Abstract
In this paper, we examined informatics challenges and opportunities related to emergency department visit data during public health emergencies. We investigated the impact of COVID-19 pandemic on the volume and acuity of adult patients visiting the emergency department (ED) of a medical center in Arizona during the pandemic compared to the pre-pandemic period. We performed a negative binomial regression analysis to understand how different public health-related mandates and statewide business opening/closing orders in Arizona affected the daily emergency department visits. The results of this study show that the average daily ED visits decreased by 20% during the COVID-19 pandemic in comparison with the same period in 2019. In addition, the business closure order had the most impact on emergency department visits in comparison to other public health mandates.
Introduction
As the COVID-19 pandemic developed and intensified throughout the United States in the early part of 2020, state governments and healthcare systems enacted a range of mitigation strategies and operational changes to address the increasing number of infections in the community. Initial public health strategies recommended avoiding unnecessary healthcare utilization to decrease virus spread and to ensure that there is enough capacity to handle spikes in COVID-19 cases [1]. In addition, different public health-related mandates, including the stay-at-home order, business closures, and mandatory wearing masks were implemented to prevent and mitigate the spread of the virus [2]. While the number of patients who visited Emergency Departments (EDs) due to COVID-19 significantly increased, health systems noticed a change in ED visits for acute care unrelated to COVID-19 [3]. Accordingly, the pattern of ED visits changed with the spread of COVID-19 in 2020. In this regard, collecting, sharing, and analyzing ED volume data are necessary for improved coordination of care and distribution of resources during high utilization times. An example of using available ED resources equitably was the Boston Marathon Bombing, where trauma patients were appropriately distributed such that trauma centers in the Boston metropolitan area were not overloaded. By recognizing spikes in patient arrivals during either mass casualty events or public health outbreaks, each hospital could call in backup providers, offload the least sick of the inpatients, and be better prepared for a potential surge of sick patients in a more timely and appropriate manner. Conversely, recognizing drastic decreases in volume ahead of time in a metropolitan area could serve as a warning or alert that something large is happening such as a new wave of pandemic or fear of becoming sick from the healthcare system. However, there are several issues relating to the ED volume data elements that have not been examined in the literature. In addition, to the best of our knowledge, the change in the pattern of ED volume and acuity, as well as the impact of public health-related mandates and state-wide business opening/closing on ED visits due to the COVID-19 pandemic, are yet to be studied in detail while considering regional factors. Therefore, in this study, we seek to answer the following questions.
-
(1)
What are the challenges of collecting, coordinating, and sharing ED volume data elements and recommendations to address those challenges?
-
(2)
How did the COVID-19 pandemic affect ED visits and acuity (in terms of Emergency Severity Index (ESI) level at triage, admissions, and specific ED activations) in a single regional hospital compared to the pre-pandemic period?
-
(3)
How did different periods of the COVID-19 pandemic in Arizona, as defined by different public health-related mandates and statewide business openings/closings, affect daily ED visits in a single regional hospital?
Background
The United States declared a national emergency on March 13, 2020, in response to the COVID-19 pandemic. Afterward, states imposed stay-at-home orders to prevent the spread of COVID-19 and relieve the burden on the healthcare system, which influenced the number and type of ED visits. Several prior studies have examined the impact of the pandemic on ED visits. We provide a review of results from these studies, along with data limitations, and other informatics challenges.
Hartnett et al. [4] investigated the effect of the COVID-19 pandemic on ED visits in the United States from January 1, 2019 to May 30, 2020. They found that ED visits in the United States declined 42% during the pandemic. They also demonstrated that ED visits associated with the patients aged less than 14 years, females, and Northeast region had the sharpest decline after the pandemic. Additionally, they showed that the proportions of infectious disease-related ED visits during the early pandemic period in 2020 were four times higher than those in the same period before the pandemic in 2019. Adjemian et al. [5] presented an update on Hartnett et al.’s [4] report; they compared the effect of the pandemic on ED visits in the United States during December 20, 2020–January 16, 2021 with those during a pre-pandemic period (December 15, 2019–January 11, 2020). According to Adjemian et al.’s [5] report, ED visits were 25% lower in December 2020-January 2021 than in the same months the previous year. In addition, Adjemian et al. [5] showed that, during the pandemic period, higher proportions of ED patients, particularly pediatric patients, are seeking treatment for mental and behavioral health issues.
Although these previous studies on the effect of COVID-19 on ED volume in the United States (i.e., [4] and [5]) show a decline in ED volume during the pandemic, there are life-threatening conditions that always require immediate emergency care, even during the pandemic. In this regard, Lange et al. [6] conducted a study of ED visits for three life-threatening acute health conditions, including myocardial infarction, stroke, hyperglycemic crisis, in the United States immediately before and after the declaration of the COVID-19 pandemic as a national emergency. They reported that ED visits for each of these health conditions declined after the declaration of the COVID-19 pandemic as a national emergency. The US ED volume data included in [4-6] were from National Syndromic Surveillance Program (NSSP) that collaborates with programs across CDC, state, and local health departments to collect electronic health data in real-time. So the findings in these studies are subject to several data-related limitations that are as follows: (1) diagnostic categories rely on the usage of certain codes which may be missing or utilized inconsistently across different institutions; (2) hospitals reporting to NSSP change over time when new facilities are established, and less frequently, when they close; and (3) NSSP data collection coverage is not uniform across all states. That is, in some states nearly all hospitals report their data, while in others, only the hospitals in certain counties report their data.
The decrease in ED volume in the United States during the pandemic could have been caused by the public fear of seeking medical care, causing the patients with time-sensitive critical conditions to delay their treatment. Kim et al. [7] compared the number of patients with serious diagnoses visiting seven EDs in greater Chicago, Illinois, during the pandemic period to that of the pre-pandemic period. This study demonstrated sharp reductions in ED visits for all major diagnosis classes (e.g., cardiac, surgical, orthopedic, neurologic, gastrointestinal, chronic respiratory) during the COVID-19 pandemic. In this study, the data are from a particular healthcare system Chicago, so the results may not be generalizable to other settings with different patient population characteristics and/or local government responses to the COVID-19 pandemic. Also, this study relies on ICD-10 coding data, which are based on the treating physician’s impression. To address this limitation, Kim et al. [7] excluded symptom-based diagnoses and included the diagnoses that often need objective findings obtained during ED evaluation. Although Kim et al. [7] used a valid and publicly available system to link ICD-10 codes to clinical diagnoses, it is possible that not all relevant ICD-10 codes for serious diseases are captured.
Jeffery et al. [1] examined ED visits and visits that led to hospital admissions in healthcare systems in five states, including Colorado, Connecticut, Massachusetts, New York, and North Carolina covering a four-month period before and during the COVID-19 pandemic. This cross-sectional study demonstrated that the ED visits in these five states significantly decreased from 41.5% to 63.5% during the pandemic. They also showed that the rates of the ED visits that led to hospital admissions were stable before the pandemic but increased from 22% to 149% during the pandemic. Since Jeffery et al.’s [1] study data are limited to ED visits to the healthcare systems of only five states, the results may not be generalizable to the other states in the United States. In addition, because their study data did not include diagnoses, they were unable to examine how ED patient case-mix have changed over time.
Westgard et al. [3] conducted a study of ED visits, demographics, characteristics, and diagnoses of the patients visiting an urban Level-1 trauma center in the United States 28 days before and 28 days after declaring a state emergency on March 13th, 2020. The results of their study show that ED visits significantly decreased after the state of emergency declaration. They also demonstrated that the decline in ED visits significantly changes by patient demographics (i.e., age, gender, and race) and visit characteristics (i.e., insurance status, arrival mode, and disposition). The data in this study are limited to only one center and a short study period, limiting the generalizability of the findings to other medical centers and the rest of the pandemic period.
Butt et al. [8] studied the volume and acuity of the patients visiting four EDs affiliated with general, cardiac, cancer, and obstetrics hospitals in Qatar during the pre-pandemic and pandemic periods. They demonstrated that the ED patient visits in both general and specialty hospitals substantially reduced during the pandemic. They also showed that the cardiac hospital and cancer hospital experienced the sharpest decline and the least decline in ED visits, respectively. Furthermore, the proportions of severely ill patients visiting EDs sharply dropped during the pandemic. The included EDs account for more than 80% of all ED visits in Qatar, making the results generalizable to all EDs in Qatar. The data in this study are limited to the first two months after the diagnosis of the first COVID-19 patient in Qatar, so the findings may change by increasing the length of the study time frame. In addition, the study data are limited to only the volume and acuity of the ED patients before and during the pandemic. Although the results show a significant decrease in ED volume due to the pandemic, the travel restrictions imposed by the State of Qatar due to the COVID-19 pandemic may have affected the volume and acuity of ED patients. However, the data studied by Butt et al. [8] did not include travel restrictions, so they could not examine the impact of travel restrictions on ED visits.
Compared to adults, children had a lower risk of COVID-19 infection, and therefore needed less emergency medical care [9]. Consequently, although many studies focused on the volume, epidemiological, and clinical characteristics of the ED visits related to the adult patients with COVID-19, data and studies on pediatric patients are limited. With this in mind, Lozzi et al. [10] studied the pediatric ED visits of five hospitals across Italy from March 1 to March 27, 2020 and showed that pediatric ED visits in March 2020 decreased by 73% in comparison to the same period in 2019. The data in this study are from only one pediatric ED in Italy, reducing the generalizability of the findings. Similar to Italy, pediatric ED visits in other countries changed during the pandemic. According to CDC, routine pediatric care in the United States decreased during the pandemic [11]. Additionally, an examination of Chinese outpatient pediatric care showed a drop in overall outpatient healthcare as well as a significant decrease in infectious complaints [12].
Social distancing, on the other hand, posed different risks to children. For example, data from a large pediatric hospital showed a threefold increase in dog bites, as well as a significant increase in national calls to poison control centers, including a high percentage of child exposures. Chaiyachati et al. [13] studied the effect of social distancing and a state-wide stay-at-home order on pediatric ED visits to a tertiary urban children’s hospital in the United States during the COVID-19 pandemic. This study compared the pediatric ED visits in 2020 after an official stay-at-home order with the ED visits in the last three years from 2017 through 2019 and showed reduced visits, increased acuity, and consistent chief complaints in 2020 in comparison with the last three years. Given that chief complaint scripts are not standardized across hospitals, the generalizability of this study is limited.
The review of literature shows that quite a few studies have been done to investigate the impact of the COVID-19 pandemic on the volume and acuity of ED patients. However, the impact of different public health mandates on ED visits; and the challenges and opportunities associated with ED visit data during the pandemic have not been extensively studied in the literature, which we seek to address in this study.
Methods
Data source
The dataset used in this study comes from a single medical center in Arizona and was collected from January 1, 2019 to August 31, 2020. The data elements were sourced from electronic medical records, quality dashboards that report the daily and monthly census, and additional specialty reports to track ESI and admission locations. Quality metrics were obtained from the hospital quality committees that track such data for state and national reporting. Diagnoses categories that are ‘suspected’ in the ED and get validated later in the course of the admission are collected and collated by existing committees as mentioned above. We used quality reporting such as MIDAS, or other validated data sets to extract information regarding ST-Elevation Myocardial Infarction (STEMI). STEMIs were obtained from the cardiovascular service line which reviews all arrivals and validates if the case was a STEMI or not for very specific reporting requirements. An overview of the informatics challenges and opportunities for improvement were obtained through direct in-person interviews with the clinical research team.
Common data elements
The initial study metrics abstracted from every ED arrival for 2019 influenza season (pre-pandemic) and 2020 (pandemic) included arrival time, arrival method, disposition type, disposition time, gender, age, ESI, chief complaint, lab results (e.g., flu A, flu B, respiratory syncytial virus, strep, respiratory pathogen polymerase chain reaction, and COVID-19) imaging results (e.g., chest X-ray (anteroposterior/lateral vs portable)). Also, the hospital metrics include daily hospital census, including total daily ED physician staffing hours, total daily trauma activations, total daily codes, transfers from an outside hospital, transfers out of the system, total daily admissions to each location (i.e., Intensive Care Unit (ICU)), acute, and Acute Palliative Care Unit), and status (i.e., total daily observations, and total daily admissions). We revised the dataset based on availability and the likelihood of obtaining data from various EDs in Arizona. The following are the current set of common data elements that we believe are needed to perform ED volume studies:
-
(1)
Daily ED visit metrics: total adult ED visits and total pediatric ED visits;
-
(2)
Monthly ED visits for each of the ESI categories (ESI is a measure of acuity, and each patient should be assigned a number from 1 (highest acuity) to 5 (lowest acuity) i.e., ESI 1, ESI 2, ESI 3, ESI 4, and ESI 5);
-
(3)
Monthly ED admissions which include admissions for medical/surgical floor, step down/intermediate, and ICU;
-
(4)
Monthly quality metrics that include ED stroke activations, ED ST-Elevation Myocardial Infarction (STEMI) activations, ED trauma activations, and ED sepsis activations. It should be noted that our study includes only adult patients, and pediatric patients were not considered in our study.
Data collection and coordination process
Coordination with other sites for obtaining data included reaching out to individuals who we thought would be interested and capable of obtaining data. This largely included previous or ongoing ED-based colleagues. We found that rapidly establishing was challenging and previous agreements did not include such uses of data for publication and would have required soliciting individual agreements with each institution to use the data. Consequently, the dataset used in this study is limited to only one medical center in Arizona, which reduced the generalizability of results. For example, we were unable to provide information regarding alternative institutions, such as urgent care, critical access, or suburban hospitals. Furthermore, given the issues and challenges that we had in obtaining data, we simplified the dataset to improve the likelihood of obtaining data. However, it is obvious that resolving data collection issues and obtaining more detailed information will result in more educated or specific findings and recommendations. For instance, simply knowing the raw volume of patient arrivals is a good starting point, but it is insufficient to know if either an increase or decrease in volume also has an increase or decrease in acuity. Are sicker patients staying home or unable to get care elsewhere? What was the impact of primary care offices closing? Did those patients requiring medication refills for diabetes or heart medications go to urgent cares or EDs for refills or did they simply go without and subsequently suffer worse outcomes due to the forced non-compliance with their medications? Other challenges we faced include separating the pediatric population from the adult population since many EDs do not have a separate pediatric department that is open 24 hours per day, and they combine and merge the census. Consequently, the data on ED adult patients had to be manually extracted from the electronic health records.
Challenges and opportunities related to data sharing
Data protection regulations
The majority of data sharing challenges were largely related to privacy and security concerns of Protected Health Information. Local institutions must approve research projects involving human participants, and this process follows internal protocols. Even within the same county, institutional review board (IRB) protocol preparation and approval processes are generally different. The main variations are based on the structure and content of the documentation, the bureaucratic processes necessary for the documentation, the time it will take for the institution to process and approve it, and the number and kind of revisions requested by the IRB. As a result, such differences served as a barrier to multisite research and led to potential delays in starting the studies. These challenges were more pronounced for sites that do not have sufficient research administration capacity.
The use of de-identified data sets or population-level data removes some if not all the concerns regarding possible re-identification of patients, but it also removes some level of necessary detail. For instance, if we wanted to see which zip codes, ethnicities, ages, or genders were most impacted, it would have been more complicated to coordinate how best to protect patients via either a safe harbor or other methods of de-identification that would also allow aggregation amongst others.
Most institutional IRBs are established to review traditional research on drugs or devices and are less familiar with more of a population-based approach nor are they comfortable with sharing data across disparate institutions. Early approaches to obtaining IRB approval as well as data collection were delayed in part due to this misunderstanding. Using more relevant language regarding de-identified data, limited data sets, and quality improvement data may have served us better.
Data formats and report structures
Some healthcare organizations tend to have established departments for the submission of data to government and regulatory agencies in many different formats to comply with the specific needs for each request or requirement. Unfortunately, many of these established departments have become less flexible to modifications of or even sharing of their data collections for fear of manipulation or alteration of it. A report created for reporting to the Centers for Medicare & Medicaid Services is either overly cleaned or processed and often misses the details that physicians expect and need to ‘tune’ their internal diagnostic algorithms. Taken out of context, meaningful cases reported for disease entities such as heart attacks or strokes may seem either exaggerated or minimized, depending on the strict requirements for inclusion or exclusion. Instead of having a readily available source of heart attack, stroke, sepsis, or even ED visit data in an understandable format, we were often met with unclear or even confusing datasets created not to improve patient care but to comply with various uncoordinated agencies. Some data were necessarily delayed
until a diagnosis was assured, either from pathology, autopsy, or discharge diagnosis reports, making real-time reporting more challenging.
Instead of replacing existing departments and reporting structures, we recommend concurrent reporting of the same data in more clinically relevant formats that can better be used for monitoring population movements and clinical outcomes as well as improvement of processes. One example could be reporting of suspected severe sepsis or septic shock versus those diagnosed. By the time the definitive diagnosis is made, it could be hours after the patient has left the ED. It is important to provide feedback that a patient either was or was not septic to better recognize and diagnose the next patient, but often physicians are less concerned about the specific reporting requirements of sepsis versus severe sepsis in individual patients.
Study design
We conducted a descriptive, cross-sectional study of volume and acuity of adult patients visiting the ED of a medical center in Arizona in 2020 (the pandemic period) compared to those in 2019 (the pre-pandemic period). We stopped data collection in August 2020, which may limit generalizability through the remainder of the pandemic. We also examined how different public health-related mandates and statewide business openings/closings in Arizona, affected daily ED visits to the medical center. We created scatter plots for comparing the total daily ED visits, monthly ED visits for each ESI (i.e., ESI 1, ESI 2, ESI 3, ESI 4, and ESI 5), monthly admissions to each hospital unit (i.e., medical/surgical unit, step down/intermediate unit, and ICU), and monthly activations of each specialty team (i.e., trauma, STEMI, stroke, and sepsis) in the medical center before the COVID-19 pandemic with those during the pandemic. To compare mean differences from the pre-pandemic period with those of pandemic period, we performed paired Wilcoxon test (also known as Wilcoxon signed-rank test). We created a boxplot and reported summary statistics for four time periods affected by public health mandates and statewide business openings/closings during the pandemic. We used the Wilcoxon test to compare the mean ED visits in these periods in pairs. Finally, we performed a negative binomial regression to predict the daily ED visits in the following months based on different variables, including being in non-infectious or early infectious periods, potential public health mandates such as business/service closures, stay-at-home order, business/service reopening, and mask mandates. All analyses were performed using R (version 4.0.5) statistical computing software.
Results
Trends in the daily ED visits before and during the COVID-19 pandemic
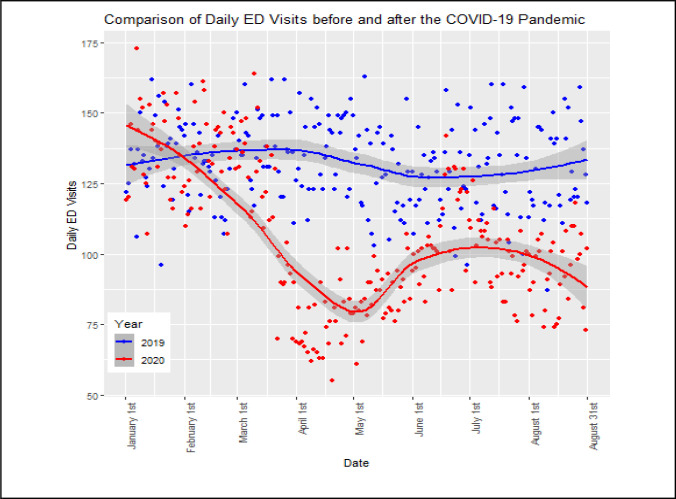
Our analyses show that, except for January, daily ED visits during the pandemic period were substantially lower than those during the pre-pandemic period (see Figure 1). The mean (±SD) of daily ED visits during the pandemic was lower than that during the pre-pandemic period (106 ± 25 vs. 132 ± 15, p < 0.05). Indeed, it decreased by 20% during the pandemic. The lowest number of ED visits occurred during April (55 visits). Although the number of daily ED visits during the pandemic has increased since the noticeable decrease in April, it remained lower than the corresponding number of daily ED visits in the previous year.
Figure 1.
Trends in the medical center’s daily ED visits before and during the COVID-19 pandemic
Daily ED visits in four specific periods
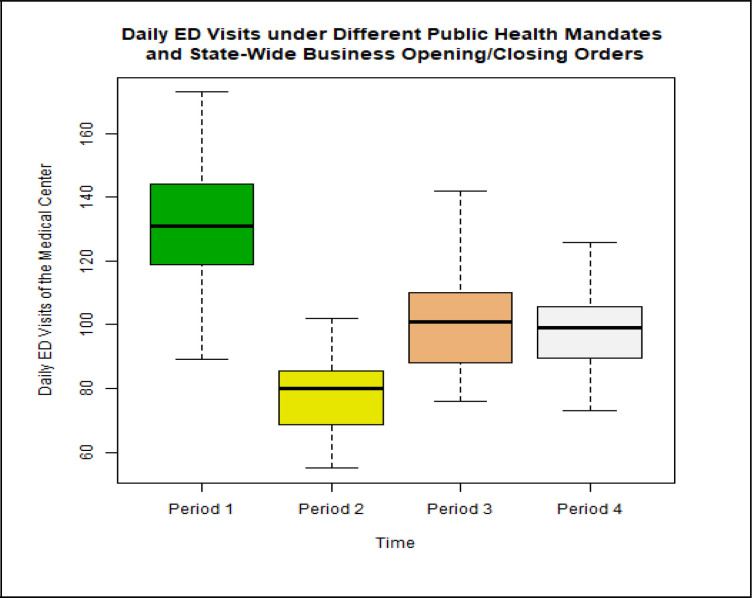
As shown in Figure 2, the medical center had its highest daily ED visits (173 visits) during the early infectious period and experienced its lowest daily ED visits (55 visits) following the stay-at-home order. After reopening businesses in Arizona, the daily ED visits increased; then, it went into a small decline following the second closure. However, there is not a significant difference between the mean (±SD) of daily ED visits in the reopening period and that in the second closure period (101 ± 17 vs. 97 ± 12, p = 0.43).
Figure 2.
Daily ED visits in four specific periods during the pandemic, including period 1 (early infectious period, Jan 1 - March 29), period 2 (Stay-at-home order, March 30-May 15), period 3 (re-opening to secondary closure, May 16 - Jun 29), period 4 (second closure to current, June 30 – current)
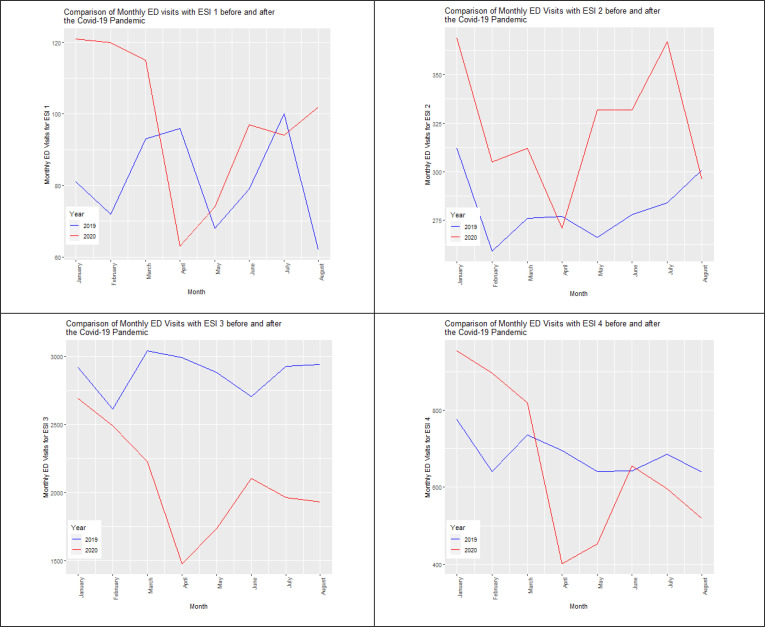
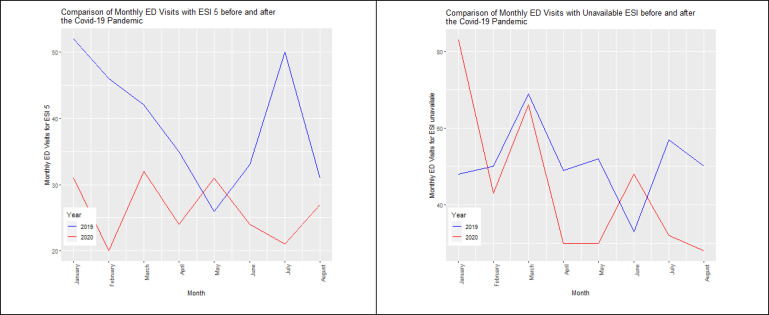
Monthly ED visits for each ESI before and during the COVID-19 pandemic
Every included patient should fit in one of the ESI categories (i.e., ESI 1, ESI 2, ESI 3, ESI 4, and ESI 5). In this measure of acuity, ESI 1 is the highest acuity and ESI 5 is the lowest acuity. ED visits with ESI 1 and ESI 2 are considered high acuity ED visits. The results show that the mean (±SD) of monthly high acuity ED visits during the pandemic was higher than that in the pre-pandemic period (421 ± 46 vs. 363 ± 22, p < 0.05) (see Table 1). Likewise, the proportion of high acuity ED visits during the pandemic was higher than that of the pre-pandemic period (13% vs. 9%, p < 0.05). As evident in Figure 3, the mean (±SD) of monthly ED visits with ESI 3 in 2020 was lower than that in 2019 (2079 ± 394 vs. 2878 ± 146, p < 0.05). However, the mean (±SD) of monthly ED visits with ESI 4 during the pandemic was not significantly different from that during the pre-pandemic period (662 ± 207 vs. 682 ± 51, p = 0.74). The results also show that the mean (±SD) of monthly ED visits with ESI 5 during the pandemic period was lower than that in the pre-pandemic period (26 ± 5 vs. 39 ± 10, p < 0.05). Accordingly, ED visits with ESI 5 had the sharpest decline (33%) during the pandemic in comparison with the other ESI categories, showing the patients with the lowest acuity were most likely to avoid visiting EDs to get medical care during the pandemic.
Table 1.
High acuity ED visits
| Month | Number of ED visits | Number of high acuity ED visits | Proportion of high acuity ED visits | |||
| 2019 | 2020 | 2019 | 2020 | 2019 | 2020 | |
| January | 4190 | 4252 | 393 | 490 | 9.4% | 11.5% |
| February | 3681 | 3875 | 331 | 425 | 9% | 11% |
| March | 4259 | 3573 | 369 | 427 | 8.7% | 12% |
| April | 4143 | 2266 | 373 | 334 | 9% | 14.7% |
| May | 3937 | 2655 | 334 | 406 | 8.5% | 15.3% |
| June | 3770 | 3263 | 357 | 429 | 9.5% | 13.1% |
| July | 4105 | 3075 | 384 | 461 | 9.4% | 15% |
| August | 4024 | 2905 | 363 | 398 | 9% | 13.7% |
Figure 3.
Trends in the monthly ED visits for each ESI before and during the COVID-19 pandemic. Figure 3 shows that, during the pandemic, the medical center had the lowest number of ED visits for each ESI in April, except for the ED visits with ESI 5.
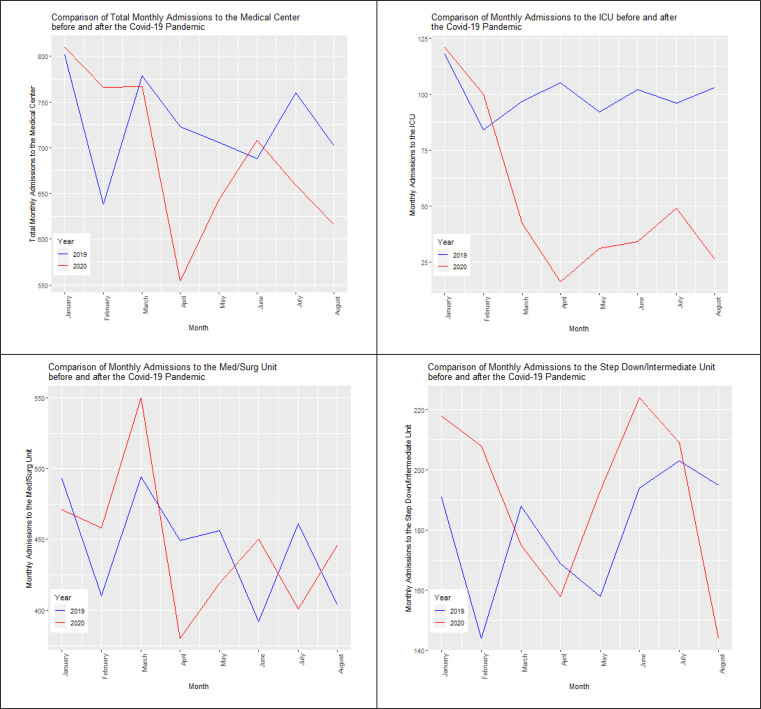
Monthly admissions to hospital care units before and during the COVID-19 pandemic
Patients presenting to emergency departments may get admitted to one of the hospital units (medical/surgical care unit, step down/intermediate care unit, intensive care unit), depending on the level of care needed. The analysis of monthly admissions to each unit shows that the center experienced a sharp decline in the number of admissions to all of its units in April after implementing a business closure order on March 19th and stay at home order on March 30th in the state of Arizona (see Figure 4). In addition, the admissions to each unit of the medical center increased in May following the reopening of businesses on May 16th. Since the declaration of public health emergency on March 11th, the medical center experienced the most admissions to each of its hospital units in June when the businesses were open and mandating wearing masks initiated on June 19th.
Figure 4.
Trends in monthly admissions to each unit of the medical center before and during the COVID-19 pandemic. As evident in Figure 4, during the pandemic, the ICU of the medical center had the sharpest decline in the number of admissions compared to the other hospital units.
According to the results, there is not a significant difference between the mean (±SD) of monthly admissions to the medical center during the pandemic period and that during the pre-pandemic period (690 ± 87 vs. 725 ± 53, p = 0.383). Also, there is not a significant difference between the mean (±SD) of monthly admissions to the step down/intermediate unit during the pandemic period and that during the pre-pandemic period (191 ± 29 vs. 180 ± 21, p = 0.461). The mean (±SD) of monthly admissions to the medical/surgical unit did not significantly change during the pandemic compared with the pre-pandemic period (447 ± 52 vs. 445 ± 39, p = 1). On the other hand, the results show that the mean (±SD) of monthly admission to the ICU during the pandemic is not the same as that during the pre-pandemic period (52 ± 38 vs. 100 ± 10, p < 0.05). Indeed, there is a sharp decline (48%) in the mean of monthly admission to the ICU during the pandemic in comparison with the pre-pandemic period. There is not a significant difference between the proportion of ED visits that get admitted during the pandemic and that during the pre-pandemic period (20.5% vs. 18.2%, p = 0.104). The proportion of the ED visits that become ICU admits during the pandemic is, however, lower than that during the pre-pandemic period (1.5% vs. 2.5%, p < 0.05) (see Table 2).
Table 2.
Number and proportion of ED visits that get admitted or become ICU admits
| Month | Number of ED visits | Number of ED visits that get admitted | Number of ED visits that become ICU admits | Proportion of ED visits that get admitted | Proportion of ED visits that become ICU admits | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | 2019 | 2020 | 2019 | 2020 | 2019 | 2020 | 2019 | 2020 | |
| January | 4190 | 4252 | 802 | 810 | 118 | 121 | 19.4% | 18.4% | 2.8% | 2.8% |
| February | 3681 | 3875 | 638 | 766 | 84 | 100 | 18.5% | 19.3% | 2.3% | 2.6% |
| March | 4259 | 3573 | 779 | 767 | 97 | 42 | 18.7% | 19.1% | 2.3% | 1.2% |
| April | 4143 | 2266 | 723 | 554 | 105 | 16 | 19.1% | 19% | 2.5% | 0.7% |
| May | 3937 | 2655 | 706 | 643 | 92 | 31 | 17.3% | 19.8% | 2.3% | 1.2% |
| June | 3770 | 3263 | 688 | 708 | 102 | 34 | 18.3% | 21.5% | 2.7% | 1.0% |
| July | 4105 | 3075 | 760 | 659 | 96 | 49 | 17.5% | 24.5% | 2.3% | 1.6% |
| August | 4024 | 2905 | 702 | 616 | 103 | 26 | 17.9% | 24.2% | 2.6% | 0.9% |
Monthly activations of each specialty team before and during the COVID-19 pandemic
The analysis of data on the number of activations of each specialty team in the medical center before and during the pandemic showed quite a few different trends. The mean of monthly trauma activations decreased by 15% during the pandemic (105 ± 18 vs. 135 ± 16, p < 0.05). Conversely, the mean of monthly sepsis activations increased by 15% during the pandemic compared to the pre-pandemic period (109 ± 14 vs. 95 ± 9, p < 0.05). There is not a significant difference between the mean (±SD) of monthly STEMI activations during and before the pandemic (2 ± 2 vs. 3 ± 1, p = 0.105). Likewise, there is not a significant difference between the mean (±SD) of monthly stroke activations during the pandemic period and that during the pre-pandemic period (4 ± 1 vs. 4 ± 3, p = 0.573).
Negative binomial regression
We performed a negative binomial regression to predict the daily ED visits in the next months based on different variables, including being in non-infectious or early infectious periods, potential public health mandates, including business/service closures, stay-at-home order, business/service reopening, and mandatory wearing masks. To do so, the number of ED visits is considered as the dependent variable. Also, each of the specific periods and each of the public health mandates is considered as a binary variable. A binary variable associated with a specific period is equal to 1 during that period. Also, a binary variable associated with a public health mandate is equal to 1 when that mandate is implemented. As shown in Table 3, business closure, stay-at-home order, and business reopening have a reverse relationship with the daily ED visits and make a decline in it. Also, business closure makes the most decrease in the daily ED visits in comparison with the other public health mandates. On the other hand, according to the results, the mandatory wearing of masks increases the daily ED visits. In addition, the medical center has more ED visits during non-infectious or early infectious periods in comparison with the pandemic period. Furthermore, daily ED visits are more during the early infectious period in comparison with the non-infectious period.
Table 3.
Negative binomial regression model results
| Variable | Coefficient | Rate Ratio | 95% Confidence Interval | |
|---|---|---|---|---|
| Intercept | 4.721 | 112.226 | 99.309 | 126.852 |
| Non-infectious period | 0.146 | 1.157 | 1.023 | 1.308 |
| Early infectious period | 0.182 | 1.199 | 1.064 | 1.351 |
| Business closure | -0.349 | 0.705 | 0.650 | 0.765 |
| Stay-at-home order | -0.011 | 0.989 | 0.896 | 1.093 |
| Business reopening | -0.157 | 0.855 | 0.762 | 0.958 |
| Mandatory wearing masks | 0.2 | 1.222 | 1.122 | 1.330 |
Conclusion
We observed that daily ED visits during the COVID-19 pandemic substantially decreased compared to the pre-pandemic period. However, it is not clear whether this reduction in the number of ED visits is because of a decline in the number of COVID-19 patients or because of a decline in the number of patients unrelated to COVID-19 who avoid visiting EDs due to the fear of seeking care in hospitals due to the pandemic. Also, the sharpest decline in the number of ED visits was in April 2020 after the implementation of state-wide business closure and stay-at-home orders. We observed an initial decrease in ED visits started just before these public health mandates, which may be because of voluntary self-isolation before the mandatory public health orders. The results show that the number of ED visits increased in May 2020. This could be because of reopening businesses and services, increasing the spread of the virus in the community, and increases in the number of patients who need to visit EDs.
ED visits with ESI 5 had the sharpest decline in comparison with the other ESI categories, suggesting that patients with the lowest acuity were most likely to avoid visiting EDs to get medical care during the pandemic. Although the proportion of ED visits resulting in ICU admission has not substantially changed in comparison with the prior year, the results show a significant decrease in the number of ICU admissions through the ED. This decline in ICU admissions raises concern that critically ill patients may not be getting timely care during the pandemic due to the fear of seeking care or travel restrictions. This ultimately delays interventions for serious health conditions and may also cause a surge in the number of ICU admissions after the pandemic subsides. It is yet to be determined whether there was an actual decrease in the number of patients who need intensive treatment during the pandemic and whether the decline in ICU admissions due to the pandemic increased the mortality rate. If confirmed, suitable strategies should be implemented to provide appropriate and prompt care to critically ill individuals. With this in mind, a more comprehensive dataset from multiple sites and for a longer time period is needed to be able to investigate the effectiveness of the public health mandates. Future extensions of this work include investigating the impact of public health mandates on the daily ED visits while adjusting for seasonality of daily ED visits.
Acknowledgment
This work was supported in part by the State of Arizona Technology and Research Initiative Fund (TRIF).
Footnotes
Equal contribution
Figures & Table
References
- 1.Jeffery MM, D’Onofrio G, Paek H, Platts-Mills TF, Soares WE, Hoppe JA, Genes N, Nath B, Melnick ER. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA internal medicine. 2020 Oct 1;180(10):1328–33. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gallaway MS, Rigler J, Robinson S, Herrick K, Livar E, Komatsu KK, Brady S, Cunico J, Christ CM. Trends in COVID-19 incidence after implementation of mitigation measures—Arizona, January 22-August 7, 2020. Morbidity and Mortality Weekly Report. 2020 Oct 9;69(40):1460. doi: 10.15585/mmwr.mm6940e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Westgard BC, Morgan MW, Vazquez-Benitez G, Erickson LO, Zwank MD. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Annals of Emergency Medicine. 2020 Nov 1;76(5):595–601. doi: 10.1016/j.annemergmed.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, Gundlapalli AV. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019-May 30, 2020. Morbidity and Mortality Weekly Report. 2020 Jun 12;69(23):699. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adjemian J. Update: COVID-19 Pandemic-Associated Changes in Emergency Department Visits—United States, December 2020-January 2021. MMWR. Morbidity and Mortality Weekly Report. 2021;70 doi: 10.15585/mmwr.mm7015a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lange SJ, Ritchey MD, Goodman AB, Dias T, Twentyman E, Fuld J, Schieve LA, Imperatore G, Benoit SR, Kite‐Powell A, Stein Z. Potential indirect effects of the COVID‐19 pandemic on use of emergency departments for acute life‐threatening conditions—United States. January-May 2020. [DOI] [PMC free article] [PubMed]
- 7.Kim HS, Cruz DS, Conrardy MJ, Gandhi KR, Seltzer JA, Loftus TM, Fant AL, McCarthy DM. Emergency Department Visits for Serious Diagnoses During the COVID‐19 Pandemic. Academic Emergency Medicine. 2020 Sep;27(9):910–3. doi: 10.1111/acem.14099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Butt AA, Azad AM, Kartha AB, Masoodi NA, Bertollini R, Abou-Samra AB. Volume and acuity of emergency department visits prior to and after COVID-19. The Journal of emergency medicine. 2020 Nov 1;59(5):730–4. doi: 10.1016/j.jemermed.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bialek S, Gierke R, Hughes M, McNamara LA, Pilishvili T. Coronavirus disease 2019 in children—United States, february 12-april 2, 2020. Morbidity and Mortality Weekly Report. 2020 Apr 10;69(14):422. doi: 10.15585/mmwr.mm6914e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iozzi L, Brambilla I, Foiadelli T, Marseglia GL, Ciprandi G. Paediatric emergency department visits fell by more than 70% during the COVID‐19 lockdown in Northern Italy. Acta paediatrica. 2020 Oct;109(10):2137–8. doi: 10.1111/apa.15458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Santoli JM. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration—United States, 2020. MMWR. Morbidity and mortality weekly report. 2020;69 doi: 10.15585/mmwr.mm6919e2. [DOI] [PubMed] [Google Scholar]
- 12.Li H, Yu G, Duan H, Fu J, Shu Q. Changes in children's healthcare visits during coronavirus Disease-2019 pandemic in Hangzhou, China. The Journal of pediatrics. 2020 Sep 1;224:146–9. doi: 10.1016/j.jpeds.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chaiyachati BH, Agawu A, Zorc JJ, Balamuth F. Trends in Pediatric Emergency Department Utilization after Institution of Coronavirus Disease-19 Mandatory Social Distancing. The Journal of Pediatrics. 2020 Nov 1;226:274–7. doi: 10.1016/j.jpeds.2020.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]