Abstract
Background
Traditional treatment methods for haemorrhoids fall into two broad groups: less invasive techniques including rubber band ligation (RBL), which tend to produce minimal pain, and the more radical techniques like excisional haemorrhoidectomy (EH), which are inherently more painful. For decades, innovations in the field of haemorrhoidal treatment have centred on modifying the traditional methods to achieve a minimally invasive, less painful procedure and yet with a more sustainable result. The availability of newer techniques has reopened debate on the roles of traditional treatment options for haemorrhoids.
Objectives
To review the efficacy and safety of the two most popular conventional methods of haemorrhoidal treatment, rubber band ligation and excisional haemorrhoidectomy. The original study has now been up dated using the same search strategy.
Search methods
We searched MEDLINE, EMBASE, CENTRAL, and CINAHL October 2010
Selection criteria
Randomised controlled trials comparing rubber band ligation with excisional haemorrhoidectomy for symptomatic haemorrhoids in adult human patients were included.
Data collection and analysis
We extracted data on to previously designed data extraction sheet. Dichtomous data were presented as relative risk and 95% confidence intervals, and continuous outcomes as weighted mean difference and 95% confidence intervals.
Main results
Three trials (of poor methodological quality) met the inclusion criteria. Complete remission of haemorrhoidal symptom was better with excisional haemorrhoidectomy (EH) (three studies, 202 patients, RR 1.68, 95% CI 1.00 to 2.83). There was significant heterogeneity between the studies (I2 = 90.5%; P = 0.0001). Similar analysis based on the grading of haemorrhoids revealed the superiority of EH over RBL for grade III haemorrhoids (prolapse that needs manual reduction) (two trials, 116 patients, RR 1.23, CI 1.04 to 1.45; P = 0.01). However, no significant difference was noticed in grade II haemorrhoids (prolapse that reduces spontaneously on cessation of straining) (one trial, 32 patients, RR 1.07, CI 0.94 to 1.21; P = 0.32) Fewer patients required re‐treatment after EH (three trials, RR 0.20 CI 0.09 to 0.40; P < 0.00001). Patients undergoing EH were at significantly higher risk of postoperative pain (three trials, fixed effect; 212 patients, RR 1.94, 95% CI 1.62 to 2.33, P < 0.00001). The overall delayed complication rate showed significant difference (P = 0.03) (three trials, 204 patients, RR 6.32, CI 1.15 to 34.89) between the two interventions.
Authors' conclusions
The present systematic review confirms the long‐term efficacy of EH, at least for grade III haemorrhoids, compared to the less invasive technique of RBL but at the expense of increased pain, higher complications and more time off work. However, despite these disadvantages of EH, patient satisfaction and patient's acceptance of the treatment modalities seems to be similar following both the techniques implying patient's preference for complete long‐term cure of symptoms and possibly less concern for minor complications. So, RBL can be adopted as the choice of treatment for grade II haemorrhoids with similar results but with out the side effects of EH while reserving EH for grade III haemorrhoids or recurrence after RBL. More robust study is required to make definitive conclusions.
One additional study was identified from the updated search (Ali 2005). However, after careful review and discussion among the authors, it was decided that this study did not meet the necessary criteria for including in the analysis. Hence, the results and conclusion remains the same.
Plain language summary
This review compares the safety and effectiveness of two of the most popular treatments for haemorrhoids, rubber band ligation (RBL) and excisional haemorrhoidectomy (EH).
When conservative treatments like change of diet or ointments do not help, people usually see a doctor for haemorrhoid removal. RBL involves placing rubber bands around haemorrhoids until they eventually fall off. There are other nonsurgical treatments for haemorrhoids but RBL is often considered the best. For more severe haemorrhoids surgical removal of the haemorrhoids (EH) may be necessary. Although it is very effective, it is more painful and invasive. This review is based upon three randomised controlled trials comparing RBL with EH, with a total of 216 patients. The trials showed that with EH, haemorrhoids did not come back as often as with RBL. EH was better for advanced haemorrhoids, known as grade III haemorrhoids. For less severe grade II haemorrhoids, RBL and EH were equally effective. EH caused more pain after the procedure, more minor complications, and required more time off work. Patient satisfaction was similar for both treatments.
This review has been up dated as of October 2010 and the search was carried out with previously used search strategy to identify any possible new randomised controlled study to include in the statistics. Only one additional paper was identified with a potential possibility to include in the study (Ali 2005). However, after a combined common decision from all the authors, it was decided to exclude the paper for the statistics because of the poor data presentation and randomisation method. After up to date search, the conclusion has not changed and the review authors conclude that RBL should be the primary treatment used for grade II haemorrhoids, and EH reserved for patients who failed after repeated RBL or grade III haemorrhoids. They recommend more research be done comparing these techniques with the many newer ones, especially stapled haemorrhoidopexy, to determine which treatment is best.
Background
Haemorrhoidal disease is ranked first amongst diseases of the rectum and large intestine, and the estimated worldwide prevalence ranges from 2.9% to 27.9%, of which more than 4% are symptomatic (Johanson 1990; Rogozina 2002). Approximately, one third of these patients seek physicians for advice. Age distribution demonstrates a Gaussian distribution with a peak incidence between 45 and 65 years with subsequent decline after 65 years (Johanson 1990; Parks 1955). Men are more frequently affected than women (Keighley 1993). The anorectal vascular cushions along with the internal anal sphincter are essential in the maintenance of continence by providing soft tissue support and keeping the anal canal closed tightly. Haemorrhoids are considered to be due to the downward displacement of these vascular cushions due to the disruption of the supporting suspensory (Treitz) muscle (Haas 1984; Thomson 1975). The haemorrhoidal symptoms may be precipitated by various factors including low fibre diet, prolonged straining, constipation, diarrhoea and hard stool (Haas 1984; Thaha 2002). Haemorrhoidal symptoms may vary from bleeding per rectum, prolapse of the haemorrhoidal cushions, pain from thrombosis, discomfort from itching, mucous discharge and incontinence especially of fluids. Based on the degree of prolapse, haemorrhoids are classified into four categories: first degree being non‐prolapsing, second degree prolapsing on straining with spontaneous reduction, third degree prolapsing on straining and requiring manual reduction while, fourth degree haemorrhoids are permanently prolapsed. The severity of symptoms does not necessarily correlate with the degree of haemorrhoids. The treatment options for symptomatic haemorrhoids have varied over time. Measures have included conservative medical management, non‐surgical treatments and various surgical techniques including stapled haemorrhoidopexy. Advice regarding high fibre diet and bulk forming agents are some of the medical interventions, which may be effective in the prevention of constipation and sequelae of haemorrhoids (Brisinda 2000; Nisar 2003). In addition, numerous commercial ointment preparations are available for symptomatic treatment but with little objective evidence of their efficacy (Nisar 2003), as well as phlebotonics such as Flavonoids. The various non‐surgical treatments include rubber band ligation (RBL), injection sclerotherapy, cryotherapy, infrared coagulation, laser therapy and diathermy coagulation; all of which may be performed as out patient procedures without anaesthesia. These non‐surgical methods are considered to be the primary option for grades one to three (grade I‐III) haemorrhoids (MacRae 1995). Of all the non‐surgical procedures, rubber band ligation seems to be the best option in terms of compliance, long‐term efficacy and side effects (MacRae 1995). Rubber band ligation (RBL) is a quick, simple, inexpensive outpatient procedure, which was originally introduced by Blaisdell (Blaisdell 1958) and later modified by Barron (Barron 1963). The rubber bands are applied on an insensitive area just above the dentate line, preferably, up to three bands in one sitting, which can be safely repeated after 4‐6 weeks time. Different techniques are practiced for application of bands including the endoscopic ligation but the commonest being the suction method. The patient should be cautioned about bleeding after 10‐14 days when the banded haemorrhoid sloughs off. The success rate of ligation treatment varies between 69% and 94% among different studies (Bat 1993). RBL is associated with a low complication rate (less than 2%) (Sardinha 2002). It may range from vaso‐vagal syncope, anal pain, minor bleeding, chronic ulcer, priapism, difficulty in urination, thrombosis of external haemorrhoids, to life threatening complications such as massive bleeding, pelvis sepsis (Barwell 1999; Bat 1993). If conservative measures fail to control symptoms, patients may be referred to a surgeon for operative management. The indications for the surgical treatment include the presence of a significant external component, hypertrophied papillae, associated fissure, extensive thrombosis or recurrence of symptoms after repeated RBL. The technique employed may be open (Milligan ‐Morgan) or closed (Ferguson) and the instruments used are scalpel, scissor, electrocautery or laser. Milligan‐Morgan haemorrhoidectomy is the gold standard and frequently performed procedure in the United Kingdom (Manson 2002). Post haemorrhoidectomy pain is the commonest problem associated with the surgical techniques. The other early complications are urinary retention (20.1%), bleeding (secondary or reactionary) (2.4% ‐ 6%) and subcutaneous abscess (0.5%). The long‐term complications include anal fissure (1% ‐2.6%), anal stenosis (1%), incontinence (0.4%), fistula (0.5%) and recurrence of haemorrhoids (Bleday 1992; Sardinha 2002). A new alternative to heamorrhoidectomy is the stapled haemorrhoidopexy, introduced by Longo in 1998 (Longo 1998). In this operative technique, the vascular cushions are repositioned to their original site using a circular stapling device, by excising a circular strip of lower rectal mucosa. The long‐term results of this procedure are still awaited. In spite of the availability of different treatment options, rubber band ligation and surgical haemorrhoidectomy are currently practised non‐surgical and surgical methods, respectively.
Objectives
This review evaluated the available evidence from randomised controlled trials comparing the two most commonly employed techniques for the treatment of symptomatic haemorrhoids, namely rubber band ligation and excisional haemorrhoidectomy with a view to ascertaining the optimal traditional treatment technique. The primary aim of this review was to compare the therapeutic efficacy (both short and long‐term) of rubber band ligation and excision haemorrhoidectomy with respect to symptom control. In addition, post‐procedure pain, days to return to work, re‐treatment rate, continence, reported complication rate, patient satisfaction and quality of life scores associated with each procedure were evaluated.
Methods
Criteria for considering studies for this review
Types of studies
We included all published randomised controlled trials comparing rubber band ligation with any form of excisional haemorrhoidectomy were included for the study. Different methods of excisional haemorrhoidectomies, irrespective of the instrument used for excision, and the status of the wound at the end of the procedure (closed or open) were eligible for inclusion if they were compared with rubber band ligation. Length of follow up was not an exclusion criteria. Randomised studies published as abstracts were included if the full version of the same was available from the authors. Quasi‐randomised, non‐randomised studies, letters and also studies comparing rubber band ligation with any non‐surgical treatment were excluded. Arrangement was in place for translation of eligible papers from other languages using available resources.
Types of participants
All patients with symptomatic haemorrhoids of any grade, without distinction for age, gender or gestation, undergoing rubber band ligation or excisional haemorrhoidectomy within a randomised controlled setting were the target patients for comparison of outcome measures.
Types of interventions
Rubber band ligation and excisional haemorrhoidectomy were the interventions included. Target interventions were any types of excisional haemorrhoidectomy, such as open, semi‐closed or closed procedures. The type of instrument used for excision nor the number of rubber bands applied was also not an exclusion criterion.
Types of outcome measures
Haemorrhoidal symptom control was the primary outcome measure addressed in this review. Duration of post procedural pain, time to return to normal activities, re‐treatment rate, patient satisfaction, and complications (incontinence, anal stenosis, sepsis, significant bleeding requiring readmission for further treatment) for each procedures were considered as secondary outcome measures. Complications were analysed and reported individually. In addition, they were indexed as either early (urinary retention, post operative haemorrhage, acute anal fissure) or delayed complications (anal stenosis, flatus incontinence, low back pain, skin bridge across anus), and reported separately as relative risk (RR) with 95% confidence interval (CI). Quality of life was also included if recorded. Authors were contacted for any missing details. Reports of symptom control may differ between studies based on the different symptoms, and can be expected to range from individual symptom analysis to overall scoring systems. To obtain a uniform report, these were categorised into a dichotomous output as described below: Cured or improved: Symptom free or mild residual symptoms but not requiring further treatment at the end of study period Unchanged or worse: No symptom improvement and requiring further intervention or suffered complication or deterioration of symptoms Common individual symptoms such as bleeding, prolapse, pain, itching, urgency and mucous discharge were considered for analysis if they were published. If interpretation of results from a published paper was too difficult, we contacted the study authors to clarify the presented data. In addition, we calculated and compared the duration of post procedural pain and re‐treatment rate for each procedure. Quality of life score was considered and commented on if reported in the study.
Search methods for identification of studies
ELECTRONIC SEARCHES: We adopted the search strategy advocated by Cochrane Colorectal Cancer Goup (CCCG). A comprehensive search of different electronic databases using a combination of free text and MESH (Medical Subject Heading) terms was undertaken to identify potential studies for inclusion in the review. The following electronic databases were searched for any trials comparing the two interventions: The Cochrane Central Register of Controlled Trials (CENTRAL), The Cochrane Library 2010 issue 9.
MEDLINE / PubMed (Searched October 2010) 1 controlled clinical trial.pt. 2 randomised controlled trial.pt. 3 randomised controlled trials/ 4 random allocation/ 5 double blind method/ 6 single blind method/ 7 or/1‐6 8 animals/not (animals/ and human/) 9 #7 not 8 10 clinical trial.pt. 11 exp clinical trials/ 12 random$.tw. 13 research design/ 14 (clin$ adj25 trial$).tw. 15 ((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).tw. 16 factorial.tw. 17 (balance$ adj2 block$).tw. 18 animals/ not (animals/ and human/) 19 or/10‐17 20 #19 not 18 21 exp HEMORRHOIDS/ 22 (hemorrhoid$ or haemorrhoid$).mp. 23 piles.mp. 24 or/21‐23 25 exp surgical procedures, operative/ or exp ligation 26 rubber band.mp. 27 ligature.mp. 28 diathermy.mp. or DIATHERMY/ 29 Milligan Morgan.mp. or Surgical/ 30 Ferguson.mp. or surgical/ 31 Digestive System Surgical Procedures/ or Milligan Morgan.mp. or Surgical/ 32 (haemorrhoidectom$ or hemorrhoidectom$).mp. 33 ligasure.mp. 34 laser.mp. or LASERS/ 35 electrocautery.mp. or Electrocoagulation/ 36 thermocoagulation.mp. 37 or/25‐36 38 #9 and 20 and 37
EMBASE (Searched October 2010) 1.exp clinical trial/ 2.comparative study/ 3.major clinical study/ 4.randomization/ 5.double blind procedure/ 6.single blind procedure/ 7.prospective study/ 8.((clinical or controlled or comparative or placebo or prospective or randomi#ed) adj3 (trial or study)).ti,ab. 9.(random$ adj7 (allocat$ or allot$ or assign$ or basis$ or divid$ or order$)).ti,ab. 10.((singl$ or doubl$ or trebl$ or tripl$) adj7 (blind$ or mask$)).ti,ab. 11.or/1‐10 12. animals/not (animals/ and human/) 13 #11 not 12 14 exp HEMORRHOIDS/ 15 (hemorrhoid$ or haemorrhoid$).mp. 16 piles.mp. 17 or/14‐16 18 exp surgical procedures, operative/ or exp ligation 19 rubber band.mp. 20 ligature.mp. 21diathermy.mp. or DIATHERMY/ 22 Milligan Morgan.mp. or Surgical/ 23 Ferguson.mp. or surgical/ 24 Digestive System Surgical Procedures/ or Milligan Morgan.mp. or Surgical/ 25 (haemorrhoidectom$ or hemorrhoidectom$).mp. 26 ligasure.mp. 27 laser.mp. or LASERS/ 28 electrocautery.mp. or Electrocoagulation/ 29 thermocoagulation.mp. 30 or/18‐29 31#13 and 17 and 30
CINAHL (Searched October 2010)
ADDITIONAL SEARCHES: Current Controlled Trials (http://controlled‐trials.com/). Ongoing Trials: National Research Register, Current Controlled Trials These were searched for the whole available period up to the most recent update of the databases at the time of the search. Bibliographies of identified papers were also scrutinised for relevant studies. Experts were contacted for advice and peer review, and to identify additional published and unpublished references. Web of Science Proceedings (the Institute for Science Information Proceedings allow access to abstracts from papers delivered at international conferences, symposia, seminars, colloquia, workshops, and conventions), Health Management Information Consortium (HMIC; this database focuses on community care and health systems management in the UK, Europe and developing countries including journals, books, reports, official publications)
Data collection and analysis
Selection of studies The titles and abstracts identified by the searches were screened independently by two authors (VS and AK). Studies that clearly did not meet the inclusion criteria were not considered further. The full text of all other articles were retrieved and further assessed for eligibility by MAT and VS independently in consultation with another author (KLC or RJCS) in case of any conflict. Studies were included if they were randomised controlled trials comparing rubber band ligation with excisional haemorrhoidectomy for symptomatic haemorrhoids in adult humans and had measured any of the stated outcome measures.
Quality assessment VS, AK and KSR independently assessed methodological quality which was carried out using standard criteria looking for: (1) allocation concealment (whether the randomisation method adequately prevented the investigator from influencing the allocation of patients to the experimental interventions); (2) blinding of participants, investigators and outcome assessors; (3) use of intention‐to‐treat analysis; and (4) completeness of follow‐up. When data were missing or incomplete, we requested clarification from the trial authors. No formal scoring was used. Studies were classified into "high", "adequate", or "inadequate" quality. Trials with adequate allocation concealment and adequate blinding, if properly explained, were considered as high quality trials. We contacted authors for missing information before categorising the study into any of the three classes. Data management VS and MAT independently extracted data from all the included studies on to a standardised data extraction form and resolved discrepancies with the third author (KLC). Included studies were analysed for the above methodological quality and for details regarding participants, interventions, comparisons and outcomes. These included studies provided the context for discussing the reliability, internal and external validity and generalisability of results. Data entry was performed by VS and crosschecked by KSR. RJCS and MAL provided expert opinion and reviewed the final manuscript before submission.
Data analysis We used Relative risk (RR) and 95% confidence intervals (CI) to summarise treatment effects when the outcomes were dichotomous and weighted mean difference (WMD) and 95% CI used when the outcome was continuous. The estimates from individual trials were pooled using the DerSimonian and Laird random‐effects model when appropriate (Der Simonian 1986). The Mantel‐Haenszel fixed‐effect model was also computed to evaluate robustness and susceptibility to outliers. Statistical heterogeneity was explored by chi2 test and expressed as I2 and P value (significant if less than 0.05). Limited availability of studies restricted the performance of subgroup analysis except analysing the results for each grade (II and III) of haemorrhoidal disease. We felt that performing sensitivity analysis was not relevant due to limited study numbers. We attempted to assess for publication bias using a funnel plot. All analyses were performed using Review Manager (RevMan) [Computer program]. Version 5.0. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2008. Each outcome category was analysed individually as per the above criteria. When we were unable to combine the outcome measure into single data, descriptive summary of the results were considered. Missing data (withdrawals/dropouts) were analysed by "Available case analysis".
Results
Description of studies
Search results The summary of the search result carried out October 2010 is given in Figure 1. A total of 1360 studies were identified in MEDLINE (n = 413), PubMed (n = 89), EMBASE (n = 764), the Cochrane Central Register for Controlled Trials (n = 4), Controlled Clinical Trials (n = 15), National Research Register (n = 38), CINAHL (n = 35) and trials from bibliography of identified trials (n = 2). Three studies comparing rubber band ligation with excisional haemorrhoidectomy met the inclusion criteria for analysing the results (Cheng 1981; Lewis 1983; Murie 1980). Additional two studies apparently met the inclusion criteria, but were excluded for what it seemed to be a duplicate publication (Murie 1982) and another due to poor data presentation and randomisation method (Ali 2005). Disease control and recurrent disease were mentioned in all three studies but control of individual symptoms including bleeding and prolapse has been accounted in one study (Murie 1980). Again, the treatment outcome based on the grading of haemorrhoid was reported in two of the included studies (Cheng 1981; Murie 1980) and unclear in one (Lewis 1983). All the trials have specified the details of post‐operative pain and significant post‐operative haemorrhage. Cheng et al and Murie et al accounted for the post‐operative urinary retention, anal stenosis and patient satisfaction whereas the latter study also looked into complications including anal fissure and low back pain in addition to the duration of time‐off from work. Incontinence to flatus (Lewis 1983) and faeces (Cheng 1981) were recorded in one study each.
1.
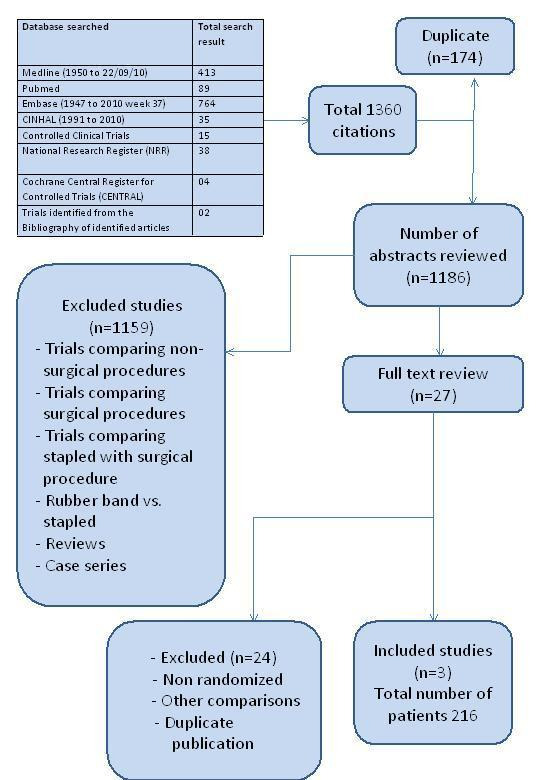
Flow chart for searches October 2010
Risk of bias in included studies
Quality of three included trials (Cheng 1981; Lewis 1983; Murie 1980) was assessed using the above‐mentioned standard criteria. The allocation concealment and blinding of investigator or assessor were not clearly reported, consequently the methodological quality of all the three included studies was considered inadequate (Table 1).
1. Methodological quality of included studies.
| Study | Allocation concealme | Blinding | Intention‐to‐treat | Lost to follow up(%) |
| Murie 1980 | Unclear | None | No | 0 (%) |
| Cheng 1981 | Unclear | None | No | 2 (3.6%) |
| Lewis 1983 | Unclear | None | No | 12 (12%) |
Effects of interventions
A total of 206 patients with varying degree of haemorrhoids were included in the review of which 63 and 58 were male patients in the RBL and EH group, respectively. The symptoms at initial recruitment into the studies are given in (Table 2). The mean duration of symptom ranged between 54 and 94 months under RBL group and, 60 and 112 months under EH among different studies. In total, 14 (15.6 %) of patients were lost to follow‐up. Control of symptoms: Both RBL and EH controlled the symptoms of bleeding (two trials, 123 patients, RR 1.12, 95% CI 0.97 to 1.29; P = 0.12) (Analysis 1.1) and prolapse (two trials, 109 patients, RR 1.05, 95% CI 0.98 to 1.12; P = 0.16) (Analysis 1.2) without significant difference between the two interventions. However, the EH achieved better overall cure rate for haemorrhoidal disease when compared to RBL (Three trials, 202 patients, RR 1.68, CI 1.00 to 2.83; P = 0.05) at the end of the trial period (Analysis 1.3). There was significant heterogeneity (I2 = 90.5%; P < 0.0001 chi2 test) between the studies. Sub group analysis based on the grading of haemorrhoids revealed the superiority of EH over RBL for grade III haemorrhoids (prolapse that needs manual reduction) (two trials, 116 patients, RR 1.23, CI 1.04 to 1.45; P = 0.01) (Analysis 1.4). However, no significant difference was noticed in grade II haemorrhoids (prolapse that reduces spontaneously on cessation of straining) (one trial, 32 patients, RR 1.07, CI 0.94 to 1.21; P = 0.32) (Analysis 1.5).
2. Demographic and symptom details of included studies.
| Study | Country | Number of patients | Age of the patients | Degree of piles | Symptoms | Mean duration of sym | Follow‐up duration |
| RBL EH | Years (Mean / SD) | II III Others | Bleeding Prolapse | Months (Mean / SD) | |||
| RBL EH | RBL EH RBL EH | RBL EH | |||||
| Murie JA 1980 | Great Britain | 50 50 | 53(15) 50(12) | 32 56 12 | 42 42 43 45 | 94(115) 112(104) | 1 year |
| Cheng FCY 1981 | Hong Kong | 30 30 | 40 49 | 60 ‐ ‐ | 20 19 10 11 | 54 60 | 1 year |
| Lewis AAM 1983 | Great Britain | 30 26 | 46(15) 49(13) | ‐ 33 23 | ‐ ‐ ‐ ‐ | 54 60 | 5/52 to 5 years |
| Total | 3 | 110 106 | ‐ ‐ | 92 89 35 | 62 61 53 56 | ‐ ‐ | ‐ |
1.3. Analysis.
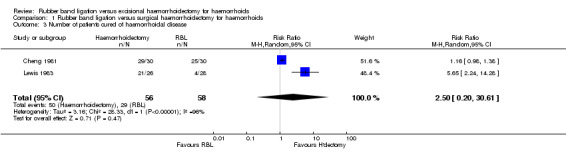
Comparison 1 Rubber band ligation versus surgical haemorrhoidectomy for haemorrhoids, Outcome 3 Number of patients cured of haemorrhoidal disease.
Re‐treatment rate: Meta‐analysis of all the three included studies inveterate a significant difference (P < 0.00001) in the re‐treatment rate favouring EH (three trials, 202 patients, RR 0.20, CI 0.09 to 0.40). Patients treated with EH have only a 20% chance of recurrence compared to RBL (Analysis 1.6). Post‐operative pain: There was significant heterogeneity among the included studies for post operative pain (I2 = 98.6%, P < 0.00001). The fixed‐effect model demonstrated that significantly more patients undergoing EH experienced postoperative pain (P < 0.00001) (three trials, 212 patients, RR 1.94, 95% CI 1.62 to 2.33) (Analysis 1.7). However, the random effects model failed to substantiate the difference (P = 0.37) (three trials, 212 patients, RR 3.11, 95% CI 0.26 to 37.90).
1.6. Analysis.
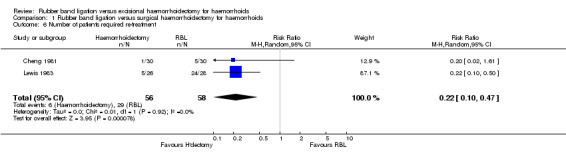
Comparison 1 Rubber band ligation versus surgical haemorrhoidectomy for haemorrhoids, Outcome 6 Number of patients required re‐treatment.
1.7. Analysis.
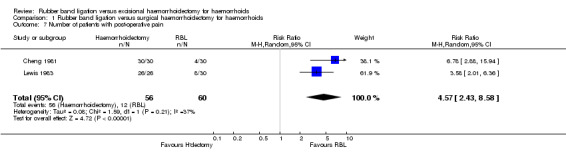
Comparison 1 Rubber band ligation versus surgical haemorrhoidectomy for haemorrhoids, Outcome 7 Number of patients with post‐operative pain.
Complications: There was no statistically significant difference on the incidence of postoperative urinary retention (two trials, 156 patients, RR 3.70, 95% CI 0.62 to 22.08) comparing EH and RBL. Similar results were obtained for postoperative haemorrhage (three trials, 212 patients, RR 3.10, 95% CI 0.63 to 15.30) and anal stenosis (two trials, 148 patients, RR 4.89, 95% CI 0.59 to 40.85) (Analysis 1.8; Analysis 1.9; Analysis 1.10). Murie et al. (Murie 1980) analysed other complications including acute anal fissure (Analysis 1.11), skin bridge across anus (Analysis 1.12) and low back pain (Analysis 1.13). There were no incidence of faecal incontinence with either procedure (Analysis 1.14) but two patients suffered flatus incontinence after EH (Analysis 1.15). Although EH was associated with an overall increase in individual complication rate, the difference did not reach statistical significance (Table 3). However, the overall delayed complication rate showed significant difference (p = 0.03) (three trials, 204 patients, RR 6.32, CI 1.15 ‐34.89) (Analysis 1.16) between the two interventions. This did not achieve significant level for overall early complication rate (Analysis 1.17).
1.8. Analysis.
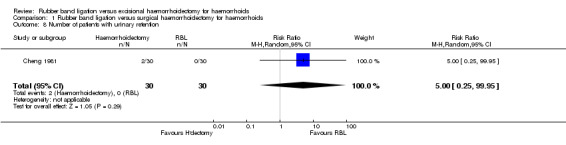
Comparison 1 Rubber band ligation versus surgical haemorrhoidectomy for haemorrhoids, Outcome 8 Number of patients with urinary retention.
1.9. Analysis.
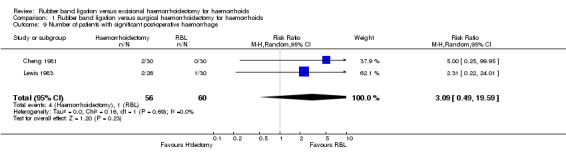
Comparison 1 Rubber band ligation versus surgical haemorrhoidectomy for haemorrhoids, Outcome 9 Number of patients with significant post‐operative haemorrhage.
1.10. Analysis.
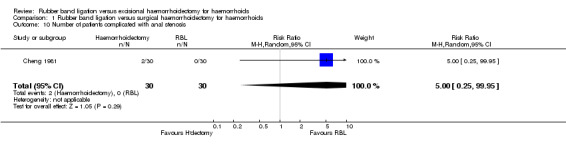
Comparison 1 Rubber band ligation versus surgical haemorrhoidectomy for haemorrhoids, Outcome 10 Number of patients complicated with anal stenosis.
1.14. Analysis.
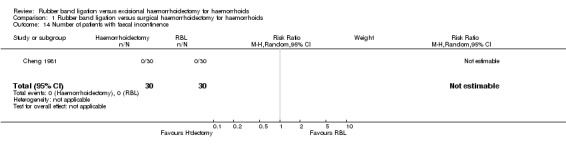
Comparison 1 Rubber band ligation versus surgical haemorrhoidectomy for haemorrhoids, Outcome 14 Number of patients with faecal incontinence.
1.15. Analysis.
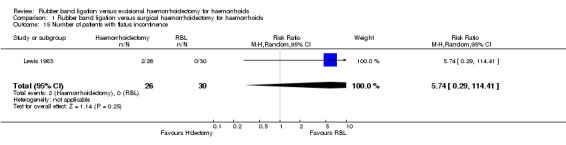
Comparison 1 Rubber band ligation versus surgical haemorrhoidectomy for haemorrhoids, Outcome 15 Number of patients with flatus incontinence.
3. Complications associated with each procedure.
| Complication | Total No. of patient | No.with complication | Relative Risk | P‐value |
| RBL EH | RBL EH | (95% Confidence Interval) | ||
| Urinary retention | 79 77 | 1 5 | 3.70 (0.62 ‐ 22.08) | 0.15 |
| Post‐operative haemorrhage | 109 103 | 1 5 | 3.10 (0.63 ‐ 15.30) | 0.16 |
| Anal stenosis | 73 75 | 0 4 | 4.89 (0.59 ‐ 40.85) | 0.14 |
| Acute anal fissure | 49 47 | 3 0 | 0.15 (0.01 ‐ 2.81) | 0.20 |
| Faecal incontinence | 30 30 | 0 0 | ‐ | ‐ |
| Flatus incontinence | 30 26 | 0 2 | 5.74 (0.29 ‐ 114.41) | 0.25 |
| Skin bridge across anus | 43 45 | 0 1 | 2.87 (0.12 ‐ 68.58) | 0.52 |
| Low back pain | 43 45 | 0 1 | 2.87 (0.12 ‐ 68.58) | 0.52 |
1.16. Analysis.
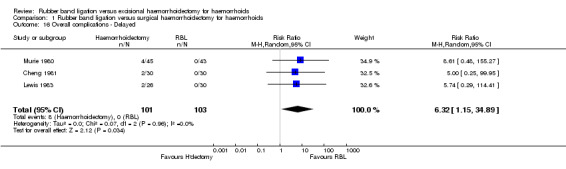
Comparison 1 Rubber band ligation versus surgical haemorrhoidectomy for haemorrhoids, Outcome 16 Overall complications ‐ Delayed.
1.17. Analysis.
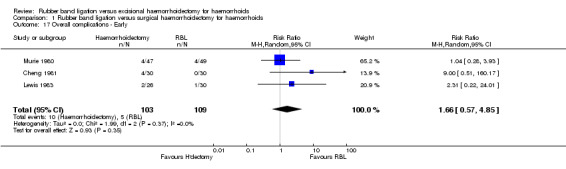
Comparison 1 Rubber band ligation versus surgical haemorrhoidectomy for haemorrhoids, Outcome 17 Overall complications ‐ Early.
Duration of time off work: Murie et al. (Murie 1980) reported the mean number of days time off from work after either treatment. Patients undergoing RBL spent significantly less number of days off work when compared to those undergoing EH (one trial, 68 patients, WMD 29.00, 95% CI 21.24 to 36.76; p < 0.00001) (Analysis 1.18).
Patient satisfaction: The reported overall patient satisfaction was similar for both EH and RBL (two studies, 148 patients, RR 1.02, 95% CI 0.94 to 1.10) (Analysis 1.19). A small proportion of patients following RBL reported a non‐significant difference compared to EH in either total dissatisfaction or lack of improvement (two studies, 73 patients, RR 0.64, 95% CI 0.19 to 2.18, p = 0.48) (Analysis 1.20).
1.19. Analysis.
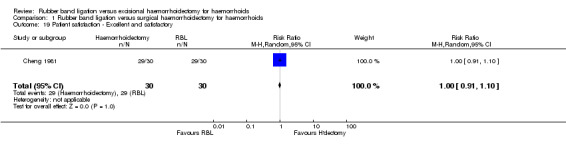
Comparison 1 Rubber band ligation versus surgical haemorrhoidectomy for haemorrhoids, Outcome 19 Patient satisfaction ‐ Excellent and satisfactory.
1.20. Analysis.
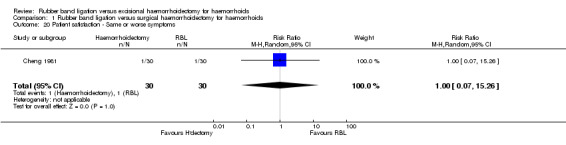
Comparison 1 Rubber band ligation versus surgical haemorrhoidectomy for haemorrhoids, Outcome 20 Patient satisfaction ‐ Same or worse symptoms.
Discussion
The need for treatment for haemorrhoids is primarily based on the subjective perception of severity of symptoms and the assignment of treatment is decided on the traditional classification of haemorrhoids (Goligher 1984), which has little to do with symptom severity. Multiplicity of treatment modalities has added to this confusion. The question of the optimal treatment technique remains unanswered despite most of the techniques in use being subjected to randomised evaluation. For decades, innovations in the field of haemorrhoidal treatment have centred on modifying the traditional methods (RBL and EH) to achieve a minimally invasive, less painful procedure and yet with a more sustainable result. Previous meta‐analyses (MacRae 1995) have concentrated on the disease outcomes of symptom relief, re‐treatment, complications and pain without addressing the equally relevant patient important outcomes. In this systematic review we have expanded on the previous work by including patient satisfaction, duration of time off work, and quality of life following treatment to allow determination of the current status of these techniques. Ability for long‐term control of the haemorrhoidal symptoms is the most obvious measure of success for any treatment method. In this review, fewer than 20% symptom recurrence and significantly fewer re‐treatments supported the efficacy of EH in comparison to RBL. This was particularly more pronounced with grade III haemorrhoids than grade II haemorrhoids. However, this difference was not reproduced when comparing individual symptoms of bleeding and prolapse. Furthermore, none of the three included studies reported on the control of other possible symptoms of haemorrhoids including itching, urgency, mucous discharge and control of perianal leakage, thereby making it difficult to comment on the level of efficacy of the techniques to control these individual symptoms. This information may be relevant in choosing the primary treatment modality given the variability of haemorrhoidal symptoms. Overall safety is of paramount importance when considering a technique to treat any disease especially when advocating a treatment option for a benign disease like haemorrhoids. Apart from control of haemorrhoidal symptoms, post procedure pain, complications and the subsequent disability are important factors based on which patients often decide whether or not to accept any treatment despite troublesome symptoms. Although, in the present study, the number of patients developing delayed postoperative complications was higher following EH, this difference did not reach statistical significance for early complications. None of the included studies have reported any major adverse events although such events have been noted to occur rarely following both these procedures (Bat 1993; Bleday 1992; Lehnhardt 2004). In addition to the patient satisfaction, quality of life and economic consequences, such as loss of productivity (duration of time off work), are also relevant in determining the acceptability of treatment methods. In the present study, two out of the three included trials reported on patient satisfaction with treatment, which was similar following both the methods. One study (Murie 1980) further explored this subject by collating patient's opinion on their willingness to undergo re‐treatment by the same primary method and found non‐significant difference only. Time off work was significantly less following RBL compared to EH in this study, highlighting the potential economic advantage of this less invasive therapy. However, escalating cost of repeated band ligation needs to be considered before any definite conclusion. None of the three included studies formally reported on the quality of life or economic consequences of either treatment.
Authors' conclusions
Implications for practice.
In summary, this systematic review confirms the long‐term efficacy of excisional haemorrhoidectomy (EH), at least for grade III haemorrhoids, compared to the less invasive technique of rubber band ligation (RBL) but at the expense of increased pain, higher complications and more time off work. Despite these disadvantages of EH, patient satisfaction and patient's acceptance of the treatment modalities seems to be similar following both the techniques implying patient's preference for complete long‐term cure of symptoms and possibly less concern for minor complications. Rubber band ligation could be adopted as treatment of choice for grade II haemorrhoids with similar results but with out the side effects of EH while reserving EH for grade III haemorrhoids or recurrent haemorrhoids after RBL. The current conclusion is not changed from the original conclusion as there were no new studies found in the literature since the original review published 2005.
Implications for research.
Health economic evaluation is essential before any definite conclusion can be made because of the increased re‐treatment rate with repeated time‐off from work associated with RBL. More solid data on this aspect of the treatment is required before drawing any definitive conclusion. Since the newer stapled haemorrhoidopexy (SH) may be an alternative to the above standard procedures in terms of cure rate, postoperative pain and early return to work, a meta‐analysis comparing EH with SH incorporating some of the latest major trials could be considered.
What's new
| Date | Event | Description |
|---|---|---|
| 25 October 2010 | New search has been performed | Converted to new review format. |
History
Protocol first published: Issue 4, 2004 Review first published: Issue 3, 2005
| Date | Event | Description |
|---|---|---|
| 25 October 2004 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
We acknowledge the Cochrane Hepato‐biliary group co‐ordinator Mrs Dimitrinka Nikolova, Copenhagen Trial Unit, Copenhagen University Hospital, Copenhagen, for translating one of our papers. We are also thankful to the Cochrane Colorectal Cancer Group for the encouragement and support in completing the work.
Data and analyses
Comparison 1. Rubber band ligation versus surgical haemorrhoidectomy for haemorrhoids.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of patients with control of bleeding | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Number of patients with control or improved prolapse symptom | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number of patients cured of haemorrhoidal disease | 2 | 114 | Risk Ratio (M‐H, Random, 95% CI) | 2.50 [0.20, 30.61] |
| 4 Grade wise disease control (Grade III) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Grade wise disease control (Grade II) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Number of patients required re‐treatment | 2 | 114 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.10, 0.47] |
| 7 Number of patients with post‐operative pain | 2 | 116 | Risk Ratio (M‐H, Random, 95% CI) | 4.57 [2.43, 8.58] |
| 8 Number of patients with urinary retention | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 5.0 [0.25, 99.95] |
| 9 Number of patients with significant post‐operative haemorrhage | 2 | 116 | Risk Ratio (M‐H, Random, 95% CI) | 3.09 [0.49, 19.59] |
| 10 Number of patients complicated with anal stenosis | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 5.0 [0.25, 99.95] |
| 11 Number of patients complicated with acute anal fissure | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Number of patients with skin bridge across anus | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Number of patients complicated with low back pain | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Number of patients with faecal incontinence | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Number of patients with flatus incontinence | 1 | 56 | Risk Ratio (M‐H, Random, 95% CI) | 5.74 [0.29, 114.41] |
| 16 Overall complications ‐ Delayed | 3 | 204 | Risk Ratio (M‐H, Random, 95% CI) | 6.32 [1.15, 34.89] |
| 17 Overall complications ‐ Early | 3 | 212 | Risk Ratio (M‐H, Random, 95% CI) | 1.66 [0.57, 4.85] |
| 18 Duration of time off work | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Patient satisfaction ‐ Excellent and satisfactory | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.91, 1.10] |
| 20 Patient satisfaction ‐ Same or worse symptoms | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.07, 15.26] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Cheng 1981.
| Methods | Study design: Random allocation but method not described Follow‐up: Minimum of 1 year | |
| Participants | 120 patients with grade II haemorrhoids Rubber band ligation (Group A): 14 male, mean age 40 years, duration of symptoms ‐ 54 months Surgical haemorrhoidectomy (Group B): 16 male, mean age 49 years, mean duration of symptoms ‐ 60 months. Other interventions were maximal anal dilatation and injection sclerotherapy | |
| Interventions | Group A (n = 30): Out patient procedure. No premedication or anaesthetic, left lateral position. Forceps to grasp and draw the base of haemorrhoidal tissue above dentate line into the Barron ligator to apply band. Two bands together at one time to each haemorrhoid. Repeated remaining classical haemorrhoid sites. Advised to avoid straining for 2 days after the procedure. Group B (n = 30): In‐patient procedure. General or spinal anaesthesia. Haemorrhoidal tissue dissected free of internal sphincter. Pedicle transfixed and excised. Vaseline gauze dressing in the anal canal. | |
| Outcomes | Number of patients requiring retreatment Number of patients with post operative pain Severity of pain Urinary retention Significant post operative haemorrhage Anal stenosis Faecal incontinence Duration of time off work Length of hospital stay Patient satisfaction | |
| Notes | Study location: Kwong Wah Hospital, Hong Kong Patients/Investigators/Outcome assessors‐Not stated; presumed none Similarity between groups (baseline) ‐ Not stated Funding source ‐ Not stated Completeness to follow‐up: Both groups followed for a minimum of one year Intention to treat analysis: Yes Exclusion criteria ‐ Described | |
Lewis 1983.
| Methods | Study design: Random allocation but method not described Follow‐up: 5 weeks to 5 years | |
| Participants | 112 patients with haemorrhoidal disease Rubber band ligation (Group A): 21 male, mean age of 46+/‐ 15 years, mean duration of symptoms ‐ 54 months, 18 grade III patients and 12 after injection sclerotherapy. Milligan Morgan haemorrhoidectomy (Group B): 13 male, mean age 49+/‐13 years, duration of symptoms ‐ 60 months, 15 grade III patients and 11 recurrent after injection sclerotherapy. Other interventions were cryotherapy using nitrous oxide probe and maximal anal dilatation (Lord's method) | |
| Interventions | Group A (n = 30): Out patient procedure. No premedication or anaesthetic, left lateral position, Forceps to grasp and draw the base of haemorrhoidal tissue above dentate line and Barron ligator to apply band. Maximum of 3 band were applied on 3 occasions at 3 weeks interval unless symptom resolved before completion of the course Group B (n = 26): In‐patient procedure. General or spinal anaesthesia. Haemorrhoidal tissue dissected free of internal sphincter. Pedicle transfixed and excised. Vaseline gauze dressing for the wound | |
| Outcomes | 5 week results: Number of patients with post operative pain Number with significant post operative haemorrhage Flatus incontinence Long term (Median 1‐2 years) results: Number required retreatment Anal stenosis | |
| Notes | Study location: Royal Free Hospital, London, United Kingdom Patients/Investigators/ ‐Not stated; presumed none Outcome assessors ‐ Independent assessor but not sure about the effectiveness of blinding. Similarity between groups (baseline) ‐ Yes Funding source ‐ Peter Samuel fund Completeness to follow‐up: 28 patients from group A and 26 from group B were followed for more than a year. Intention to treat analysis: Yes Exclusion criteria ‐ Described | |
Murie 1980.
| Methods | Study design: Random allocation but method not described Follow‐up: 1 year | |
| Participants | 100 patients with grade II and III haemorrhoidal disease. Rubber band ligation (Group A): 29 male, mean age ‐ 53 +/‐ 15 years, mean duration of symptoms ‐ 94 +/‐ 115 months Surgical haemorrhoidectomy (n = 50) (Group B) ‐28 male, mean age ‐50 +/‐ 12 years, mean duration of symptoms ‐ 112+/‐104 months Patients with associated other anorectal and colonic diseases were excluded | |
| Interventions | Group A (n = 50): Out patient procedure with out premedication or anaesthetic, in left lateral position, forceps to grasp and draw the base of haemorrhoidal tissue, above dentate line, into the Barron ligatior. Two size zero bands applied togather. Repeated at two other classic haemoorhoidal positions at first session. Group B (n = 50): In patient procedure under general or spinal anaesthesia. After preliminary anal stretch haemorrhoidal tissue dissected free of internal sphincter. Pedicle transfixed with chromic catgut and excised. Petroleum jelly gauze dressing into the anal canal. | |
| Outcomes | Post operative pain Urinary retention Significant post operative bleeding Acute anal fissure Anal stenosis Skin bridge across anus Low back pain Number of patients requiring retreatment Total number of retreatments Number of patients off work Duration of time off work Patient satisfaction | |
| Notes | Study location: Western Infirmary, Glasgow, United Kingdom Patients/Investigators/Outcome assessors‐Not stated; presumed none. Similarity between groups (baseline) ‐ Yes Funding source ‐ Not stated Completeness to follow‐up: 43 and 45 in Group A and B, respectively Exclusion criteria ‐ Described | |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adekunle 1984 | Comparison of surgical excision haemorrhoidectomy with diathermy excision |
| Ali 2005 | Poor quality and not a properly conducted controlled randomised study |
| Ambrose 1983 | Comparison of rubber band ligation with photocoagulation |
| Arabi 1977 | Rubber band ligation compared with lateral sphincterotomy |
| Carapeti 1998 | Double‐blind randomised controlled trial of effect of metronidazole on pain after day‐case haemorrhoidectomy |
| Filingeri 2004 | Comparison of two surgical techniques |
| Forster 1996 | Rubber band ligation not compared with surgical haemorrhoidectomy |
| Gartell 1985 | Rubber band ligation compared with sclerotherapy |
| Griffith 1987 | Rubber band ligation compared with contact bipolar diathermy rather than any surgical procedure |
| Hardy 1975 | Comparison between surgical haemorrhoidectomy and anal dilatation |
| Hiltunen 1992 | Surgical haemorrhoidectomy not compared with rubber band ligation |
| Jones 1974 | This study not focussed on the two interventions we are interested |
| Keighley 1979 | Rubber band ligation compared with other non operative methods |
| Lacerda‐Filho 1997 | Compared in‐patient with out‐patient haemorrhoidectomy |
| MacRae 1995 | Meta‐analysis comparing hemorrhoidal treatment modalities |
| Murie 1982 | Duplicate publication of the same data |
| Narro 2004 | Single treatment report for haemorrhoidal artery ligation |
| O'Callaghan 1982 | Milligan‐Morgan haemorrhoidectomy compared cryo surgery and not with rubber band ligation |
| Rasmussen 1991 | Another procedure (Incision of strangulated haemorrhoids) has been done along with rubber band ligation. No like with like comparison |
| Read 1982 | Prospective non‐comparative study |
| Seow‐Choen 1992 | Comparison of scissor excision with diathermy excision |
| Sim 1981 | Rubber band ligation with sclerosant therapy |
| Templeton 1983 | Rubber band ligation compared with infrared coagulation |
| Wehrmann 2004 | Randomised study comparing different modes of application of rubber band |
Contributions of authors
KSR and VS developed search strategy. VS and MAT searched the data base for eligible papers. AK contributed for identifying any potential new papers in the latest version of the review. The full text of all other articles were retrieved and further assessed for eligibility by MAT, AK and VS independently in consultation with a fourth author (KLC). VS and MAT extracted data on to a previously designed data extraction sheet in the original review. Data entry was cross checked by KSR. Methodological quality was assessed by KSR, AK and VS. RJCS and MAL guided the authors by their personal expertise and, reviewed the final draft.
Declarations of interest
None known
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Cheng 1981 {published data only}
- Cheng FCY, Shum DWP, Ong GB. The treatment of second degree haemorrhoids by injection, rubber band ligation, maximal anal dilatation, and haemorrhoidectomy: a prospective clinical trial. Australian and New Zealand journal of surgery 1981;51(5):458‐62. [DOI] [PubMed] [Google Scholar]
Lewis 1983 {published data only}
- Lewis AAM, ROGERS HS, Leighton M. Trial of maximal anal dilatation, cryotherapy and elastic band ligation as alternatives to haemorrhoidectomy in the treatment of large prolapsing haemorrhoids. British Journal of Surgery 1983;70:54‐56. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Murie 1980 {published data only}
- Murie JA, Mackenzie I, Sim AJW. Comparison of rubber band ligation and haemorrhoidectomy for second‐ and third‐degree haemorrhoids: A prospective clinical trial. British Journal of Surgery 1980;67(11):786‐788. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Adekunle 1984 {published data only}
- Adekunle OO, Kolawole JF. A comparative study of excisional surgery and cryohaemorrhoidectomy. African Journal of Medicine & Medical Sciences 1984;13(1‐2):7‐13. [MEDLINE: ] [PubMed] [Google Scholar]
Ali 2005 {published data only}
- Ali U, Khan AS. Rubber Band Ligation versus Open Haemorrhoidectomy: A study of 100 cases. Journal of Postgraduate Medical Institute 2005;19(3):31 7‐22. [Google Scholar]
Ambrose 1983 {published data only}
- Ambrose NS, Hares MM, Alexander‐Williams J, Keighley MR. Prospective randomised comparison of photocoagulation and rubber band ligation in treatment of haemorrhoids.. British Medical Journal Clinical Research Ed. 1983;286(6375):1389‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Arabi 1977 {published data only}
- Arabi Y, Gatehouse D, Alexander‐Williams J, Keighley MR. Rubber band ligation or lateral subcutaneous sphincterotomy for the treatment of haemorrhoids. British Journal of Surgery 1977;64(10):737‐40. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Carapeti 1998 {published data only}
- Carapeti EA, Kamm MA, McDonald PJ, Phillips RK. Double‐blind randomised controlled trial of effect of metronidazole on pain after day‐case haemorrhoidectomy. Lancet 1998;351(9097):169‐72. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Filingeri 2004 {published data only}
- Filingeri V, Gravante G, Baldessari E, Grimaldi M, Casciani CU. Prospective randomised trial of submucosal haemorrhoidectomy with radiofrequency bistoury vs. conventional Park's operation. Techniques in Coloproctology 2004;8(1):31‐6. [DOI] [PubMed] [Google Scholar]
Forster 1996 {published data only}
- Froster CF, Sussmann HE, Patzelt‐Wenczler R. Optimization of the Barron ligature treatment of 2nd and 3rd‐degree haemorrhoids using a therapeutic troika. Schweizerische Rundschau fur Medizin Praxis 1996;85(46):1476‐81. [MEDLINE: ] [PubMed] [Google Scholar]
Gartell 1985 {published data only}
- Gartell PC, Sheridan RJ, McGinn FP. Out‐patient treatment of haemorrhoids: a randomized trial to compare rubber band ligation with phenol injection. British Journal of Surgery 1985;72(6):478‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Griffith 1987 {published data only}
- Griffith CDM, Morris DL, Wherry DC, Hardcastle JD. Out patient treatment of haemorrhoids: a randomised trial comparing contact bipolar diathermy with rubber band ligation. Coloproctology 1987;6:332‐334. [Google Scholar]
Hardy 1975 {published data only}
- Hardy KJ, Wheatley IC, Heffernan EB. Anal dilatation and haemorrhoidectomy. A prospective study. Medical Journal of Australia 1975;2(3):88‐91. [MEDLINE: ] [PubMed] [Google Scholar]
Hiltunen 1992 {published data only}
- Hiltunen KM, Matikainen M. Anal dilatation, lateral subcutaneous sphincterotomy and haemorrhoidectomy for the treatment of second and third degree haemorrhoids. A prospective randomized study. International Surgery 1992;77(4):261‐3. [MEDLINE: ] [PubMed] [Google Scholar]
Jones 1974 {published data only}
- Jones CB. A comparative study of the methods of treatment for haemorrhoids. Proceedings of the Royal Society of Medicine 1974;67(1):51‐3. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Keighley 1979 {published data only}
- Keighley MR, Buchmann P, Minervini S, Arabi Y, Alexander‐Williams J. Prospective trial of minor surgical procedures and high fibre diet for haemorrhoids. British Medical Journal 1979;2(6196):967‐9. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lacerda‐Filho 1997 {published data only}
- Lacerda‐Filho A, Cunha‐Melo JR. Outpatient haemorrhoidectomy under local anaesthesia. European Journal of Surgery 1997;163(12):935‐40. [MEDLINE: ] [PubMed] [Google Scholar]
MacRae 1995 {published data only}
- MacRae HM, McLeod RS. Comparison of Hemorrhoidal Treatment Modalities. A meta‐analysis. Dis Colon Rectum 1995;38(7):687‐94. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Murie 1982 {published data only}
- Murie JA, Sim AJ, Mackenzie I. Rubber band ligation versus haemorrhoidectomy for prolapsing haemorrhoids: a long term prospective clinical trial. British Journal of Surgery 1982;69(9):536‐38. [DOI] [PubMed] [Google Scholar]
Narro 2004 {published data only}
- Narro JL. Haemorrhoid therapy with doppler guided haemorrhoidal artery ligation via proctoscope KM‐25. A new alternative to haemorrhoidectomy and rubber band ligation?. Zentralblatt fur Chirurgie 2004;129(3):208‐210. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
O'Callaghan 1982 {published data only}
- O'Callaghan JD, Matheson TS, Hall R. Inpatient treatment of prolapsing piles: cryosurgery versus Milligan‐Morgan haemorrhoidectomy.. British Journal of Surgery 1982;69(3):157‐9. [DOI] [PubMed] [Google Scholar]
Rasmussen 1991 {published data only}
- Rasmussen O, Larsen KGL, Naver L, Christiansen J. Emergency haemorrhoidectomy compared with incision and banding for the treatment of acute strangulated haemorrhoids: A prospective randomised study. European Journal of Surgery 1991;157:613‐614. [PubMed] [Google Scholar]
Read 1982 {published data only}
- Read MG, Read NW, Haynes WG, Donnelly TC, Johnson AG. A prospective study of the effect of haemorrhoidectomy on sphincter function and faecal continence. British Journal of Surgery 1982;69(7):396‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Seow‐Choen 1992 {published data only}
- Seow‐Choen F, Ho YH, Ang HG, Goh HS. Prospective, randomized trial comparing pain and clinical function after conventional scissors excision/ligation vs. diathermy excision without ligation for symptomatic prolapsed hemorrhoids. Diseases of the colon and rectum 1992;35(12):1165‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Sim 1981 {published data only}
- Sim AJ, Murie JA, Mackenzie I. Comparison of rubber band ligation and sclerosant injection for first and second degree haemorrhoids‐ a prospective clinical trial. Acta Chirurgica Scandinavica 1981;147(8):717‐20. [MEDLINE: ] [PubMed] [Google Scholar]
Templeton 1983 {published data only}
- Templeton JL, Spence RA, Kennedy TL, Parks AG, Mackenzie G, Hanna WA. Comparison of infrared coagulation and rubber band ligation for first and second degree haemorrhoids: a randomised prospective clinical trial. British Medical Journal Clinical Research Ed.. 1983;286(6375):1387‐9. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wehrmann 2004 {published data only}
- Wehrmann T, Riphaus A, Feinstein J, Stergiou N. Hemorrhoidal elastic band ligation with flexible videoendoscopes: a prospective, randomized comparison with the conventional technique that uses rigid proctoscopes.. Gastrointestinal endoscopy 2004;60(2):191‐5. [DOI] [PubMed] [Google Scholar]
Additional references
Barron 1963
- Barron J. Office ligation of internal hemorrhoids. American journal of Surgery 1963;105(4):563‐570. [DOI] [PubMed] [Google Scholar]
Barwell 1999
- Barwell J, Watkins RM, Lloyd‐Davies E, Wilkins DC. Life‐Threatening Retroperitoneal Sepsis After Hemorrhois Injection Sclerotherapy. Report of a case. Diseases of the colon and rectum 1999;42(3):421‐23. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Bat 1993
- Bat L, Melzer E, Koler M, Dreznick Z. Complications of Rubber Band Ligation of Symptomatic Internal Hemorrhoids. Diseases of the colon and rectum 1993;36(3):287‐290. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Blaisdell 1958
- Blaisdell PC. Office ligation of internal hemorrhoids. American journal of Surgery 1958;96(3):401‐404. [DOI] [PubMed] [Google Scholar]
Bleday 1992
- Bleday R, Pena JP, Rothenberger DA, Goldberg SM, Buls JG. Symptomatic Hemorrhoids: Current Incidence and Complications of Operative Therapy. Diseases of the colon and rectum 1992;35(5):477‐481. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Brisinda 2000
- Brisinda G. How to treat haemorrhoids: Prevention is best; haemorrhoidectomy needs skilled operators. BMJ 2000;321(7261):582‐3. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Der Simonian 1986
- Simonian R, Laird N. Meta‐analysis in clinical trials. Controlled clinical trials 1986;7:177‐88. [DOI] [PubMed] [Google Scholar]
Goligher 1984
- Goligher J, Duthie H, Nixon H. Surgery of the Anus Rectum and Colon. 5. London: Baillière Tindall, 1984. [Google Scholar]
Haas 1984
- Haas PA, Fox TA Jr, Haas GP. The Pathogenesis of haemorrhoids. Diseases of the colon and rectum 1984;27(7):442‐50. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Johanson 1990
- Johanson JF, Sonnenberg A. The prevalence of haemorrhoids and chronic constipation: an epidemiological study. Gastroenterology 1990;98(2):380‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Keighley 1993
- Keighley MRB. Surgery of Anus, Rectum and Colon. 1. Vol. 1, WB Saunders publishers, 1993:295‐8. [Google Scholar]
Lehnhardt 2004
- Lehnhardt M, Steinstrauesser L, Drueke D, Muehlberger T, Steinau HU, Homann HH. Fournier's gangrene after Milligan‐Morgan haemorrhoidectomy requiring subsequent abdominoperineal resection of the rectum: report of a case. Diseases of the colon and rectum 2004;47(10):1729‐33. [DOI] [PubMed] [Google Scholar]
Longo 1998
- Longo A. Treatment of Hemorrhoid Disease by Reduction in Mucosal and Haemorrhoidal Products with a Circular Stapling Device ‐ New Procedure.. Proceedings of the 6th World Congress of Endoscopic Surgery, Rome, Italy. Rome, Italy, 1998.
Manson 2002
- Monson JRT, Mortenson NJ, Hartley J. Procedures for Prolapsing Haemorrhoids (PPH) or Stapled Anopexy. Consensus Document for Association of Coloproctology of Great Britain and Ireland. ACPGBI, 2003.
Nisar 2003
- Nisar P, Scholefield JH. Managing haemorrhoids. BMJ 2003;327(7419):847‐851. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Parks 1955
- Parks AG. De Haemorrhois. A study in surgical history. Guy's Hospital report 1955;104:135‐50. [PubMed] [Google Scholar]
Rogozina 2002
- Rogozina VA. Hemorrhoids. Eksperimental'Naia i Klinicheskaia Gastroenterologiia 2002;4:93‐6. [MEDLINE: ] [PubMed] [Google Scholar]
Sardinha 2002
Thaha 2002
- Thaha MA, Campbell KL, Steele RJC. Non‐operative treatment for haemorrhoidal disease. Cochrane Database of Systematic Reviews 2002, Issue 3. [DOI: 10.1002/14651858.CD003771] [DOI] [Google Scholar]
Thomson 1975
- Thomson WHF. The nature of Haemorrhoids. British Journal of Surgery 1975;62(7):542‐52. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]


