Abstract
Purpose of Review
Cognitive impairment and depression continue to be common among people with HIV (PWH) in the combination antiretroviral therapy (ART) era. A better understanding of the biological mechanisms that may underpin these disorders is needed. The purpose of this review is to describe published findings on soluble biomarkers from blood and cerebrospinal fluid (CSF) that have been associated with either cognition or depression among PWH in the setting of ART.
Recent Findings
Several biomarkers, including those that reflect viral persistence, monocyte/macrophage activation, and other processes, are associated with cognition and depressive symptoms. Some but not all results have been consistent across multiple studies. More research has been published on biomarkers of cognition relative to biomarkers of depression (particularly from CSF).
Summary
More studies are needed that investigate multiple biomarkers to understand the role of distinct but additive pathways in these disorders and to guide the development of new therapies.
Keywords: HIV, AIDS, Neurocognitive disorders, Biomarkers, Cerebrospinal fluid
Introduction
While people with HIV (PWH) are surviving significantly longer in the combination antiretroviral therapy (ART) era, end organ diseases including central nervous system (CNS) complications remain common. Specifically, both HIV-associated neurocognitive disorder (HAND) and HIV-associated depression are prevalent. HAND encompasses three different categories: HIV-associated dementia (HAD), minor neurocognitive disorder (MND), and asymptomatic neurocognitive impairment (NCI). Large cohort studies demonstrate that HAND rates continue to be high in PWH on ART even when confounding comorbidities are excluded [1, 2]. A recently published meta-analysis found a worldwide HAND prevalence in the ART era of 42.6% (95% Confidence Interval [CI] 39.7–45.5%) [3]. In a subset of 51 studies in which greater than 90% of participants were on ART, the prevalence of HAND remained essentially constant at 43.1% (95% CI 38.1–48.2%). Another recent meta-analysis similarly showed a global HAND prevalence among PWH of greater than 40% [4]. Diminished cognition has been associated with multiple adverse outcomes in the setting of HIV. Worse cognition can predict worse ART medication adherence [5], which is known to place PWH at higher risk for clinical complications as well as HIV transmission [6, 7]. Cognitive impairment in the setting of HIV is associated with worse quality of life [8] and increased mortality [9, 10].
Similarly, heightened risk for depression in PWH has also been recognized for decades [11, 12]. The Women’s Interagency HIV Study (WIHS) in the USA, for instance, found that 20% of women with HIV have major depressive disorder (MDD) based on diagnostic interview (compared to 10% nationally), and 32.4% experience MDD in their lifetime (versus 22.9% nationally) [13, 14]. The medical monitoring project also found that depression prevalence is significantly higher in men with HIV (prevalence ratio = 3.1) compared to a cohort of individuals from the general population [15]. Like HAND, depression in PWH is associated with multiple adverse clinical outcomes, including worse ART adherence and virologic control [16, 17]. PWH with chronic depression symptoms are approximately twice as likely to die compared to PWH with few or no depression symptoms [18].
More research is needed to better understand the pathogenesis of both HAND and depression in PWH. If a better understanding of these disorders is established, targeted treatments and preventions could be evaluated more effectively. In this review, we examine published evidence on soluble biomarkers from both blood and cerebrospinal fluid (CSF) in relation to cognition and depressive symptoms in PWH. Because of the established relationship between uncontrolled HIV replication and HAND as well as the pressing need to better understand the pathogenesis of HIV CNS complications despite virologic suppression, this review is limited to studies in which the majority of PWH were receiving ART. We have also limited the review to studies that reported domain scores or global performance (studies that only reported associations with individual test scores were not included). While cognitive impairment and depression can be concurrent and can influence each other’s course, for the purpose of this review, we will discuss them as separate entities. Lastly, this review will be limited to a discussion of adults. While cognitive impairment is also problematic among children with HIV [19], discussion of the pediatric literature is beyond the scope of this review.
Soluble Biomarkers of Cognition During HIV Infection (Table 1)
Table 1.
Selected biomarkers of cognition during HIV in setting of ART
| Category | Biomarker | Fluid |
|---|---|---|
| HIV persistence | HIV DNA | PBMC, monocytes, CSF cells |
| HIV RNA | CSF | |
| HIV Tat Protein | CSF | |
| Co-infection | Anti-Cytomegalovirus IgG | CSF |
| Toxoplasma IgG status, IgG level | Blood | |
| Monocyte/macrophage activation | Soluble CD14 | Blood, CSF |
| Neopterin | Blood, CSF | |
| Soluble CD163 | Blood | |
| Inflammatory cytokines | Tumor Necrosis Factor | Blood |
| Interleukin 6 | Blood | |
| Interferon alpha | Blood | |
| Chemokines | CCL2 | CSF, PBMC |
| Interleukin 8 | PBMC | |
| CXCL10 | Blood | |
| Immune cell characteristics | CD14 + CD38 + | PBMC |
| CD14 + + CD16 + CD163 + | PBMC | |
| CD4 + CD16 + + | PBMC | |
| CD4 + /CD8 + ratio | PBMC, CSF cells | |
| HLA-DR on CD4 + | PBMC, CSF cells | |
| HLA-DR on CD8 + | PBMC, CSF cells | |
| Neuronal markers | Neurofilament Light | Blood, CSF |
| Microtubule associated protein2 | CSF | |
| Markers of microbial translocation | (1 → 3)-β-D-Glucan | Blood |
| Intestinal fatty acid-binding protein | Blood | |
| Acute phase reactants | C-reactive protein | Blood |
Biomarkers of HIV Persistence and Co-infection with Other Pathogens
HIV eradication has proven to be extremely elusive because the virus establishes latent reservoirs in long-lived immune cells, some of which have the ability to clonally expand [20]. Growing evidence supports the hypothesis that magnitude of HIV reservoir is linked to cognitive impairment. HIV DNA levels from peripheral blood mononuclear cells (PBMC) were significantly higher among individuals with HIV-associated dementia (HAD) in a study of 49 PWH by Shiramizu et al., even after taking into account virologic suppression with ART [21]. The relationship between higher HIV DNA from PBMC and cognitive impairment was later confirmed in an analysis that included participants with milder impairment forms [22]. The same group also evaluated the relationship between cognition and HIV DNA in a longitudinal study of 27 individuals starting ART in Thailand [23]. At 48 weeks after ART initiation, the median HIV DNA level remained elevated among individuals with HAD compared to adults who were not demented, despite suppression of plasma HIV RNA. Additionally, decline in monocyte HIV DNA over time was associated with cognitive improvement. These studies suggest that the size of the peripheral HIV reservoir (particularly from cells of the monocyte lineage which potentially traffic to the CNS) may influence cognitive health, and that improvement on ART may be dependent on reduction of this reservoir. Moving to the CNS compartment, a study by Spudich et al. produced congruent findings. Specifically, a group of 69 participants on suppressive ART underwent CSF sampling as well as comprehensive cognitive testing* [24]. HIV DNA was detected from CSF cell pellets in 48% of participants, and cognitive performance was significantly worse in those with detectable CSF HIV DNA. This strengthens the possibility of a relationship between the HIV reservoir on ART and cognition. Interestingly, detection of CSF HIV DNA was not associated with blood PBMC HIV DNA levels in the study by Spudich et al., which raises the possibility that the peripheral reservoir affects cognition by mechanisms that are independent of the CNS reservoir. From a longitudinal perspective, a study from Australia found that increase in PBMC HIV DNA over time was associated with decline in motor skill and verbal fluency despite effective ART among 80 PWH [25]. However, this study did not find an association between baseline PBMC HIV DNA and cognition, which contrasts with the other studies. Peripheral HIV DNA levels continue to decay during ART over the first 4 years of therapy [26]. Therefore, the HIV DNA reservoirs of the participants in the Australian study may have decayed to a point that the contribution of this factor to cognition was too small to be detected. The relationship between HIV DNA from blood cells and cognition appears to be consistent across HIV clades. Specifically, a recently published study from South Africa with clade C-infected individuals showed that lymphocyte HIV DNA level was higher among participants with cognitive impairment [27].
HIV RNA can be detected at low levels by single copy assay (SCA) while being undetectable with commercially available assays. The presence of HIV RNA by SCA could indicate replication-competent virus in the setting of ART (though HIV RNA released from infected cells without production of intact virions is another explanation). In a study of 220 PWH on suppressive ART who also underwent comprehensive cognitive testing, 42% had detectable CSF HIV RNA by SCA despite having undetectable plasma and CSF HIV RNA by commercially available assay [28]. At baseline, having a detectable CSF HIV RNA at the same time as having an undetectable plasma HIV RNA (CNS discordance) was associated with worse cognitive performance (see Fig. 1). Among participants followed longitudinally, a persistently undetectable CSF HIV RNA by SCA during the study was associated with cognitive improvement (see Fig. 2). These findings again support the concept that a larger CNS HIV reservoir is detrimental to cognition in the setting of ART. Somewhat counterintuitively, this study showed that when analyzed as a continuous outcome, higher CSF HIV RNA was associated with better cognition. However, a significant change in HIV RNA is generally considered to be at least 0.3–0.5 log10 copies/milliliter (mL), meaning that small numerical changes in the absolute copies/mL may not be meaningful [29].
Fig. 1.
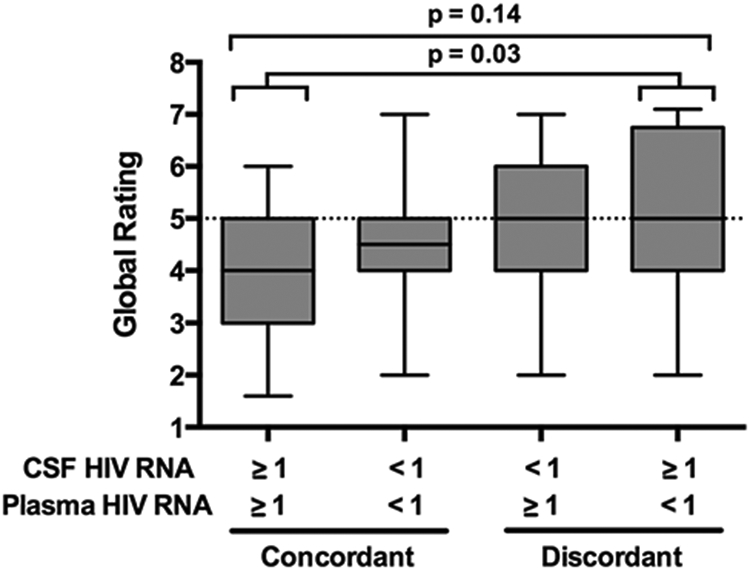
CSF-plasma HIV discordance is associated with worse cognitive performance
Fig. 2.
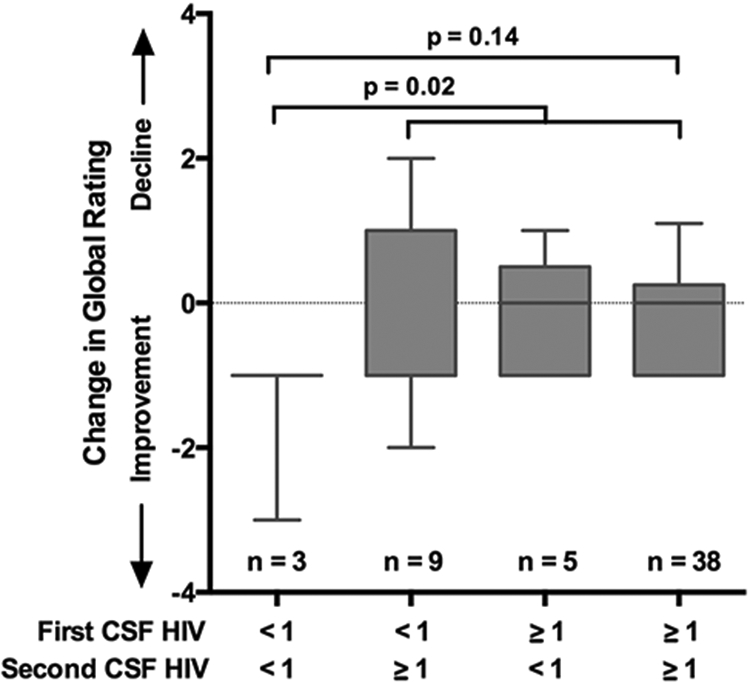
A persistently undetectable CSF HIV RNA was associated with cognitive improvement
HIV protein production also reflects the viral reservoir. These proteins are sometimes detected in the CNS despite ART. Most notably, the transactivator of transcription (Tat) enhances the efficiency for HIV transcription and in one study was found to be detectable from CSF in 36.8% of 68 individuals on ART [30]. While the relationship with global cognitive function was not significant in this study, individuals with detectable CSF Tat had significantly worse performance in the cognitive domains of information processing and motor speed.
Taken together, these studies of HIV persistence biomarkers during ART appear to demonstrate a relationship between greater magnitude of viral persistence (particularly in the CNS) and worse cognition. While these markers are often not detectable in the setting of ART, assays that are more sensitive to their presence continue to be refined [31], and in the future may provide even greater understanding of the relationship between viral persistence and cognition. Other pathogens may also play a role in cognitive impairment during HIV. While invasive disease from cytomegalovirus (CMV) has become rare in the ART era, the majority of PWH have CMV infection in a latent state. This low level CMV may increase inflammation and endothelial activation and may trigger adverse consequences. Higher anti-CMV IgG level in CSF is associated with worse cognition in PWH on suppressive ART [32]. Another common co-infection in PWH is with the parasite Toxoplasma gondii. While known for causing encephalitis in PWH with low CD4 + T-cell counts, it appears that latent Toxoplasma infection has detrimental cognitive consequences among PWH with higher CD4 + T-cell counts. In a study of 263 PWH mostly on ART, latent Toxoplasma infection (defined by blood IgG positivity) was associated with cognitive impairment [33]. Additionally, higher quantitative anti-Toxoplasma IgG level from blood was associated with worse cognitive performance.
Biomarkers of Monocyte/Macrophage Activation
The presence of activated monocytes in blood was found to be related to HAD in the pre-ART era [34], inspiring continued investigations of monocyte activation in the ART era. Soluble CD14 (sCD14) represents the soluble form of the 53 kilodalton (KD) membrane antigen CD14, a glycosyl-phosphatidylinositol-anchored cell surface molecule expressed primarily on monocytes and macrophages [35]. This molecule amplifies cytokine release [36]. In a mostly ART-treated cohort (n = 97), Lyons et al. found that plasma sCD14 concentrations were higher in impaired individuals (particularly learning and attention domains) and negatively correlated with cognitive performance as a continuous variable (Spearman’s rho = −0.21, p = 0.036) [37]. Using the same cohort, this group also found a significant relationship between higher CSF sCD14 and worse cognition [38]. However, the relationship in that analysis was driven by participants who did not have virologic suppression despite ART. A relationship between higher plasma sCD14 and decreased cognition was also found in the WIHS. In a study of 253 women participants (74% of whom were PWH), higher plasma sCD14 concentration was associated with significantly worse performance in verbal learning, executive function, and psychomotor speed (p < 0.01), as well as verbal memory (p = 0.04) [39]. When limiting the analysis to HIV + women with full virologic suppression, higher sCD14 was associated with worse performance only in the executive function domain. Since lipopolysaccharide (LPS) binds to CD14 and causes its shedding [35], sCD14 concentrations may also reflect the increased microbial gut translocation that occurs during HIV infection, and therefore may not be exactly specific to monocyte activation [40].
Neopterin is a biochemical product of the guanosine triphosphate pathway and is excreted by activated monocytes and macrophages [41]. With the intrinsic immune cells of the CNS being of the monocyte lineage, increased neopterin concentrations may reflect increased activity of these cells in the setting of HIV. This is evidenced by the fact that CSF neopterin concentrations from PWH remain elevated despite long-term virologic suppression on ART [41, 42]. In the ART era, a study of 99 PWH (90% male), all on suppressive ART, evaluated the relationship between CSF neopterin and cognition [43]. Among participants with impairment, CSF neopterin concentrations were 33% higher than participants without impairment, a statistically significant difference. A relationship between higher CSF neopterin concentration and cognitive impairment was also shown in a small substudy of the CNS HIV Anti-Retroviral Therapy Effects Research (CHARTER) cohort in the USA [44]. Plasma concentrations of neopterin also remain elevated in PWH despite ART, and a small study from Thailand found that plasma neopterin concentration was significantly higher in women with HIV on ART who had cognitive impairment compared to those who were not impaired [45]. Like the studies on sCD14, the neopterin studies suggest that both peripheral and CNS monocyte activation may be related to cognition. However, it is also possible that these biomarkers, when observed in different compartments, simply reflect global burden (though some studies propose that CSF neopterin is mostly brain derived and should be thought of separately from plasma neopterin) [46].
Another biomarker of monocyte/macrophage activation is CD163, which is expressed highly by macrophages and serves as a scavenger molecule to prevent hemoglobin toxicity. sCD163 is the soluble form of this antigen and is elevated in inflammatory disease states [44]. Within the CHARTER cohort, Burdo et al. found that plasma concentrations of sCD163 were higher among participants with impairment in both learning and executive function domains [44]. Plasma sCD163 concentration also remained high in participants with impairment over time. In contrast, no relationship was found between CSF sCD163 concentration and cognition. This could have been a function of the relatively small sample size (n = 34) that limited statistical power. Additionally, the CSF may reflect monocyte activation (cells which are abundant in CSF but have relatively low expression of CD163) but may not necessarily reflect macrophage activation (cells which are not abundant in CSF, but are abundant in actual brain tissue and have high expression of CD163). While this study involved a cohort that was over 80% men, a similar relationship between plasma sCD163 and cognition was identified in the same WIHS study that evaluated sCD14 in women [39]. Specifically, higher plasma sCD163 concentration was associated with worse overall cognitive performance (p < 0.001) that was driven by worse performance in the domains of verbal learning, verbal memory, executive function, and psychomotor speed (p < 0.001 for all comparisons), plus fine motor skills (p = 0.01). When limiting the analysis to HIV + women with virologic suppression, higher plasma concentration of sCD163 was associated with worse overall cognitive performance (p = 0.04) and worse performance in the domains of verbal memory (p = 0.003), psychomotor speed (p = 0.01), and fine motor skills (p = 0.004).
Inflammatory Cytokines and Other Biomarkers of Acute Inflammation
Tumor necrosis factor alpha (TNFα) is an inflammatory cytokine that is persistently elevated in the blood of PWH despite ART [47], and is associated with oligodendrocyte necrosis and neurotoxicity [48]. In a study from Romania of 144 young adults who were infected with HIV as children (with HIV clade F), higher plasma TNFα concentration was associated with cognitive impairment in multivariable analyses that controlled for HIV RNA [49]. In a US study, higher plasma TNFα was associated with the development of HAD over time [50]. Interleukin 6 (IL-6) is another pro-inflammatory cytokine that has been implicated in inflammatory neuropathology [51]. In another CHARTER substudy, Sattler et al. found a relationship between higher plasma IL-6 and worse cognition, a finding that was driven by individuals with higher waist circumference. This raises the possibility that some biomarkers are associated with cognition through interactions with comorbidities. In the study from Romania, higher plasma IL-6 was also associated with cognitive impairment in multivariable analysis [49]. Increased interferon alpha (IFNα) concentration has been observed during HIV infection, and this cytokine has a direct neurotoxic role in both animal models and in humans [52, 53]. Among PWH without virologic suppression, higher CSF IFNα concentration has been associated with worse cognitive performance [54, 55]. While research involving this cytokine is limited among PWH with virologic suppression, a small study by Cassol et al. involving 22 inflammatory biomarkers showed that plasma concentrations of IFNα 2b (the predominant IFNα subtype expressed in PWH) [56] was most predictive of cognitive impairment over time in the setting of virologic suppression [57]. In a study from WIHS that incorporated longitudinal visits, Rubin et al. showed that variability of C-reactive protein (CRP), an acute phase reactant, was most predictive of cognitive impairment in women with HIV [58]. This variability was associated most strongly with worse performance in executive function, attention/working memory, and psychomotor speed domains.
Chemokines
Chemokines recruit leukocytes, and in so doing may cause inflammatory damage or attract cells which are latently infected with HIV that have the potential to reactivate. In a study from Thailand involving stimulated CD14 + PBMC from PWH on suppressive ART, higher levels of IL-8 and CCL2 (also known as MCP-1, linked to HAD in the pre-ART era [59]) observed after stimulation were each associated with the presence of HAND [60]. CXCL10 (also known as IP-10) is a chemokine induced by IFNγ and produced by macrophages, astrocytes, and other cells [61]. This chemokine is one of the first inflammatory biomarkers to become elevated in acute HIV and thus its production is very sensitive to the presence of HIV [62]. In the study from Romania, higher plasma CXCL10 was associated with an increase in cognitive impairment, but interestingly this relationship was limited to the subgroup of study participants who were women [49].
Immune Cell Characteristics
A study of peripheral monocyte subtypes from Italy found that while none was associated with cross-sectional NP performance in 54 PWH, greater levels of CD14 + CD38 + cells and lower levels of CD14 + + CD16 + CD163 + cells were each associated with a significant decrease in memory performance over time [63]. In another study, a significant correlation was found between higher percentage of CD4 + CD16 + + in blood and worse cognitive performance in PWH after 48 weeks of ART [64]. In a study of 86 PWH in Germany, Grauer et al. found that lower CD4 + /CD8 + ratio in both blood and CSF correlated with increasing cognitive impairment, and that the presence of HLA-DR on both CD4 + and CD8 +cells in blood and CSF was also associated with higher grade of impairment [65]. This group also found relationships with cognition based on effector-memory lymphocyte status and lymphocyte programmed death (PD)-1 expression. Other studies suggest that the relationship between certain cytokines and cognition stems from the extent of cytokine production by CSF CD8 + T cells. Specifically, CSF CD8 +T cells from PWH with cognitive impairment express higher levels of TNFα, IFNγ, and IL-2 [66].
Neuronal Markers
Neurofilaments are highly phosphorylated proteins that are integral elements of the neuronal cytoskeleton [67]. The expression of these proteins is particularly high in large myelinated axons, where they comprise approximately 85% of cytoskeleton proteins [68]. Neurofilaments consist of three subunits with different molecular weights: light (68 kDa), medium (150 kDa), and heavy (190–210 kDa). Of these three subunits, neurofilament light (NfL) is the most abundant and the most soluble. NFL was first characterized in CSF [69], and higher CSF NFL concentration is associated with the presence of cognitive impairment among PWH in both univariable and multivariable models* [70]. Using single molecule digital enzyme-linked immunosorbent assay (simoa), NfL can now be reliably quantified from blood [71]. Similar to CSF NfL concentration, higher plasma NfL concentration is associated with worse global cognitive performance in PWH [72]. Exosomes are small extracellular vesicles that are shed from all cells. They are important in normal cell to cell communication as they contain cellular proteins, mRNA transcripts, and miRNAs [73]. Neuron-derived exosomes (NDEs) are specific to the CNS and are enriched with CNS-derived proteins, including NfL. A study characterizing NDE from blood showed that NfL levels from NDE were higher in PWH who had cognitive impairment [74]. These studies provide examples of the emerging technologies that may allow for a better understanding of CNS pathologies through blood samples.
Microtubules are also crucial elements of the neuronal cytoskeleton [75]. Microtubules additionally serve as high-ways for axonal transport, and microtubule-associated proteins (MAPs) are needed to maintain their organization. MAP2 specifically forms cross-bridges between microtubules, participates in organelle transport, and is a critical stabilizer of microtubules in mature dendrites [76, 77]. In a group of 27 PWH mostly on ART, Avdoshina et al. showed that CSF MAP2 concentration was significantly higher among individuals with cognitive impairment. This again suggests that HAND is linked at least in part to neuronal degeneration [78]. This study also showed that blockage of interaction between HIV gp120 and microtubules in vitro serves to limit neurotoxicity and could represent a future treatment approach for HAND.
Markers of Intestinal Microbial Translocation
With the gut dysbiosis and altered gut permeability that occurs in PWH [79], biomarkers of microbial translocation are associated with inflammation and inflammation-associated disorders, including HAND. (1 → 3)-β-D-Glucan (BDG) is a polysaccharide cell wall component of most fungal species (including Candida), and thus is a marker of microbial translocation. Higher blood concentration of BDG correlates with worse global neurocognitive performance among PWH on ART [80]. Increased blood concentrations of intestinal fatty acid-binding protein (I-FABP), another marker of microbial gut translocation, was similarly found to be associated with worse cognitive performance among PWH with virologic suppression in East Africa [81]. Interestingly, the investigation of the same relationship was found to be insignificant among women with HIV in the USA in WIHS [39]. The high prevalence of diarrheal diseases among PWH in sub-Saharan Africa [82] could lead to altered gut permeability in this population and may be a factor in these discrepant findings.
Other Biomarkers
Galectin-9 is a β-galactoside-binding animal lectin of the galectin family that is expressed ubiquitously in tissues and cells. Galectin-9 is a key immune regulatory molecule that maintains the stability of the CNS under normal physiological conditions [83]. In a subset of older PWH, higher CSF Galectin-9 concentration was shown to negatively correlate with cognitive performance [84]. Discovery studies of similar molecules (using the techniques of lipidomics, metabolomics, and proteomics) have shown promise for the identification of novel biomarkers of cognition in PWH [85-87]. There is also building evidence of a vascular component of cognitive impairment during HIV via soluble biomarkers including those that are vascular growth factors [88-90], though imaging measures may be more suited to measure vascular disease. Other blood biomarkers that have been associated with cognition in the setting of ART include cystatin B, cystatin C, cathepsin B, citrate, and succinate [91-93]. Other CSF molecules that have been associated with cognition in the setting of ART include biomarkers of iron status [89].
Combinations of Biomarkers
The diversity of biomarkers linked to cognition in PWH suggests that multiple pathologic pathways may be involved. More research is needed to test if combinations of these biomarkers may be even more informative as a means to understand cognition. A study of 98 PWH used multiple biomarkers with both a mixed modeling and recursive partitioning approach to predict cognition change over time [94]. While only CSF CCL2 was predictive of cognitive change over time with the mixed modeling approach, recursive partitioning identified several biomarkers (including sCD14, TNFα, CCL2, and CXCL12) that contributed to either improvement or worsening of cognition. A WIHS analysis of combination biomarker signatures also found significant relationships with cognitive change over time. Four combinatory signatures were distinct in HIV + women with virologic suppression. Three of these combinations (which included biomarkers associated with chemotaxis and inflammation) were associated with overall and domain-specific cognitive worsening over time [95]. More research that incorporates multiple biomarkers is needed to evaluate the relative contribution of different pathways to cognition in PWH.
Soluble Biomarkers of Depression During HIV (Table 2)
Table 2.
Selected biomarkers of depression during HIV in setting of ART
| Category | Biomarker | Fluid |
|---|---|---|
| HIV persistence | HIV RNA | CSF |
| Monocyte/macrophage activation | Soluble CD14 | Blood |
| Inflammatory cytokines | Interleukin 6 | Blood |
| Tumor Necrosis Factor | Blood | |
| Interleukin 15 | Blood | |
| Interleukin 12 p40/p70 | Blood | |
| Granulocyte Colony Stimulating Factor | Blood | |
| Chemokines | CXCL10 | Blood |
| Coagulation | D-dimer | Blood |
| Neurotransmitters | Dopamine | CSF |
| Homovanillic acid | CSF | |
| Acute phase reactants | C-reactive Protein | Blood |
Biomarkers of HIV Persistence
Similar to HAND, evidence has also emerged that greater HIV persistence in the CNS is associated with depressive symptoms. Also from the CHARTER cohort, an analysis of longitudinal visits was undertaken to evaluate the relationship of CSF or plasma HIV RNA detectability and development of moderate-severe depressive symptoms despite ART. Detectable CSF HIV RNA (at a level of ≥ 50 copies/mL) was associated with a 4.7-fold increase in new onset depression, while detectable plasma HIV RNA was not significantly associated with new onset depression [96]. This study indicates that, as with cognition, depression symptoms are related to higher levels of HIV in the CNS despite ART.
Cytokines, Chemokines, and Other Markers of Acute Inflammation
In a recent pilot study from the USA, 32 PWH were evaluated with a panel of biomarkers for inflammation, coagulation, and vascular function in relation to depression. Plasma TNFα along with age, glucose levels, and glycosylated hemoglobin were identified as the biomarkers that most strongly predicted depression based on the Patient Health Questionnaire (PHQ)-9 [97]. In a study from Puerto Rico, PWH with at least mild symptoms of depression based on the PHQ-9 had significantly higher plasma concentrations of CXCL10, IL-15, GCSF, and IL-12 p40/p70, which is notable considering the small sample size of the study (n = 23) [98]. In a larger study from Italy, 102 PWH were grouped by depression symptoms with latent class analysis [99]. Higher IL-6 concentration in blood was characteristic of participants in the class marked by moderate/severe somatic symptoms (but less severe cognitive-affective symptoms). This suggests that different symptoms of depression during HIV might be influenced by different biological pathways. In a cross-sectional study of 201 PWH in Uganda, plasma IL-6 and TNFα were both significantly associated with major depressive disorder (MDD) as identified by Mini International Neuropsychiatric Interview [100]. IL-6 concentration was significantly higher among participants with MDD compared to those without (median 22.4 vs. 5.8 pg/mL; p < 0.0001). The group then tested associations with depression by multivariable logistic regression. The odds of MDD increased with increasing levels of IL-6 with an adjusted odds ratio of 0.98 (95% CI, 0.97–0.99, p < 0.001). Meanwhile, participants with very high levels of TNFα (> 500 pg/mL) had a markedly increased risk of MDD (aOR = 3.98, 95% CI, 1.29–12.33).
A study of 316 PWH from Nepal evaluated the relationship between C-reactive protein (CRP) and depression symptoms via BDI-I [101]. In multivariable linear regression that accounted for demographic and disease characteristics, the relationship between increasing log serum CRP concentrations and increasing depression symptom score was linear and significant (B = 1.13, p = 0.001). In a multivariable logistic regression analysis from the same study, participants with a serum CRP level of > 3 mg/L had 2.3-fold higher odds of depression compared to those with serum CRP level of ≤ 3 mg/L (p = 0.005). A small but significant relationship between higher serum CRP and clinically significant depression symptoms was also found among PWH in an analysis from the Multicenter AIDS Cohort Study (MACS, which was limited to men) in the USA [102].
Biomarkers of Monocyte Activation
In the military Veterans Aging Cohort Study (VACS) in the USA that included 1546 participants (with the vast majority of participants being male), higher plasma sCD14 concentration was associated with a slight increase in PHQ-9 somatic depression symptoms among PWH [103]. This relationship remained significant when incorporating other factors that influence depression symptoms including alcohol and drug use.
Coagulation Markers
In the same VACS analysis [103], plasma D-dimer was investigated. Similarly to sCD14, higher D-dimer concentration was associated with a slight increase in PHQ-9 somatic symptoms among PWH. However, this relationship became not statistically significant after incorporating other factors such as alcohol and drug use into the models.
Neurotransmitters
Studies on CSF biomarkers of depression in HIV are sparse, highlighting an important need for more research. However, Saloner et al. recently published an analysis of 225 adults (123 of whom were PWH) in which they investigated CSF concentrations of dopamine and its metabolite homovanillic acid (HVA) in relation to depression symptoms using the Beck Depression Inventory-(BDI) II* [104]. Correlational analyses between dopaminergic biomarkers and individual BDI-II domains revealed significant associations between higher cognitive symptoms of depression and lower HVA (r = −0.22, p = 0.016) and dopamine (r = −0.20, p = 0.025) z-scores among PWH. In multivariable models, there were significant interactions between both HIV and dopamine as well as HIV and HVA in relation to depression symptoms. Specifically, lower HVA z-scores significantly related to higher BDI-II scores in HIV + (b = −2.14, r = −0.19, p = 0.034), yet did not significantly relate to BDI-II scores in people without HIV (b = 1.55, r = 0.14, p 0.146). A significant interaction in the same direction was also present between HIV status and dopamine in association with BDI-II scores (b = −3.15, p = 0.033). These relationships were present when accounting for lifetime methamphetamine use disorder, which while not common (5–10% of participants), was associated with higher BDI-II scores.
Combinations of Biomarkers
An analysis of 1727 participants from the MACS in the USA included 19 plasma markers of inflammation and then performed exploratory factor analysis in relationship to Center for Epidemiological Studies Depression (CES-D) scores (with score > 20 representing clinically relevant depression symptoms)* [102]. A factor that included plasma concentrations of soluble TNFα receptor 2, soluble interleukin-2 receptor α, soluble CD27, B-cell activating factor, CXCL10, soluble IL6 receptor, sCD14, and sGP130 was associated with 9% higher odds of CES-D > 20 among PWH (OR = 1.09, 95% CI, 1.03–1.16) with each standard deviation increase. The significant association with depression remained even when changing the CES-D cutoff to > 16. Factor analysis was also employed in a CHARTER substudy of depressive symptoms using BDI-II scores as the outcome [105]. The factor that included IL-6, D-dimer, and CRP was associated with increasing depressive symptoms. Interestingly, this finding was limited to the men in the study.
Conclusions
With cognitive impairment and depression continuing to be significant challenges for PWH, a better understanding of these disorders is needed in order to design more effective treatments. Viral persistence, inflammation, microbial translocation, and neuronal injury appear to all have some role based on current soluble biomarker evidence (though significantly more evidence exists related to cognition compared to depression). A significant challenge for the field is to understand whether the pathways represented by the biomarkers are distinct and additive, or if they are all part of one complicated pathway. Because cognitive impairment and depression often co-occur, more research is also needed to disentangle how these pathways contribute to each disorder and how the disorders contribute to each other, as suggested by recent studies [106]. Given the lack of cure for HIV, the onus is on the field to elucidate these pathways and their interactions in order to move towards treatments that will improve quality of life for individuals with HIV.
Acknowledgements
The authors also gratefully acknowledge funding from the following sources: R21 MH118092, R01 AG062387 (Principal Investigator: A. Anderson) and P30AI050409 (Emory Center for AIDS Research).
Footnotes
Conflict of Interest The authors declare no competing interests.
Human and Animal Rights and Informed Consent This article does not contain any studies with animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have beenhighlighted as:
• Of importance
- 1.Heaton RK, Clifford DB, Franklin DR Jr, et al. HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: CHARTER Study. Neurology. 2010;75:2087–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sacktor N, Skolasky RL, Seaberg E, et al. Prevalence of HIV-associated neurocognitive disorders in the Multicenter AIDS Cohort Study. Neurology. 2016;86:334–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang Y, Liu M, Lu Q, et al. Global prevalence and burden of HIV-associated neurocognitive disorder: a meta-analysis. Neurology. 2020;95:e2610–21. [DOI] [PubMed] [Google Scholar]
- 4.Wei J, Hou J, Su B, et al. The prevalence of Frascati-criteria-based HIV-associated neurocognitive disorder (HAND) in HIV-infected adults: a systematic review and meta-analysis. Front Neurol. 2020;11:581346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ettenhofer ML, Foley J, Castellon SA, Hinkin CH. Reciprocal prediction of medication adherence and neurocognition in HIV/AIDS. Neurology. 2010;74:1217–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen MS, Chen YQ, McCauley M, et al. Antiretroviral therapy for the prevention of HIV-1 transmission. N Engl J Med. 2016;375:830–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Strategies for Management of Antiretroviral Therapy Study G, El-Sadr WM, Lundgren J, et al. CD4+ count-guided interruption of antiretroviral treatment. N Engl J Med. 2006; 355:2283–96. [DOI] [PubMed] [Google Scholar]
- 8.Tozzi V, Balestra P, Galgani S, et al. Neurocognitive performance and quality of life in patients with HIV infection. AIDS Res Hum Retroviruses. 2003;19:643–52. [DOI] [PubMed] [Google Scholar]
- 9.Saylor D, Nakigozi G, Nakasujja N, et al. HIV associated neurocognitive disorder leads to death. Abstract 425. 2019 Conference on Retroviruses and Opportunistic Infections, Seattle, Washington, March 4–7; 2019. [Google Scholar]
- 10.Tozzi V, Balestra P, Serraino D, et al. Neurocognitive impairment and survival in a cohort of HIV-infected patients treated with HAART. AIDS Res Hum Retroviruses. 2005;21:706–13. [DOI] [PubMed] [Google Scholar]
- 11.Bing EG, Burnam MA, Longshore D, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiatry. 2001;58:721–8. [DOI] [PubMed] [Google Scholar]
- 12.Ciesla JA, Roberts JE. Meta-analysis of the relationship between HIV infection and risk for depressive disorders. Am J Psychiatry. 2001;158:725–30. [DOI] [PubMed] [Google Scholar]
- 13.Cook JA, Burke-Miller JK, Steigman PJ, et al. Prevalence, comorbidity, and correlates of psychiatric and substance use disorders and associations with HIV risk behaviors in a multisite cohort of women living with HIV. AIDS Behav. 2018;22:3141–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rubin LH, Maki PM. HIV, depression, and cognitive impairment in the era of effective antiretroviral therapy. Curr HIV/AIDS Rep. 2019;16:82–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Do AN, Rosenberg ES, Sullivan PS, et al. Excess burden of depression among HIV-infected persons receiving medical care in the united states: data from the medical monitoring project and the behavioral risk factor surveillance system. PloS one. 2014;9:e92842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Horberg MA, Silverberg MJ, Hurley LB, et al. Effects of depression and selective serotonin reuptake inhibitor use on adherence to highly active antiretroviral therapy and on clinical outcomes in HIV-infected patients. J Acquir Immune Defic Syndr. 2008;47:384–90. [DOI] [PubMed] [Google Scholar]
- 17.Kacanek D, Jacobson DL, Spiegelman D, Wanke C, Isaac R, Wilson IB. Incident depression symptoms are associated with poorer HAART adherence: a longitudinal analysis from the Nutrition for Healthy Living study. J Acquir Immune Defic Syndr. 2010;53:266–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ickovics JR, Hamburger ME, Vlahov D, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV Epidemiology Research Study.JAMA, J Am Med Assoc. 2001;285:1466–74. [DOI] [PubMed] [Google Scholar]
- 19.Paul R, Apornpong T, Prasitsuebsai W, et al. Cognition, emotional health, and immunological markers in children with long-term nonprogressive HIV. J Acquir Immune Defic Syndr. 2018;77:417–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ndung’u T, McCune JM, Deeks SG. Why and where an HIV cure is needed and how it might be achieved. Nature. 2019;576:397–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shiramizu B, Gartner S, Williams A, et al. Circulating proviral HIV DNA and HIV-associated dementia. AIDS. 2005;19:45–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shiramizu B, Williams AE, Shikuma C, Valcour V. Amount of HIV DNA in peripheral blood mononuclear cells is proportional to the severity of HIV-1-associated neurocognitive disorders. J Neuropsychiatry Clin Neurosci. 2009;21:68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Valcour VG, Shiramizu BT, Sithinamsuwan P, et al. HIV DNA and cognition in a Thai longitudinal HAART initiation cohort: the SEARCH 001 Cohort Study. Neurology. 2009;72:992–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.•.Spudich S, Robertson KR, Bosch RJ, et al. Persistent HIV-infected cells in cerebrospinal fluid are associated with poorer neurocognitive performance. J Clin Invest. 2019;129:3339–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cysique LA, Hey-Cunningham WJ, Dermody N, Chan P, Brew BJ, Koelsch KK. Peripheral blood mononuclear cells HIV DNA levels impact intermittently on neurocognition. PloS one. 2015;10:e0120488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Besson GJ, Lalama CM, Bosch RJ, et al. HIV-1 DNA decay dynamics in blood during more than a decade of suppressive antiretroviral therapy. Clin Infect Dis. 2014;59:1312–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ruhanya V, Jacobs GB, Nyandoro G, et al. Peripheral blood lymphocyte proviral DNA predicts neurocognitive impairment in clade C HIV. J Neurovirol. 2020;26:920–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anderson AM, Munoz-Moreno JA, McClernon DR, et al. Prevalence and correlates of persistent HIV-1 RNA in cerebrospinal fluid during antiretroviral therapy. J Infect Dis. 2017;215:105–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hughes MD, Johnson VA, Hirsch MS, et al. Monitoring plasma HIV-1 RNA levels in addition to CD4+ lymphocyte count improves assessment of antiretroviral therapeutic response. ACTG 241 Protocol Virology Substudy Team. Ann Intern Med. 1997;126:929–38. [DOI] [PubMed] [Google Scholar]
- 30.Henderson LJ, Johnson TP, Smith BR, et al. Presence of Tat and transactivation response element in spinal fluid despite antiretroviral therapy. AIDS. 2019;33(Suppl 2):S145–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anderson AM, Tyor WR, Mulligan MJ, Waldrop-Valverde D, Lennox JL, Letendre SL. HIV p24 antigen is quantifiable at low concentrations in human cerebrospinal fluid with digital ELISA and is associated with decreased neuropsychological performance. Clin Infect Dis. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Letendre S, Bharti A, Perez-Valero I, et al. Higher anti-cytomegalovirus immunoglobulin G concentrations are associated with worse neurocognitive performance during suppressive antiretroviral therapy. Clin Infect Dis. 2018;67:770–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bharti AR, McCutchan A, Deutsch R, et al. Latent Toxoplasma infection and higher Toxoplasma gondii immunoglobulin G levels are associated with worse neurocognitive functioning in HIV-infected adults. Clin Infect Dis. 2016;63:1655–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pulliam L, Gascon R, Stubblebine M, McGuire D, McGrath MS. Unique monocyte subset in patients with AIDS dementia. Lancet. 1997;349:692–5. [DOI] [PubMed] [Google Scholar]
- 35.Nockher WA, Bergmann L, Scherberich JE. Increased soluble CD14 serum levels and altered CD14 expression of peripheral blood monocytes in HIV-infected patients. Clin Exp Immunol. 1994;98:369–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cauwels A, Frei K, Sansano S, et al. The origin and function of soluble CD14 in experimental bacterial meningitis. J Immunol. 1999;162:4762–72. [PubMed] [Google Scholar]
- 37.Lyons JL, Uno H, Ancuta P, et al. Plasma sCD14 is a biomarker associated with impaired neurocognitive test performance in attention and learning domains in HIV infection. J Acquir Immune Defic Syndr. 2011;57:371–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kamat A, Lyons JL, Misra V, et al. Monocyte activation markers in cerebrospinal fluid associated with impaired neurocognitive testing in advanced HIV infection. J Acquir Immune Defic Syndr. 2012;60:234–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Imp BM, Rubin LH, Tien PC, et al. Monocyte activation is associated with worse cognitive performance in HIV-infected women with virologic suppression. J Infect Dis. 2017;215:114–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Manner IW, Baekken M, Kvale D, et al. Markers of microbial translocation predict hypertension in HIV-infected individuals. HIV Med. 2013;14:354–61. [DOI] [PubMed] [Google Scholar]
- 41.Hagberg L, Cinque P, Gisslen M, et al. Cerebrospinal fluid neopterin: an informative biomarker of central nervous system immune activation in HIV-1 infection. AIDS Res Ther. 2010;7:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yilmaz A, Price RW, Spudich S, Fuchs D, Hagberg L, Gisslen M. Persistent intrathecal immune activation in HIV-1-infected individuals on antiretroviral therapy. J Acquir Immune Defic Syndr. 2008;47:168–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Eden A, Marcotte TD, Heaton RK, et al. Increased intrathecal immune activation in virally suppressed HIV-1 infected patients with neurocognitive impairment. PloS one. 2016;11:e0157160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Burdo TH, Weiffenbach A, Woods SP, Letendre S, Ellis RJ, Williams KC. Elevated sCD163 in plasma but not cerebrospinal fluid is a marker of neurocognitive impairment in HIV infection. AIDS. 2013;27:1387–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Krebs SJ, Slike BM, Sithinamsuwan P, et al. Sex differences in soluble markers vary before and after the initiation of antiretroviral therapy in chronically HIV-infected individuals. AIDS. 2016;30:1533–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kuehne LK, Reiber H, Bechter K, Hagberg L, Fuchs D. Cerebrospinal fluid neopterin is brain-derived and not associated with blood-CSF barrier dysfunction in non-inflammatory affective and schizophrenic spectrum disorders. J Psychiatr Res. 2013;47:1417–22. [DOI] [PubMed] [Google Scholar]
- 47.Wada NI, Jacobson LP, Margolick JB, et al. The effect of HAART-induced HIV suppression on circulating markers of inflammation and immune activation. AIDS. 2015;29:463–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Selmaj KW, Raine CS. Tumor necrosis factor mediates myelin and oligodendrocyte damage in vitro. Ann Neurol. 1988;23:339–46. [DOI] [PubMed] [Google Scholar]
- 49.Burlacu R, Umlauf A, Marcotte TD, et al. Plasma CXCL10 correlates with HAND in HIV-infected women. J Neurovirol. 2020;26:23–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sevigny JJ, Albert SM, McDermott MP, et al. Evaluation of HIV RNA and markers of immune activation as predictors of HIV-associated dementia. Neurology. 2004;63:2084–90. [DOI] [PubMed] [Google Scholar]
- 51.Weaver JD, Huang MH, Albert M, Harris T, Rowe JW, Seeman TE. Interleukin-6 and risk of cognitive decline: Mac Arthur studies of successful aging. Neurology. 2002;59:371–8. [DOI] [PubMed] [Google Scholar]
- 52.Sas AR, Bimonte-Nelson H, Smothers CT, Woodward J, Tyor WR. Interferon-alpha causes neuronal dysfunction in encephalitis. J Neurosci. 2009;29:3948–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fritz-French C, Tyor W. Interferon-alpha (IFNalpha) neurotoxicity. Cytokine Growth Factor Rev. 2012;23:7–14. [DOI] [PubMed] [Google Scholar]
- 54.Anderson AM, Fennema-Notestine C, Umlauf A, et al. CSF biomarkers of monocyte activation and chemotaxis correlate with magnetic resonance spectroscopy metabolites during chronic HIV disease. J Neurovirol. 2015;21:559–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rho MB, Wesselingh S, Glass JD, et al. A potential role for interferon-alpha in the pathogenesis of HIV-associated dementia. Brain Behav Immun. 1995;9:366–77. [DOI] [PubMed] [Google Scholar]
- 56.Lehmann C, Taubert D, Jung N, et al. Preferential upregulation of interferon-alpha subtype 2 expression in HIV-1 patients. AIDS Res Hum Retroviruses. 2009;25:577–81. [DOI] [PubMed] [Google Scholar]
- 57.Cassol E, Misra V, Morgello S, Gabuzda D. Applications and limitations of inflammatory biomarkers for studies on neurocognitive impairment in HIV infection. J Neuroimmune Pharmacol. 2013;8:1087–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rubin LH, Benning L, Keating SM, et al. Variability in C-reactive protein is associated with cognitive impairment in women living with and without HIV: a longitudinal study. J Neurovirol. 2018;24:41–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gonzalez E, Rovin BH, Sen L, et al. HIV-1 infection and AIDS dementia are influenced by a mutant MCP-1 allele linked to increased monocyte infiltration of tissues and MCP-1 levels. Proc Natl Acad Sci USA. 2002;99:13795–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Agsalda-Garcia MA, Sithinamsuwan P, Valcour VG, et al. Brief Report: CD14+ enriched peripheral cells secrete cytokines unique to HIV-associated neurocognitive disorders. J Acquir Immune Defic Syndr. 2017;74:454–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Majumder S, Zhou LZ, Ransohoff RM. Transcriptional regulation of chemokine gene expression in astrocytes. J Neurosci Res. 1996;45:758–69. [DOI] [PubMed] [Google Scholar]
- 62.Stacey AR, Norris PJ, Qin L, et al. Induction of a striking systemic cytokine cascade prior to peak viremia in acute human immunodeficiency virus type 1 infection, in contrast to more modest and delayed responses in acute hepatitis B and C virus infections. J Virol. 2009;83:3719–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fabbiani M, Muscatello A, Perseghin P, et al. Brief Report: Peripheral monocyte/macrophage phenotypes associated with the evolution of cognitive performance in HIV-infected patients. J Acquir Immune Defic Syndr. 2017;76:219–24. [DOI] [PubMed] [Google Scholar]
- 64.Robertson K, Landay A, Miyahara S, et al. Limited correlation between systemic biomarkers and neurocognitive performance before and during HIV treatment. J Neurovirol. 2020;26:107–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Grauer OM, Reichelt D, Gruneberg U, et al. Neurocognitive decline in HIV patients is associated with ongoing T-cell activation in the cerebrospinal fluid. Ann Clin Transl Neurol. 2015;2:906–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Schrier RD, Hong S, Crescini M, et al. Cerebrospinal fluid (CSF) CD8+ T-cells that express interferon-gamma contribute to HIV associated neurocognitive disorders (HAND). PloS one. 2015;10:e0116526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Van Geel WJ, Rosengren LE, Verbeek MM. An enzyme immunoassay to quantify neurofilament light chain in cerebrospinal fluid. J Immunol Methods. 2005;296:179–85. [DOI] [PubMed] [Google Scholar]
- 68.Yilmaz A, Blennow K, Hagberg L, et al. Neurofilament light chain protein as a marker of neuronal injury: review of its use in HIV-1 infection and reference values for HIV-negative controls. Expert Rev Mol Diagn. 2017;17:761–70. [DOI] [PubMed] [Google Scholar]
- 69.Abdulle S, Mellgren A, Brew BJ, et al. CSF neurofilament protein (NFL) – a marker of active HIV-related neurodegeneration. J Neurol. 2007;254:1026–32. [DOI] [PubMed] [Google Scholar]
- 70.•.Guha D, Mukerji SS, Chettimada S, et al. CSF extracellular vesicles and neurofilament light protein as biomarkers of CNS injury in HIV-infected patients on antiretroviral therapy. AIDS. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gisslen M, Price RW, Andreasson U, et al. Plasma concentration of the neurofilament light protein (NFL) is a biomarker of CNS injury in HIV infection: a cross-sectional study. EBioMedicine. 2016;3:135–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Anderson AM, Easley KA, Kasher N, et al. Neurofilament light chain in blood is negatively associated with neuropsychological performance in HIV-infected adults and declines with initiation of antiretroviral therapy. J Neurovirol. 2018;24:695–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pulliam L, Sun B, Mustapic M, Chawla S, Kapogiannis D. Plasma neuronal exosomes serve as biomarkers of cognitive impairment in HIV infection and Alzheimer’s disease. J Neurovirol. 2019;25:702–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sun B, Fernandes N, Pulliam L. Profile of neuronal exosomes in HIV cognitive impairment exposes sex differences. AIDS. 2019;33:1683–92. [DOI] [PubMed] [Google Scholar]
- 75.Lasser M, Tiber J, Lowery LA. The role of the microtubule cytoskeleton in neurodevelopmental disorders. Front Cell Neurosci. 2018;12:165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shiomura Y, Hirokawa N. Colocalization of microtubule-associated protein 1A and microtubule-associated protein 2 on neuronal microtubules in situ revealed with double-label immunoelectron microscopy. J Cell Biol. 1987;104:1575–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shiomura Y, Hirokawa N. The molecular structure of microtubule-associated protein 1A (MAP1A) in vivo and in vitro. An immunoelectron microscopy and quick-freeze, deep-etch study. J Neurosci. 1987;7:1461–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Avdoshina V, Mahoney M, Gilmore SF, et al. HIV influences microtubule associated protein-2: potential marker of HIV-associated neurocognitive disorders. AIDS. 2020;34:979–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Brenchley JM, Price DA, Schacker TW, et al. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med. 2006;12:1365–71. [DOI] [PubMed] [Google Scholar]
- 80.Hoenigl M, de Oliveira MF, Perez-Santiago J, et al. (1–>3)-beta-D-glucan levels correlate with neurocognitive functioning in HIV-infected persons on suppressive antiretroviral therapy: a cohort study. Medicine. 2016;95:e3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Munoz-Nevarez LA, Imp BM, Eller MA, et al. Monocyte activation, HIV, and cognitive performance in East Africa. J Neurovirol. 2020;26:52–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Campbell JD, Moore D, Degerman R, et al. HIV-infected Ugandan adults taking antiretroviral therapy with CD4 counts >200 cells/muL who discontinue cotrimoxazole prophylaxis have increased risk of malaria and diarrhea. Clin Infect Dis. 2012;54:1204–11. [DOI] [PubMed] [Google Scholar]
- 83.Liang T, Ma C, Wang T, et al. Galectin-9 promotes neuronal restoration via binding TLR-4 in a rat intracerebral hemorrhage model. Neuromolecular Med. 2020. [DOI] [PubMed] [Google Scholar]
- 84.Premeaux TA, D’Antoni ML, Abdel-Mohsen M, et al. Elevated cerebrospinal fluid Galectin-9 is associated with central nervous system immune activation and poor cognitive performance in older HIV-infected individuals. J Neurovirol. 2019;25:150–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bandaru VV, Mielke MM, Sacktor N, et al. A lipid storage-like disorder contributes to cognitive decline in HIV-infected subjects. Neurology. 2013;81:1492–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bora A, Ubaida Mohien C, Chaerkady R, et al. Identification of putative biomarkers for HIV-associated neurocognitive impairment in the CSF of HIV-infected patients under cART therapy determined by mass spectrometry. J Neurovirol. 2014;20:457–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cassol E, Misra V, Dutta A, Morgello S, Gabuzda D. Cerebrospinal fluid metabolomics reveals altered waste clearance and accelerated aging in HIV patients with neurocognitive impairment. AIDS. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cysique LA, Brew BJ. Vascular cognitive impairment and HIV-associated neurocognitive disorder: a new paradigm. J Neurovirol. 2019;25:710–21. [DOI] [PubMed] [Google Scholar]
- 89.Kallianpur AR, Gittleman H, Letendre S, et al. Cerebrospinal fluid ceruloplasmin, haptoglobin, and vascular endothelial growth factor are associated with neurocognitive impairment in adults with HIV infection. Mol Neurobiol. 2019;56:3808–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Montoya JL, Iudicello J, Fazeli PL, et al. Elevated markers of vascular remodeling and arterial stiffness are associated with neurocognitive function in older HIV+ adults on suppressive antiretroviral therapy. J Acquir Immune Defic Syndr. 2017;74:134–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cantres-Rosario Y, Plaud-Valentin M, Gerena Y, Skolasky RL, Wojna V, Melendez LM. Cathepsin B and cystatin B in HIV-seropositive women are associated with infection and HIV-1-associated neurocognitive disorders. AIDS. 2013;27:347–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hileman CO, Azzam S, Schlatzer D, et al. Plasma citrate and succinate are associated with neurocognitive impairment in older people with HIV. Clin Infect Dis. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kalayjian RC, Robertson KR, Albert JM, et al. Plasma cystatin C associates with HIV-associated neurocognitive disorder but is a poor diagnostic marker in antiretroviral therapy-treated individuals. J Acquir Immune Defic Syndr. 2019;81:e49–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Marcotte TD, Deutsch R, Michael BD, et al. A concise panel of biomarkers identifies neurocognitive functioning changes in HIV-infected individuals. Journal of neuroimmune pharmacology : the official journal of the Society on Neuroimmune Pharmacol. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Rubin LH, Xu Y, Norris PJ, et al. Early inflammatory signatures predict subsequent cognition in long-term virally suppressed women with HIV. Front Integr Neurosci. 2020; 14:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hammond ER, Crum RM, Treisman GJ, et al. Persistent CSF but not plasma HIV RNA is associated with increased risk of new-onset moderate-to-severe depressive symptoms; a prospective cohort study. J Neurovirol. 2016;22:479–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zuniga JA, Harrison ML, Henneghan A, Garcia AA, Kesler S. Biomarkers panels can predict fatigue, depression and pain in persons living with HIV: a pilot study. Appl Nurs Res. 2020;52:151224. [DOI] [PubMed] [Google Scholar]
- 98.Rivera-Rivera Y, Garcia Y, Toro V, et al. Depression correlates with increased plasma levels of inflammatory cytokines and a dysregulated oxidant/antioxidant balance in HIV-1-infected subjects undergoing antiretroviral therapy. J Clin Cell Immunol .2014; 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Norcini Pala A, Steca P, Bagrodia R, et al. Subtypes of depressive symptoms and inflammatory biomarkers: an exploratory study on a sample of HIV-positive patients. Brain Behav Immun. 2016;56:105–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Musinguzi K, Obuku A, Nakasujja N, et al. Association between major depressive disorder and pro-inflammatory cytokines and acute phase proteins among HIV-1 positive patients in Uganda. BMC Immunol. 2018;19:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Poudel-Tandukar K, Bertone-Johnson ER, Palmer PH, Poudel KC. C-reactive protein and depression in persons with human immunodeficiency virus infection: the Positive Living with HIV (POLH) Study. Brain Behav Immun. 2014;42:89–95. [DOI] [PubMed] [Google Scholar]
- 102.•.Lu H, Surkan PJ, Irwin MR, et al. Inflammation and risk of depression in HIV: prospective findings from the Multicenter AIDS Cohort Study. Am J Epidemiol. 2019;188:1994–2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Stewart JC, Polanka BM, So-Armah KA, et al. Associations of total, cognitive/affective, and somatic depressive symptoms and antidepressant use with cardiovascular disease-relevant biomarkers in HIV: Veterans Aging Cohort Study. Psychosom Med. 2020;82:461–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.•.Saloner R, Cherner M, Grelotti DJ, et al. Lower CSF homovanillic acid relates to higher burden of neuroinflammation and depression in people with HIV disease. Brain Behav Immun. 2020;90:353–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ellis R Higher levels of plasma inflammation biomarkers are associated with depressed mood and quality of life in aging, virally suppressed men, but not women, with HIV. Brain Behav Immun. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Saloner R, Paolillo EW, Heaton RK, et al. Chronically elevated depressive symptoms interact with acute increases in inflammation to predict worse neurocognition among people with HIV. J Neurovirol. 2021;27:160–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


