Abstract
Objective
A lot of research has focused on the field of chemotherapy-induced peripheral neuropathy (CIPN). In this study, we performed a bibliometric analysis of CIPN-related publications to identify the key research areas and trends over the last 20 years.
Methods
We searched the Web of Science core collection for publications related to CIPN that were published between January 2001 and September 2021. We then performed bibliometric analysis and visualization using Microsoft Excel 2019, VOSviewer, and the Bibliometric online analysis platform (https://bibliometric.com/).
Results
In total, we identified 2,188 eligible publications in the field of CIPN, with an increasing trend in the annual number of publications. The United States and Italy were dominant in the CIPN field. Supportive Care in Cancer was the most productive journal. G. Cavaletti and A.A. Argyriou published the largest number of papers. Of all institutions, the University of Milano-Bicocca, Italy, published the highest number of papers. Analysis of the co-occurrence of keywords revealed the specific characteristics relating to the four main clusters: oxaliplatin, paclitaxel, pain management, and quality of life (QOL). Newly emerging research focusses predominantly on neuroinflammatory mechanisms and non-pharmacological interventions for CIPN.
Conclusion
This bibliometric study reviewed the evolutionary trends in CIPN research and identified current research hotspots and research trends. In addition, we identified journals, institutions, and authors, with the highest levels of impact to enhance the collaboration and learning.
Keywords: chemotherapy-induced peripheral neuropathy, bibliometric analysis, research hotspots, publications, VOSviewer
Introduction
Chemotherapy-induced peripheral neuropathy (CIPN) has become a rising health concern due to the increasing number of cancer survivors and prolonged survival rates. CIPN is a prevalent clinical problem in over 50% of patients treated with neurotoxic medications and undoubtedly increases the burden on patients and healthcare coverage (1, 2). Approximately 30% of patients still report varying degrees of CIPN 6 months after chemotherapy; this condition has a notable effect on the lives in cancer survivors (3, 4). A previous study on the ovarian cancer showed that the symptoms of CIPN did not diminish until 3 years after the end of treatment (5). At present, the mechanistic studies predominantly focus on the dorsal root ganglion injury, microtubule injury, mitochondrial dysfunction, oxidative stress, neuroinflammation, and the dysfunction of membrane channels (6, 7). There is no effective strategy for preventing CIPN and no recognized therapeutic agent at the present time. Only duloxetine is recommended for the chemotherapy-induced neuropathic pain (8, 9). Over the past two decades, thousands of published manuscripts have reported mechanistic, diagnostic, therapeutic, and preventive studies of CIPN, making it very difficult for researchers to identify highly influential articles and research hotpots. Manual literature searches can no longer accurately identify potential trends in the development of CIPN. Therefore, there is an urgent need to develop new literature retrieval strategies for the fast data collation and mining.
Bibliometric analysis is a statistical method used for the analysis and visualization of key characteristics from published articles and the identification of research trends in a specific field using online literature databases (10, 11). Bibliometric analysis provides us with tools to analyze the publications qualitatively and quantitatively and identify significant research hotspots and trends. In addition, bibliometric analysis can accurately identify the most influential researchers, manuscripts, journals, and institutions (12). Bibliometrics has been applied widely in a variety of medical fields, such as complementary and alternative medicine (13), oncology (14), infectious diseases (15), nursing (16), and encephalopathy (17). Although there is a significant body of literature available for CIPN, these publications have not been summarized and analyzed. Therefore, in the present study, we conducted a comprehensive bibliometric analysis of publications related to CIPN from 2001 to 2021. Our goal was to gain enhanced understanding of existing research hotspots and potential trends and provide useful reference guidelines for future researchers.
Materials and Methods
Data Selection
We screened the Web of Science Core Collection (WoSCC, Clarivate Analytics) between January 2001 and September 2021 to identify publications related to CIPN. The details of search terms are shown in Supplementary Table 1. There was no limit to the word term “peripheral”; this strategy aimed to avoid omissions as much as possible. Only papers published in English were considered. The title and abstract were reviewed and screened by two independent reviewers; a third reviewer decided on any disagreements. Figure 1 shows the flow chart of study identification and selection.
Figure 1.
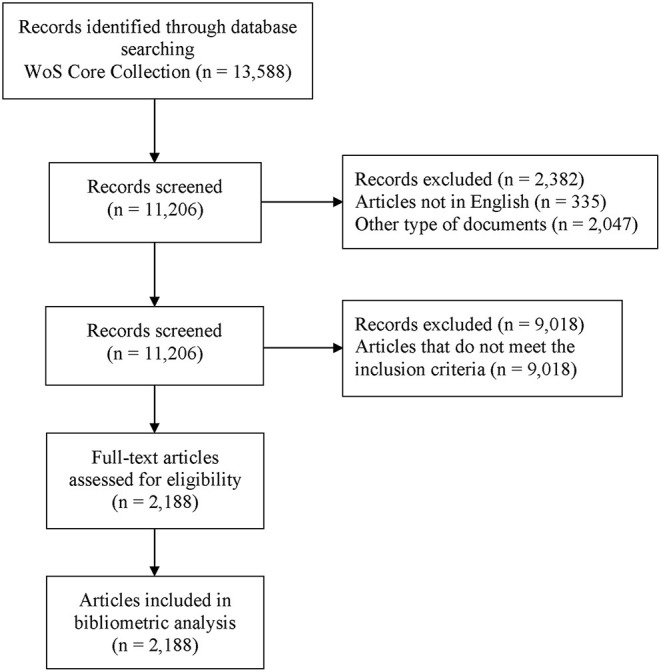
Flowchart of study identification and selection.
Data Analysis and Visualization
A range of key information was extracted from the articles that met the required criteria, such as title, author, research institution, country or region, keywords, year of publication, source, number of citations, 2020 impact factor (IF), and Hirsch index (H-index). All records were downloaded from the WoSCC for further analysis. Microsoft Excel 2019, VOSviewer (Version 1.6.15, Leiden University, The Netherlands), the Bibliometric online analysis platform (https://bibliometric.com/), and the biblioshiny package from R language (18) were used for data processing and visualization of the above variables. The H-index was defined as the number of papers published and cited ≥ h; thus, helped to identify the high-quality output from given researchers (19). VOSviewer is a scientific software package for the bibliometric analysis and visualization (20).
Results
Publication Characteristics
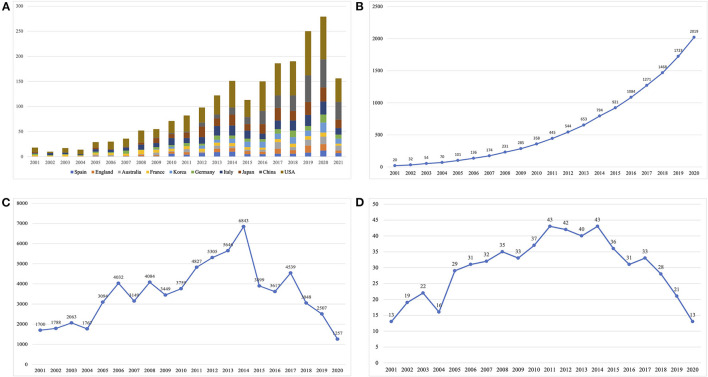
Literature searches identified a total of 13,588 publications from the WoSCC. Based on the titles and abstracts of all articles screened by the reviewers, 2,188 studies met the inclusion criteria and were included for further data extraction that included 1,899 articles (86.7%) and 289 reviews (14.3%). Figure 1 summarizes the research characteristics of these publications. A growing trend in publication number was observed, indicating the increasing attention and interest in the CIPN field (Figures 2A,B). In addition, we constructed publication trends for the CIPN field using Microsoft Excel 2019 (y = 0.0373x3 – 0.3597x2 + 6.2327x + 4.782, R2 = 0.9876); these analyses indicated that there will be more than 500 publications related to CIPN by 2025. Additionally, we found that the number of citations increased rapidly after 2005 and reached the highest level in 2014 (Figure 2C). Overall, 170 studies were cited more than 100 times. The average H-index in this field was 30, peaking in 2011 and 2014 (Figure 2D). Collectively, these data showed that significant progress had been achieved in the CIPN field over the last decade, particularly between 2011 and 2014.
Figure 2.
The number of publications, the number of citations, and the Hirsch index (H-index) for chemotherapy-induced peripheral neuropathy (CIPN): (A) the annual number of publications in major countries; (B) the annual cumulative number of publications; (C) the annual citation number of publications, and (D) the annual H-index of publications.
The Distribution of Publications by Country
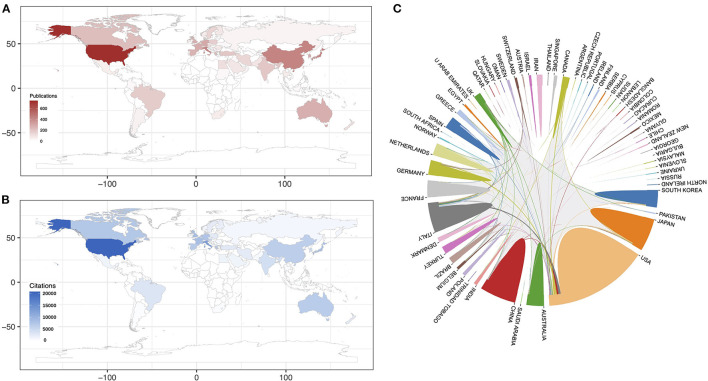
A total of 69 countries and regions were involved in the publication of the 2,188 articles and reviews. The United States contributed the most significant number of publications (740), followed by Italy (247), Japan (246), China (243), and Germany (116) (Figure 3A). The United States (29, 866), Italy (11,371), and Japan (4,961), were associated with the highest number of citations, thus showing the comparative breadth of these countries in this field (Figure 3B). Despite the small number of publications, France, and the Netherlands had more citations on average than the most countries, indicating the high quality of the studies carried out in these countries. Close research cooperation between countries is known to drive technological and research advances. Figure 3C shows the cooperation between countries in the CIPN field. We found closer cooperation among the United States, Italy, Germany, and other countries, while China and Japan were associated with lower levels of international cooperation.
Figure 3.
Countries associated with the CIPN field between 2001 and 2021: (A) the number of publications arising from various countries; (B) the total number of citations from various countries, and (C) international collaboration between countries.
The Distribution of Publications by Institution
Table 1 shows the top 10 institutions in terms of publication number, total citations, and the average number of citations. The University of Milano-Bicocca, the University of Michigan, the Mayo Clinic, and the MD Anderson Cancer Center had the most vital partnerships with other institutions.
Table 1.
The top 10 institution in terms of publications in the chemotherapy-induced peripheral neuropathy (CIPN) field.
| Institution | Country | Publications | Total citations | Average citation |
|---|---|---|---|---|
| University of Milano-Bicocca | Italy | 117 | 5,976 | 51.08 |
| Mayo Clinic | USA | 82 | 5,075 | 61.89 |
| MD Anderson Cancer Center | USA | 82 | 3,273 | 39.91 |
| University of Michigan | USA | 65 | 2,596 | 39.94 |
| University of Sydney | USA | 45 | 965 | 21.44 |
| Johns Hopkins University | USA | 43 | 1,306 | 30.37 |
| University of California, San Francisco |
USA | 43 | 1,361 | 31.65 |
| University of Florence | USA | 39 | 1,457 | 37.36 |
| Dana-Farber Cancer Institute | USA | 36 | 1,940 | 53.89 |
| Kyung Hee University | Korea | 34 | 417 | 12.26 |
Author Distribution
We identified the 15 most influential authors in the CIPN field based on the H-index and the number of publications (Table 2). Scholars from Italy (5/15) made an enormous contribution to the CIPN field. G. Cavaletti had the highest H-index, number of publications, and total citations. Notably, although two Greek researchers were described as the most influential in terms of publications, Greek institutions are not included in Table 1, which we believe is mainly because the same author marked different institutions in different papers. In addition, we analyzed the collaborative relationships between highly productive authors in this field (Supplementary Figure 1). Based on a partnership map, we identified several key research teams, such as those of G. Cavaletti, S. B. Park, P. M. Dougherty, and C. I. Loprinzi; all these authors had close collaborative relationships with each other.
Table 2.
The top 15 most influential authors.
| Author | Country | Articles (n) | Total citations | Average citations | H-index |
|---|---|---|---|---|---|
| Cavaletti G | Italy | 113 | 3,511 | 31.07 | 44 |
| Argyriou AA | Greece | 48 | 1,566 | 32.63 | 26 |
| Park SB | England | 46 | 887 | 19.28 | 17 |
| Alberti P | Italy | 42 | 941 | 22.40 | 20 |
| Bruna J | Spain | 41 | 973 | 23.73 | 22 |
| Loprinzi CI | USA | 39 | 1,423 | 36.49 | 25 |
| Goldstein D | Australia | 38 | 918 | 24.16 | 16 |
| Smith EML | USA | 38 | 1,088 | 28.63 | 15 |
| Kalofonos HP | Greece | 37 | 1,304 | 35.24 | 25 |
| Dougherty PM | USA | 36 | 1,249 | 34.69 | 27 |
| Ghelardini C | Italy | 35 | 405 | 11.57 | 18 |
| Marmiroli P | Italy | 31 | 973 | 31.39 | 19 |
| Mannelli LD | Italy | 30 | 358 | 11.93 | 17 |
| Egashira N | Japan | 29 | 433 | 14.93 | 15 |
| Velasco R | Spain | 29 | 656 | 22.62 | 17 |
Journal Distribution
Analysis showed that a total of 544 journals were involved in CIPN research during our study period. Table 3 shows the top 15 most productive journals in the CIPN field. Over the past 20 years, Supportive Care in Cancer had the highest number of publications; this was followed by Pain and Molecular Pain. PAIN, Supportive Care in Cancer, and the Journal of Clinical Oncology, were the top three journals with the most citations. Notably, the Journal of Clinical Oncology had the highest average number of citations; this indicated the higher quality of manuscripts published in this journal.
Table 3.
The top 15 most productive journals between 2001 and 2021.
| Journal | No. of texts | Citations | Average citations | H-index | IF (2020) | 5-year IF |
|---|---|---|---|---|---|---|
| Supportive Care in Cancer | 107 | 3,029 | 28.31 | 31 | 3.603 | 3.958 |
| PAIN | 56 | 4,099 | 73.20 | 32 | 6.961 | 7.704 |
| Molecular Pain | 40 | 1,613 | 40.33 | 22 | 3.395 | 3.615 |
| Experimental Neurology | 39 | 2,060 | 52.82 | 21 | 5.33 | 5.34 |
| Journal of the Peripheral Nervous System | 38 | 1,378 | 36.26 | 19 | 3.494 | 3.455 |
| PLoS One | 35 | 1,160 | 33.14 | 17 | 3.24 | 3.788 |
| Cancer Chemotherapy and Pharmacology | 34 | 785 | 23.09 | 16 | 3.333 | 3.402 |
| Clinical Cancer Research | 30 | 1,778 | 59.27 | 23 | 12.531 | 12.836 |
| Scientific Reports | 30 | 387 | 12.90 | 12 | 4.379 | 5.133 |
| International Journal of Molecular Sciences | 27 | 234 | 8.67 | 7 | 5.923 | 6.132 |
| Neuroscience Letters | 26 | 839 | 32.27 | 13 | 3.036 | 2.855 |
| European Journal of Cancer | 25 | 2,070 | 82.80 | 20 | 9.162 | 9.305 |
| Journal of Pain | 24 | 1,391 | 57.96 | 15 | 5.820 | 7.061 |
| Journal of Pharmacological Sciences | 24 | 336 | 14.00 | 11 | 3.337 | 3.432 |
| Neuropharmacology | 24 | 671 | 27.96 | 16 | 5.25 | 5.283 |
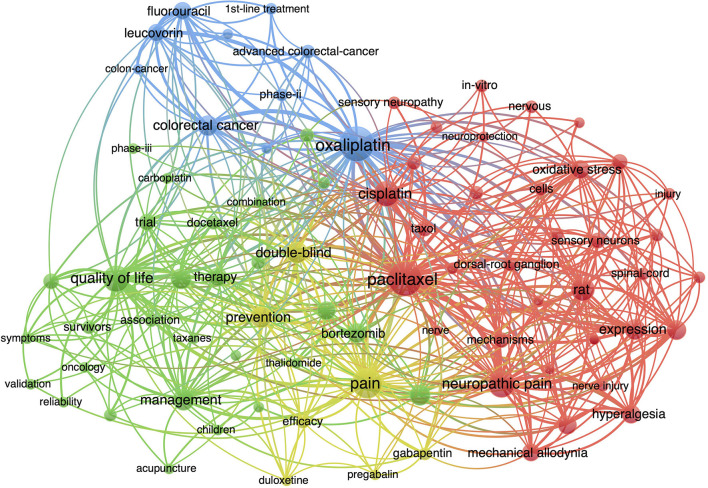
Analysis of Hotspots and Trends in Research
The distribution of co-occurring keywords and keywords plus were analyzed using VOSviewer to identify key trends and directions in the CIPN field. Descriptive keywords such as “peripheral neuropathy,” “neurotoxicity,” “cancer,” and “chemotherapy” were excluded. Keywords with frequencies >40 were analyzed; this analysis identified 80 keywords with the highest relevance (Figure 4). These keywords were divided into four clusters: (i) oxaliplatin, (ii) paclitaxel, (iii) pain management, (iv) and quality of life (QOL).
Figure 4.
Visualization of keywords related to CIPN research between 2000 and 2021.
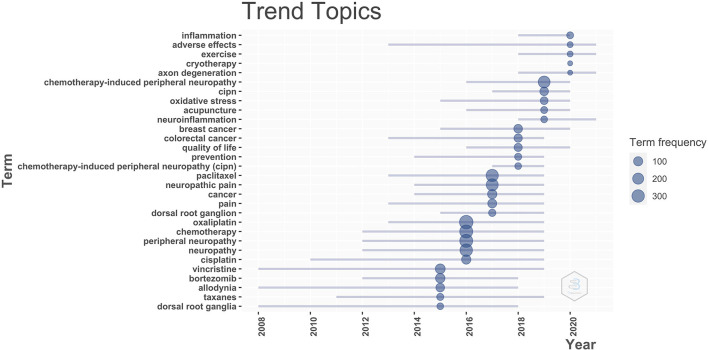
Next, we identified research trends in the field of CIPN so that these could be used as a reference for future researchers. We analyzed and visualized the temporal trends of keyword occurrences (Figure 5). Emerging trends in research on CIPN over the most recent 5 years included studies of neuroinflammatory mechanisms and non-pharmacological treatments, such as exercise, cryotherapy, and acupuncture. These topics offer potential research directions for the future.
Figure 5.
Timeline of research trends in the field of CIPN.
Discussion
In this study, we conducted a bibliometric analysis of publications related to CIPN over the past two decades so that we could identify key hotspots and trends in CIPN research. We found that the number of publications related to CIPN research have increased rapidly since 2001. We observed a gradual increase in the number of publications related to CIPN research, especially after 2010, thus showing that this field will remain a hot topic of interest for researchers over the coming years. Our analysis showed that the United States plays an essential role in CIPN research, followed by Italy, Japan, and China; about 56.4% of all publications were published by researchers in the United States. In addition, the United States dominated our results in terms of publication output, total citations, and international collaborations. The high ranking of France and the Netherlands in terms of total citations indicates the high quality of the research activity in these countries. With regards to international cooperation, the United States, Italy, and Germany, were found to collaborate closely with other countries, while China and Japan collaborate to a lesser extent; this may be the reason for their low ranking in the number of citations. International collaboration should be strengthened in China and Japan so that higher quality publications can be disseminated.
When considering the top 10 institutions with the highest impact, we found that 70% were in the United States. The University of Milan-Bicocca from Italy contributed the highest number of publications and total citations, indicating that this institution publishes higher quality articles and could be considered for further collaboration and learning. In terms of authors, G. Cavaletti, A. A. Argyriou, S. S. Park, P. Alberti, and J. Bruna had the highest number of individual publications and all made significant contributions to the progression of CIPN research. In addition, studies by P. M. Dougherty, C. I. Loprinzi, and A. A. Argyriou had the highest average number of citations, thus indicating that these authors publish high quality research in the field of CIPN. Moreover, it is evident from the network that these teams maintain close collaboration with each other; this is why they can produce high quality publications. Our analysis showed that a number of journals are publishing CIPN-related research; the journals that have published the most articles on CIPN were Supportive Care in Cancer, Pain, Molecular Pain, and Experimental Neurology.
Current Research Hotpots
Based on the keywords co-occurrence analysis, we were able to classify CIPN research into two key hotspots, as described below.
(I). Oxaliplatin- and Paclitaxel-Induced Peripheral Neuropathy
Neurotoxicity is commonly associated with the application of oxaliplatin and paclitaxel and therefore has gained high levels of clinical attention. Oxaliplatin-induced peripheral neuropathy (OIPN) can be classified as either acute or chronic, with a 50–90% incidence of acute neurotoxicity and a 60–80% incidence of chronic neurotoxicity (21–23). Acute OIPN usually presents with distal sensory abnormalities and dullness induced by the cold stimuli or abnormal pharyngeal sensation (24, 25). Chronic OIPN may manifest as numbness at the ends of the extremities, pain, or sensory ataxia (26). The clinical manifestations of paclitaxel-induced peripheral neurotoxicity (PIPN) are similar to those of OIPN, while 30% of patients with PIPN experience neuropathic pain (27). Large interpersonal variability exists in the intensity of the symptoms experienced by patients with OIPN and PIPN; this variability is closely related to the cumulative dose of chemotherapy, the schedule, and combination therapy (26, 28). Pre-existing risk factors, such as diabetes, hemoglobin, age, body mass index, high alcohol consumption, and genetic predisposition, are all known to increase the incidence of such diseases (29–32). In addition, the severity of CIPN has been shown to be proportional to the number of comorbidities at baseline (33). Despite recent progress, our ability to provide effective prevention and treatment strategies for CIPN remain limited. Therefore, a key direction for the future is to develop high-quality clinical research to identify effective drugs that can prevent and treat CIPN.
(II). Pain Management and QOL Issues in Patients with CIPN
Due to a lack of effective control measures, over 80% of cancer survivors experience neuropathic pain during chemotherapy. Only duloxetine is moderately recommended to relieve the chemotherapy-induced peripheral neuropathic pain (CIPNP) (8). Different types of chemotherapeutic agents can cause CIPNP and do so via a range of different mechanisms, such as mitochondrial damage, increased ion channel activity, neuronal injury, and inflammation, and oxidative stress (34, 35). Although chemotherapeutic agents exhibit different pathophysiology profiles, they also have overlapping contributions to the pathogenesis of neuropathic pain and may be targets for the prevention or treatment. Pain management in post-chemotherapy patients is an issue that has yet to be resolved. However, current treatment strategies have been associated with poor levels of clinical efficacy. Subsequent studies should be based on mechanisms rather than symptoms to obtain more evidence for treatment. Notably, the application of analgesic drugs must not compromise antitumor efficacy and increase the incidence of other adverse effects. Therefore, monotherapy is still recommended for the management of CIPNP (35). In addition, CIPN increases the burden on patients and has a significant and long-term impact on patient QOL (36–38). Patients with severe CIPN are more likely to experience fatigue, depression, and anxiety (5, 39). Therefore, QOL in cancer survivors cannot be ignored during the treatment and care, making this a significant topic for long-term research.
Future Frontiers
Based on our review of the timeline of research topics for CIPN prior to 2021, we forecast that two research topics will play significant roles in the future, as follows.
(I). Study of Neuroinflammatory Mechanisms
Peripheral neuropathies are characterized by the axonal degeneration and nerve damage. Neuroinflammation has been proven to be associated with a variety of neuropathic pain models (e.g., diabetic neuropathy and traumatic nerve injury) (40, 41). Chemotherapeutic drugs can accumulate in nerve axons and dorsal root ganglia, which, in addition to activation of the immune system and immune-like glial cells (such as satellite glial cells and Schwann cells), may lead to neuroinflammation and thus to the development of CIPN (42, 43). In addition, the involvement of neuroinflammation in the pathological process of CIPN has been demonstrated in the central nervous system (44, 45). The features and mechanisms of the neuroinflammatory process differ and are dependent on the type of chemotherapeutic agents. In summary, a better understanding of the mechanisms of neuroinflammation may help us to develop useful future strategies to improve the management of CIPN. Notably, recent studies have found that ganglioside-monosialic acid (GM1), a neuroprotective agent, is effective in preventing the neurotoxicity during chemotherapy. A high-quality randomized controlled trial in colorectal cancer found that GM1 significantly reduced the incidence and severity of PIPN reported by subjects (46). Another study on breast cancer reported similar results (47). These studies may be a significant advance in neurotoxic intervention strategies for paclitaxel drugs.
(II). Non-pharmacological Interventions for CIPN
Although many drugs and preparations have been proven to exert neuroprotective effects in basic research, most of these drugs lack the support of clinical research data or have been proven to be invalid by phase III clinical studies, such as calcium and magnesium (48–50). Therefore, researchers have increasingly focused on non-pharmacological interventions, such as acupuncture, exercise, and herbal medicine. Acupuncture has shown a positive effect on CIPN, but heterogeneous design, and variability in outcome measures make it difficult to evaluate its impact (51). Notably, compared with invasive acupuncture treatment, transcutaneous electrical nerve stimulation (TENS), an inexpensive, non-invasive, and self-administered technique, is being intensively investigated as a possible adjunct to pharmacological treatment of CIPN (52, 53). Furthermore, a meta-analysis of exercise interventions reported potentially positive treatment effects (54). Combined exercise protocols (sensorimotor, endurance, and strength training) appear to greater levels of improvement in patients with CIPN (55). However, the quality of evidence and strength of recommendation put forward by these clinical reports were compromised by shortcomings in study design, sample size, and assessment methods. As a result, these promising therapies have not been recommended for the prevention and treatment of CIPN (49). Further investigation is now needed to increase the credibility and reliability of such research. Larger sample, multicenter randomized controlled studies need to be considered in future study protocols to confirm the efficacy and clarify risks.
This study has some limitations that need to be considered. First, due to software limitations, we were unable to conduct a cross-check with multiple high-quality databases, such as Pubmed and Embase; this may have led to an incomplete selection of literature. Second, the dynamic update of the databases caused a certain lag in our literature screening. Finally, due to the relatively large number of publications, some papers may have been omitted by manual screening.
Conclusions
Our bibliometric analysis of the literature identified 2,188 publications related to CIPN between 2001 and 2021. Our analysis identified specific countries, institutions, authors, and journals, that made significant contributions to this field of research during the study period. We focused on specific research topics to explore the trends in CIPN research. Oxaliplatin, paclitaxel, QOL, and pain management, remain the current research targets in the CIPN field. Neuroinflammation provides a potential direction for the study of CIPN mechanisms. Non-pharmacological therapies, such as exercise and acupuncture therapy, will become a key research focus in the future to identify the possible beneficial treatment combinations.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
JG, MH, and GW contributed to concept, design, and manuscript writing. ZG and LL were responsible for literature search, data acquisition, data analysis, and statistical analysis. CH and JY contributed to data acquisition, supervision, and edited the manuscript. JH and YJ reviewed the manuscript. All authors read and approved the final manuscript.
Funding
This research was supported by the National Natural Science Foundation of China (Reference: 82004339), the Project of National Clinical Research Base of Traditional Chinese Medicine in Jiangsu Province (Reference: JD2019SZXYB02), the Jiangsu Province TCM Leading Talent Training project (Reference: SLJ0211), the Jiangsu Science and Technology Department Social Development-Clinical Frontier Technology (Reference: BE2019767 and BRA2019100), and the Scientific Research Project of Jiangsu Provincial Health Commission (Reference: H2019095).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2021.793663/full#supplementary-material
Details of search strategy.
The collaborative relationships between different authors.
References
- 1.Pike CT, Birnbaum HG, Muehlenbein CE, Pohl GM, Natale RB. Healthcare costs and workloss burden of patients with chemotherapy-associated peripheral neuropathy in breast, ovarian, head and neck, and nonsmall cell lung cancer. Chemother Res Pract. (2012) 2012:913848. 10.1155/2012/913848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Colvin LA. Chemotherapy-induced peripheral neuropathy: where are we now? Pain. (2019) 160(Suppl. 1):S1–10. 10.1097/j.pain.0000000000001540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones D, Zhao F, Brell J, Lewis MA, Loprinzi CL, Weiss M, et al. Neuropathic symptoms, quality of life, and clinician perception of patient care in medical oncology outpatients with colorectal, breast, lung, and prostate cancer. J Cancer Surviv. (2015) 9:1–10. 10.1007/s11764-014-0379-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ma J, Kavelaars A, Dougherty PM, Heijnen CJ. Beyond symptomatic relief for chemotherapy-induced peripheral neuropathy: targeting the source. Cancer. (2018) 124:2289–98. 10.1002/cncr.31248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ezendam NP, Pijlman B, Bhugwandass C, Pruijt JF, Mols F, Vos MC, et al. Chemotherapy-induced peripheral neuropathy and its impact on health-related quality of life among ovarian cancer survivors: results from the population-based PROFILES registry. Gynecol Oncol. (2014) 135:510–7. 10.1016/j.ygyno.2014.09.016 [DOI] [PubMed] [Google Scholar]
- 6.Han Y, Smith MT. Pathobiology of cancer chemotherapy-induced peripheral neuropathy (CIPN). Front Pharmacol. (2013) 4:156. 10.3389/fphar.2013.00156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zajaczkowska R, Kocot-Kepska M, Leppert W, Wrzosek A, Mika Wordliczek J. Mechanisms of chemotherapy-induced peripheral neuropathy. Int J Mol Sci. (2019) 20:1451. 10.3390/ijms20061451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith EM, Pang H, Cirrincione C, Fleishman S, Paskett ED, Ahles T, et al. Effect of duloxetine on pain, function, and quality of life among patients with chemotherapy-induced painful peripheral neuropathy: a randomized clinical trial. JAMA. (2013) 309:1359–67. 10.1001/jama.2013.2813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Takenaka M, Iida H, Matsumoto S, Yamaguchi S, Yoshimura N, et al. Successful treatment by adding duloxetine to pregabalin for peripheral neuropathy induced by paclitaxel. Am J Hosp Palliat Care. (2013) 30:734–6. 10.1177/1049909112463416 [DOI] [PubMed] [Google Scholar]
- 10.Ellegaard O, Wallin JA. The bibliometric analysis of scholarly production: how great is the impact? Scientometrics. (2015) 105:1809–31. 10.1007/s11192-015-1645-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Donthu N, Kumar S, Mukherjee D, Pandey N, Lim WM. How to conduct a bibliometric analysis: an overview and guidelines. J Business Res. (2021) 133:285–96. 10.1016/j.jbusres.2021.04.070 [DOI] [Google Scholar]
- 12.Zhai X, Zhao J, Wang Y, Wei X, Li G, Yang Y, et al. Bibliometric analysis of global scientific research on lncRNA: a swiftly expanding trend. Biomed Res Int. (2018) 2018:7625078. 10.1155/2018/7625078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang YP, Hu RX, Han M, Lai BY, Liang SB, Chen BJ, et al. Evidence base of clinical studies on Qi Gong: a bibliometric analysis. Comp Ther Med. (2020) 50:102392. 10.1016/j.ctim.2020.102392 [DOI] [PubMed] [Google Scholar]
- 14.Lai H, Jiang W, Zhao J, Dinglin X, Li Y, Li S, et al. Global trend in research and development of CDK4/6 inhibitors for clinical cancer therapy: a bibliometric analysis. J Cancer. (2021) 12:3539–47. 10.7150/jca.51609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang W, Zhang J, Ma R. The prediction of infectious diseases: a bibliometric analysis. Int J Environ Res Public Health. (2020) 17:6218. 10.3390/ijerph17176218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yanbing S, Ruifang Z, Chen W, Shifan H, Hua L, Zhiguang D. Bibliometric analysis of Journal of Nursing Management from 1993 to 2018. J Nurs Manag. (2020) 28:317–31. 10.1111/jonm.12925 [DOI] [PubMed] [Google Scholar]
- 17.Qi B, Jin S, Qian H, Zou Y. Bibliometric analysis of chronic traumatic encephalopathy research from 1999 to 2019. Int J Environ Res Public Health. (2020) 17:1–15. 10.3390/ijerph17155411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aria M, Cuccurullo C. Bibliometrix: an R-tool for comprehensive science mapping analysis. J Informetr. (2017) 11:959–75. 10.1016/j.joi.2017.08.00733219880 [DOI] [Google Scholar]
- 19.Hirsch JE. An index to quantify an individual's scientific research output. Proc Natl Acad Sci USA. (2015) 102:16569–72. 10.1073/pnas.0507655102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perianes-Rodriguez A, Waltman L, van Eck NJ. Constructing bibliometric networks: a comparison between full and fractional counting. J Informetr. (2016) 10:1178–95. 10.1016/j.joi.2016.10.006 [DOI] [Google Scholar]
- 21.Argyriou AA, Cavaletti G, Antonacopoulou A, Genazzani AA, Briani C, Bruna J, et al. Voltage-gated sodium channel polymorphisms play a pivotal role in the development of oxaliplatin-induced peripheral neurotoxicity: results from a prospective multicenter study. Cancer. (2013) 119:3570–7. 10.1002/cncr.28234 [DOI] [PubMed] [Google Scholar]
- 22.Shahriari-Ahmadi A, Fahimi A, Payandeh M, Sadeghi M. Prevalence of oxaliplatin-induced chronic neuropathy and influencing factors in patients with colorectal cancer in Iran. Asian Pac J Cancer Prev. (2015) 16:7603–6. 10.7314/APJCP.2015.16.17.7603 [DOI] [PubMed] [Google Scholar]
- 23.Palugulla S, Dkhar SA, Kayal S, Narayan SK. Oxaliplatin-induced peripheral neuropathy in south Indian cancer patients: a prospective study in digestive tract cancer patients. Indian J Med Paediatr Oncol. (2017) 38:502–7. 10.4103/ijmpo.ijmpo_143_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilson RH, Lehky T, Thomas RR, Quinn MG, Floeter MK, Grem JL. Acute oxaliplatin-induced peripheral nerve hyperexcitability. J Clin Oncol. (2002) 20:1767–74. 10.1200/JCO.2002.07.056 [DOI] [PubMed] [Google Scholar]
- 25.Pachman DR, Qin R, Seisler DK, Smith EM, Beutler AS, Ta LE, et al. Clinical course of oxaliplatin-induced neuropathy: results from the randomized phase iii trial N08CB (Alliance). J Clin Oncol. (2015) 33:3416–22. 10.1200/JCO.2014.58.8533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grothey A. Clinical management of oxaliplatin-associated neurotoxicity. Clin Colorectal Cancer. (2005) 5(Suppl. 1):S38–46. 10.3816/CCC.2005.s.006 [DOI] [PubMed] [Google Scholar]
- 27.Reyes-Gibby CC, Morrow PK, Buzdar A, Shete S. Chemotherapy-induced peripheral neuropathy as a predictor of neuropathic pain in breast cancer patients previously treated with paclitaxel. J Pain. (2009) 10:1146–50. 10.1016/j.jpain.2009.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chaudhry V, Rowinsky EK, Sartorius SE, Donehower RC, Cornblath DR. Peripheral neuropathy from taxol and cisplatin combination chemotherapy: clinical and electrophysiological studies. Ann Neurol. (1994) 35:304–11. 10.1002/ana.410350310 [DOI] [PubMed] [Google Scholar]
- 29.Eckhoff L, Feddersen S, Knoop AS, Ewertz M, Bergmann TK. Docetaxel-induced neuropathy: a pharmacogenetic case-control study of 150 women with early-stage breast cancer. Acta Oncol. (2015) 54:530–7. 10.3109/0284186X.2014.969846 [DOI] [PubMed] [Google Scholar]
- 30.Molassiotis A, Cheng HL, Leung KT, Li YC, Wong KH, Au JSK, et al. Risk factors for chemotherapy-induced peripheral neuropathy in patients receiving taxane- and platinum-based chemotherapy. Brain Behav. (2019) 9:e01312. 10.1002/brb3.1312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gu J, Lu H, Chen C, Gu Z, Hu M, Liu L, et al. Diabetes mellitus as a risk factor for chemotherapy-induced peripheral neuropathy: a meta-analysis. Support Care Cancer. (2021) 29:7461–9. 10.1007/s00520-021-06321-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mizrahi D, Park SB, Li T, Timmins HC, Trinh T, Au K, et al. Hemoglobin, body mass index, and age as risk factors for paclitaxel- and oxaliplatin-induced peripheral neuropathy. JAMA Netw Open. (2021) 4:e2036695. 10.1001/jamanetworkopen.2020.36695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Battaglini E, Goldstein D, Grimison P, McCullough S, Mendoza-Jones P, Park SB. Chemotherapy-induced peripheral neurotoxicity in cancer survivors: predictors of long-term patient outcomes. J Natl Compr Canc Netw. (2021) 19:821–8. 10.6004/jnccn.2021.70260 [DOI] [PubMed] [Google Scholar]
- 34.Park HJ. Chemotherapy induced peripheral neuropathic pain. Korean J Anesthesiol. (2014) 67:4–7. 10.4097/kjae.2014.67.1.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sisignano M, Baron R, Scholich K, Geisslinger G. Mechanism-based treatment for chemotherapy-induced peripheral neuropathic pain. Nat Rev Neurol. (2014) 10:694–707. 10.1038/nrneurol.2014.211 [DOI] [PubMed] [Google Scholar]
- 36.Mols F, Beijers AJ, Vreugdenhil G, Verhulst A, Schep G, Husson O. Chemotherapy-induced peripheral neuropathy, physical activity and health-related quality of life among colorectal cancer survivors from the PROFILES registry. J Cancer Surviv. (2015) 9:512–22. 10.1007/s11764-015-0427-1 [DOI] [PubMed] [Google Scholar]
- 37.Miaskowski C, Mastick J, Paul SM, Abrams G, Cheung S, Sabes JH, et al. Impact of chemotherapy-induced neurotoxicities on adult cancer survivors' symptom burden and quality of life. J Cancer Surviv. (2018) 12:234–45. 10.1007/s11764-017-0662-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haidinger R, Bauerfeind I. Long-term side effects of adjuvant therapy in primary breast cancer patients: results of a web-based survey. Breast Care. (2019) 14:111–6. 10.1159/000497233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bonhof CS, van de Poll-Franse LV, Vissers PAJ, Wasowicz DK, Wegdam JA, Revesz D, et al. Anxiety and depression mediate the association between chemotherapy-induced peripheral neuropathy and fatigue: results from the population-based PROFILES registry. Psychooncology. (2019) 28:1926–33. 10.1002/pon.5176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Austin PJ, Moalem-Taylor G. The neuro-immune balance in neuropathic pain: involvement of inflammatory immune cells, immune-like glial cells and cytokines. J Neuroimmunol. (2010) 229:26–50. 10.1016/j.jneuroim.2010.08.013 [DOI] [PubMed] [Google Scholar]
- 41.Sandireddy R, Yerra VG, Areti A, Komirishetty P, Kumar A. Neuroinflammation and oxidative stress in diabetic neuropathy: futuristic strategies based on these targets. Int J Endocrinol. (2014) 2014:674987. 10.1155/2014/674987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Warwick RA, Hanani M. The contribution of satellite glial cells to chemotherapy-induced neuropathic pain. Eur J Pain. (2013) 17:571–80. 10.1002/j.1532-2149.2012.00219.x [DOI] [PubMed] [Google Scholar]
- 43.Westbom C, Thompson JK, Leggett A, MacPherson M, Beuschel S, Pass H, et al. Inflammasome modulation by chemotherapeutics in malignant mesothelioma. PLoS ONE. (2015) 10:e0145404. 10.1371/journal.pone.0145404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fumagalli G, Monza L, Cavaletti G, Rigolio R, Meregalli C. Neuroinflammatory process involved in different preclinical models of chemotherapy-induced peripheral neuropathy. Front Immunol. (2020) 11:626687. 10.3389/fimmu.2020.626687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mozafari N, Ashrafi H, Azadi A. Targeted drug delivery systems to control neuroinflammation in central nervous system disorders. J Drug Delivery Sci Technol. (2021) 66:102802. 10.1016/j.jddst.2021.102802 [DOI] [Google Scholar]
- 46.Wang DS, Wang ZQ, Chen G, Peng JW, Wang W, Deng YH, et al. Phase III randomized, placebo-controlled, double-blind study of monosialotetrahexosylganglioside for the prevention of oxaliplatin-induced peripheral neurotoxicity in stage II/III colorectal cancer. Cancer Med. (2020) 9:151–9. 10.1002/cam4.2693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Su Y, Huang J, Wang S, Unger JM, Arias-Fuenzalida J, Shi Y, et al. The effects of ganglioside-monosialic acid in taxane-induced peripheral neurotoxicity in patients with breast cancer: a randomized trial. J Natl Cancer Inst. (2020) 112:55–62. 10.1093/jnci/djz086 [DOI] [PubMed] [Google Scholar]
- 48.Jordan B, Margulies A, Cardoso F, Cavaletti G, Haugnes HS, Jahn P, et al. Systemic anticancer therapy-induced peripheral and central neurotoxicity: ESMO-EONS-EANO clinical practice guidelines for diagnosis, prevention, treatment and follow-up. Ann Oncol. (2020) 31:1306–19. 10.1016/j.annonc.2020.07.003 [DOI] [PubMed] [Google Scholar]
- 49.Loprinzi CL, Lacchetti C, Bleeker J, Cavaletti G, Chauhan C, Hertz DL, et al. Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: ASCO guideline update. J Clin Oncol. (2020) 38:3325–48. 10.1200/JCO.20.01399 [DOI] [PubMed] [Google Scholar]
- 50.Derman BA, Davis AM. Recommendations for prevention and management of chemotherapy-induced peripheral neuropathy. JAMA. (2021) 326:1058–9. 10.1001/jama.2021.7458 [DOI] [PubMed] [Google Scholar]
- 51.Kutcher AM, LeBaron VT. Evaluating acupuncture for the treatment of chemotherapy-induced peripheral neuropathy: an integrative review. West J Nurs Res. (2021) 9:1–11. 10.1177/0193945921992538 [DOI] [PubMed] [Google Scholar]
- 52.Gewandter JS, Chaudari J, Ibegbu C, Kitt R, Serventi J, Burke J, et al. Wireless transcutaneous electrical nerve stimulation device for chemotherapy-induced peripheral neuropathy: an open-label feasibility study. Support Care Cancer. (2019) 27:1765–74. 10.1007/s00520-018-4424-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Song SY, Park JH, Lee JS, Kim JR, Sohn EH, Jung MS, et al. A randomized, placebo-controlled trial evaluating changes in peripheral neuropathy and quality of life by using low-frequency electrostimulation on breast cancer patients treated with chemotherapy. Integr Cancer Ther. (2020) 19:1534735420925519. 10.1177/1534735420925519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lin WL, Wang RH, Chou FH, Feng IJ, Fang CJ, Wang HH. The effects of exercise on chemotherapy-induced peripheral neuropathy symptoms in cancer patients: a systematic review and meta-analysis. Support Care Cancer. (2021) 29:5303–11. 10.1007/s00520-021-06082-3 [DOI] [PubMed] [Google Scholar]
- 55.Duregon F, Vendramin B, Bullo V, Gobbo S, Cugusi L, Di Blasio A, et al. Effects of exercise on cancer patients suffering chemotherapy-induced peripheral neuropathy undergoing treatment: a systematic review. Crit Rev Oncol Hematol. (2018) 121:90–100. 10.1016/j.critrevonc.2017.11.002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Details of search strategy.
The collaborative relationships between different authors.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.