Abstract
BACKGROUND
The quick sequential organ failure assessment (qSOFA) is recommended to identify sepsis and predict sepsis mortality. However, some studies have recently shown its poor performance in sepsis mortality prediction. To enhance its effectiveness, researchers have developed various revised versions of the qSOFA by adding other parameters, such as the lactate-enhanced qSOFA (LqSOFA), the procalcitonin-enhanced qSOFA (PqSOFA), and the modified qSOFA (MqSOFA). This study aimed to compare the performance of these versions of the qSOFA in predicting sepsis mortality in the emergency department (ED).
METHODS
This retrospective study analyzed data obtained from an electronic register system of adult patients with sepsis between January 1 and December 31, 2019. Receiver operating characteristic (ROC) curve analyses were performed to determine the area under the curve (AUC), with sensitivity, specificity, and positive and negative predictive values calculated for the various scores.
RESULTS
Among the 936 enrolled cases, there were 835 survivors and 101 deaths. The AUCs of the LqSOFA, MqSOFA, PqSOFA, and qSOFA were 0.740, 0.731, 0.712, and 0.705, respectively. The sensitivity of the LqSOFA, MqSOFA, PqSOFA, and qSOFA were 64.36%, 51.40%, 71.29%, and 39.60%, respectively. The specificity of the four scores were 70.78%, 80.96%, 61.68%, and 91.62%, respectively. The LqSOFA and MqSOFA were superior to the qSOFA in predicting in-hospital mortality.
CONCLUSIONS
Among patients with sepsis in the ED, the performance of the PqSOFA was similar to that of the qSOFA and the values of the LqSOFA and MqSOFA in predicting in-hospital mortality were greater compared to qSOFA. As the added parameter of the MqSOFA was more convenient compared to the LqSOFA, the MqSOFA could be used as a candidate for the revised qSOFA to increase the performance of the early prediction of sepsis mortality.
Keywords: Quick sequential organ failure assessment, In-hospital mortality, Sepsis, Lactate- enhanced qSOFA, Modified qSOFA
INTRODUCTION
Sepsis is one of the leading causes of mortality worldwide, characterized by infection-induced physiological, pathological, and biochemical abnormalities resulting in significant healthcare and social implications.[1–4] In the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)[1], experts recommend the use of quick sequential organ failure assessment (qSOFA) for the diagnosis of sepsis and screening of patients with severe sepsis who are at higher risk of mortality.[1,5]
The criteria of the qSOFA to predict poor outcomes in adult patients with sepsis are a respiratory rate of ≥22 breaths per minute, systolic blood pressure of ≤100 mmHg (1 mmHg=0.133 kPa), and altered mentation. The qSOFA is fast and straightforward, making it appropriate for emergency department (ED) use. However, recent studies have shown the poor performance of qSOFA in predicting sepsis mortality.[6–9] To enhance its effectiveness, researchers have developed various revised versions of the qSOFA by including additional parameters, including the lactate-enhanced qSOFA (LqSOFA),[10] the procalcitonin (PCT)-enhanced qSOFA (PqSOFA),[11] and the modified qSOFA (MqSOFA).[12]
LqSOFA assigned a lactate level of ≥2 mmol/L one point based on the qSOFA score assignment method. Similarly, the PqSOFA assigned an additional point if PCT was at a threshold of >0.5 ng/mL. Likewise, the MqSOFA assigned an additional point calculated from the ratio of peripheral oxygen saturation and a fraction of inspired oxygen (SpO2/FiO2 ratio); a score of 0 was assigned if the SpO2/FiO2 ratio was ≥315, 1 point if 314–236, and 2 points if ≤235. For the details of the revised versions of the qSOFA, see the Supplementary Table 1.
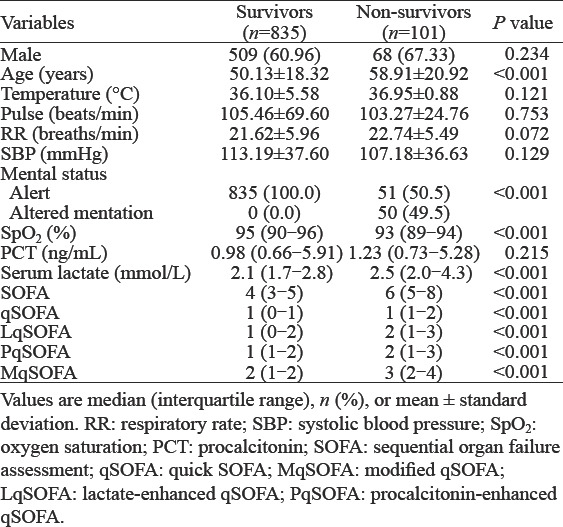
Table 1.
Comparison of the baseline characteristics of survivors and non-survivors
However, there are few studies verifying and comparing the effectiveness of these revised versions. Therefore, we aimed to evaluate these revised versions of the qSOFA as an in-hospital mortality indicator and for the prognosis of patients with sepsis.
METHODS
Study design
This retrospective study reviewed data obtained from an electronic register system of patients with sepsis who visited West China Hospital. The electronic register system was a part of Hospital Information System (HIS) in which emergency physicians recorded the information of patients.
The local Institutional Review Committee approved the study and waived the requirement for informed consent due to the retrospective nature of the study. The study complied with the international ethical guidelines for human research, such as the Declaration of Helsinki. The accessed data were anonymized.
Settings and subjects
This study included 974 adult patients diagnosed with sepsis in the ED of West China Hospital between January 1 and December 31, 2019. Patients with the following characteristics were included: (1) age ≥18 years and; (2) diagnosis of sepsis (based on the Sepsis-3 criteria,[1] sepsis was defined as life-threatening organ dysfunction caused by the infection. Organ dysfunction was identified as a sequential organ failure assessment (SOFA) score ≥2. The exclusion criteria were: (1) lack of information which hindered the calculation of scores; (2) lack of outcome information; and (3) patients who were intubated when they arrived at the ED.
For all included cases, the following data were retrieved from the electronic register system: demographic characteristics; inital vital signs (body temperature, heart rate, systolic and diastolic blood pressure, and respiratory rate); inital mental status (alert, verbal, pain, unresponsive [AVPU] system); inital oxygen saturation level, initial bedside lactate; initial PCT; other parameters used to calculate the scoring system, and final diagnosis. The outcome was death or survival at discharge. The observation point for survival calculations was set as the discharge time of the last admitted patient.
Statistical analysis
Data analysis was conducted using the SPSS 20.0 (IBM, USA) and MedCalc 18.2.1 (MedCalc Software Ltd., Belgium). Continuous variables are presented as means with standard deviations or median with interquartile range and were compared using the Student’s t-test or Mann-Whitney U-test. Categorical variables are described as number and composition ratios and were compared using the Chi-square test or Fisher’s exact test (when the expected value was <5 in one cell).
Receiver operating characteristic (ROC) curve analyses were conducted to evaluate the effectiveness of different score systems as predictors of mortality. The performance of these scoring systems to discriminate between survivors and non-survivors was evaluated by calculating the area under the curve (AUC) of ROC with a 95% confidence interval. The AUCs were compared using Delong’s approach.[13,14] The cut-off value for each scoring scale was determined as the maximum value of Youden’s index.
Finally, the corresponding accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) related to the optimal cut-off point for each score were calculated. A P-value <0.05 was considered statistically significant.
RESULTS
Among the 974 patients, 38 were excluded due to missing data. In total, 936 patients were included in the final analysis of the study (Figure 1).
Figure 1.
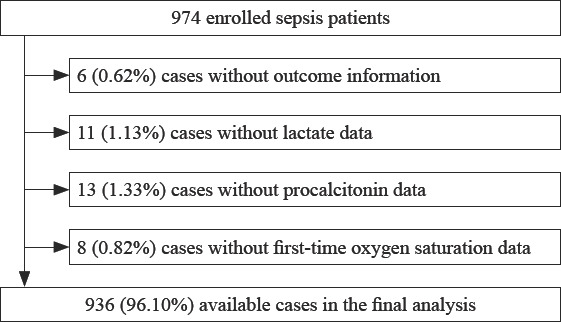
Flow chart of case exclusions.
Among the enrolled cases, there were 835 survivors and 101 deaths. The age of survivors (50.13±18.32 years) was significantly younger than that of the non-survivors (58.91±20.92 years) (P<0.05). Moreover, the mental status, oxygen saturation, serum lactate, qSOFA, MqSOFA, LqSOFA, and PqSOFA were significantly different between the two groups (P<0.05). However, no significant difference was observed on sex, temperature, respiratory rate, systolic blood pressure, and PCT between the two groups (Table 1).
Among the four score systems, ROC curve analysis found that LqSOFA was the best predictor of in-hospital mortality of sepsis patients, with an AUC of 0.740, followed by MqSOFA, PqSOFA, and qSOFA with AUC of 0.731, 0.712, and 0.705, respectively (Table 2, Figure 2).
Table 2.
The performance of scores with different cut-offs in predicting in-hospital mortality of sepsis patients
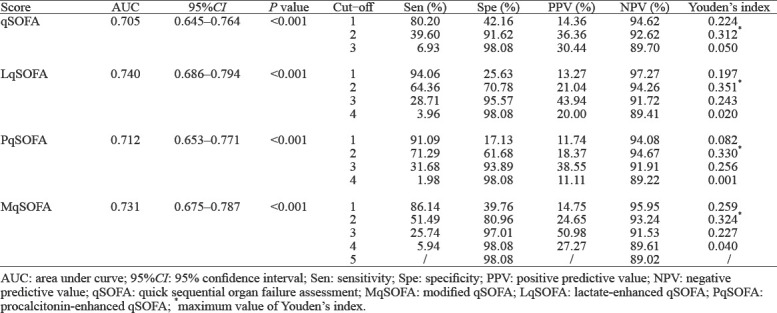
Figure 2.
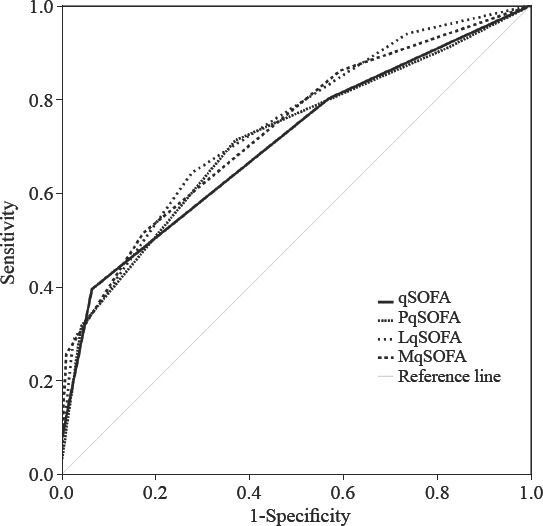
ROC curves of different versions of the qSOFA in predicting in-hospital mortality. ROC: receiver operating characteristic; qSOFA: quick sequential organ failure assessment; LqSOFA: lactate-enhanced qSOFA; MqSOFA: modified qSOFA; PqSOFA: procalcitonin- enhanced qSOFA.
Based on the maximum Youden’s index, an optimum cut-off value of 2 was used to predict in-hospital mortality using the LqSOFA, with a sensitivity, specificity, PPV, and NPV of 64.36%, 70.78%, 21.04%, and 94.26%, respectively. The optimum cut-off value of MqSOFA was 2 with sensitivity, specificity, PPV, and NPV of 51.49%, 80.96%, 24.65%, and 93.24%, respectively. Likewise, an optimum cut-off value of 2 was used in the PqSOFA, with sensitivity, specificity, PPV, and NPV of 71.29%, 61.68%, 18.37%, and 94.67%, respectively. The optimum cut-off value of qSOFA was 2 points with sensitivity, specificity, PPV, and NPV of 39.60%, 91.62%, 36.36%, and 92.62%, respectively (Table 2).
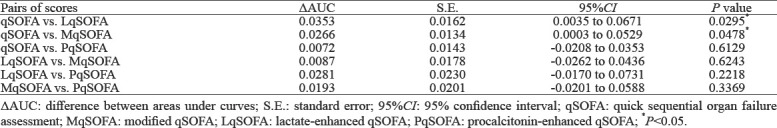
There were significant differences of AUCs between the LqSOFA and qSOFA and between the MqSOFA and qSOFA (both P<0.05). However, no other significant difference was observed (Table 3).
Table 3.
Pairwise comparison of AUC of scores for predicting in-hospital mortality of sepsis patients
DISCUSSION
The recent increase in sepsis mortality has raised the awareness of the importance of early risk stratification among emergency physicians. Since 2016, early identification and in-hospital mortality prediction of patients with sepsis in the ED with qSOFA has been recommended.[1] The simplicity and availability of the qSOFA has warranted its wide use in the ED.[15]
However, our study showed that the sensitivity and specificity of the qSOFA in predicting in-hospital mortality in patients with sepsis were 39.60% and 91.62%, respectively, indicating a weak sensitivity. Our result is consistent with recent studies that emphasized the poor performance of qSOFA in the prediction of sepsis mortality.[16, 17] A retrospective study by Moskowitz et al[18] found that the qSOFA had a sensitivity and specificity of 39% and 87%, respectively, when used in predicting in-hospital mortality at the time of ED presentation among 24,164 patients with sepsis. Similarly, a prospective study by Askim et al[19] on 1,535 adult patients found that the qSOFA had a sensitivity and specificity of 16% and 96%, respectively, in predicting mortality at the time of ED presentation. Other studies found that the sensitivity of the qSOFA in predicting mortality ranged from 13% to 90%, while the specificity ranged from 86% to 96%.[8, 20–22]
These studies indicated acceptable qSOFA specificity but unsatisfactory sensitivity, which was consistent with our results. However, high sensitivity is more important than high specificity in predicting sepsis mortality.[23] This is due to the higher risk and cost of false negativity compared to false positivity in patients with high mortality risk.[23, 24]
Based on previous studies, researchers have recently added simplely available indices to the qSOFA to improve sensitivity. In a retrospective study of 836 patients, Liu et al[10] introduced bedside serum lactate and put forward the LqSOFA, which was shown to be superior to the qSOFA. Our findings were consistent with their study, indicating the superiority of the LqSOFA compared to the qSOFA (P<0.05). Additionally, previous studies have shown the effectiveness of lactate as a predictor of sepsis mortality;[25–27] therefore, lactate will expectedly increase the effectiveness of the qSOFA in predicting sepsis mortality.[28, 29] This addition to the qSOFA for comprehensive scoring could help emergency physicians to make clinical decisions by combining two indicators instead of using one in isolation.
The SpO2/FiO2 ratio is associated with respiratory status; some studies have included it as a key parameter for sepsis mortality.[30,31] In a retrospective study of 1,137 cases, Guarino et al[12] introduced the SpO2/FiO2 ratio into the qSOFA and developed a modified qSOFA (MqSOFA), which showed better accuracy than the qSOFA. Our study also suggested that the performance of MqSOFA was better than qSOFA. Therefore, the MqSOFA may be a viable tool in predicting sepsis mortality.
Xia et al[11] added PCT to the qSOFA and developed the PqSOFA, which was indicated to have a higher sensitivity but lower specificity in predicting sepsis mortality compared to qSOFA in a retrospective study of 821 patients. However, no significant difference was observed between the AUCs of the PqSOFA and the qSOFA in our research. Similarly, previous studies have inconsistent results regarding the effectiveness of PCT as a predictor of sepsis mortality.[32–35] Therefore, further studies are required to determine the utility of the PqSOFA as a revised scoring system for the early prediction of sepsis.
According to our results, the best among the four score systems was the LqSOFA, followed by the MqSOFA, PqSOFA, and qSOFA. Generally, the revised qSOFAs obtained better sensitivity and accuracy in predicting the mortality of sepsis patients than the qSOFA; however, the results remain unsatisfactory. Among the revised versions of the qSOFA, LqSOFA and MqSOFA had similar performance in predicting sepsis mortality (P>0.05). The additional parameters from these measures can be obtained rapidly and conveniently; therefore, the LqSOFA and MqSOFA can be used in the early assessment of mortality in the ED. SpO2/FiO2 ratio is more convenient than lactate; therefore, we suggest that the MqSOFA can be used as a candidate for the revised qSOFA to increase the performance of early prediction of sepsis mortality. Furthermore, both the LqSOFA and PqSOFA require a bedside test to be calculated. The MqSOFA was the only altered version of the qSOFA, which contains completely clinical information that makes this score helpful in pre-hospital settings.
This study had several limitations. Firstly, the study population was small. Further studies employing a large sample will provide a higher level of evidence for assessing these scores. Additionally, pre-hospital care was neglected because of unavailable information. Secondly, because of the nature of the retrospective study, we identified altered mentation using the AVPU system. Indeed, altered mentation in the qSOFA should be explained as a different mental status of the patient. Even so, since the altered mentation of each score uses the AVPU system, we believe that this has little effect on the comparison of each score. However, this may affect the test characteristics of each score. Therefore prospective research should be carried out in the future. Finally, our single-center study may cause selection bias. Further multi-center studies are required to validate the performance of these revised qSOFAs prospectively.
CONCLUSIONS
Among the three revised qSOFAs, the PqSOFA had a higher sensitivity and lower specificity than the qSOFA; however, their performances were similar. Moreover, the values of the LqSOFA and MqSOFA in predicting in-hospital mortality were greater compared to the qSOFA. As the added parameter of the MqSOFA was more convenient compared than that of the LqSOFA, the MqSOFA is a potential candidate for the revised qSOFA to increase the performance of the early prediction of sepsis mortality.
ACKNOWLEDGEMENTS
We would like to thank all the physicians and nurses who worked in the hospital for helping us collect the data.
Footnotes
Funding: None.
Ethical approval: The local Institutional Review Committee approved the study and waived the requirement for informed consent due to the retrospective nature of the study. The study complied with the international ethical guidelines for human research, such as the Declaration of Helsinki. The accessed data were anonymized.
Conflicts of interests: All authors declared no conflicts of interests.
Contributors: HH conceived the study, designed the trial, and obtained research funding. HH and JYJ supervised the conduct of the data collection from the database, and managed the data, including quality control. HH and NY provided statistical advice on study design and analyzed the data. All the authors drafted the manuscript, and contributed substantially to its revision.
All the supplementary files in this paper are available at http://wjem.com.cn.
REFERENCES
- 1.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315(8):801–10. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vincent JL, Marshall JC, Namendys-Silva SA, François B, Martin-Loeches I, Lipman J, et al. Assessment of the worldwide burden of critical illness:the intensive care over nations (ICON) audit. Lancet Respir Med. 2014;2(5):380–6. doi: 10.1016/S2213-2600(14)70061-X. [DOI] [PubMed] [Google Scholar]
- 3.Fleischmann C, Scherag A, Adhikari NK, Hartog CS, Tsaganos T, Schlattmann P, et al. Assessment of global incidence and mortality of hospital-treated sepsis. Current estimates and limitations. Am J Respir Crit Care Med. 2016;193(3):259–72. doi: 10.1164/rccm.201504-0781OC. [DOI] [PubMed] [Google Scholar]
- 4.Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787–94. doi: 10.1001/jama.2010.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shu E, Ives Tallman C, Frye W, Boyajian JG, Farshidpour L, Young M, et al. Pre-hospital qSOFA as a predictor of sepsis and mortality. Am J Emerg Med. 2019;37(7):1273–8. doi: 10.1016/j.ajem.2018.09.025. [DOI] [PubMed] [Google Scholar]
- 6.Song JU, Sin CK, Park HK, Shim SR, Lee J. Performance of the quick sequential (sepsis-related) organ failure assessment score as a prognostic tool in infected patients outside the intensive care unit:a systematic review and meta-analysis. Crit Care. 2018;22(1):28. doi: 10.1186/s13054-018-1952-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maitra S, Som A, Bhattacharjee S. Accuracy of quick sequential organ failure assessment (qSOFA) score and systemic inflammatory response syndrome (SIRS) criteria for predicting mortality in hospitalized patients with suspected infection:a meta-analysis of observational studies. Clin Microbiol Infect. 2018;24(11):1123–9. doi: 10.1016/j.cmi.2018.03.032. [DOI] [PubMed] [Google Scholar]
- 8.Liu YC, Luo YY, Zhang X, Shou ST, Gao YL, Lu B, et al. Quick sequential organ failure assessment as a prognostic factor for infected patients outside the intensive care unit:a systematic review and meta-analysis. Intern Emerg Med. 2019;14(4):603–15. doi: 10.1007/s11739-019-02036-0. [DOI] [PubMed] [Google Scholar]
- 9.Fernando SM, Tran A, Taljaard M, Cheng W, Rochwerg B, Seely AJE, et al. Prognostic accuracy of the quick sequential organ failure assessment for mortality in patients with suspected infection:a systematic review and meta-analysis. Ann Intern Med. 2018;168(4):266–75. doi: 10.7326/M17-2820. [DOI] [PubMed] [Google Scholar]
- 10.Liu SJ, He CQ, He W, Jiang T. Lactate-enhanced-qSOFA (LqSOFA) score is superior to the other four rapid scoring tools in predicting in-hospital mortality rate of the sepsis patients. Ann Transl Med. 2020;8(16):1013. doi: 10.21037/atm-20-5410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xia YQ, Zou LQ, Li DZ, Qin Q, Hu H, Zhou YW, et al. The ability of an improved qSOFA score to predict acute sepsis severity and prognosis among adult patients. Medicine (Baltimore) 2020;99(5):e18942. doi: 10.1097/MD.0000000000018942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guarino M, Gambuti E, Alfano F, de Giorgi A, Maietti E, Strada A, et al. Predicting in-hospital mortality for sepsis:a comparison between qSOFA and modified qSOFA in a 2-year single-centre retrospective analysis. Eur J Clin Microbiol Infect Dis. 2021;40(4):825–31. doi: 10.1007/s10096-020-04086-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hu H, Yao N, Qiu YR. Predictive value of 5 early warning scores for critical COVID-19 patients. Disaster Med Public Health Prep. 2020:1–8. doi: 10.1017/dmp.2020.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves:a nonparametric approach. Biometrics. 1988;44(3):837–45. [PubMed] [Google Scholar]
- 15.Waligora G, Gaddis G, Church A, Mills L. Rapid systematic review:the appropriate use of quick sequential organ failure assessment (qSOFA) in the emergency department. J Emerg Med. 2020;59(6):977–83. doi: 10.1016/j.jemermed.2020.06.043. [DOI] [PubMed] [Google Scholar]
- 16.Perman SM, Mikkelsen ME, Goyal M, Ginde A, Bhardwaj A, Drumheller B, et al. The sensitivity of qSOFA calculated at triage and during emergency department treatment to rapidly identify sepsis patients. Sci Rep. 2020;10(1):20395. doi: 10.1038/s41598-020-77438-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hwang SY, Jo IJ, Lee SU, Lee TR, Yoon H, Cha WC, et al. Low accuracy of positive qSOFA criteria for predicting 28-day mortality in critically ill septic patients during the early period after emergency department presentation. Ann Emerg Med. 2018;71(1):1–9.e2. doi: 10.1016/j.annemergmed.2017.05.022. [DOI] [PubMed] [Google Scholar]
- 18.Moskowitz A, Patel PV, Grossestreuer AV, Chase M, Shapiro NI, Berg K, et al. Quick sequential organ failure assessment and systemic inflammatory response syndrome criteria as predictors of critical care intervention among patients with suspected infection. Crit Care Med. 2017;45(11):1813–9. doi: 10.1097/CCM.0000000000002622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Askim Å, Moser F, Gustad LT, Stene H, Gundersen M, Åsvold BO, et al. Poor performance of quick-SOFA (qSOFA) score in predicting severe sepsis and mortality - a prospective study of patients admitted with infection to the emergency department. Scand J Trauma Resusc Emerg Med. 2017;25(1):56. doi: 10.1186/s13049-017-0399-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huson MA, Kalkman R, Grobusch MP, van der Poll T. Predictive value of the qSOFA score in patients with suspected infection in a resource limited setting in Gabon. Travel Med Infect Dis. 2017;15:76–7. doi: 10.1016/j.tmaid.2016.10.014. [DOI] [PubMed] [Google Scholar]
- 21.Donnelly JP, Safford MM, Shapiro NI, Baddley JW, Wang HE. Application of the Third International Consensus Definitions for Sepsis (Sepsis-3) Classification:a retrospective population-based cohort study. Lancet Infect Dis. 2017;17(6):661–70. doi: 10.1016/S1473-3099(17)30117-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Forward E, Konecny P, Burston J, Adhikari S, Doolan H, Jensen T. Predictive validity of the qSOFA criteria for sepsis in non-ICU inpatients. Intensive Care Med. 2017;43(6):945–6. doi: 10.1007/s00134-017-4776-2. [DOI] [PubMed] [Google Scholar]
- 23.Oduncu AF, Kıyan GS, Yalçınlı S. Comparison of qSOFA, SIRS, and NEWS scoring systems for diagnosis, mortality, and morbidity of sepsis in emergency department. Am J Emerg Med. 2021;48:54–9. doi: 10.1016/j.ajem.2021.04.006. [DOI] [PubMed] [Google Scholar]
- 24.Goulden R, Hoyle MC, Monis J, Railton D, Riley V, Martin P, et al. qSOFA, SIRS and NEWS for predicting inhospital mortality and ICU admission in emergency admissions treated as sepsis. Emerg Med J. 2018;35(6):345–9. doi: 10.1136/emermed-2017-207120. [DOI] [PubMed] [Google Scholar]
- 25.Cecconi M, Evans L, Levy M, Rhodes A. Sepsis and septic shock. Lancet. 2018;392(10141):75–87. doi: 10.1016/S0140-6736(18)30696-2. [DOI] [PubMed] [Google Scholar]
- 26.Vincent JL, Quintairos E, Silva A, Couto L, Jr, Taccone FS. The value of blood lactate kinetics in critically ill patients:a systematic review. Crit Care. 2016;20(1):257. doi: 10.1186/s13054-016-1403-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khodashahi R, Sarjamee S. Early lactate area scores and serial blood lactate levels as prognostic markers for patients with septic shock:a systematic review. Infect Dis (Lond) 2020;52(7):451–63. doi: 10.1080/23744235.2020.1749298. [DOI] [PubMed] [Google Scholar]
- 28.Baumann BM, Greenwood JC, Lewis K, Nuckton TJ, Darger B, Shofer FS, et al. Combining qSOFA criteria with initial lactate levels:Improved screening of septic patients for critical illness. Am J Emerg Med. 2020;38(5):883–9. doi: 10.1016/j.ajem.2019.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Sinto R, Suwarto S, Lie KC, Harimurti K, Widodo D, Pohan HT. Prognostic accuracy of the quick Sequential Organ Failure Assessment (qSOFA)-lactate criteria for mortality in adults with suspected bacterial infection in the emergency department of a hospital with limited resources. Emerg Med J. 2020;37(6):363–9. doi: 10.1136/emermed-2018-208361. [DOI] [PubMed] [Google Scholar]
- 30.Leopold SJ, Ghose A, Plewes KA, Mazumder S, Pisani L, Kingston HWF, et al. Point-of-care lung ultrasound for the detection of pulmonary manifestations of malaria and sepsis:an observational study. PLoS One. 2018;13(12):e0204832. doi: 10.1371/journal.pone.0204832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rice TW, Wheeler AP, Bernard GR, Hayden DL, Schoenfeld DA, Ware LB, et al. Comparison of the SpO2/FiO2 ratio and the PaO2/FiO2 ratio in patients with acute lung injury or ARDS. Chest. 2007;132(2):410–7. doi: 10.1378/chest.07-0617. [DOI] [PubMed] [Google Scholar]
- 32.Pepper DJ, Sun JF, Rhee C, Welsh J, Powers JH, 3rd, Danner RL, et al. Procalcitonin-guided antibiotic discontinuation and mortality in critically ill adults:a systematic review and meta-analysis. Chest. 2019;155(6):1109–18. doi: 10.1016/j.chest.2018.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Robati Anaraki M, Nouri-Vaskeh M, Abdoli Oskouie S. Effectiveness of procalcitonin-guided antibiotic therapy to shorten treatment duration in critically-ill patients with bloodstream infections:a systematic review and meta-analysis. Infez Med. 2020;28(1):37–46. [PubMed] [Google Scholar]
- 34.Liu D, Su LX, Han GC, Yan P, Xie LX. Prognostic value of procalcitonin in adult patients with sepsis:a systematic review and meta-analysis. PLoS One. 2015;10(6):e0129450. doi: 10.1371/journal.pone.0129450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.AlRawahi AN, AlHinai FA, Doig CJ, Ball CG, Dixon E, Xiao ZW, et al. The prognostic value of serum procalcitonin measurements in critically injured patients:a systematic review. Crit Care. 2019;23:390. doi: 10.1186/s13054-019-2669-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


