Abstract
We report successful helminthic transmission of Ehrlichia risticii, the causative agent of Potomac horse fever, using trematode stages collected from Juga yrekaensis snails. The ehrlichial agent was isolated from the blood of experimentally infected horses by culture in murine monocytic cells and identified as E. risticii ultrastructurally and by characterization of three different genes.
Ehrlichia risticii is the causative agent of Potomac horse fever (PHF), a febrile colitis of horses reported in North America and Europe (17, 20). The mode of transmission of E. risticii infection and the reservoir of infection have remained unknown. Other ehrlichial agents are tick transmitted; however, evidence of tick transmission has not been found for E. risticii (4, 8, 19). Recent identification of a close genetic relationship between E. risticii and Neorickettsia helminthoeca isolated from a fluke (Nanophyetus salmincola) suggested that the vector of E. risticii might be a trematode (12, 15). We demonstrated the presence of E. risticii genes in virgulate cercariae from operculate freshwater snails from an area of northern California where PHF is prevalent (2, 13). On the basis of these findings, we formed the hypothesis that snails and their trematodes are involved in the life cycle of E. risticii. Here we report the biological, ultrastructural, and genetic identification of E. risticii in trematode stages collected from freshwater snails and helminthic transmission of E. risticii to horses.
Collection and processing of the snails.
Freshwater snails were collected in October 1998 from a stream that flows through a pasture in Weed, California (Siskiyou County), with a history of PHF in some resident horses. Eighty collected snails, of the species Juga yrekaensis, were extracted from their shells by using sterile scissors and tweezers and kept in phosphate-buffered saline containing antibiotics (10,000 U of penicillin G per ml and 10,000 μg of streptomycin per ml). The mixture was briefly vortexed to allow disruption of the fragile snail tissue and release of the trematode stages. A 50-μl volume of each mixture containing trematode stages and snail tissue was processed for DNA extraction by the use of a previously described alkaline extraction protocol for genomic DNA (18). The templates were tested by a nested PCR that amplifies a 527-bp segment of the 16S rRNA gene of E. risticii as described elsewhere (1). Of the 80 processed freshwater snails, 10 (12.5%) were positive in the nested PCR. The infectious material was prepared as follows: the trematode stages (sporocyst and cercaria) from the PCR-positive snails were removed from the initial mixture by the use of a pipette until no trematode stages were released from the snail tissue by vortexing. The snail-tissue-free infectious material contained a total of 9,600 sporocysts and 208,000 cercariae.
Horses.
Seven healthy 5- to 20-year-old horses, five mares and two geldings, were used as experimental animals (Table 1). The horses were housed in a vector-proof facility at the Equine Research Laboratory, University of California, Davis. Prior to inoculation, the horses tested negative for antibodies to E. risticii by indirect fluorescent antibody assay. The procedures for inoculation and care of the horses were approved by the Animal Care and Use Administrative Committee at the University of California, Davis, and the animal holding facilities are accredited by the American Association for the Accreditation of Laboratory Animal Care. Two horses (no. 1 and 2) were each inoculated subcutaneously with 4,800 sporocysts and 104,000 cercariae. We transfused 100 ml of citrate-treated whole blood collected from horse 1 on day 18 postexposure (fourth day of illness) into two horses (no. 3 and 4) and 100 ml of citrate-treated whole blood collected from horse 2 by day 21 postexposure (second day of illness) into horse 5. Horse 6 was inoculated intravenously with 108 mouse macrophages infected to 80% with E. risticii collected from horse 5 during the acute stage of disease. One additional horse (no. 7), inoculated with uninfected mouse macrophages, served as a control. The inoculated animals were monitored daily for evidence of clinical abnormalities.
TABLE 1.
Experimental infection of horses with E. risticii, the agent of PHF
| Horse | Age (yrs) | Sex | Breed | Origin of challenge |
|---|---|---|---|---|
| 1 | 20 | Mare | Arabian | Trematode stages (sporocyst and cercaria) from snails |
| 2 | 5 | Mare | Warmbred | Trematode stages (sporocyst and cercaria) from snails |
| 3 | 16 | Mare | Thoroughbred | Whole citrated blood from horse 1 |
| 4 | 14 | Mare | Thoroughbred | Whole citrated blood from horse 1 |
| 5 | 14 | Mare | Thoroughbred | Whole citrated blood from horse 2 |
| 6 | 13 | Gelding | Arabian | Mouse macrophages infected with E. risticii from horse 5 |
| 7 | 9 | Gelding | Thoroughbred | Uninfected mouse macrophages |
Laboratory examinations.
Blood was collected from all horses into 10-ml evacuated glass tubes with and without anticoagulant (Vacutainer; Becton Dickinson, Franklin Lakes, N.J.) beginning on the day of experimental infection (day zero) and daily thereafter for 30 days. The leukocyte, erythrocyte, and platelet counts were determined. E. risticii antibodies were detected by the indirect fluorescent antibody assay procedure of Madigan et al. (9). DNA was extracted from peripheral blood leukocytes and from 1 g of feces by using a QIAamp Blood DNA Extraction Kit (Qiagen, Valencia, Calif.). The extracted DNA was subjected to nested PCR as described by Barlough et al. (1). E. risticii was isolated in mouse macrophage cell line P388D1 (American Type Culture Collection, Manassas, Va.) from the buffy coat cells of citrate-treated whole blood of horses 5 and 6 on the second day of fever, using a method previously described for E. risticii (6), and ultrastructurally characterized by light microscopy and transmission electron microscopy.
Sequencing of amplified PCR products.
Nested-PCR products of the 16S rRNA gene from the in vitro-grown E. risticii strain, blood, and fecal samples from horses 1 to 6 were selected for sequencing. Segments of two additional ehrlichial genes, the groEL heat shock protein gene and the 51-kDa major antigen gene, of the in vitro-grown E. risticii strain were amplified essentially as described elsewhere (2, 13). The fragments were purified by the use of a gel extraction kit (QIAquick Gel Extraction Kit; Qiagen). DNA sequencing of both strands of each purified PCR product was performed with a fluorescence-based sequencing system (Applied Biosystems, Foster City, Calif.).
Results.
Horse 1 developed a fever on day 15 after inoculation; this was followed by depression, anorexia, decrease in borborygmal sounds, production of cow-like feces, ventral edema, and leukopenia. The horse recovered after 8 days of sickness without treatment. The nested PCR of the blood buffy coat was positive on day 11 and remained positive through day 25, while that of the feces was positive on day 17 and remained positive through day 28. The serum antibody titer increased from 20 on day 21 to 160 by day 30.
Horse 2 showed fever on day 19 after inoculation, followed by depression, anorexia, decrease in borborygmal sounds, watery diarrhea, leukopenia, and thrombocytopenia. This horse was treated for 5 days, starting on day 24 postexposure, with intravenous oxytetracycline (6.6 mg/kg of body weight every 12 h). The nested PCR of the blood buffy coat became positive on day 13 and remained positive through day 25, while that of the feces became positive on day 21 and remained positive through day 25. The serum antibody titer increased from 20 on day 23 to 40 by day 30.
Horses 3 and 4 developed a fever on days 12 and 13, respectively. These horses developed classical clinical signs of and hematological findings compatible with PHF. Both horses were treated with oxytetracycline and responded to therapy, making uneventful recoveries over the next 48 h. The nested PCR of the blood buffy coat became positive on day 8 (horse 3) or 11 (horse 4) and remained positive through day 20 for both horses. The feces of both horses were nested-PCR positive from day 13 (horse 4) or 14 (horse 3) until day 16 postexposure. By day 30 postinfection, seroconversion had occurred, with titers of 80 and 160 for horses 3 and 4, respectively.
Horse 5 developed the typical clinical and hematological findings of PHF, and the nested PCRs of the blood buffy coat and feces became positive on days 14 and 17, respectively. The nested PCRs remained positive through day 20, when horse 5 was euthanized for necropsy. The pathological findings were consistent with PHF (3).
Horse 6 developed the typical clinical and hematological findings of PHF, and the nested PCR of the blood buffy coat became positive on day 7 and remained positive through day 13, when this horse was euthanized for necropsy. The pathological findings were similar to the findings for horse 5 and were consistent with PHF (3). The inoculation of uninfected mouse macrophages into horse 7 was uneventful.
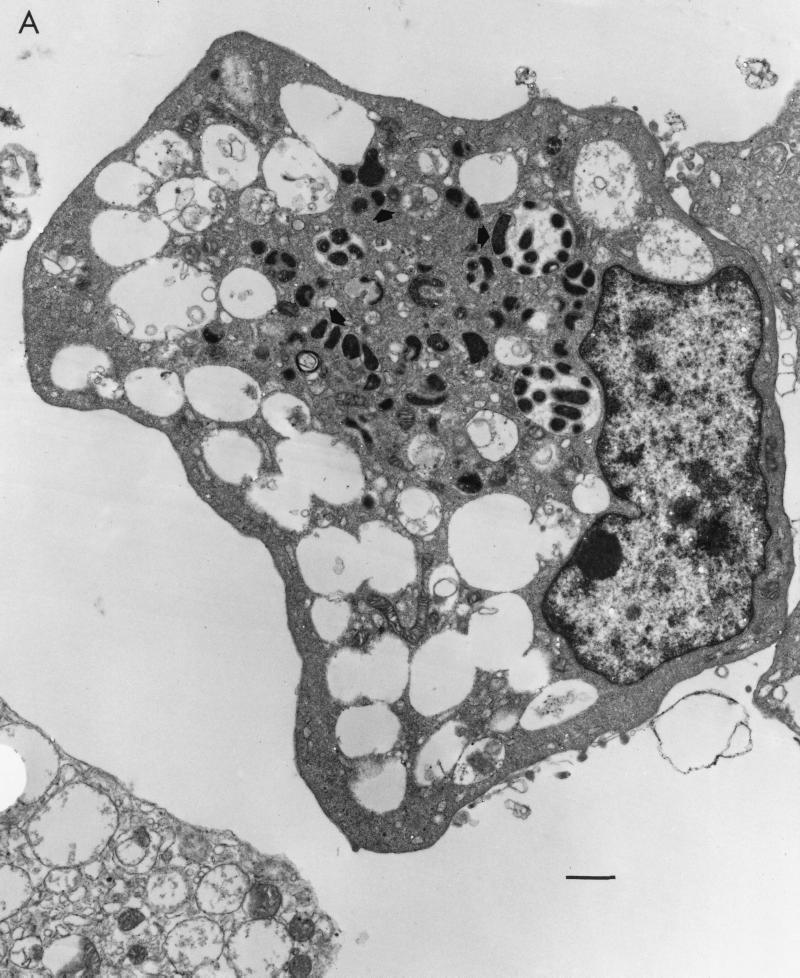
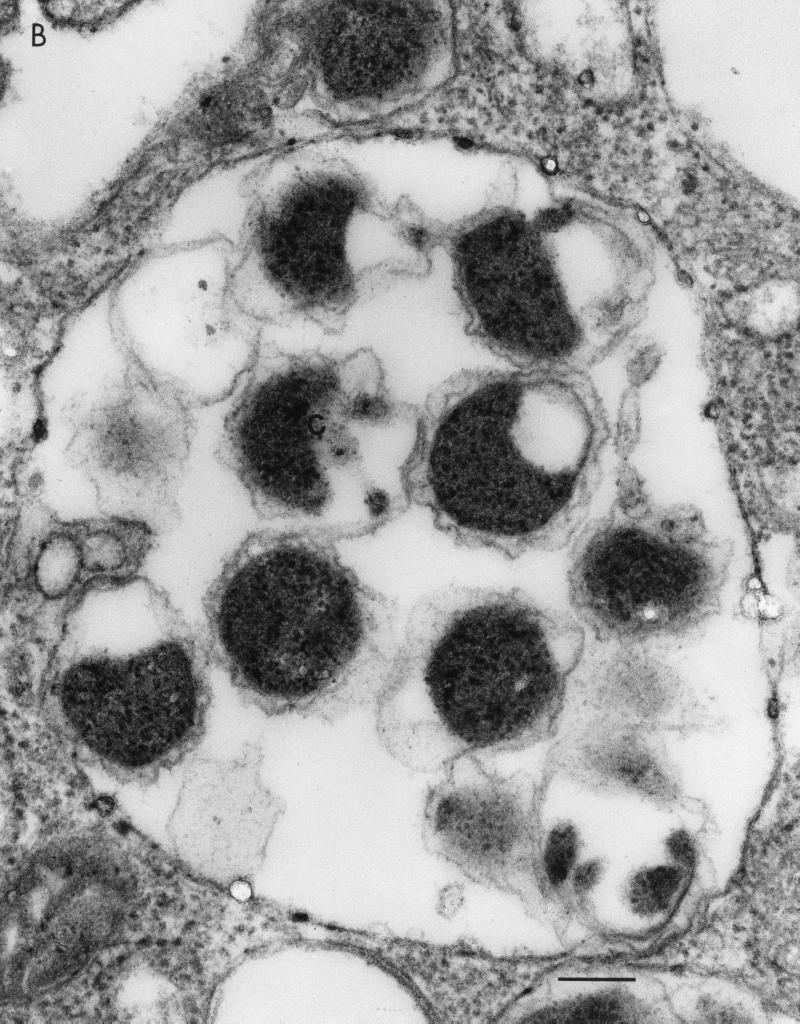
The organism initially isolated from the buffy coats of horses 5 and 6 was successfully propagated in vitro under standard conditions for E. risticii as described previously (6). Using Wright's stain, intracytoplasmic microorganisms resembling rickettsiae were observed in the cultivated mouse macrophages after 10 to 14 days of incubation. Transmission electron microscopy clearly revealed numerous round to oval double-membraned microorganisms, surrounded by a distinct cytoplasmic vacuolar membrane (Fig. 1), which were identical to E. risticii ultrastructurally (5, 16). The nucleotide sequences of the PCR products from snails, blood, and feces of experimentally exposed horses were all identified as part of the 16S rRNA gene of E. risticii. The three gene sequences (16S rRNA gene fragment, groEL heat shock protein gene fragment, and 51-kDa major antigen gene fragment) from the cultivated agent were virtually identical to those of E. risticii from horses and snails that had originated in northern California and were clearly similar to the gene sequences of other variants of E. risticii reported previously (13).
FIG. 1.
(A) Transmission electron micrograph of ehrlichial organisms (arrows) in cytoplasmic vacuoles of mouse macrophage culture. Bar, 1 μm. (B) Transmission electron micrograph, at a higher magnification, showing ultrastructure of the culture-derived causative agent of equine monocytic ehrlichiosis. Single organisms are surrounded by a distinct cytoplasmic vacuolar membrane. Note the rippled outer membrane of the organism. Bar, 0.2 μm.
Discussion.
Despite intensive research efforts for over 20 years, PHF has remained a mystery because the life cycle of the agent and the mode of transmission are unknown. The involvement of an aquatic environment in the life cycle of E. risticii has been recently demonstrated through the detection of this organism in trematodes that use operculate freshwater snails as intermediate hosts (2, 13). In this study, we uncovered a part of the mystery, and here we describe the first helminth-associated transmission of E. risticii in horses.
The trematode isolation technique used in this study allowed us to collect and test specifically trematodes without snail tissue, which is potentially an inhibitor of PCR. The described method for the detection of helminth-associated ehrlichial organisms from freshwater snails may be utilized in the study of other ehrlichiae with unknown vectors, such as Ehrlichia sennetsu, which infects humans.
The clinical signs and hematological changes observed in horses 1 and 2 after infection with trematodes were consistent with PHF. We showed that helminthic infection not only is possible but that it produces a clinical disease similar to that seen in naturally infected horses and in horses infected with blood from acutely sick horses or with E. risticii grown in cell culture (5, 7, 10, 11, 14).
We are aware that subcutaneous transmission does not necessarily mimic the natural route of infection, which most likely is oral, via ingestion of infectious trematode stages. Since E. risticii infection is known to be transmitted by whole blood, we infected three additional horses by intravenous transfusion of blood collected from horses 1 and 2 during the acute stage of the disease. The clinical findings for horses 3, 4, and 5 and the pathological picture of horse 5 were consistent with PHF.
To prove that the organism described in this study is the causative agent of PHF, we cultured the agent isolated from horse 5 in a continuous cell line. Ultrastructurally, the agent was similar to E. risticii according to criteria established by Rikihisa (16). The molecular characterization of the etiological agent from the mouse macrophages, performed on three genes, indicated that the source organism closely resembled E. risticii, and the sequences of all three genes were virtually identical to those of equine and snail E. risticii strains from northern California (13).
To test the cell culture isolate for pathogenicity, and to fulfill the criteria of Koch's postulates, we successfully transmitted the agent to horse 6. Consequently, we were able to reisolate the agent from the blood of horse 6. Thus, our results provide evidence that E. risticii infection involves a helminth trematode life cycle stage in freshwater snails and that E. risticii exists in nature in an aquatic habitat.
Nucleotide sequence accession numbers.
The sequences for the E. risticii agent newly reported in this paper have been assigned the following GenBank accession numbers: AF179351 for the 16S rRNA gene fragment, AF179349 for the groEL heat shock protein gene fragment, and AF179350 for the 51-kDa major antigen gene fragment.
Acknowledgments
We thank Paul Lee and Bob Munn for performing the electron microscopy, Robert Fairley for performing necropsy and histopathology procedures, and Jerold Theis for valuable discussions and inspiration. We thank the technicians of the clinical laboratory for the hematological examinations and the caretakers at the Center for Equine Health for their assistance throughout this study.
This work was supported by a grant from the Center for Equine Health, School of Veterinary Medicine, University of California, Davis, with funds provided by the Oak Tree Racing Association, the State of California satellite wagering fund, and contributions by private donors. N.P. is supported by the Schweizerische Stiftung für Medizinisch-Biologische Stipendien, Hoffmann-La Roche AG, Basel, Switzerland.
REFERENCES
- 1.Barlough J E, Rikihisa Y, Madigan J E. Nested polymerase chain reaction for detection of Ehrlichia risticii genomic DNA in infected horses. Vet Parasitol. 1997;68:367–373. doi: 10.1016/s0304-4017(96)01083-7. [DOI] [PubMed] [Google Scholar]
- 2.Barlough J E, Reubel G H, Madigan J E, Vredevoe L K, Miller P E, Rikihisa Y. Detection of Ehrlichia risticii, the agent of Potomac horse fever, in freshwater stream snails (Pleuroceridae: Juga spp.) from northern California. Appl Environ Microbiol. 1998;64:2888–2893. doi: 10.1128/aem.64.8.2888-2893.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cordes D O, Perry B D, Rikihisa Y, Chickering W R. Enterocolitis caused by Ehrlichia sp. in the horse (Potomac horse fever) Vet Pathol. 1986;23:471–477. doi: 10.1177/030098588602300418. [DOI] [PubMed] [Google Scholar]
- 4.Hahn N E, Fletcher M, Rice R M, Kocan K M, Hansen J W, Hair J A, Barker R W, Perry B D. Attempted transmission of Ehrlichia risticii, causative agent of Potomac horse fever, by the ticks Dermacentor variabilis, Rhipicephalus sanguineus, Ixodes scapularis, and Amblyomma americanum. Exp Appl Acarol. 1990;8:41–50. doi: 10.1007/BF01193380. [DOI] [PubMed] [Google Scholar]
- 5.Holland C J, Ristic M, Cole A I, Johnson P, Baker G, Goetz T. Isolation, experimental transmission, and characterization of causative agent of Potomac horse fever. Science. 1985;227:522–524. doi: 10.1126/science.3880925. [DOI] [PubMed] [Google Scholar]
- 6.Holland C J, Weiss E, Burgdorfer W, Cole A I, Kakoma I. Ehrlichia risticii sp. nov.: etiological agent of equine monocytic ehrlichiosis (synonym, Potomac horse fever) Int J Syst Bacteriol. 1985;35:524–526. [Google Scholar]
- 7.Knowles R C, Anderson C W, Shipley W D, Whitlock R H, Perry B D, Davidson J P. Acute equine diarrhea syndrome (AEDS): a preliminary report. Proc Am Assoc Equine Pract. 1983;29:353–357. [Google Scholar]
- 8.Levine J F, Levy M G, Nicholson W L, Gager R B. Attempted Ehrlichia risticii transmission with Dermacentor variabilis (Acari: Ixodidae) J Med Entomol. 1990;27:931–933. doi: 10.1093/jmedent/27.5.931. [DOI] [PubMed] [Google Scholar]
- 9.Madigan J E, Rikihisa Y, Palmer J E, DeRock E, Mott J. Evidence for a high rate of false-positive results with the indirect fluorescent antibody test for Ehrlichia risticii antibody in horses. J Am Vet Med Assoc. 1995;207:1448–1453. [PubMed] [Google Scholar]
- 10.Palmer J E. Potomac horse fever. Vet Clin N Am Equine Pract. 1993;9:399–410. doi: 10.1016/s0749-0739(17)30406-6. [DOI] [PubMed] [Google Scholar]
- 11.Perry B D, Rikihisa Y, Saunders G K. Intradermal transmission of Potomac horse fever. Vet Rec. 1985;116:246–247. doi: 10.1136/vr.116.9.246. [DOI] [PubMed] [Google Scholar]
- 12.Pretzman C, Ralph D, Stothard D R, Fuerst P A, Rikihisa Y. 16S rRNA gene sequence of Neorickettsia helminthoeca and its phylogenetic alignment with members of the genus Ehrlichia. Int J Syst Bacteriol. 1995;45:207–211. doi: 10.1099/00207713-45-2-207. [DOI] [PubMed] [Google Scholar]
- 13.Reubel G H, Barlough J E, Madigan J E. Production and characterization of Ehrlichia risticii, the agent of Potomac horse fever, from snails (Pleuroceridae: Juga spp.) in aquarium culture and genetic comparison to equine strains. J Clin Microbiol. 1998;36:1501–1511. doi: 10.1128/jcm.36.6.1501-1511.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rikihisa Y, Perry B D. Causative ehrlichial organisms in Potomac horse fever. Infect Immun. 1985;49:513–517. doi: 10.1128/iai.49.3.513-517.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rikihisa Y. Cross-reacting antigens between Neorickettsia helminthoeca and Ehrlichia species, shown by immunofluorescence and Western immunoblotting. J Clin Microbiol. 1991;29:2024–2029. doi: 10.1128/jcm.29.9.2024-2029.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rikihisa Y. The tribe Ehrlichieae and ehrlichial diseases. Clin Microbiol Rev. 1991;4:286–308. doi: 10.1128/cmr.4.3.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ristic M. Current strategies in research on ehrlichiosis. In: Williams J C, Kakoma I, editors. Ehrlichiosis: a vector-borne disease of animals and humans. Boston, Mass: Kluwer Academic Publishers; 1990. pp. 136–153. [Google Scholar]
- 18.Rudbeck L, Dissing J. Rapid, simple alkaline extraction of human genomic DNA from whole blood, buccal epithelial cells, semen and forensic stains for PCR. BioTechniques. 1998;25:588–592. doi: 10.2144/98254bm09. [DOI] [PubMed] [Google Scholar]
- 19.Schmidtmann E T, Robl M G, Carroll J F. Attempted transmission of Ehrlichia risticii by field-captured Dermacentor variabilis (Acari: Ixodidae) Am J Vet Res. 1986;47:2393–2395. [PubMed] [Google Scholar]
- 20.van der Kolk J H, de Groot J. Equine monocytic ehrlichiosis (EME), a review. Tijdschr Diergeneeskd. 1991;116:721–727. [PubMed] [Google Scholar]