Abstract
The majority of prostate cancer survivors do not meet physical activity (PA) recommendations. Although technology has shown to promote PA, engagement has been a challenge. This mixed method study characterizes survivors’ needs and preferences for digital walking programs Through focus groups and surveys, we engaged prostate cancer support groups to describe PA motivators and barriers, interest in improving PA, and preferences for design features of a future digital walking program. Identified motivators (peers, positive thinking) and barriers (health issues) reflect PA needs that impact engagement. The most preferred features include: (1) well-curated, specific content, (2) individualized feedback from trusted sources, (3) moderated peer discussion, and (4) support from small teams and peer mentors. These findings inform digital PA programs that survivors will find engaging and can promote PA.
Introduction
Prostate cancer is the second most common cancer in men with 1 in 8 diagnosed during his lifetime.1 With an estimated 248,530 new cases of prostate cancer in 20211 and a 5-year relative survival rate of 98%2, more than 3.1 M men in the United States are prostate cancer survivors1. Given the high disease burden of prostate cancer there is a need to identify strategies to improve quality of life among cancer survivors. Regular physical activity (PA) improves fitness, vitality and quality of life among cancer survivors5, 6, delays cancer progression7, and reduces the risk of prostate cancer mortality8. Despite the protective benefits of PA for prostate cancer survivorship 85% of prostate cancer survivors report not meeting PA recommendations9.
Even though traditional supervised exercise programs show effectiveness in improving PA for prostate cancer survivors,10 barriers including cost, lack of time and support, access to facilities, and exercise partners, as well as disease-specific barriers like treatment side effects (e.g., urinary incontinence, fatigue) can limit engagement in these programs11-12. There is an opportunity to leverage engaging digital technologies in distance-based programs that bring support to survivors in their own neighborhoods and communities as a feasible low cost alternative.
Digital PA programs provide the opportunity to deliver behavior change techniques13,14 (e.g., goal setting, feedback, social support) via an easy to access, low cost and scalable modality. Digital PA programs that use technologies like fitness trackers, mobile phones, social media have been shown to promote PA among prostate cancer survivors15-17. Yet, lack of adherence and sustained engagement in these digital interventions by prostate cancer survivors limits the effectiveness of these interventions17-19. Thus, a major gap in prior research is how to design digital PA programs that prostate cancer patients will find engaging and want to use. There is a need to understand what type of digital technology appeals most to prostate cancer survivors and how to package existing behavior change features in these digital tools to promote PA.
To address this gap, we engaged prostate cancer survivors and their loved ones in focus groups to understand their needs and preferences for digital walking interventions We particularly focused on walking as it is one of the most accessible forms of PA that requires no training and might be sustainable throughout a patient's life. The purpose of this study was to characterize the user needs and design preferences of digital walking programs that leverage fitness trackers and social media features for prostate cancer survivors. Findings offer guidance to inform the design of supportive PA content, self-tracking features, and peer support elements of digital tools that can promote walking.
Methods
We conducted a concurrent mixed methods20 study with focus groups and surveys. Study procedures were approved by the University of Washington Institutional Review Board. We recruited from prostate cancer support groups in the Seattle metropolitan area from July to August 2018 for focus groups conducted at regularly scheduled support group meetings. Each focus group lasted for 60-90 minutes, was moderated by a team member and comprised 3 parts.
First, the moderated led group discussion on perceived benefits and barriers of walking. Participants wrote down ideas to the question “If you had a magic wand what is that one thing that would help you walk more”. The moderator collected these “magic wand” ideas marked on index cards and read examples aloud to ground group discussion on PA motivators and barriers. This discussion helped to establish and characterize user needs for digital PA programs.
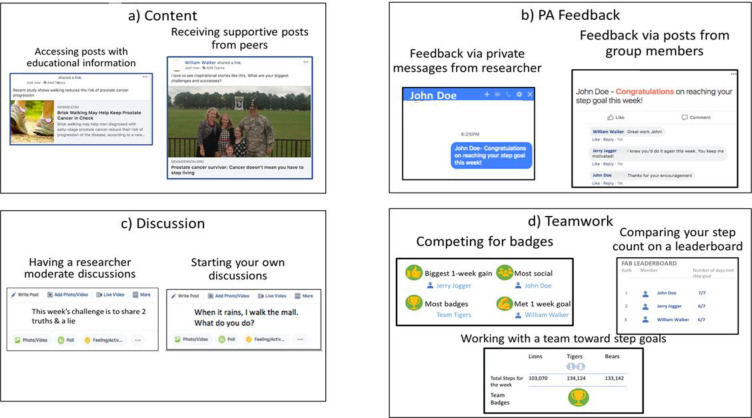
Second, the facilitator introduced the design concept of a digital walking program that incorporated a fitness tracker (i.e., Fitbit) and a social media-based platform (i.e., Facebook) to increase step count. The features of the digital walking program were designed based on best practice and evidence-based recommendations13,14,21 to facilitate personalized goal tracking, feedback, and social support. We collected qualitative data on design features participants prefer across 4 sets of options presented through mock interfaces: content, PA feedback, group discussion, and teamwork (Figure 1). Participants discussed likes and dislikes about these feature and ways each could be improved.
Figure 1.
Mock interfaces for design features: A) Content, B) PA feedback, C) group discussion, and d) teamwork
Third, after the focus group, participants completed an optional exit survey to report participant characteristics (i.e., demographics, technology experience), interest in improving PA (not at all interested, somewhat interested, very interested), and importance of each design feature (not important, less important, more important, most important).
Data analysis
Focus group sessions were audio recorded and transcribed for qualitative analysis. Two members of the research team took notes during each session to supplement transcripts. We deductively coded this data with a high-level a priori coding schema: PA motivators, PA barriers, and preferences for each of the 4 features (i.e., content, PA feedback, group discussion, and teamwork). A team member (SS) analyzed transcripts using the coding schema in Dedoose22. The researchers (AL and SS) met during the coding process to discuss sub-codes and refine coding categories.
We quantitatively analyzed survey data with SPSS 26.0 (SPSS Inc). We used descriptive statistics to summarize participant characteristics, interest in using digital PA programs, and preferred design features based on ratings of importance. We used inferential statistics to compare interest level and preferences for design features across all participants and among the 3 focus group sessions. We used Friedman tests (X2) to assess differences across participants and Kruskal Wallis tests (H) to assess differences among groups. We used Dunn tests (Z)23 with a Bonferroni adjustment for post hoc pairwise comparisons for significant results.
Results
1. Participants
Across the 3 focus groups (FG1, FG2, FG3), we engaged 61 members of prostate cancer support groups, of whom 49 responded to the survey (80%). Table 1 summarizes the characteristics of survey respondents who were predominantly older white males, college educated or greater, and 44 reported having been diagnosed within 4 months to 21 years (mean = 7 SD=6). Respondents who were prostate cancer survivors indicated a range of treatments (e.g., radiation, cryotherapy, cyber knife). Of the 5 respondents who did not report having a prostate cancer diagnosis, three identified as a spouse, and one as a caregiver, and one did not report their role. The majority of respondents reported using the internet and smartphones, but less than half reported using social media and less than one quarter reported using a fitness tracker.
Table 1.
Characteristics of survey respondents
| All (n=49) | FG 1 (n=20) | FG 2 (n=11) | FG 3 (n=18) | |||||
|---|---|---|---|---|---|---|---|---|
| Mean(sd) Range | N (%) | Mean (sd) Range | N (%) | Mean (sd) Range | N (%) | Mean (sd) Range | N (%) | |
| Age | 72(7) 59-89 |
72(5) 60-79 |
72(10) 59-89 |
73(7) 59-83 |
||||
|
Sex Male Female |
45 (92) 4 (8) |
18 (90) 2 (10) |
11(100) 0 |
16 (89) 2 (11) |
||||
|
Race White Non-white Declined to state |
43 (88) 4 (8) 2 (4) |
18 (90) 1 (5) 1 (5) |
9 (82) 2 (18) 0 |
16 (89) 1 (6) 1 (6) |
||||
|
Ethnicity Hispanic/Latino Not Hispanic/Latino Declined to state |
0 (0) 43 (88) 6 (12) |
0 17 (85) 3 (15) |
0 9 (82) 2 (18) |
0 17 (94) 1 (6) |
||||
|
Education High school College Advanced degree Doctorate Decline to state |
9 (18) 17 (35) 20(41) 2 (4) 1 (2) |
3 (15) 6 (30) 9 (45) 2 (10) 0 |
2 (18) 4 (36) 5 (45) 0 0 |
4 (22) 7 (39) 6 (33) 0 1 (6) |
||||
|
Technology use Use Internet Use smartphone Use social media Use a fitness tracker |
46 (94) 37 (76) 19 (39) 11 (22) |
20 (100) 14 (70) 8 (40) 7 (35) |
10 (91) 9 (82) 2 (18) 0 |
16 (89) 14 (78) 9 (50) 4 (22) |
||||
2. Motivators and Barriers to PA
Across focus groups a range of “magic wand” ideas surfaced. Table 2 summarizes a few of these ideas. We categorized ideas as technology-based (e.g., reminders, virtual competitions), peer support (e.g., walking buddy, coach), and other ideas, such as “a zapper”.
Table 1:
“Magic Wand” ideas from participants
| Technology-based ideas | Peer support ideas | Other ideas |
|---|---|---|
|
|
|
As the group discussed these magic wand ideas, participants described individual experiences with PA and key PA motivators and barriers surfaced, which we summarize below.
PA motivators: Participants expressed both internal and external motivators for PA. Participants told us that considering PA as likable and fun is an important internal motivator for PA. For example:
“Let’s start with basics – what do you like to do? I like to go for a walks and runs in forests, I like to move in beautiful places….If you are happy when you are walking, you are in magic land. So that’s what I do. I walk the trails and the cliffs .. and I wouldn’t miss it for the world. So that’s like we get things turned around just get the tools that makes it work. What works for us and what’s suits our nature.” (FG 3)
“Nobody likes boring exercises! It needs to be made fun and it could be anything from dance classes to you know going on group walks or things like that….rather than that just going to the gym and going for a walk there are a lot of other things you can do to get the exercise that are a lot more fun at the same time. Sometimes people don’t connect fun activities with exercise you don’t even know. But it is.” (FG 3)
Participants also indicated that personal characteristics, like fear of failure, serve as internal motivators:
“I hated failing. That [failure] was more of a push than the rewards for being successful.” (FG2)
Another participant expressed the value of positive attitude and thinking as an internal PA motivator:
“Positive attitude is probably the basic for my good health.…There are a lot of opportunities for good health like health clubs, there are things that people can do that don’t get enough exposure. People get on a positive line of thought and those problems start to get away if you start doing what’s best for you.” (FG 3)
In addition to internal motivators, participants also indicated external motivators from others. Advice from healthcare providers was a key motivator for many, for example, participants shared:
“My doctor told me that I can start hormone therapy and one of the side effects is that it weakens your structural system, and so you need to do some basic strength exercise to combat that down. Well that was the only motivation I needed, it’s just that.” (FG 2)
“I asked the surgeon “what’s the best exercise I can do”? He said “Walking. You need to walk”. And then he added “Not just walk but you’ve got to press yourself.” (FG 2)
Peers were also described as external motivators for PA. For example, participants told us:
“The people that I know, or I’ve come to know, at the YMCA that work out at the same time I do. And they’ve become friends. And I look forward to seeing them… they are friends. I feel like letting them down if I didn’t [go].” (FG 2)
“I think the strongest motivation or motivator would be other people in the group. I don’t know if one of them is not feeling well, the others might go “we missed you.” (FG 1)
Finally, participants indicated the importance of family for motivating them to get more PA:
“My wife is on Fitbit she gets these badges for walking across and stuff like that. She’s competed against other family members for a while. There was a kind of competition and things you know.” (FG 2)
PA barriers: Participants focused on health factors that negatively impact PA, such as recovering from medical procedures or health conditions. For example, participants told us:
“When you have something happen like surgery or an acute event it’s like you lose a lot of ground and need a lot of support on the way back.” (FG 3)
“if someone has irritable bowel it makes it a challenge to head outside without having facilities nearby.”(FG 1)
3. Interest in improving PA
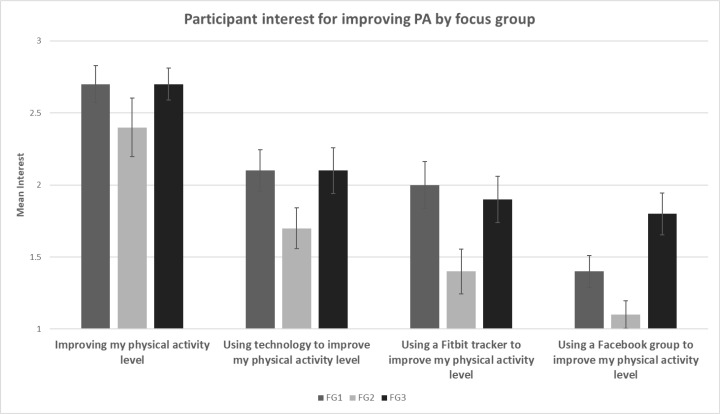
Figure 2 summarizes interest level of survey respondents by focus group. Across all participants, there was high interest in “Improving my PA level” (mean =2.6, SD= 0.6), but less interest in “Using technology to improve my PA level” (mean=2.0, SD= 0.6), “Using a Fitbit tracker to improve PA level” (mean=1.8, SD= 0.7), or “Using a Facebook group to improve my PA level” (mean=1.5, SD= 0.6). Across all participants, this interest varied significantly (χ2 (3) = 77.50, p<0.001). Post hoc pairwise comparisons show significantly greater interest in “Improving my PA level” than improving PA level by (1) using technology (Z= 0.967, p<0.002), (2) using Fitbit (Z=1.272, p<0.001), or (3) using a Facebook group (Z=1.804 p<0.001). We also found significantly greater interest across all participants in using technology to improve PA level than using a Facebook group to improve PA level (Z=0.837, p=0.011).
Figure 2:
Interest in four options for improving PA by focus group (1 = “Not at all interested”; 3 = “Very Interested”)
Among the three focus groups, there was a significant difference in interest for using a Facebook group to improve PA level (H (2) = 11.367, p = 0.003). Post hoc pairwise comparison indicated this difference was between FG2 and FG3 (Z=15.167, p = 0.004). There were no other significant differences among focus groups.
Group discussion supported these differences and provided insight into participants’ somewhat guarded interest in technologies like Fitbit trackers and Facebook. Use of these technologies was generally low (Table 1) but not universal. One participant expressed challenges with using technology for PA because:
“The technology changes so quickly” (FG 3)
Other participants shared negative experiences and challenges with wearable devices:
“I had a Fitbit and it really helped me walk. But it fell apart in less than a year.“ (FG 1)
“If you ride a bike for an hour, you get this many calories burned. If you walk for an hour, you get this many calories burned - when it is quite different when you're going up that big hill or down that big hill. So, I like a little bit more finding ways of getting a little bit more specific.” (FG 2)
Some participants who were not social media users expressed disinterest:
“I don't want to participate in a Facebook which I don't belong to now.” (FG 2)
However, other participants liked the idea of using technology to track PA data, schedule PA, and for reminders. Participants also expressed interest in using technology for self-monitoring:
“So you can do self-evaluation of where you are at… A bunch of data there that he [referring to a coach] compares to your age group. If there was something similar where you could do your own self-evaluation will be helpful.” (FG 3)
Some participants also liked being part of an online group. For example, one participant stated:
“Even in this group I mean there is probably 6 or so different categories of pace or style or even interest. I mean if we can network with real people, that’s the motivation that people like this go for I think…” (FG1)
4. Preferred design features of digital walking programs
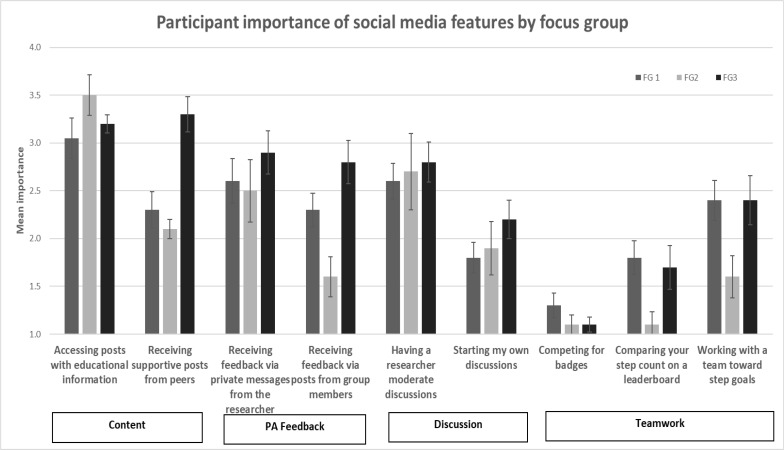
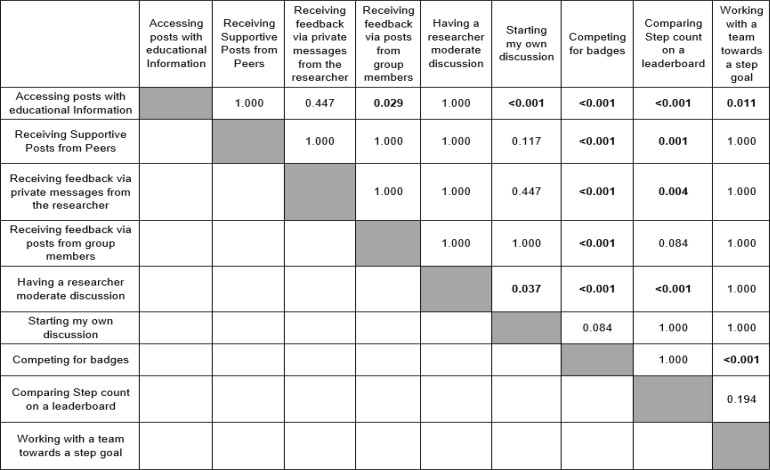
Figure 3 summarizes survey respondents’ mean importance ratings for the nine design options categorized by content, PA feedback, discussion and teamwork. Across all participants, there was a significant difference in perceived importance across the nine design options (X2 = 126.301, p <0.001). Post hoc comparisons (Table 2) indicate that some features, such as “accessing posts with educational information”, were rated significantly more important than “receiving feedback via posts from group members” (z=2.024, p=0.029), “starting my own discussion” (z=3.024,p<0.001), “competing for badges” (z=4.866,p<0.001), “comparing step count on a leaderboard” (z=3.866,p<0.001), and “working with a team towards a step goal” (z=2.813, p=0.011). In contrast, “competing for badges” was rated less important than all other options except “starting my own discussions” (Z=3.044 p=0.084).
Figure 3:
Participant importance of social media features by focus group (1= not important; 4= most important)
We describe quantitative differences and qualitative comments that support differences within the four sets of options categorized by content, PA feedback, discussion and teamwork below
Content options: Across all participants, the highest rated feature on average was “accessing posts with educational content” (mean = 3.2 out of 5, SD= 0.7). However, there were a not significant difference between importance of this option and “receiving supporting posts from peers” (mean = 2.6, SD= 0.9). Among focus groups, there was a significant difference in importance of “receiving supportive posts from peers” (H (2) = 14.615, p < 0.001). Post hoc comparisons found this difference was between FG2 and FG3 (z= -3.141, p = 0.005) and between FG1 and FG3 (z= -3.354, p = 0.002).
Focus group discussion helps explain and further define these design preferences. Participants indicated that they preferred receiving authoritative information from researchers, coaches, mentors, and clinicians. They expressed interest in receiving quality information that was well curated. Participants also expressed greater interest in receiving information that was specific to prostate cancer than general PA information.
“Well curated, authoritative, interesting content is key.” (P48, FG3)
“When I first got diagnosed with prostate cancer that’s what I did it [referring to finding information on google] and you get all kinds of information too much, perhaps if it was something like this that's more directed it could be more useful” (FG 3)
Other types of information participants preferred related to personalized exercise, activities, healthy diet and recipes, and goal setting.
PA feedback options: Overall, participants rated the importance of “receiving feedback via private messages from the researcher” (mean = 2.7, SD=1.0) higher than “receiving feedback via posts from group members” (mean = 2.3, SD =0.9), but this difference was not significant. Among focus groups there was a significant difference in importance of “receiving feedback via posts from group members” (H (2) = 11.076, p = 0.004). Post hoc comparisons found this difference was between FG2 and FG3 (Z=-3.302, p = 0.003).
Through discussion, participants further describe these preferences. Some indicated that rather than receiving PA feedback from strangers (e.g., people on social media they do not know) they would prefer receiving feedback either from an “accountability partner”, such as a “moderator”, “coach”, or “matched peer”. Participants expressed a preference for in-person meetings to get to know other participants, such a peer support person, before joining a social media-based PA program. Some felt that meeting in-person could help build trust, shared goals, and motivate progress toward PA goals.
“So it should be someone we know, we like and trust - it takes about a meeting or two probably. “(FG1)
“I think the strongest motivation or motivator would be other people in the group. I don’t know if one of them is not feeling well the other might go “we missed you”. (FG1)
Some participants were also open to receiving automated feedback from technology:
“Just some kind of feedback that ‘You made it!’ doesn't need to come from a person”(FG 2)
Discussion options: Across all participants, the importance of “having a researcher moderate discussions” (mean = 2.7, SD =0.9) was rated significantly higher than “starting my own discussions” (mean = 2.0, SD =0.8) (z=3.286, p=0.037). There were no significant differences among focus groups for these two discussion options.
Despite the quantitative preference for moderated over self-initiated discussions from surveys, focus group discussion indicated that participants preferred a combination of moderated and peer discussion. They were interested in discussing with a group they were familiar with who shared a similar situation. Many participants indicated that the support group they were currently a part of provided them with opportunities for discussion and a similar group discussion online might be similarly beneficial.
“We can always use more data and information and that’s the stuff we would like to see. Research thoughts about what we can do better and mitigate any of the side effects and to work on not having again those kind of stuff but food not to eat, what foods to eat more of, dietary concerns if those things are proven to be effective and helpful.” (FG2)
Teamwork options: Across all participants, the importance of “working with a team toward step goals” (mean = 2.3, SD = 1.0) was rated higher than “comparing your step count on a leaderboard” (mean = 1.6, SD=0.8), which was rated higher than “competing for badges” (mean = 1.2 , SD=0.4). There was a significant difference between competing for badges and working with a team towards a step goal (Z = -4.436, p<0.001). There was no significant difference among focus groups for any of the 3 teamwork options.
Focus group discussion further describes these preferences. Most participants were not interested in competing with one another, which they attributed to age. Some participants indicated they were a little competitive, while most others indicated that they were only interested in competing with themselves and not against others. Thus, participants expressed little interest in competing for badges or comparing goals on a leaderboard for rewards and incentives.
“I could care less if John Doe who I don't know has 10 million steps doesn't do me.. it's not going to motivate me any further” (FG 2)
“FGP (female) - I think competing for badges is not for our age group maybe for younger age group but just did you make your goal yeah did you set a goal did you make your goal if you did give yourself a pat on the back if you did great” (FG 3)
In contrast to competition, rewards, and incentives, participants expressed much greater interest in working with a team towards PA goals, sharing experiences, mentoring each other and motivating each other. Participants preferred closed groups with opportunities to socialize, learn from each other, share information, and find exercise partners or walking buddies.
“The only part about the teams, the last one, ‘working with the team towards step goals’ is if there is a way to set up a team where we can help each other and things more kind of like a mentorship type stuff if somebody is really struggling is there a role I can play to help that person in that process by being a team member with them and maybe that would help them. I might look at that.” (FG 2)
Discussion
Few studies have examined prostate cancer survivors’ needs and design preferences for digital walking programs, despite their potential. Through this concurrent mixed methods study, members of prostate cancer support groups offered valuable input that informs development of digital walking programs that have potential to engage users and thus promote PA. The qualitative data from the focus groups helped with interpretation of the quantitative survey data and provided context to the results. Findings are important because prostate cancer survivors need PA support and experience barriers to program access and meeting national PA recommendations. Yet there has been little in the way of design guidance for engaging digital programs for this population. Our findings offer a first step by providing this design guidance based on the perspectives of prostate cancer survivors.
Our findings indicate that prostate cancer survivors express an interest in overcoming exercise barriers and improving their PA. When designing any digital program for this group it is valuable to consider features that reduce barriers and enhance internal motivators (e.g., fun, positive thinking) and offer connections with external motivators, such as providers, family, and peers. Even though the participants indicated moderate interest using technology to improve PA in surveys they also provided a range of technology based magic wand ideas to help them walk more (e.g., reminders, virtual community etc.). When designing interventions for prostate cancer survivors, care should be taken to address low technology use and guarded technology interests. Consider utilizing technology that is easy to use and simple for participants to perform desired functions (e.g., tracking data, setting reminders).
Based on our findings we recommend that a digital walking program for prostate cancer survivors be designed to: 1) provide well curated and specific content - both authoritative material from professionals and experiential material from peers; 2) provide individualized feedback (e.g., how one is doing relative to one’s own goals) based on tracked data or advice from a trusted, experienced source; 3) provide capabilities for a moderated discussion and the ability to facilitate discussions with peers (e.g., “Has anyone else dealt with the problem I am experiencing?”); and 4) enable users to work with peers to share interests, motivate each other, and find walking partners rather than compete. Our results indicate that a well-designed digital walking program that combines fitness trackers with social features (e.g find walking partners, motivate each other) could potentially increase access to and extend the reach of PA programs that better support survivors.
Facilitating behavior change for PA is multifaceted and complex. The behavior change intervention literature indicates that goal setting, feedback, self-monitoring, and social support (i.e. a combination of personal, interpersonal and environmental factors) should be considered when designing digital behavior change interventions for older adults.24 Yet care needs to be taken to match the behavior change technique to design features that users prefer and most likely to use. For example, our results indicate that participants lacked interest in competing for badges, even though these types of digital rewards are a feature that has been shown as beneficial in young adult cancer survivors24,25.Our findings offer a first step by offering guidance for design of engaging digital programs for prostate cancer survivors.
Findings should be evaluated in the context of some limitations. We conducted 3 focus groups in a single metropolitan area that limit could generalizability of findings. We explored the potential of designing engaging digital technology to promote PA in a sample that was low in both social media use and fitness tracker use. Lack of experience may have limited the ability for participants to imagine using these features. In addition, limitations like having certain dominant individuals in a group and other response biases that are inherent in focus groups might have influenced the data. Future work should extend the study to a broader audience, such as prostate cancer survivors who do not have access to support groups, diverse patients with respect to education, race ethnicity, and include more caregivers and friends. Future research should also evaluate feasibility and effectiveness of a digital walking program designed for prostate cancer survivors. Despite these limitations, our study has several strengths that include directly engaging future technology users and our mixed methods approach. Conducting focus groups at existing support group meetings, where participants regularly meet and are socially connected, facilitated a rich conversation and sharing of ideas.
Conclusion
Given the need to increase PA in prostate cancer survivors but lack of guidance for well-designed digital PA programs to facilitate behavior change, our findings characterize needs and design preferences for digital walking programs. Participants expressed interest in improving PA and expressed preferences for design of specific features for program content, PA feedback, discussion, and teamwork. Digital walking programs that are designed to meet these needs and preferences could enhance engagement by facilitating an accessible, convenient, and scalable solution for improving PA among prostate cancer survivors.
Table 2:
p values of pairwise comparisons of content options across all survey respondents (n=49)
References
- 1.American Cancer Society [Internet] Key Statistics for Prostate Cancer. Atlanta, GA: American Cancer Society; 2020. https://www.cancer.org/cancer/prostate-cancer/about/key-statistics.html . Date accessed February/2021. [Google Scholar]
- 2.Prostate Cancer Foundation [Internet] Prostate Cancer Survival Rates. Monica, CA: Prostate Cancer Foundation; 2020. www.pcf.org/about-prostate-cancer/what-is-prostate-cancer/prostate-cancer-survival-rates/ Date accessed February/2021. [Google Scholar]
- 3.Edwards BK, Noone AM, Mariotto AB, et al. Annual Report to the Nation on the status of cancer, 1975-2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer. 2014;120(9):1290–314. doi: 10.1002/cncr.28509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kornblith AB, Herr HW, Ofman US, et al. Quality of life of patients with prostate cancer and their spouses. The value of a data base in clinical care. Cancer. 1994;73(11):2791–802. doi: 10.1002/1097-0142(19940601)73:11<2791::aid-cncr2820731123>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 5.Schmitz K, Holtzman J, Courneya KS, et al. Controlled physical activity trials in cancer survivors: A systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2005;14(7):1588–1595. doi: 10.1158/1055-9965.EPI-04-0703. [DOI] [PubMed] [Google Scholar]
- 6.Thorsen L, Courneya KS, Stevinson C, Fosså SD. A systematic review of physical activity in prostate cancer survivors: outcomes, prevalence, and determinants. Supportive Care in Cancer. 2008;16(9):987–997. doi: 10.1007/s00520-008-0411-7. [DOI] [PubMed] [Google Scholar]
- 7.Richman EL, Kenfield SA, et al. Physical activity after diagnosis and risk of prostate cancer progression: Data from the cancer of the prostate strategic urologic research endeavor. Cancer Res. 2011;71(11):3889–95. doi: 10.1158/0008-5472.CAN-10-3932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kenfield SA, Stampfer MJ, Giovannucci E, Chan JM. Physical activity and survival after prostate cancer diagnosis in the health professionals follow-up study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2011;29(6):726. doi: 10.1200/JCO.2010.31.5226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arem H, Mama SK, Duan X, Rowland JH, Bellizzi KM, Ehlers DK. Prevalence of Healthy Behaviors among Cancer Survivors in the United States: How Far Have We Come? Cancer Epidemiol Biomarkers Prev. 2020;29(6):1179–1187. doi: 10.1158/1055-9965.EPI-19-1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baumann F, Zopf E, Bloch W. Clinical exercise interventions in prostate cancer patients–a systematic review of randomized controlled trials. Supportive Care in Cancer. 2012;20(2):221–233. doi: 10.1007/s00520-011-1271-0. [DOI] [PubMed] [Google Scholar]
- 11.Clifford BK, Mizrahi D, Sandler CX, et al. Barriers and facilitators of exercise experienced by cancer survivors: a mixed methods systematic review. Supportive Care in Cancer. 2018;26(3):685–700. doi: 10.1007/s00520-017-3964-5. [DOI] [PubMed] [Google Scholar]
- 12.Fox L, Wiseman T, Cahill D, et al. Barriers and facilitators to physical activity in men with prostate cancer: A qualitative and quantitative systematic review. Psycho-Oncology. 2019;28(12):2270–2285. doi: 10.1002/pon.5240. [DOI] [PubMed] [Google Scholar]
- 13.Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- 14.Elaheebocus S, Weal M, Morrison L, Yardley L. Peer-based social media features in behavior change interventions: Systematic review. J Med Internet Res. 2018;20(2):e20. doi: 10.2196/jmir.8342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coughlin S.S., Caplan L.S., Stone R. Use of consumer wearable devices to promote physical activity among breast, prostate, and colorectal cancer survivors: a review of health intervention studies. J Cancer Surviv. 2020;14:386–392. doi: 10.1007/s11764-020-00855-1. [DOI] [PubMed] [Google Scholar]
- 16.Khoo S, Mohbin N, Ansari P, Al-Kitani M, Müller AM. mHealth Interventions to Address Physical Activity and Sedentary Behavior in Cancer Survivors: A Systematic Review. International Journal of Environmental Research and Public Health. 2021;18(11):5798. doi: 10.3390/ijerph18115798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roberts AL, Fisher A, Smith L, Heinrich M, Potts HWW. Digital health behaviour change interventions targeting physical activity and diet in cancer survivors: a systematic review and meta-analysis. J Cancer Surviv. 2017;11(6):704–719. doi: 10.1007/s11764-017-0632-1. doi: 10.1007/s11764-017-0632-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams V, Brown N, Becks A, Pekmezi D, Demark-Wahnefried W. Narrative review of Web-based healthy lifestyle interventions for cancer survivors. Ann Rev Res. 2020;5(4) doi: 10.19080/arr.2020.05.555670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Forbes CC, Blanchard CM, Mummery WK, Courneya KS. Feasibility and preliminary efficacy of an online intervention to increase physical activity in Nova Scotian cancer survivors: A randomized controlled trial. JMIR Cancer. 2015;1(2):e12–e12. doi: 10.2196/cancer.4586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Plano Clark VL, Ivankova NV. Mixed methods research : a guide to the field. Sage Publications; 2016. [Google Scholar]
- 21.Stockwell S, Schofield P, Fisher A, et al. Digital behavior change interventions to promote physical activity and/or reduce sedentary behavior in older adults: A systematic review and meta-analysis. Exp Gerontol. 2019;120:68–87. doi: 10.1016/j.exger.2019.02.020. [DOI] [PubMed] [Google Scholar]
- 22.Dedoose 8.3.43 Web application for managing, analyzing, and presenting qualitative and mixed method research data. SocioCultural Research Consultants, LLC. 2019. www.dedoose.com.
- 23.Dunn OJ. Multiple Comparisons Using Rank Sums. Technometrics. 1964;6(3):241–252. [Google Scholar]
- 24.Devine KA, Viola AS, Coups EJ, Wu YP. Digital health interventions for adolescent and young adult cancer survivors. JCO Clinical Cancer Informatics. 2018;(2):1–15. doi: 10.1200/CCI.17.00138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mendoza JA, Baker KS, Moreno MA, et al. A Fitbit and Facebook mHealth intervention for promoting physical activity among adolescent and young adult childhood cancer survivors: A pilot study. Pediatr Blood Cancer. 2017;64(12) doi: 10.1002/pbc.26660. [DOI] [PubMed] [Google Scholar]