Abstract
Introduction
Surgical abortion is one of the commonly conducted procedures worldwide. Nevertheless, pregnant women still complain of procedural and postoperative pain despite the use of advanced anesthesia. It is vital to women’s reproductive healthcare to improve postsurgical pain management to achieve the lowest level of pain.
Methods
This randomized, double-blind, parallel-controlled clinical trial compared the analgesic effects between nalbuphine and sufentanil in patients who underwent first-trimester surgical abortion. In total, 224 patients were allocated randomly into (a) the sufentanil group that received sufentanil (0.1 ug/kg) combined propofol, and (b) the nalbuphine group that received nalbuphine (0.1 mg/kg) combined propofol. Postoperative pain scores, propofol injection pain, intraoperative analgesic effect, adverse events, and degree of satisfaction were recorded as outcome measures.
Results
The pain scores in the nalbuphine group were lower than those in the sufentanil group at 15 min, 30 min, 1 h, and 6 h after surgical abortion. In addition, the incidence and intensity of propofol injection pain were lower in the nalbuphine group. The degree of satisfaction of the patients in the nalbuphine group was higher than that in the sufentanil group. The intraoperative analgesic effect, hemodynamic fluctuation, and adverse events were comparable between the two groups.
Conclusions
Nalbuphine combined with propofol is superior to sufentanil combined with propofol for first-trimester abortion surgeries.
Clinical Trial Registration
The trial was registered at www.chictr.org.cn, identifier ChiCTR2000040243.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40122-021-00334-0.
Keywords: Nalbuphine, Postoperative pain, Propofol injection pain, Sufentanil, Surgical abortion
Key Summary Points
| Why carry out this study? |
| There are about 56.3 million abortions every year worldwide with physical and mental damage to pregnant woman despite advanced anesthesia methods. |
| Nalbuphine, a synthesized partial κ-agonist/μ-antagonist opioid, had better analgesia effect than μ-agonist opioid in visceral pain models. |
| What was learned from the study? |
| Among the women who underwent first-trimester surgical abortion, nalbuphine 0.1 mg/kg combined with propofol significantly reduced postoperative pain and propofol injection pain. |
| The intraoperative analgesic effects of nalbuphine were comparable with an equivalent dose of sufentanil. |
| The combination of propofol and nalbuphine is effective and safe in first-trimester surgical abortions. |
Digital Features
This article is published with digital features, including slide deck, to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.16803634.
Introduction
On a global scale, 35 abortions occur per 1000 women in the age range of 15–44 years every year. The annual number of abortions was approximately 56.3 million in the period 2010–2014 [1]. Of all the first-trimester abortions, 74% are surgical abortions. Surgical abortion is one of the most extensively recommended and utilized abortion methods [2]. Despite the use of advanced anesthesia methods, pregnant women still complain of procedural [3] and postoperative pain [4]. Inadequate pain control may lead to several adverse effects, such as increased risk factors for chronic pain and increased morbidity [5]. Proper perioperative pain management with the lowest level of pain is vital to women’s reproductive health care.
No validated guidelines exist for pain control in first-trimester surgical abortion [6]. In China, sedative drugs combined with analgesics are commonly used to alleviate pain and anxiety following surgical abortion. Sufentanil, one of the highly potent μ-agonist opioids, is one of the more commonly used analgesics in outpatient surgery [7]. However, the use of μ-receptor agonists is associated with pruritis, constipation, urinary retention, nausea, and vomiting [8].
Nalbuphine, a synthesized partial κ-agonist/μ-antagonist opioid, is used to control mild-to-severe pain. Sun et al. [9] and Xi et al. [10] found that nalbuphine successfully controlled pain and may be a suitable alternative to sufentanil. Owing to κ-agonist actions, nalbuphine was more effective than μ-agonist opioids in visceral pain models [11]. Previous studies had demonstrated that nalbuphine resulted in lower pain sensations at rest and reduced uterine cramping pain, and thus provided better analgesic effects after Cesarean sections [9]. To our knowledge, the studies that compare nalbuphine with sufentanil in surgical abortion cases have been limited. Therefore, the primary aim of this study was to compare intraoperative and postoperative analgesia between sufentanil and nalbuphine in patients who undergo outpatient surgical abortion.
Propofol is the most extensively used intravenous anesthetic in outpatient surgery owing to its rapid onset and rapid recovery profile. However, propofol injection pain is still a common problem in the practice of anesthesia. Its incidence varies from 28 to 90% according to different situations [12, 13]. Wang et al. revealed that pretreatment with nalbuphine decreased propofol injection pain compared with lidocaine [14]. Pure μ-agonist opioids, like remifentanil and sufentanil, had also been used to relieve injection pain [15]. There have been no reported comparison studies between nalbuphine and sufentanil regarding propofol injection pain. Therefore, the secondary purpose of the current study was to determine the better opioid for propofol injection pain treatments in patients who undergo outpatient surgical abortion procedures.
Methods
Study Design
This single-center, randomized, double-blind, parallel-controlled trial was conducted at The First Affiliated Hospital of Anhui Medical University in Hefei from November 2020 to January 2021. Institutional review board approval (PJ2020-12-41) was obtained from the Ethics Committee of The First Affiliated Hospital of Anhui Medical University. Written informed consent was obtained from all participants and the trial was registered at Chinese Clinical Trial Registry (ChiCTR2000040243). The study was performed in accordance with the Declaration of Helsinki.
Participants
First-trimester women undergoing elective painless surgical abortion complying with the state laws and regulations were screened for eligibility for the trial. The inclusion criteria included patients aged between 18 and 45 years, American Society of Anesthesiologists physical status I or II, and a gestational age below 12 weeks. Patients with severe hepatic and renal dysfunction, history of chronic pain, preoperative use of nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids, psychiatric disorders, allergies to nalbuphine or other anesthetic drugs, and emergency re-operations at the time of enrollment, were excluded.
Randomization and Blinding
Eligible participants were randomly allocated at a 1:1 ratio to the sufentanil group and the nalbuphine group by a statistician using SPSS (version 23.0, SPSS Inc., Chicago, IL, USA). The statistician was not involved in patient recruitment or the delivery of medication. The group assignments were contained in sequentially numbered sealed envelopes. An anesthetic nurse who was not involved in the study prepared the study agents in identical 20-ml syringes according to the group assignments. Attending anesthesiologists assigned the intervention to participants using the prepared, identical looking study agents. All patients, surgeons, attending anesthesiologists, and follow-up anesthesiologists were blinded to group assignments. The randomization code was revealed after the follow-up ended or for patients with severe adverse events.
Interventions
All the participants fasted for 8 h and were deprived of water for 2 h before surgery. When patients arrived in the outpatient operation room, intravenous access was established with an 18-G intravenous catheter in dorsal hand vein by the same senior nurse, and no premedication was administered. Standard monitoring including electrocardiograph, heart rate (HR), noninvasive blood pressure (BP), and pulse oxygen saturation were established, and the vital signs pre-induction were recorded. Patients received preoxygenation at a flowrate of 3 l/min with a fiscal mask.
Patients in the sufentanil group received sufentanil 0.1 μg/kg [7] and patients in the nalbuphine group received nalbuphine 0.1 mg/kg for anesthesia induction. Two minutes later, the attending anesthesiologists manually injected 0.5 mg/kg propofol over a period of 15 s. After evaluating the propofol injection pain, an additional amount of propofol (dose of 1.0 mg/kg) was injected to complete the surgical abortion. When patients lost consciousness, the surgical gynecological procedure began. If patients exhibited body movements during the procedure, an additional propofol injection (dose in the range of 0.4–0.8 mg/kg) was administered. Patients were transferred to the recovery room after the end of surgery to recover consciousness.
Outcomes
The primary outcome was postoperative pain. We evaluated the degrees of postoperative pain at 15 min, 30 min, 1 h, and 6 h following the operation based on a numerical rating scale. A score of 0 indicates no pain and a score of 10 indicates the most severe pain. Secondary outcomes included propofol injection pain and an intraoperative analgesic effect. Propofol injection pain was evaluated by a study-blinded follow-up anesthesiologist based on a four-point verbal rating scale [16]: a score of 0 indicated no pain, a score of 1 indicated mild pain (only reported pain in response to questions without behavioral signs), a score of 2 indicated moderate pain (reported pain spontaneously without question or accompanied by behavioral signs), and a score of 3 indicated severe pain (strong vocal response or accompanied by arm withdrawal, facial grimacing, or tears). Intraoperative pain intensity was assessed based on the modified behavioral pain scale (BPS) for non-intubated patients (BPS-NI) (Table S1 in supplementary material) [17]. The modified BPS-NI included three parts: facial expression, movements of the upper and lower limbs, and vocalizations. A total score > 5 indicated that patients experienced intolerable pain during the procedure.
Tertiary outcomes included perioperative hemodynamic changes, adverse events, and patient satisfaction scores. We recorded systolic and diastolic BP, mean arterial pressure (MAP), and HR at T1 (before anesthesia induction), T2 (cervical dilation), T3 (suction aspiration), and T4 (end of the surgery). The occurrence of perioperative adverse events, including tachycardia (> 100 beats per minute [bpm]), bradycardia (< 50 bpm), hypertension (BP > 20% increase from baseline or MAP > 110 mmHg), hypotension (BP > 30% decrease from baseline or MAP < 60 mmHg), respiratory depression (respiratory rate < 8 bpm or partial oxygen saturation < 90%), dizziness, and postoperative nausea and vomiting (PONV) were recorded. The presence of PONV was scored according to the following states and scores: no nausea (0), slight nausea (1), moderate nausea (2), or vomiting (3). The degree of satisfaction was assessed 6 h following surgery based on a scale from 0–3: not satisfied (0), somewhat satisfied (1), moderately satisfied (2), and highly satisfied (3).
Sample Size Calculation
According to our pilot data, we estimated that the mean pain score at 30 min following surgery was 2, and the standard deviation (SD) was equal to 1. With a two-tailed α value of 0.05, power of 90%, and boundaries of efficiency 0.5, a total of 86 patients in each group were required to detect the advantage of nalbuphine. Owing to skewed distribution of the pain score, a nonparametric test for analysis should be used. The sample size needed for a Mann–Whitney U test would be expanded by 1.053 times because the power efficiency of this was expected to be approximately equal to 95% compared with the Student’s t test [18]. Considering a 10% follow-up rate loss, the sample size needed to be expanded by 1.1 times. Finally, we needed 200 patients to detect possible superior outcomes of nalbuphine.
Statistical Analysis
We used the Shapiro–Wilk test to investigate data for normality. The data which satisfied the normal distribution were presented as mean ± SD, and the comparison between groups was performed by a two-tailed Student’s t test. Continuous variables of a non-normal distribution were presented as medians (interquartile range [IQR]), and comparison between groups was performed by the Mann–Whitney U test. For categorical variables, data were described with numbers (frequency), and the χ2 test was used for statistical comparisons. The Mann–Whitney U test was also used for ranked data, such as intensity of propofol injection pain, severity of PONV, and degree of satisfaction. The statistical analyses were performed with SPSS. Two-sided p values < 0.05 were considered statistically significant.
Results
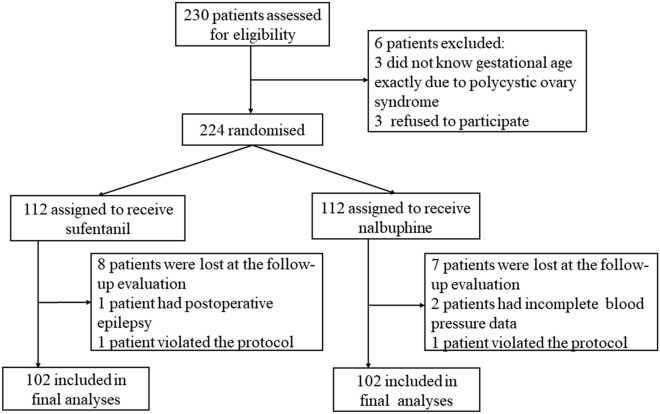
In total, 230 patients were screened for eligibility, and 224 patients proceeded to randomization with 112 allocated to the sufentanil group and 112 to the nalbuphine group. An additional ten patients were excluded from the sufentanil group: eight patients were lost in the follow-up examination, one experienced postoperative epilepsy, and one violated the protocol. Similarly, ten patients were excluded from the nalbuphine group: seven patients were lost in the follow-up evaluation, two had incomplete blood pressure data, and one patient violated the protocol. Finally, 102 patients in each group were included in the final analysis (Fig. 1). Baseline demographic characteristics were comparable between the two groups. There was no significant difference in cervical dilation, surgical characteristics, recovery time, and propofol dosage between the two groups (Table 1).
Fig. 1.
CONSORT flow chart. CONSORT Consolidated Standards of Reporting Trials
Table 1.
Characteristics of the patients and intraoperative data
| Variable | Sufentanil group | Nalbuphine group | p value |
|---|---|---|---|
| Age, years | 28.81 ± 5.69 | 29.40 ± 6.27 | 0.484 |
| Height, cm | 162.07 ± 4.22 | 162.09 ± 4.72 | 0.975 |
| Weight, kg | 56.62 ± 7.97 | 55.02 ± 6.56 | 0.117 |
| BMI | 21.52 ± 2.77 | 20.93 ± 2.27 | 0.099 |
| Gestational age, weeks | 7 (7–8) | 7 (6–8) | 0.301 |
| ASA status (I/II) | 89/13 | 95/7 | 0.159 |
| Dysmenorrhea (n, %) | 30 (29.41%) | 32 (31.37%) | 0.761 |
| History of Cesarean section (n, %) | 27 (26.47%) | 23 (22.55%) | 0.515 |
| History of vaginal delivery (n, %) | 38 (37.25%) | 37 (36.27%) | 0.885 |
| Cervical dilation, mm (7.5/8.0/8.5) | 71/29/2 | 69/31/2 | 0.769 |
| Surgery time, min | 5 (4–6) | 5 (4–6) | 0.838 |
| Anesthesia time, min | 7 (6–8) | 7 (6–8) | 0.813 |
| Recovery time, min | 1 (0–1) | 1 (0–1) | 0.657 |
| Propofol dosage, mg/kg | 2.13 ± 0.32 | 2.15 ± 0.31 | 0.571 |
Data were expressed as mean ± SD, median (interquartile range), or n (%)
BMI body mass index, ASA American Society of Anesthesiologist
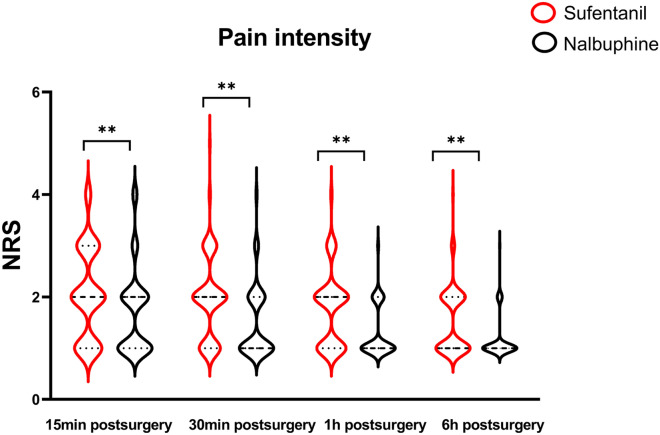
The pain was significantly lower in intensity postoperatively in the nalbuphine group at 15 min (p < 0.001), 30 min (p < 0.001), 1 h (p < 0.001), and 6 h (p < 0.001) (Table 2). Moreover, the proportion of patients with lower pain score in the nalbuphine group was larger (Fig. 2, Table S2 in supplementary material). A pain score of 1 was registered for 31 patients (30.39%) in the sufentanil group at 15 min compared with 49 patients (48.04%) in the nalbuphine group. The number of patients who had a score of 1 were 30 (29.41%) in the sufentanil group and 62 (60.78%) in the nalbuphine group at 30 min postoperatively; 40 (39.22%) and 74 (72.55%) at 1 h postoperatively, and 56 (54.90%) and 88 (86.27%) at 6 h postoperatively. However, the number of intraoperative body movements and the number of patients with BPS-NI > 5 were similar between the two groups (Table 2). There was no difference in the number of patients for all scores in the BPS-NI scale (Fig. S1 in supplementary material). The intensity and the incidence (48.04 vs. 80.39%, p < 0.001) of propofol injection pain were lower in the nalbuphine group (Table 2).
Table 2.
Analgesic effect between the two groups
| Variable | Sufentanil group | Nalbuphine group | p value |
|---|---|---|---|
| Pain 15 min postsurgery | 2 (1–3) | 2 (1–2) | < 0.001 |
| Pain 30 min postsurgery | 2 (1–2) | 1 (1–2) | < 0.001 |
| Pain 1 h postsurgery | 2 (1–2) | 1 (1–2) | < 0.001 |
| Pain 6 h postsurgery | 1 (1–2) | 1 (1–1) | < 0.001 |
| No. of intraoperative body movement | 1 (0–2) | 1 (0–2) | 0.205 |
| BPS-NI > 5 (n, %) | 15 (14.71%) | 12 (11.76%) | 0.535 |
| Propofol injection pain | < 0.001 | ||
| 0 (n, %) | 20 (19.61%) | 53 (51.96%) | |
| 1 (n, %) | 48 (47.06%) | 40 (39.22%) | |
| 2 (n, %) | 28 (27.45%) | 6 (5.88%) | |
| 3 (n, %) | 6 (5.88%) | 3 (2.94%) |
Data were expressed as median (interquartile range), or n (%). BPS-NI behavioral pain scale for non-intubated patients. 0 = no pain, 1 = mild pain (only reported pain in response to question without behavioral sign), 2 = moderate pain (reported pain spontaneously without question or accompanied by behavior sign), 3 = severe pain (strong vocal response or accompanied by arm withdrawal, facial grimacing, or tears)
Fig. 2.
Pain intensity comparison following surgery. Comparison of postoperative pain between the two studied groups. The red frame represents the sufentanil group and the black frame represents the nalbuphine group (**p < 0.01 compared with sufentanil group; NRS numeric rating scale)
The MBP and HR were similar between the two groups at T1, T2, T3, and T4 (Fig. 3). There were no statistical differences in the incidence of hypotension, hypertension, bradycardia, and dizziness. One patient in the nalbuphine group and none in the sufentanil group had respiratory depression. The degree and incidence of PONV were comparable (32.25% in the sufentanil group vs. 28.43% in the nalbuphine group, p = 0.543) between the two groups. Patients in the nalbuphine group had a higher degree of satisfaction than that in the sufentanil group (p = 0.007). One patient in the sufentanil group was unsatisfied with the anesthesia owing to postoperative pain (Table 3).
Fig. 3.
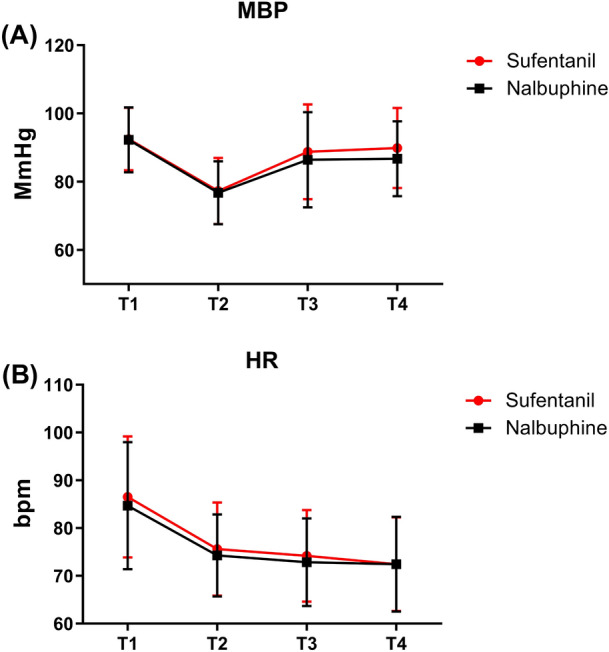
Intraoperative hemodynamic changes. Comparison of mean blood pressure (A) and heart rate (B) between the two studied groups. Data are expressed as mean ± SD. (**p < 0.01, compared with sufentanil group; T1, enter the operating room; T2, dialation of the cervix. T3, negative pressure suction; T4, end of the surgery; MBP mean blood pressure, HR heart rate, bpm beats per minute)
Table 3.
Perioperative adverse events and patients’ satisfaction
| Variable | Sufentanil group | Nalbuphine group | p value |
|---|---|---|---|
| Hypertension (n, %) | 12 (11.76%) | 8 (7.84%) | 0.346 |
| Hypotension (n, %) | 13 (13.73%) | 15 (15.69%) | 0.684 |
| Bradycardia (n, %) | 3 (2.94%) | 3 (2.94%) | / |
| Respiratory depression (n, %) | 0 (0%) | 1 (0.98%) | 0.999 |
| Dizziness (n, %) | 16 (14.71%) | 23 (22.55%) | 0.213 |
| Nausea/vomiting | 0.516 | ||
| 0 (n, %) | 69 (67.65%) | 73 (71.57%) | |
| 1 (n, %) | 13 (12.75%) | 16 (15.69%) | |
| 2 (n, %) | 15 (14.70%) | 4 (3.92%) | |
| 3 (n, %) | 5 (4.90%) | 9 (8.82%) | |
| Satisfaction | 0.007 | ||
| 0 (n, %) | 1 (0.98%) | 0 (0%) | |
| 1 (n, %) | 23 (22.55%) | 11 (10.78%) | |
| 2 (n, %) | 52 (50.98%) | 51 (50.00%) | |
| 3 (n, %) | 26 (25.49%) | 40 (39.22%) |
Data were expressed as n (%). Nausea/vomiting: 0 = no nausea, 1 = slight nausea, 2 = moderate nausea, 3 = vomiting. Satisfaction: 0 = not satisfied, 1 = somewhat satisfied, 2 = moderate satisfied, 3 = highly satisfied
Discussion
In this study, we compared the analgesia effect of sufentanil and nalbuphine in patients who underwent surgical abortion. The study demonstrated that nalbuphine combined with propofol had lower postoperative pain, propofol injection pain, and a higher degree of satisfaction compared with sufentanil combined with propofol. However, the intraoperative analgesic effect was similar between these two opioids. The adverse events, such as respiratory depression, dizziness, nausea, and vomiting, were comparable.
Surgical abortion can cause physical and mental damage to pregnant women. The pain women experience after surgical abortion comes from the cramping associated with the involution of the uterus [19]. Pain due to uterine contraction represents a common form of visceral pain. In visceral pain models, κ-agonists appeared to be the most effective class of opioid agonists [11]. The uterus is mainly innervated by sympathetic and parasympathetic nerves from the spinal cord. The κ-receptor is mainly found in the spinal cord. By contrast, the μ-receptor is mainly found in the brain [8]. Hence, nalbuphine, a κ-receptor agonist, yielded a higher concentration in the spinal cord. It has been proven that nalbuphine provides better analgesic effects after Cesarean surgery [9]. Our results are consistent with a previous report [20] in which the use of nalbuphine (dose of 0.25 mg/kg) for the termination of pregnancy was associated with improved postoperative analgesia, and was more satisfactory compared with fentanyl. Nalbuphine and morphine are considered to have equal analgesic effects [21], and the analgesic potency of sufentanil is 1000 times more effective than morphine [22]. Hence, in this study, we used nalbuphine (0.1 mg/kg) as an equivalent drug to sufentanil (0.1 μg/kg). Zeng et al. have proven that nalbuphine (0.1 mg/kg) combined with propofol provides physical and mental safety in the hysteroscopic anesthesia [23].
Pain perception is affected by physical and psychosocial elements and their interactions [6]. Previous studies have demonstrated that young age, nulliparity, and dysmenorrhea were associated with increased pain following abortion [24]. In addition, a history of vaginal delivery correlates with decreased pain [25]. Gestational age and the amount of cervical dilation have also been shown to influence the pain experience [26]. To avoid these confounders, we used a random allocation to balance the physical and psychosocial elements that might affect pain. The age, gestational age, ASA status, dysmenorrhea, history of Cesarean section, history of vaginal delivery, and cervical dilation were comparable between the two groups in the present study.
Strategies used to reduce intraoperative pain are important for significant public health owing to the large number of first-trimester surgical abortions. Surgical abortion, particularly cervical dilation and suction aspiration, is associated with pain. In this study, these two opioids had similar intraoperative analgesic effects. Both groups yielded similar fluctuations in MAP and HR at T1, T2, T3, and T4. MAP and HR at cervical dilation (T2) and suction aspiration (T1) were still lower than that before anesthesia induction (T1). Incidences associated with BPS-NI > 5 were similar between the two groups (14.71 vs. 11.76%, p = 0.535), and most of the patients had satisfactory analgesic effects. In conclusion, both of these opioids can suppress procedural pain effectively.
Although propofol injection pain may not be a serious complication, anesthetists face it almost every day owing to its high incidence. Most patients remember it as one of the most unpleasant experiences, especially in outpatient surgeries. The exact mechanism of propofol injection pain was still not well explained. It contains immediate pain owing to the irritation of the endothelial layers in veins, and also delayed pain owing to mediators, such as kininogen, from the kinin cascade [27]. A number of remedies are used to relieve propofol injection pain, such as lignocaine, NSAIDs, and opioids [28]. In our study, we compared sufentanil and nalbuphine, and found that patients in the nalbuphine group had a lower incidence (48.04 vs. 80.39%, p < 0.001) and intensity of propofol injection pain. Compared with a previous study, the incidence of the nalbuphine group in our study was higher than 27% [14], and the incidence of sufentanil group in our study was higher than 75% [15]. Being female, a young age, and dorsal hand veins may account for higher incidence of propofol injection pain in the present study. It has been demonstrated that opioids may relieve propofol injection pain via their mediation with central [29] or peripheral [30] opioid receptors. Based on the results that showed that nalbuphine is significantly better than sufentanil in suppressing propofol injection pain, we hypothesized that nalbuphine alleviate propofol injection pain mainly through the κ receptor
Compared with sufentanil, intravenous administration of nalbuphine (0.1 mg/kg) yielded similar symptoms of hypertension, hypotension, bradycardia, and dizziness. Because of the low dosage of these two opioids, there was almost no adverse effect of respiratory depression. Although the frequency and severity of PONV were comparable between the two groups, PONV constitutes a common problem with the termination of pregnancy. The high incidence of PONV may be associated with the emotional state of the patient, the oxytocic agent used, and the type of the anesthetic technique [31]. In addition, patients in the nalbuphine group with a higher degree of satisfaction may be attributed to a smaller propofol injection and postoperative pain. Therefore, clinicians may choose nalbuphine as the preferred analgesic in surgical abortion.
There are several limitations associated with this study. Firstly, we compared just one dosage of nalbuphine and sufentanil on the analgesic effect in women who underwent first-trimester surgical abortion. Additional research comparing other doses is required. Secondly, we did not conduct stress hormone tests, such as adrenocorticotropic hormone and cortisol. In addition, all of the participants in this study were female. Accordingly, caution should be exercised when the results and conclusions of this study are extended to the general population. Future research including both males and females is needed to further compare analgesic effects between nalbuphine and sufentanil. Furthermore, we did not use any other instruments to measure physical and psychosocial elements, which can affect pain perception.
Conclusions
In conclusion, among the women who underwent first-trimester surgical abortion, nalbuphine combined with propofol significantly reduced postoperative pain and propofol injection pain and increased the degree of patient satisfaction without significant side effects. However, the intraoperative analgesic effects were comparable. Nalbuphine combined with propofol is superior to sufentanil when combined with propofol in first-trimester surgical abortion cases.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank all the participants of the study. We thank the Yichang Renfu Pharmaceutical Co., Ltd. and Fresenius Kabi Pharmaceutical Co., Ltd. for providing sufentanil, nalbuphine, and propofol.
Funding
This study and the journal’s Rapid Service Fee were funded by the Joint Project of Anesthesiology and Pharmacology (No. 2021lcxk002).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Panpan Fang, Jing Qian, and Jianming Ding. The first draft of the manuscript was written by Panpan Fang and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
Panpan Fang, Jing Qian, Jianming Ding, Xiao Pan, Han Su, and Xuesheng Liu declare that they have nothing to disclose.
Compliance with Ethics Guidelines
The study was conducted at the First Affiliated Hospital of Anhui Medical University from November 2020 to January 2021, in accordance with the Declaration of Helsinki. The study was approved by the hospital’s Research Ethics Committee (The First Affiliated Hospital of Anhui Medical University Ethics Committee, PJ 2020-12-41) and was registered in the Chinese Clinical Trial Registry (ChiCTR2000040243, Principal investigator: Xuesheng Liu, Date of registration: 2020-11-26). Written informed consent was obtained from all participants in this study.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1.Sedgh G, Bearak J, Singh S, et al. Abortion incidence between 1990 and 2014: global, regional, and subregional levels and trends. Lancet. 2016;388(10041):258–267. doi: 10.1016/S0140-6736(16)30380-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yonke N, Leeman LM. First-trimester surgical abortion technique. Obstet Gynecol Clin N Am. 2013;40(4):647–670. doi: 10.1016/j.ogc.2013.08.006. [DOI] [PubMed] [Google Scholar]
- 3.O'Connell K, Jones HE, Simon M, et al. First-trimester surgical abortion practices: a survey of National Abortion Federation members. Contraception. 2009;79(5):385–392. doi: 10.1016/j.contraception.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 4.Mustafa-Mikhail S, Assaraf S, Abecassis P, et al. Comparison between lornoxicam and paracetamol for pain management after dilation and curettage for abortion. Isr Med Assoc J. 2017;19(9):543–546. [PubMed] [Google Scholar]
- 5.Glare P, Aubrey KR, Myles PS. Transition from acute to chronic pain after surgery. Lancet. 2019;393(10180):1537–1546. doi: 10.1016/S0140-6736(19)30352-6. [DOI] [PubMed] [Google Scholar]
- 6.Renner RM, Jensen JT, Nichols MD, Edelman AB. Pain control in first-trimester surgical abortion: a systematic review of randomized controlled trials. Contraception. 2010;81(5):372–388. doi: 10.1016/j.contraception.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 7.Deng C, Wang X, Zhu Q, Kang Y, Yang J, Wang H. Comparison of nalbuphine and sufentanil for colonoscopy: a randomized controlled trial. PLoS ONE. 2017;12(12):e0188901. doi: 10.1371/journal.pone.0188901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trescot AM, Datta S, Lee M, Hansen H. Opioid pharmacology. Pain Physician. 2008;11(2 Suppl):S133–S153. doi: 10.36076/ppj.2008/11/S133. [DOI] [PubMed] [Google Scholar]
- 9.Sun S, Guo Y, Wang T, Huang S. Analgesic effect comparison between nalbuphine and sufentanil for patient-controlled intravenous analgesia after cesarean section. Front Pharmacol. 2020;11:574493. doi: 10.3389/fphar.2020.574493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xi MY, Li SS, Zhang C, Zhang L, Wang T, Yu C. Nalbuphine for analgesia after orthognathic surgery and its effect on postoperative inflammatory and oxidative stress: a randomized double-blind controlled trial. J Oral Maxillofac Surg. 2020;78(4):528–537. doi: 10.1016/j.joms.2019.10.017. [DOI] [PubMed] [Google Scholar]
- 11.Riviere PJ. Peripheral kappa-opioid agonists for visceral pain. Br J Pharmacol. 2004;141(8):1331–1334. doi: 10.1038/sj.bjp.0705763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mangar D, Holak EJ. Tourniquet at 50 mmHg followed by intravenous lidocaine diminishes hand pain associated with propofol injection. Anesth Analg. 1992;74(2):250–252. doi: 10.1213/00000539-199202000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Dubey PK, Kumar A. Pain on injection of lipid-free propofol and propofol emulsion containing medium-chain triglyceride: a comparative study. Anesth Analg. 2005;101(4):1060–1062. doi: 10.1213/01.ane.0000166951.72702.05. [DOI] [PubMed] [Google Scholar]
- 14.Wang J, Duan J, Xie C, Yu Y, Lu Y. Comparison between intravenous nalbuphine and lidocaine in reducing propofol-induced injection pain during gastroscopy: a randomized controlled trial. Pain Ther. 2020;9(2):563–571. doi: 10.1007/s40122-020-00188-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Honarmand A, Safavi M. Prevention of propofol-induced injection pain by sufentanil: a placebo-controlled comparison with remifentanil. Clin Drug Investig. 2008;28(1):27–35. doi: 10.2165/00044011-200828010-00004. [DOI] [PubMed] [Google Scholar]
- 16.Lee SH, Lee SE, Chung S, Lee HJ, Jeong S. Impact of time interval between remifentanil and propofol on propofol injection pain. J Clin Anesth. 2016;34:510–515. doi: 10.1016/j.jclinane.2016.06.029. [DOI] [PubMed] [Google Scholar]
- 17.Chanques G, Payen JF, Mercier G, et al. Assessing pain in non-intubated critically ill patients unable to self-report: an adaptation of the Behavioral Pain Scale. Intensive Care Med. 2009;35(12):2060–2067. doi: 10.1007/s00134-009-1590-5. [DOI] [PubMed] [Google Scholar]
- 18.Page VJ, Ely EW, Gates S, et al. Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope-ICU): a randomised, double-blind, placebo-controlled trial. Lancet Respir Med. 2013;1(7):515–523. doi: 10.1016/S2213-2600(13)70166-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paliulyte V, Drasutiene GS, Ramasauskaite D, Bartkeviciene D, Zakareviciene J, Kurmanavicius J. Physiological uterine involution in primiparous and multiparous women: ultrasound study. Obstet Gynecol Int. 2017;2017:6739345. doi: 10.1155/2017/6739345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bone ME, Dowson S, Smith G. A comparison of nalbuphine with fentanyl for postoperative pain relief following termination of pregnancy under day care anaesthesia. Anaesthesia. 1988;43(3):194–197. doi: 10.1111/j.1365-2044.1988.tb05538.x. [DOI] [PubMed] [Google Scholar]
- 21.Zeng Z, Lu J, Shu C, et al. A comparison of nalbuphine with morphine for analgesic effects and safety: meta-analysis of randomized controlled trials. Sci Rep. 2015;5:10927. doi: 10.1038/srep10927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sun Z, Zhu Z, Yang G, Zheng H. The 95% effective dose of nalbuphine in patient-controlled intravenous analgesia for patients undergoing laparoscopic total hysterectomy compared to equivalent sufentanil. Medicine (Baltimore) 2020;99(22):e20424. doi: 10.1097/MD.0000000000020424. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 23.Zeng R, Dong S, Wei Y. Influences of different doses of nalbuphine combined with propofol on the anesthetic effects, hemodynamics, inflammation and immunity of patients undergoing hysteroscopic surgery. Panminerva Med. 2020. [DOI] [PubMed]
- 24.Bélanger E, Melzack R, Lauzon P. Pain of first-trimester abortion: a study of psychosocial and medical predictors. Pain. 1989;36(3):339–350. doi: 10.1016/0304-3959(89)90094-8. [DOI] [PubMed] [Google Scholar]
- 25.Lui MW, Ho PC. First trimester termination of pregnancy. Best Pract Res Clin Obstet Gynaecol. 2020;63:13–23. doi: 10.1016/j.bpobgyn.2019.06.004. [DOI] [PubMed] [Google Scholar]
- 26.Moayedi G, Tschann M. Pain management for first-trimester uterine aspiration. Obstet Gynecol Surv. 2018;73(3):174–181. doi: 10.1097/OGX.0000000000000544. [DOI] [PubMed] [Google Scholar]
- 27.Tan CH, Onsiong MK. Pain on injection of propofol. Anaesthesia. 1998;53(5):468–476. doi: 10.1046/j.1365-2044.1998.00405.x. [DOI] [PubMed] [Google Scholar]
- 28.Desousa KA. Pain on propofol injection: causes and remedies. Indian J Pharmacol. 2016;48(6):617–623. doi: 10.4103/0253-7613.194845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wrench IJ, Girling KJ, Hobbs GJ. Alfentanil-mediated analgesia during propofol injection: no evidence for a peripheral action. Br J Anaesth. 1996;77(2):162–164. doi: 10.1093/bja/77.2.162. [DOI] [PubMed] [Google Scholar]
- 30.Aouad MT, Siddik-Sayyid SM, Al-Alami AA, Baraka AS. Multimodal analgesia to prevent propofol-induced pain: pretreatment with remifentanil and lidocaine versus remifentanil or lidocaine alone. Anesth Analg. 2007;104(6):1540–1544. doi: 10.1213/01.ane.0000261520.34879.09. [DOI] [PubMed] [Google Scholar]
- 31.Fujii Y. Prevention of nausea and vomiting during termination of pregnancy. Int J Gynaecol Obstet. 2010;111(1):3–7. doi: 10.1016/j.ijgo.2010.05.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.