenerational caregiving for frail older people: a multiple case study. Nurs Health Sci 2017;19 (1):81–87. [DOI] [PubMed] [Google Scholar]
- 81.Zencir M, Kuzu N, Beser NG, Ergin A, Catak B, Sahiner T. Cost of Alzheimer's disease in a developing country setting. Int J Geriatr Psychiatry 2005;20 (7):616–622. [DOI] [PubMed] [Google Scholar]
- 82.Parker JM, Hill MN. A review of advanced practice nursing in the United States, Canada, Australia and Hong Kong Special Administrative Region (SAR), China. Int J Nurs Sci 2017;4 (2):196–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Provencher V, Carbonneau H, Levasseur M, Poulin V, Filiatrault J, Giroux D, et al. Exploring the impact of a new intervention to increase participation of frail older adults in meaningful leisure activities. Act Adapt Aging 2018;42 (1):1–18. [Google Scholar]
- 84.Patricia M, Simone, Amie L Haas. Frailty, leisure activity and functional status in older adults: relationship with subjective well being. Clin Gerontol 2013;36 (4):275–293. [Google Scholar]
- 85.World Health Organization. Monitoring sustainable development goals–indicator 3.8.2 [Internet]. World Health Organization; n.d. [cited 2020 Aug 28]. Available from: https://www.who.int/data/gho/data/themes/topics/indicator-groups/indicator-group-details/GHO/sdg-target-3.8-achieve-universal-health-coverage-(uhc)-including-financial-risk-protection. [Google Scholar]