Abstract
Severe cognitive impairments and cognitive distortions are core to schizophrenia-spectrum disorders (SSDs) and are associated with deteriorated social functioning. Despite well-established efficacy of group psychosocial therapies targeting cognitive health in SSDs, dissemination of these programs remains limited. Remote delivery offers a promising strategy for increasing the programs' accessibility. Yet, little research has evaluated group therapies for cognitive health delivered in this way. Thus, we aimed to assess, from participants' and therapists' perspectives, the feasibility, acceptability, as well as levels and process of engagement in a videoconference delivery of group psychosocial therapies for SSD patients' cognitive health. Participants, outpatients, attended Action Based Cognitive Remediation or Metacognitive Training, both adapted for videoconference. Then, participants and therapists completed post-therapy questionnaires. Of the 28 participants attending at least one session, 75% completed more than half of sessions and seven dropped out. Technology did not appear to significantly hinder participation in the programs. All completing participants reported a positive experience with therapy, 67% were not bothered by the distance from the therapist, and 77% trusted that the information shared was kept confidential. Therapist-rated levels of attention M = 7.5/9 (SD = 1.04), participation M = 6.91/9 (SD = 1.32), and social interactions M = 5.31/9 (SD = 1.96) were satisfactory. Nonetheless, participants indicated that they would have appreciated more social interactions with group members. These positive results validate the earliest stage in the implementation process for remote group therapies targeting cognitive health in SSDs. Remote delivery promises to improve access to therapies targeting cognitive health and, ultimately, facilitate functional recovery for SSD patients.
Keywords: Cognitive remediation, Psychosis, Metacognition, Videoconferencing, Digital mental health, Digital implementation
1. Introduction
Schizophrenia-spectrum disorders (SSDs) are some of the most debilitating mental disorders, imposing tremendous burdens on patients, their families, and communities (Chong et al., 2016; Goeree et al., 2005). Symptom relapses and deteriorations in social functioning are common in SSDs (Carpenter and Strauss, 1991; Leucht et al., 2003). Moreover, most with an SSD show substantial cognitive impairments like difficulties in verbal memory, executive functions, and attention (Schaefer et al., 2013). Additionally, cognitive distortions present in psychosis regularly result in biases and errors in reasoning, as well as misinterpretations when processing information (Dudley et al., 2016; Moritz and Woodward, 2005; Ross et al., 2015). These cognitive impairments and distortions are core SSD elements, adversely impacting clinical symptoms (Bell et al., 2006) and functioning (Lepage et al., 2014; Sauvé et al., 2020; Sheffield et al., 2018).
Currently, no pharmacotherapy reliably improves cognitive health for people with SSDs (for review see Harvey, 2009; Nielsen et al., 2015; Sheffield et al., 2018). Given its importance in outcomes, several psychosocial therapies targeting cognitive health have been developed. Cognitive Remediation, a group of interventions using cognitive exercises to improve cognitive health and functional outcomes (Bowie et al., 2020), is one example. Related psychosocial group therapies, Action Based Cognitive Remediation (ABCR; Bowie, 2018) and Metacognitive Training (MCT; Moritz and Woodward, 2007) are feasible, acceptable (Bowie et al., 2017; Eichner and Berna, 2016), and effective for improving cognitive health and general functioning when delivered in-person (Bowie et al., 2017, Eichner and Berna, 2016, Lejeune et al., 2021, Penney et al., 2021, Philipp et al., 2019, Vita et al., 2021). Note that feasibility is the capacity of patients to participate in therapy and that of therapists to administer therapy (Proctor et al., 2011). Acceptability is the subjective impressions of the therapy, i.e., satisfaction and believed appropriateness (Bowen et al., 2009; Proctor et al., 2011). Despite reliable effectiveness, these interventions are not yet widely implemented in clinical settings.
Implementing group psychosocial therapies for cognitive health remotely is promising, remote therapy may reach people unwilling to attend in-person therapy, and/or those in isolated areas (Gentry et al., 2019; Lecomte et al., 2020). However, little is known about the feasibility or acceptability of remote group therapies for cognitive health in SSD patients. Preliminary work on related remote therapies has evaluated either individual therapies targeting cognitive health (reviewed by Best, 2020), therapies targeting cognitive health using a combination of in-person groups and individual online homework (Medalia et al., 2021), or group therapies not specifically targeting cognitive health (Cognitive Behavioural Therapy for psychosis: Lecomte et al., 2020, Acceptance and Commitment Therapy: Wood et al., 2020). Generally, these studies have found the programs feasible, acceptable, and as efficacious as in-person; similar to what has been found with other populations (see Gentry et al., 2019). However, Medalia et al. (2021) reported that technological access and abilities were lacking in the SSD population, considerably hindering the feasibility of remote therapy. Another potential concern of the remote setting is engagement, the extent to which participants get involved in therapy (by participating, being attentive, interacting with others; Tetley et al., 2011). Engagement is important to consider as it may be hindered in remote settings (Casey and Clough, 2016), and since engagement predicts treatment gains (Barrett et al., 2008; Best et al., 2020; Tetley et al., 2011).
As few studies have assessed remote group therapies targeting cognitive health in the SSD population, we aimed to evaluate, from participants' and therapists' perspectives, the feasibility, acceptability, as well as levels and process of engagement in a videoconference delivery of ABCR and MCT. This investigation is a crucial first step in implementating remote group therapies for SSD patients' cognitive health (Bowen et al., 2009; Pearson et al., 2020; Proctor et al., 2011).
2. Methods
2.1. Participants & procedure
Criteria for participation included being 18 years or older, speak English or French, and be an outpatient followed/treated for a psychotic disorder at a psychiatric hospital. Participants were required to provide an emergency contact and their primary clinician must have considered them symptomatically stable, able to participate in group therapy, able to access and use digital technology, and have access to a private space. Exclusion criteria included current hospitalization, having an intellectual disability, a history of brain trauma, or a neurological disorder. To improve the generalizability of therapists' feedback, eight therapists were involved in this project (for therapist characteristics, see Table 1; for characteristics by therapy group see supplemental Table S1). No therapist administered both ABCR and MCT.
Table 1.
Therapist characteristics.
| Characteristic | Overall (n = 8) |
|---|---|
| Sex (male/female) | 3/5 |
| First time group therapy (n) | 50% |
| Education (n) | |
| MD and/or PhD | 4 |
| PhD candidate | 1 |
| M.Sc. candidate | 1 |
| B.A./B.Sc. candidate | 2 |
This article presents data from the initial stages of a pragmatic trial regarding the implementation and efficacy of remotely delivered group therapies for cognitive health in SSDs. Reported here are feedback from participants and therapists regarding feasibility, acceptability, and engagement (measures described below). Assessments were completed remotely via teleconferencing or internet questionnaires (using Zoom for Healthcare™ or Castor electronic data capture™, respectively). Participants were compensated with a $25 gift card upon completing each evaluation (see supplemental Fig. S1 for study timeline). Efficacy data from this study are beyond the scope of this article.
2.2. Group therapies targeting cognitive health
After pre-therapy assessments, participants chose between ABCR and MCT, both delivered via videoconference (Zoom for Healthcare™). ABCR, developed by Bowie et al. (2017), targets neurocognitive performance with computerized cognitive exercises, therapist led-group discussions to develop problem-solving strategies, and role-plays to apply cognitive skills and strategies to daily life (for meta-analyses of cognitive remediation see Vita et al., 2021). Note that in adapting for remote delivery, ABCR's role-plays were modified, and some were replaced with group discussions. MCT, developed by Moritz and Woodward (2007), targets cognitive biases (e.g., jumping to conclusions, bias against disconfirmatory evidence) via psychoeducation and group exercises to foster reflections about how participants come to conclusions and integrate new information (for narrative review see Moritz et al., 2014, meta-analyses: Penney et al., 2021, Philipp et al., 2019, Sauvé et al., 2020). Robust evidence supports both programs' efficacy. Sessions occurred twice a week. ABCR sessions lasted 90 min for seven to 8 weeks (14 to 16 sessions, see supplement). MCT sessions lasted 45–60 min for 6 weeks (10 sessions plus introduction and conclusion sessions). If desired, participants could take part in both interventions successively; only data from the first intervention were analyzed. In addition to research participants, 18 patients attended one of the therapy programs offered by this project without consenting to participate in research. Homework exercises were assigned in both programs but were not required.
As suggested by an expert working group (Bowie et al., 2020), both programs were administered by two trained clinicians—including at least one licensed neuropsychologist—and included cognitive exercises, procedures to develop problem-solving strategies, and procedures to promote transfer to real-world functioning. To facilitate attention and foster engagement in the remote setting, feedback from previous cohorts was considered and slight changes were made to the presentation's style and the groups' administration. To keep content nearly identical to that of the respective therapy manuals, changes were made in concert with some of their developers (ABCR: C. R. Bowie; MCT: M. Menon; see Appendix I in supplemental materials for summary of changes).
2.3. Measures
2.3.1. Participants
2.3.1.1. Symptoms, functioning & cognition
The Positive and Negative Syndrome Scale 6 (PANSS-6; DeVriendt et al., 1990, Ostergaard et al., 2016) and the Personal and Social Performance scale (PSP; Morosini et al., 2000), were used to assess SSD symptoms and general functioning, respectively; both measures are clinician-rated. The Cambridge Neuropsychological Test Automated Battery (CANTAB), completed online, was used to measure spatial working memory (SWMBE468), executive functions (OTSPFC), and attention (RVPA'; see Backx et al., 2020). The California Verbal Learning Test II (CVLT-II) measured verbal memory (Woods et al., 2006; Thiruselvam and Hoelzle, 2020). All cognitive measurements were age and sex standardized. Diagnoses, age at onset, duration of illness, and medication information were retrieved from consenting participants' medical charts.
2.3.1.2. Feasibility & acceptability
The number of completers, the percentage of sessions attended, and the number of dropouts—including, when available, reasons for discontinuing therapy—were used as measures of feasibility. Participants completing more than 50% of therapy sessions were considered completers. Dropouts were those who attended at least one session but fewer than half of sessions (as in Bowie et al., 2017, Connell et al., 2006).
The Acceptability, Usability, Safety, and Impact Questionnaire (adapted from Alvarez-Jimenez et al., 2013) consists of 18 items regarding participants' experiences with the therapy; each item rated from one (strongly disagree) to five (strongly agree). This questionnaire also includes an open-ended item regarding factors that would potentially facilitate interest in therapy. The Satisfaction with Therapy Questionnaire (STQ) assessed acceptability with five subsections: 1) Expectations and perceptions of progress made during therapy; 2) Beliefs of the extent to which they gained cognitive behavioural therapy skills and knowledge from the therapy; 3) Perception of the usefulness of homework; 4) Ratings of therapists' attributes; and 5) Satisfaction with therapy (Lawlor et al., 2017). Each item is rated on a five-point Likert scale (higher scores reflecting a better evaluation of therapy); each sections' items are averaged representing subscores.
2.3.1.3. Engagement
Therapists, after every session, and for each participant in attendance, rated participant's levels of attention, participation, and social interactions in therapy. Each type of engagement was rated from one to nine; higher scores indicate more engagement (see Appendix II in supplemental materials). Scores were averaged across sessions then across participants. The eTherapy Attitudes and Process questionnaire (eTAP; Clough et al., 2019a) assessed participants' process of engagement in the remote therapy. The questionnaire, based on the Theory of Planned Behavior (Ajzen, 1991), measures: perceived behavioural control; behavioural intentions; attitudes towards engaging in remote therapy (behavioural attitudes); and the perceived social pressure to—or not to—engage with therapy (subjective norm). Each construct contains four items rated on a seven-point Likert scale (“strongly disagree” to “strongly agree”); each construct's items are averaged for a subscore. In theory, higher scores indicate a higher likelihood of engaging in therapy.
2.3.2. Therapists
2.3.2.1. Feasibility, acceptability & engagement
Therapists completed the Feasibility of Intervention Measure, the Acceptability of Intervention Measure, and the Intervention Appropriateness Measure (Weiner et al., 2017). Each of these measures includes four items rated on a five-point Likert scale from “completely disagree” to “completely agree.” Each measure's items were averaged, for the measure's total score. Therapists also completed a Therapist's Questionnaire developed for this study by an experienced psychiatrist/psychologist (DRC) based on the Theoretical Domains Framework—a framework for the implementation of psychosocial therapies (Atkins et al., 2017; Birken et al., 2017; Huijg et al., 2014). This questionnaire consists of eight items rated on a five-point Likert scale, assessing the feasibility and acceptability of the therapies from the therapist's perspectives. Lastly, the eTherapy Attitudes and Process questionnaire Therapist version (eTAP-T; Clough et al., 2019b) assessed the therapist's process of engagement in therapy. This questionnaire measures domains identical to eTAP (above).
2.4. Analyses
Participant and therapist responses were analyzed using descriptive statistics. Responses to the open-ended question were grouped and related to domains relevant to the implementation of remote psychosocial interventions (Bell et al., 2020; Borghouts et al., 2021). Chi-squared statistics and Mann–Whitney–Wilcoxon ranked tests were used as appropriate to compare groups. Spearman rank correlations were conducted between baseline cognition and measures of engagement as such associations have been previously discussed (Best et al., 2020; Bonnín et al., 2021; Thomas et al., 2018).
3. Results
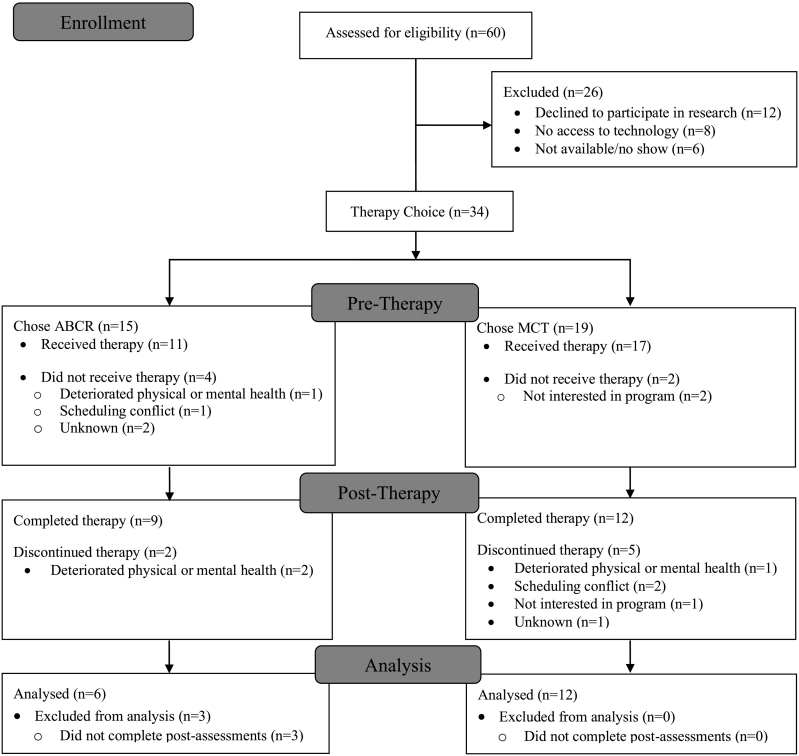
Twenty-eight participants attended at least one therapy session, see Fig. 1 for CONSORT diagram (Moher et al., 2001). Table 2 shows participants' pre-therapy characteristics: participants were symptomatically stable (PANSS-6: M = 13.2, SD = 4.4) and had marked difficulties in at least one functioning domain (PSP: M = 52.2, SD = 17.0). Dropouts had a lower age of onset (U(19,7) = 104, p = .03). For baseline characteristics by therapy condition and completion status, see supplemental Tables S2–S3. Results from both ABCR and MCT are described together as these groups did not differ on measures of feasibility, acceptability, or engagement outcomes (see supplemental Tables S4–S10 and Figs. S2–S3). All eight therapists completed questionnaires.
Fig. 1.
CONSORT flow diagram.
Table 2.
Pre-therapy participant characteristics.
| Baseline characteristic | Completers (n = 21) | Dropouts (n = 7) |
|---|---|---|
| Sex: (male/female) | 12/9 | 3/4 |
| Age: M (SD) | 33.9 (11.8) | 27.1 (5.9) |
| Age of onset: M (SD) | 27.5 (6.7)‡ | 19.0 (8.9)⁎ |
| Duration of illness: M (SD) | 7.8 (9.9)‡ | 8.0 (6.9) |
| Chlorpromazine equivalents (mg): M (SD) | 520.0 (483.0)a | 354.0 (140.1)b, † |
| PANSS-6: M (SD) | 13.8 (4.2) | 11.3 (4.6) |
| PSP: M (SD) | 49.1 (15.7) | 61.4 (18.8) |
| CANTAB RVPA′: M (SD) | −0.6 (0.8)ζ | −0.2 (0.5)‡ |
| CANTAB SWMBE468: M (SD) | 0.1 (1.6)ζ | −0.4 (1.9)‡ |
| CANTAB OTSPSFC: M (SD) | 0.4 (1.1)ζ | −1.0 (1.3)‡ |
| CVLT-II Trial 5: M (SD) | −0.9 (1.4) | 0.1 (0.4) |
| Diagnoses: (n) | ||
| Schizophrenia | 5 | 2 |
| Schizoaffective disorder | 4 | 2 |
| Delusional disorder | – | 1 |
| Dissociative disorder | 1 | – |
| Mood disorder with psychotic features | 5 | – |
| Other specified SSD | 1 | – |
| Unspecified SSD | 4 | 2 |
| Undiagnosed, high risk for psychosis | 1 | – |
Note. PANSS-6: Positive and Negative Syndrome Scale-6 item. PSP: Personal and Social Performance scale. CANTAB: Cambridge Neuropsychological Test Automated Batteries; RVPA′: Rapid Visual Information Processing task A′, measure of sustained attention; SWMBE468: Spatial Working Memory task: Between errors 468, a measure of spatial working memory; OTSPSFC: One Touch Stockings task: problem solved on first choice, a measure of executive functions including reasoning and problem solving; CVLT-II: California Verbal Learning Test II. All cognitive measures standardized considering age and sex. SSD: schizophrenia-spectrum disorder.
See Supplemental Table S2–S3 for breakdown by therapy group.
indicates p < .05.
One missing result.
Two missing results.
Six missing results.
Four participants not on antipsychotics.
Two participants not on antipsychotics.
3.1. Participants
3.1.1. Feasibility & acceptability
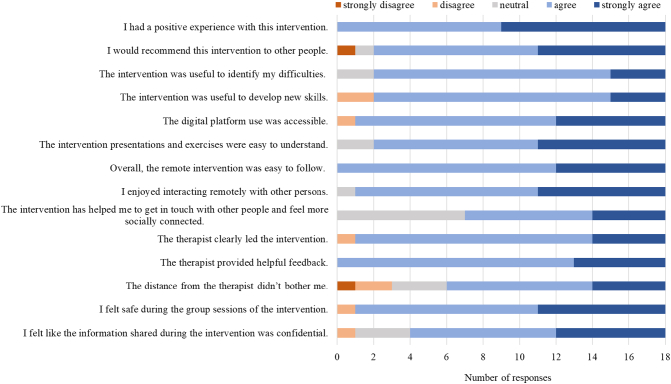
Twenty-one participants (75%) completed therapy and seven (25%) dropped out. On average, completers attended 79% of therapy sessions. Fig. 2 shows results for the Acceptability, Usability, Safety, and Impact Questionnaire. Notably, all participants reported having a positive experience with therapy and most (67%) were not bothered by the distance with the therapist. When asked what factors would facilitate interest in these therapies, the most frequent responses were more social interactions (e.g., getting to know other group members better, in-person meetings; 12%); a willingness to learn (12%); therapist training and positive therapist characteristics (e.g., compassion; 9%); holding sessions in the evening (6%); encouraging and congratulating participants (6%); and financial help (e.g., for internet; 6%; see supplement for complete data). On the STQ, participants rated therapist attributes at M = 4.64/5 (SD = 0.37); overall satisfaction M = 4.44/5 (SD = 0.62); expectation and perception of progress M = 4.33/5 (SD = 0.36); usefulness of homework M = 4.33/5 (SD = 0.59); and the extent to which they gained cognitive behavioural therapy skills/knowledge M = 3.53/5 (SD = 0.56).
Fig. 2.
Acceptability, Usability, Safety, and Impact Questionnaire responses.
3.1.2. Engagement
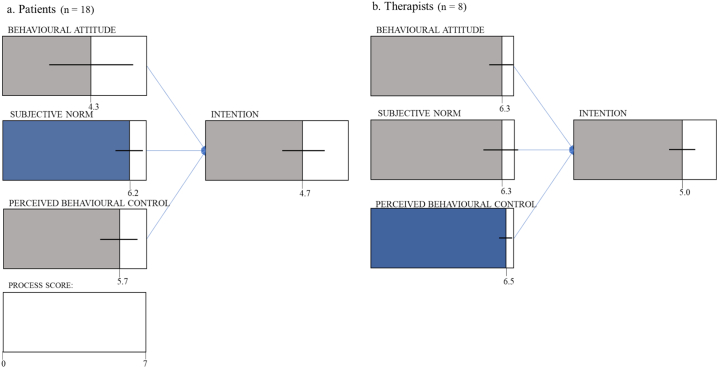
As rated by clinicians, engagement during therapy sessions was generally high: attention M = 7.57/9 (SD = 1.04), participation M = 6.91/9 (SD = 1.32), with social interactions rated somewhat lower M = 5.31/9 (SD = 1.96). Regarding participants' processes of engagement, depicted in Fig. 3a, subjective norms were rated highest M = 6.21/7 (SD = 0.67) and behavioural attitudes rated lowest M = 4.33/7 (SD = 2.05). No correlations between baseline cognitive measures and engagement scores were significant when controlling for multiple comparisons (see supplemental Table S11).
Fig. 3.
e-Therapy Attitudes and Process Questionnaire (eTAP) results.
Note. a: Participants' engagement processes. b: Therapists' process of engagement. Numbers indicate mean scores, domain with highest average indicated in blue. Standard deviation represented with horizontal lines. Adapted from Ajzen, 1991.
3.2. Therapists
3.2.1. Feasibility, acceptability & engagement
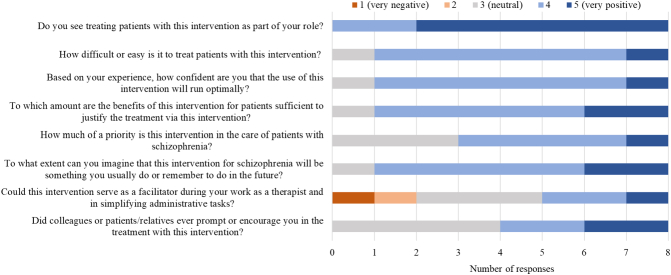
Therapists rated these remote group therapies highly for the feasibility of intervention M = 4.81/5 (SD = 0.29), acceptability of intervention M = 4.69/5 (SD = 0.42), and appropriateness of the intervention M = 4.41/5 (SD = 0.48). As Fig. 4 illustrates, the therapist questionnaire results were similarly as positive. Moreover, therapists reported that the ability to encourage participants to complete exercises and experience using videoconferencing was helpful. Regarding processes of engagement, therapists rated all processes highly: perceived behavioural control was highest M = 5.68/7 (SD = 0.91) and intention of engaging with therapy was lowest M = 4.74/7 (SD = 1.04), see Fig. 3b. Results of therapist feedback by program administered are reported in supplemental Figs. S4–S5 and Tables S12–S14.
Fig. 4.
Therapist questionnaire responses.
4. Discussion
This preliminary study suggests that remote group therapies targeting cognitive health in SSDs are feasible and acceptable for participants and therapists. Levels of engagement were also satisfactory in this remote group setting. Participant feedback indicated that increased social interactions with the group members would be appreciated. Despite differences in therapeutic activities, ABCR and MCT did not appear to differ on feasibility, acceptability, nor engagement. Thus, our results suggest that various therapies for SSD patients' cognitive health can be feasible, acceptable, and engaging when delivered remotely.
The feasibility of these therapies was clearly established. Attendance and dropout rates were in line with those found for in-person therapy (e.g., Bowie et al., 2017; Eichner and Berna, 2016). Many reasons for dropping out have been previously reported in studies of in-person therapies (e.g., Jensen et al., 2014) and, therefore, are not inherently linked to technology. Further, while access to technology was a prerequisite for participation in this study, only eight patients of the 60 assessed were excluded for that reason. Indeed, a significant portion of patients appear to have the required technological access and ability to join, participate, and benefit from remote group therapies; a conclusion supported by previous reports (e.g., Lal et al., 2015; Miu et al., 2020; Wood et al., 2020; Young et al., 2020) and a systematic review and meta-analysis by Firth et al. (2016). While access to technology did not significantly hinder the feasibility of our study of therapies for SSD patient's cognitive health, this was not the case for a previous study by Medalia et al. (2021). Three characteristics of the present study may explain the difference between our conclusions and those of Medalia et al. (2021). Firstly, Medalia et al. (2021)'s sample appears older than ours. Older age has been associated with less access to technology (Firth et al., 2016; Young et al., 2020). Regarding technological ability, while some participants in our study required technological assistance from therapists, no technological problems impeded participants from completing therapy. Second, in the present study, participants successfully attended and completed videoconference therapy and its activities from a computer or smartphone; Medalia et al. (2021)'s study appears to have required access to a computer. Perhaps smartphones are more accessible than laptop or desktop computers, and therefore, improve feasibility of remote therapies (in line with Torous and Keshavan, 2020, Young et al., 2020). While it is plausible that the effectiveness of remote therapy is moderated by the type of technological device used, this remains an open question. Third, it is possible that access to technology differs for SSD populations in Canada and in the United States of America. Lal et al. (2015), surveying from the same pool of Canadian patients as those recruited for this study, found that the majority had access to a laptop device (70% of their 67 participants), a desktop at home (52%), and at least 44% had access to a smartphone. This latter result is higher than the 35% of psychosis patients with smartphone access reported by Firth et al. (2016)'s review, despite being reported in similar years. Ultimately, the differences between our findings and those of Medalia et al. (2021)’s suggest that feasibility of remote therapies for cognition in the SSD population may depend on participant characteristics, the remote programs' technical requirements, and the country.
Participants' feedback regarding these remote therapies was very positive: most were not bothered by the distance from the therapists and would recommend the therapy to others. This feedback resembles that of the homologous in-person group therapies (Eichner and Berna, 2016). Moreover, we found that group cohesiveness—a key element of group therapy (Lecomte et al., 2016)—could be retained in the remote group setting: most participants felt like the information shared in the remote group remained confidential, with many sharing personal and private experiences in the group. Similarly, therapists found these remote group therapies acceptable, believing them to be useful and important for patients. Such positive impressions are crucial for the implementation and further development of such programs (Atkins et al., 2017; Stirman et al., 2016).
Participants were attentive, participated well, and enjoyed many social interactions during these remote therapies. In line with past findings, we did not find statistically significant associations between baseline cognition and measures of engagement (Bonnín et al., 2021). To improve engagement, it is important to explore how participants' beliefs regarding therapy can be improved—this process of engagement was rated lowest by participants. Though the non-specific nature of group therapies may dampen beliefs of personal benefits, emphasizing links between therapy and everyday life may improve these beliefs (Bowie et al., 2020). The participants' and therapists' processes of engagement appeared to be different, the perceptions of both groups should be kept in mind when implementing remote therapies for cognitive health.
The results strongly suggest that participants would appreciate more social interactions with the group members: quantitative responses regarding social interactions were often more ambiguous than other responses (e.g., feelings of social connectedness) and social interactions were a common theme when asked what might facilitate interest in these therapies. Previous studies of remote group therapies in this population and others have reported similarly (Gentry et al., 2019, Wood et al., 2020, for suggestions regarding adaptations for the remote setting see Dark et al., 2021). It is worth considering how to foster social interactions in a remote group setting, particularly as increased group cohesion improves engagement in remote therapies (Borghouts et al., 2021). Further, while the digital medium places different constraints on social interactions, it may also provide new opportunities for promoting interactions (e.g., breakout rooms, instant messages, additional co-therapists, addition of ice-breaker activities, see Appendix I in supplement for our list of changes).
4.1. Limitations
The small sample is the chief limitation of this study; a limitation inherent to preliminary studies like these (e.g., Lecomte et al., 2020; Wood et al., 2020). To use our small sample optimally, we combined therapy programs when interpreting our results. While specific therapy programs may differ on feasibility, acceptability and engagement, our supplemental analyses did not reveal considerable differences between therapy groups on these outcomes. Additional data would strengthen inferences. Second, no comparisons to in-person group programs were conducted in this study. Besides the difficulty of such groups in the context of COVID-19 health restrictions, the broader study that this article reports on was designed to address the implementation and dissemination of these group therapies; comparison to in-person therapies was beyond the study's scope. Thirdly, most of the therapists involved in this study have research interests and may not properly represent those working as full-time clinicians. This may explain, for example, why therapists rated eTAP-T's intention process of engagement as lowest: these therapists may not intend on administering these therapies regularly simply due to their professional interests. This result may say little about the remote therapies themselves. Studies involving more full-time clinicians would help with generalizations to purely clinical settings. Fourthly, the therapist-rated engagement scales have yet to be validated, limiting the interpretation of these scores. However, this clinical tool is based on precise scoring criteria, was developed by group therapists at the Douglas Mental Health University Institute and remains in use for clinical group settings.
5. Conclusion
This preliminary study validates the earliest stage of the implementation process for remote group therapies targeting cognitive health in SSD. In addition to assessing the effectiveness of these remote group therapies, with consideration to the type of technological device used, future work should include larger samples with diverse clinical teams. Further, adapting these therapies for the remote group setting—paying special attention to improving social interactions—is warranted. This work is likely to ensure SSD patients' access to therapies for cognitive health, ultimately facilitating functional recovery.
Ethical approval
This study was approved by the Douglas Mental Health University Institute Research Ethics Board (IUSMD-20-25).
Funding sources
A Knowledge Mobilization grant (3c-KM-56) from Healthy Brains Healthy Lives supported this study. ML is supported by a James McGill Professorship. KL is supported by a Mitacs accelerate fellowship. ÉT is supported by a Canadian Institutes of Health Research postdoctoral fellowship (#171198).
CRediT authorship contribution statement
Daniel Mendelson: Methodology, Validation, Formal analysis, Investigation, Data Curation, Writing-Original draft preparation, Writing - Review & Editing, Visualization. Élisabeth Thibaudeau: Writing - Review & Editing, Data Curation, Investigation, Supervision. Geneviève Sauvé: Conceptualization, Writing - Review & Editing, Data Curation, Funding acquisition. Katie Lavigne: Conceptualization, Resources, Funding acquisition, Writing - Review & Editing. Christopher R. Bowie: Conceptualization, Resources, Funding acquisition, Writing - Review & Editing. Todd S. Woodward: Conceptualization, Funding acquisition, Writing - Review & Editing. Mahesh Menon: Conceptualization, Resources, Funding acquisition, Writing - Review & Editing. Martin Lepage: Conceptualization, Methodology, Resources, Writing - Review & Editing, Supervision, Funding acquisition. Delphine Raucher-Chéné: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Data Curation, Writing - Review & Editing, Visualization, Supervision, Project administration, Funding acquisition.
Declaration of competing interest
The authors have declared no conflicts of interest regarding this study. ML reports grants from Otsuka Lundbeck Alliance, diaMentis, personal fees from Otsuka Canada, personal fees from Lundbeck Canada, grants and personal fees from Janssen, and personal fees from MedAvante-Prophase, outside of the submitted work. CRB reports grants from Lundbeck, Takeda, and diaMentis, outside of the submitted work.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.scog.2021.100230.
Appendix A. Supplementary data
Supplementary material
References
- Ajzen I. Organizational Behavior And Human Decision Processes. Vol. 50. 1991. The theory of planned behavior; pp. 179–211. [Google Scholar]
- Alvarez-Jimenez M., Bendall S., Lederman R., Wadley G., Chinnery G., Vargas S., Larkin M., Killackey E., McGorry P.D., Gleeson J.F. On the HORYZON: moderated online social therapy for long-term recovery in first episode psychosis. Schizophr. Res. 2013;143:143–149. doi: 10.1016/j.schres.2012.10.009. [DOI] [PubMed] [Google Scholar]
- Atkins L., Francis J., Islam R., O'Connor D., Patey A., Ivers N., Foy R., Duncan E.M., Colquhoun H., Grimshaw J.M., Lawton R., Michie S. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement. Sci. 2017;12:77. doi: 10.1186/s13012-017-0605-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backx R., Skirrow C., Dente P., Barnett J.H., Cormack F.K. Comparing web-based and lab-based cognitive assessment using the Cambridge neuropsychological test automated battery: a within-subjects counterbalanced study. J. Med. Internet Res. 2020;22 doi: 10.2196/16792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett M.S., Chua W.J., Crits-Christoph P., Gibbons M.B., Casiano D., Thompson D. Early withdrawal from mental health treatment: implications for psychotherapy practice. Psychotherapy (Chic) 2008;45:247–267. doi: 10.1037/0033-3204.45.2.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell I.H., Lim M.H., Thomas N. Elsevier; 2020. The Therapeutic Use of Digital Technologies in Psychosis. A Clinical Introduction to Psychosis. [Google Scholar]
- Bell V., Halligan P.W., Ellis H.D. Explaining delusions: a cognitive perspective. Trends Cogn. Sci. 2006;10:219–226. doi: 10.1016/j.tics.2006.03.004. [DOI] [PubMed] [Google Scholar]
- Best M.W. Canadian Institute of Health Research; 2020. CIHR Knowledge Synthesis: Examining the Efficacy of Evidence-based Psychosocial Interventions for Schizophrenia-spectrum Disorders Delivered Through Virtual Care. [Google Scholar]
- Best M.W., Milanovic M., Tran T., Leung P., Jackowich R., Gauvin S., Leibovitz T., Bowie C.R. Motivation and engagement during cognitive training for schizophrenia spectrum disorders. Schizophr. Res. Cogn. 2020;19 doi: 10.1016/j.scog.2019.100151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birken S.A., Powell B.J., Presseau J., Kirk M.A., Lorencatto F., Gould N.J., Shea C.M., Weiner B.J., Francis J.J., Yu Y., Haines E., Damschroder L.J. Combined use of the consolidated framework for implementation research (CFIR) and the theoretical domains framework (TDF): a systematic review. Implement. Sci. 2017;12:2. doi: 10.1186/s13012-016-0534-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonnín C.D.M., Solé B., Reinares M., García-Estela A., Samalin L., Martínez-Arán A., Sánchez-Moreno J., Colom F., Vieta E., Hidalgo-Mazzei D. Does cognitive impairment in bipolar disorder impact on a SIMPLe app use? J. Affect. Disord. 2021;282:488–494. doi: 10.1016/j.jad.2020.12.168. [DOI] [PubMed] [Google Scholar]
- Borghouts J., Eikey E., Mark G., de Leon C., Schueller S.M., Schneider M., Stadnick N., Zheng K., Mukamel D., Sorkin D.H. Barriers to and facilitators of user engagement with digital mental health interventions: systematic review. J. Med. Internet Res. 2021;23 doi: 10.2196/24387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen D.J., Kreuter M., Spring B., Cofta-Woerpel L., Linnan L., Weiner D., Bakken S., Kaplan C.P., Squiers L., Fabrizio C., Fernandez M. How we design feasibility studies. Am. J. Prev. Med. 2009;36:452–457. doi: 10.1016/j.amepre.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowie C.R. Kingston; Ontario: 2018. Action-based Cognitive Remediation. [Google Scholar]
- Bowie C.R., Bell M.D., Fiszdon J.M., Johannesen J.K., Lindenmayer J.-P., McGurk S.R., Medalia A.A., Penadés R., Saperstein A.M., Twamley E.W., Ueland T., Wykes T. Cognitive remediation for schizophrenia: an expert working group white paper on core techniques. Schizophr. Res. 2020;215:49–53. doi: 10.1016/j.schres.2019.10.047. [DOI] [PubMed] [Google Scholar]
- Bowie C.R., Grossman M., Gupta M., Holshausen K., Best M.W. Action-based cognitive remediation for individuals with serious mental illnesses: effects of real-world simulations and goal setting on functional and vocational outcomes. Psychiatr. Rehab. J. 2017;40:53–60. doi: 10.1037/prj0000189. [DOI] [PubMed] [Google Scholar]
- Carpenter W.T., Jr., Strauss J.S., Jr. The prediction of outcome in schizophrenia. IV: eleven-year follow-up of the Washington IPSS cohort. J. Nerv. Ment. Dis. 1991;179:517–525. doi: 10.1097/00005053-199109000-00001. [DOI] [PubMed] [Google Scholar]
- Casey L., Clough B. In: The Psychology of Social Networking Vol 1: Personal Experience in Online Communities. Riva G., Wiederhold B.K., Cipresso P., editors. Walter de Gruyter GmbH; Germany: 2016. Making and keeping the connection: Improving consumer attitudes and engagement in e-mental health interventions. [Google Scholar]
- Chong H.Y., Teoh S.L., Wu D.B., Kotirum S., Chiou C.F., Chaiyakunapruk N. Global economic burden of schizophrenia: a systematic review. Neuropsychiatr. Dis. Treat. 2016;12:357–373. doi: 10.2147/NDT.S96649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clough B.A., Eigeland J.A., Madden I.R., Rowland D., Casey L.M. Development of the eTAP: a brief measure of attitudes and process in e-interventions for mental health. Internet Interv. 2019;18 doi: 10.1016/j.invent.2019.100256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clough B.A., Rowland D.P., Casey L.M. Development of the eTAP-T: a measure of mental health professionals' attitudes and process towards e-interventions. Internet Interv. 2019;18 doi: 10.1016/j.invent.2019.100288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell J., Grant S., Mullin T. Client initiated termination of therapy at NHS primary care counselling services. Couns. Psychother. Res. 2006;6:60–67. [Google Scholar]
- Dark F., Miles A., Madson K., Strochnetter E. Adapting evidence-based group therapies following COVID-19 restrictions. Australas. Psychiatry. 2021;103985622110404 doi: 10.1177/10398562211040461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devriendt X., Lapierre Y., Kay S.R., Opler L.A., Fiszbein A. 1990. Échelle de syndrome positif et negatif (PANSS): Manuel de cotation (abrégé) [Google Scholar]
- Dudley R., Taylor P., Wickham S., Hutton P. Psychosis, delusions and the "Jumping to Conclusions" reasoning bias: a systematic review and meta-analysis. Schizophr. Bull. 2016;42:652–665. doi: 10.1093/schbul/sbv150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eichner C., Berna F. Acceptance and efficacy of metacognitive training (MCT) on positive symptoms and delusions in patients with schizophrenia: a meta-analysis taking into account important moderators. Schizophr. Bull. 2016;42:952–962. doi: 10.1093/schbul/sbv225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth J., Cotter J., Torous J., Bucci S., Firth J.A., Yung A.R. Mobile phone ownership and endorsement of “mHealth” among people with psychosis: a meta-analysis of cross-sectional studies. Schizophr. Bull. 2016;42:448–455. doi: 10.1093/schbul/sbv132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentry M.T., Lapid M.I., Clark M.M., Rummans T.A. Evidence for telehealth group-based treatment: a systematic review. J. Telemed. Telecare. 2019;25:327–342. doi: 10.1177/1357633X18775855. [DOI] [PubMed] [Google Scholar]
- Goeree R., Farahati F., Burke N., Blackhouse G., O'Reilly D., Pyne J., Tarride J.E. The economic burden of schizophrenia in Canada in 2004. Curr. Med. Res. Opin. 2005;21:2017–2028. doi: 10.1185/030079905X75087. [DOI] [PubMed] [Google Scholar]
- Harvey P.D. Pharmacological cognitive enhancement in schizophrenia. Neuropsychol. Rev. 2009;19:324–335. doi: 10.1007/s11065-009-9103-4. [DOI] [PubMed] [Google Scholar]
- Huijg J.M., Gebhardt W.A., Crone M.R., Dusseldorp E., Presseau J. Discriminant content validity of a theoretical domains framework questionnaire for use in implementation research. Implement. Sci. 2014;9:11. doi: 10.1186/1748-5908-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen H.H., Mortensen E.L., Lotz M. Drop-out from a psychodynamic group psychotherapy outpatient unit. Nord. J. Psychiatry. 2014;68:594–604. doi: 10.3109/08039488.2014.902499. [DOI] [PubMed] [Google Scholar]
- Lal S., Dell'Elce J., Malla A.K. Technology access and use among young adults with a first episode of psychosis. Psychiatr. Serv. 2015;66:764–765. doi: 10.1176/appi.ps.201400580. [DOI] [PubMed] [Google Scholar]
- Lawlor C., Sharma B., Khondoker M., Peters E., Kuipers E., Johns L. Service user satisfaction with cognitive behavioural therapy for psychosis: associations with therapy outcomes and perceptions of the therapist. Br. J. Clin. Psychol. 2017;56:84–102. doi: 10.1111/bjc.12122. [DOI] [PubMed] [Google Scholar]
- Lecomte T., Abdel-Baki A., Francoeur A., Cloutier B., Leboeuf A., Abadie P., Villeneuve M., Guay S. Group therapy via videoconferencing for individuals with early psychosis: a pilot study. Early Interv. Psychiatry. 2020:eip.13099.. doi: 10.1111/eip.13099. [DOI] [PubMed] [Google Scholar]
- Lecomte T., Leclerc C., Wykes T. Oxford University Press; 2016. Essential Elements of Group Therapy. Group CBT for Psychosis. [Google Scholar]
- Lejeune J.A., Northrop A., Kurtz M.M. A meta-analysis of cognitive remediation for schizophrenia: efficacy and the role of participant and treatment factors. Schizophr. Bull. 2021;47:997–1006. doi: 10.1093/schbul/sbab022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lepage M., Bodnar M., Bowie C.R. Neurocognition: clinical and functional outcomes in schizophrenia. Can. J. Psychiatr. 2014;59:5–12. doi: 10.1177/070674371405900103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leucht S., Barnes T.R., Kissling W., Engel R.R., Correll C., Kane J.M. Relapse prevention in schizophrenia with new-generation antipsychotics: a systematic review and exploratory meta-analysis of randomized, controlled trials. Am. J. Psychiatry. 2003;160:1209–1222. doi: 10.1176/appi.ajp.160.7.1209. [DOI] [PubMed] [Google Scholar]
- Medalia A., Saperstein A.M., Stefancic A., Meyler S., Styke S., Qian M., Liu J., Cabassa L.J. Feasibility and acceptability of remotely accessed cognitive remediation for schizophrenia in public health settings. Psychiatry Res. 2021;301 doi: 10.1016/j.psychres.2021.113956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miu A.S., Vo H.T., Palka J.M., Glowacki C.R., Robinson R.J. Teletherapy with serious mental illness populations during COVID-19: telehealth conversion and engagement. Couns. Psychol. Q. 2020:1–18. [Google Scholar]
- Moher D., Schulz K.F., Altman D.G. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet. 2001;357:1191–1194. [PubMed] [Google Scholar]
- Moritz S., Andreou C., Schneider B.C., Wittekind C.E., Menon M., Balzan R.P., Woodward T.S. Sowing the seeds of doubt: a narrative review on metacognitive training in schizophrenia. Clin. Psychol. Rev. 2014;34:358–366. doi: 10.1016/j.cpr.2014.04.004. [DOI] [PubMed] [Google Scholar]
- Moritz S., Woodward T.S. Jumping to conclusions in delusional and non-delusional schizophrenic patients. Br. J. Clin. Psychol. 2005;44:193–207. doi: 10.1348/014466505X35678. [DOI] [PubMed] [Google Scholar]
- Moritz S., Woodward T.S. Metacognitive training for schizophrenia patients (MCT): a pilot study on feasibility, treatment adherence, and subjective efficacy. German Journal of Psychiatry. 2007;10(3):69–78. [Google Scholar]
- Morosini P.L., Magliano L., Brambilla L., Ugolini S., Pioli R. Development, reliability and acceptability of a new version of the DSM-IV Social and Occupational Functioning Assessment Scale (SOFAS) to assess routine social functioning. Acta Psychiatr. Scand. 2000;101:323–329. [PubMed] [Google Scholar]
- Nielsen R.E., Levander S., Kjaersdam Telléus G., Jensen S.O.W., Østergaard Christensen T., Leucht S. Second-generation antipsychotic effect on cognition in patients with schizophrenia-a meta-analysis of randomized clinical trials. Acta Psychiatrica Scandinavica. 2015;131(3):185–196. doi: 10.1111/acps.12374. [DOI] [PubMed] [Google Scholar]
- Ostergaard S.D., Lemming O.M., Mors O., Correll C.U., Bech P. PANSS-6: a brief rating scale for the measurement of severity in schizophrenia. Acta Psychiatr. Scand. 2016;133:436–444. doi: 10.1111/acps.12526. [DOI] [PubMed] [Google Scholar]
- Pearson N., Naylor P.J., Ashe M.C., Fernandez M., Yoong S.L., Wolfenden L. Guidance for conducting feasibility and pilot studies for implementation trials. Pilot Feasibility Stud. 2020;6:167. doi: 10.1186/s40814-020-00634-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penney, D., Sauvé, G., Mendelson, D., Thibaudeau, É., Moritz, S. & Lepage, M. 2021 In preparation. Efficacy, Maintenance Effects, and Moderators of Metacognitive Training (MCT) for Psychosis: A Systematic Review and Meta-analysis. PROSPERO 2021 CRD42021259291 Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021259291.
- Philipp R., Kriston L., Lanio J., Kühne F., Härter M., Moritz S., Meister R. Effectiveness of metacognitive interventions for mental disorders in adults—A systematic review and meta-analysis (METACOG) Clin. Psychol. Psychother. 2019;26:227–240. doi: 10.1002/cpp.2345. [DOI] [PubMed] [Google Scholar]
- Proctor E., Silmere H., Raghavan R., Hovmand P., Aarons G., Bunger A., Griffey R., Hensley M. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Admin. Pol. Ment. Health. 2011;38:65–76. doi: 10.1007/s10488-010-0319-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross R.M., McKay R., Coltheart M., Langdon R. Jumping to conclusions about the beads task? A meta-analysis of delusional ideation and data-gathering. Schizophr. Bull. 2015;41:1183–1191. doi: 10.1093/schbul/sbu187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sauvé G., Lavigne K.M., Pochiet G., Brodeur M.B., Lepage M. Efficacy of psychological interventions targeting cognitive biases in schizophrenia: a systematic review and meta-analysis. Clin. Psychol. Rev. 2020;78 doi: 10.1016/j.cpr.2020.101854. [DOI] [PubMed] [Google Scholar]
- Schaefer J., Giangrande E., Weinberger D.R., Dickinson D. The global cognitive impairment in schizophrenia: consistent over decades and around the world. Schizophr. Res. 2013;150:42–50. doi: 10.1016/j.schres.2013.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheffield J.M., Karcher N.R., Barch D.M. Cognitive deficits in psychotic disorders: a lifespan perspective. Neuropsychol. Rev. 2018;28:509–533. doi: 10.1007/s11065-018-9388-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stirman S.W., Gutner C.A., Langdon K., Graham J.R. Bridging the gap between research and practice in mental health service settings: an overview of developments in implementation theory and research. Behav. Ther. 2016;47:920–936. doi: 10.1016/j.beth.2015.12.001. [DOI] [PubMed] [Google Scholar]
- Tetley A., Jinks M., Huband N., Howells K. A systematic review of measures of therapeutic engagement in psychosocial and psychological treatment. J. Clin. Psychol. 2011;67:927–941. doi: 10.1002/jclp.20811. [DOI] [PubMed] [Google Scholar]
- Thiruselvam I., Hoelzle J.B. Refined measurement of verbal learning and memory: application of item response theory to California Verbal Learning Test – Second Edition (CVLT-II) learning trials. 2020;35:90–104. doi: 10.1093/arclin/acy097. [DOI] [PubMed] [Google Scholar]
- Thomas M.L., Bismark A.W., Joshi Y.B., Tarasenko M., Treichler E.B.H., Hochberger W.C., Zhang W., Nungaray J., Sprock J., Cardoso L., Tiernan K., Attarha M., Braff D.L., Vinogradov S., Swerdlow N., Light G.A. Targeted cognitive training improves auditory and verbal outcomes among treatment refractory schizophrenia patients mandated to residential care. Schizophr. Res. 2018;202:378–384. doi: 10.1016/j.schres.2018.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torous J., Keshavan M. COVID-19, mobile health and serious mental illness. Schizophr. Res. 2020;218:36–37. doi: 10.1016/j.schres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vita A., Barlati S., Ceraso A., Nibbio G., Ariu C., Deste G., Wykes T. Effectiveness, core elements, and moderators of response of cognitive remediation for schizophrenia: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. 2021;78:848–858. doi: 10.1001/jamapsychiatry.2021.0620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner B.J., Lewis C.C., Stanick C., Powell B.J., Dorsey C.N., Clary A.S., Boynton M.H., Halko H. Psychometric assessment of three newly developed implementation outcome measures. Implement. Sci. 2017;12:108. doi: 10.1186/s13012-017-0635-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood H.J., Gannon J.M., Chengappa K.N.R., Sarpal D.K. Group teletherapy for first-episode psychosis: piloting its integration with coordinated specialty care during the COVID-19 pandemic. 2020;8 doi: 10.1111/papt.12310. [DOI] [PubMed] [Google Scholar]
- Woods S.P., Delis D.C., Scott J.C., Kramer J.H., Holdnack J.A. The California Verbal Learning Test – second edition: test-retest reliability, practice effects, and reliable change indices for the standard and alternate forms. Arch. Clin. Neuropsychol. 2006;21:413–420. doi: 10.1016/j.acn.2006.06.002. [DOI] [PubMed] [Google Scholar]
- Young A.S., Cohen A.N., Niv N., Nowlin-Finch N., Oberman R.S., Olmos-Ochoa T.T., Goldberg R.W., Whelan F. Mobile phone and smartphone use by people with serious mental illness. Psychiatr. Serv. 2020;71:280–283. doi: 10.1176/appi.ps.201900203. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material