To the Editor.
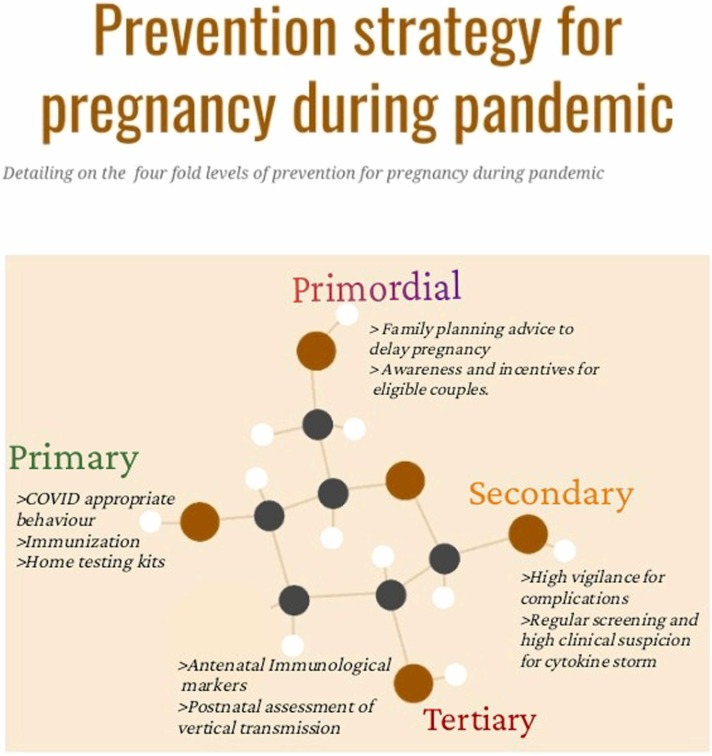
Pregnancy is an immunocompromised state and infections during pregnancy is likely to alter the immunological functioning. Long-term neurobiological changes in the fetus are associated with maternal infections during pregnancy. Velloso et al., have highlighted the role of alteration in the immunological state (persistently increased level of Interleukin-6 in pregnant females with COVID 19 which can potentially impact neuro-gliogenesis in fetus which in turn may result in deficit in sociability in the newborn (Velloso et al., 2021)). It is well known that COVID-19 infection causes alteration in the level of cytokines, particularly interleukin-6, which become more intense during phases of cytokine storm. COVID-19 being an emerging and evolving disease, studies on the long-term fetal outcomes will take time to have final grounds; thus, we want to discuss a four-fold level of prevention which can be utilized to prevent the risks and the severity of the impact of potential fetal outcomes.
The primordial level of prevention involves creating awareness to prevent a certain risk factor from developing in an entire population through a change in social and environmental conditions. The magnitude and peak of COVID 19 infection is unpredictable but pregnancy as a risk factor could be planned. Therefore, increasing awareness on family planning and providing contraceptive advice to delay planning for pregnancy during the pandemic needs to be implemented. It's critical to emphasise here that it's a couple's decision when to try to conceive, but that the risks and benefits of going ahead vs. waiting should be carefully weighed, that a variety of options should be provided, and that discussions with healthcare providers should be conducted in a non-judgmental manner. Telehealth services can provide a crucial role in providing family planning, prenatal and antenatal counselling to eligible couples.(Aziz et al., 2020) Government policies highlighting the need for planned and delayed pregnancy during the pandemic or incentivization of Healthcare workers and couples adopting contraceptive measures could prove beneficial.
Primary level of prevention includes specific measures taken for a targeted healthy population. The physiological changes during pregnancy can alter due to COVID 19 infection. Thus, steps like avoiding contact with infected/suspected patients, frequent hand washing, wearing masks, social distancing, avoiding crowds, public gatherings and excessive outdoor activities becomes imperative during pregnancy. Immunization is also being advocated and though ethically prohibited for testing in pregnancy, none of the available evidence points to an adverse outcome following vaccination in pregnancy. Regular nasal and oropharyngeal swab tests even in asymptomatic females are necessary to prevent chances of development of COVID 19 Infection. Home testing kits use, rapid test for COVID-19 and high clinical suspicion needs to be maintained.
Secondary prevention necessitates early identification of COVID-19. A recent meta-analysis of 24 studies and 136 females concluded that pre-term birth rate in COVID 19 positive females was 37.7% (thrice than that of general US patients at 12%) and caesarean section delivery rate was 76% ( more than double the general US population average) (Matar et al., 2021). Similarly, a high rate of institutional stillbirth and neonatal mortality was reported in a large prospective study by Kc et al. (2020). Pregnant females who already detected with COVID-19 should thus remain at high vigilance for advancement of disease (to prevent cytokine storm).
Tertiary level prevention targets both clinical and outcome stages for preventing severity of disease and its associated sequelae. A systematic review assessing obstetric outcomes pointed out that 34.62% of the pregnant patients had obstetric complications and vertical transmission rate evaluated through SARS-CoV-2 nucleic acid tests was 3.91% (Chi et al., 2021). Routine testing of immunological markers, including CRP, TNF alpha, IL 6 and IL 1 levels are necessary post stratification of admitted patients. Pro-inflammatory milieu can even lead to an increased chances of possible obstetric complications and long and short-term Fetal outcomes. To prevent neurodevelopmental brain disorders, close monitoring of IL-6 during early postnatal period is necessary (Cavalcante et al., 2021). Neonatal oropharyngeal swab testing and nucleic acid tests of placental blood and secretions should be included for assessing vertical transmission. Rapid testing may be useful in giving the infection status early. Similarly, children born from COVID-19 positive mothers should be periodically screened for neurodevelopmental disorders and schizophrenia in due course of time. The mothers should also be given options of family planning at the time of delivery, if they have completed their family.
The suggested four-fold level of prevention is summarized in the form of Fig. 1 highlighting the necessary steps to be implemented in every step.
Fig. 1.
Prevention strategies during pandemic pregnancy.
Ethical approval
Not applicable.
Funding
None.
CRediT authorship contribution statement
The idea conception and planning were done by Sujita Kumar Kar. The original write and revisions were made by Surobhi Chatterjee. The write-up was further analyzed, evaluated and revised by Sujita Kumar Kar.
Disclosure of interest
The authors declare no conflict of interest.
Acknowledgements
Nil.
Conflict of interest
Nil.
Financial disclosure
Nil.
References
- Aziz A., Zork N., Aubey J.J., Baptiste C.D., D’Alton M.E., Emeruwa U.N., Fuchs K.M., Goffman D., Gyamfi-Bannerman C., Haythe J.H., LaSala A.P., Madden N., Miller E.C., Miller R.S., Monk C., Moroz L., Ona S., Ring L.E., Sheen J.-J., Spiegel E.S., Simpson L.L., Yates H.S., Friedman A.M. Telehealth for high-risk pregnancies in the setting of the COVID-19 pandemic. Am. J. Perinatol. 2020;37:800–808. doi: 10.1055/s-0040-1712121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavalcante M.B., Cavalcante C.T., de M.B., Sarno M., Barini R., Kwak-Kim J. Maternal immune responses and obstetrical outcomes of pregnant women with COVID-19 and possible health risks of offspring. J. Reprod. Immunol. 2021;143 doi: 10.1016/j.jri.2020.103250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi J., Gong W., Gao Q. Clinical characteristics and outcomes of pregnant women with COVID-19 and the risk of vertical transmission: a systematic review. Arch. Gynecol. Obstet. 2021;303:337–345. doi: 10.1007/s00404-020-05889-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kc A., Gurung R., Kinney M.V., Sunny A.K., Moinuddin M., Basnet O., Paudel P., Bhattarai P., Subedi K., Shrestha M.P., Lawn J.E., Målqvist M. Effect of the COVID-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: a prospective observational study. Lancet Glob. Health. 2020;8:e1273–e1281. doi: 10.1016/S2214-109X(20)30345-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matar R., Alrahmani L., Monzer N., Debiane L.G., Berbari E., Fares J., Fitzpatrick F., Murad M.H. Clinical Presentation and Outcomes of Pregnant Women With Coronavirus Disease 2019: a systematic review and meta-analysis. Clin. Infect. Dis. . Publ. Infect. Dis. Soc. Am. 2021;72:521–533. doi: 10.1093/cid/ciaa828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velloso F.J., Wadhwa A., Kumari E., Carcea I., Gunal O., Levison S.W. Modestly increasing systemic interleukin-6 perinatally disturbs secondary germinal zone neurogenesis and gliogenesis and produces sociability deficits. Brain Behav. Immun. 2021;101:23–36. doi: 10.1016/j.bbi.2021.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]