Abstract
Precision medicine presents challenges for effective return of results (ROR) to patients, particularly for variants of uncertain significance (VUS) where the need for genetic counseling and the impact of results are underexplored. We investigated patients’ experiences with VUS ROR. Through interviews we compared experiences of patients who were referred to genetic counseling with those not referred. Although participants from both groups (n=16) reported curious enthusiasm and relief after ROR, the 5 referred participants reported less confusion, less disappointment, and better confidence in understanding their results than the 11 non-referred participants. Although VUS did not impact healthcare or daily lives, some participants who shared VUS fostered communication about future healthcare. Suggested ROR improvements included patient-friendly terminology, on-demand education, and ongoing consultation. Although patient experience of VUS improved when ROR involved expert consultation, scarcity of genetic counselors presents challenges. Improving the ROR process with patient-centered solutions could enhance the patient experience of receiving VUS.
Introduction
As precision medicine becomes integrated into healthcare, questions emerge about how best to return genetic results to patients, particularly for variants of uncertain significance (VUS). VUS are genetic changes for which the association with disease is unknown. Although the American College of Medical Genetics and Genomics recommends reporting incidental or secondary findings from actionable genes that are not the target of testing in clinical practice,1,2 they recommend against returning VUS as a secondary finding. However, when VUS are primary findings, detected for a gene that is the target of the ordered test, VUS are generally clinically returned even though most are not clinically actionable nor found to be pathogenic.3
Strategies for returning genomic results range from in-person/phone consultation4,5 to passive notification through patient portals or mailed letters.6 Prior work has examined patient experience with return of genomic results in general. For example, patient-friendly genomic test reports have been designed to improve patient engagement and understanding of complex genetic data.7 More advanced tools for returning results, such as “My46”, offer self-guided management of results.8 Other researchers have infused direct-to-consumer personal genomic reports interactive features to enhance understanding.9 Prior work has examined patient experience with such patient-facing strategies for return of genomic test results. For example, patient-facing genomic reports have been shown to improve patient communication with providers, educators, and therapists, which led to increased engagement and satisfaction.10 Yet, how such strategies impact the patient experience of receiving VUS remains poorly understood.
Clift et al.11 call attention to the potential for patient misinterpretation of VUS and the need for counseling and education for both patients and providers. Although the behavioral and experiential consequences of receiving a VUS results are not well studied, early evidence suggests taking caution in how VUS are returned. In a study on return of Lynch Syndrome related VUS results, Soloman et al.12 found that patients may be surprised by VUS and interpret its clinical significance in a wide range of ways. Similarly, patients who received VUS demonstrated mixed understanding and expressed both uncertainty about the impact of VUS on clinical management and concern for family members’ wellbeing.13 However, these studies did not examine the impact of how results were returned on patients’ experiences. Given the uncertainty associated with VUS, better understanding this experience can inform effective return of result (ROR) strategies that patients find acceptable.
Methods
The objective of this qualitative study was to investigate the ROR experience of patients for VUS. We conducted semi-structured interviews to compare participants’ experiences of receiving VUS with and without referral to clinical genetics.
Study setting and recruitment
This study takes place within the context of The Electronic Medical Records and Genomics network (eMERGE).14 eMERGE began in 2007 to develop best practices for genomic research in bio-repositories linked with electronic health records (EHR). As a collaborating site in eMERGE, Kaiser Permanente Washington and the University of Washington conducted a comprehensive program of genomic discovery and clinical implementation research15 in which genetic results for bio-repository participants were integrated into the EHR.
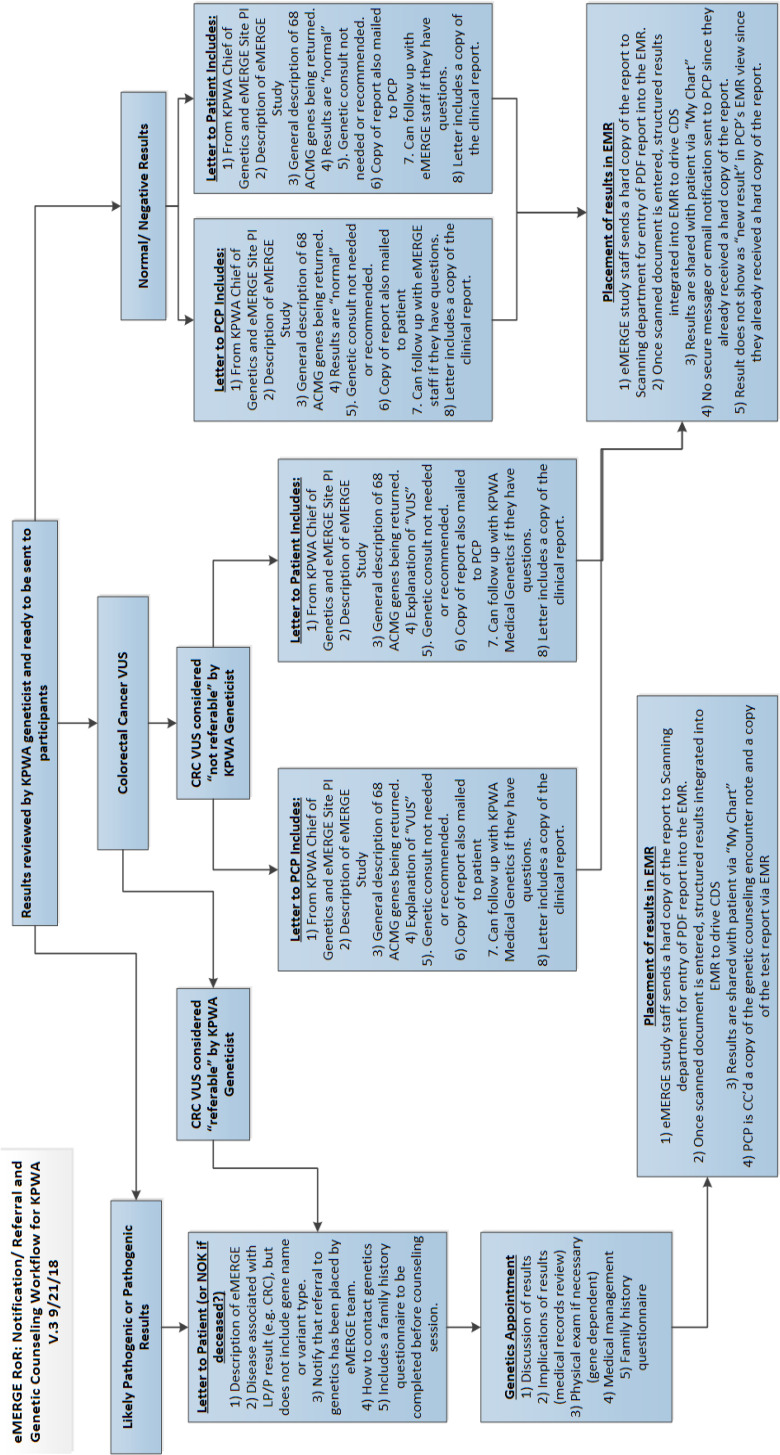
Our study population was eMERGE participants with a colorectal cancer (CRC) diagnosis or colon polyps and a VUS, including those referred and not referred to clinical genetics to receive counseling for their VUS. Only participants with a VUS in one of the genes associated with Lynch syndrome were referred for genetic counseling and in-person ROR. Other VUS were not offered genetic counseling (Figure 1). Inclusion criteria were being a Kaiser Permanente member and remembering receiving the VUS.
Figure 1.
Colorectal cancer VUS ROR workflow detailing how participants were assigned referred/non-referred status after review by Kaiser Permanente Washington (KPWA) geneticist and how results were sent to patients.
Participants with a VUS who were referred to genetic counseling received a mailed letter describing the study and results written at 8th grade level and a referral for clinical genetics consultation. Results were returned during consultation, and then placed in the EHR and accessible to the participant via the patient portal. The participant’s primary care provider was sent a copy of the results and consultation. Participants with a VUS who were not referred also received the mailed letter, and their results were sent to their primary care providers and placed in the EHR, where they were accessible to the patient via the patient portal. Participants who were not referred were considered an appropriate comparison as they did not have a VUS in one of the Lynch syndrome genes and as a result did not receive in-person genetic consultation.
We sent study invitation letters to 108 participants of whom 32 were referred (30%) and 76 were not referred (70%). Forty-six (43%) responded (17 referred, 29 not referred) and completed a phone screening. Of those screened, 29 declined (11 referred, 18 not referred) and one who was referred failed to meet inclusion criteria.
Data collection and analysis
From March to April of 2019, one member of the research team (AH) conducted interviews using a semi-structured guide covering participants’ experience with the VUS ROR process (Table 1). Interview questions covered the following domains: 1) emotional and cognitive reactions to receiving VUS, 2) whether and how they shared results with healthcare providers, family, or friends, 3) perceived impact of results on their healthcare and daily life, and 4) recommended improvements to the ROR process given perceived benefits and barriers. We collected age, gender, race, ethnicity, education, and self-reported familiarity with genetics on a 5-point Likert scale from 1 “not at all familiar” to 5 “extremely familiar”.
Table 1.
Interview guide
| Domain | Prompt |
| Reaction to VUS |
|
| Sharing VUS | Did you discuss or share your results with anyone?
|
| Perceived impact |
|
| Recommended improvements |
|
Interviews were audio-recorded and transcribed for qualitative analysis. Two coders (HP, AH) used template analysis16 to deductively code transcripts in Dedoose17 following the four domains of the interview guide. Once the coders achieved intercoder reliability of K=0.90 on a 25% sample of transcript excerpts, the remaining transcripts were split between coders and independently coded. After coding was complete, we compared experiences by domain between participants who were referred and not referred.
Results
Participants
Of the 16 participants (P1-P16), 5 were referred for genetic counseling (P5, P6, P8, P10, P12) and 11 were not referred. Participants were largely white, non-Hispanic/Latino, and female, ranged in age from 43 to 82 years old (mean=66), and had varied education and familiarity with genetics (Table 2).
Table 2.
Participant Demographics
| All N (%) | Referred N (%) | Not referred N (%) | ||
| Age | Mean age (SD)Median (range) | 66 (11) years 69 (43-82) years |
72 (7) years 73 (63-82) years |
63 (11) years 68 (43-75) years |
| Sex | Male Female |
5 (31%) 11 (69%) |
2 (40%) 3 (60%) |
3 (27%) 8 (73%) |
| Race | White African-American More than 1 race Undisclosed |
11 (69%) 1 (6%) 1 (6%) 3 (19%) |
4 (80%) - 1 (20%) - |
7 (64%) 1 (9%) - 3 (27%) |
| Ethnicity | Hispanic or Latino Not Hispanic or LatinoUndisclosed |
- 15 (94%) 1 (6%) |
- 5 (100%) - |
- 8 (73%) 3 (27%) |
| Education level | High school degreeCollege degree Post graduate degree Undisclosed |
3 (19%) 7 (44%) 6 (37%) - |
- 2 (40%) 3 (60% - |
1 (9%) 4 (37%) 3 (27%) 3 (27%) |
| Familiarity with genetics (out of 5) | Median (range) | 2 (1-4) | 3 (2-4) | 2 (1-4) |
| CRC status | Colon polyp CRC diagnosis | 12 (75%) 4 (25%) |
3 (60%) 2 (40%) |
9 (82%) 2 (18%) |
1. Reaction to VUS
Participants’ emotional reactions varied when asked “Overall, how would you describe your experience with receiving your results?”. Those who were referred primarily reported enthusiasm, curiosity, and relief:
“I like that kind of stuff so I was excited to get it. Didn't really understand what it was.” (P6, referred)
“[I felt] curious and intrigued … It was something that I was kind of interested in, seeing how it happened and what the results were.” (P12, referred)
“I was a little bit relieved, I guess, because from the day I had the colonoscopy and they took the sample, I -- the surgeon said, you know, I saved your life. And then -- but everybody else since then has been very noncommittal as to whether I had cancer or not. And so finally, this study, I will say that, that it came right out in front and said it was cancerous.” (P5, referred)
Although most who were not referred shared similar sentiments of curious enthusiasm and relief, a few expressed confusion and disappointment:
“Well, it was confusing. They said I had a marker … but the implication was that I had cancer.” (P1, not referred)
“[I felt] a little concerned because they still -- I mean, I just remember they weren't being specific … I haven't really been told exactly what they have found ... So I'm still a little confused.” (P4, not referred)
When asked “How well did you understand your results?”, most participants expressed challenges. Six of the 11 participants who were not referred indicated they did not understand the results on their own:
“I was excited about taking the test, but I don't remember understanding the results … I know it was disappointing because I didn't understand … so it didn't make, you know, much sense to me.” (P2, not referred)
“I thought it was a little bit too much in medical terms … and it was kind of hard to understand.” (P13, not referred)
“It was a lot of inconclusive stuff, and I don't remember learning a lot.” (P15, not referred)
In contrast, referred participants reported feeling more confident in understanding the results after speaking with the genetic counselor:
“[I] didn't really understand what it was. I went in for an interview [genetic counseling] which helped more … I sat down one on one … and went through, you know, I think there was a list of genes and things that impacted me … It was very informative.” (P6, referred)
“You really definitely need to have the one-on-one with a geneticist or someone in the genetics department to explain the technical sides… There has to be that discussion.” (P8, referred)
“We were able to sit down with the person … she walked us through it … It was clear. Both my wife and I understood it clearly.” (P10, referred)
2. Sharing VUS
Most participants (13/16) shared their results through email or conversation with family members, primarily children, spouses, or siblings. Most participants with colon polyps (11/12) shared with family whereas two of the four with CRC did so.
Most participants who shared with family, both those who were referred and those who were not referred, expressed a duty to share VUS with family in case of future health implications:
“But the fact that I did, in fact, have a marker was something that I wanted to let my family members know. ... They need to be aware of that. They needed to take action and that needed to be part of their health strategies.
… I remember being very clear with my nieces and with my brother.” (P10, referred)
“I sat him [son] down and said, do you realize that this could be a possibility, you know, this really could, and it's important that find out as much as you can about this, whether genetically you would be at risk” (P3, not refereed)
“I just emailed them [my kids] that I was in this study and it looked -- and I had the marker for colon cancer and they should put that information somewhere so they have it at the ready if they need it.” (P1, not referred)
However, other participants were selective in sharing with select family members due to inherent uncertainly in VUS:
“I talked to one of them, my sister, and said no, I'm not going to go any further than that. You know, we're all in our 70s and 80s. And there's no sense in me stirring people up. Well, yeah. Because -- because -- because the results are so iffy. So uncertain. It even says of ‘uncertain significance.’ That doesn't mean anything to me. So I'm not going to get people to worry about stuff they don't -- can't do anything about.” (P5, referred)
In contrast to the majority of participant who shared with family, only five participants explicitly shared with a healthcare provider. Of those five, four had colon polyps and one had a diagnosis of CRC. For example, one of the two referred participants who shared with a healthcare provider made a copy of the VUS letter and gave it to them:
“[I] couldn't remember if this was passed on to my doctor or not, but I did make a copy and gave it to him … so I figured they must know about it.” (P6, referred)
The three participants who were not referred and shared results with providers talked about the value that providers can add to help interpret and bring meaning to VUS results and their impact on future healthcare:
“Well, I asked my gastroenterologist if it [VUS] was meaningful in the plan that we had developed. ‘Should I?’, you know -- so we had a conversation.” (P1, not referred)
The majority of participants chose not to share their results with their healthcare providers. Some participants reached the conclusion that sharing with their provider was not warranted:
“And the first thing it [result] says is that there is a variant of unknown significance. So it may or may not mean something. We don't know if it means anything. And so -- and then reading through the report, it was clearly all scientific language. And the conclusion was you don't need to talk to your doctor about it. Nobody's really going to contact you because we don't know what this means”. (P7, not referred)
“Nobody seems to be alarmed by the information in this report, so I'm not going to let it alarm me if I have some -- one gene that looks a little weird… They're not telling me that there's any particular risk. Some unknown possible risk but we don't know, and there are a whole bunch of big words too in scientific medical language about what it is. But clearly, they don't care if I understand it, because they would have put it in different language.“ (P7, not referred)
3 Perceived impact of VUS
No participants reported changes to their healthcare based on receiving VUS results. However, four participants described how receiving results reinforced healthy lifestyle choices in daily life, such as diet and cancer screening.
4. Recommended improvements
Despite barriers to understanding VUS, most participants found benefit from receiving VUS. Participants who were not referred reported increased awareness of their genetic makeup and feelings of altruism from participating in research. Participants who were referred found benefit in genetic counseling, ability to ask questions, and additional information they received beyond the mailed report.
Participants from both groups recommended patient-centered improvements to the VUS ROR process. Most participants (11/16) recommended expert consultation, links to videos, and primers on genetics and VUS:
“I do think it would be really helpful for people to get the results face-to-face with a professional who could explain what was done and what the results meant and describe the process more thoroughly if someone wanted the process described more thoroughly. I think I had a pretty good understanding of genetic testing and how that operates and what kinds of things they're discovering and all of that. But I think that rather than just getting, you know, a typical result of a test in the mail.” (P10, referred)
“I'd rather speak to somebody so I could say, well, … what am I doing wrong? You know, if it's not genetic, then what am I doing wrong? You know? Am I overweight? Am I drinking too much? Am I not getting enough exercise? Should I eat carrots? You know, things like that. Those questions I would have liked to have asked of the people that did this type of testing” (P3, not referred)
To address drawbacks, such as feeling hindered by confusing medical jargon and inability to find clarifying resources, several participants who were not referred suggested framing explanations in lay terminology and providing education resources:
“Well, just more in lay terms. Like on additional notes, you know, they have KC and Q1 92 percent, you know, PM as to 93, you know, that kind of thing. You have no idea what all that means…They detailed, you know, the interpretations and what they did, but I don't -- maybe it's just me, but I didn't understand a lot of it. " (P13, not referred)
“You know how, like, when you read a medical paper or a legal paper there are footnotes that you can read further about this if you go to this source. So that could be kind of helpful for people. Even if it was as simple as, you know, an article on the basics of genetic studies.” (P16, not referred)
Participants who were referred also suggested improving after-visit documentation, more timely communication, and the potential for future consultation:
“Maybe if a CD was made of the interview at the time, that you could take with you would just accompany the written information. That way down the road you could plug it in as you're looking through the written information and have that explanation freshen you. “(P6, referred)
“I think there was a delay in the time between getting the results and having the conversation, so I think people who maybe are not as comfortable with the healthcare system and terminology might prefer a closer time opportunity to discuss the information sent to them in the mail.” (P12, referred)
Discussion
In several ways, ROR experiences differed between participants who were referred and not referred to genetic counseling for VUS. Those who were referred reported less confusion, less disappointment, and more confidence in understanding their VUS than non-referred participants. Although some participants who were not referred also expressed positive experiences, confusion and frustration with the ROR process was evident. Several participants did not understand their results and desired expert consultation and clarifying resources. Although VUS did not appear to impact healthcare, participants who shared VUS may have fostered communication about future healthcare. All participants offered suggestions that can inform healthcare systems in patient-centered improvements to the ROR process that prioritize patient experience (e.g., patient-friendly terminology, on-demand education, ongoing consultation).
Many patients want to be included in deciding what genetic results are returned18 and find value in the results beyond clinical utility,19 yet we know comparatively little about patients’ perceptions of VUS. Although the consequences of receiving VUS are not well studied, early evidence suggests taking caution in how VUS are returned.11 Patients may misinterpret VUS and interpret their clinical significance diversely.12 For example, some women with BRCA1/2 VUS pursue mastectomy and/or salpingo-oophorectomy.20 Other work demonstrates similar mixed patient interpretation of uncertainty and implications of VUS.13 However, these studies did not examine the impact of how results were returned on patients’ experiences. Our sample may limit transferability of findings. Because participants who were referred had a VUS in one of the Lynch syndrome genes and those who were not referred did not, group differences beyond referral could have impacted results. Given limitations of our small homogeneous sample, future work whose scope is broader and examines potential racial and other disparities is needed to fully understand best-practice communication methods and gauge patient understanding. Although our small sample was from a single health system, our findings add in-depth insight for patients’ experiences into this poorly understood topic.
The process through which patients receive VUS matters - a text report alone may be insufficient and leave patients without needed assistance to interpret the results. Patients may experience less confusion, less disappointment, and greater confidence in understanding VUS when ROR involves expert consultation. Given the scarcity of genetic counselors, our findings present challenges for meeting the needs of patients in the era of precision medicine, Patient-centered solutions, such as virtual agents,21 educational portals,22,23 and patient-friendly formats7 could scale support to reach diverse audiences. However, future work should demonstrate the value and acceptability of such solutions to patients. More fundamentally, our findings give pause to whether the benefits of returning VUS outweigh the potential risks when genetics consultation is not indicated.
Conclusion
Healthcare systems should gauge the needs of patients and report genetic results in patient-friendly ways. Although genetic counselors are critical to effective ROR, information technology and processes that carefully consider patient experience could ease emerging challenges of precision medicine.
Acknowledgments
We wish to thank our participants as well as Suhk Mahknoon and Stephanie M. Fullerton who provided helpful feedback on this manuscript. This work was supported by NIH/NHGRI grants U01HG008657 and 2R01LM011563.
Figures & Table
References
- 1.Green RC, Berg JS, Grody WW, Kalia SS, Korf BR, Martin CL, et al. ACMG recommendations for reporting of incidental findings in clinical exome and genome sequencing. Genet Med. 2013;15(7):565–74. doi: 10.1038/gim.2013.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kalia SS, Adelman K, Bale SJ, Chung WK, Eng C, Evans JP, et al. Recommendations for reporting of secondary findings in clinical exome and genome sequencing, 2016 update (ACMG SF v2.0): A policy statement of the American College of Medical Genetics and Genomics. Genet Med. 2017 Feb 1;19(2):249–55. doi: 10.1038/gim.2016.190. [DOI] [PubMed] [Google Scholar]
- 3.Harrison SM, Rehm HL. Is “likely pathogenic” really 90% likely? Reclassification data in ClinVar [Internet] Vol. 11. Genome Medicine. BioMed Central Ltd; 2019. [cited 2021 Jul 3]. Available from: https://pubmed.ncbi.nlm.nih.gov/31752965/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kinney AY, Steffen LE, Brumbach BH, Kohlmann W, Du R, Lee JH, et al. Randomized noninferiority trialof telephone delivery of BRCA1/2 genetic counseling compared with in-person counseling: 1-Year follow-up. J Clin Oncol. 2016 Aug 20;34(24):2914–24. doi: 10.1200/JCO.2015.65.9557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christensen KD, Uhlmann WR, Roberts JS, Linnenbringer E, Whitehouse PJ, Royal CDM, et al. A randomized controlled trial of disclosing genetic risk information for Alzheimer disease via telephone. Genet Med. 2018 Jan 1;20(1):132–41. doi: 10.1038/gim.2017.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roberts JS, Chen CA, Uhlmann WR, Green RC. Effectiveness of a condensed protocol for disclosing APOE genotype and providing risk education for Alzheimer disease. Genet Med. 2012 Aug;14(8):742–8. doi: 10.1038/gim.2012.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haga SB, Mills R, Pollak KI, Rehder C, Buchanan AH, Lipkus IM, et al. Developing patient-friendly genetic and genomic test reports: Formats to promote patient engagement and understanding. Genome Med. 2014 Jul 31;6(7) doi: 10.1186/s13073-014-0058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tabor HK, Jamal SM, Yu JH, Crouch JM, Shankar AG, Dent KM, Anderson N, Miller DA, Futral BT, Bamshad MJ. My46: a Web-based tool for self-guided management of genomic test results in research and clinical settings. Genetics in Medicine. 2017 Apr;19(4):467–75. doi: 10.1038/gim.2016.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shaer O, Nov O, Okerlund J, Balestra M, Stowell E, Ascher L, et al. Informing the design of direct-to-consumer interactive personal genomics reports. J Med Internet Res [Internet] 2015 Jun 1 [cited 2021 Jul 2];17(6):e146. doi: 10.2196/jmir.4415. Available from: https://www.jmir.org/2015/6/e146 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams JL, Rahm AK, Zallen DT, Stuckey H, Fultz K, Fan AL, Bonhag M, Feldman L, Segal MM, Williams MS. Impact of a patient-facing enhanced genomic results report to improve understanding, engagement, and communication. Journal of genetic counseling. 2018 Apr;27(2):358–69. doi: 10.1007/s10897-017-0176-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clift K, Macklin S, Halverson C, McCormick JB, Abu Dabrh AM, Hines S. Vol. 11. Journal of Community Genetics. Springer; 2020. Patients’ views on variants of uncertain significance across indications; pp. p. 139–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Solomon I, Harrington E, Hooker G, Erby L, Axilbund J, Hampel H, et al. Lynch Syndrome Limbo: Patient Understanding of Variants of Uncertain Significance. J Genet Couns. 2017 Aug 1;26(4):866–77. doi: 10.1007/s10897-017-0066-y. [DOI] [PubMed] [Google Scholar]
- 13.Makhnoon S, Shirts BH, Bowen DJ. Journal of Genetic Counseling. John Wiley and Sons Inc.; 2019. Patients’ perspectives of variants of uncertain significance and strategies for uncertainty management; pp. p. 313–25. [DOI] [PubMed] [Google Scholar]
- 14.Electronic Medical Records and Genomics (eMERGE) Network | NHGRI [Internet] [cited 2020 Jun 12]. Available from: https://www.genome.gov/Funded-Programs-Projects/Electronic-Medical-Records-and- Genomics-Network-eMERGE.
- 15.Zouk H, Venner E, Lennon NJ, Muzny DM, Abrams D, Adunyah S, et al. Harmonizing Clinical Sequencingand Interpretation for the eMERGE III Network. Am J Hum Genet [Internet] 2019 Sep 5 [cited 2020 Aug 28];105(3):588–605. doi: 10.1016/j.ajhg.2019.07.018. Available from: /pmc/articles/PMC6731372/?report=abstract . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crabtree B, Miller W. Using Codes and Code Manuals: A Template Organizing Style of Interpretation. Doing Qual Res (2nd ed) [Internet] 1999 Aug 1 [cited 2020 Jun 12]. Available from: https://scholarlyworks.lvhn.org/family-medicine/53 .
- 17.Dedoose Version 8.3.17, web application for managing, analyzing, and presenting qualitative and mixedmethod research data [Internet] SocioCultural Research Consultants, LLC. 2020. [cited 2020 Dec 6]. Available from: www.dedoose.com .
- 18.Clift KE, Halverson CME, Fiksdal AS, Kumbamu A, Sharp RR, McCormick JB. Patients’ views onincidental findings from clinical exome sequencing. Appl Transl Genomics. 2015 Mar 1;4:38–43. doi: 10.1016/j.atg.2015.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Halverson CME, Clift KE, McCormick JB. Was it worth it? Patients’ perspectives on the perceived value of genomic-based individualized medicine. J Community Genet. 2016 Apr 1;7(2):145–52. doi: 10.1007/s12687-016-0260-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murray ML, Cerrato F, Bennett RL, Jarvik GP. Follow-up of carriers of BRCA1 and BRCA2 variants of unknown significance: Variant reclassification and surgical decisions [Internet] Genetics in Medicine. Genet Med. 2011 [cited 2020 Aug 28];Vol. 13:p. 998–1005. doi: 10.1097/GIM.0b013e318226fc15. Available from: https://pubmed.ncbi.nlm.nih.gov/21811163/ [DOI] [PubMed] [Google Scholar]
- 21.Schmidlen T, Schwartz M, DiLoreto K, Kirchner HL, Sturm AC. Patient assessment of chatbots for thescalable delivery of genetic counseling. J Genet Couns. 2019 Dec 1;28(6):1166–77. doi: 10.1002/jgc4.1169. [DOI] [PubMed] [Google Scholar]
- 22.What do the results of genetic tests mean? - Genetics Home Reference - NIH [Internet] [cited 2020 Jun 12]. Available from: https://ghr.nlm.nih.gov/primer/testing/interpretingresults .
- 23.eMERGE Network. MyResults. Available from: https://myresults.org/