Abstract
Loneliness is common in psychosis and occurs along a continuum. Here we investigate inter-relationships between loneliness, three-dimensional schizotypy, and depressive symptoms before and during the COVID-19 pandemic.
The sample included 507 university students (48.3% participated before and 51.7% during the COVID-19 pandemic) who completed the Multidimensional Schizotypy Scale-Brief, the Counseling Center Assessment of Psychological Symptoms depression scale and the University of California, Los Angeles Loneliness Scale. Schizotypy and depression scores were regressed onto loneliness individually and in multiple regressions.
The cohorts did not differ in any of the schizotypy domains (all p > .29). Depressive symptoms (p = .05) and loneliness (p = .006) were higher during the pandemic than before. Across cohorts, loneliness was significantly associated with positive (β = 0.23, p < .001), negative (β = 0.44, p < .001), and disorganised schizotypy (β = 0.44, p < .001), and with depression (β = 0.72, p < .001). Schizotypy together explained a significant amount of variance in loneliness (R2 = 0.26), with significant associations with positive (β = −0.09, p = .047), negative (β = 0.31, p < .001) and disorganised schizotypy (β = 0.34, p < .001). When depression was included (β = 0.69, p < .001), only positive (β = −0.09, p = .008) and negative schizotypy (β = 0.22, p < .001) significantly predicted loneliness.
When all schizotypy dimensions and depression were considered together, only negative schizotypy and depression significantly predicted loneliness. Loneliness and depressive symptoms were higher during the pandemic, but this did not relate to cohort differences in schizotypy.
Keywords: Loneliness, Schizotypy, Psychosis continuum, Depression, COVID-19
Highlights
-
•
Loneliness is uniquely associated with negative schizotypy and depression, but not disorganised schizotypy.
-
•
Certain aspects of positive schizotypy may protect against loneliness.
-
•
Loneliness and depressive symptoms were higher in students during the COVID-19 pandemic than before.
-
•
Cohorts of students assessed before and during the pandemic showed similar levels of schizotypy.
1. Introduction
Loneliness is defined as a distressing experience occurring when the quality or quantity of social relationships is perceived as insufficient to fulfil the social need (Hawkley, 2018). It refers to a subjective perception of social relations that is not necessarily related to objective social isolation. While often a transient experience, loneliness can become chronic. Initial feelings of loneliness are believed to function as a biological survival mechanism, guiding individuals to adjust their behaviours towards pro-sociality (Cacioppo et al., 2006). Through the unpleasant feeling, often described as the social equivalent of hunger or physical pain (Cacioppo and Hawkley, 2005), individuals are alarmed of their threatened social network and encouraged to tend to their social relationships. This mechanism might enhance the motivation to approach social situations and ensure that individuals stay part of the social flock (Cacioppo et al., 2006). However, loneliness also appears to have negative consequences, such as negative attributional biases, which increase an individual's focus on social threats and rejective social content. It has been shown that lonely people pay more visual attention to socially threatening stimuli (Bangee et al., 2014), and that they are quicker to differentiate socially threatening from non-threatening stimuli (Cacioppo et al., 2016). This enhanced attention to negative social stimuli can lead to a vicious cycle of loneliness, in which negative attributional biases enforce the perception of social threats, making it difficult to trust and to obtain social relationships (Cacioppo and Hawkley, 2005).
Given its implications for social threat perception, loneliness might be particularly problematic for individuals with schizophrenia, who often experience paranoia, which may be aggravated with increased social threats. Loneliness constitutes a significant problem in schizophrenia (Eglit et al., 2018; Lim et al., 2018; Michalska da Rocha et al., 2018). An estimated 80% of people with schizophrenia experience loneliness, which is markedly more than the estimate of 35% in the general population (Stain et al., 2012). Previous research has linked loneliness to both onset (Chau et al., 2019; Hoffman, 2007), and maintenance (Kwapil et al., 2012; Lim et al., 2018) of psychotic symptoms. Kwapil et al. (2012) suggested that the positive symptom dimension is characterised by an ambivalent need for social interactions; when alone, individuals with positive symptoms desire social company, but when with others they desire to be alone. Importantly, the desire to be alone was mostly a result of anxious fears of negative evaluation – and not due to lack of pleasure in social interactions. As loneliness constitutes the discrepancy between preferred and actual social interactions (Hawkley, 2018), it is likely that the ambivalent social need within the positive dimension inhibits optimal social functioning and confers specific vulnerability to loneliness. In accord with this, loneliness has been linked to paranoia in both clinical and non-clinical samples (Chau et al., 2019; Lamster et al., 2017a; Lamster et al., 2017b), and to social anxiety, depression, and even the onset of positive psychotic symptoms in healthy individuals (Le et al., 2019; Lim et al., 2016). On the other hand, the negative symptoms of schizophrenia might be associated with a complete loss of interest in social interactions, due to low social motivation (Rabinowitz et al., 2012; Robertson et al., 2014). However, as negative symptoms are characterised by avolition, anhedonia and asociality (American Psychiatric Association, 2013), contributing to a general disinterest in social interactions (Kwapil et al., 2012), it seems intuitive that those who experience more negative symptoms might be less prone to loneliness. In line with this, social anhedonia has been linked to a higher preference for solitude and it has been argued that the need to belong has gone awry in the socially anhedonic (Silvia and Kwapil, 2011).
Research on loneliness and psychotic symptomatology has made use of the psychosis continuum, ranging from subclinical schizotypal traits to full-blown clinical psychosis (Barrantes-Vidal et al., 2015; Kwapil and Barrantes-Vidal, 2015). Schizotypy is thought to reflect the vulnerability for schizophrenia, implying shared underlying etiology (Barrantes-Vidal et al., 2015; Kwapil and Barrantes-Vidal, 2015; Lenzenweger, 2018; Meehl, 1962), and thus representing a useful construct for modeling schizophrenia. Studies examining loneliness across the psychosis continuum have found stable associations with positive and negative schizotypal traits (Badcock et al., 2016; Chau et al., 2019; Le et al., 2019; Michalska da Rocha et al., 2018). However, research has largely neglected the disorganised symptom dimension (Kemp et al., 2018; Kwapil et al., 2020; Nelson et al., 2013). Disorganised symptoms comprise cognitive aspects and include communication and attention difficulties which may hinder appropriate social communication. Furthermore, impairments in social cognitive processes (e.g., mentalising, emotion recognition, and social perception) have been linked to severity of disorganised symptoms (de Sousa et al., 2019), which may complicate the ability to interpret social situations. Disorganised symptoms have been found to predict social functioning impairments in both occupational and leisure settings in at-risk psychosis patients (Eslami et al., 2011). Therefore, it seems plausible that disorganised symptoms may contribute to loneliness. Conversely, it is possible that loneliness confers a risk for disorganised symptoms, as suggested by longitudinal studies linking loneliness to subsequent cognitive decline (Hannemann et al., 2020; Lara et al., 2019; Zhou et al., 2019). Due to the heterogeneity of schizotypy, the degree to which the different symptom dimensions link to loneliness is important. However, more research is needed to establish the associations between loneliness and the different schizotypy dimensions, in particularly the disorganised dimension.
The ongoing corona-virus disease (COVID-19) pandemic has demonstrated the impact of reduced social interactions on mental health. People were isolated from social and occupational settings, and some have had to isolate due to risk of contracting the disease. Social distancing measures had a noticeable toll on mental health (Esteves et al., 2021; Jia et al., 2020; Loades et al., 2020; Savage et al., 2020). A recent review by the COVID-19 Mental Disorders Collaborators (Santomauro et al., 2021) has estimated that the prevalence of major depressive disorder has increased by 27.6%, while anxiety disorders increased by 25.6% globally. The pandemic has offered a natural opportunity for examining the relationship between loneliness and schizotypy (Daimer et al., 2021). We therefore investigated the association between loneliness and positive, negative, and disorganised schizotypy before and during the pandemic.
We hypothesized that loneliness would be associated with all three dimensions of schizotypy. Based on previous associations between paranoia and loneliness, as well as anxious avoidance of social situations despite a desire to engage, positive schizotypy was expected to be positively associated with loneliness. Negative schizotypy was expected to be negatively associated with loneliness, due to suggestions of a higher preference for solitude, diminished need to belong and low social motivation. Furthermore, we expected a positive association between disorganised schizotypy and loneliness, due to hypothesized difficulties with adequate responding to social cues. To understand the relationship between loneliness and negative schizotypy, it is important to acknowledge the overlap between negative and depressive symptoms. Symptoms including amotivation, avolition, anhedonia and anergia are thought to occur within both domains (Krynicki et al., 2018) and constitute a conceptual overlap which makes it difficult to distinguish between depressive and negative symptoms. Also, loneliness has been associated with depression in previous research (e.g., (Erzen and Çikrikci, 2018; Qualter et al., 2010)). Therefore, we included a measure of depressive symptoms to account for the overlap with negative schizotypy.
2. Method
2.1. Sample
The sample consisted of 507 students from City University of London (90.3% females, 9.3% males, and 0.4% others), aged 17–54 (M = 19.75, SD = 3.62). Data for 245 participants (48.3%) was collected in between November and January 2020 (before the pandemic), while data for the remaining 262 (51.7%) participants was collected between November and January 2021 (during the pandemic). Participants were recruited through a university call conducted through email, campus news and social media. Questionnaires were presented online using the Qualtrics software. Participants were required to be above 17 years old and fluent in English. All participants gave informed consent prior to participation. This study was approved by the City University of London Psychology Ethics Committee.
2.2. Measures
2.2.1. Schizotypal traits
The Multidimensional Schizotypy Scale-Brief (MSS-B) (Gross et al., 2018), was used to assess positive, negative, and disorganised schizotypy. The scale comprises 38 questions of which 13 items measure positive, 13 negative, and 12 disorganised traits. Participants rate each question as either (1) “True” or (0) “False”, and a higher score indicates higher trait-schizotypy. All three subscales showed good internal consistency: positive α = 0.79, negative α = 0.74 and disorganised α = 0.89.
2.2.2. Loneliness
Loneliness was measured using the University of California, Los Angeles (UCLA) Loneliness Scale Version 3 (Russell, 1996). The scale comprises 20 items. Participants rate each question of a scale from 1 (never) to 2 (often), and a higher total score indicates higher loneliness. The UCLA scale showed good internal consistency in the current sample α = 0.90.
2.2.3. Depression
The Counseling Center Assessment of Psychological Symptoms (CCAPS-62) was used to measure depression (Locke et al., 2011). The depression subscale includes 13 items such as “I feel worthless” and “I have thoughts of ending my life” for which participants respond on a 5-point Likert scale ranging from 0 (not at all like me) to 4 (extremely like me). The CCAPS-62 depression subscale showed good internal consistency in the current sample α = 0.85.
2.2.4. Statistical analyses
Statistical analyses were conducted using SPSS 27. Independent sample t-tests were used to investigate differences in MSS-B, UCLA, and CCAPS-62 depression scores between cohorts, i.e. before (pre-COVID-19) and during the pandemic (during COVID-19). Regression analyses were conducted on (1) positive schizotypy and loneliness, (2) negative schizotypy and loneliness, (3) disorganised schizotypy and loneliness, and (4) depressive symptoms and loneliness. Interaction terms between cohort and the three schizotypy dimensions and depression were added to the regression models to examine whether the relationships differed between cohorts. Finally, all schizotypy dimensions and depression were entered in a multiple regression analysis to examine their unique contribution to loneliness. We report standardized regression coefficients. Intercorrelations between all variables are reported.
3. Results
3.1. Sample characteristics
Sample characteristics are displayed in Table 1. Participants showed higher loneliness [t(504) = −2.78, p = .006], and depressive symptoms [t(501) = −1.97, p = .049], during compared to before the COVID-19 pandemic. There were no significant cohort differences in positive t(492) = −1.05, p = .29, negative [t(492) = −1.01, p = .31], or disorganised schizotypy [t(492) = −0.59, p = .55].
Table 1.
Participant characteristics.
| Pre-COVID-19 Cohort (N = 245) | During COVID-19 Cohort (N = 262) | Combined cohorts (N = 507) |
|
|---|---|---|---|
| Age, mean (SD) [range] | 19.92 (4.53) [18–50] | 19.71 (3.43) [17–54] | 19.75 (3.62) [17–54] |
| Gender (N%) | |||
| Female | 220 (89.8%) | 238 (90.8%) | 458 (90.3%) |
| Male | 24 (9.8%) | 23 (8.8%) | 47 (9.3%) |
| Other | 1 (0.4%) | 1 (0.4%) | 2 (0.4%) |
| Ethnicity, N(%) | |||
| Black/Black British | 20 (8.2%) | 20 (7.6%) | 40 (7.9%) |
| Asian/Asian British | 103 (42.2%) | 114 (43.5%) | 217 (42.9%) |
| White/White British | 85 (34.8%) | 82 (31.3%) | 167 (33.0%) |
| Mixed/other/prefer not to say | 37 (15.1%) | 46 (17.5%) | 82 (16.2%) |
| UCLA loneliness, mean (SD) [range] | 41.26 (0.10) [22–73] | 43.84 (10.37) [22-73]⁎ | 42.59 (10.5) [22–73] |
| MSS-B, mean (SD) [range] | |||
| Positive schizotypy | 3.02 (2.98) | 3.29 (2.86) | 3.16 (2.92) [0−13] |
| Negative schizotypy | 2.83 (2.65) | 3.07 (2.66) | 2.96 (2.66) [0−12] |
| Disorganised schizotypy | 3.29 (3.61) | 3.48 (3.50) | 3.39 (3.56) [0–12] |
| CCAPS-62 depression, mean (SD) [range] | 1.48 (0.91) | 1.64 (0.90)⁎ | 1.57 (0.91) [0–3.92] |
Abbreviations: UCLA; University of California Los Angeles Loneliness Scale version-3. MSS-B; Multidimensional Schizotypy-Scale Brief. CCAPS; Counseling Center Assessment of Psychological Symptoms.
Significant at p < .05.
3.2. Relationships between loneliness and schizotypy
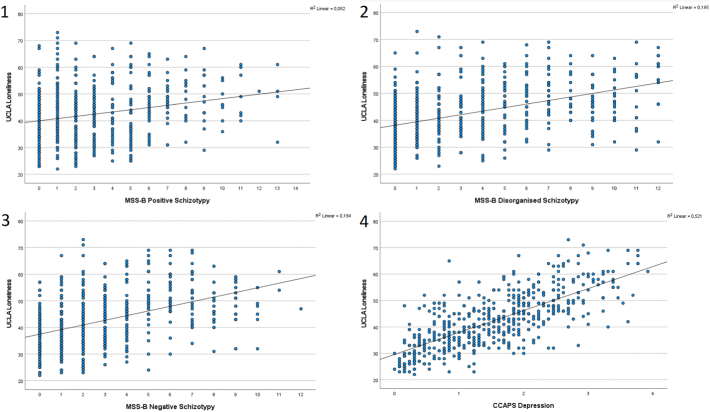
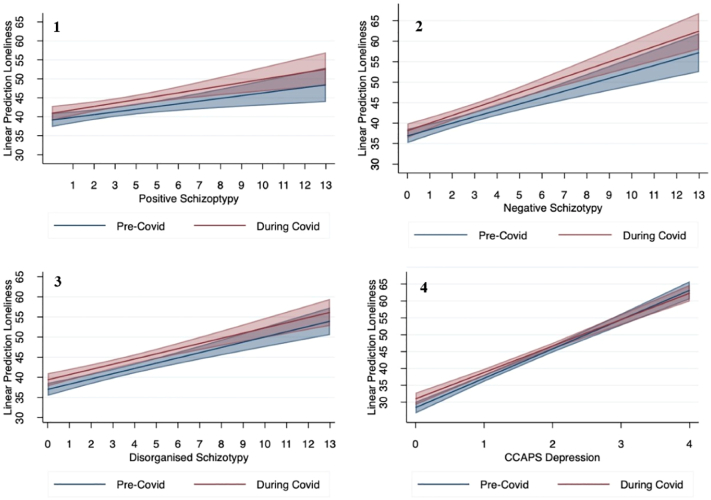
Intercorrelations between all variables are reported in Table 2. Simple regression analyses showed that loneliness was significantly associated with all three schizotypy dimensions, most strongly with negative [β = 0.44, t(493) = 10.87, p < .001, 95% CI (0.36–0.52), Fig. 1], and disorganised schizotypy [β 0.44, t(493) = 10.90, p < .001, 95% CI (0.36–0.52), Fig. 1], and to a lesser extent with positive schizotypy [β = 0.23, t(493) = 5.22, p < .001, 95% CI (0.14–0.32), Fig. 1]. To explore whether the strength of the relationships between loneliness and schizotypy varied between cohorts, interactions between the three schizotypy dimensions, depression, and loneliness were added to the models. All interactions were non-significant (positive schizotypy [β = 0.05, t(493) = 0.58, p = .57], negative schizotypy [β = 0.07,t(493) = 0.96, p = .34], disorganised schizotypy [β = −0.01,t(493) = −0.07, p = .95], see Table 3 and Fig. 2). Therefore, for the multiple regression analysis cohorts were grouped together. The multiple regression analysis modelled the relationship between loneliness and all three schizotypy dimensions. Schizotypy explained a significant amount of variance in loneliness (F(3,493) = 58.43, p < .001, R2 = 0.26, R2Adjusted = 0.26). Negative schizotypy [(β = 0.31, t(493) = 6.72, p < .001), 95% CI (0.21–0.39)], disorganised schizotypy [(β = 0.34, t(493) = 6.69, p < .001), 95% CI (0.24–0.44)], and positive schizotypy [(β = −0.09, t(493) = −1.99, p = .047), 95% CI (−0.19–0.01)] significantly predicted loneliness.
Table 2.
Intercorrelations, multicollinearity statistics and internal consistency for all scales.
| Multicollinearity (Tolerance, VIF) | Internal consistency (α) | 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|---|---|
| 1. Positive schizotypy | 0.65 (1.55) | 0.79 | 1 | ||||
| 2. Negative schizotypy | 0.71 (1.42) | 0.74 | 0.42⁎⁎ | 1 | |||
| 3. Disorganised schizotypy | 0.41 (2.17) | 0.89 | 0.58⁎⁎ | 0.51⁎⁎ | 1 | ||
| 4. UCLA loneliness | – | 0.90 | 0.23⁎⁎ | 0.44⁎⁎ | 0.44⁎⁎ | 1 | |
| 5. CCAPS depression | 0.63 (1.59) | 0.85 | 0.36⁎⁎ | 0.40⁎⁎ | 0.60⁎ | 0.72⁎⁎ | 1 |
Abbreviations: UCLA: University of California Los Angeles; MSS-B: multidimensional schizotypy-scale brief; CCAPS: Counseling Center Assessment of Psychological Symptoms.
Significant at p < .001.
Fig. 1.
Relationship between scores on the University of California (UCLA) loneliness scale and 1) positive, 2) disorganised, 3) negative schizotypy (MSS-B) and 4) depression (CCAPS).
Table 3.
Regression of schizotypy on loneliness by cohort.
| Dependent variable: UCLA Loneliness |
Pre-COVID cohort |
During COVID cohort |
||
|---|---|---|---|---|
| Predictor variable | β (95% CI) | p | β (95% CI) | p |
| MSS-B | ||||
| Positive schizotypy | 0.20 (0.08–0.32) | 0.002 | 0.25 (0.12–0.37) | <0.001 |
| Negative schizotypy | 0.39 (0.28–0.51) | <0.001 | 0.47 (0.36–0.58) | <0.001 |
| Disorganised schizotypy | 0.44 (0.33–0.55) | <0.001 | 0.43 (0.32–0.54) | <0.001 |
| CCAPS depression | 0.76 (0.66–0.83) | <0.001 | 0.68 (0.59–0.77) | <0.001 |
Abbreviations: MSS-B: multidimensional schizotypy-scale brief; CCAPS: Counseling Center Assessment of Psychological Symptoms.
Fig. 2.
Linear regression of schizotypy and depression on University of California (UCLA) loneliness scores for the pre-COVID-19 (blue) and during COVID-19 cohort (red) with 95% confidence intervals. (1) Multidimensional Schizotypy Scale-Brief (MSS-B) positive schizotypy, (2) MSS-B negative schizotypy, (3) MSS-B disorganised schizotypy, and (4) Counseling Center Assessment of Psychological Symptoms (CCAPS) depression. Overlap of confidence intervals is represented by the shaded middle area.
3.3. Relationships between loneliness, schizotypy and depression
Simple regression analysis showed a significant association between depression and loneliness [β = 0.72, t(502) = 23.33, p < .001, 95% CI (0.66–0.78), Fig. 1]. The interaction between cohort year and depression was not significant [β = -0.09,t(499) = −1.21, p = .27]. Therefore, for the multiple regression analysis cohorts were grouped together. The model included loneliness, all three schizotypy dimensions and depression. Schizotypy and depression explained a significant amount of variance in loneliness (F(4,493) = 158.25, p < .001, R2 = 0.56, R2Adjusted = 0.56). Depression was the strongest predictor of loneliness, [(β = 0.69, t(493) = 18.37, p < .001), 95% CI (0.62–0.77)]. Positive schizotypy [(β = −0.09, t(493) = −2.65, p = .008), 95% CI (−0.17 – -0.03)] and negative schizotypy [(β = 0.22, t(493) = 6.19, p = .001), 95% CI (0.15–0.29)] also significantly predicted loneliness. Disorganised schizotypy [(β = −0.03, t(493) = −0.62, p = .53), 95% CI (−0.11–0.06)] no longer predicted loneliness significantly.
4. Discussion
This study investigated the relationship between loneliness and positive, negative, and disorganised schizotypy in two cohorts of students prior to and during the COVID-19 pandemic. All schizotypy domains were individually associated with loneliness. In contrast to our hypothesis the strongest effects were present for negative and disorganised schizotypy. When all three domains were included in the model, the association with positive schizotypy reversed. When depression was accounted for, negative schizotypy remained a significant contributor to loneliness, thus highlighting negative schizotypy as a potential risk factor for loneliness. Disorganised schizotypy was no longer significantly related to loneliness. We found higher levels of loneliness and depressive symptoms in participants who completed the study during the pandemic, supporting findings of others (Esteves et al., 2021; Jia et al., 2020; Killgore et al., 2020; Li et al., 2020; Palgi et al., 2020). However, this was not dependent on the level of schizotypy, which did not differ between cohorts.
4.1. The role of schizotypy in loneliness
In line with a proposed relationship between psychosis proneness and loneliness (Chau et al., 2019; Hoffman, 2007; Lim et al., 2018), we found significant individual relationships between higher scores on the three dimensions of schizotypy and loneliness. Notably, the largest effect sizes occurred for negative and disorganised schizotypy, underlining the importance of cognitive disorganisation and social motivation with respect to perceived social isolation. The positive association between disorganised schizotypy and loneliness is in line with previously established links, where disorganised schizotypy has been associated with greater emotional ambivalence, communication disturbances, increased reactivity to negative affect, lower cognitive control (Kerns, 2006; Kerns and Becker, 2008; Minor and Cohen, 2010), and social functioning impairments in individuals at-risk for psychosis (Eslami et al., 2011). Indeed, the ability to self-regulate thoughts, emotions and behaviour is thought to be vital for successful social functioning (Hawkley and Cacioppo, 2010). Findings that planning and working memory functions predict loneliness in elderly (Sin et al., 2021) lend further support to this. Thus, disorganisation may affect the ability to follow conversations and interact in socially appropriate ways, which in turn may foster loneliness. Conversely, it is also possible that loneliness contributes to disorganised schizotypy, for example by accelerating cognitive decline, which has previously been linked to loneliness in older adults (Boss et al., 2015; Lara et al., 2019; Tilvis et al., 2004). Several longitudinal studies have found associations between loneliness and decreased cognitive function at follow-up (Hannemann et al., 2020; Lara et al., 2019; Zhou et al., 2019), but mechanisms remain largely unknown (Kidambi and Lee, 2020). However, in the current sample of younger individuals the findings do not seem to support the notion that loneliness is causally related to disorganised schizotypy, given the significantly higher levels of loneliness in the face of stable levels of disorganised schizotypy across cohorts. The current data is cross-sectional and the results should be interpreted with caution. Longitudinal and experimental investigations are needed to investigate this question further.
Given that negative schizotypy is characterised by avolition, anhedonia and asociality (Kwapil et al., 2018), which may contribute to a general disinterest in social interactions (Silvia and Kwapil, 2011), it was expected to constitute a lower social need and a higher preference for solitude. In line with this negative symptoms have been established as important predictor of social functioning in chronic psychosis (Kaneko, 2018; Strauss et al., 2012; Weinberg et al., 2009), and in at-risk populations (Corcoran et al., 2011; Schlosser et al., 2015). Our finding that higher negative symptoms are related to higher loneliness was unexpected and suggests that negative symptoms do not change perceived ideals of social interactions (e.g., wanting to interact socially with friends). Alternatively, and in line with a possible relationship between the negative symptom dimension and salience (Chun et al., 2019), a lack of reward associated with negative symptoms may constitute a vulnerability for loneliness, rather than a diminished social need (Chun et al., 2019; Kwapil et al., 2012). That is, negative symptoms may diminish the rewarding effects of social interactions while leaving the need for social interaction unaffected. If increased schizotypy can be explained by attenuated expected pleasure (motivation) or attenuated pleasure derived from social interactions, conventional anti-loneliness strategies might not be effective in reducing loneliness in this population (Bessaha et al., 2020).
A further possible explanation for the link between higher loneliness and negative schizotypy is that negative schizotypy overlaps with depression (Matthews et al., 2016). Social disinterest, low social motivation and apathy are shared core characteristics (Edwards et al., 2019). We found the strongest association between loneliness and the CCAPS-62 depression subscale. Other research in university students with high and low schizotypy found that the diminished pleasure and motivational deficits, which are characteristic of the negative schizotypy dimension (Silvia and Kwapil, 2011), were fully mediated by depressive symptoms (Campellone et al., 2016). Importantly, in our study the strength of the association between negative schizotypy and loneliness was slightly reduced, but negative schizotypy remained a significant predictor of loneliness when depressive symptoms were accounted for. Thus, the relationship between negative schizotypy and loneliness cannot be fully explained by an overlap with depressive symptoms and highlights a unique role with respect to loneliness. Our finding that depressive symptoms accounted for the association between loneliness and disorganised schizotypy is in line with a previous study (Jaya et al., 2017), and may reflect the cognitive effects of depression (Rock et al., 2014).
Our results showed that higher positive schizotypy is related to higher loneliness when examined individually, as previously shown (Lamster et al., 2017b; Riggio and Kwong, 2009; Sündermann et al., 2014). Surprisingly, we found that positive schizotypy was associated with lower loneliness when negative and disorganised dimensions and depression were accounted for. This may be due to a suppressor effect (Paulhus et al., 2004). The shared variance caused by overlap between dimensions is removed, revealing a unique association between positive schizotypy and lower loneliness. A similar pattern was observed in a recent experience-sampling study measuring social functioning and affect across schizotypal dimensions (Kwapil et al., 2020). The potential protective effects of positive schizotypy against loneliness may be explained by aspects, such as magical thinking, which has been linked to creativity, well-being, openness to experience and spiritual connectedness (Badzakova-Trajkov et al., 2011; Crespi et al., 2019; Mohr and Claridge, 2015; Polner et al., 2018). In healthy individuals, magical thinking may function as a cognitive defence mechanism, by which individuals attempt to rationalise about the uncertainties of life (Williams and Irwin, 1991). This mechanism may be governed by an adaptive cognitive style, by which individuals allow rational thinking and magical thinking to complement each other. By contrast, individuals high in disorganised schizotypy and those with schizophrenia may lack the cognitive reasoning ability needed to meaningfully integrate magical experiences in an adaptive framework, and instead tend to attribute such experiences to randomness (Williams and Irwin, 1991). In support of this theory, the association between schizotypy and affective response to paranormal experiences has been found to be moderated by cognitive disorganisation (Schofield and Claridge, 2007). It has been reported that individuals with high cognitive disorganisation describe their paranormal experiences as distressing, whereas those with low cognitive disorganisation describe them as pleasant (Schofield and Claridge, 2007). Others reported associations between magical thinking and odd beliefs and the tendency to believe in conspiracy theories was mediated by the degree of analytical thinking (Barron et al., 2018). This highlights a potentially protective role of paranormal beliefs and magical thinking, as moderated by cognitive organisation. If the link between positive schizotypy and increased loneliness is indeed mediated by disorganised schizotypy, a larger focus on cognitive remediation strategies may be useful to target loneliness within this population.
4.2. COVID-19 and mental health
Our findings that loneliness and depressive symptoms were higher during the COVID-19 pandemic than before are in line findings of others (Esteves et al., 2021; Jia et al., 2020; Killgore et al., 2020; Li et al., 2020; Palgi et al., 2020). This underlines the negative impact of the pandemic on mental health in students, which likely depends on many factors. Participants who were assessed during the pandemic may have differed in terms of perceived risk of developing a mental health problem and loneliness, as well as in their willingness to talk about it, due to an increased focus on these topics in the media. Such media coverage may have primed participants to answer a certain way, however it may also have increased the awareness about mental health in general, which may have reduced stigmatisation and in turn increased individuals' willingness to admit to experiencing challenges. It may be useful for future studies to explore perceptions of mental health stigmatisation and prevalence, to gain further insights into these mechanisms.
4.3. Conclusion
Loneliness was associated with all three schizotypy dimensions individually, but when examined in conjunction it was most strongly associated with negative schizotypy and depression. This highlights the importance of investigations into the three-dimensional model of schizotypy to gain a better understanding of loneliness across the psychosis continuum and suggests that social motivation and anhedonia could be key targets for loneliness interventions. Further research is necessary to examine the directionality of effects.
CRediT authorship contribution statement
RC, CH, SG, AF: conception and design of the study, or acquisition of data, and interpretation of data.
RC, AF: data analysis.
Declaration of competing interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- American Psychiatric Association . American Psychiatric Association; Arlington, VA: 2013. Diagnostic and Statistical Manual of Mental Disorders : DSM-5. [Google Scholar]
- Badcock J.C., Barkus E., Cohen A.S., Bucks R., Badcock D.R. Loneliness and schizotypy are distinct constructs, separate from general psychopathology. Front. Psychol. 2016;7:1018. doi: 10.3389/fpsyg.2016.01018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badzakova-Trajkov G., Häberling I.S., Corballis M.C. Magical ideation, creativity, handedness, and cerebral asymmetries: a combined behavioural and fMRI study. Neuropsychologia. 2011;49(10):2896–2903. doi: 10.1016/j.neuropsychologia.2011.06.016. [DOI] [PubMed] [Google Scholar]
- Bangee M., Harris R.A., Bridges N., Rotenberg K.J., Qualter P. Loneliness and attention to social threat in young adults: findings from an eye tracker study. Personal. Individ. Differ. 2014;63:16–23. [Google Scholar]
- Barrantes-Vidal N., Grant P., Kwapil T.R. The role of schizotypy in the study of the etiology of schizophrenia spectrum disorders. Schizophr. Bull. 2015;41 Suppl 2(Suppl. 2):S408–S416. doi: 10.1093/schbul/sbu191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barron D., Furnham A., Weis L., Morgan K.D., Towell T., Swami V. The relationship between schizotypal facets and conspiracist beliefs via cognitive processes. Psychiatry Res. 2018;259:15–20. doi: 10.1016/j.psychres.2017.10.001. [DOI] [PubMed] [Google Scholar]
- Bessaha M.L., Sabbath E.L., Morris Z., Malik S., Scheinfeld L., Saragossi J. A systematic review of loneliness interventions among non-elderly adults. Clin. Soc. Work. J. 2020;48(1):110–125. [Google Scholar]
- Boss L., Kang D.-H., Branson S. Loneliness and cognitive function in the older adult: a systematic review. Int. Psychogeriatr. 2015;27(4):541–553. doi: 10.1017/S1041610214002749. [DOI] [PubMed] [Google Scholar]
- Cacioppo J.T., Hawkley L.C. People Thinking About People: The Vicious Cycle of Being a Social Outcast in One's Own Mind, The Social Outcast: Ostracism, Social Exclusion, Rejection, and Bullying. Psychology Press; New York, NY, US: 2005. pp. 91–108. [Google Scholar]
- Cacioppo Hawkley, Ernst J.M., Burleson M., Berntson G.G., Nouriani B., Spiegel D. Loneliness within a nomological net: an evolutionary perspective. J. Res. Pers. 2006;40(6):1054–1085. [Google Scholar]
- Cacioppo S., Bangee M., Balogh S., Cardenas-Iniguez C., Qualter P., Cacioppo J.T. Loneliness and implicit attention to social threat: a high-performance electrical neuroimaging study. Cogn. Neurosci. 2016;7(1–4):138–159. doi: 10.1080/17588928.2015.1070136. [DOI] [PubMed] [Google Scholar]
- Campellone T.R., Elis O., Mote J., Sanchez A.H., Kring A.M. Negative symptoms in psychometrically defined schizotypy: the role of depressive symptoms. Psychiatry Res. 2016;240:181–186. doi: 10.1016/j.psychres.2016.04.020. [DOI] [PubMed] [Google Scholar]
- Chau, Zhu C., So S.H. Loneliness and the psychosis continuum: a meta-analysis on positive psychotic experiences and a meta-analysis on negative psychotic experiences. Int. Rev. Psychiatry. 2019;31(5-6):471–490. doi: 10.1080/09540261.2019.1636005. [DOI] [PubMed] [Google Scholar]
- Chun C.A., Brugger P., Kwapil T.R. Aberrant salience across levels of processing in positive and negative schizotypy. Front. Psychol. 2019;10:2073. doi: 10.3389/fpsyg.2019.02073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corcoran C.M., Kimhy D., Parrilla-Escobar M.A., Cressman V.L., Stanford A.D., Thompson J., David S.B., Crumbley A., Schobel S., Moore H., Malaspina D. The relationship of social function to depressive and negative symptoms in individuals at clinical high risk for psychosis. Psychol. Med. 2011;41(2):251–261. doi: 10.1017/S0033291710000802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crespi B., Dinsdale N., Read S., Hurd P. Spirituality, dimensional autism, and schizotypal traits: the search for meaning. PLOS ONE. 2019;14(3) doi: 10.1371/journal.pone.0213456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daimer S., Mihatsch L., Ronan L., Murray G.K., Knolle F. Subjective impact of the COVID-19 pandemic on schizotypy and general mental health in Germany and the United Kingdom, for independent samples in May and in October 2020. Front. Psychol. 2021;12:667848. doi: 10.3389/fpsyg.2021.667848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Sousa P., Sellwood W., Griffiths M., Bentall R.P. Disorganisation, thought disorder and socio-cognitive functioning in schizophrenia spectrum disorders. Br. J. Psychiatry. 2019;214(2):103–112. doi: 10.1192/bjp.2018.160. [DOI] [PubMed] [Google Scholar]
- Edwards C.J., Garety P., Hardy A. The relationship between depressive symptoms and negative symptoms in people with non-affective psychosis: a meta-analysis. Psychol. Med. 2019;49(15):2486–2498. doi: 10.1017/S0033291719002381. [DOI] [PubMed] [Google Scholar]
- Eglit G.M.L., Palmer B.W., Martin A.S., Tu X., Jeste D.V. Loneliness in schizophrenia: construct clarification, measurement, and clinical relevance. PLoS One. 2018;13(3) doi: 10.1371/journal.pone.0194021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erzen E., Çikrikci Ö. The effect of loneliness on depression: a meta-analysis. Int. J. Soc. Psychiatry. 2018;64(5):427–435. doi: 10.1177/0020764018776349. [DOI] [PubMed] [Google Scholar]
- Eslami A., Jahshan C., Cadenhead K.S. Disorganized symptoms and executive functioning predict impaired social functioning in subjects at risk for psychosis. J. Neuropsychiatr. Clin. Neurosci. 2011;23(4):457–460. doi: 10.1176/appi.neuropsych.23.4.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esteves C.S., Oliveira C.R.D., Argimon I.I.D.L. Social distancing: prevalence of depressive, anxiety, and stress symptoms among Brazilian students during the COVID-19 pandemic. Frontiers in Public Health. 2021;8(923) doi: 10.3389/fpubh.2020.589966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross G.M., Kwapil T.R., Raulin M.L., Silvia P.J., Barrantes-Vidal N. The multidimensional schizotypy scale-brief: scale development and psychometric properties. Psychiatry Res. 2018;261:7–13. doi: 10.1016/j.psychres.2017.12.033. [DOI] [PubMed] [Google Scholar]
- Hannemann T.V., Bristle J., Wagner M. Cognition, loneliness and social isolation: a cross-national, longitudinal exploration. Eur. J. Pub. Health. 2020;30(Supplement_5) [Google Scholar]
- Hawkley L. 2018. Loneliness, Encyclopædia Britannica Encyclopedia Britannica.https://www.britannica.com/science/loneliness [Google Scholar]
- Hawkley L.C., Cacioppo J.T. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann. Behav. Med. 2010;40(2):218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman R.E. A social deafferentation hypothesis for induction of active schizophrenia. Schizophr. Bull. 2007;33(5):1066–1070. doi: 10.1093/schbul/sbm079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaya E., Hillmann T., Reininger K., Gollwitzer A., Lincoln T. Loneliness and psychotic symptoms: the mediating role of depression. Cogn. Ther. Res. 2017;41:1–11. [Google Scholar]
- Jia R., Ayling K., Chalder T., Massey A., Broadbent E., Coupland C., Vedhara K. Mental health in the UK during the COVID-19 pandemic: cross-sectional analyses from a community cohort study. BMJ Open. 2020;10(9) doi: 10.1136/bmjopen-2020-040620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaneko K. Negative symptoms and cognitive impairments in schizophrenia: two key symptoms negatively influencing social functioning. Yonago Acta Med. 2018;61(2):91–102. doi: 10.33160/yam.2018.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp K.C., Gross G.M., Barrantes-Vidal N., Kwapil T.R. Association of positive, negative, and disorganized schizotypy dimensions with affective symptoms and experiences. Psychiatry Res. 2018;270:1143–1149. doi: 10.1016/j.psychres.2018.10.031. [DOI] [PubMed] [Google Scholar]
- Kerns J.G. Schizotypy facets, cognitive control, and emotion. J. Abnorm. Psychol. 2006;115(3):418–427. doi: 10.1037/0021-843X.115.3.418. [DOI] [PubMed] [Google Scholar]
- Kerns J.G., Becker T.M. Communication disturbances, working memory, and emotion in people with elevated disorganized schizotypy. Schizophr. Res. 2008;100(1):172–180. doi: 10.1016/j.schres.2007.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kidambi N., Lee E.E. Insight into potential mechanisms linking loneliness and cognitive decline: commentary on "Health factors as potential mediator the longitudinal effect of loneliness on general cognitive ability". Am. J. Geriatr. Psychiatry. 2020;28(12):1284–1286. doi: 10.1016/j.jagp.2020.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore W.D.S., Cloonan S.A., Taylor E.C., Lucas D.A., Dailey N.S. Loneliness during the first half-year of COVID-19 lockdowns. Psychiatry Res. 2020;294 doi: 10.1016/j.psychres.2020.113551. [DOI] [PubMed] [Google Scholar]
- Krynicki C.R., Upthegrove R., Deakin J.F.W., Barnes T.R.E. The relationship between negative symptoms and depression in schizophrenia: a systematic review. Acta Psychiatr. Scand. 2018;137(5):380–390. doi: 10.1111/acps.12873. [DOI] [PubMed] [Google Scholar]
- Kwapil T.R., Barrantes-Vidal N. Schizotypy: looking back and moving forward. Schizophr. Bull. 2015;41 Suppl 2(Suppl. 2):S366–S373. doi: 10.1093/schbul/sbu186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwapil T.R., Brown L.H., Silvia P.J., Myin-Germeys I., Barrantes-Vidal N. The expression of positive and negative schizotypy in daily life: an experience sampling study. Psychol. Med. 2012;42(12):2555–2566. doi: 10.1017/S0033291712000827. [DOI] [PubMed] [Google Scholar]
- Kwapil T.R., Gross G.M., Silvia P.J., Raulin M.L., Barrantes-Vidal N. Development and psychometric properties of the multidimensional schizotypy scale: a new measure for assessing positive, negative, and disorganized schizotypy. Schizophr. Res. 2018;193:209–217. doi: 10.1016/j.schres.2017.07.001. [DOI] [PubMed] [Google Scholar]
- Kwapil T.R., Kemp K.C., Mielock A., Sperry S.H., Chun C.A., Gross G.M., Barrantes-Vidal N. Association of multidimensional schizotypy with psychotic-like experiences, affect, and social functioning in daily life: comparable findings across samples and schizotypy measures. J. Abnorm. Psychol. 2020;129(5):492–504. doi: 10.1037/abn0000522. [DOI] [PubMed] [Google Scholar]
- Lamster F., Lincoln T.M., Nittel C.M., Rief W., Mehl S. The lonely road to paranoia. A path-analytic investigation of loneliness and paranoia. Compr. Psychiatry. 2017;74:35–43. doi: 10.1016/j.comppsych.2016.12.007. [DOI] [PubMed] [Google Scholar]
- Lamster F., Nittel C., Rief W., Mehl S., Lincoln T. The impact of loneliness on paranoia: an experimental approach. J. Behav. Ther. Exp. Psychiatry. 2017;54:51–57. doi: 10.1016/j.jbtep.2016.06.005. [DOI] [PubMed] [Google Scholar]
- Lara E., Caballero F.F., Rico-Uribe L.A., Olaya B., Haro J.M., Ayuso-Mateos J.L., Miret M. Are loneliness and social isolation associated with cognitive decline? Int. J. Geriatr. Psychiatry. 2019;34(11):1613–1622. doi: 10.1002/gps.5174. [DOI] [PubMed] [Google Scholar]
- Le T.P., Cowan T., Schwartz E.K., Elvevåg B., Holmlund T.B., Foltz P.W., Barkus E., Cohen A.S. The importance of loneliness in psychotic-like symptoms: data from three studies. Psychiatry Res. 2019;282 doi: 10.1016/j.psychres.2019.112625. [DOI] [PubMed] [Google Scholar]
- Lenzenweger M.F. Schizotypy, schizotypic psychopathology, and schizophrenia: hearing echoes, leveraging prior advances, and probing new angles. Schizophr. Bull. 2018;44(suppl_2):S564–s569. doi: 10.1093/schbul/sby083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Yang Z., Qiu H., Wang Y., Jian L., Ji J., Li K. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatry. 2020;19(2):249–250. doi: 10.1002/wps.20758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim M., Rodebaugh T., Zyphur M., Gleeson J. Loneliness over time: the crucial role of social anxiety. J. Abnorm. Psychol. 2016;125 doi: 10.1037/abn0000162. [DOI] [PubMed] [Google Scholar]
- Lim M.H., Gleeson J.F.M., Alvarez-Jimenez M., Penn D.L. Loneliness in psychosis: a systematic review. Soc. Psychiatry Psychiatr. Epidemiol. 2018;53(3):221–238. doi: 10.1007/s00127-018-1482-5. [DOI] [PubMed] [Google Scholar]
- Loades M.E., Chatburn E., Higson-Sweeney N., Reynolds S., Shafran R., Brigden A., Linney C., McManus M.N., Borwick C., Crawley E. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry. 2020;59(11):1218–1239.e1213. doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locke B.D., Buzolitz J.S., Lei P.-W., Boswell J.F., McAleavey A.A., Sevig T.D., Dowis J.D., Hayes J.A. Development of the counseling center assessment of psychological symptoms-62 (CCAPS-62) J. Couns. Psychol. 2011;58(1):97. doi: 10.1037/a0021282. [DOI] [PubMed] [Google Scholar]
- Matthews T., Danese A., Wertz J., Odgers C.L., Ambler A., Moffitt T.E., Arseneault L. Social isolation, loneliness and depression in young adulthood: a behavioural genetic analysis. Soc. Psychiatry Psychiatr. Epidemiol. 2016;51(3):339–348. doi: 10.1007/s00127-016-1178-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meehl P.E. Schizotaxia, schizotypy, schizophrenia. Am. Psychol. 1962;17(12):827–838. [Google Scholar]
- Michalska da Rocha B., Rhodes S., Vasilopoulou E., Hutton P. Loneliness in psychosis: a meta-analytical review. Schizophr. Bull. 2018;44(1):114–125. doi: 10.1093/schbul/sbx036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minor K.S., Cohen A.S. Affective reactivity of speech disturbances in schizotypy. J. Psychiatr. Res. 2010;44(2):99–105. doi: 10.1016/j.jpsychires.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Mohr C., Claridge G. Schizotypy—do not worry, it is not all worrisome. Schizophr. Bull. 2015;41(suppl_2):S436–S443. doi: 10.1093/schbul/sbu185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson M.T., Seal M.L., Pantelis C., Phillips L.J. Evidence of a dimensional relationship between schizotypy and schizophrenia: a systematic review. Neurosci. Biobehav. Rev. 2013;37(3):317–327. doi: 10.1016/j.neubiorev.2013.01.004. [DOI] [PubMed] [Google Scholar]
- Palgi Y., Shrira A., Ring L., Bodner E., Avidor S., Bergman Y., Cohen-Fridel S., Keisari S., Hoffman Y. The loneliness pandemic: loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affect. Disord. 2020;275:109–111. doi: 10.1016/j.jad.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulhus D.L., Robins R.W., Trzesniewski K.H., Tracy J.L. Two replicable suppressor situations in personality research. Multivariate Behav. Res. 2004;39(2):303–328. doi: 10.1207/s15327906mbr3902_7. [DOI] [PubMed] [Google Scholar]
- Polner B., Simor P., Kéri S. Insomnia and intellect mask the positive link between schizotypal traits and creativity. PeerJ. 2018;6 doi: 10.7717/peerj.5615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qualter P., Brown S.L., Munn P., Rotenberg K.J. Childhood loneliness as a predictor of adolescent depressive symptoms: an 8-year longitudinal study. Eur. Child Adolesc. Psychiatry. 2010;19(6):493–501. doi: 10.1007/s00787-009-0059-y. [DOI] [PubMed] [Google Scholar]
- Rabinowitz J., Levine S.Z., Garibaldi G., Bugarski-Kirola D., Berardo C.G., Kapur S. Negative symptoms have greater impact on functioning than positive symptoms in schizophrenia: analysis of CATIE data. Schizophr. Res. 2012;137(1–3):147–150. doi: 10.1016/j.schres.2012.01.015. [DOI] [PubMed] [Google Scholar]
- Riggio H.R., Kwong W.Y. Social skills, paranoid thinking, and social outcomes among young adults. Personal. Individ. Differ. 2009;47(5):492–497. [Google Scholar]
- Robertson B.R., Prestia D., Twamley E.W., Patterson T.L., Bowie C.R., Harvey P.D. Social competence versus negative symptoms as predictors of real world social functioning in schizophrenia. Schizophr. Res. 2014;160(1–3):136–141. doi: 10.1016/j.schres.2014.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rock P.L., Roiser J.P., Riedel W.J., Blackwell A.D. Cognitive impairment in depression: a systematic review and meta-analysis. Psychol. Med. 2014;44(10):2029–2040. doi: 10.1017/S0033291713002535. [DOI] [PubMed] [Google Scholar]
- Russell D.W. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J. Pers. Assess. 1996;66(1):20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Santomauro D.F., Mantilla Herrera A.M., Shadid J., Zheng P., Ashbaugh C., Pigott D.M., Abbafati C., Adolph C., Amlag J.O., Aravkin A.Y., Bang-Jensen B.L., Bertolacci G.J., Bloom S.S., Castellano R., Castro E., Chakrabarti S., Chattopadhyay J., Cogen R.M., Collins J.K., Dai X., Dangel W.J., Dapper C., Deen A., Erickson M., Ewald S.B., Flaxman A.D., Frostad J.J., Fullman N., Giles J.R., Giref A.Z., Guo G., He J., Helak M., Hulland E.N., Idrisov B., Lindstrom A., Linebarger E., Lotufo P.A., Lozano R., Magistro B., Malta D.C., Månsson J.C., Marinho F., Mokdad A.H., Monasta L., Naik P., Nomura S., O’Halloran J.K., Ostroff S.M., Pasovic M., Penberthy L., Reiner R.C., Jr., Reinke G., Jr., Ribeiro A.L.P., Jr., Sholokhov A., Jr., Sorensen R.J.D., Jr., Varavikova E., Jr., Vo A.T., Jr., Walcott R., Jr., Watson S., Jr., Wiysonge C.S., Jr., Zigler B., Jr., Hay S.I., Jr., Vos T., Jr., Murray C.J.L., Jr., Whiteford H.A., Jr., Ferrari A.J., Jr. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage M.J., James R., Magistro D., Donaldson J., Healy L.C., Nevill M., Hennis P.J. Mental health and movement behaviour during the COVID-19 pandemic in UK university students: prospective cohort study. Ment. Health Phys. Act. 2020;19 [Google Scholar]
- Schlosser D.A., Campellone T.R., Biagianti B., Delucchi K.L., Gard D.E., Fulford D., Stuart B.K., Fisher M., Loewy R.L., Vinogradov S. Modeling the role of negative symptoms in determining social functioning in individuals at clinical high risk of psychosis. Schizophr. Res. 2015;169(1):204–208. doi: 10.1016/j.schres.2015.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schofield K., Claridge G. Paranormal experiences and mental health: schizotypy as an underlying factor. Personal. Individ. Differ. 2007;43(7):1908–1916. [Google Scholar]
- Silvia P.J., Kwapil T.R. Aberrant asociality: how individual differences in social anhedonia illuminate the need to belong. J. Pers. 2011;79(6):1315–1332. doi: 10.1111/j.1467-6494.2010.00702.x. [DOI] [PubMed] [Google Scholar]
- Sin E., Shao R., Lee T.M.C. The executive control correlate of loneliness in healthy older people. Aging Ment. Health. 2021;25(7):1224–1231. doi: 10.1080/13607863.2020.1749832. [DOI] [PubMed] [Google Scholar]
- Stain H.J., Galletly C.A., Clark S., Wilson J., Killen E.A., Anthes L., Campbell L.E., Hanlon M.C., Harvey C. Understanding the social costs of psychosis: the experience of adults affected by psychosis identified within the second australian National Survey of psychosis. Aust. N. Z. J. Psychiatry. 2012;46(9):879–889. doi: 10.1177/0004867412449060. [DOI] [PubMed] [Google Scholar]
- Strauss G.P., Sandt A.R., Catalano L.T., Allen D.N. Negative symptoms and depression predict lower psychological well-being in individuals with schizophrenia. Compr. Psychiatry. 2012;53(8):1137–1144. doi: 10.1016/j.comppsych.2012.05.009. [DOI] [PubMed] [Google Scholar]
- Sündermann O., Onwumere J., Kane F., Morgan C., Kuipers E. Social networks and support in first-episode psychosis: exploring the role of loneliness and anxiety. Soc. Psychiatry Psychiatr. Epidemiol. 2014;49(3):359–366. doi: 10.1007/s00127-013-0754-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilvis R.S., Kähönen-Väre M.H., Jolkkonen J., Valvanne J., Pitkala K.H., Strandberg T.E. Predictors of cognitive decline and mortality of aged people over a 10-year period. J. Gerontol. A Biol. Sci. Med. Sci. 2004;59(3):268–274. doi: 10.1093/gerona/59.3.m268. [DOI] [PubMed] [Google Scholar]
- Weinberg D., Shahar G., Davidson L., McGlashan T.H., Fennig S. Longitudinal associations between negative symptoms and social functioning in schizophrenia: the moderating role of employment status and setting. Psychiatry Interpers.Biol. Process. 2009;72(4):370–381. doi: 10.1521/psyc.2009.72.4.370. [DOI] [PubMed] [Google Scholar]
- Williams L.M., Irwin H.J. A study of paranormal belief, magical ideation as an index of schizotypy and cognitive style. Personal. Individ. Differ. 1991;12(12):1339–1348. [Google Scholar]
- Zhou Z., Mao F., Zhang W., Towne S.D., Jr., Wang P., Fang Y. The association between loneliness and cognitive impairment among older men and women in China: a nationwide longitudinal study. Int. J. Environ. Res. Public Health. 2019;16(16):2877. doi: 10.3390/ijerph16162877. [DOI] [PMC free article] [PubMed] [Google Scholar]