Abstract
Due to the continuous rise of global temperatures and heatwaves worldwide as a result of climate change, concerns for the health and safety of working populations have increased. Workers in the food production chain, particularly farmworkers, are especially vulnerable to heat stress due to the strenuous nature of their work, which is performed primarily outdoors under poor working conditions. At the cross-section of climate change and farmworkers' health, a scoping review was undertaken to summarize the existing knowledge regarding the health impacts associated with climate change and heat stress, guide future research toward better understanding current and future climate change risks, and inform policies to protect the health and safety of agricultural workers. A systematic search of 5 electronic databases and gray literature websites was conducted to identify relevant literature published up until December 2021. A total of 9045 records were retrieved from the searches, of which 92 articles were included in the final review. The majority of the reviewed articles focused on heat-related illnesses (n = 57) and kidney diseases (n = 28). The risk factors identified in the reviewed studies included gender, dehydration, heat strain, wearing inappropriate clothing, workload, piece-rate payment, job decision latitude, and hot environmental conditions. On the other hand, various protective and preventive factors were identified including drinking water, changing work hours and schedule of activities, wearing appropriate clothing, reducing soda consumption, taking breaks in shaded or air-conditioned areas, and increasing electrolyte consumption in addition to improving access to medical care. This review also identified various factors that are unique to vulnerable agricultural populations, including migrant and child farmworkers. Our findings call for an urgent need to expand future research on vulnerable agricultural communities including migrant workers so as to develop effective policies and interventions that can protect these communities from the effects of heat stress.
Keywords: agricultural workers, farmworkers, climate change, global warming, heat stress, heat exposure, occupational health
Introduction
Climate change has led to a significant increase in global average temperatures; temperatures on average have increased by about 1.1°C since pre-industrial times (1). In addition, the intensity, frequency, and duration of heatwaves have been rapidly increasing around the globe (2). Nineteen out of the 20 warmest years on record have occurred since 2000 (3). Between 1950 and 2017, a majority of the world's regions has been experiencing at least one extra day of heatwave per decade (4). It is predicted that the trend of rising temperatures and the occurrence of more frequent, longer, and more intense extreme heat events will continue in the future (5, 6). By the end of the century, 1.2 billion people are expected to be affected by heat stress, which is four times the number of people that are currently affected by extreme heat (7). Exposure to high temperatures can result in various adverse health impacts. These range from acute health effects to more severe and chronic conditions and in extreme circumstances these impacts can even lead to death (8–10). The consequences of global warming are expected to have disproportionate impacts on countries and communities that have contributed the least to the problem and are the least able to adapt to heat stress (11).
Compared to the general public, working populations, including farmworkers, are more susceptible to heat stress. The combined effect of the metabolic heat produced internally from heavy physical activity and the external heat from the surrounding environment contributes to the high risk of heat stress among workers (12, 13). Workers engaged in strenuous work at temperatures >35°C are likely to experience heat stress (14). In addition, some occupations require workers to wear protective clothing, which can inhibit sweat evaporation and normal heat dissipation thus exacerbating their risk of heat stress (15). Furthermore, workers who perform their tasks outdoors are vulnerable to heat stress due to prolonged exposure to solar radiation, while workers in indoor settings can also be exposed to heat exposure from the heat generated from work processes or equipment (16). Recent publications warn that climate change is expected to intensify the duration and magnitude of occupational heat stress (17). Projections for the year 2030 estimate the loss of 880,000 work-life-years due to occupational heat stroke mortality in both indoor and outdoor workplaces (18). The impact of rising heat in the workplace is likely to affect the implementation of the 2030 Sustainable Development Goals (SDGs), including those related to poverty, food security, health, decent work, and economic growth and inequality (19).
The agricultural workforce has been recognized as a vulnerable occupational group with an increased risk of adverse health outcomes from rising global temperatures (20, 21). In fact, occupational heat-related mortality is 35 times higher among agricultural workers compared to workers from other industries (22). Agricultural workers are often exposed to hot environmental conditions, which exceed international standards (23–25). In addition, the literature identified several work-related factors that exacerbate the risk of heat stress among agriculture workers, which include (1) performance of intensive manual labor (26), (2) piece-rate payment that encourages agricultural laborers to work beyond their physical limits and avoid taking breaks to rest or hydrate (27, 28), and (3) the lack of control over workplace health and safety practices and adequate access to water, shade, or rest breaks (29, 30). In addition to the harsh working conditions, agricultural workers also face poor living conditions including a lack of access to clean drinking water, adequate housing, and basic social and health care services (31, 32). Furthermore, the majority of farmworkers live in low socioeconomic conditions, whereby a study found that the levels of extreme poverty are four times higher among agricultural workers as compared to non-agricultural workers (33).
Globally, migrants account for an increasing share of the agricultural workforce, with 16.7 million migrants engaged in the agricultural sector worldwide (34). The migration of agricultural workers is driven by various social, economic, and environmental factors that are likely to get exacerbated with climate change, leading to a greater flow of migrants especially from low-income countries (35). Migrant agricultural workers often face unique vulnerabilities that affect their health and wellbeing and increase their risks of heat-related health outcomes. Migrant agricultural workers are subjected to unsafe working conditions and increased workplace harassment (36–38). In addition, these workers are not protected by labor regulations and are not represented in labor unions; they often also face language and cultural barriers and lack access to social security (39).
Several interlinkages between climate change, farmworkers' health, and food production have been identified in the literature. Climate change is expected to impact agricultural production, leading to higher levels of poverty and food insecurity among agricultural workers (40). Furthermore, it is projected that farmworkers will only be able to work for a fraction of the hours they currently work due to rising heat stress. This can lead to a further decline in agricultural production (41). One estimate projects that the agricultural sector will account for 60% of the global working hours lost due to heat stress by the year 2030 (19). Moreover, heat related health outcomes among agricultural workers will also reduce their productivity (42). Although agricultural workers play a critical role in food production, studies have shown that they are highly food insecure; they endure precarious working conditions and earn low wages that hinder access to food (43). In addition, the loss of productivity is expected to exacerbate their food insecurity, especially in small-scale and subsistence agriculture (44).
Heat-related Illnesses (HRI) are the most common health effects experienced by agricultural workers as a result of their prolonged exposure to high temperatures (30, 40–42). HRI are a continuum of diseases, ranging from mild symptoms such as heavy sweating, dizziness, fatigue, vomiting, headaches, and muscle cramps to more severe conditions such as life-threatening heat strokes (12). Occupational heat exposure and dehydration have also been linked to an epidemic of chronic kidney diseases referred to as “chronic disease of unknown etiology (CKDu)” among agricultural communities in several hot regions including Central America and Southeast Asia (43–45). In addition, agricultural workers laboring in hot conditions are at an increased risk for workplace injuries due to increased fatigue, reduced alertness, deterioration in psychomotor abilities, and loss of concentration (46, 47).
With the continuous increase in global temperatures and the severity of its impact on the health and safety of the agricultural workforce globally, a scoping review is needed to summarize the existing knowledge regarding the impact of climate change, particularly extreme heat exposure on farmworkers' health and the available prevention strategies to alleviate these impacts on farmworkers. Thus, the aims of this review are to: (1) summarize the available evidence on the effects of climate change on farmworkers' health with a focus on heat-related illnesses, (2) identify the risk factors for heat-related illnesses among farmworkers, and (3) review the preventive measures that are used to minimize heat stress exposure among farmworkers. To the best of our knowledge, no other reviews has been carried out to study the effects of climate change and heat stress on the health and safety of farmworkers. This work also informs policymakers to develop more effective policies and programs to protect vulnerable farming communities from the impacts of climate change.
Methods
Search Strategy
To meet our objectives and map the available literature on this topic, we conducted a scoping review following the PRISMA extension for Scoping Reviews (PRISMA-ScR) (48). In line with this protocol, we developed a search strategy using a combination of controlled vocabulary such as Medical Subject Headings (MeSH) and keywords for each of the 5 selected electronic databases: Medline, Embase, Scopus, CINAHL, and Web of Science. The search strategies are detailed in the Supplementary Material (Supplementary Table S1). Two concepts were used in our search strategy: (1) heat exposure and (2) agricultural setting.
Keywords used for heat exposure included: extreme temperature, thermal comfort, thermal sensation, global warming, heatwave, and climate variability.
Keywords used for agricultural setting included: farmworker, farmer, harvester, grower, agriculturalist, and agricultural worker.
No restrictions were applied on the year of publication and language to capture the maximum number of articles that have addressed the topic in the literature. Specific health outcomes were also not included in the search strategy to capture all heat-related health effects covered in the medical and public health literature that was published in the selected databases.
In addition, the websites of international agencies (ILO, WHO, and UNDP) and agricultural databases (AGRIS FAO and AgEcon) were manually searched to identify relevant articles. The reference lists were also checked in the gray literature to find additional studies that could be relevant for the review. The database search was conducted on December 6, 2021 and the gray literature search was conducted on December 24, 2021.
Eligibility Criteria
We aimed to reduce the restrictions in the eligibility criteria so as to explore most of the available literature on heat-related health outcomes among farmworkers. We considered as eligible for this scoping review the following:
Outcome of interest: Studies assessing: (1) Health outcomes related to heat exposure; (2) Risk and protective factors associated with health outcomes; and (3) Preventive measures. We excluded studies assessing outcomes not related to heat stress and studies that calculate the effects with simulations or models instead of actual measurements in humans.
Population of interest: Farmworkers of all age groups.
Context of interest: Studies assessing the impact of occupational heat exposure on workers' health and safety.
Study design: Primary studies including quantitative and qualitative methods. We excluded editorials, commentaries, letters to the editors, reviews, reports, and conference abstracts.
Selection Process
Two stages for the screening and selection of articles were carried out independently and in duplicates by two reviewers (M.K. and D.A.H.) and guided by the pre-established eligibility criteria. Calibration exercises were conducted by the 2 reviewers (M.K. and D.A.H.) to assess and refine, if necessary, the screening questions and ensure the validity of the selection process. The records that were deemed eligible for inclusion by the two reviewers during the title and abstract screening phase were screened at the full-text stage. Disagreements about inclusion in the full-text screening were resolved through discussion until consensus was reached between both reviewers. If consensus could not be reached, a third reviewer (R.R.H.) was consulted to resolve the disagreement.
Data Abstraction and Analysis
Data were extracted from the included articles by one of the reviewers (M.K.), using a pre-established data abstraction form. This form was developed and reviewed by the authors of this review. A calibration exercise was conducted by the 2 reviewers (M.K. and D.A.H.) before the data abstraction phase. The calibration allowed the 2 reviewers to assess and refine the fields/data items in the form and to ensure the validity of the data abstraction process (i.e., the same information is extracted by both reviewers). Information relating to the study characteristics and the findings were extracted from each selected study. These included: (1) first author and year of publication, (2) study location and region, (3) study design, (4) study population and sample size, (5) heat exposure metric, (6) period of heat exposure and study duration, (7) methods of data collection (8) data analysis, (9) heat-related health outcome, (10) risk factors, (11) protective factors and (12) preventative measures.
Data on health outcomes, risk and protective factors, and preventative measures were descriptively summarized and analyzed to identify research gaps. Furthermore, statistically significant risk and protective factors from quantitative studies and all factors from qualitative studies were classified into superordinate categories.
Results
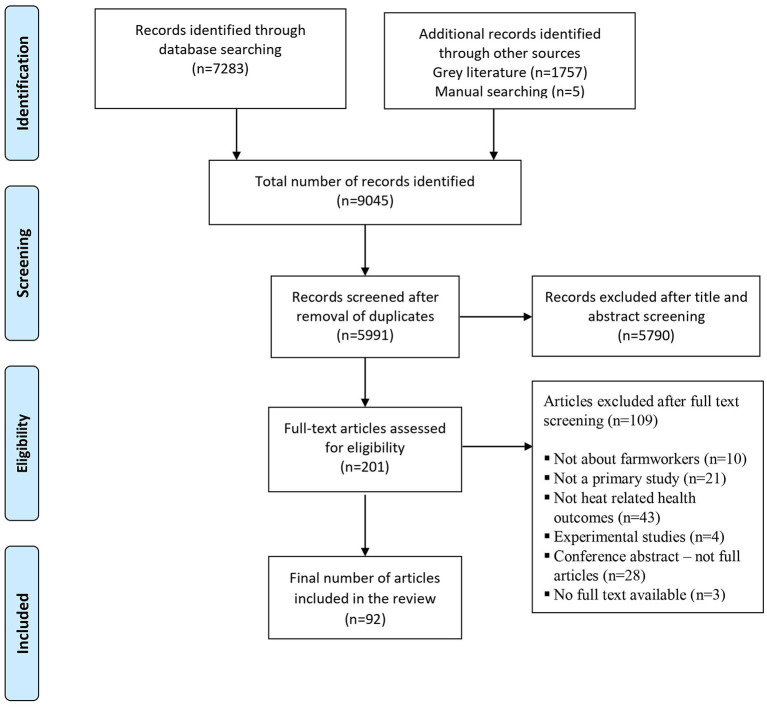
The selection process of the articles is presented in Figure 1 using the PRISMA flow diagram. 7,283 records were identified from the database search, while an additional 1,757 records were identified through searching of gray literature. In addition, 5 records were identified through manual searching. 5,991 records remained for the title and abstract screening stage after duplicate removal. After completing the title and abstract screening of the identified records, 201 articles remained for full-text screening. One hundred nine records were excluded for various reasons as listed in the flow diagram and 92 records were included for the final review.
Figure 1.
Flow chart of selection process for included studies.
Descriptive Characteristics of Included Studies
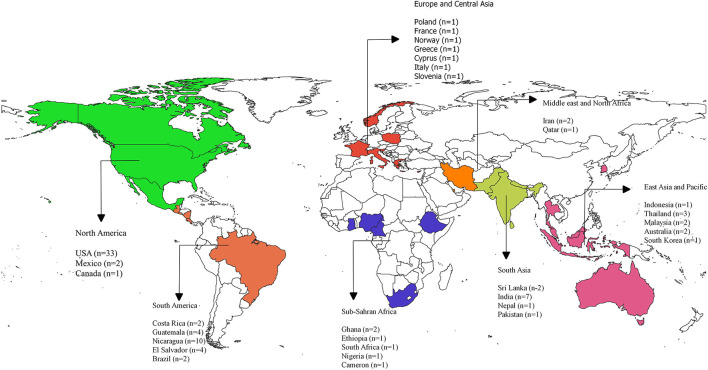
Table 1 presents the descriptive characteristics of the studies included in this review. The results reveal an increase in the number of articles published on the topic over the last couple of years. The highest number of publications was in 2019, with 16 articles published that year. The majority of reviewed articles were quantitative studies, which included cross-sectional (n = 65; 71%), longitudinal (n = 15; 16%) and comparative studies (n = 1; 1%). The remaining articles used qualitative (n = 9; 10%) and mixed methods designs (n = 2; 2%). In addition, the majority of the reviewed articles used questionnaires (n = 69; 75%), followed by physiological measurements (n = 38; 41%) and biological sampling (n = 36; 39%) as data collection tools. While some studies used interview/focus groups (n = 7; 8%), the rest of the articles used observations (n = 3; 3%). The majority of the included articles focused on agricultural workers/farmworkers (n = 54; 59%) and sugarcane farmers/cutters (n = 23; 25%). While the remaining articles studied pesticide applicators (n = 1;1%), nursery workers (n = 1; 1%), sheep shearers (n = 1; 1%), tractor driver (n = 1; 1%), forestry (n = 2; 2%), harvesters (n = 4; 4%), fernery workers (n = 3; 3%), crop workers (n = 1;1%), horticulture workers (n = 1;1%) and vineyard workers (n = 1; 1%). The majority of the reviewed studies were conducted in North America (n = 36; 39%), followed by South America (n = 22; 24%), and South Asia (n = 11; 12%). The remaining articles were distributed among East Asia and the Pacific (n = 9; 10%), Europe and Central Asia (n = 6; 7%), the Middle East and North Africa (n = 3; 3%), and Sub-Saharan Africa (n = 6; 7%). Figure 2 presents a map of the geographical distribution of the studies by country.
Table 1.
Descriptive characteristics of the included articles.
| Characteristics | N | % |
|---|---|---|
| Study design | ||
| Quantitative studies | ||
| Cross-sectional | 65 | 71 |
| Longitudinal | 15 | 16 |
| Comparative | 1 | 1 |
| Qualitative | 9 | 10 |
| Mixed methods | 2 | 2 |
| Data collection methods | ||
| Questionnaire | 69 | 75 |
| Biological sampling | 36 | 39 |
| Physiological measurements | 38 | 41 |
| Interview/focus group | 7 | 8 |
| Observation | 3 | 3 |
| Study population | ||
| Forestry workers | 2 | 2 |
| Farmworkers/agricultural workers | 54 | 59 |
| Fernery workers | 3 | 3 |
| Tractor driver | 1 | 1 |
| Nursery workers | 1 | 1 |
| Horticulture | 1 | 1 |
| Harvesters | 4 | 4 |
| Crop workers | 1 | 1 |
| Pesticide applicators | 1 | 1 |
| Sheep shearers | 1 | 1 |
| Sugarcane workers/cutters | 23 | 25 |
| Vineyard workers | 1 | 1 |
| Region | ||
| North America | 36 | 39 |
| South America | 22 | 24 |
| Middle East and North Africa | 3 | 3 |
| South Asia | 11 | 12 |
| East Asia and Pacific | 9 | 10 |
| Europe and Central Asia | 6 | 7 |
| Sub-Saharan Africa | 6 | 7 |
Figure 2.
Geographical distribution of the included studies. “n” denotes the number of publications in each country; USA, United States of America.
The types of heat-related health outcomes assessed in the included studies are presented in Table 2. The most common heat-related health outcome assessed was HRI (n = 57; 62%). Twenty-seven out of 57 of these studies relied on self-reported HRI symptoms (25, 27, 30, 40–42, 49–69), while 21 measured various physiological parameters such as core body temperature, skin temperature, heart rate, blood pressure, changes in body weight, or urine specific gravity (61, 68, 70–88). Another commonly assessed heat-related health outcome was kidney disease (n = 28; 30%). Several of these studies determined the prevalence of Chronic Kidney Disease (CKD), (89–91) Acute Kidney Injury (AKI) (28, 92–97), and Incident Kidney Injury (IKI) among agricultural workers (98–100). The remaining articles assessed other health outcomes including cardiorespiratory symptoms (n = 1; 1%), respiratory diseases (n = 2; 2%), injuries (n = 1; 1%), reproductive health (n = 1; 1%), skin disorders (n = 1; 1%), and diabetes and hypertension (n = 1; 1%).
Table 2.
Heat-related health outcomes of included studies.
| Heat-related outcomes | N | % |
|---|---|---|
| Heat-related illnesses | 57 | 62 |
| Kidney diseases | 28 | 30 |
| Cardiorespiratory symptoms | 1 | 1 |
| Respiratory diseases | 2 | 2 |
| Injuries | 1 | 1 |
| Skin disorders | 1 | 1 |
| Reproductive health | 1 | 1 |
| Diabetes and hypertension | 1 | 1 |
A variety of heat exposure metrics were used to measure heat stress in the included studies. Overall, 41 articles employed some form of heat exposure metric. Some of these studies used simple ambient weather metrics, including temperature (n = 8; 9%) and relative humidity (n = 4; 4%). In addition, composite indices accounting for temperature and other weather parameters were used such as the Wet Bulb Globe Temperature (WBGT) index (n = 33; 36%), heat index (n = 6; 7%), heat stress index (n = 2; 2%), humidex (n = 2; 2%) and universal thermal climate Index (n = 2; 2%).
Factors Associated With Heat-Related Outcomes
Seventeen articles reported risk or protective factors for HRI, 15 of which reported statistical measures of association, while 3 reported potential factors without a statistical analysis to determine the significance of the association with HRI. In addition, 23 out of 28 studies assessing kidney disease identified various risk or protective factors.
Factors Associated With HRI
Work Organization and Management
Workload.
Three studies assessed the association between core body temperature and workload that was measured using an accelerometer among U.S. farmworkers (Table 2) (74, 75, 79). Two of these studies found that there was a 12% increase in the odds of reaching or exceeding 38°C for every 100 kilocalories of energy expended among fernery workers (74, 79). Similarly, Vega-Arroyo et al. (75) found that an increase in the work rate was associated with higher core body temperatures (β = 0.006, 95% CI: 0.004, 0.009).
Work Duration.
One study found that work duration was associated with greater cardiac strain among vineyard workers (β: 0.219; 95% CI: 0.033–0.405) (85).
Payment Method.
Three studies identified piece-rate payment as a potential risk factor for HRI (Table 3) (27, 101, 102). However, only one study measured the association between HRI and piece-rate payment and found a significant association (OR: 6.20; 95% CI: 1.11–34.54) (27). In contrast, one study did not find a significant association between piece-rate work and HRI (60).
Table 3.
Risk and protective factors associated with HRI.
| Factors | Risk factor | Protective factor | No significant association | Comment* |
|---|---|---|---|---|
| Work organization and management | ||||
| Workload | Mac (79) Mac et al. (74) Vega-Arroyo et al. (75) | Suggested evidence of increased risk of HRI | ||
| Payment method | Crowe et al. (102) Spector et al. (27) Luque et al. (101) | Arcury et al. (60) | Suggested evidence of increased risk of HRI | |
| Job decision latitude | Hansen et al. (29) Lam et al. (103) | Suggested evidence of increased risk of HRI | ||
| Work safety climate | Wilmsen et al. (104) | Limited evidence of increased risk of HRI | ||
| Task duration | Grimbuhler and Viel (85) | Limited evidence of increased risk of HRI | ||
| Behavioral factors | ||||
| Rest in shaded area | Riccò et al. (63) | Fleischer et al. (30) | Limited evidence of reduced risk of HRI | |
| Extra breaks | Fleischer et al. (30) Arnold et al. (51) |
Spector et al. (27) Riccò et al. (63) | Inconsistent or conflicting evidence | |
| Change work hours and activities | Mirabelli et al. (40) | Limited evidence of reduced risk of HRI | ||
| Reduce soda consumption | Fleischer et al. (30) | Limited evidence of reduced risk of HRI | ||
| Fluid intake | Kiatkitroj et al. (69) | Limited evidence of reduced risk of HRI | ||
| Wear excessive clothing | Kiatkitroj et al. (69) | Limited evidence of reduced risk of HRI | ||
| Accessibility to heat prevention and treatment | ||||
| Culture and language | Hansen et al. (29) Lam et al. (103) | Suggested evidence of increased risk of HRI | ||
| Access to toilet | Spector et al. (27) | Limited evidence of increased risk of EHI | ||
| Access to medical attention | Fleischer et al. (30) | Limited evidence of reduced risk of HRI | ||
| Sociodemographic factors | ||||
| Gender | ||||
| Female gender | Mac (79) Mac et al. (74) Mutic et al. (57) Kiatkitroj et al. (69) | Riccò et al. (63) Vega-Arroyo et al. (75) | Suggested evidence of increased risk of HRI | |
| Male gender | Grimbuhler and Viel (85) | |||
| Older age | Arcury et al. (60) Arcury et al. (49) Arnold et al. (51) | Spector et al. (27) | Mutic et al. (57) Riccò et al. (63) Vega-Arroyo et al. (75) Mac et al. (74) Grimbuhler and Viel (85) | Inconsistent or conflicting evidence |
| Migrant status | Riccò et al. (63) Mutic et al. (57) Arcury et al. (49) Arnold et al. (51) | no evidence from increased risk of HRI | ||
| Environmental conditions | ||||
| Hot environmental conditions | Vega-Arroyo et al. (75) Gun and Budd (72) | Mac et al. (74) | Suggested evidence of increased risk of HRI | |
| Grimbuhler and Viel (85) Ioannou et al. (87) Mohammadian et al. (84) |
Suggested evidence: Two or more of the reviewed studies identified the same risk or protective factor.
Limited evidence: Only one study identified the risk or protective factor.
Inconsistent or conflicting evidence: One or more studies identified a specific risk or protective factor while one or more studies identified a contradictory association or a non-significant association.
No evidence: No studies identified a significant association.
criteria used to evaluate the risk factors.
Job Decision Latitude.
Two qualitative studies identified that a lack of control over workplace conditions prevented agricultural workers from accessing HRI preventative measures, such as clean drinking water, shade, and bathroom facilities (29, 103).
Work Safety Climate.
One qualitative study reported through a case study that migrant forestry workers employed by companies with a poor work safety climate were less likely to obtain adequate treatment for various injuries including HRI and to achieve full recovery (104).
Behavioral Factors
In the reviewed studies, various behavioral factors were identified as protective against heat stress, including drinking water (69), reducing soda consumption (30), and changing work hours and activities (40) (Table 3). One study identified that wearing excessive clothing is associated with greater odds of reporting HRI (69). In contrast, other behavioral factors assessed in the reviewed studies such as sun safety behavior and HRI training were reported to have no significant association with HRI symptoms (27, 30, 40, 55, 63).
Accessibility to Heat Prevention and Treatment.
Various risk factors related to accessibility to heat prevention and treatment were identified in the reviewed studies (Table 3). One study identified that a lack of access to bathroom facilities was a risk factor for HRI (27), while another reported that greater access to medical attention was protective for HRI (30). Furthermore, two qualitative studies identified that cultural and language barriers could increase the risk of HRI by preventing workers from understanding proper safety training requirements (29) or interfering with HRI treatment (103).
Sociodemographic Factors
Age.
Three studies identified increasing age as a risk factor for HRI among child farmworkers (49, 51, 60). However, evidence regarding the effect of age on HRI among adult farmworkers was inconsistent between studies. One study reported that increasing age was associated with 0.92 times lower odds of HRI among crop workers (OR: 0.92; 95% CI: 0.87–0.98) (27). In contrast, some studies found that younger workers were more likely to have higher HRI, although the association between age and HRI was not significant (57, 63, 74, 75).
Gender.
Four studies identified female gender to be associated with increasing HRI (Table 3) (57, 69, 74, 79). Two studies found that female fernery workers were 5.38 times more likely to have core body temperature reaching or exceeding 38°C as compared to males after adjusting for energy expenditure (OR: 5.38, 95% CI: 1.03–18.30) (74, 79). In contrast, other studies found no significant association between female gender and HRI (63, 75). In addition, one study identified that male gender was associated with increased mean skin temperature among vineyard workers (β: 1.447; 95% CI: 0.922–1.972) (85).
Migrant Status.
Several studies found no association between migrant status or nationality and increased risk of HRI (49, 51, 57, 63).
Environmental Conditions.
Five studies identified a strong association between HRI and hot environmental conditions as measured by WBGT (Table 3) (72, 75, 84, 85, 87). Vega-Arroyo et al. (75) reported that WBGT was associated with higher core body temperatures (β: 0.03, 95% CI: 0.017–0.05) among migrant farmworkers. In addition, dry bulb temperature was associated with an increase in cardiac strain, including mean heart rate (β: 4.084; 95% CI: 0.442–7.726), relative cardiac cost (β: 3.652; 95% CI: 0.888–6.416), and cardiac workload score (β: 0.644; 95% CI: −0.046–1.334) among vineyard workers (85). However, Mac et al. (74) found that the average WBGT was not a significant predictor of elevated core body temperatures among fernery workers.
Factors Associated With Kidney Disease
Work Organization and Management
Workload.
Two studies conducted in the US reported a positive association between the workload, measured using an accelerometer, and cross-shift AKI among agricultural workers; the reported odds ratios ranged between 1.01 and 1.92 (Table 4) (93, 95). In addition, several studies showed that workers performing the most strenuous tasks had a greater decline in kidney function over a harvest season as compared to workers conducting less strenuous tasks (Table 4) (93, 96, 105, 106). Hansson et al. (100) found that burned cane cutters and seed cutters (who conduct more strenuous tasks) had significantly lower cross-harvest eGFR and higher IKI as compared to field support staff and drip irrigation workers. Similarly, Laws et al. (105) found a significant increase in kidney injury biomarkers (NGAL, NAG, and IL-18) among field workers (cane cutters, seeders, seed cutters, agrichemical applicators, and irrigators) as compared to non-field workers (drivers and factory workers).
Table 4.
Risk and protective factors associated with kidney diseases.
| Factors | Risk factor | Protective Factor | No significant Association | Comment* |
|---|---|---|---|---|
| Work organization and management | ||||
| Workload | Hansson et al. (100) Moyce et al. (95) Moyce et al. (93) Laws et al. (105) Laws et al. (106) Kupferman et al. (96) Moyce et al. (93) | Suggested evidence of increased risk of kidney disease | ||
| Piece-rate payment | Moyce et al. (28) Moyce et al. (95) Moyce et al. (94) | Suggested evidence of increased risk of kidney disease | ||
| Physiological factors | ||||
| Dehydration | Butler-Dawson et al. (92) Sorensen et al. (107) López-Gálvez et al. (108) | Moyce et al. (28) | Suggested evidence of increased risk of kidney disease | |
| Heat strain | López-Gálvez et al. (108) Moyce et al. (28) | Suggested evidence of increased risk of kidney disease |
||
| Behavioral factors | ||||
| Fluid consumption | ||||
| Increased fluid consumption | Moyce et al. (93) | García-Trabanino et al. (109) | Wesseling et al. (110) López-Gálvez et al. (108) | Inconsistent or conflicting evidence |
| Lower fluid consumption | Pundee et al. (111) | |||
| Electrolyte intake | Butler-Dawson et al. (92) Hansson et al. (99) Laws et al. (105) Laws et al. (106) Wesseling et al. (110) |
Suggested evidence of increased risk of kidney disease | ||
| Sugary beverage intake | Hansson et al. (99) Raines et al. (112) | Butler-Dawson et al. (113) Butler-Dawson et al. (92) Moyce et al. (93) | Inconsistent or conflicting evidence | |
| Medications and lifestyle factors | ||||
| NSAIDs use | Butler-Dawson et al. (92) Hansson et al. (99) | Sorensen et al. (107) Wesseling et al. (110) | Inconsistent or conflicting evidence | |
| Sociodemographic factors | ||||
| Female gender | Moyce et al. (28) Jayasekara et al. (114) | Suggested evidence of increased risk of kidney disease | ||
| Socioeconomic status | Jayasekara et al. (114) | Limited evidence of increased risk of kidney disease | ||
| Environmental conditions | ||||
| Agrochemical exposure | Raines et al. (112) García-Trabanino et al. (109) López-Gálvez et al. (108) | Laws et al. (105) Ekiti et al. (91) Fitria et al. (90) Wesseling et al. (110) | Inconsistent or conflicting evidence | |
| Hot environmental conditions | García-Trabanino et al. (109) Raines et al. (112) Sorensen et al. (107) Mix et al. (97) | Suggested evidence of increased risk of kidney disease |
Suggested evidence: Two or more of the reviewed studies identified the same risk or protective factor.
Limited evidence: Only one study identified the risk or protective factor.
Inconsistent or conflicting evidence: One or more studies identified a specific risk or protective factor while one or more studies identified a contradictory association or a non-significant association.
criteria used to evaluate the risk factors.
Payment Method.
Three studies conducted in the US identified piece-rate work as a risk factor for cross-shift AKI among agricultural workers with an odds ratio ranging from 3.02 to 4.52 (Table 4) (28, 94, 95).
Physiological Factors
Dehydration.
Evidence from 3 studies suggested that dehydration was a risk factor for the development of kidney disease among agricultural workers (Table 4) (92, 107, 108). One of these studies found a significant decrease in eGFR of 11.99 mL/min/1.73 m2 (95% CI: −16.88, −7.10) among dehydrated farmworkers when compared to those who were normally hydrated (108). However, one study did not find an association between dehydration and kidney disease (28).
Heat Strain.
Two studies found a significant association between heat strain that was measured using the physiological strain index and the decline in kidney function (28, 108). López-Gálvez et al. (108) found that for every 1% increase in PSI, there was a significant decrease in eGFR of 0.16 mL/min/1.73 m2 (95% CI: −0.15, −0.06).
Behavioral Factors
Fluid Consumption.
Four studies assessed the association between fluid consumption and kidney disease among agricultural workers (Table 4) (28, 107–109, 111). Overall, the studies showed conflicting evidence regarding the effects of fluid consumption on kidney disease. Two studies showed that an increase in fluid consumption was beneficial for preventing kidney disease (109, 111). In contrast, two studies found that fluid consumption was not associated with reduced kidney function (108, 110).
Electrolyte Consumption.
Five studies conducted in Central America identified an association between greater electrolyte intake and improved kidney function (Table 4) (99, 105, 106, 110, 113). Butler-Dawson et al. (92) showed that lower electrolyte intake was associated with higher odds of AKI among sugarcane workers in Guatemala (OR: 0.94, 95% CI: 0.89–0.99). Similarly, Hansson et al. (99) showed that electrolyte consumption was associated with lower IKI (IR: 0.5, 95% CI: 0.2–0.9). In addition, three studies showed that increasing electrolyte consumption was associated with improved kidney function biomarkers (105, 106, 110).
Sugar Consumption.
Two studies conducted in Central America reported that sugar consumption was a risk factor for kidney diseases (Table 4) (99, 112). Raines et al. (112) identified that daily bolis consumption, which is a sugary rehydration packet, was associated with reduced eGFR (OR: 1.48, 95% CI: 1.02–2.14) (112). In contrast, other studies found no association between intake of sugary beverages and kidney disease (Table 4) (92, 93, 113). Overall, evidence regarding the effect of sugar consumption on the decline in kidney function was inconsistent.
Medications and Lifestyle Factors
Two studies in Central America identified non-steroidal anti-inflammatory drugs (NSAIDs) use as a risk factor for kidney disease among sugarcane workers (Table 4) (92, 99). One of these studies found that dehydration in combination with NSAIDs use was associated with higher odds of AKI (OR: 8.38, 95% CI: 1.67–42.16) (92). However, three other studies found that NSAIDs use was not significantly associated with kidney dysfunction among sugarcane workers (100, 107, 110). Overall, the evidence regarding the effect of NSAIDs on the development of kidney disease remains inconsistent.
Sociodemographic Factors
The sociodemographic factors that were identified as risk factors include gender and poor socioeconomic conditions. Jayasekara et al. (114) found a significant correlation between higher income and lower heat stress-dehydration symptom scores among agricultural workers in India, indicating that poor socioeconomic conditions can increase the risk of kidney disease. In addition, evidence from the study suggested an increased risk of kidney disease among females (28, 114).
Environmental Conditions
Hot Environmental Conditions.
Five studies identified hot environmental conditions as a risk factor for reduced kidney function. Three of these studies were conducted in Central America among sugarcane workers (Table 4) (107, 109, 112). One of these studies identified that an increase in the average WBGT by 1°C was associated with a 1.6% decline in cross-shift eGFR. In addition, two other studies were conducted in the U.S. focusing on the association between hot environmental conditions and cross-shift AKI among agricultural workers (28, 97). Mix et al. (97) found that each 5°F increase in mean heat index was associated with a 47% increase in the likelihood of AKI among migrant agricultural workers.
Agrochemical Exposure.
Evidence regarding the effect of agrochemical exposure on the development of kidney disease remains conflicting. Two studies conducted in Central America found a significant association between agrochemical exposure and the decline in eGFR (Table 4) (40, 109). Moreover, one study conducted in Mexico reported that farmworkers, who are more likely to be exposed to pesticides, experienced a greater decline in eGFR (β: −29.17; 95% CI: −37.26, −21.17) (Table 4) (108). In contrast, other studies conducted in Central America (105, 110) and nonendemic regions (90, 91) did not find a significant association between pesticide use and kidney disease (Table 4).
Vulnerable Populations
Migrant Farmworkers
Twenty-two studies focused specifically on migrant farmworkers in the U.S. (30, 40, 49–52, 55–58, 60, 78, 81, 82, 101, 104, 108, 115–118), Mexico (108), Ethiopia (65), and Australia (29). Three of these studies were focused on migrant Latino farmworkers, who have changed residence from one geographic location to another in search of agricultural work (49, 51, 60). According to the results of the reviewed studies, migrant farmworkers experience high levels of HRI symptoms with HRI prevalence ranging between 18 and 79% (30, 52, 55, 56, 58, 115). In addition, one study found that 33% of migrant agricultural workers in the U.S. experienced AKI (97). Only a few studies assessed the risk and protective factors associated with heat-related health outcomes among migrant farmworkers (30, 40, 50, 55, 97, 108). Three studies identified several risk factors to be unique to migrant agricultural workers, including lack of control over workplace conditions, poor work safety climate, and cultural and language barriers (29, 103, 104). Another risk factor, common for both migrant and non-migrant agricultural workers, was hot environmental conditions (97).
Child Farmworkers
Child farmworkers were the target population in 4 studies that examined the experiences, risk factors, and preventive measures associated with HRI (49–51, 60). These studies reported that child farmworkers faced a poor work safety climate and often lacked access to healthcare, sanitation facilities, and proper heat prevention measures (49–51, 60). HRI prevalence was high in this population with nearly half of the child farmworkers reporting at least one HRI symptom in the previous 12 months according to one study (51).
Identified Gender Differences in Health Outcomes and Associated Factors
Two studies used gender stratification to compare risk factors for kidney disease between males and females (28, 93). One of these studies found an association between kidney disease and (1) piece-rate work (OR: 102.81, 95% CI: 7.32–1443.20) and (2) years working in agriculture (OR: 1.12, 95% CI: 1.01–1.24) among female agricultural workers (28). Meanwhile, heat strain was associated with higher odds of AKI among males (OR: 1.31, 95% CI: 1.01–1.70). The second study found that picking or harvesting crops was a risk factor for kidney disease among males (OR: 4.12, 95% CI: 1.87–9.08) (93).
One of the reviewed studies compared HRI symptoms between male and female agricultural workers and identified several symptoms to be more prevalent among females than males, including headache, exhaustion, fainting, fatigue, and nausea or vomiting (62). Another study found that the prevalence of HRI symptoms among male and female sugarcane farmers was 30.4 and 59.5%, respectively (69).
Preventive Measures
The most common preventive measures identified in the included studies were maintain proper hydration, taking breaks in shaded areas, going to air-conditioned places during or after work, changing work hours and activities, and taking extra breaks (40, 50–52, 62, 63, 116). Water was found to be the most commonly consumed beverage in addition to sports drinks, energy drinks, soda, fruit juice, and coffee to maintain hydration (56, 61, 97, 116). Some studies also reported that the consumption of electrolyte solutions among agricultural workers reduced heat stress (98, 101). Several studies also reported the practice of wearing head protection such as baseball caps, hats, bandannas, and hoods from sweatshirts as a means of reducing heat stress (52, 55, 56, 63). In addition to head protection, wearing different types of clothing were used to protect against heat stress. These included wearing long-sleeved shirts, long pants, and light-colored or lightweight shirts (52, 55, 56, 62, 101, 116). Other commonly used preventive measures include acclimatization (52, 116), HRI training (63, 116, 117), wearing sunglasses and sunscreen (55, 63), and the use of rest stations or fans (56, 116). Preventative measures that were less common among the reviewed studies included eating a traditional diet (119) and bathing in cold water (53, 116).
Discussion
This is the first scoping review that aims to describe the health outcomes, risk factors, and preventative measures related to occupational heat stress among agricultural communities globally. The most common heat-related health effects identified in this review were HRI and kidney disease. The majority of the reviewed studies were conducted in Central and South America.
Factors Associated With HRI
Various risk factors associated with HRI were identified in the reviewed studies, including gender, workload, piece-rate payment, job decision latitude, cultural and language barriers, and hot environmental conditions. Although the evidence was limited, other risk factors that were found to have some form of association with HRI were reducing soda consumption and increasing access to regular breaks.
In addition, various work organization and management factors were associated with increased risk of HRI among agricultural populations, including workload and piece-rate payment. Several studies have shown that agricultural workers frequently perform strenuous physical activities under that payment method (97, 120). While piece-rate payment may incentive agricultural workers to work faster, it may also cause the workers to take fewer breaks to rest or to drink water (103, 120–122). However, some argue that adopting a piece-rate payment system can allow farmworkers to modify their work effort more easily during different heat exposure levels as compared to workers that are paid an hourly wage (123).
Another risk factor related to work organization and management was the lack of job decision latitude in agricultural workplaces. This results in a lack of control over certain HRI preventative measures such as shade availability and proximity to bathroom and water facilities (30, 116). This is likely due to the presence of a power imbalance between employers and agricultural workers, which prevents workers from making decisions about their health and safety or complaining about poor working conditions. In addition, migrant farmworkers often strive to keep their jobs at any cost, particularly since their legal status is tied to their employment (36).
A limited number of articles from the reviewed studies showed that various behavioral factors can be protective against HRI, such as taking breaks in the shade and increasing access to regular breaks. According to the Occupational Safety and Health Administration (OSHA) guidelines, workers should rest for 15 min each hour when WBGT exceeds 26°C, 30 minutes of rest each hour when WBGT reaches 28°C, and 45 min of rest each hour when WBGT reaches 30°C (124). However, the loss of working hours can reduce productivity and affect income and food security in agricultural workers and their families (125). On the other hand, studies have shown that improved access to rest breaks combined with an efficient intervention program can be effective in reducing heat-related health outcomes with minimal impacts on food production (59, 126).
In addition, a few studies suggested that reducing soda consumption can be protective for HRI among farmworkers. In fact, soda consumption is common among agricultural workers, who drink it to increase alertness and productivity (56, 61, 97, 103, 116). According to OSHA guidelines, workers should be encouraged to choose water over soda and other drinks containing caffeine and high sugar content since these products can increase the risk of dehydration (127).
Furthermore, several risk factors related to accessibility to heat prevention measures and treatment have been identified. One of these risk factors is cultural and language barriers that can affect the prevention and treatment of HRI among farmworkers. These language and cultural barriers prevent migrant farmworkers from understanding health and safety information (128–130) or accessing health care services (129).
Findings from the reviewed studies indicated that female agricultural workers were more likely to experience HRI as compared to their male counterparts. This may be due to lower water consumption, as females lack access to sanitation facilities when working in agricultural settings (131) and are less comfortable taking breaks to drink water (117). However, the research shows that agricultural tasks are often segregated by gender with the more strenuous tasks being performed by men, consequently increasing their risk of HRI (121).
However, the effect of other demographic variables such as age and migrant status were either inconclusive or limited. The reviewed articles show conflicting evidence concerning the association between age and HRI among adult farmworkers. Older farmworkers are more likely to be knowledgeable about HRI preventative measures and treatment due to greater experience (27). However, other sociodemographic factors, such as migrant status, were reported to be associated with HRI but were not identified as risk factors in the reviewed studies (30, 50, 52).
Another risk factor for HRI that was identified in the reviewed studies was hot environmental conditions. Therefore, occupational health agencies recommend various preventative measures that can be implemented to reduce heat exposure while working in hot conditions. OSHA has established four risk categories based on heat index values (127). OSHA recommends that preventative measures should be a function of the risk category.
Factors Associated With Kidney Disease
Various risk factors associated with HRI were identified in the reviewed studies, including gender, workload, piece-rate payment, and hot environmental conditions. Meanwhile, electrolyte consumption was identified as protective for kidney disease. Although the evidence was either limited or conflicting, other risk factors that were found to have some form of association with kidney disease included sugary beverage intake, fluid consumption, NSAIDs use, and poor socioeconomic conditions.
Various factors related to work organization and management have been identified as risk factors for kidney disease. Evidence from the studies identified in this review suggests that heavy workload is significantly associated with kidney diseases. In addition, the reviewed studies indicated that sugarcane cutters had a higher prevalence of reduced kidney function. Sugarcane cutters required unusually high physical exertion and fast repetitive movements with a machete (132, 133). In addition, the findings of this review suggest that piece-rate work is significantly associated with kidney diseases among agricultural workers. This payment method can cause agricultural workers to push themselves beyond their physical limits to earn as much as they can and to take fewer breaks to rest or drink water leading to a higher risk of heat stress and dehydration and consequently to the development of kidney disease.
Evidence from the reviewed studies indicates that several physiological factors including dehydration and heat strain are associated with kidney disease. Similarly, research shows that dehydration due to the loss of body water is well known to be associated with chronic kidney disease (134). In addition, heat strain resulting from heavy physical workload and hot environmental conditions can lead to kidney injury (99, 135).
An important behavioral factor that can affect the development of kidney diseases among agricultural workers was the adopted hydration practices. Evidence from the reviewed studies suggests that the intake of electrolyte solutions can be protective against kidney disease. According to the US National Institute for Occupational Safety and Health (NIOSH), electrolyte replacement should be provided to workers in the form of sports drinks containing balanced electrolytes if excessive sweating occurs for 4 or more hours in hot conditions (12). On the other hand, OSHA guidelines recommend water consumption but do not comment on electrolyte replacement (127). However, various studies reported that agricultural workers consumed low amounts of electrolyte solutions (92, 105).
Furthermore, our findings suggest that rehydration with sugary beverages may be a risk factor for kidney disease among agricultural workers, although the current studies remain inconclusive. The literature shows that sugary beverage intake has been reported as a risk factor for kidney disease in several experimental studies (136). Similarly, the effect of fluid consumption on the development of kidney disease has also been contradictory across the reviewed studies. In fact, the literature has reported that the fluid consumption of agricultural workers was often below the recommendations of occupational health agencies and consequently resulted in a greater risk of kidney disease (58, 69, 93, 111).
Evidence from the reviewed literature regarding the effect of NSAIDs use on kidney disease was found to be contradictory. However, the literature indicates that recurrent dehydration or volume depletion can be exacerbated by NSAIDs use (137, 138). In addition, a systematic review published in 2018 indicated that NSAIDs were found to be significantly associated with CKDu in Mesoamerica (139).
Various sociodemographic factors were also identified as risk factors for kidney disease in the current review. Findings from the reviewed studies suggest that female agricultural workers are at a greater risk of kidney disease as compared to their male counterparts. However, two systematic reviews identified in the literature showed a positive association between males and CKDu (139, 140). In addition, a limited number of studies indicated that low socioeconomic status is associated with an increased risk of kidney disease. This is consistent with the literature, which indicates that CKDu is mainly concentrated in poor agricultural communities characterized by heavy use of agrochemicals, hot and humid environments, and harsh working conditions at agricultural workplaces (141).
The majority of studies suggest that hot environmental conditions are significantly associated with kidney diseases, especially among sugarcane workers in Central America. This is consistent with the findings reported in the literature that indicate that occupational heat stress is a primary factor in the development of CKDu (43, 142, 143). In fact, various studies found that sugarcane workers in Central America are exposed to high levels of heat exposure (24, 109).
Another environmental factor related to kidney disease is agrochemical exposure. The majority of the reviewed studies suggest a lack of association between pesticides and kidney disease among agricultural populations. Similarly, a systematic review found no significant association between pesticides and CKDu in agricultural workers in Mesoamerica (139). Yet, another systematic review recommended that better exposure assessments are needed before ruling out pesticides as a cause of CKDu, since the past studies did not examine biomarkers of agrochemical exposure and instead relied only on self-reports of work practices and history (144).
Vulnerable Populations
The reviewed literature indicates that migrant agricultural workers are at particularly high risk for heat-related health outcomes, including HRI and kidney disease. Our results also showed that some of the risk and protective factors can be unique and distinct to the migrant agricultural workforce. Moreover, migrant agricultural workers face several barriers that prevent them from adhering to appropriate heat prevention measures or seeking proper treatment including lack of control over workplace conditions, poor work safety climate, and cultural and language barriers (29, 103, 104). In addition, various studies have reported that migrant farmworkers lack access to common heat preventative measures including prevention training, regular breaks, areas with shade, and drinking water (30, 52, 55, 116). Furthermore, few studies have assessed heat-related health effects among child farmworkers. However, child farmworkers face various physiological and behavioral differences that raise their vulnerability to heat stress as compared to their adult counterparts (145). Further research is still needed to determine the prevalence of heat-related health effects as well as to determine the risk and protective factors among these vulnerable workers so as to design more effective preventative measures tailored to these populations. In addition, there is a need for paying a greater attention to the impacts of the poor working conditions and the high poverty levels that face these farmworkers so as to better understand their vulnerabilities to heat-related health effects.
Gender Differences in Health Outcomes and Associated Factors
Piece-rate payment and years working in agriculture were identified as risk factors for kidney disease among females (28). Female agricultural workers, who are paid by piece, have an additional incentive to avoid visiting the bathroom during their work shift. Other reasons include the lack of adequate sanitation facilities in agricultural workplaces and the risk of sexual harassment or assault, which usually occurs around bathroom facilities. As a result, women limit their water consumption which leads to an increased risk of kidney disease (28). In addition, women working for longer durations in the agricultural sector experience frequent chronic delayed urination, which increases their risks of developing kidney diseases (28). Moreover, males are more likely to perform strenuous tasks such as picking or harvesting, which increases their risk of heat stress (28, 95).
However, the reviewed studies have not thoroughly investigated the differences in the prevalence of heat-related health effects and associated risk factors between male and female farmworkers. Since it is well established that men and women perform distinct agricultural tasks and have different occupational exposures even when given a similar job classification in studies (37, 117, 146), the use of a gender-sensitive approach in research is necessary to identify specific gender risk factors (147). Future studies should also compare the prevalence of heat-related health outcomes among male and female agricultural workers to gain a greater understanding of gender differences in vulnerability to heat stress.
Preventive Measures
Various heat preventive measures practiced by agricultural workers have been identified in the reviewed studies. The most common administrative preventive measures included drinking more water, taking breaks in shaded areas, going to air-conditioned places during or after work, changing work hours and activities, and taking extra breaks. In addition, a few studies showed that agricultural workers practice acclimatization by gradually increasing the number of work hours at the start of the season, which is an important protective measure for HRI. OSHA has recommended the “Water. Rest. Shade.” guidelines to reduce heat stress in hot working environments (148). Furthermore, a systematic review has also identified similar preventative measures practiced by outdoor workers (149).
In addition, several studies identified various sun safety behaviors commonly used by agricultural workers, including clothing practices such as wearing long-sleeved and light-colored shirts and long pants. Furthermore, several studies reported that agricultural workers also use sunscreen and sunglasses as well as head protection such as baseball caps, hats, bandannas, and hoods. NIOSH recommends that workers should wear breathable, light-colored, and loose-fitting clothing when working in hot environmental conditions (150), while OSHA encourages workers to use sunscreen and other protections from direct sunlight such as wearing hats (127).
On the other hand, several reviewed studies showed that agricultural workers lack access to adequate cooling measures such as shade, water, sanitation facilities, HRI training, and rest breaks (30, 55, 116). Furthermore, workplace culture can prevent the effective implementation of these preventive measures (29, 103).
Research Limitations, Literature Gaps, and Implications for Future Research
The findings of this review demonstrate that there is limited information on health outcomes related to occupational heat stress among agricultural workers globally. The US represents the country with the highest number of HRI studies. In addition, the majority of studies assessing the prevalence of kidney disease have been concentrated in Central America. However, various hot regions such as Sub-Saharan Africa, the Middle East and North Africa, and Southeast Asia host millions of vulnerable agricultural workers and thus the need for studies assessing the impacts of hot temperatures on health outcomes in these populations is imperative (151, 152). Therefore, more studies are required globally to quantify the burden of heat-related health effects, especially as working conditions and environmental heat exposure often vary from one country to another.
In addition, most studies examining the role of heat stress and dehydration on the development of kidney disease have been concentrated in Central America. Since the adverse impacts of heat stress on kidney function is expected to increase due to rising global temperatures, future studies should focus on other agricultural communities exposed to hot environmental conditions to gain a better understanding of the relationship between occupational heat stress and kidney health and its interaction with other possible etiologic factors. Furthermore, evidence regarding the effect of high temperatures on various health outcomes, such as occupational injuries and mental health, was found to be limited in the reviewed studies (153–155).
Limited evidence was found in the current review on the potential effects of various risk or protective factors such as acclimatization status, hydration practices, training, migrant status, and poor socioeconomic conditions on HRI and kidney disease prevalence. Therefore, future studies should investigate in more detail these factors. In addition, there is a need for qualitative studies that can provide a critical social lens for the analysis of heat-related health outcomes in the vulnerable farmworker populations. These can improve our understanding of the role that these factors have regarding HRI so that effective policies and programs can be developed. Another important limitation identified in the reviewed studies was the reliance on cross-sectional design to assess the association between potential risk factors and HRI. Various behavioral factors, which are protective for HRI, have been identified as risk factors. Therefore, longitudinal studies would be better equipped to assess workers' risk of occupational heat stress and can also address reverse causality.
Improved Methods of Exposure Assessment
Greater consistency in assessment tools used to examine heat-related health outcomes among farmers may be beneficial for future research. The identification of risk or protective factors associated with heat stress or kidney disease requires the design of consistent and comparative multisite studies in high-risk populations. Most studies assessing the prevalence of HRI relied mainly on self-reported HRI symptoms, using questionnaires that have not been validated. Comparison of HRI symptoms between studies is difficult due to different reporting periods, number of symptoms, and case definitions of HRI. Instead, heat exposure could be better assessed using validated questionnaires that can be modified and applied to local conditions, such as the HOTHAPS (The High Occupational Temperature, Health, and Productivity Suppression) questionnaire was used in some of the included studies (25, 62). In addition, objective measures of HRI are needed to provide more valid estimates of the prevalence of heat stress and dehydration among agricultural populations. These include measuring core body temperature through the use of an ingestible temperature pill (75, 78, 79, 95). Future research should also define objective measures of physical activity using accelerometers (156) or heart rate monitors (157) to measure the heat load generated by the performance of specific agricultural jobs.
Policies, Regulations, and Recommendations
In light of the existential and global threat of climate change, outdoor workers including agricultural workers are at the forefront of exposure to occupational heat stress (149, 158). It is critical that policymakers design labor protection and occupational health and safety policies to protect vulnerable agricultural communities from the effects of climate change, including heat stress (159). Furthermore, current and future heat protection standards and guidelines have to be developed in a manner that ensures that they are suitable for local environmental conditions and the physical requirements of the agricultural tasks involved. Thus, farm managers or supervisors ought to implement appropriate administrative and engineering measures such as the provision of water, shade, and rest breaks as well as provide better education and training instead of relying on the voluntary will of workers to implement heat preventative measures. Moreover, employers ought to develop and implement health surveillance programs that can detect early physiological responses of HRI among vulnerable workers (127, 160). In addition, implementing health surveillance can also provide evidence about the effectiveness of different preventive measures (160). Furthermore, it is necessary to work with various stakeholders throughout the global food supply chain to strengthen labor protections and ensure compliance with regulations. High-income countries could join effort with low- and middle-income countries to implement adaptation measures in the agricultural sector that protect the health and safety of farmworkers and ensure their food security (10, 150). Greater mechanization can be introduced in labor-intensive activities to reduce the level of physical activity required by workers thereby reducing heat stress (87). Furthermore, farming activities can be modified to reduce the risk of excessive exposure to heat by changing the timing of work activities or implementing best practices to reduce the time and work intensity needed (161). Other measures include monitoring of local weather conditions to plan agricultural activities accordingly (19).
However, commonly recommended administrative measures are sometimes ineffective in reducing the risk of heat stress among agricultural workers, especially as global temperatures continue to rise. Hence, various technological and engineering solutions should be developed to protect vulnerable agricultural communities from the effects of heat stress. Recent technological advancements have led to the rapid growth in the development of personal or microclimate cooling systems, such as personal cooling garments and cooling vests that can provide a convenient and flexible method to reduce heat stress and improve thermal comfort among working populations, including agricultural workers (87, 162–164). Other measures include various engineering controls including the use of mechanical aids to reduce the levels of physical activity (87, 165). However, these technical solutions may not be applicable in developing countries and marginalized communities due to their costs but could be easily implemented in developed countries. In addition, there is a need for field-based research to examine the effectiveness and practicality of these measures across different work settings and regions.
Strengths and Limitations of the Current Review
To the authors' current knowledge, this is the first scoping review that aims to describe the prevalence, risk factors, and preventative measures of occupational heat stress among agricultural populations. All health outcomes related to occupational heat stress among agricultural workers were assessed. A wide range of literature formed the basis for this review as both peer-reviewed studies and gray literature published in various languages were included with no restriction on publication date. This scoping review can provide an overview of current research in the field and can be used as a starting point to guide future research to assess heat-related health outcomes among farmworkers.
However, similar to other scoping reviews, a limitation to this current scoping review is the lack of quality assessment of the included studies. Furthermore, the comparability of risk factors and prevalence of heat-related health effects between various regions and agricultural populations were difficult to perform due to the use of different measurement instruments and different groups of farmworkers in most studies.
Conclusion
Given the projected increase in global temperatures and extreme heat events due to climate change, the adverse health impacts of occupational heat stress on agricultural communities are likely to increase in the future. This scoping review provides a comprehensive overview of heat-related health effects among agricultural populations as well as risk factors and preventative measures used to minimize heat stress exposure among farmworkers. Knowledge of risk factors and preventative measures is essential for reducing the burden of heat stress among agricultural workers. Thus, this scoping review is an important step toward synthesizing the knowledge base and highlighting areas for future research. The risk factors identified for both kidney disease and HRI include female gender, dehydration, heat strain, wearing inappropriate clothing, workload, piece-rate payment, job decision latitude, and hot environmental conditions. On the other hand, various protective factors were identified including drinking water, changing work hours and schedule of activities, reducing soda consumption, and increasing electrolyte consumption in addition to improving access to medical care. However, limited evidence was found regarding the effect of various factors such as acclimatization status, hydration practices, training, migrant status, and poor socioeconomic conditions on the prevalence of both HRI and kidney disease. The current review also identified various factors that are unique to vulnerable populations working in the agricultural sector, including migrant and child farmworkers. In addition, this review found that the current knowledge is largely based on findings from countries in North and Central America. Large gaps remain with regards to quantifying the burden of heat-related health outcomes among agricultural workers in hot regions such as Sub-Saharan Africa, the Middle East and North Africa, and Southeast Asia. These areas host millions of heat stress vulnerable agricultural workers that are understudied. Therefore, more studies are required globally to quantify the burden of heat stress and to identify understudied risk and protective factors among vulnerable agricultural communities in different geographical regions.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
RH and ME: conceptualization. LH: database search strategy. ME, DH, and RH: literature review, screening articles and drafting early drafts and the manuscript. ME, RH, DH, IA, and MH: revising the final draft of the manuscript. All authors approved the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.782811/full#supplementary-material
References
- 1.IPCC . AR6 Climate Change 2021: The Physical Science Basis. Available from: https://www.ipcc.ch/report/ar6/wg1/ [DOI] [PMC free article] [PubMed]
- 2.Perkins SE. A review on the scientific understanding of heatwaves—Their measurement, driving mechanisms, and changes at the global scale. Atmos Res. (2015). 164:242–67. 10.1016/j.atmosres.2015.05.01421690131 [DOI] [Google Scholar]
- 3.NASA. Global Temperature. (2021). Available from: https://climate.nasa.gov/vital-signs/global-temperature/#:~:text=The%20year%202020%20tied%20with,National%20Oceanic%20and%20Atmospheric%20Administration
- 4.Perkins-Kirkpatrick SE, Lewis SC. Increasing trends in regional heatwaves. Nat Commun. (2020) 11:3357. 10.1038/s41467-020-16970-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.IPCC . Global warming of 1.5°C. Available from: https://www.ipcc.ch/site/assets/uploads/sites/2/2019/05/SR15_SPM_version_report_LR.pdf
- 6.IPCC . Special Report on Climate Change and Land. Available from: https://www.ipcc.ch/site/assets/uploads/2019/11/SRCCL-Full-Report-Compiled-191128.pdf
- 7.Li D, Yuan J, Kopp RE. Escalating global exposure to compound heat-humidity extremes with warming. Environ Res Lett. (2020) 15:064003. 10.1088/1748-9326/ab7d04 [DOI] [Google Scholar]
- 8.Green H, Bailey J, Schwarz L, Vanos J, Ebi K, Benmarhnia T. Impact of heat on mortality and morbidity in low and middle income countries: A review of the epidemiological evidence and considerations for future research. Environ Res. (2019) 171:80–91. 10.1016/j.envres.2019.01.010 [DOI] [PubMed] [Google Scholar]
- 9.Song X, Wang S, Hu Y, Yue M, Zhang T, Liu Y, et al. Impact of ambient temperature on morbidity and mortality: an overview of reviews. Sci Total Environ. (2017) 586:241–254. 10.1016/j.scitotenv.2017.01.212 [DOI] [PubMed] [Google Scholar]
- 10.Amegah AK, Rezza G, Jaakkola JJ. Temperature-related morbidity and mortality in Sub-Saharan Africa: a systematic review of the empirical evidence. Environ Int. (2016) 91:133–49. 10.1016/j.envint.2016.02.027 [DOI] [PubMed] [Google Scholar]
- 11.Atwoli L, Baqui AH, Benfield T, Bosurgi R, Godlee F, Hancocks S, et al. Call for emergency action to limit global temperature increases, restore biodiversity, and protect health. BMJ. (2021) 374:n1734. 10.1136/bmj.n1734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.NIOSH . Criteria for a Recommended Standard Occupational Exposure to Heat and Hot Environments. Available from: https://www.cdc.gov/niosh/docs/2016-106/pdfs/2016-106.pdf?id=10.26616/NIOSHPUB2016106
- 13.ACGIH . TLVs and BEIs: Based on the Documentation of the Threshold Limit Values for Chemical Substances and Physical Agents & Biological Exposure Indices. Cincinnati. Available from: http://dl.mozh.org/up/acgih-2015.pdf
- 14.Parsons K. Human Thermal Environments: The Effects of Hot, Moderate, and Cold Environments on Human Health, Comfort, and Performance, Third Edition. (2014). p. 1–586. 10.1201/b16750 [DOI] [Google Scholar]
- 15.Holmér I. Protective clothing in hot environments. Ind Health. (2006) 44:404–13. 10.2486/indhealth.44.404 [DOI] [PubMed] [Google Scholar]
- 16.Xiang J, Bi P, Pisaniello D, Hansen A. Health impacts of workplace heat exposure: an epidemiological review. Ind Health. (2014) 52:91–101. 10.2486/indhealth.2012-0145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Flouris AD, Dinas PC, Ioannou LG, Nybo L, Havenith G, Kenny GP, et al. Workers' health and productivity under occupational heat strain: a systematic review and meta-analysis. Lancet Planet Health. (2018) 2:e521–31. 10.1016/S2542-5196(18)30237-7 [DOI] [PubMed] [Google Scholar]
- 18.Kjellstrom T, Lemke B, Otto M, Hyatt O, Dear K. Occupational Heat Stress: Contribution to WHO Project on “Global Assessment of the Health Impacts of Climate Change”, Which Started in 2009. Available from: http://climatechip.org/sites/default/files/publications/TP2014_4_Occupational_Heat_Stress_WHO.pdf
- 19.ILO . Working on a Warmer Planet: The Impact of Heat Stress on Labour Productivity and Decent Work. Available from: https://www.ilo.org/wcmsp5/groups/public/—dgreports/—dcomm/—publ/documents/publication/wcms_711919.pdf
- 20.Tigchelaar M, Battisti DS, Spector JT. Work Adaptations Insufficient to Address Growing Heat Risk for U.S. Agricultural Workers. Environ Res Lett. (2020) 15:094035. 10.1088/1748-9326/ab86f4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Petropoulos ZE, Ramirez-Rubio O, Scammell MK, Laws RL, Lopez-Pilarte D, Amador JJ, et al. Brooks, climate trends at a hotspot of chronic kidney disease of unknown causes in Nicaragua, 1973–2014. Int J Environ Res Public Health. (2021) 18:5418 10.3390/ijerph18105418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gubernot DM, Anderson GB, Hunting KL. Characterizing occupational heat-related mortality in the United States. 2000–2010: an analysis using the Census of Fatal Occupational Injuries database. Am J Ind Med. (2015) 58:203–11. 10.1002/ajim.22381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frimpong K, Van Etten EJE, Oosthuzien J, Fannam Nunfam V. Heat exposure on farmers in northeast Ghana. Int J Biometeorol. (2017) 61:397–406. 10.1007/s00484-016-1219-7 [DOI] [PubMed] [Google Scholar]
- 24.Crowe J, Wesseling C, Solano BR, Umaña MP, Ramírez AR, Kjellstrom T, et al. Heat exposure in sugarcane harvesters in Costa Rica. Am J Ind Med. (2013) 56:1157–64. 10.1002/ajim.22204 [DOI] [PubMed] [Google Scholar]
- 25.Sahu S, Sett M, Kjellstrom T. Heat exposure, cardiovascular stress and work productivity in rice harvesters in India: implications for a climate change future. Ind Health. (2013) 51:424–31. 10.2486/indhealth.2013-0006 [DOI] [PubMed] [Google Scholar]
- 26.Staal Wästerlund D. Managing Heat in Agricultural Work: Increasing Worker Safety and Productivity by Controlling Heat Exposure. Available from: http://www.fao.org/3/i9179en/I9179EN.pdf
- 27.Spector JT, Krenz J, Blank KN. Risk factors for heat-related illness in Washington crop workers. J Agromed. (2015) 20:349–59. 10.1080/1059924X.2015.1047107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moyce S, Mitchell D, Armitage T, Tancredi D, Joseph J, Schenker M. Heat strain, volume depletion and kidney function in California agricultural workers. Occup Environ Med. (2017) 74:402–9. 10.1136/oemed-2016-103848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hansen AL, Williams S, Hanson-Easey S, Varghese BM, Bi P, Heyworth J, et al. Using a qualitative phenomenological approach to inform the etiology and prevention of occupational heat-related injuries in Australia. Int J Environ Res Public Health. (2020) 17:846. 10.3390/ijerph17030846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fleischer NL, Tiesman HM, Sumitani J, Mize T, Amarnath KK, Bayakly AR, et al. Public health impact of heat-related illness among migrant farmworkers. Am J Prev Med. (2013) 44:199–206. 10.1016/j.amepre.2012.10.020 [DOI] [PubMed] [Google Scholar]
- 31.Habib RR, Mikati D, Hojeij S, El Asmar K, Chaaya M, Zurayk R. Associations between poor living conditions and multi-morbidity among Syrian migrant agricultural workers in Lebanon. Eur J Public Health. (2016) 26:1039–44. 10.1093/eurpub/ckw096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Öztaş D, Koc A, Akbaba M. Living conditions, access to healthcare services, and occupational health and safety conditions of migrant seasonal agricultural workers in the Çukurova Region. J Agromed. (2018) 23:262–9. 10.1080/1059924X.2018.1470048 [DOI] [PubMed] [Google Scholar]
- 33.Castañeda A, Doan D, Newhouse D, Nguyen MC, Uematsu H, Azevedo JP. A new profile of the global poor. World Develop. (2018) 101:250–67. 10.1016/j.worlddev.2017.08.002 [DOI] [Google Scholar]
- 34.ILO . ILO Global Estimates on Migrant Workers: Results and Methodology. Available from: https://www.refworld.org/pdfid/586f55584.pdf
- 35.FAO . Migration, Agriculture and Climate Change: Reducing Vulnerabilities and Enhancing Resilience. Available from: http://www.fao.org/3/i8297en/I8297EN.pdf
- 36.Caxaj CS, Cohen A. “I Will Not Leave My Body Here”: Migrant Farmworkers' Health and Safety Amidst a Climate of Coercion. Int J Environ Res Public Health. (2019) 16:2643. 10.3390/ijerph16152643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Habib RR, Ziadee M, Abi Younes E, Harastani H. Syrian refugee child workers: Gender differences in ergonomic exposures and musculoskeletal health. Appl Ergon. (2020) 83:102983. 10.1016/j.apergo.2019.102983 [DOI] [PubMed] [Google Scholar]
- 38.Hiott AE, Grzywacz JG, Davis SW, Quandt SA, Arcury TA. Migrant farmworker stress: mental health implications. J Rural Health. (2008) 24:32–9. 10.1111/j.1748-0361.2008.00134.x [DOI] [PubMed] [Google Scholar]
- 39.Svensson M, Urinboyev R, Svensson A, Lundqvist P, Littorin M, Albin M. Migrant agricultural workers and their socio-economic, occupational and health conditions—a literature review. SSRN Working Papers Ser. (2013). 10.2139/ssrn.2297559 [DOI] [Google Scholar]
- 40.Mirabelli MC, Quandt SA, Crain R, Grzywacz JG, Robinson EN, Vallejos QM, et al. Symptoms of heat illness among Latino farm workers in North Carolina. Am J Prev Med. (2010) 39:468–71. 10.1016/j.amepre.2010.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sadiq LS, Hashim Z, Osman M. The Impact of Heat on Health and Productivity among Maize Farmers in a Tropical Climate Area. J Environ Public Health. (2019) 2019:9896410. 10.1155/2019/9896410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sen J, Nag PK. Human susceptibility to outdoor hot environment. Sci Total Environ. (2019) 649:866–75. 10.1016/j.scitotenv.2018.08.325 [DOI] [PubMed] [Google Scholar]
- 43.Wesseling C, Glaser J, Rodríguez-Guzmán J, Weiss I, Lucas R, Peraza S, et al. Chronic kidney disease of non-traditional origin in Mesoamerica: a disease primarily driven by occupational heat stress. Rev Panam Salud Publica. (2020) 44:e15. 10.26633/RPSP.2020.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Venugopal V, Rojas-Valverde D, Robles A, Arias E, Glaser J, Dally M. Report From the Third International Workshop on Chronic Kidney Diseases of Uncertain/Non-Traditional Etiology in Mesoamerica and Other Regions. Available from: https://www.niehs.nih.gov/news/assets/docs_a_e/ckdu_report_508.pdf
- 45.Smith DJ, Pius LM, Plantinga LC, Thompson LM, Mac V, Hertzberg VS. Heat stress and kidney function in farmworkers in the US: a scoping review. J Agromed. (2021) 31:1–10. 10.1080/1059924X.2021.1893883 [DOI] [PubMed] [Google Scholar]
- 46.Riccò M. Air temperature exposure and agricultural occupational injuries in the Autonomous Province of Trento (2000-2013, North-Eastern Italy). Int J Occup Med Environ Health. (2018) 31:317–31. 10.13075/ijomeh.1896.01114 [DOI] [PubMed] [Google Scholar]
- 47.Spector JT, Bonauto DK, Sheppard L, Busch-Isaksen T, Calkins M, Adams D, et al. A case-crossover study of heat exposure and injury risk in outdoor agricultural workers. PLoS ONE. (2016) 11:e0164498. 10.1371/journal.pone.0164498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 49.Arcury TA, Arnold TJ, Quandt SA, Chen H, Kearney GD, Sandberg JC, et al. Health and occupational injury experienced by Latinx child farmworkers in North Carolina, USA. Int J Environ Res Public Health. (2019) 17:248. 10.3390/ijerph17010248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Arcury TA, Summers P, Talton JW, Chen H, Sandberg JC, Spears Johnson CR, et al. Heat illness among North Carolina Latino farmworkers. J Occup Environ Med. (2015). 57:1299–304. 10.1097/JOM.0000000000000552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Arnold TJ, Arcury TA, Sandberg JC, Quandt SA, Talton JW, Mora DC, et al. Heat-related illness among Latinx child farmworkers in North Carolina: a mixed-methods study. New Solut. (2020) 30:111–26. 10.1177/1048291120920571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bethel JW, Harger R. Heat-related illness among Oregon farmworkers. Int J Environ Res Public Health. (2014) 11:9273–85. 10.3390/ijerph110909273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Budhathoki NK, Zander KK. Socio-economic impact of and adaptation to extreme heat and cold of farmers in the food bowl of Nepal. Int J Environ Res Public Health. (2019) 16:1578. 10.3390/ijerph16091578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Crowe J, Nilsson M, Kjellstrom T, Wesseling C. Heat-related symptoms in sugarcane harvesters. Am J Ind Med. (2015) 58:541–8. 10.1002/ajim.22450 [DOI] [PubMed] [Google Scholar]
- 55.Kearney GD, Hu H, Xu X, Hall MB, Balanay JA. Estimating the prevalence of heat-related symptoms and sun safety-related behavior among Latino farmworkers in Eastern North Carolina. J Agromed. (2016) 21:15–23. 10.1080/1059924X.2015.1106377 [DOI] [PubMed] [Google Scholar]
- 56.Luque JS, Becker A, Bossak BH, Grzywacz JG, Tovar-Aguilar JA, Guo Y. Knowledge and practices to avoid heat-related illness among hispanic farmworkers along the Florida-Georgia line. J Agromed. (2020) 25:190–200. 10.1080/1059924X.2019.1670312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mutic AD, Mix JM, Elon L, Mutic NJ, Economos J, Flocks J, et al. Classification of Heat-related illness symptoms among Florida farmworkers. J Nurs Scholarsh. (2018) 50:74–82. 10.1111/jnu.12355 [DOI] [PubMed] [Google Scholar]
- 58.Smith DJ, Ferranti EP, Hertzberg VS, Mac V. Knowledge of heat-related illness first aid and self-reported hydration and heat-related illness symptoms in migrant farmworkers. Workplace Health Saf. (2021) 69:15–21. 10.1177/2165079920934478 [DOI] [PubMed] [Google Scholar]
- 59.Bodin T, García-Trabanino R, Weiss I, Jarquín E, Glaser J, Jakobsson K, et al. Intervention to reduce heat stress and improve efficiency among sugarcane workers in El Salvador: Phase 1. Occup Environ Med. (2016) 73:409–16. 10.1136/oemed-2016-103555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Arcury TA, Quandt SA, Arnold TJ, Chen H, Daniel SS. Occupational Injuries of Latinx Child Farmworkers in North Carolina: associations with work safety culture. J Occup Environ Med. (2020) 62:853–8. 10.1097/JOM.0000000000001982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Culp K, Tonelli S. Heat-related illness in midwestern hispanic farmworkers: a descriptive analysis of hydration status and reported symptoms. Workplace Health Saf. (2019) 67:168–78. 10.1177/2165079918813380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pogacar T, Crepinšek Z, Bogataj L, Nybo L. Comprehension of climatic and occupational heat stress amongst agricultural advisers and workers in Slovenia. Acta Agriculturae Slovenica. (2017) 109:545–54. 10.14720/aas.2017.109.3.06 [DOI] [Google Scholar]
- 63.Riccò M, Vezzosi L, Bragazzi NL, Balzarini F. Heat-related illnesses among pesticide applicators in North-Eastern Italy (2017). J Agromed. (2020) 25:52–64. 10.1080/1059924X.2019.1606745 [DOI] [PubMed] [Google Scholar]
- 64.Frimpong K, Oosthuizen JD, Van Etten EJ. Experiences of heat stress vulnerability and climate change among farmers in Ghana. J Environ Earth Sci. (2014) 4:100–110. [Google Scholar]
- 65.Alemu Gelaye K, Debalke G, Awoke Ayele T, Fekadu Wolde H, Sisay MM, Teshome DF, et al. Occupational health problems among seasonal and migrant farmworkers in Ethiopia: a cross-sectional study. Risk Manage Healthcare Policy. (2021) 14:4447–56. 10.2147/RMHP.S323503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Silpasuwan P, Sujirarat D, Kongtip P, Inbamrung S, Woskie S. Hazard exposure with health and safety outcomes hinder the work ability of salt farm workers in Thailand. Sumer J Med Healthc. (2019) 2:125–33. [PMC free article] [PubMed] [Google Scholar]
- 67.How V, Singh S, Dang T, Guo HR. Factors associated with health-risk perception of heat waves among agroecological and conventional farmers in the tropics. Int J Clim Change Impacts Resp. (2021) 14:45–60. 10.18848/1835-7156/CGP/v14i01/45-60 [DOI] [Google Scholar]
- 68.Venugopal V, Latha PK, Shanmugam R, Krishnamoorthy M, Omprashanth R, Lennqvist R, et al. Epidemiological evidence from south Indian working population-the heat exposures and health linkage. J Expo Sci Environ Epidemiol. (2021) 31:177–86. 10.1038/s41370-020-00261-w [DOI] [PubMed] [Google Scholar]
- 69.Kiatkitroj K, Arphorn S, Tangtong C, Maruo SJ, Ishimaru T. Risk factors associated with heat-related illness among sugarcane farmers in Thailand. Ind Health. (2021). 10.2486/indhealth.2021-0161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lumingu HMM, Dessureault P. Physiological responses to heat strain: a study on personal monitoring for young workers. J Therm Biol. (2009). 34:299–305. 10.1016/j.jtherbio.2009.04.001 [DOI] [Google Scholar]
- 71.Wagoner RS, López-Gálvez NI, de Zapien JG, Griffin SC, Canales RA, Beamer PI. An occupational heat stress and hydration assessment of agricultural workers in North Mexico. Int J Environ Res Public Health. (2020) 17:2102. 10.3390/ijerph17062102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gun RT, Budd GM. Effects of thermal, personal and behavioural factors on the physiological strain, thermal comfort and productivity of Australian shearers in hot weather. Ergonomics. (1995) 38:1368–84. 10.1080/00140139508925195 [DOI] [PubMed] [Google Scholar]
- 73.Biggs C, Paterson M, Maunder E. Hydration status of South African forestry workers harvesting trees in autumn and winter. Ann Occup Hyg. (2011) 55:6–15. 10.1093/annhyg/meq068 [DOI] [PubMed] [Google Scholar]
- 74.Mac VVT, Tovar-Aguilar JA, Elon L, Hertzberg V, Economos R, McCauley LA. Elevated core temperature in Florida fernery workers: results of a pilot study. Workplace Health Saf. (2019). 67:470–80. 10.1177/2165079919849466 [DOI] [PubMed] [Google Scholar]
- 75.Vega-Arroyo AJ, Mitchell DC, Castro JR, Armitage TL, Tancredi DJ, Bennett DH, et al. Impacts of weather, work rate, hydration, and clothing in heat-related illness in California farmworkers. Am J Ind Med. (2019) 62:1038–46. 10.1002/ajim.22973 [DOI] [PubMed] [Google Scholar]
- 76.Das B, Ghosh T, Gangopadhyay S. Prevalence of musculoskeletal disorders and occupational health problems among groundnut farmers of West Bengal, India. J Hum Ergol (Tokyo). (2013) 42:1–12. 10.11183/jhe.42.14 [DOI] [PubMed] [Google Scholar]
- 77.Das B, Ghosh T, Gangopadhyay S. Child work in agriculture in West Bengal, India: assessment of musculoskeletal disorders and occupational health problems. J Occup Health. (2013) 55:244–58. 10.1539/joh.12-0185-OA [DOI] [PubMed] [Google Scholar]
- 78.Mitchell DC, Castro J, Armitage TL, Vega-Arroyo AJ, Moyce SC, Tancredi DJ, et al. Recruitment, methods, and descriptive results of a physiologic assessment of Latino farmworkers: the California Heat Illness Prevention Study. J Occup Environ Med. (2017) 59:649–58. 10.1097/JOM.0000000000000988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Mac VVT. Characterizing Heat-Related Illness in Florida Farmworkers: A Feasibility Study (2016).28118110 [Google Scholar]
- 80.Lundgren K, Kuklane K, Venugopal V. Occupational heat stress and associated productivity loss estimation using the PHS model (ISO 7933): a case study from workplaces in Chennai, India. Glob Health Action. (2014) 7:25283. 10.3402/gha.v7.25283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Stoklosa H, Kunzler N, Ma ZB, Luna JCJ, de Vedia GM, Erickson TB. Pesticide exposure and heat exhaustion in a migrant agricultural worker: a case of labor trafficking. Ann Emerg Med. (2020) 76:215–8. 10.1016/j.annemergmed.2020.03.007 [DOI] [PubMed] [Google Scholar]
- 82.CDC . Heat related Deaths among Crop Workers—United States, 1992-2006 (2008). [PubMed] [Google Scholar]
- 83.Miller CW. Heat exhaustion in tractor drivers. Occup Health. (1982) 34:361–5. [PubMed] [Google Scholar]
- 84.Mohammadian M, Heidari H, Charkhloo E, Dehghani A. Heat stress and physiological and perceptual strains of date harvesting workers in palm groves in Jiroft. Work. (2020) 66:625–36. 10.3233/WOR-203205 [DOI] [PubMed] [Google Scholar]
- 85.Grimbuhler S, Viel JF. Heat stress and cardiac strain in French vineyard workers. Ann Work Expo Health. (2021) 65:390–6. 10.1093/annweh/wxaa115 [DOI] [PubMed] [Google Scholar]
- 86.Sandsund M, Wiggen Ø, Holmen IM, Thorvaldsen T. Work strain and thermophysiological responses in Norwegian fish farming—a field study. Ind Health. (2021). 10.2486/indhealth.2020-0259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ioannou LG, Mantzios K, Tsoutsoubi L, Nintou E, Vliora M, Gkiata P, et al. Occupational heat stress: multi-country observations and interventions. Int J Environ Res Public Health. (2021) 18:6303. 10.3390/ijerph18126303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hamerezaee M, Dehghan SF, Golbabaei F, Fathi A, Zamanian Z. Comparison of different heat stress indices for assessing farmers' exposure to heat stress. Iran J Publ Health. (2020) 49:1810−2. 10.18502/ijph.v49i9.4107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Raju DSSK, Kiranmayi P, Vijaya Rachel K. Climate change and chronic kidney disease. Asian J Pharm Clin Res. (2014) 7:53–7. Available online at: https://innovareacademics.in/journals/index.php/ajpcr/article/view/95332005319 [Google Scholar]
- 90.Fitria L, Prihartono NA, Ramdhan DH, Wahyono TYM, Kongtip P, Woskie S. Environmental and occupational risk factors associated with chronic kidney disease of unknown etiology in West Javanese rice farmers, Indonesia. Int J Environ Res Public Health. (2020) 17:4521. 10.3390/ijerph17124521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ekiti ME, Zambo JB, Assah FK, Agbor VN, Kekay K, Ashuntantang G. Chronic kidney disease in sugarcane workers in Cameroon: a cross-sectional study. BMC Nephrol. (2018) 19:10. 10.1186/s12882-017-0798-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Butler-Dawson J, Krisher L, Yoder H, Dally M, Sorensen C, Johnson RJ, et al. Evaluation of heat stress and cumulative incidence of acute kidney injury in sugarcane workers in Guatemala. Int Arch Occup Environ Health. (2019) 92:977–90. 10.1007/s00420-019-01426-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Moyce S, Mitchell D, Vega A, Schenker M. Hydration choices, sugary beverages, and kidney injury in agricultural workers in California. J Nurs Scholarsh. (2020) 52:369–78. 10.1111/jnu.12561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Moyce S, Joseph J, Tancredi D, Mitchell D, Schenker M. Cumulative incidence of acute kidney injury in California's agricultural workers. J Occup Environ Med. (2016) 58:391–7. 10.1097/JOM.0000000000000668 [DOI] [PubMed] [Google Scholar]
- 95.Moyce S, Armitage T, Mitchell D, Schenker M. Acute kidney injury and workload in a sample of California agricultural workers. Am J Ind Med. (2020) 63:258–68. 10.1002/ajim.23076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kupferman J, Ramírez-Rubio O, Amador JJ, López-Pilarte D, Wilker EH, Laws RL, et al. Acute kidney injury in sugarcane workers at risk for Mesoamerican nephropathy. Am J Kidney Dis. (2018) 72:475–82. 10.1053/j.ajkd.2018.04.014 [DOI] [PubMed] [Google Scholar]
- 97.Mix J, Elon L, Vi Thien Mac V, Flocks J, Economos E, Tovar-Aguilar AJ, et al. Hydration status, kidney function, and kidney injury in Florida agricultural workers. J Occup Environ Med. (2018) 60:e253–60. 10.1097/JOM.0000000000001261 [DOI] [PubMed] [Google Scholar]
- 98.Glaser J, Hansson E, Weiss I, Wesseling C, Jakobsson K, Ekström U, et al. Preventing kidney injury among sugarcane workers: promising evidence from enhanced workplace interventions. Occup Environ Med. (2020) 77:527–34. 10.1136/oemed-2020-106406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hansson E, Glaser J, Jakobsson K, Weiss I, Wesseling C, Lucas RAI, et al. Pathophysiological mechanisms by which heat stress potentially induces kidney inflammation and chronic kidney disease in sugarcane workers. Nutrients. (2020) 12:1639. 10.3390/nu12061639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hansson E, Glaser J, Weiss I, Ekström U, Apelqvist J, Hogstedt C, et al. Workload and cross-harvest kidney injury in a Nicaraguan sugarcane worker cohort. Occup Environ Med. (2019) 76:818–26. 10.1136/oemed-2019-105986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Luque JS, Bossak BH, Davila CB, JA Tovar-Aguilar JA. “I Think the Temperature was 110 Degrees!”: work safety discussions among hispanic farmworkers. J Agromed. (2019) 24:15–25. 10.1080/1059924X.2018.1536572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Crowe J, van Wendel de Joode B, Wesseling C. A pilot field evaluation on heat stress in sugarcane workers in Costa Rica: what to do next? Glob Health Action. (2009) 2. 10.3402/gha.v2i0.2062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lam M, Krenz J, Palmández P, Negrete M, Perla M, Murphy-Robinson H, Spector JT. Identification of barriers to the prevention and treatment of heat-related illness in Latino farmworkers using activity-oriented, participatory rural appraisal focus group methods. BMC Public Health. (2013) 13:1004. 10.1186/1471-2458-13-1004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wilmsen C, de Castro AB, Bush D, Harrington MJ. System failure: work organization and injury outcomes among Latino forest workers. J Agromed. (2019) 24:186–96. 10.1080/1059924X.2019.1567421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Laws RL, Brooks DR, Amador JJ, Weiner DE, Kaufman JS, Ramírez-Rubio O, et al. Biomarkers of kidney injury among Nicaraguan sugarcane workers. Am J Kidney Dis. (2016) 67:209–17. 10.1053/j.ajkd.2015.08.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Laws RL, Brooks DR, Amador JJ, Weiner DE, Kaufman JS, Ramírez-Rubio O, et al. Changes in kidney function among Nicaraguan sugarcane workers. Int J Occup Environ Health. (2015) 21:241–50. 10.1179/2049396714Y.0000000102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Sorensen CJ, Butler-Dawson J, Dally M, Krisher L, Griffin BR, Johnson RJ, et al. Risk factors and mechanisms underlying cross-shift decline in kidney function in Guatemalan sugarcane workers. J Occup Environ Med. (2019) 61:239–50. 10.1097/JOM.0000000000001529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.López-Gálvez N, Wagoner R, Canales RA, Ernst K, Burgess JL, de Zapien J, et al. Longitudinal assessment of kidney function in migrant farm workers. Environ Res. (2021) 202:111686. 10.1016/j.envres.2021.111686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.García-Trabanino R, Jarquín E, Wesseling C, Johnson RJ, González-Quiroz M, Weiss I, et al. Heat stress, dehydration, and kidney function in sugarcane cutters in El Salvador—a cross-shift study of workers at risk of Mesoamerican nephropathy. Environ Res. (2015) 142:746–55. 10.1016/j.envres.2015.07.007 [DOI] [PubMed] [Google Scholar]
- 110.Wesseling C, Aragón A, González M, Weiss I, Glaser J, Rivard CJ, et al. Heat stress, hydration and uric acid: a cross-sectional study in workers of three occupations in a hotspot of Mesoamerican nephropathy in Nicaragua. BMJ Open. (2016) 6:e011034. 10.1136/bmjopen-2016-011034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Pundee R, Kongtip P, Nankongnab N, Anutrakulchai S, Robson MG, Woskie S. Cross-shift change of acute kidney injury biomarkers in sugarcane farmers and cutters. Hum Ecol Risk Assess. (2021) 27:1170–87. 10.1080/10807039.2020.1812049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Raines N, González M, Wyatt C, Kurzrok M, Pool C, Lemma T, et al. Risk factors for reduced glomerular filtration rate in a Nicaraguan community affected by Mesoamerican nephropathy. MEDICC Rev. (2014) 16:16–22. 10.37757/MR2014.V16.N2.4 [DOI] [PubMed] [Google Scholar]
- 113.Butler-Dawson J, Krisher L, Asensio C, Cruz A, Tenney L, Weitzenkamp D, et al. Risk factors for declines in kidney function in sugarcane workers in Guatemala. J Occup Environ Med. (2018) 60:548–58. 10.1097/JOM.0000000000001284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Jayasekara KB, Kulasooriya PN, Wijayasiri KN, Rajapakse ED, Dulshika DS, Bandara P, et al. Relevance of heat stress and dehydration to chronic kidney disease (CKDu) in Sri Lanka. Prev Med Rep. (2019) 15:100928. 10.1016/j.pmedr.2019.100928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Culp K, Tonelli S, Ramey SL, Donham K, Fuortes L. Preventing heat-related illness among Hispanic farmworkers. Aaohn J. (2011) 59:23–32. 10.1177/216507991105900104 [DOI] [PubMed] [Google Scholar]
- 116.Bethel JW, Spector JT, Krenz J. Hydration and cooling practices among farmworkers in Oregon and Washington. J Agromed. (2017) 22:222–8. 10.1080/1059924X.2017.1318100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Stoecklin-Marois M, Hennessy-Burt T, Mitchell D, Schenker M. Heat-related illness knowledge and practices among California hired farm workers in The MICASA Study. Ind Health. (2013) 51:47–55. 10.2486/indhealth.2012-0128 [DOI] [PubMed] [Google Scholar]
- 118.Flocks J, Vi Thien Mac V, Runkle J, Tovar-Aguilar JA, Economos J, McCauley LA. Female farmworkers' perceptions of heat-related illness and pregnancy health. J Agromed. (2013) 18:350–58. 10.1080/1059924X.2013.826607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Frimpong K, Odonkor S, Kuranchie F, Nunfam V. Evaluation of heat stress impacts and adaptations: perspectives from smallholder rural farmers in Bawku East of Northern Ghana. Heliyon. (2020) 6:e03679. 10.1016/j.heliyon.2020.e03679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Toupin D, LeBel L, Dubeau D, Imbeau D, Bouthillier L. Measuring the productivity and physical workload of brushcutters within the context of a production-based pay system. Forest Policy Econ. (2007) 9:1046–55. 10.1016/j.forpol.2006.10.001 [DOI] [Google Scholar]
- 121.Mitchell DC, Castro J, Armitage TL, Tancredi DJ, Bennett DH, Schenker MB. Physical activity and common tasks of California farm workers: California Heat Illness Prevention Study (CHIPS). J Occup Environ Hyg. (2018) 15:857–69. 10.1080/15459624.2018.1519319 [DOI] [PubMed] [Google Scholar]
- 122.Quandt SA, Arnold TJ, Mora DC, Sandberg JC, Daniel SS, Arcury TA. Hired Latinx child farm labor in North Carolina: the demand-support-control model applied to a vulnerable worker population. Am J Ind Med. (2019) 62:1079–90. 10.1002/ajim.23039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Pan Q, Sumner DA, Mitchell DC, Schenker M. Compensation incentives and heat exposure affect farm worker effort. PLoS ONE. (2021) 16:e0259459. 10.1371/journal.pone.0259459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.OSHA. OSHA Technical Manual. Section III Chapter 4: Heat Stress. (1999). Available from: https://www.osha.gov/otm/section-3-health-hazards/chapter-4
- 125.UNDP . Climate Change and Labor: Impacts of Heat in the Workplace. Available from: https://www.undp.org/sites/g/files/zskgke326/files/publications/Climate%20and%20Labour%20Issue%20Paper_28%20April%202016_v1_lowres.pdf
- 126.Wegman DH, Apelqvist J, Bottai M, Ekström U, García-Trabanino R, Glaser J, et al. Intervention to diminish dehydration and kidney damage among sugarcane workers. Scand J Work Environ Health. (2018) 44:16–24. 10.5271/sjweh.3659 [DOI] [PubMed] [Google Scholar]
- 127.OSHA . Using the Heat Index: A Guide for Employers. Available from: https://wiagribusiness.org/safety/heat_index_guide.pdf
- 128.Arcury TA, Estrada JM, Quandt SA. Overcoming language and literacy barriers in safety and health training of agricultural workers. J Agromed. (2010) 15:236–48. 10.1080/1059924X.2010.486958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Viveros-Guzmán A, Gertler M. Latino Farmworkers in Saskatchewan: language barriers and health and safety. J Agromed. (2015) 20:341–8. 10.1080/1059924X.2015.1048400 [DOI] [PubMed] [Google Scholar]
- 130.Farquhar SA, Goff NM, Shadbeh N, Samples J, Ventura S, Sanchez V, et al. Occupational health and safety status of indigenous and Latino farmworkers in Oregon. J Agric Saf Health. (2009) 15:89–102. 10.13031/2013.25417 [DOI] [PubMed] [Google Scholar]
- 131.Oxfam . Human Cost of Sugar: Living and Working Conditions of Migrant Cane cutters in Maharashtra. Available from: https://www.oxfamindia.org/sites/default/files/2020-02/%23Human%20Cost%20of%20Sugar_Maharashtra%20Case.pdf
- 132.Lucas RAI, Bodin T, García-Trabanino R, Wesseling C, Glaser J, Weiss I, et al. Heat stress and workload associated with sugarcane cutting—an excessively strenuous occupation! Extrem Physiol Med. (2015) 4:A23. 10.1186/2046-7648-4-S1-A23 [DOI] [Google Scholar]
- 133.Leite MR, Zanetta DMT, Trevisan IB, Burdmann EA, Santos UP. Sugarcane cutting work, risks, and health effects: a literature review. Rev Saude Publica. (2018) 52:80. 10.11606/s1518-8787.2018052000138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Roncal-Jimenez C, Lanaspa MA, Jensen T, Sanchez-Lozada LG, Johnson RJ. Mechanisms by which dehydration may lead to chronic kidney disease. Ann Nutr Metab. (2015) 66:10–3. 10.1159/000381239 [DOI] [PubMed] [Google Scholar]
- 135.Roncal-Jimenez C, García-Trabanino R, Barregard L, Lanaspa MA, Wesseling C, Harra T, et al. Heat stress nephropathy from exercise-induced uric acid crystalluria: a perspective on Mesoamerican nephropathy. Am J Kidney Dis. (2016) 67:20–30. 10.1053/j.ajkd.2015.08.021 [DOI] [PubMed] [Google Scholar]
- 136.Chapman CL, Johnson BD, Sackett JR, Parker MD, Schlader ZJ. Soft drink consumption during and following exercise in the heat elevates biomarkers of acute kidney injury. Am J Physiol Regul Integr Comp Physiol. (2019) 316:R189. 10.1152/ajpregu.00351.2018 [DOI] [PubMed] [Google Scholar]
- 137.Correa-Rotter R, Wesseling C, Johnson RJ. CKD of unknown origin in Central America: the case for a Mesoamerican nephropathy. Am J Kidney Dis. (2014) 63:506–20. 10.1053/j.ajkd.2013.10.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Weiner DE, McClean MD, Kaufman JS, Brooks DR. The Central American epidemic of CKD. Clin J Am Soc Nephrol. (2013) 8:504–11. 10.2215/CJN.05050512 [DOI] [PubMed] [Google Scholar]
- 139.González-Quiroz M, Pearce N, Caplin B, Nitsch D. What do epidemiological studies tell us about chronic kidney disease of undetermined cause in Meso-America? A systematic review and meta-analysis. Clin Kidney J. (2018) 11:496–506. 10.1093/ckj/sfx136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Lunyera J, Mohottige D, Von Isenburg M, Jeuland M, Patel UD, Stanifer JW. CKD of uncertain etiology: a systematic review. Clin J Am Soc Nephrol. (2016) 11:379–85. 10.2215/CJN.07500715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Orantes-Navarro CM, Herrera-Valdés R, Almaguer-López M, López-Marín L, Vela-Parada XF, Hernandez-Cuchillas M, et al. Toward a comprehensive hypothesis of chronic interstitial nephritis in agricultural communities. Adv Chronic Kidney Dis. (2017) 24:101–6. 10.1053/j.ackd.2017.01.001 [DOI] [PubMed] [Google Scholar]
- 142.Correa-Rotter R, García-Trabanino R. Mesoamerican nephropathy. Semin Nephrol. (2019) 39:263–71. 10.1016/j.semnephrol.2019.02.004 [DOI] [PubMed] [Google Scholar]
- 143.Glaser J, Lemery J, Rajagopalan B, Diaz HF, García-Trabanino R, Taduri G, et al. Climate change and the emergent epidemic of ckd from heat stress in rural communities: the case for heat stress nephropathy. Clin J Am Soc Nephrol. (2016) 11:1472–83. 10.2215/CJN.13841215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Valcke M, Levasseur ME, Soares da Silva A, Wesseling C. Pesticide exposures and chronic kidney disease of unknown etiology: an epidemiologic review. Environ Health. (2017) 16:49. 10.1186/s12940-017-0254-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Grubenhoff JA, du Ford K, Roosevelt GE. Heat-related illness. Clin Pediatric Emerg Med. (2007) 8:59–64. 10.1016/j.cpem.2007.02.006 [DOI] [Google Scholar]
- 146.Mix JM, Elon LVV, Mac T, Flocks J, Economos J, Tovar-Aguilar AJ, et al. Physical activity and work activities in Florida agricultural workers. Am J Ind Med. (2019) 62:1058–67. 10.1002/ajim.23035 [DOI] [PubMed] [Google Scholar]
- 147.Habib RR, Hojeij S, Elzein K. Gender in occupational health research of farmworkers: a systematic review. Am J Ind Med. (2014) 57:1344–67. 10.1002/ajim.22375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.OSHA . Water. Rest. Shade (n.d.). Available from: https://www.osha.gov/heat-exposure/water-rest-shade
- 149.Habibi P, Moradi G, Moradi A, Heydari A. The impacts of climate change on occupational heat strain in outdoor workers: A systematic review. Urban Clim. (2021) 36:100770. 10.1016/j.uclim.2021.100770 [DOI] [Google Scholar]
- 150.NIOSH. Heat Stress—Heat Related Illness. (2018). Available from: https://www.cdc.gov/niosh/topics/heatstress/heatrelillness.html
- 151.ILO . Global Employment Trends 2014: Risk of a jobless recovery? Available from: https://www.ilo.org/wcmsp5/groups/public/—dgreports/—dcomm/—publ/documents/publication/wcms_233953.pdf
- 152.Kjellstrom T, Briggs D, Freyberg C, Lemke B, Otto M, Hyatt O. Heat, human performance, and occupational health: a key issue for the assessment of global climate change impacts. Annu Rev Public Health. (2016) 37:97–112. 10.1146/annurev-publhealth-032315-021740 [DOI] [PubMed] [Google Scholar]
- 153.Varghese BM, Hansen A, Bi P, Pisaniello D. Are workers at risk of occupational injuries due to heat exposure? A comprehensive literature review. Safety Sci. (2018) 110:380–92. 10.1016/j.ssci.2018.04.02723430237 [DOI] [Google Scholar]
- 154.Kjellstrom T, Butler AJ, Lucas RM, Bonita R. Public health impact of global heating due to climate change: potential effects on chronic non-communicable diseases. Int J Public Health. (2010) 55:97–103. 10.1007/s00038-009-0090-2 [DOI] [PubMed] [Google Scholar]
- 155.Cianconi P, Betrò S, Janiri L. The impact of climate change on mental health: a systematic descriptive review. Front Psychiatry. (2020) 11:74. 10.3389/fpsyt.2020.00074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Hills AP, Mokhtar N, Byrne NM. Assessment of physical activity and energy expenditure: an overview of objective measures. Front Nutr. (2014) 1:5. 10.3389/fnut.2014.00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Wegman D, Crowe J, Hogstedt C, Jakobsson K, Wesseling C. Mesoamerican Nephropathy: Report from the Second International Research Workshop on MeN (2016). [Google Scholar]
- 158.Moda HM, Filho WL, Minhas A. Impacts of climate change on outdoor workers and their safety: some research priorities. Int J Environ Res Public Health. (2019) 16:3458. 10.3390/ijerph16183458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Chirico F, Taino G. Climate change and occupational health of outdoor workers: an urgent call to action for European policymakers. Environ Dis. (2019) 3:77–9. 10.4103/ed.ed_15_18 [DOI] [Google Scholar]
- 160.Chirico F, Magnavita N. The significant role of health surveillance in the occupational heat stress assessment. Int J Biometeorol. (2019) 63:193–4. 10.1007/s00484-018-1651-y [DOI] [PubMed] [Google Scholar]
- 161.Yengoh GT, Ardö J. Climate Change and the Future Heat Stress Challenges among Smallholder Farmers in East Africa. Atmosphere. (2020) 11:753. 10.3390/atmos11070753 [DOI] [Google Scholar]
- 162.Chan APC, Yi W, Wong FKW. Evaluating the effectiveness and practicality of a cooling vest across four industries in Hong Kong. Facilities. (2016) 34:511–34. 10.1108/F-12-2014-0104 [DOI] [Google Scholar]
- 163.Choi JW, Kim MJ, Lee JY. Alleviation of heat strain by cooling different body areas during red pepper harvest work at WBGT 33 degrees C. Ind Health. (2008) 46:620–8. 10.2486/indhealth.46.620 [DOI] [PubMed] [Google Scholar]
- 164.Chan AP, Song W, Yang Y. Meta-analysis of the effects of microclimate cooling systems on human performance under thermal stressful environments: potential applications to occupational workers. J Therm Biol. (2015) 49–50:16–32. 10.1016/j.jtherbio.2015.01.007 [DOI] [PubMed] [Google Scholar]
- 165.Lundgren K, Kuklane K, Gao C, Holmér I. Effects of heat stress on working populations when facing climate change. Ind Health. (2013) 51:3–15. 10.2486/indhealth.2012-0089 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.