Abstract
The digitalization of the healthcare systems has resulted in a deluge of big data and has prompted the rapid growth of data science in medicine. Many informatics tools, such as data science, which is the field of study dedicated to the principled extraction of knowledge from complex data, can also introduce benefits into implementation science, quality improvement (QI), and primary care research. The increased amount of primary care QI initiatives, availability of practice facilitation-related data, the need for better evidence-based care, and the complexity of challenges make the use of data science techniques and data-driven research particularly appealing to primary care. Recent advances in the usability, applicability, and interpretability of data science models offer promising applications to implementation science. Despite the increasing number of studies and publications in the field, thus far there have been few examples of combining informatics and implementation framework to facilitate primary care studies. We designed and developed an informatics-driven implementation research framework to provide a coherent rationale and justification of the complex interrelationships among features, strategies, and outcomes. The proposed framework is a principle-guided tool designed to improve the specification, reproducibility, and testable causal pathways involved in implementation research projects in primary care settings.
Introduction
Implementation science
Implementation research is the scientific study of methods to promote the systematic uptake of research findings and other evidence-based practices into routine practice, and, hence, to improve the quality and effectiveness of health services and care. This relatively new field includes the study of influences on health care professionals and organizational behaviors.1 Implementation science shares many characteristics, and the rigorous approach, of clinical research. Implementation science in primary care involves investigation at multi-levels, and the targets of investigation include the patients, health care providers, primary care clinics, organization, community, society, and health system.
Informatics in primary care
Health care systems, especially primary care, suffer from major gaps between evidence and practice, unexplained practice variations, and suboptimal quality.2 Although health information technologies (HIT), such as information processing, and management are key to health care delivery and considerable evidence to improvements in health care quality and patient safety, primary care has a longstanding gap in the implementation of evidence-based practices and informatics packages. Informatics in primary care includes the development, installation, and implementation of electronic systems and relevant applications, including hardware, software, networking, and communication tools.3 In the past decade, IT development activities within the health care industry have increased as executives and providers recognized the urgent need for strategic information management and inadequacies of traditional information storage, retrieval, and analysis tools. However, most IT investments in primary care lack feasible guidelines for implementation and maintain sustainable improvement.4
Implementation of informatics packages or tools in primary care has two main domains: (1) HIT infrastructure implementation. For example, implementing or updating electronic health record (EHR) systems to enable automated mechanisms for capturing data, and facilitate clinical decision making; (2) leveraging the clinical decision support (CDS) systems to improve health care providers’ performance and generate measurable metrics to evaluate the performance, such as efficiency, effectiveness, cost, efficacy, etc.
In general, most health care information systems are composed of automated billing and financial management, patient admission, discharge, transfers and registration, coordination of communications infrastructure, claims processing, customer service, and electronic data sharing. The informatics infrastructure needed for primary care includes feasible data collection methods, data repositories, clinical event monitoring, health care standards including standardized terminologies, digital sources of evidence, data-mining techniques, and communication technologies.5
The informatics system in primary care needs to interface with, and assist, patients, health care providers, primary care managers, health care organizations, communities, and the public.
This study aims to design and develop an informatics-driven implementation research framework to provide a coherent rationale and justification of the complex interrelationships among features, strategies, and outcomes. We will adapt the typical evaluation logic model to integrate existing implementation science frameworks and informatics models as their core elements while keeping to the same aim of facilitating the causal modeling.
Methods
Framework
To develop the informatics-driven implementation research framework, we adopted the Implementation Research Logic Model (IRLM) that was developed by Smith et al.6 This model enables a pipeline format for primary care systems that support the adoption and delivery of health practices by involving multiple levels factors within or outside the system and having its own unique characteristics. This framework also incorporated the key elements of the FITT (Fit between Individuals, Task and Technology) framework.7
Results
Features
Features are variables or factors that may impact the implementation (i.e., barriers and facilitators). All the features can be mapped onto the Consolidated Framework for Implementation Research (CFIR) framework.8 In some cases, features may act as moderators or mediators, thus indicating that they are links in a chain of causal mechanisms.9
Informatics domains
Task
Tasks in primary care include collecting medical history, gathering preventive service information, completing forms, screening disease, diagnosing, tracking diagnostic data, making treatment protocols, proposing interventions, educating patients about self-care activities and medications, refilling prescriptions, receiving and resolving patients’ inquiries, referral tracking, and arranging home health care.10,11
Technology
In primary care, technology and informatics system have several key elements. In general, a primary care clinic should have an available EHR to enable patients and providers to conduct shared decision-making. EHRs store personal health data, reliable patient-specific tools, and resources. EHRs provide every patient and their caregivers with the necessary information required for optimal care. They can help patients to better understand the complexity of medical care and more readily participate in clinical decision-making and preventive health behaviors. Electronic health information exchange (HIE) ensures security, privacy, and system compatibility.12 The exchange between organizations facilitates sharing of patient information at the point of the care delivery to eliminate unnecessary testing, improve safety, and facilitate efforts to improve health care quality and patient safety Clinicians in primary care can leverage CDS can help health care providers utilize state-of-the-art medical knowledge in treatment decisions. CDS provides information management tools for the acquisition, manipulation, application, distribution, and display of appropriate patient- and task-specific clinical data to providers and patients that is conducive to correct, timely, and evidence-based clinical decision-making. Computerized provider order entry (CPOE) can help the tracking and analysis of health care processes.13 CPOE for tests, medicine, and procedures has the potential to decrease medical error, improve quality. It can help providers coordinate and collect patient-specific information. Population-based health care systems support the creation of large, integrated databases of patient-specific information that allow real-time management of populations of similar patients. These databases can facilitate the evaluation of new implementation strategies and provide insights into new associations between management approaches and health states.14
All of these tools coordinate information dissemination and sharing from various databases to equip the provider in providing patient-specific, appropriate, timely, and evidence-based care.15
Individual
For implementation research in primary care, there are several key stakeholders during the process, including primary care leaders, managers. Quality improvement practice facilitators are implementation scientists are also important because they work closely with primary care leaders and staff as partners and break down the research-practice divide in order to achieve the ultimate goal of increasing the public health impact. Table 1 demonstrates the informatics-driven interventions and strategies for implementation projects in primary care based on the three domains.16
Table 1.
Informatics-driven interventions and strategies for implementation projects in primary care
| Informatics domain | Interventions and Strategies |
|---|---|
| Task |
|
| Technology |
|
| Individual |
|
Implementation strategies
Intervention Characteristics
Intervention Characteristics are key attributes of interventions that influence the success of implementation.22 Information technology management encompasses primary care, its infrastructure, strategies for use, and expected outcomes. Implementation research in primary care requires the support and resources of the organization and leadership. Most primary care systems have limited resources for QI. Resource allocation warrants close examination to maximize the benefits of the delivery of safe, effective, efficient, and high-quality care. Factors influencing organizational decisions surrounding implementation need to explore the characteristics of clinical conditions, practices, and settings, outstanding gaps, expected costs and benefits. The implementation research should be tailored to the needs of the organization. A balanced assessment of the effectiveness and costs of the system is needed to make successful implementation efforts.
Inner Setting
The inner setting is an active interacting facet and not just as a backdrop in implementation. Most primary care clinics are still at the stages ranging from considering adoption through early implementation. The lack of financial support for widespread informatics applications is considered a primary barrier to its implementation by both managers and clinicians.23 The financial burden of implementation, including acquisition and implementation costs, slow and uncertain financial payoffs, and disruption to clinical practices, is directly related to both the size of primary care and its readiness for conversion.
Outer Setting
An effective implementation needs stakeholders outside of the organization, such as policymakers, state and federal entities, and various participants (e.g., physicians, other providers, hospitals, payers, etc.).
Characteristics of Individuals
Organizations, including primary care, are made up of individuals. This framework can facilitate the understating of the interplay between individuals and their ripple effects through their teams, units, networks, and organizations on implementation. Clinicians desire a system that allows them to review and act upon test results safely and efficiently. Taking full advantage of informatics may require a team approach, where active involvement of interdisciplinary groups of providers and users is important. HIT use may empower patients in their exchange with providers and promotes the alignment of care between hospitals/clinics and patients' homes. Human factors such as system usability, process complexity, and user-engagement methods routinely influence the implementation.24
Process
A crucial first step for the organization in the implementation process is to assess both current informatics capabilities and estimate future needs.25 Equally important is the assessment of readiness for major organizational change, such as the ability to invest in change management and training, as well as the culture and processes needed to support implementation.26 Informatics systems to be implemented need to align with processes within the primary care to allow evolution and adaptation.27 On an individual level, the organization and its management need to involve end users' input in improving their work practices. They also need to consider other factors, such as the usability, usefulness, and flexibility of informatics tools and individualized training that will influence uptake. On a system level, a supportive culture, visibility of positive results from IT use, and a realistic timeline will enhance implementation.28
Outcomes
Outcomes include target clinical outcomes, health service outcomes, or indicators of implementation processes. Among these, implementation outcomes are the effects of deliberate and purposive actions to implement new treatments, practices, and services in primary care.29 The interrelated nature of implementation outcomes may present as non-linear, complex, or dynamic sequences of adoption by a delivery agent. Outcomes earlier in the sequence can be conceptualized as mediators and mechanisms of strategies on later implementation outcomes. Specifying which strategies are theoretically intended to affect which outcomes, through which mechanisms of action, is crucial for improving the reproducibility and generalizability of implementation research in primary care and validating the results.
Discussion
A number of exciting challenges face the rapidly developing field of health and biomedical informatics in primary care. Integration of implementation science methodologies into primary care will speed the development of evidence-based interventions that have demonstrable public health impacts. Testing and validating the theories that underlie implementation efforts is needed to enhance the development of next-generation analytic methods and interventions. This informatics-driven framework used systems thinking that allows us better understand how each element in the system interacts and impacts each other, thus proposing intervention strategies accordingly.
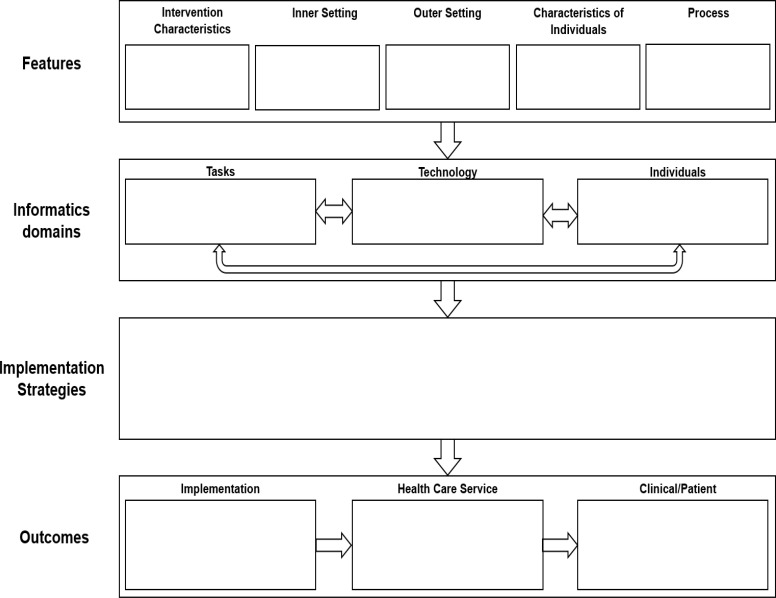
The proposed informatics-driven implementation research framework provides a compact visual depiction of implementation research studies. Its use in the planning, executing, reporting, and synthesizing of implementation research could increase the rigor and transparency of complex studies that ultimately could improve reproducibility—a challenge in the field—by offering a common structure to increase consistency and a method for more clearly specifying links and pathways to test theories.6 The proposed framework would be a useful and generalizable guideline for future practice facilitation projects, QI initiatives, and health care intervention implementation studies.
Conclusion
We designed and developed an informatics-driven implementation research framework to provide a coherent rationale and justification of the complex interrelationships among features, strategies, and outcomes. The promise of implementation science lies in the ability to conduct rigorous and reproducible research, to clearly understand the findings, and to synthesize findings from which generalizable conclusions can be drawn and actionable
recommendations for practice change emerge. The proposed framework is a principle-guided tool designed to improve the specification, reproducibility, and testable causal pathways involved in implementation research projects in primary care settings.
Figures & Table
Figure 1.
Informatics-driven implementation research framework standard template
References
- 1.Eccles MP, Mittman BS. Springer; 2006. Welcome to implementation science. [Google Scholar]
- 2.Doebbeling BN, Chou AF, Tierney WM. Priorities and strategies for the implementation of integrated informatics and communications technology to improve evidence-based practice. Journal of general internal medicine. 2006;21(2):S50. doi: 10.1111/j.1525-1497.2006.00363.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ye J, Ma Q. The Effects and Patterns among Mobile Health, Social Determinants, and Physical Activity: A Nationally Representative Cross-Sectional Study. AMIA Summits on Translational Science Proceedings. 2021. [PMC free article] [PubMed]
- 4.Office GA. Use of Information Technology for Selected Health Care Functions. 2003.
- 5.Bakken S, Hripcsak G. An informatics infrastructure for patient safety and evidence‐based practice in home healthcare. Journal for Healthcare Quality. 2004;26(3):24–30. doi: 10.1111/j.1945-1474.2004.tb00492.x. [DOI] [PubMed] [Google Scholar]
- 6.Smith JD, Li DH, Rafferty MR. The implementation research logic model: a method for planning, executing, reporting, and synthesizing implementation projects. Implementation Science. 2020;15(1):1–12. doi: 10.1186/s13012-020-01041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ammenwerth E, Iller C, Mahler C. IT-adoption and the interaction of task, technology and individuals: a fit framework and a case study. BMC medical informatics and decision making. 2006;6(1):3. doi: 10.1186/1472-6947-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation science. 2009;4(1):1–15. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lewis CC, Klasnja P, Powell BJ, et al. From classification to causality: advancing understanding of mechanisms of change in implementation science. Frontiers in public health. 2018;6:136. doi: 10.3389/fpubh.2018.00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Edwards ST, Rubenstein LV, Meredith LS, et al. Who is responsible for what tasks within primary care: perceived task allocation among primary care providers and interdisciplinary team members. Paper presented at: Healthcare 2015. [DOI] [PubMed]
- 11.Feinglass J, Wang JA, Ye J, Tessier R, Kim H. Hospital Care for Opioid use in Illinois, 2016-2019. The Journal of Behavioral Health Services & Research. 2021. pp. 1–13. [DOI] [PMC free article] [PubMed]
- 12.Ye J. The role of health technology and informatics in a global public health emergency: practices and implications from the COVID-19 pandemic. JMIR Medical Informatics. 2020;8(7):e19866. doi: 10.2196/19866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ye J. Pediatric mental and behavioral health in the period of quarantine and social distancing with COVID-19. JMIR pediatrics and parenting. 2020;3(2):e19867. doi: 10.2196/19867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sittig DF, Hazlehurst BL, Palen T, Hsu J, Jimison H, Hornbrook M. A clinical information system research agenda for Kaiser Permanente. Permanente J. 2002;6(3) [Google Scholar]
- 15.Ye J, Wang Z, Hai J. Social networking service, patient-generated health data, and population health informatics: patterns and implications for using digital technologies to support mental health. medRxiv. 2021:2021.2006.2011.21258777. [DOI] [PMC free article] [PubMed]
- 16.Burke EK, De Causmaecker P, Berghe GV, Van Landeghem H. The state of the art of nurse rostering. Journal of scheduling. 2004;7(6):441–499. [Google Scholar]
- 17.Ye J, Sanchez-Pinto LN. Three data-driven phenotypes of multiple organ dysfunction syndrome preserved from early childhood to middle adulthood. AMIA Annual Symposium Proceedings. 2020. [PMC free article] [PubMed]
- 18.Ye J, Yao L, Shen J, Janarthanam R, Luo Y. Predicting mortality in critically ill patients with diabetes using machine learning and clinical notes. BMC Medical Informatics and Decision Making. 2020;20(11):1–7. doi: 10.1186/s12911-020-01318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ye J, Li N, Lu Y, Cheng J, Xu Y. A portable urine analyzer based on colorimetric detection. Analytical Methods. 2017;9(16):2464–2471. [Google Scholar]
- 20.Ye J, Zhang R, Bannon JE, et al. Identifying Practice Facilitation Delays and Barriers in Primary Care Quality Improvement. The Journal of the American Board of Family Medicine. 2020;33(5):655–664. doi: 10.3122/jabfm.2020.05.200058. [DOI] [PubMed] [Google Scholar]
- 21.Ye J. The impact of electronic health record-integrated patient-generated health data on clinician burnout. Journal of the American Medical Informatics Association. 2021;28(5):1051–1056. doi: 10.1093/jamia/ocab017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilson PM, Petticrew M, Calnan MW, Nazareth I. Disseminating research findings: what should researchers do? A systematic scoping review of conceptual frameworks. Implementation Science. 2010;5(1):1–16. doi: 10.1186/1748-5908-5-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Valdes I, Kibbe D, Tolleson G, Kunik M, Petersen L. Barriers to proliferation of electronic medical records. Journal of Innovation in Health Informatics. 2004;12(1):3–9. doi: 10.14236/jhi.v12i1.102. [DOI] [PubMed] [Google Scholar]
- 24.Pagliari C, Gilmour M, Sullivan F. Electronic Clinical Communications Implementation (ECCI) in Scotland: a mixed‐methods programme evaluation. Journal of Evaluation in Clinical Practice. 2004;10(1):11–20. doi: 10.1111/j.1365-2753.2004.00475.x. [DOI] [PubMed] [Google Scholar]
- 25.Major LF, Turner MG, Boronow JJ, Andrulewicz M. Assessing the information management requirements for behavioral health providers/Practitioner application. Journal of Healthcare Management. 2003;48(5):323. [PubMed] [Google Scholar]
- 26.Stablein D, Welebob E, Johnson E, Metzger J, Burgess R, Classen DC. Understanding hospital readiness for computerized physician order entry. The Joint Commission Journal on Quality and Safety. 2003;29(7):336–344. doi: 10.1016/s1549-3741(03)29041-9. [DOI] [PubMed] [Google Scholar]
- 27.Lenz R, Kuhn KA. Towards a continuous evolution and adaptation of information systems in healthcare. International journal of medical informatics. 2004;73(1):75–89. doi: 10.1016/j.ijmedinf.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 28.Saleem JJ, Patterson ES, Militello L, Render ML, Orshansky G, Asch SM. Exploring barriers and facilitators to the use of computerized clinical reminders. Journal of the American Medical Informatics Association. 2005;12(4):438–447. doi: 10.1197/jamia.M1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Administration and policy in mental health and mental health services research. 2011;38(2):65–76. doi: 10.1007/s10488-010-0319-7. [DOI] [PMC free article] [PubMed] [Google Scholar]