Abstract
Background
College students face several sources of stress. Self-guided stress management interventions offer an excellent opportunity for scaling up evidence-based interventions for self-management of these stresses. However, little is known about the overall effects of these interventions. Increasing this understanding is essential because self-guided stress management interventions might be a cost-effective and acceptable way of providing help to this important segment of the population during a critical life course stage.
Methods
We carried out a systematic literature search of bibliographical databases (PubMed, PsycINFO, Embase, and Cochrane Library) for randomized controlled trials (RCTs) of self-guided stress management interventions published up through April 2020. We conducted two separate meta-analyses for perceived stress, depression, and anxiety. The first included interventions for general college student samples. The second included studies for students with high levels of perceived stress.
Results
The first meta-analysis included 26 studies with 29 intervention-control comparisons based on a total of 4468 students. The pooled effect size was small but statistically significant (g = 0.19; 95% CI [0.10, 0.29]; p < 0.001). Results showed moderate heterogeneity across studies [I2 = 48%; 95% CI (19, 66%)]. The second meta-analysis, included four studies based on a total of 491 students with high levels of stress. The pooled effect size was small but statistically significant (g = 0.34; 95% CI [0.16, 0.52]; p < 0.001). Results showed no heterogeneity across studies (I2 = 0%; 95% CI [0, 79%]), but risk of bias was substantial.
Discussion
Our results suggest that self-guided stress management programs may be effective when compared to control conditions, but with small average effects. These programs might be a useful element of a multi-component intervention system. Given the psychological barriers to treatment that exist among many college students, self-help interventions might be a good first step in facilitating subsequent help-seeking among students reluctant to engage in other types of treatment. More studies should be conducted to investigate these interventions, sample specifications, mediating effects, and individual-level heterogeneity of effects.
Keywords: Self-help, College students, Stress management, Unguided interventions
Highlights
-
•
College students encounter stressors in several domains.
-
•
Self-guided stress management interventions can be cost-effective and more acceptable.
-
•
Self-guided stress management programs may have a small effect on stress, depression, or anxiety.
1. Introduction
College students experience a range of stressors related to this specific phase in life such as leaving home, being more independent, gaining new responsibilities, and overcoming new academic demands (Sussman and Arnett, 2014). A considerable proportion of college students report elevated levels of perceived stress defined as the appraisal of stressors as threats that exceed one's coping abilities and result in a feeling of being overwhelmed (Cohen et al., 2020; Leppink et al., 2016). Prolonged psychological stress is closely associated with mental disorders (Auerbach et al., 2018; Beiter et al., 2015; Karyotaki et al., 2020; Mortier et al., 2018), and also has consequences for academic performance (Bruffaerts et al., 2018), campus engagement (Salzer, 2012), and college drop-out (Eisenberg et al., 2009). Chronic psychological stress may also lead to more serious mental health disorders later in life (Cohen et al., 2007; De Girolamo et al., 2015). Moreover, the first onset of common mental disorders generally occurs during young adulthood (Kessler et al., 2007). Therefore psychological interventions for college students may play a critical role in prevention and early intervention with these mental disorders (Karyotaki et al., 2020).
Recent evidence suggests that stress management programs and psychological treatments for common mental disorders are both effective in decreasing perceived stress and clinically significant symptoms of anxiety and depression among college students (Amanvermez et al., 2020; Cuijpers et al., 2016; Cuijpers et al., 2021; Harrer et al., 2019b). However, college students' treatment uptake is low (Bruffaerts et al., 2019) and access to psychological treatments for common mental disorders is limited due to several barriers such as system-related and scheduling issues (Leviness et al., 2019; Marsh and Wilcoxon, 2015; Stallman and Shochet, 2009; Watkins et al., 2011). In addition, students can be reluctant to seek professional mental health treatment because of unwillingness to define themselves as having a mental disorder and fear of stigma (Ebert et al., 2019; Marsh and Wilcoxon, 2015). Moreover, mental health needs may not be fulfilled sufficiently at university counseling centers since face-to-face interventions generally require resources such as trained personnel (e.g. therapist or coach) (Leviness et al., 2019). Given these barriers, delivering evidence-based interventions designed to provide help with stress management in a self-help format might be a more practical and psychologically acceptable approach.
A self-help intervention is defined as a standardized intervention in which participants apply the intervention manual independently from a professional guide or therapist (Cuijpers and Schuurmans, 2007). Self-help interventions are sometimes facilitated by a trained practitioner or in a group format to stimulate adherence and use group processes to enhance therapeutic effects. They can also be self-administered by individual users (National Institute for Health and Care Excellence, 2020). Self-help interventions have enormous potential to maximize scalability because of their low cost and flexibility in terms of the times in which they can be used, and their ability to overcome system-related barriers (e.g. long waiting list) and attitudinal barriers (e.g. embarrassment, preference for self-management) (Czyz et al., 2013; Levin et al., 2016; Mains and Scogin, 2003). Moreover, self-administered stress management interventions may be more acceptable to college students than to other segments of the population due to the greater digital literacy of college students (Fairburn and Patel, 2017; Richardson et al., 2009).
Recent controlled studies found that self-help interventions can be effective in reducing depression and anxiety (Andrews et al., 2018; Bennett et al., 2019; Cuijpers et al., 2019; Karyotaki et al., 2021). However, these studies generally focused on clinical or sub-clinical populations with depression or anxiety. Meta-analytical evidence is generally lacking for non-clinical samples who experience elevated levels of perceived stress. In addition, the systematic reviews that exist on this topic combine digital programs with and without human support (Davies et al., 2014; Heber et al., 2017; Lattie et al., 2019). Given that supported self-help interventions are more expensive than their unsupported counterparts, it would be useful to have meta-analytic evidence on the effects of each separately. In the current report, we aimed to present such an analysis of self-help interventions for stress management delivered without human support, which we henceforth refer to as self-guided.
To date, the effects of self-guided stress management interventions at a meta-analytic level have generally been examined in samples of people with physical illness (Ugalde et al., 2017) or adults seeking help for the management of work-related stress (Richardson and Rothstein, 2008). However, there is growing literature investigating the effects of self-guided stress management interventions among unrestricted samples of college students. Therefore, we focused on individual self-guided stress management interventions, excluding both self-help groups and guided self-help interventions. In our study, we anticipated differences between college student samples in terms of inclusion characteristics, thus, we investigated the effects of stress management interventions for two college student samples separately: (1) those who were recruited regardless of their perceived stress scores (hereinafter referred to as unselected college students), and (2) those who were recruited into studies delivered exclusively to students with high levels of perceived stress based on a cut-off score on a standardized stress scale (hereinafter referred to as preselected college students).
2. Methods
The results of the systematic review and meta-analysis were reported following the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) Statement (Liberati et al., 2009).
2.1. Protocol and registration
Methods of the planned search strategy, inclusion criteria, and data analysis were prospectively identified. This study has been preregistered in the Open Science Framework (OSF). The preregistered protocol can be retrieved via https://osf.io/23vck.
2.2. Eligibility criteria
We included studies that were 1) RCTs in which 2) a self-guided self-help stress management intervention compared to 3) a control condition (care-as-usual, waiting list, or attention control, etc.) in 4) a higher education setting. Included data were based on continuous outcomes for perceived stress, psychological distress, depression, and/or anxiety. Psychological stress/distress is considered a generic concept. In this study, we defined psychological stress/distress as a non-specific emotional and behavioral response resulting from external or internal demands (Cohen et al., 1995, pp. 6–7; Cohen et al., 2016; Ridner, 2004). Therefore, we decided to examine symptoms of depression and anxiety as outcomes next to stress symptoms as they are often reported together and in some cases used interchangeably in studies testing the effectiveness of stress management programs. Further, depressive and anxiety symptoms are two of the most common emotional health problems, and thus, they are conceptually embedded within the definition of psychological distress (Ridner, 2004). Despite their phenomenologically unique characteristics (e.g., depression is characterized as low positive affect, lack of motivation, loss of interest, or hopelessness, while anxiety is characterized by symptoms of physical hyperarousal such as restlessness or irritability), they share substantial non-specific components with each other (Hammen, 2015; Henry and Crawford, 2005; Lovibond and Lovibond, 1995; Monroe, 2008; Watson et al., 1995). Given the strong associations between these emotional problems and the high comorbidity, in this meta-analysis, we included depression and anxiety outcomes to get a more comprehensive overview of the effectiveness of stress management interventions.
We defined two different eligibility criteria for two meta-analyses in terms of the target population. In the first meta-analysis, we only included studies with unselected college students. In the second study, we included studies preselected college students based on a cut-off score on a perceived stress scale. Self-guided stress management intervention is defined as a psychological intervention addressing psychological stress and coping skills in which individuals follow the program without the help of a care provider. We added self-guided stress management programs in any format including web-based, mobile phone applications, book, or audio. We included studies if participants were in contact with the research staff only with the purpose of technical support (e.g. if they had problems in accessing the platform in the online intervention) or data collection. Only RCTs in English were added to our study.
We excluded peer support groups and guided self-help interventions in which a coach/therapist provided personalized feedback on the student's progress. We excluded studies if the recruitment focus was not stress. Following this, we excluded studies addressing interventions for depressive and/or anxiety symptoms, worry, procrastination, sleep difficulties, or eating behaviors. We also excluded studies if they were not published in peer-reviewed journals (such as conference papers, or dissertations).
2.3. Search strategy
We retrieved publications from the four main bibliographic databases namely, PubMed, PsycINFO, Embase, and Cochrane Library up until 29.04.2020. We had already established this database to be used in another study examining the guided or in-person stress management interventions (Amanvermez et al., 2020). We updated this database using the same search strings. We filtered results by RCTs and according to age groups. Full search strings are presented in Appendix A. We also searched a database which includes psychological interventions in college students that was developed by another research group. Details related to this database can be found at https://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017068758.
2.4. Selection of studies
After retrieving studies from the databases and removing duplicates, two researchers (YA and RZ) independently screened the studies based on the titles and abstracts. Following the first screening, full-texts of the selected studies were examined for eligibility. Disagreements between the two assessors were discussed with the senior researchers (EK, LDW, or PC).
2.5. Data extraction and classification
Two researchers independently extracted the data including 1) the characteristics of the studies (author, publication year, country), 2) characteristics of the interventions (theoretical background, format, length), 3) characteristics related to the study design (type of control condition, inclusion criteria of the participants, outcomes, time of assessments, compensation, study attrition rate), and 4) characteristics of the participants (age, percentage of the female students, target student population, recruitment strategy, type of the university). We extracted the percentage of female students to describe trends in gender distribution in the included studies because previous studies have shown that female participants were more likely to utilize psychological interventions (Davies et al., 2014; Harrer et al., 2019b).
We classified selected study characteristics to run subgroup analysis. Stress management programs were grouped according to the theoretical background under four categories based on common therapeutic strategies: 1) cognitive-behavioral therapy (CBT), 2) third-wave therapies (TW), 3) skills-training, and 4) mind-body interventions. Stress management programs including components such as cognitive restructuring or stress inoculation strategies were assessed under the CBT-based stress management programs (Ong et al., 2004). Programs including techniques of acceptance or mindfulness concepts in combination with CBT strategies such as acceptance and commitment therapy (ACT), or mindfulness-based cognitive behavior therapy (MBCT) were classified under TW (Hayes and Hofmann, 2017). Skills training programs included components to improve particular skills to manage stress (e.g. improving present control skills). Mind-body interventions were the programs that mainly used mindfulness, meditation, biofeedback, or relaxation techniques (Astin et al., 2003; Ong et al., 2004). We classified the length of the intervention as brief, moderate, and long if they were delivered for 1–4 weeks, 5–8 weeks, and 8+ weeks, respectively. We have classified the modalities if they were delivered in online format (including web-based stress management programs, and/or mobile phone applications) or others (book and/or audio).
The number of participants, mean scores, and standard deviation of control and intervention conditions at post-test were extracted to calculate the effect size. If these data were not available, we extracted other available statistics (i.e., p-value, t score, or effect size) that allowed us to calculate the effect size. If no relevant information was reported for calculating effect size, then we contacted the author. If the author did not respond, we excluded this study from our analysis. We could not retrieve relevant data from the published reports of four studies. After contacting the authors, we could obtain the relevant data for three studies (Nguyen-Feng et al., 2015; Nguyen-Feng et al., 2019; Walsh et al., 2019), which allowed us to calculate effect sizes. However, we could not retrieve the relevant data for one study which was excluded.
2.6. Quality assessment
The risk of bias was assessed by the revised Cochrane risk-of-bias tool for randomized trials (RoB 2) (Sterne et al., 2019). RoB 2 includes five domains: (1) bias arising from the randomization process; (2) bias due to deviations from intended interventions; (3) bias due to missing outcome data; (4) bias in the measurement of the outcome; and (5) bias in the selection of the reported result (Sterne et al., 2019). However, in the present study, the domain assessing the bias in the measurement of the outcome was omitted as all studies used self-reported measures. This issue inherently precludes the blinding of the outcome assessor. Therefore we assessed only four domains in the RoB 2 tool.
Two independent assessors (YA and RZ) assessed each study for these domains by answering the signaling questions. By doing this, we had results of low risk of bias, some concerns, or high risk of bias at the domain level. Then we determined the overall risk of bias of each study as low, some concerns, and high risk of bias. The overall risk of bias of the study was determined to be low if at least two domains had low risk and no high risk of bias at any domain. The overall risk of bias was considered high if at least two domains had a high risk of bias or all domains had some concerns. The studies that did not meet these criteria were evaluated as containing “some concerns” (e.g. studies having “some concerns” at three domains and low risk of bias at one domain). Discrepancies between assessments were discussed by two assessors. Senior researchers (EK, LDW, or PC) were consulted if discrepancies were not solved as a result of the discussion.
2.7. Meta-analyses
We conducted two separate meta-analyses using the Comprehensive Meta-Analysis (CMA) software package and the meta (Schwarzer, 2007), metafor (Viechtbauer, 2010), and dmetar (Harrer et al., 2019a) packages in R version 4.0.2. We calculated the effect size of each study using the CMA by pooling all continuous outcomes of perceived stress, anxiety, and/or depression within a study. Then we used R to calculate the pooled effect size, perform additional analyses including subgroup analyses, sensitivity analysis, and test publication bias.
We calculated the effect size of each study using the mean, standard deviation, and the number of students in the intervention and control conditions at post-test assessment. If multiple outcomes were reported within one study, first we calculated a synthetic effect size per study. If there is high association between targeted outcomes, this would result in high correlation between errors of these outcomes. In such case, combining outcomes first within the study and generating one effect size per study is recommended (Borenstein et al., 2009). In our main analysis, we pooled the combined effect size from each study by taking into account the high correlation between these outcomes. Therefore we calculated one effect size (Hedges' g) for each study separately. Then we pooled the effect sizes. As an additional analysis, we also examined the effect of stress management programs on each outcome separately. We conducted the meta-analyses under the random-effects model due to the wide variability of studies. An effect size of 0.2, 0.5, and 0.8 was interpreted as small, moderate, and large, respectively (Cohen, 1988). We also calculated the number needed to treat (NNT) to improve the understandability of the findings (Kraemer and Kupfer, 2006). Heterogeneity of the effect sizes across studies was calculated using I2 (Ioannidis et al., 2007). Heterogeneity was deemed to be low, moderate, and high if the I2 value was quantified 25%, 50%, and 75% respectively (Higgins et al., 2003). We also calculated the 95% CI around I2.
2.8. Publication bias
Publication bias was assessed by inspection of the funnel plot and testing the asymmetry of the funnel plot performing Egger's test of the intercept (Egger et al., 1997). We estimated the number of missing studies from the funnel plot, and re-calculated the effect size after imputation the missing studies with Duval and Tweedie's trim and fill procedure (Duval and Tweedie, 2000).
2.9. Additional analyses
A series of subgroup analyses using the mixed-effects model was conducted with the studies for unselected college students to examine whether the effects are different in terms of the study or intervention characteristics. We conducted subgroup analyses for the type of control (AC vs. WL vs. CAU), theoretical background (CBT vs. TW vs. skills training vs. mind-body), length of the studies (brief vs. moderate vs. long), intervention format (online vs. others), compensation (yes vs. no), recruitment strategies (campus vs. subject pool vs. online vs. mixed), and risk of bias assessment (high vs. some concerns vs. low). We also conducted a sensitivity analysis including only studies with a low risk of bias to obtain the most accurate findings.
3. Results
3.1. Study selection
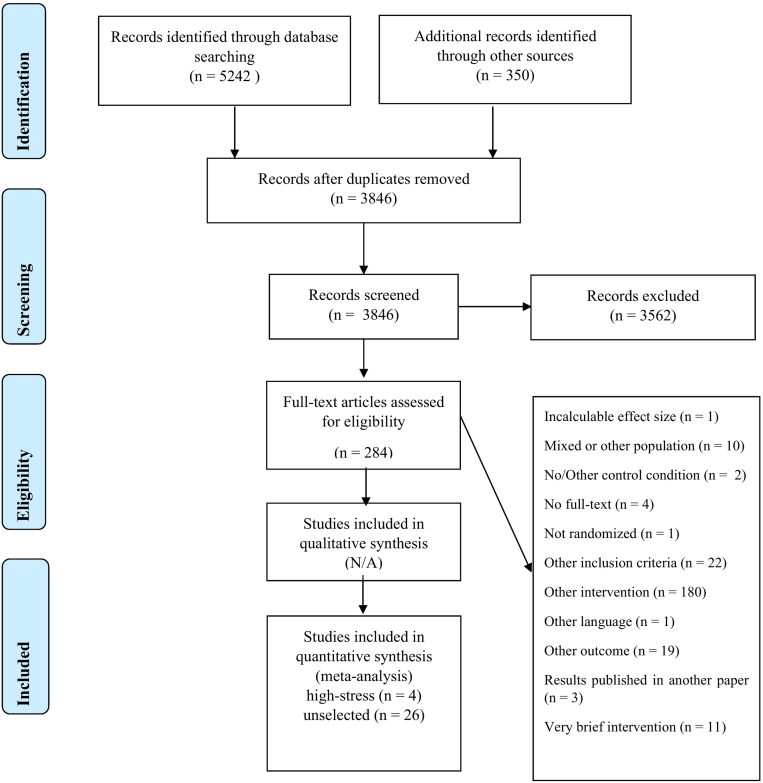
Our searches resulted in 5242 studies from the database search and 350 from the other source. After removing the duplicates, we had a total of 3846 studies. The records were screened based on the title and abstract and 3562 studies did not meet inclusion criteria and were excluded. Following this, we screened the full-text of 284 remaining studies for eligibility. As a result, we retrieved 26 studies with 29 comparisons for the unselected college samples and four studies for preselected students. Details of this process and reasons for the exclusion of the studies can be seen in Fig. 1.
Fig. 1.
PRISMA flow diagram.
3.2. Study characteristics
Studies with unselected college students consisted of 4468 participants in total (intervention groups: N = 2400; control groups: N = 2068). Fourteen out of 26 studies compared the intervention to a waiting list (WL) group, while comparisons were made with an attention control (AC) in 10 studies, and care-as-usual (CAU) in two studies. Among 29 comparisons, 13 of them were mind-body interventions, seven interventions were based on TW approaches. There were six skills training and three CBT-based programs. Almost all studies were conducted in high-income countries. Half of the studies were conducted in the USA. Two studies were in the UK, New Zealand, Canada, and Australia. The rest were conducted in Sweden, France, Ireland, and Thailand. Study characteristics can be seen in Table 1.
Table 1.
Study characteristics for studies with unselected college students.
| Study | Recruitment | Student sample | Conditions | Drop out % | Theoretical background | Format | Reminder | Length | Age | Female % | Compensation | University type | Country |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Barry et al., 2019 | Online | Graduate | 1. Mindfulness program 2. WL |
12.00% | TW | Audio | No | 8-week | 38 | 81.50% | No | Public | AUS |
| Burger and Lockhart, 2017 | Subject Pool | Undergraduate | 1) Mindfulness meditation 2)WL |
13.33% | TW | Online | No | 4-week | ns | 72.00% | No | ns | USA |
| Cavanagh et al., 2013 | Mixed | General | 1). Mindfulness program 2) WL |
44.00% | TW | Online | Yes | 2-week | 24.7 | 88.46% | No | ns | UK |
| Fehring, 1983 | Campus | General | 1) Benson's relaxation technique (BRT) 2) Benson's relaxation technique augmented with GSR biofeedback (BAR) 3) CAU |
13.33% | MB | Book + Audio + GSR II recorder | No | 8-week | 22.8 | 78.20% | No | Private | USA |
| Flett et al., 2019 | Subject Pool | Undergraduate | 1) Mindfulness meditation (Headspace) 2) Mindfulness meditation (Smiling Mind) 3) AC |
0.09% | TW | Online | Yes | 10-day | 20.08 | ns | Yes | Public | NZ |
| Flett et al., 2020 | Online | Undergraduate | 1) Mindfulness meditation (Headspace) 2) WL |
22.00% | TW | Online | Yes | 3-month | 17.87 | 67.60% | Yes | Public | NZ |
| Frazier et al., 2015 | Subject Pool | Psychology | 1) Present control intervention 2) AC (stress information only) |
43.20% | ST | Online | Yes | 2-week | ns | 75.00% | Yes | ns | USA |
| Hazlett-Stevens and Oren, 2017 | Mixed | General | 1) MBSR bibliotherapy 2) WL |
26.00% | TW | Book + Audio | Yes | 10-week | 22.1 | 75.00% | Yes | ns | USA |
| Hockemeyer and Smyth, 2002 | Campus | General | 1) Stress management workbook 2) AC |
10.00% | CBT | Book + Audio | No | 4-week | 20.7 | 53.70% | Yes | ns | USA |
| Kanekar et al., 2010 | Online | International | 1) Skills training 2) AC (wellness intervention) |
35.00% | ST | Online | Yes | 2-month | 24.67 | 12.80% | Yes | ns | USA |
| Kvillemo et al., 2016 | Campus | General | 1) Internet-based mindfulness training 2) AC |
45.56% | TW | Online | Yes | 8-week | 29 | 73.68% | Yes | ns | SWE |
| Lee and Jung, 2018 | Campus | Undergraduate | 1. Destressify 2. WL |
20.87% | TW | Online | Yes | 4-week | 20.6 | 63.00% | Yes | Public | CAN |
| Levin et al., 2014 | Mixed | Undergraduate | 1) ACT on college life 2) WL |
2.61% | TW | Online | Yes | 3 week | 18.37 | 53.90% | Yes | ns | USA |
| Levin et al., 2016 | Mixed | Undergraduate | 1) ACT-CL website 2) AC (mental health education website) |
23.50% | TW | Online | Yes | 3-week | 21.61 | 76.90% | Yes | ns | USA |
| Melnyk et al., 2015 | Online | Undergraduate | 1) COPE 2) AC |
23.14% | CBT | Online | No | 7-week | 18.6 | 86.40% | Yes | Public | USA |
| Muto et al., 2011 | Mixed | International | 1) Get Out of Your Mind and Into Your Life book 2) WL |
12.85% | TW | Book | No | 8-week | 23.6 | 62.86% | Yes | Public | USA |
| Nguyen-Feng et al., 2015 | Campus | Psychology | 1) Web-based stress management intervention 2) WL |
16.86% | ST | Online | No | 5-week | ns | 62.00% | Yes | ns | USA |
| Nguyen-Feng et al., 2017 | Campus | Psychology | 1) A mindfulness plus present control intervention 2) A mindfulness only intervention 3) AC (stress information) |
30.13% | ST | Online | Yes | 4-week | ns | 75.00% | Yes | ns | USA |
| Nguyen-Feng et al., 2019 | Campus | Undergraduate | 1) Ecological momentary intervention 2) AC (ecological momentary assessment) |
16.23% | ST | Online | Yes | 2-week | 21.3 | 77.00% | Yes | ns | USA |
| O’Driscoll et al., 2019 | Mixed | Undergraduate | 1) Online mindfulness 2) WL | 62.59% | TW | Online | Yes | 4-week | ns | 76.90% | No | Mixed | IRE |
| Paholpak et al., 2012 | Campus | Undergraduate | 1) Breathing meditation 2) CAU |
0.00% | MB | Audio | No | 4-week | 23.28 | 50.00% | No | Public | TH |
| Saleh et al., 2018 | Mixed | General | 1) I'm managing my stress 2) WL |
57.03% | CBT | Online | Yes | 4-week | 22.54 | 81.25% | Yes | Public | FR |
| Taylor et al., 2014 | Campus | General | 1) MBCT-SH book 2) WL |
5.00% | TW | Book + Audio | Yes | 8-week | 28.61 | 81.00% | No | ns | UK |
| Viskovich and Pakenham, 2020 | Mixed | General | 1) YOLO Program 2) WL |
41.99% | TW | Online | Yes | 4-week | 26.85 | 67.80% | No | ns | AUS |
| Walsh et al., 2019 | Mixed | General | 1) Wildflowers 2) AC |
20.37% | TW | Online | No | 3-week | 20.01 | 84.00% | Yes | Public | CAN |
| Yang et al., 2018 | Online | Undergraduate | 1) Headspace 2) WL |
7.95% | TW | Online | No | 4-week | 25.11 | 64.00% | No | Private | USA |
Note. AC: active control; AUS: Australia; CAN: Canada; CAU: care-as-usual; CBT: cognitive behavior therapy; FR: France; IRE: Ireland; MB: mind-body; NZ: New Zealand; ST: skills training; SWE: Sweden; TH: Thailand; TW: third wave therapy; UK: United Kingdom; USA: United States of America; WL: waiting list.
In the meta-analysis of studies with preselected students, a total of 491 participants were included (intervention groups: N = 235; control groups: N = 256). Of four studies, two studies used AC as a comparison group and the other two studies used WL. Two interventions were based on skills training, one incorporated CBT techniques, and one was designed based on TW principles. With regard to the inclusion criteria of the participants, two studies used a cut-off score based on the Perceived Stress Scale (PSS-10) (Cohen and Williamson, 1988). One study used the Depression Anxiety and Stress Scale (DASS-21) stress or anxiety sub-scale (Lovibond and Lovibond, 1995), and one study used the Perceived Control Over Stressful Events Scale (PCOSES) (Frazier et al., 2011). Three studies were conducted in the USA, and one study was in the UK. Study characteristics can be seen in Table 2.
Table 2.
Study characteristics for studies with preselected college students.
| Author | Recruitment | Student sample | Inclusion criteria | Conditions | Drop out % | Theoretical background | Format | Reminder | Weeks | Age | Female | Compensation | University type | Country |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chiauzzi et al., 2008 | Campus | Undergraduate | PSS-10 > 14 | 1) MyStudentBodyStress 2) AC |
2.08% | ST | Online | Yes | 2-week | ns | 51.46% | No | Mixed | USA |
| Hintz et al., 2015 | Subject pool | Psychology | PCOSES ≤ 3 | 1) Present control intervention, 2) The present control intervention plus feedback, 3) AC |
30.00% | ST | Online | Yes | 2-week | ns | 70% | Yes | ns | USA |
| Huberty et al., 2019 | Mixed | Undergraduate | PSS-10 ≥ 14 | 1) Mindfulness meditation (CALM) 2) WL |
19.26% | TW | Online | Yes | 8-week | 21.13 | 88% | Yes | Public | USA |
| Ponzo et al., 2020 | Mixed | General | DASS-21-S > 14 or DASS-21-A > 7 | 1) Biobase program 2) WL |
55.72% | CBT | online | Yes | 4-week | 19.87 | 63.01% | Yes | ns | UK |
Note. AC: active control, CAU: care-as usual, CBT: cognitive behavior therapy; DASS: Depression Anxiety Stress Scale; PCOSES: Perceived Control over Stressful Events Scale; PSS: Perceived Stress Scale; ST: skills training; TW: third wave therapy; UK: United Kingdom; USA: United States of America; WL: waiting list.
The study dropout rate was calculated using the number of participants who were included in the study but lost to post-test assessment. Overall, 27.77% (ranging from 0% to 62.59%) of the unselected college students, and 28.8% (ranging from 2.08 to 55.72%) of the pre-selected college students did not provide complete data.
3.3. Quality assessment
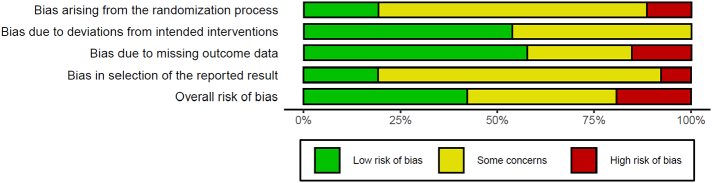
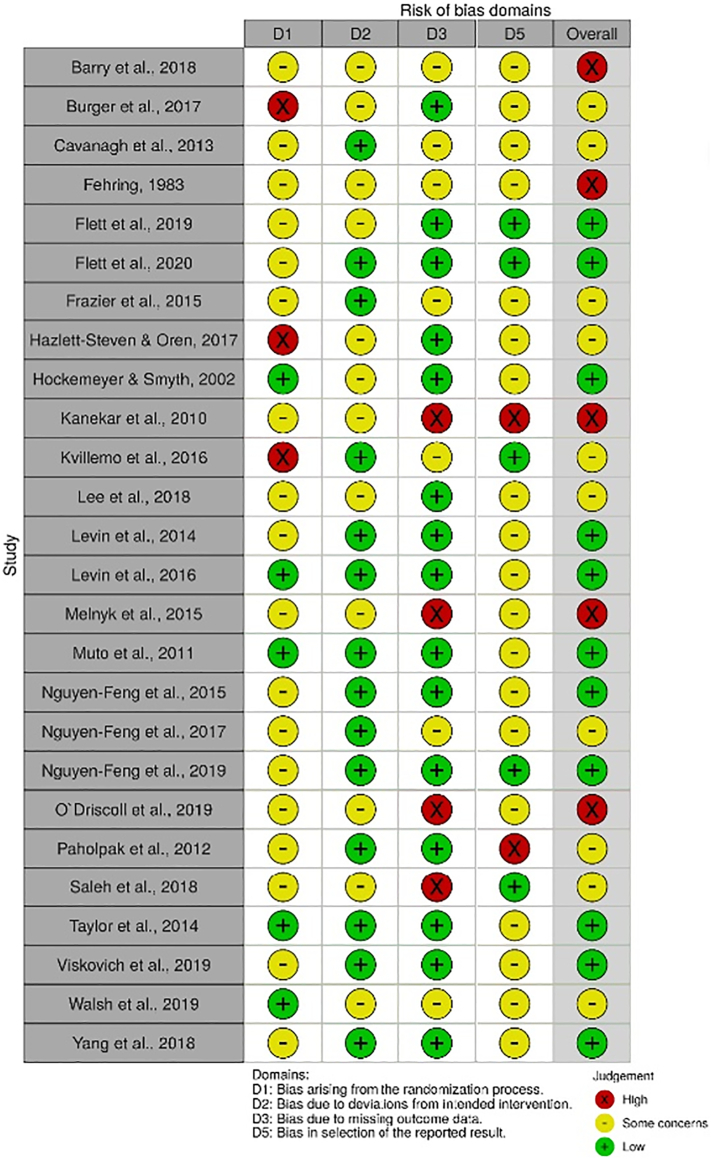
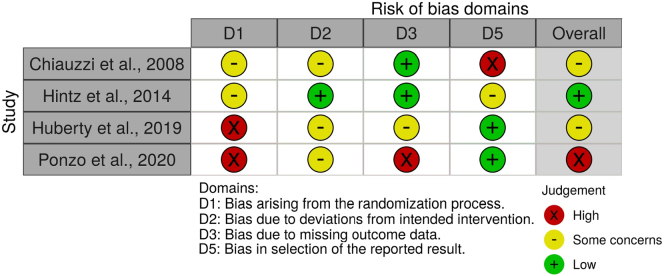
The overall risk of bias in all studies was considerable. Studies with unselected college students showed that the randomization process was handled/reported adequately in only five out of 26 studies. The risk of bias arising from the deviations from intended interventions showed that fourteen studies fulfilled the criteria for low risk. In fifteen studies, missing outcome data were properly managed or reported in a detailed way. We assessed only five studies as having a low risk of bias for the selection of the reported results. In total, eleven studies were judged to have an overall low risk of bias, ten studies had some concerns, and five studies had an overall high risk of bias. The visual demonstration of the risk of bias assessments can be seen in Figs. 2 and 3.
Fig. 2.
Risk of bias summary for studies with unselected college students.
Fig. 3.
Risk of bias summary for studies with unselected college students.
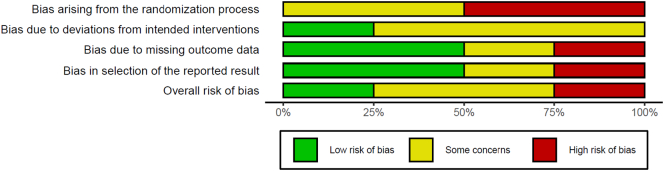
Among the studies with preselected college students, the randomization process was either not reported elaborately or had some concerns. We assessed only one study having a low risk of bias in the domain of deviations from the intended interventions. Two out of four studies were assessed as having a low risk of bias for missing outcome data. Two studies were deemed to be having a low risk of bias for the selection of the reported result. Overall, there was a low risk of bias in one study, some concerns in two studies, and a high risk of bias in one study. The risk of bias assessments of the studies with preselected college students can be seen in Figs. 4 and 5 in detail.
Fig. 4.
Risk of bias summary for studies with preselected college students.
Fig. 5.
Risk of bias summary for studies with preselected college students.
3.4. Main analyses
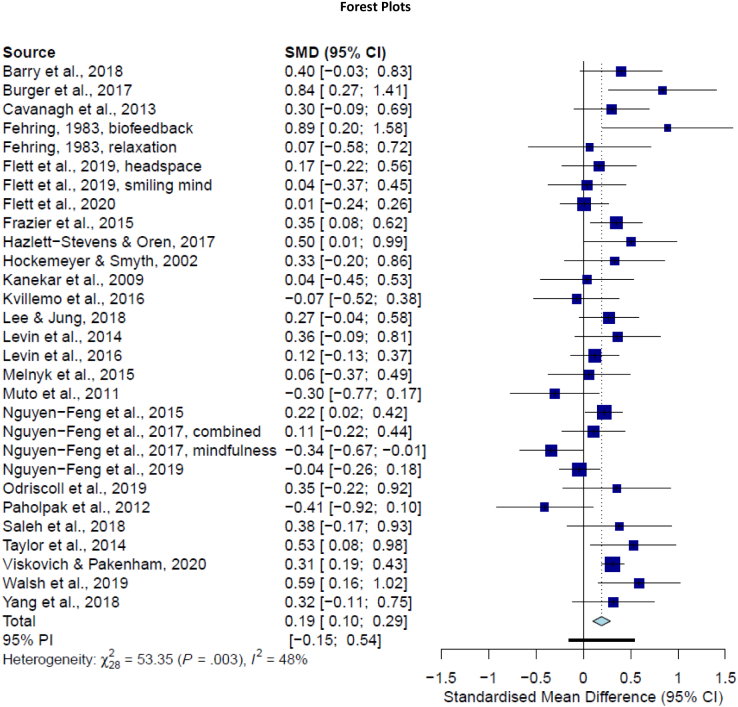
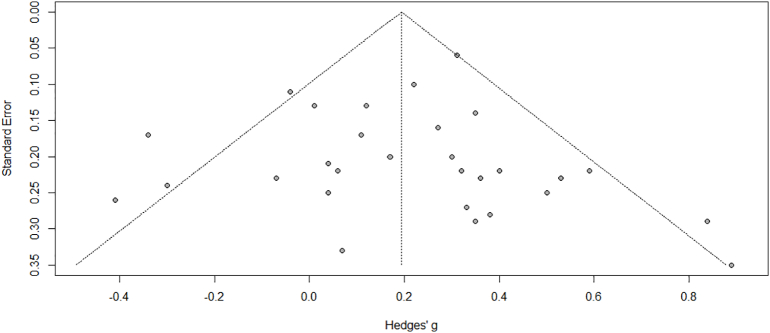
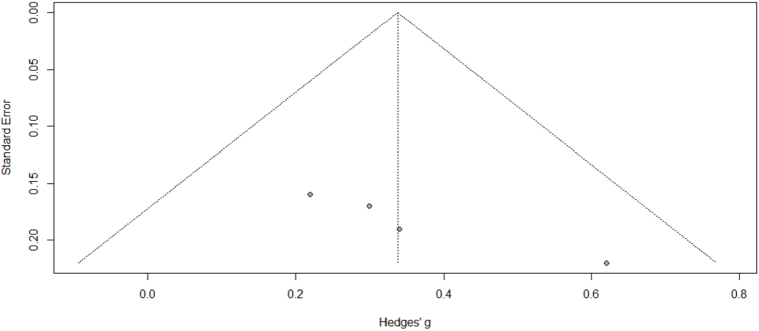
The overall effect size of the self-guided stress management program in comparison to a control condition at post-test was small but statistically significant for the unselected student samples (g = 0.19; 95% CI [0.10, 0.29]; p < 0.001; n = 29) with moderate heterogeneity across studies (I2 = 48%; 95% CI [19–66%]). NNT was 9.43. Based on inspection of the forest plot (Fig. 6), we found two outliers (Nguyen-Feng et al., 2017, mindfulness intervention, and Paholpak et al., 2012). After removing the outliers, the effect size was still low (g = 0.23; 95% CI [0.14, 0.31]; p < 0.001; n = 27; I2 = 30%; 95% CI [0–56%]). As a result of separate analyses for each outcome, we found a small effect size for stress (g = 0.25; 95% CI [0.15–0.35]; p < 0.001; n = 26), depression (g = 0.14; 95% CI [0.03–0.26]; p = 0.016; n = 19), and anxiety (g = 0.11; 95% CI [0.00–0.21]; p = 0.045; n = 19). Heterogeneity across studies was moderate for stress (I2 = 53%), depression (I2 = 59%), and anxiety (I2 = 46%). The prediction interval ranged from −0.15 to 0.54. All details are presented in Table 3. We also found an indication of publication bias for studies with unselected samples based on the inspection of the funnel plot (Fig. 8). Egger's test of the intercept was not significant (intercept: 0; 95% CI: −1.14–1.14, t = 0, p = 0.99) yet Duval and Tweedie's trim and fill procedure resulted in one imputed study. Adjusted effect size was small (g = 0.18, 95% CI [0.09; 0.28], p < 0.001).
Fig. 6.
Forest plot for comparisons of self-guided stress management programs for unselected college students to control conditions at posttest.
Table 3.
Pooled effects of self-guided stress management programs for unselected college students on target outcomes compared with control groups.
| Effect size |
p | Heterogeneity |
NNT | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | g | 95% CI | p | I2 | 95% CI around I2 | ||||
| Overall effects | 29 | 0.19 | 0.10–0.29 | 0.000 | 48 | 19–66 | 9.43 | ||
| Removing two outliers | 27 | 0.23 | 0.14–0.31 | 0.000 | 30 | 0–56 | 7.69 | ||
| Symptom outcomes | |||||||||
| Stress | 26 | 0.25 | 0.15–0.35 | 0.000 | 53 | 28–70 | 7.14 | ||
| Anxiety | 19 | 0.11 | 0.00–0.21 | 0.045 | 46 | 8–69 | 16.13 | ||
| Depression | 19 | 0.14 | 0.03–0.26 | 0.016 | 59 | 33–75 | 12.82 | ||
| Only low risk of bias | 12 | 0.17 | 0.06–0.28 | 0.003 | 41 | 0–70 | 10.42 | ||
| Only low and some concerns | 23 | 0.18 | 0.08–0.29 | 0.001 | 54 | 26–71 | 9.80 | ||
| Subgroup analyses | |||||||||
| Theoretical background | CBT | 3 | 0.23 | −0.06–0.51 | 0.60 | 0.41 | 0 | 0–80 | 7.69 |
| Mind-body | 13 | 0.21 | 0.05–0.37 | 0.06 | 41 | 0–69 | 8.47 | ||
| Skills training | 6 | 0.07 | −0.12–0.26 | 0.02 | 61 | 6–84 | 25 | ||
| TW | 7 | 0.29 | 0.11–0.46 | 0.07 | 48 | 0–78 | 6.17 | ||
| Comparison group | Attention control | 12 | 0.10 | −0.03–0.23 | 0.08 | 0.11 | 39 | 0–69 | 17.86 |
| CAU | 3 | 0.16 | −0.59–0.90 | 0.01 | 78 | 27–93 | 11.11 | ||
| Waiting list | 14 | 0.28 | 0.17–0.38 | 0.19 | 24 | 0–60 | 6.41 | ||
| Length | Brief | 18 | 0.20 | 0.08–0.32 | <0.01 | 0.99 | 53 | 20–72 | 8.93 |
| Moderate | 9 | 0.18 | 0.00–0.37 | 0.10 | 41 | 0–73 | 9.80 | ||
| Long | 2 | 0.21 | −0.26–0.68 | 0.08 | 67 | 0–93 | 8.47 | ||
| ITT | Yes | 15 | 0.15 | 0.04–0.27 | <0.01 | 0.24 | 56 | 21–75 | 11.90 |
| No | 14 | 0.27 | 0.11–0.43 | 0.08 | 37 | 0–67 | 6.58 | ||
| Recruitment | Campus | 11 | 0.13 | −0.07–0.32 | <0.01 | 0.23 | 58 | 18–79 | 13.51 |
| Mixed | 9 | 0.28 | 0.20–0.37 | 0.64 | 0 | 0–054 | 6.41 | ||
| Online | 6 | 0.10 | −0.09–0.30 | 0.27 | 22 | 0–66 | 17.86 | ||
| Subject pool | 3 | 0.33 | −0.06–0.72 | 0.02 | 75 | 17–92 | 5.43 | ||
| Format | Online | 21 | 0.18 | 0.09–0.28 | 0.02 | 0.72 | 43 | 4–66 | 9.80 |
| Other | 8 | 0.24 | −0.06–0.53 | 0.01 | 62 | 17–82 | 7.46 | ||
| Reminder | Yes | 18 | 0.17 | 0.07–0.27 | 0.03 | 0.47 | 43 | 0–67 | 10.42 |
| No | 11 | 0.25 | 0.05–0.46 | <0.01 | 57 | 16–78 | 7.14 | ||
| Compensation | Yes | 19 | 0.13 | 0.03–0.23 | 0.06 | 0.04 | 36 | 0–63 | 13.51 |
| No | 10 | 0.34 | 0.16–0.51 | 0.08 | 41 | 0–72 | 5.26 | ||
| Risk of bias | High | 6 | 0.26 | 0.03–0.49 | 0.02 | 0.74 | 12 | 0–78 | 6.85 |
| Some concerns | 11 | 0.21 | 0.01–0.42 | 0.04 | 65 | 34–82 | 8.47 | ||
| Low | 12 | 0.17 | 0.06–0.28 | 0.00 | 41 | 0–70 | 10.42 | ||
Fig. 8.
Funnel plot of studies with unselected college students.
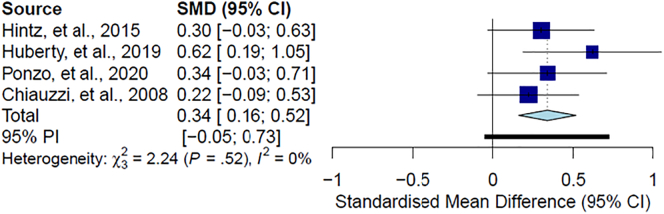
Meta-analysis of the studies with preselected college students yielded a low effect size (g = 0.34; 95% CI [0.16–0.52]; p < 0.001; n = 4) with zero heterogeneity (I2 = 0%; 95% CI [0–79%]). NNT was 5.26. We found no outlier based on the inspection of the forest plot (Fig. 7). We performed the separate analyses for outcomes and found a non-significant small effect size for stress (g = 0.27; 95% CI [−0.04, 0.58]; p = 0.087; n = 3), significant small effect for depression (g = 0.29; 95% CI [0.10–0.49]; p < 0.001; n = 3), and anxiety (g = 0.38; 95% CI [0.18–0.58]; p = 0.003; n = 3). Our results yielded moderate heterogeneity for stress (I2 = 56%), zero heterogeneity for depression (I2 = 0%) and anxiety (I2 = 0%). The prediction interval ranged from −0.05 to 0.73. The results can be seen in Table 4. Following the evaluation of the funnel plot in studies for preselected samples, findings did not suggest an indication of publication bias (Fig. 9). Egger's test was significant (intercept: 6.173, 95% CI [3.92– 8.42], t = 5.375, p = 0.033) which suggest a publication bias. After performing Duval and Tweedie's trim and full procedure, we found no imputed studies.
Fig. 7.
Forest plot for comparisons of self-guided stress management programs for preselected college students to control conditions at posttest.
Table 4.
Pooled effects of self-guided stress management programs for preselected college students on target outcomes compared with control groups.
| n | Effect size |
Heterogeneity |
NNT | ||||
|---|---|---|---|---|---|---|---|
| g | 95% CI | p | I2 | 95% CI around I2 | |||
| Overall effects | 4 | 0.34 | 0.16–0.52 | 0.000 | 0 | 0–79 | 5.26 |
| Symptom outcomes | |||||||
| Stress | 3 | 0.27 | −0.04–0.58 | 0.087 | 56 | 0–88 | 6.58 |
| Anxiety | 3 | 0.38 | 0.18–0.58 | 0.000 | 0 | 0–20 | 4.72 |
| Depression | 3 | 0.29 | 0.10–0.49 | 0.003 | 0 | 0–66 | 6.17 |
Fig. 9.
Funnel plot of studies with preselected college students.
3.5. Subgroup analyses, and sensitivity analysis
We performed several subgroup analyses for the studies with unselected samples. We found no significant associations between the theoretical background, control condition, length of the intervention, ITT, recruitment strategies, sending reminders, and the intervention format. We found a significant association (p = 0.04) between the effect size and compensation in favor of no compensation (g = 0.34; 95% CI [0.16–0.51]; n = 10) versus presence of compensation (g = 0.13; 95% CI [0.03– 0.23]; n = 19). All results are presented in Table 3. We could not perform any subgroup analysis with the studies for preselected samples due to a lack of a sufficient number of studies to run such analysis.
Sensitivity analysis for studies only having an overall low risk of bias showed that effect size was low (g = 0.17; 95% CI [0.06–0.28]; p = 0.003; n = 12). The number of studies with preselected samples did not permit us to run sensitivity analysis.
3.6. Meta-analyses of longer-term outcomes
Few studies assessed follow-up outcomes of the self-guided stress management programs, and follow-up time points varied widely across studies. Nevertheless, we pooled the findings of long-term effects up to 6-month follow-up for unselected samples, and found a non-significant effect (g = 0.01; 95% CI [−0.10–0.12]; p = 0.821; n = 12, I2 = 24%). Similarly, we ran the analysis only with studies assessing the outcomes up to 3-months follow-up and found no significant effect for unselected samples (g = 0.00; 95% CI [−0.13–0.13]; p = 0.963; n = 9, I2 = 36%). We calculated the long-term effects of self-guided stress management interventions up to 3-month in the preselected samples, and we found small and statistically significant effect size (g = 0.31; 95% CI [0.08–0.53]; p = 0.007; n = 3, I2 = 0%).
4. Discussion
We conducted two meta-analyses of the RCTs, one with unselected college samples and one with preselected college students with high levels of perceived stress, investigating the effectiveness of self-guided stress management interventions for college students. We included 26 studies with 29 comparisons for the unselected college students in the first meta-analysis and four studies for preselected students in the second meta-analysis. We found a small and statistically significant effect size of the self-guided stress management interventions for perceived stress, depression, and anxiety for the unselected student populations in comparison to the control condition. We also found a small and statistically significant effect size for the preselected students. The risk of bias was considerable in the included studies.
Systematic assessments of psychological interventions among college students have been studied for several mental health problems, however, to our knowledge, this is the first study pooling the results of all self-guided stress management interventions specifically for college students. Previous meta-analyses of self-guided programs found small effects in working populations (Carolan et al., 2017; Stratton et al., 2017) and in general populations (Heber et al., 2017) on stress and psychological distress. Although evidence of self-guided stress management programs for the non-clinical college student populations is limited, one meta-analysis of digital interventions reported a low effect size on stress, anxiety, and depression (Harrer et al., 2019b). Our results also align with other meta-analytic studies examining the internet-based interventions for non-clinical or subclinical depression/anxiety (Deady et al., 2017; Zhou et al., 2016).
A possible explanation behind the low effects of self-guided interventions may be related to the lack of human reciprocal contact. Several studies have demonstrated the superiority of guided interventions over self-guided programs in improving symptoms of common mental disorders (Baumeister et al., 2014; Domhardt et al., 2019; Karyotaki et al., 2021). Human support has been seen as a possible mechanism of change, as it was found to be associated with higher numbers of completed sessions and increased completer rates (Domhardt et al., 2019; Karyotaki et al., 2021; Nixon et al., 2021), which could be related to better intervention outcomes (Karyotaki et al., 2021). The superior effects of guided interventions may be related to the concept of supportive accountability defined as the social presence and/or dynamic interaction that stimulates the motivation to continue the intervention (Mohr et al., 2011). In addition, as noted earlier, the therapeutic relationship has been suggested as a crucial common factor, which can stimulate behavioral change in psychological interventions (Graves et al., 2017; Wampold, 2015). Thus, the lack of reflective processes and feedback while transferring the knowledge from the intervention to everyday life might limit the effects of the self-guided interventions (Conley et al., 2016; Pleva and Wade, 2006; Rosen, 1993; Rozental et al., 2014).
However, we should note that most of the existing evidence around the relative effectiveness of guided and unguided interventions is derived from studies focusing on changes in depressive and anxiety symptoms. Therefore, it remains unclear whether guided and self-guided stress management programs produce differential effects. Future studies should examine this comparison in a head-to-head fashion to shed light into the differential effectiveness of guided and self-guided interventions for psychological stress/distress. It is also plausible that the effectiveness of self-guided stress management programs may be increased by the provision of on-demand support or personalized automated messages. For instance, individuals with high levels of stress may find guidance on-demand more beneficial than regular guidance as they can maintain control over the intervention and request social support whenever it is necessary. Previous studies on psychological problems, such as stress or perfectionism, showed that internet-based interventions with guidance on-demand yielded similar effects with guided interventions (Zarski et al., 2016; Zetterberg et al., 2019). Moreover, in these studies, individuals contacted coaches rarely possibly due to the lack of perceived need for additional support. These findings do not necessarily imply lack of need for guided interventions because close monitoring and individualized feedback may be particularly relevant for certain groups like those who are at high risk of experiencing negative effects (Rozental et al., 2014). Therefore, different types and intensities of guidance in stress management programs, as well as predictors of differential response with regard to different guidance formats should be investigated thoroughly in future studies. Moreover, technological advancements could offer innovative tools to increase the effects of self-guided interventions. Persuasive technology strategies, particularly using automated reminders may be another cost-effective strategy to improve intervention outcomes by increasing engagement (Kelders et al., 2012; Brouwer et al., 2011). However, timing, frequency, content, and format (i.e., SMS, push notification, or email) of the automated reminders should be investigated with careful consideration since some participants may perceive them as stressful (Dennison et al., 2013). Last but not least, it is possible that some individuals benefit equally from guided and self-guided interventions as we have seen in the case of depression (Karyotaki et al., 2021). Such hypothesis, however, remains to be investigated in future research.
The low effect size could also be explained by sample characteristics. Our results showed that little improvement is possible in unselected student samples. In addition, studies targeting students with high levels of perceived stress yielded a slightly higher effect size than unselected student samples. Previously, higher baseline stress scores were found to be associated with the larger effect size of a web-based stress management program (Coudray et al., 2019). Studies also provided evidence on the larger effects in preselected student samples than unselected ones (Amanvermez et al., 2020; Conley et al., 2016; Harrer et al., 2019b). However, there are still unanswered questions about which students benefit most from self-guided stress management programs, as we did not directly test or compare this in the present study. Besides, it is not clear if stress management programs are also effective for people with subthreshold depression or anxiety, although recent RCT studies showed promising results (Harrer et al., 2021; Weisel et al., 2018).
In this study, the study dropout rates were comparable to those reported by studies on internet-based interventions for common mental health problems (Christensen et al., 2009; 1–50%; Harrer et al., 2019b; 2–50%; Melville et al., 2010; 0–82%). Nevertheless, it is important to differentiate between study dropout and intervention dropout. Intervention dropout refers to the situation in which the participant stops following the intervention before receiving the recommended dose (Donkin et al., 2011). It would have been important to investigate the possible impact of intervention dropout as it can be associated with the intervention outcomes (Karyotaki et al., 2017). However, the substantial variability of measuring/reporting the intervention adherence across the included studies prevented us from investigating this issue. This has been found as a general problem in similar interventions (Beintner et al., 2019). Future research should establish consensus about reporting criteria on adherence in digital intervention trials and investigate predictors and consequences of intervention dropout in self-guided stress management programs.
A large number of college students are experiencing stresses in several domains and scalable stress management interventions for college students are needed at universities (Karyotaki et al., 2020). The present study indicated that unselected student samples and students with pre-existing stress symptoms can benefit in the aggregate from self-guided stress management programs. These results allowed us to advance our knowledge of the effects of these programs in more detail.
Despite these strengths, some limitations should be emphasized while interpreting our results. First, we could only retrieve four studies targeting preselected samples and the number of participants was small in this meta-analysis. These results are underpowered and more studies should be conducted with large sample sizes to confirm our findings. Second, the risk of bias was substantial in the included studies. This limits the reliability of our results. Also, we modified the RoB 2 tool by removing one domain related to bias in outcome measurement and altering the criteria for assessing the overall risk of bias in each study, as this tool did not fit perfectly with the psychotherapy research. Third, the ecological validity of our study is unclear because individuals in RCTs may be more motivated to follow the intervention compared to real-world users of self-help (Cuijpers et al., 2010; Furmark et al., 2009). Moreover, we were not able to generalize our results to different (cultural) contexts. Our results generally were retrieved from the studies including predominantly female students pursuing a 4-year college education. This limits the representativeness of our results in students other than female, and non-college attending peers. Similarly, included studies were mainly conducted in high-income western countries, and our results may not be applicable for college students in low and middle-income countries, because there may be differences in sources of stress and contextual issues relating to the implementation of the interventions (Evans-Lacko and Thornicroft, 2019). Fourth, we are not aware of research on individual participant differences in response to self-guided stress management interventions. We still do not know whether these aggregate effects represent small homogeneous effects across all students or if there is a subset of students for whom these interventions have substantial effects and a larger subset for whom the interventions have no effects or possibly even negative effects. Investigation of this individual-level heterogeneity is critical for advancing our understanding of the most appropriate role for self-help interventions among college students. Such knowledge may help us in targeting the interventions to those who are most likely to benefit. Fifth, all studies used self-report measurements for stress, depression, and anxiety. Therefore, we could not investigate the effects of self-guided stress management programs on the biological measurement of stress such as cortisol. Sixth, the field of self-help has changed dramatically as more interventions have been developed based on information and communications technology (Haug et al., 2012; Rosen, 1993). Self-help tools such as books, websites, or mobile phone applications are used by large populations and barely evidence-based (Rosen, 1993; Walsh et al., 2019). Therefore, the effects of the self-help tools apart from the ones used in RCTs are unclear.
Despite these limitations and the need for more high-quality research, our study showed that self-guided stress management interventions are potentially beneficial for college students in general and college students with elevated levels of stress. These results are important from the public health standpoint, as several implications can be addressed for both implementations of the programs in higher education and future research. Self-guided stress management programs are offering great promise for college students because a large group of students may benefit from psychological interventions at a low cost. Although self-guided stress management programs yielded a small effect size, and possibly will not be a substitute for in-person interventions for more severe cases, such programs can be offered for college students as first-line mental health support within a stepped care framework.
Self-help approaches can be successful to prevent or alleviate the high stress and associated mental problems among college students. Although we found small effects of these programs, the effects might be larger for specific subgroups of students. Students may have different responses to these programs based on their characteristics (e.g. pre-existing symptoms). To this end, an in-depth investigation should be done addressing the preferences, needs, and opinions of subgroups within college students. This also requires further research inquiring into the effects of these programs using individual-participant data. Exploring the changing mechanisms in these programs will also contribute to the implementation of these programs.
Lack of human support has been repeatedly mentioned as a limitation in similar programs. On the other hand, self-help may increase willingness to seek professional help among college students. Therefore, innovative methods are worth investigating such as the different ways of increasing adherence and transferring common factors associated with improvement in face-to-face/guided programs into self-guided interventions. Internet-based interventions may be preferable since more personalized and scalable interventions can be designed based on the unique goals and needs of individuals. As a result, the most accurate strategies can be developed to outreach college students who are in the need of mental health help but do not access the relevant resources due to barriers.
Funding
The first author of this manuscript is funded for her doctoral studies by the Ministry of National Education, the Republic of Turkey.
CRediT authorship contribution statement
Yagmur Amanvermez: Conceptualization, Writing – original draft, Writing – review & editing, Validation. Ruiying Zhao: Writing – review & editing, Validation. Pim Cuijpers: Conceptualization, Writing – review & editing, Validation. Leonore M. de Wit: Conceptualization, Writing – review & editing, Validation. David D. Ebert: Writing – review & editing, Validation. Ronald C. Kessler: Writing – review & editing, Validation. Ronny Bruffaerts: Writing – review & editing, Validation. Eirini Karyotaki: Conceptualization, Writing – review & editing, Validation.
Declaration of competing interest
In the past 3 years, Dr. Kessler was a consultant for Datastat, Inc., Holmusk, RallyPoint Networks, Inc., and Sage Therapeutics. He has stock options in Mirah, PYM, and Roga Sciences.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.invent.2022.100503.
Appendix A. Supplementary data
Search Strings for the Systematic Literature Review.
References
- Amanvermez Y., Rahmadiana M., Karyotaki E., de Wit L., Ebert D.D., Kessler R.C., Cuijpers P. Stress management interventions for college students: A systematic review and meta-analysis. Clinical Psychology: Science and Practice. 2020;March doi: 10.1111/cpsp.12342. [DOI] [Google Scholar]
- Andrews G., Basu A., Cuijpers P., Craske M.G., Mcevoy P., English C.L., Newby J.M. Computer therapy for the anxiety and depression disorders is effective, acceptable and practical health care: an updated meta-analysis. J. Anxiety Disord. 2018;55(January):70–78. doi: 10.1016/j.janxdis.2018.01.001. [DOI] [PubMed] [Google Scholar]
- Astin J.A., Shapiro S.L., Eisenberg D.M., Forys K.L. Mind-body medicine: state of the science, implications for practice. J. Am. Board Fam. Pract. 2003;16:131–147. doi: 10.3122/jabfm.16.2.131. [DOI] [PubMed] [Google Scholar]
- Auerbach R.P., Mortier P., Bruffaerts R., Alonso J., Benjet C., Cuijpers P., Demyttenaere K., Ebert D.D., Green J.G., Hasking P., Murray E., Nock M.K., Pinder-Amaker S., Sampson N.A., Stein D.J., Vilagut G., Zaslavsky A.M., Kessler R.C., WHO WMH-ICS Collaborators WHO World Mental Health Surveys International College Student Project: Prevalence and distribution of mental disorders. J. Abnorm. Psychol. 2018;127(7):623–638. doi: 10.1037/abn0000362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry K.M, Woods M, Martin A, Stirling C, Warnecke E. A randomized controlled trial of the effects of mindfulness practice on doctoral candidate psychological status. J. Am. Coll. Health. 2019;67(4):299–307. doi: 10.1080/07448481.2018.1515760. [DOI] [PubMed] [Google Scholar]
- Baumeister H., Reichler L., Munzinger M., Lin J. The impact of guidance on internet-based mental health interventions—a systematic review. Internet Interv. 2014;1(4):205–215. [Google Scholar]
- Beintner I., Vollert B., Zarski A.C., Bolinski F., Musiat P., Görlich D., Ebert D.D., Jacobi C. Adherence reporting in randomized controlled trials examining manualized multisession online interventions: systematic review of practices and proposal for reporting standards. J. Med. Internet Res. 2019;21(8) doi: 10.2196/14181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beiter R., Nash R., Mccrady M., Rhoades D., Linscomb M., Clarahan M., Sammut S. The prevalence and correlates of depression, anxiety, and stress in a sample of college students. J. Affect. Disord. 2015;173:90–96. doi: 10.1016/j.jad.2014.10.054. [DOI] [PubMed] [Google Scholar]
- Bennett S.D., Cuijpers P., Ebert D.D., McKenzie Smith M., Coughtrey A.E., Heyman I., Manzotti G., Shafran R. Practitioner review: unguided and guided self-help interventions for common mental health disorders in children and adolescents: a systematic review and meta-analysis. J. Child Psychol. Psychiatry. 2019;60(8):828–847. doi: 10.1111/jcpp.13010. [DOI] [PubMed] [Google Scholar]
- Borenstein M., Hedges L.V., Higgins J.P., Rothstein H.R. Introduction to Meta-analysis. 2009. Multiple outcomes or time-points within a study. [Google Scholar]
- Brouwer W., Kroeze W., Crutzen R., de Nooijer J., de Vries N.K., Brug J., Oenema A. Which intervention characteristics are related to more exposure to internet-delivered healthy lifestyle promotion interventions? A systematic review. J. Med. Internet Res. 2011;13(1) doi: 10.2196/jmir.1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruffaerts R., Mortier P., Kiekens G., Auerbach R.P., Cuijpers P., Demyttenaere K., Green J.G., Nock M.K., Kessler R.C. Mental health problems in college freshmen: prevalence and academic functioning. J. Affect. Disord. 2018;225:97–103. doi: 10.1016/j.jad.2017.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruffaerts R., Mortier P., Auerbach R.P., Alonso J., Hermosillo De la Torre A.E., Cuijpers P., Demyttenaere K., Ebert D.D., Green J.G., Hasking P., Stein D.J., Ennis E., Nock M.K., Pinder-Amaker S., Sampson N.A., Vilagut G., Zaslavsky A.M., Kessler R.C., WHO WMH-ICS Collaborators Lifetime and 12-month treatment for mental disorders and suicidal thoughts and behaviors among first year college students. Int. J. Methods Psychiatr. Res. 2019;28(2) doi: 10.1002/mpr.1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burger K.G., Lockhart J.S. Meditation's effect on attentional efficiency, stress, and mindfulness characteristics of nursing students. J. Nurs. Educ. 2017;56(7):430–434. doi: 10.3928/01484834-20170619-08. [DOI] [PubMed] [Google Scholar]
- Carolan S., Harris P.R., Cavanagh K. Improving employee well-being and effectiveness: systematic review and meta-analysis of web-based psychological interventions delivered in the workplace. J. Med. Internet Res. 2017;19(7) doi: 10.2196/jmir.7583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanagh K., Strauss C., Cicconi F., Griffiths N., Wyper A., Jones F. A randomised controlled trial of a brief online mindfulness-based intervention. Behav. Res. Ther. 2013;51(9):573–578. doi: 10.1016/j.brat.2013.06.003. [DOI] [PubMed] [Google Scholar]
- Chiauzzi E., Brevard J., Thurn C., Decembrele S., Lord S. MyStudentBody–Stress: an online stress management intervention for college students. J. Health Commun. 2008;13(6):555–572. doi: 10.1080/10810730802281668. [DOI] [PubMed] [Google Scholar]
- Christensen H., Griffiths K.M., Farrer L. Adherence in internet interventions for anxiety and depression: systematic review. J. Med. Internet Res. 2009;11(2) doi: 10.2196/jmir.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. second edition. 1988. Statistical power analysis for the behavioral sciences. [DOI] [Google Scholar]
- Cohen S., Kessler R.C., Gordon L.U. Measuring Stress: A Guide for Health and Social Scientists. 1995. Strategies for measuring stress in studies of psychiatric and physical disorders; pp. 3–26. [Google Scholar]
- Cohen S., Gianaros P.J., Manuck S.B. A stage model of stress and disease. Perspect. Psychol. Sci. 2016;11(4):456–463. doi: 10.1177/1745691616646305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Murphy M., Prather A. Ten surprising facts about stressful life events and disease risk. Annu. Rev. Psychol. 2020;577–597 doi: 10.1146/annurev-psych-010418-102857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Williamson G.M. The Social Psychology of Health. 1988. Perceived stress in a probability sample of the United States; pp. 31–67. [Google Scholar]
- Cohen S., Janicki-Deverts D., Miller G.E. Psychological stress and disease. J. Am. Med. Assoc. 2007;298(14):1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- Conley C.S., Durlak J.A., Shapiro J.B., Kirsch A.C., Zahniser E. A meta-analysis of the impact of universal and indicated preventive technology-delivered interventions for higher education students. Prev. Sci. 2016;17(6):659–678. doi: 10.1007/s11121-016-0662-3. [DOI] [PubMed] [Google Scholar]
- Coudray C., Palmer R., Frazier P. Moderators of the efficacy of a web-based stress management intervention for college students. J. Couns. Psychol. 2019;66(6):747–754. doi: 10.1037/cou0000340. [DOI] [PubMed] [Google Scholar]
- Cuijpers P., Donker T., Van Straten A., Li J., Andersson G. Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychol. Med. 2010;40(12):1943–1957. doi: 10.1017/S0033291710000772. [DOI] [PubMed] [Google Scholar]
- Cuijpers P., Miguel C., Ciharova M., Aalten P., Batelaan N., Salemink E., Spinhoven P., Struijs S., de Wit L., Gentili C., Ebert D., Harrer M., Bruffaerts R., Kessler R.C., Karyotaki E. Prevention and treatment of mental health and psychosocial problems in college students: an umbrella review of meta-analyses. Clin. Psychol. Sci. Pract. 2021;28(3):229–244. doi: 10.1037/cps0000030. [DOI] [Google Scholar]
- Cuijpers P., Noma H., Karyotaki E., Cipriani A., Furukawa T. Effectiveness and acceptability of cognitive behavior therapy delivery formats in adults with depression a network meta-analysis. JAMA Psychiat. 2019;76(7):700–707. doi: 10.1001/jamapsychiatry.2019.0268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P., Schuurmans J. Self-help interventions for anxiety disorders: an overview. Curr. Psychiatry Rep. 2007;9(4):284–290. doi: 10.1007/s11920-007-0034-6. [DOI] [PubMed] [Google Scholar]
- Cuijpers P., Cristea I.A., Ebert D.D., Koot H.M., Auerbach R.P., Bruffaerts R., Kessler R.C. Psychological treatment of depression in college students: a metaanalysis. Depression and Anxiety. 2016;33(5):400–414. doi: 10.1002/da.22461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czyz E.K., Horwitz A.G., Eisenberg D., Kramer A., King C.A. Self-reported barriers to professional help seeking among college students at elevated risk for suicide. J. Am. Coll. Health. 2013;61(7):398–406. doi: 10.1080/07448481.2013.820731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies E.B., Morriss R., Glazebrook C. Computer-delivered and web-based interventions to improve depression, anxiety, and psychological well-being of university students: a systematic review and meta-analysis. J. Med. Internet Res. 2014;16(5):1–22. doi: 10.2196/jmir.3142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Girolamo G., Dagani J., Purcell R., Cocchi A., Mcgorry P.D. Age of onset of mental disorders and use of mental health services: needs, opportunities and obstacles. Epidemiol. Psychiatr. Sci. 2015;21(1):47–57. doi: 10.1017/S2045796011000746. [DOI] [PubMed] [Google Scholar]
- Deady M., Choi I., Calvo R.A., Glozier N., Christensen H., Harvey S.B. eHealth interventions for the prevention of depression and anxiety in the general population: A Systematic Review and Meta-analysis. 2017. pp. 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennison L., Morrison L., Conway G., Yardley L. Opportunities and challenges for smartphone applications in supporting health behavior change: qualitative study. J. Med. Internet Res. 2013;15(4) doi: 10.2196/jmir.2583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domhardt M., Geßlein H., von Rezori R.E., Baumeister H. Internet- and mobile-based interventions for anxiety disorders: a meta-analytic review of intervention components. Depress. Anxiety. 2019;36(3):213–224. doi: 10.1002/da.22860. [DOI] [PubMed] [Google Scholar]
- Donkin L., Christensen H., Naismith S.L., Neal B., Hickie I.B., Glozier N. A systematic review of the impact of adherence on the effectiveness of e-therapies. J. Med. Internet Res. 2011;13(3) doi: 10.2196/jmir.1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duval S., Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000 doi: 10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Ebert D.D., Mortier P., Kaehlke F., Bruffaerts R., Baumeister H., Auerbach R.P., Alonso J., Vilagut G., Martínez K.U., Lochner C., Cuijpers P., Kuechler A.M., Green J., Hasking P., Lapsley C., Sampson N.A., Kessler R.C., WHO World Mental Health—International College Student Initiative collaborators Barriers of mental health treatment utilization among first-year college students: First cross-national results from the WHO World Mental Health International College Student Initiative. Int. J. Methods Psychiatr. Res. 2019;28(2) doi: 10.1002/mpr.1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. Br. Med. J. 1997 doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg D., Golberstein E., Hunt J.B. Mental health and academic success in college. B.E. J. Econ. Anal. Policy. 2009;9(1) doi: 10.2202/1935-1682.2191. [DOI] [Google Scholar]
- Evans-Lacko S., Thornicroft G. Viewpoint: WHO world mental health surveys international college student initiative: implementation issues in low- and middle-income countries. Int. J. Methods Psychiatr. Res. 2019;28(2):1–5. doi: 10.1002/mpr.1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn C.G., Patel V. The impact of digital technology on psychological treatments and their dissemination. Behav. Res. Ther. 2017;88:19–25. doi: 10.1016/j.brat.2016.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fehring R.J. Effects of biofeedback-aided relaxation on the psychological stress symptoms of college students. Nurs. Res. 1983;32(6):362–366. doi: 10.1097/00006199-198311000-00009. [DOI] [PubMed] [Google Scholar]
- Flett J.A., Conner T.S., Riordan B.C., Patterson T., Hayne H. App-based mindfulness meditation for psychological distress and adjustment to college in incoming university students: a pragmatic, randomised, waitlist-controlled trial. Psychol. Health. 2020;35(9):1049–1074. doi: 10.1080/08870446.2019.1711089. [DOI] [PubMed] [Google Scholar]
- Flett J.A., Hayne H., Riordan B.C., Thompson L.M., Conner T.S. Mobile mindfulness meditation: a randomised controlled trial of the effect of two popular apps on mental health. Mindfulness. 2019;10(5):863–876. doi: 10.1007/s12671-018-1050-9. [DOI] [Google Scholar]
- Frazier P., Keenan N., Anders S., Perera S., Shallcross S., Hintz S. Perceived past, present, and future control and adjustment to stressful life events. J. Pers. Soc. Psychol. 2011;100(4):749–765. doi: 10.1037/a0022405. [DOI] [PubMed] [Google Scholar]
- Frazier P., Meredith L., Greer C., Paulsen J.A., Howard K., Dietz L.R., Qin K. Randomized controlled trial evaluating the effectiveness of a web-based stress management program among community college students. Anxiety Stress Coping. 2015;28(5):576–586. doi: 10.1080/10615806.2014.987666. [DOI] [PubMed] [Google Scholar]
- Furmark T., Carlbring P., Hedman E., Sonnenstein A., Clevberger P., Bohman B.…Andersson G. Guided and unguided self-help for social anxiety disorder: Randomised controlled trial. Br. J. Psychiatry. 2009;195(5):440–447. doi: 10.1192/bjp.bp.108.060996. [DOI] [PubMed] [Google Scholar]
- Graves T.A., Tabri N., Thompson-Brenner H., Franko D.L., Eddy K.T., Bourion-Bedes S., Brown A., Constantino M.J., Flückiger C., Forsberg S., Isserlin L., Couturier J., Paulson Karlsson G., Mander J., Teufel M., Mitchell J.E., Crosby R.D., Prestano C., Satir D.A., Simpson S., Sly R., Lacey J.H., Stiles-Shields C., Tasca G.A., Waller G., Zaitsoff S.L., Rienecke R., Le Grange D., Thomas J.J. A meta-analysis of the relation between therapeutic alliance and treatment outcome in eating disorders. Int. J. Eat. Disord. 2017;50:323–340. doi: 10.1002/eat.22672. [DOI] [PubMed] [Google Scholar]
- Hammen C.L. Stress and depression: old questions, new approaches. Curr. Opin. Psychol. 2015;4:80–85. [Google Scholar]
- Harrer M., Cuijpers P., Furukawa T.A., Ebert D.D. Doing meta-analysis with R: a hands-on guide. 2019. https://bookdown.org/MathiasHarrer/Doing_Meta_Analysis_in_R/
- Harrer M., Adam S.H., Baumeister H., Cuijpers P., Karyotaki E., Auerbach R.P., Ebert D.D. Internet interventions for mental health in university students: a systematic review and meta-analysis. Int. J. Methods Psychiatr. Res. 2019;28(2):1–18. doi: 10.1002/mpr.1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrer M., Apoliario-Hagen J., Fritsche L., Salewski C., Apolin J., Zarski A., Ebert D.D. Effect of an internet- and app-based stress intervention compared to online psychoeducation in university students with depressive symptoms?: results of a randomized controlled trial. Internet Interv. 2021;24(February) doi: 10.1016/j.invent.2021.100374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haug T., Nordgreen T., Öst L.G., Havik O.E. Self-help treatment of anxiety disorders: a meta-analysis and meta-regression of effects and potential moderators. Clin. Psychol. Rev. 2012;32(5):425–445. doi: 10.1016/j.cpr.2012.04.002. [DOI] [PubMed] [Google Scholar]
- Hayes S.C., Hofmann S.G. The third wave of cognitive behavioral therapy and the rise of process-based care. World Psychiatry. 2017;16(3):245–246. doi: 10.1002/wps.20442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazlett-Stevens H., Oren Y. Effectiveness of mindfulness-based stress reduction bibliotherapy: a preliminary randomized controlled trial. J. Clin. Psychol. 2017;73(6):626–637. doi: 10.1002/jclp.22370. [DOI] [PubMed] [Google Scholar]
- Heber E., Ebert D.D., Lehr D., Cuijpers P., Berking M., Nobis S., Riper H. The benefit of web- and computer-based interventions for stress: a systematic review and meta-analysis. J. Med. Internet Res. 2017;19(2) doi: 10.2196/jmir.5774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry J.D., Crawford J.R. The short-form version of the depression anxiety stress scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2005;44(2):227–239. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. Br. Med. J. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hintz S., Frazier P.A., Meredith L. Evaluating an online stress management intervention for college students. Journal of Counseling Psychology. 2015;62(2):137–147. doi: 10.1037/cou0000014. [DOI] [PubMed] [Google Scholar]
- Hockemeyer J., Smyth J. Evaluating the feasibility and efficacy of a self-administered manual-based stress management intervention for individuals with asthma: results from a controlled study. Behav. Med. 2002;27(4):161–172. doi: 10.1080/08964280209596041. [DOI] [PubMed] [Google Scholar]
- Huberty J., Green J., Glissmann C., Larkey L., Puzia M., Lee C. Efficacy of the mindfulness meditation mobile app “Calm” to reduce stress among college students: randomized controlled trial. JMIR Mhealth Uhealth. 2019;7(6):e14273. doi: 10.2196/14273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ioannidis J.P.A., Patsopoulos N.A., Evangelou E. Uncertainty in heterogeneity estimates in meta-analyses. BMJ. 2007;335(7626):914–916. doi: 10.1136/bmj.39343.408449.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karyotaki E., Riper H., Twisk J., Hoogendoorn A., Kleiboer A., Mira A.…Cuijpers P. Efficacy of self-guided internet-based cognitive behavioral therapy in the treatment of depressive symptoms: a meta-analysis of individual participant data. JAMA Psychiat. 2017;74(4):351–359. doi: 10.1001/jamapsychiatry.2017.0044. [DOI] [PubMed] [Google Scholar]
- Kanekar A., Sharma M., Atri A. Enhancing social support, hardiness, and acculturation to improve mental health among Asian Indian international students. Int. Q. Community Health Educ. 2010;30(1):55–68. doi: 10.2190/IQ.30.1.e. [DOI] [PubMed] [Google Scholar]
- Karyotaki E., Cuijpers P., Albor Y., Alonso J., Auerbach R.P., Bruffaerts R., Kessler R.C. Sources of stress and their associations with mental disorders among college students: results of the World Health Organization World Mental Health Surveys International College Student Initiative. Front. Psychol. 2020;11:1759. doi: 10.3389/fpsyg.2020.01759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karyotaki E., Efthimiou O., Miguel C., Bermpohl F.M.G., Furukawa T.A., Cuijpers P.…Forsell Y. Internet-based cognitive behavioral therapy for depression: a systematic review and individual patient data network meta-analysis. JAMA Psychiat. 2021;78(4):361–371. doi: 10.1001/jamapsychiatry.2020.4364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelders S.M., Kok R.N., Ossebaard H.C., Van Gemert-Pijnen J.E. Persuasive system design does matter: a systematic review of adherence to web-based interventions. J. Med. Internet Res. 2012;14(6) doi: 10.2196/jmir.2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Amminger G.P., Aguilar-Gaxiola S., Alonso J., Lee S., Üstün T.B. Age of onset of mental disorders: a review of recent literature. Curr. Opin. Psychiatry. 2007;20(4):359–364. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer H.C., Kupfer D.J. Size of treatment effects and their importance to clinical research and practice. Biol. Psychiatry. 2006;59(11):990–996. doi: 10.1016/j.biopsych.2005.09.014. [DOI] [PubMed] [Google Scholar]
- Kvillemo P., Brandberg Y., Bränström R. Feasibility and outcomes of an internet-based mindfulness training program: A pilot randomized controlled trial. JMIR Mental Health. 2016;3(3) doi: 10.2196/mental.5457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lattie E.G., Adkins E.C., Winquist N., Stiles-shields C., Eileen Q., Graham A.K. Digital mental health interventions for depression, anxiety, and enhancement of psychological well-being among college students: systematic review. J. Med. Internet Res. 2019;21(7) doi: 10.2196/12869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee R.A., Jung M.E. Evaluation of an mhealth app (destressify) on university students’ mental health: Pilot trial. J. Med. Internet Res. 2018;5(1) doi: 10.2196/mental.8324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leppink E.W., Odlaug B.L., Lust K., Christenson G., Grant J.E. The young and the stressed: stress, impulse control, and health in college students. J. Nerv. Ment. Dis. 2016;204(12):931–938. doi: 10.1097/NMD.0000000000000586. [DOI] [PubMed] [Google Scholar]
- Levin M.E., Hayes S.C., Pistorello J., Seeley J.R. Web-based self-help for preventing mental health problems in universities: comparing acceptance and commitment training to mental health education. J. Clin. Psychol. 2016;72(3):207–225. doi: 10.1002/jclp.22254. [DOI] [PubMed] [Google Scholar]
- Levin M.E., Pistorello J., Seeley J.R., Hayes S.C. Feasibility of a prototype web-based acceptance and commitment therapy prevention program for college students. J. Am. Coll. Heal. 2014;62(1):20–30. doi: 10.1080/07448481.2013.843533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leviness P., Gorman K., Braun L., Services A., Koenig L., Health C., Services A. 2019. The Association for University and College Counseling Center Directors Annual Survey: 2019.https://www.aucccd.org/assets/documents/Survey/2019%20AUCCCD%20Survey-2020-05-31-PUBLIC.pdf [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A.…Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J. Clin. Epidemiol. 2009;62(10):e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- Lovibond P.F., Lovibond S.H. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the Beck depression and anxiety inventories. Behav. Res. Ther. 1995;33(3):335–343. doi: 10.1007/BF02511245. [DOI] [PubMed] [Google Scholar]
- Mains J.A., Scogin F.R. The effectiveness of self-administered treatments: a practice-friendly review of the research. J. Clin. Psychol. 2003;59(2):237–246. doi: 10.1002/jclp.10145. [DOI] [PubMed] [Google Scholar]
- Marsh C.N., Wilcoxon S.A. Underutilization of mental health services among college students: an examination of system-related barriers. J. Coll. Stud. Psychother. 2015;29(3):227–243. doi: 10.1080/87568225.2015.1045783. [DOI] [Google Scholar]
- Melnyk B.M., Amaya M., Szalacha L.A., Hoying J., Taylor T., Bowersox K. Feasibility, acceptability, and preliminary effects of the COPE online cognitive-behavioral skill-building program on mental health outcomes and academic performance in freshmen college students: a randomized controlled pilot study. J. Child Adolesc. Psychiatr. Nurs. 2015;28(3):147–154. doi: 10.1111/jcap.12119. [DOI] [PubMed] [Google Scholar]
- Melville K.M., Casey L.M., Kavanagh D.J. Dropout from internet-based treatment for psychological disorders. Br. J. Clin. Psychol. 2010;49(4):455–471. doi: 10.1348/014466509X472138. [DOI] [PubMed] [Google Scholar]
- Mohr D.C., Cuijpers P., Lehman K. Supportive accountability: a model for providing human support to enhance adherence to eHealth interventions. J. Med. Internet Res. 2011;13(1) doi: 10.2196/jmir.1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe S.M. Modern approaches to conceptualizing and measuring human life stress. Annu. Rev. Clin. Psychol. 2008;4:33–52. doi: 10.1146/annurev.clinpsy.4.022007.141207. [DOI] [PubMed] [Google Scholar]
- Mortier P., Cuijpers P., Kiekens G., Auerbach R.P., Demyttenaere K., Green J.G.…Bruffaerts R. The prevalence of suicidal thoughts and behaviours among college students: a meta-analysis. Psychol. Med. 2018;48(4):554–565. doi: 10.1017/S0033291717002215. [DOI] [PubMed] [Google Scholar]
- Muto T., Hayes S.C., Jeffcoat T. The effectiveness of acceptance and commitment therapy bibliotherapy for enhancing the psychological health of Japanese college students living abroad. Behav. Ther. 2011;42(2):323–335. doi: 10.1016/j.beth.2010.08.009. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence . NICE guideline CG123. 2020. Common mental health disorders: identification and pathways to care.http://books.google.com/books?hl=en&lr=&id=_8h2mZD9w1IC&oi=fnd&pg=PA79&dq=Common+mental+health+disorders&ots=Sp4_V4D9iH&sig=qQck0LdU26ypNwwC5XnHvmD2Qss Retrieved from. [PubMed] [Google Scholar]
- Nguyen-Feng V.N., Frazier P.A., Greer C.S., Howard K.G., Paulsen J.A., Meredith L., Kim S. A randomized controlled trial of a web-based intervention to reduce distress among students with a history of interpersonal violence. Psychol. Violence. 2015;5(4):444–454. [Google Scholar]
- Nguyen-Feng V.N., Greer C.S., Frazier P. Using online interventions to deliver college student mental health resources: evidence from randomized clinical trials. Psychol. Serv. 2017;14(4):481. doi: 10.1037/ser0000154. [DOI] [PubMed] [Google Scholar]
- Nguyen-Feng V.N., Frazier P.A., Greer C.S., Howard K.G., Paulsen J.A., Meredith L., Kim S. A randomized controlled trial of a web-based intervention to reduce distress among students with a history of interpersonal violence. Psychol. Violence. 2015;5(4):444–454. [Google Scholar]
- Nixon P., Boß L., Heber E., Ebert D.D., Lehr D. A three-armed randomised controlled trial investigating the comparative impact of guidance on the efficacy of a web-based stress management intervention and health impairing and promoting mechanisms of prevention. BMC Public Health. 2021;21(1):1–18. doi: 10.1186/s12889-021-11504-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Driscoll M., Byrne S., Byrne H., Lambert S., Sahm L.J. An online mindfulness-based intervention for undergraduate pharmacy students: results of a mixed-methods feasibility study. Curr. Pharm. Teach. Learn. 2019;11(9):858–875. doi: 10.1016/j.cptl.2019.05.013. [DOI] [PubMed] [Google Scholar]
- Ong L., Linden W., Young S. Stress management what is it? J. Psychosom. Res. 2004;56:133–137. doi: 10.1016/S0022-3999(03)00128-4. [DOI] [PubMed] [Google Scholar]
- Paholpak S., Piyavhatkul N., Rangseekajee P., Krisanaprakornkit T., Arunpongpaisal S., Pajanasoontorn N.…Unprai P. Breathing meditation by medical students at Khon Kaen University: Effect on psychiatric symptoms, memory, intelligence and academic acheivement. J. Med. Assoc. Thail. 2012;95(3):461–469. [PubMed] [Google Scholar]
- Pleva J., Wade T.D. Guided self-help versus pure self-help for perfectionism: a randomised controlled trial. Behav. Res. Ther. 2006;45:849–861. doi: 10.1016/j.brat.2006.08.009. [DOI] [PubMed] [Google Scholar]
- Richardson K.M., Rothstein H.R. Effects of occupational stress management intervention programs: a meta-analysis. J. Occup. Health Psychol. 2008;13(1):69–93. doi: 10.1037/1076-8998.13.1.69. [DOI] [PubMed] [Google Scholar]
- Ponzo S., Morelli D., Kawadler J.M., Hemmings N.R., Bird G., Plans D. Efficacy of the digital therapeutic mobile app biobase to reduce stress and improve mental well-being among university students: Randomized controlled trial. JMIR Mhealth Uhealth. 2020;8(4) doi: 10.2196/17767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson R., Richards D.A., Barkham M. Self-help books for people with depression: a scoping review. J. Ment. Health. 2009;17(5):543–552. doi: 10.1080/09638230802053334. [DOI] [Google Scholar]
- Ridner S.H. Psychological distress: concept analysis. J. Adv. Nurs. 2004;45(5):536–545. doi: 10.1046/j.1365-2648.2003.02938.x. [DOI] [PubMed] [Google Scholar]
- Rosen G.M. Self-help or hype? Comments on psychology’s failure to advance self-care. Prof. Psychol. Res. Pract. 1993;24(3):340–345. doi: 10.1037//0735-7028.24.3.340. [DOI] [Google Scholar]
- Rozental A., Andersson G., Boettcher J., Ebert D.D., Cuijpers P., Knaevelsrud C., Ljótsson B., Kaldo V., Titov N., Carlbring P. Consensus statement on defining and measuring negative effects of Internet interventions. Internet Interv. 2014;1(1):12–19. doi: 10.1016/j.invent.2014.02.001. [DOI] [Google Scholar]
- Saleh D., Camart N., Sbeira F., Romo L. Can we learn to manage stress? A randomized controlled trial carried out on university students. PLoS ONE. 2018;13(9) doi: 10.1371/journal.pone.0200997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salzer M.S. A comparative study of campus experiences of college students with mental illnesses versus a general college sample. J. Am. Coll. Heal. 2012;60(1):1–7. doi: 10.1080/07448481.2011.552537. [DOI] [PubMed] [Google Scholar]
- Schwarzer G. R News. Vol. 7. 2007. Meta: an R package for meta-analysis.http://cran.r-project.org/doc/Rnews/ Retrieved from. [Google Scholar]
- Stallman H.M., Shochet I. Prevalence of mental health problems in Australian university health services. Aust. Psychol. 2009;44(2):122–127. doi: 10.1080/00050060902733727. [DOI] [Google Scholar]
- Sterne J.A.C., Savović J., Page M.J., Elbers R.G., Blencowe N.S., Boutron I., Higgins J.P.T. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366(August) doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- Stratton E., Lampit A., Choi I., Calvo R.A., Harvey S.B., Glozier N. Effectiveness of eHealth interventions for reducing mental health conditions in employees: a systematic review and meta-analysis. PloS one. 2017;12(12) doi: 10.1371/journal.pone.0189904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman S., Arnett J.J. Emerging adulthood: developmental period facilitative of the addictions. Eval. Health Profess. 2014;37(2):147–155. doi: 10.1177/0163278714521812. [DOI] [PubMed] [Google Scholar]
- Taylor B.L., Strauss C., Cavanagh K., Jones F. The effectiveness of self-help mindfulness-based cognitive therapy in a student sample: a randomised controlled trial. Behav. Res. Ther. 2014;63(December 2014):63–69. doi: 10.1016/j.brat.2014.09.007. [DOI] [PubMed] [Google Scholar]
- Ugalde A., Haynes K., Boltong A., White V., Krishnasamy M., Schofield P., Aranda S., Livingston P. Self-guided interventions for managing psychological distress in people with cancer–a systematic review. Patient Educ. Couns. 2017;100(5):846–857. doi: 10.1016/j.pec.2016.12.009. [DOI] [PubMed] [Google Scholar]
- Viechtbauer W. Conducting meta-analyses in R with the metafor. J. Stat. Softw. 2010;36(3):1–48. [Google Scholar]
- Viskovich S., Pakenham K.I. Randomized controlled trial of a web-based Acceptance and Commitment Therapy (ACT) program to promote mental health in university students. J. Clin. Psychol. 2020;76(6):929–951. doi: 10.1002/jclp.22848. [DOI] [PubMed] [Google Scholar]
- Walsh K.M., Saab B.J., Farb N.A.S. Effects of a mindfulness meditation app on subjective well-being: active randomized controlled trial and experience sampling study. J. Med. Internet Res. 2019;21(1) doi: 10.2196/10844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wampold B.E. How important are the common factors in psychotherapy?An update. World Psychiatry. 2015;14(3):270–277. doi: 10.1002/wps.20238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins D.C., Hunt J.B., Eisenberg D. Increased demand for mental health services on college campuses: perspectives from administrators. Qual. Soc. Work. 2011;11(3):319–337. doi: 10.1177/1473325011401468. [DOI] [Google Scholar]
- Watson D., Clark L.A., Weber K., Assenheimer J.S., Strauss M.E., McCormick R.A. Testing a tripartite model: II. Exploring the symptom structure of anxiety and depression in student, adult, and patient samples. J. Abnorm. Psychol. 1995;104(1):15. doi: 10.1037//0021-843x.104.1.15. [DOI] [PubMed] [Google Scholar]
- Weisel K.K., Lehr D., Heber E., Zarski A., Riper H., Ebert D.D. Severely burdened individuals do not need to be excluded from internet-based and mobile-based stress management: effect modifiers of treatment outcomes from three randomized controlled trials. J. Med. Internet Res. 2018;20(6) doi: 10.2196/jmir.9387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang E., Schamber E., Meyer R.M.L., Gold J.I. Happier healers: randomized controlled trial of mobile mindfulness for stress management. J. Altern. Complement. Med. 2018;24(5):505–513. doi: 10.1089/acm.2015.0301. [DOI] [PubMed] [Google Scholar]
- Zarski A.C., Lehr D., Berking M., Riper H., Cuijpers P., Ebert D.D. Adherence to internet-based mobile-supported stress management: a pooled analysis of individual participant data from three randomized controlled trials. J. Med. Internet Res. 2016;18(6) doi: 10.2196/jmir.4493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zetterberg M., Carlbring P., Andersson G., Berg M., Shafran R., Rozental A. Internet-based cognitive behavioral therapy of perfectionism: comparing regular therapist support and support upon request. Internet Interv. 2019;17 doi: 10.1016/j.invent.2019.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou T., Li X., Pei Y., Gao J., Kong J. Internet-based cognitive behavioural therapy for subthreshold depression: a systematic review and meta-analysis. BMC Psychiatry. 2016;16(1):356. doi: 10.1186/s12888-016-1061-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search Strings for the Systematic Literature Review.