Abstract
Background:
Artificial intelligence-based technology systems offer an alternative solution for diabetic retinopathy (DR) screening compared with standard, in-office dilated eye examinations. We performed a cost-effectiveness analysis of Automated Retinal Image Analysis System (ARIAS)-based DR screening in a primary care medicine clinic that serves a low-income patient population.
Methods:
A model-based, cost-effectiveness analysis of two DR screening systems was created utilizing data from a recent study comparing adherence rates to follow-up eye care among adults ages 18 or older with a clinical diagnosis of diabetes. In the study, the patients were prescreened with an ARIAS-based, nonmydriatic (undilated), point-of-care tool in the primary care setting and were compared with patients with diabetes who were referred for dilated retinal screening without prescreening, as is the current standard of care. Using a Markov model with microsimulation resulting in a total of 600 000 simulated patient experiences, we calculated the incremental cost-utility ratio (ICUR) of the two screening approaches, with regard to five-year cost-effectiveness of DR screening and treatment of vision-threatening DR.
Results:
At five years, ARIAS-based screening showed similar utility as the standard of care screening systems. However, ARIAS reduced costs by 23.3%, with an ICUR of $258 721.81 comparing the current practice to ARIAS.
Conclusions:
Primary care-based ARIAS DR screening is cost-effective when compared with standard of care screening methods.
Keywords: artificial intelligence, cost-effectiveness analysis, diabetic retinopathy, healthcare economics, machine learning technology, public health
Introduction
Visual impairment secondary to diabetic retinopathy (DR) can be mitigated by regular screening eye examinations, which aids timely diagnosis and appropriate treatment. 1 For patients with DR, their disease course closely tracks their environment, access to healthcare, and economic resources. Improvements in screening and treatment of DR have led to an overall decrease in the prevalence of blindness caused by diabetic eye disease in recent years. However, these benefits are primarily observed in high-resource settings. 2 In the United States, rates of screening for DR in high-resource settings can be as high as 60%, 3 while some underserved patient populations are screened at rates less than 20%. 4 This discrepancy in rates of DR screening highlights the need to develop strategies that extend the benefits of monitoring and treatment for DR to all patients.
Efforts leveraging artificial intelligence (AI)-based technology are increasingly being used to improve the availability of DR screening. Automated Retinal Image Analysis Systems (ARIAS) can detect DR with high specificity and sensitivity. To date, the literature investigating ARIAS primarily focuses on its diagnostic accuracy as compared with manual grading of fundus photographs, and two ARIAS systems—IDx-DR and most recently EyeArt 2.0—have been approved by the FDA for clinical use in the United States.5-10
Although ARIAS are highly reliable tools for detecting DR,5,11 their value—or cost-effectiveness—to health care systems is less well understood. We sought to model short-term cost-effectiveness using data from a recent prospective study conducted within our institution’s health system analyzing adherence to recommended follow-up ophthalmic care among low-income adults with diabetes, after the implementation of an ARIAS-based screening program in a primary care clinic. We hypothesized that implementation of ARIAS in this low-income primary care setting would be cost-effective compared with the current standard of care in which all patients with diabetes are referred for annual dilated retinal examination.
Subjects, Materials, and Methods
Overview and Participant Data
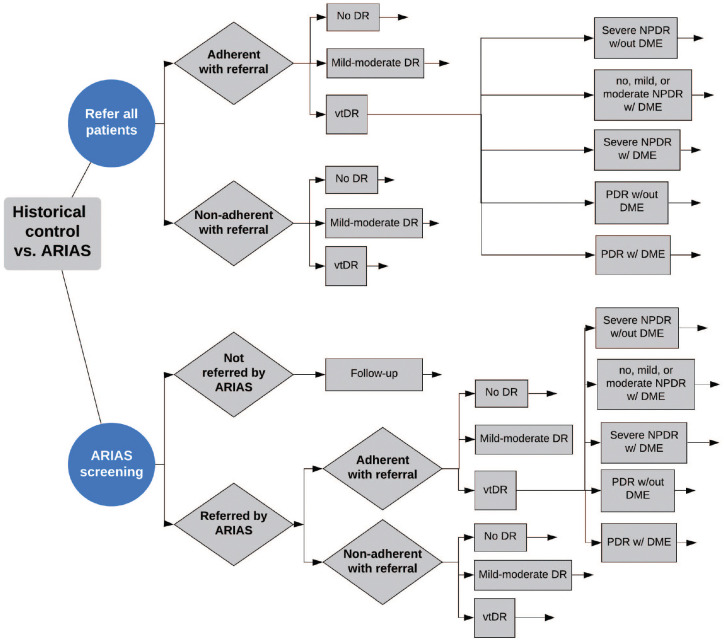
We constructed a decision tree to conduct a cost-effectiveness analysis comparing two screening strategies via Markov modeling with microsimulation. The experimental strategy involved ARIAS screening of all adult patients with diabetes performed in the primary care clinic, whereas the reference strategy was current standard of care: referring all patients with diabetes for a dilated screening eye examination.12-14 Our model used customized data for our institution derived from a prospective study performed by our group to examine the effects of an ARIAS-based primary care clinic DR screen on patient adherence to ophthalmic follow-up recommendations. 15 Briefly, 179 adults with diabetes were screened with ARIAS, performed using nonmydriatic (undilated) retinal photography and image grading with EyeArt 2.0 (Eyenuk, Inc., Woodland Hills, CA, USA; of note, EyeArt 2.0 recently received FDA clearance for clinic use of autonomous detection of DR, including vision-threatening DR [vtDR]). After screening using the system, most patients received their results immediately during the visit, including the severity of their DR, a picture of their fundus photograph, and recommended follow-up interval with an eye care specialist. Patients with referable DR (moderate DR or greater), vtDR (any central diabetic macular edema [DME] or severe DR or greater), or who had inconclusive screening results were referred for ophthalmic consultation. As is typical of many referrals primary care providers in our health care system make to specialists, a follow-up referral examination was scheduled by phone subsequent to the initial PCP encounter. Rates of adherence to these recommendations were then compared with historical adherence rates to ophthalmic consultation among adults with diabetes from the same clinic. We used the baseline demographic data, referral rates and adherence rates (Table 1), and DR severity distributions described in the referenced study for the present economic modeling analysis. 15
Table 1.
Referral and Adherence Rates and Diabetic Retinopathy (DR) Severity Prevalence between the Current Practice and ARIAS Cohorts.
| Current practice | ARIAS | Source | |
|---|---|---|---|
| % Referred for dilated eye examination | 100 | 50.8 | Liu et al. 15 |
| % Adherent with eye examination referral | 11.5 | 54.9 | |
| % Of all screened patients with completed eye examination | 11.5 | 27.9 | |
| % Mild-moderate diabetic retinopathy | 35.7 | 26.0 | |
| % Vision-threatening diabetic retinopathy | 7.5 | 10.0 |
ARIAS, Automated Retinal Image Analysis System.
DR Disease States
We defined vtDR as the presence of any central diabetic macular edema (DME), presence of severe nonproliferative DR (NPDR), or presence of proliferative DR (PDR) (Figure 1). After adjusting published epidemiologic data to reflect the racial/ethnic demographics among patients at our institution, we estimated the prevalence of each possible vtDR subtype or “state” (Table 2) and used these estimates in the economic model.16-19 As described in greater detail in the next section, treatment and complication rates during year one and years two to five for possible treatment approaches, as well as the rates of progression to severe vision loss (SVL) among patients who were treated, were based on the Diabetic Retinopathy Clinical Research Network (DRCR) Protocol I and S studies.18-22 The rate of progression to SVL for patients with vtDR who did not receive treatment was modeled based on epidemiologic data. These figures can be found in Table 3.18-23
Figure 1.
Truncated and simplified decision tree comparing Automated Retinal Image Analysis System screening to standard of care.
Table 2.
Modeled Prevalence of vtDR Subtypes with Associated Treatment Approach.
| Subtype of vtDR | Prevalence among all adults with vtDR (%) | Treatment approach | Source |
|---|---|---|---|
| Severe NPDR without DME | 91.0 | Close monitoring three times annually | Varma et al 16 |
| No or mild-moderate DR with DME | 5.8 | DRCR Protocol I, ranibizumab with deferred laser arm | Zhang et al 17 |
| Severe NPDR with DME | 0.6 | DRCR Protocol I, ranibizumab with deferred laser arm | Gross et al 18 |
| PDR without DME | 2.1 | DRCR Protocol S, PRP arm | Elman et al 19 |
| PDR with DME | 0.6 | DRCR Protocol S, ranibizumab arm | Elman et al 19 |
Note: Figures weighted to reflect the WUSTL primary care patient population.
DME, diabetic macular edema; DR, diabetic retinopathy; DRCR, Diabetic Retinopathy Clinical Research Network; NPDR, nonproliferative DR; PDR, proliferative DR; vtDR, vision-threatening DR.
Table 3.
Modeled Per-Patient Costs of Treatment and Complications for Year One and Years Two to Five for DME, PDR, and PDR with DME.
| Year 1 DME only per-patient treatment cost | Number | Cost ($) | Per-patient cost ($) | Source |
| No. of visits year one | 10 | Expert opinion, more conservative than the number listed in Qin 24 | ||
| Dilated examination | 10 | 101.27 | 1012.70 | |
| OCT | 10 | 41.81 | 418.10 | |
| No. of injections | 9 | 101.99 | 917.91 | Qin 24 |
| % Focal laser | 32.0 | 512.12 | 163.88 | Qin 24 |
| Subtotal | 2512.59 | |||
| 0.5-mg ranibizumab | 9 | 2114.06 | 19 026.54 | # of injections: Qin 24 price: Hutton et al. 14 , adjusted to 2019 dollars |
| Total cost with ranibizumab | 21 539.13 | |||
| Year one DME only per-patient complications cost | Proportion (%) | Cost ($) | Per-patient cost ($) | Source |
| % Retinal detachment | 0.5 | 2556.44 | 12.78 | Elman et al. 19 |
| % Vitrectomy | 2.0 | 3715.83 | 74.32 | |
| % Endophthalmitis | 0.5 | 3240.00 | 16.20 | |
| % Cataract surgery | 6.5 | 3229.80 | 209.94 | |
| % Elevated IOP | 2.0 | 767.00 | 15.34 | |
| Total | 328.58 | |||
| Years two to five DME only annual average per-patient treatment cost | Number | Cost ($) | Per-patient cost ($) | Source |
| No. of visits per year | 7 | Expert opinion, more conservative than the number listed in Elman et al. 21 ; Qin 24 | ||
| Dilated examination | 7 | 101.27 | 708.89 | |
| OCT | 7 | 41.81 | 292.67 | |
| No. of injections | 4.25 | 101.99 | 433.46 | Elman et al. 21 ; Qin 24 |
| % Focal laser | 12.8 | 512.12 | 65.30 | |
| Subtotal | 1500.31 | |||
| 0.5-mg ranibizumab | 4.25 | 2114.06 | 8984.76 | No. of injections: Elman et al. 21 ; Qin 24 price: Hutton et al. 14 , adjusted to 2019 dollars |
| Total | 10 485.07 | |||
| Years two to five DME only average annual per-patient complication cost | Proportion (%) | Cost ($) | Per-patient cost ($) | Source |
| % Retinal detachment | 0.3 | 2556.44 | 6.46 | Elman et al. 19 ; Gross et al. 20 ; Elman et al. 21 |
| % Vitrectomy | 0.7 | 3715.83 | 27.78 | |
| % Endophthalmitis | 0.3 | 3240.00 | 10.13 | Elman et al. 19 ; Gross et al. 20 estimating 0.25% per year for years three to five |
| % Cataract surgery | 6.4 | 3229.80 | 205.09 | Elman et al. 19 ; Gross et al. 20 ; Elman et al. 21 |
| % Elevated IOP | 2.8 | 767.00 | 21.09 | |
| Total | 270.54 | |||
| Year one PDR per-patient treatment cost (PRP arm) | Number | Cost ($) | Per-patient cost ($) | Source |
| No. of visits year one | 5 | Expert opinion, more conservative than the number listed in Gross et al. 18 | ||
| Dilated examination | 5 | 101.27 | 506.35 | |
| OCT | 5 | 41.81 | 209.05 | |
| No. of initial PRP sessions | 1.55 | 314.26 | 485.69 | Gross et al. 18 |
| % Follow-up PRP | 34.8% | 314.26 | 109.46 | |
| No. of injections | 1.4 | 101.99 | 142.79 | |
| % Focal laser | 4.0% | 512.12 | 20.48 | |
| Subtotal | 1473.82 | |||
| 0.5-mg ranibizumab | 1.4 | 2114.06 | 2959.68 | No. of injections: Gross et al. 18 price: Hutton et al. 14 , adjusted to 2019 dollars |
| Total with ranibizumab | 4433.50 | |||
| Year one PDR per-patient complications cost (PRP arm) | Proportion (%) | Cost ($) | Per-patient cost ($) | Source |
| % Retinal detachment | 5.0 | 2556.44 | 127.82 | Gross et al. 18 |
| % Vitrectomy | 7.5 | 3715.83 | 278.69 | |
| % Endophthalmitis | 0.0 | 3240.00 | 0.00 | |
| % Cataract surgery | 3.0 | 3229.80 | 96.89 | |
| % Elevated IOP | 6.5 | 767.00 | 49.86 | |
| Total | 553.26 | |||
| Years two to five PDR annual per-patient treatment cost (PRP arm) | Number | Cost ($) | Per-patient cost ($) | Source |
| No. of visits per year | 3 | Expert opinion, more conservative than the number listed in Bressler et al. 22 | ||
| Dilated examination | 3 | 101.27 | 303.81 | |
| OCT | 3 | 41.81 | 125.43 | |
| % Follow-up PRP | 4.6 | 314.26 | 14.58 | Bressler et al. 22 |
| No. of injections | 1 | 101.99 | 101.99 | Gross et al. 18 |
| % Focal laser | 0.25 | 512.12 | 1.29 | |
| Subtotal | 547.10 | |||
| 0.5-mg ranibizumab | 1 | 2114.06 | 2114.06 | No. of injections: Gross et al. 18 price: Hutton et al. 14 , adjusted to 2019 dollars |
| Total | 2661.16 | |||
| Years two to five PDR annual per-patient complications cost (PRP arm) | Proportion (%) | Cost ($) | Per-patient cost ($) | Source |
| % Retinal detachment | 3.3 | 2556.44 | 84.36 | Bressler et al. 22 |
| % Vitrectomy | 2.9 | 3715.83 | 106.83 | |
| % Endophthalmitis | 0.0 | 3240.00 | 0.00 | |
| % Cataract surgery | 4.0 | 3229.80 | 129.19 | |
| % Elevated IOP | 2.9 | 767.00 | 22.05 | |
| Total | 342.44 | |||
| Year one PDR and DME treatment cost (ranibizumab arm) | Number | Cost ($) | Per-patient cost ($) | Source |
| No. of visits year one | 10 | Expert opinion, more conservative than the number listed in Gross et al. 18 | ||
| Dilated examination | 10 | 101.27 | 1012.70 | |
| OCT | 10 | 41.81 | 418.10 | |
| No. of initial PRP sessions | 1.5455 | 314.26 | 485.69 | Gross et al. 18 |
| % Follow-up PRP | 6.0 | 314.26 | 29.14 | |
| No. of injections | 8.9 | 101.99 | 907.71 | |
| % Focal laser | 9.5 | 512.12 | 48.65 | |
| Subtotal | 2901.99 | |||
| 0.5-mg ranibizumab | 8.9 | 2114.06 | 18 815.13 | No. of injections: Gross et al. 18 price: Hutton et al. 14 , adjusted to 2019 dollars |
| Total with ranibizumab | 21 717.13 | |||
| Year one PDR and DME complications cost (ranibizumab arm) | Proportion (%) | Cost ($) | Per-patient cost ($) | Source |
| % Retinal detachment | 3.0 | 2556.44 | 76.69 | Gross et al. 18 |
| % Vitrectomy | 2.0 | 3715.83 | 74.32 | |
| % Endophthalmitis | 3240.00 | 0.00 | ||
| % Cataract surgery | 1.0 | 3229.80 | 32.30 | |
| % Elevated IOP | 4.5 | 767.00 | 34.52 | |
| Total | 217.82 | |||
| Years two to five PDR and DME annual per-patient treatment cost (ranibizumab arm) | Number | Cost ($) | Per-patient cost | Source |
| No. of visits per year | 5 | Expert opinion, more conservative than the number listed in Bressler et al. 22 | ||
| Dilated examination | 5 | 101.27 | 506.35 | |
| OCT | 5 | 41.81 | 209.05 | |
| % Follow-up PRP | 2.0 | 314.26 | 6.29 | Bressler et al. 22 , expert opinion |
| No. of injections | 2.65 | 101.99 | 270.27 | Bressler et al. 22 |
| % Focal laser | 3.88 | 512.12 | 19.84 | Bressler et al. 22 |
| Subtotal | 1011.80 | |||
| 0.5-mg ranibizumab | 2.65 | 2114.06 | 5602.26 | No. of injections: Bressler et al. 22 price: Hutton et al. 14 , adjusted to 2019 dollars |
| Total | 6614.06 | |||
| Years two to five PDR and DME annual per-patient complications cost (ranibizumab arm) | Proportion (%) | Cost ($) | Per-patient cost ($) | Source |
| % Retinal detachment | 0.75 | 2556.44 | 19.17 | Bressler et al. 22 |
| % Vitrectomy | 2.3 | 3715.83 | 83.61 | |
| % Endophthalmitis | 0.0 | 3240.00 | 0.00 | |
| % Cataract surgery | 4.3 | 3229.80 | 137.27 | |
| % Elevated IOP | 2.88 | 767.00 | 22.05 | |
| Total | 262.10 |
DME, diabetic macular edema; IOP, intraocular pressure; OCT, optical coherence tomography; PDR, proliferative diabetic retinopathy; PRP, pan-retinal photocoagulation.
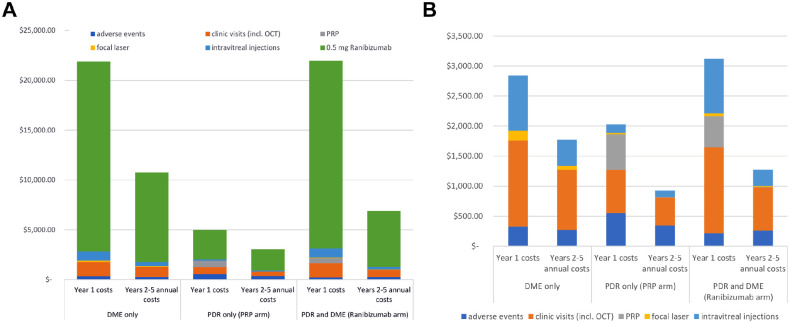
Costs and Other Data
Costs were drawn from Medicare 2019 allowable charges using current procedural terminology (CPT) codes and other cost estimates in the recently published literature, adjusted to reflect 2019 dollars.12-14,25 Per-patient treatment and complication costs for year one were as outlined in the respective studies for the relevant vtDR pathology. Annual per-patient treatment and complication costs for years two to five were modeled as the average for all treatments/complications reported between years two to five in the respective protocols for the patient’s corresponding retinopathy. These figures attempted to capture the overall cost from the payor’s perspective for the diagnosis and treatment of different vtDR states. In rare instances where the data were unclear, most notably regarding the number of annual visits to an ophthalmologist for vtDR treatment and monitoring (ie, the number of patient visits in DRCR Protocols I and S likely overestimate those of actual clinical practice), appeal to conservative expert opinion was made. All variables used in the model are listed in Tables 3 and 4.14,18-22,24,26,27 For disease that was below the threshold for treatment (severe NPDR without DME), we performed modeling based on an assumption that such patients would be examined three times per year. For treatable disease, three approaches were modeled: (1) DME in no DR or any nonproliferative DR was treated per the deferred laser arm of DRCR Protocol I; (2) PDR without DME was treated per the PRP arm of DRCR Protocol S; and (3) concurrent PDR and DME were treated per the ranibizumab arm of DRCR Protocol S (Table 2). Per-patient treatment and complication costs among the three treatment approaches were calculated for year one and years two to five (Figure 2A and B). Future outcomes were discounted at a future rate of 3% to reflect their present value.
Table 4.
List of Treatment and Complication Costs.
| Item | Cost ($) | Source |
|---|---|---|
| Dilated eye examination | 101.27 | 2019 Medicare CPT: 92004 and 92014 |
| Optical coherence tomography | 41.81 | 2019 Medicare CPT: 92134 |
| Intravitreal injection | 101.99 | 2019 Medicare CPT: 67028 |
| Focal laser | 512.12 | 2019 Medicare CPT: 67210 |
| Pan-retinal photocoagulation | 314.26 | 2019 Medicare CPT: 67228 |
| 0.5-mg ranibizumab medication | 2114.06 | Hutton et al. 14 |
| Retinal detachment repair | 2556.44 | |
| Vitrectomy | 3715.83 | |
| Endophthalmitis | 3240.00 | Schmier et al. 26 |
| Cataract extraction with intraocular lens placement | 3229.80 | Hutton et al. 14 |
| Elevated intraocular pressure | 767.00 | Li et al. 27 |
Note: Published costs before 2019 were adjusted to reflect 2019 US dollars.
CPT: current procedural terminology.
Figure 2.
Estimated per-patient costs by vtDR subtype during year one and years two to five. A, with or B, without medication costs included. Shown are adverse events costs (purple), clinic visit costs (orange), cost of pan-retinal photocoagulation (gray), cost of focal laser therapy (yellow), intravitreous injection procedure costs (light blue), and medication costs for 0.5-mg ranibizumab (green).
As ARIAS is primarily a secondary prevention strategy, all patients were modeled with good initial visual acuity of 20/30 or better in the better-seeing eye. SVL was defined as progression to visual acuity worse than 20/200 in the better-seeing eye, and rates of development of SVL in treated and untreated patients were based on the published literature as described above (Table 3).23,28
Primary and Secondary Outcome Measures
The primary outcome measure was the incremental cost-utility ratio (ICUR) of current screening practice compared with ARIAS screening, a value generally used to quantify the incremental cost associated with a one-unit increase in utility of one health intervention compared to another. 29 Using Markov modeling with microsimulation over a five-year period, the ICUR was determined by dividing the difference in average direct per-patient costs between the two screening strategies by the difference in mean health utility values between the strategies. For each of the two screening strategies, secondary outcome measures included the predicted proportion of patients with vtDR who were adherent with eye examination referral, and incident development of SVL after five years.
Health Economic Analysis
Health utility is a measure of quality of life with a time component that is ultimately totaled to calculate quality-adjusted life years (QALY). Utility values used in our model were obtained from previous studies converting visual acuity to QALY.12-14,28,30 When two sources reported different QALY approximations for the same visual acuity, the more conservative, that is, higher, utility value was chosen.28,30 For health utility changes associated with treatment by either ranibizumab and/or pan-retinal photocoagulation (PRP), we used utility values previously published (Table 5). 14
Table 5.
Utility Values for Vision States and Disease Treatments.
| State | Utility | Range tested | Source |
|---|---|---|---|
| Baseline | 0.87 | 0.8 to 1.0 | Brown et al. 30 |
| Severe vision loss | 0.66 | 0.5 to 0.77 | |
| Utility change, PRP treatment if no DME | −0.0075 | −0.2 to +0.2 | Hutton et al. 14 |
| Utility change, PRP treatment if DME | −0.019 | −0.2 to +0.2 | |
| Utility change, ranibizumab treatment if no DME | 0.0095 | −0.2 to +0.2) | |
| Utility change, ranibizumab treatment if DME | 0.0335 | −0.2 to +0.2 | |
| Death | 0 | N/A |
Note: Severe vision loss defined as VA 20/200 or worse in the better-seeing eye.
DME, diabetic macular edema; DR, diabetic retinopathy; PRP, pan-retinal photocoagulation.
As the primary care clinic at our institution serves approximately 3000 patients with diabetes each year, the relevant per-patient ARIAS screening costs were calculated using this number (Table 6). Published long-term outcome data from Protocols I and S extended to year five, allowing us to use these data in our five-year model.20,22 Furthermore, these data guided our analysis of the model using a two-stage Monte Carlo simulation consisting of 100 iterations of bootstrap sampling of 3000 individual patients modeled over five years, in each branch of the decision tree allowing a comparison of 3000 patients in the current practice branch to be compared with 3000 patients in the ARIAS branch. This resulted in a total of 600 000 simulated patient experiences (100 × 3000 × 2 decision tree branches). Treatment costs and utility for the two management strategies across each of the trials were summed to create means and SDs permitting calculation of the ICUR.
Table 6.
Estimated Per-Patient ARIAS Screening Costs.
| Value ($) | Per-patient cost ($) | Source | |
|---|---|---|---|
| CR-2 fundus photo camera | 16 000.00 | 5.33 | Internet search |
| Camera maintenance per year | 1000.00 | 0.33 | Expert opinion |
| Eyenuk annual software subscription | 5000.00 | 1.67 | Expert opinion |
| Staff labor to complete screening | 10.00 | 2019, “Patient care technician” (https://www.indeed.com/cmp/Barnes–jewish-Hospital/salaries) | |
| ARIAS Medicare reimbursement | 13.69 | 2019 Medicare CPT: 92228-TC | |
| Total | 31.02 |
Note: Per-patient cost based on 3000 patients screened per year.
ARIAS, Automated Retinal Image Analysis System; CPT, current procedural terminology.
Sensitivity Analyses
One-way sensitivity analyses were performed for key variables. Subsequently, the variables were substituted with distributions to facilitate probability sensitivity analyses. Use of distributions instead of variable point estimates allowed for exploration of variables that may be exerting excessive influence while accounting for changes in multiple variables (as compared with a one-way sensitivity analysis where all other variables remain constant). Variables were tested over a distribution range (Table 7). The willingness-to-pay, or the dollar amount that health care decision-makers would be willing to pay for a one-unit increase in effectiveness, was set at $100 000.13,14
Table 7.
Model Distributions and Range Tested.
| Variable | Point estimate | SD |
|---|---|---|
| Mean patient age | 57 | 5 |
| Baseline utility | 0.84 | 0.21 |
| SVL utility | 0.66 | 0.165 |
| Cost of 0.5-mg ranibizumab medication ($) | 2114.06 | 528.52 |
| Total cost for ARIAS screening ($) | 31.02 | 7.76 |
| Cost of DME treatment for year one ($) | 2512.59 | 628.15 |
| Cost of DME treatment for years two to five ($) | 1500.31 | 375.08 |
| Cost of DME complications for year one ($) | 328.58 | 82.14 |
| Cost of DME complications for years two to five ($) | 270.54 | 67.64 |
| Cost of eye exam (OCT + DFE) ($) | 143.08 | 35.77 |
| Cost of DME and PDR complications for year one ($) | 217.82 | 54.46 |
| Cost of DME and PDR complications for years two to five ($) | 262.10 | 65.52 |
| Cost of DME and PDR treatment for year one ($) | 2901.99 | 725.50 |
| Cost of DME and PDR treatment for years two to five ($) | 1011.80 | 252.95 |
| Cost of PDR only complications for year one ($) | 553.26 | 138.31 |
| Cost of PDR only complications for years two to five ($) | 342.44 | 85.61 |
| Cost of PDR only treatment for year one ($) | 1473.82 | 368.45 |
| Cost of PDR only treatment for years two to five ($) | 582.87 | 145.72 |
| Probability adherent, ARIAS (%) | 54.90 | 13.73 |
| Probability adherent, current practice (%) | 11.50 | 2.88 |
| Probability referred, ARIAS (%) | 50.80 | 12.70 |
| Probability vtDR, ARIAS (%) | 10.00 | 2.50 |
| Probability vtDR progress to SVL, non-adherent (%) | 7.40 | 1.85 |
| Probability vtDR, current practice (%) | 7.46 | 1.86 |
| Probability adherent patients develop SVL | 2.00 | 0.50 |
| Probability patient has DR after ARIAS screening (%) | 26.00 | 6.50 |
| Probability patient has DR among all patients in the current practice group (%) | 35.70 | 8.93 |
| Probability patient has NPDR with DME if they have vtDR | 5.96 | 1.49 |
| Probability patient has DME only if screen positive for vtDR (%) | 5.82 | 1.46 |
| Probability patient has PDR only if they have vtDR (%) | 2.07 | 0.52 |
| Probability patient has PDR with DME if they have vtDR (%) | 0.56 | 0.14 |
ARIAS, Automated Retinal Image Analysis System; DFE, dilated fundus examination; DME, diabetic macular edema; DR, diabetic retinopathy; NPDR, nonproliferative DR; OCT, optical coherence tomography; PDR, proliferative DR; SVL, severe vision loss; vtDR, vision-threatening DR.
Statistical Software
Modeling was performed using TreeAge Pro software (TreeAge Pro 2019, R1. TreeAge Software, Williamstown, MA, USA) using methods similar to those in previously published cost-effectiveness literature.12-14 Additional statistical analysis was performed using STATA/IC software version 14.2 (StataCorp LP, College Station, TX, USA) with alpha set at 0.05.
Results
Main Outcome Measures
We determined the absolute and incremental costs and utility between the current practice and ARIAS groups (Table 8). At five years, current practice showed comparable utility as ARIAS, but at a much greater cost. We calculated a 23.3% reduction in cost in the ARIAS group compared with standard practice (P < .001). Comparing current practice to ARIAS screening, we computed an ICUR of $258 721.81.
Table 8.
Cost-effectiveness Comparison of ARIAS Versus the Current Practice.
| Group | Cost, 2019 US$ | Utility, QALYs | Cost utility ratio | Incremental cost ($) | Incremental utility | ICUR ($/QALY) |
|---|---|---|---|---|---|---|
| ARIAS | 1596.99 | 4.942 | 323.1 | |||
| Current practice | 2082.91 | 4.944 | 421.3 | 485.92 | 0.00188 | 258 721.81 |
| Statistical testing using Monte Carlo simulation (1000 samples) | ||||||
| Variable | Current practice | ARIAS | Percentage of increase or decrease | P value | ||
| Cost ($) | 2082.91 | 1596.99 | 23.3 | <.001 | ||
| Cost SD ($) | 583.90 | 526.31 | ||||
| Effect | 4.944 | 4.942 | 0.04 | .989 | ||
| Effect SD | 1.017 | 1.023 | ||||
ARIAS, Automated Retinal Image Analysis System; ICUR, incremental cost-utility ratio; QALYs, quality-adjusted life years.
Sensitivity Analysis
In one-way sensitivity analysis, the cost-effectiveness of ARIAS was robust across a wide range of variability in individual model inputs (Table 9). The model favored ARIAS until the price of 0.5-mg ranibizumab fell below $80.26 (not including the cost of the injection procedure). Additionally, ARIAS was cost-effective up to a combined cost of ARIAS screening of $161.14 per screening and up to the standard of care eye examination adherence rate of 71.5%. The full list of the nine variables that had a threshold value leading to a reversal of the cost-effectiveness analysis from favoring ARIAS to favoring current practice, in addition to select variables that notably did not have a threshold value, are included in Table 9. All other variables not included in Table 9 had no significant effects on cost-effectiveness.
Table 9.
One-way Sensitivity Threshold Testing with Notable Variables without Threshold Values.
| Variable | Modeled point estimate | Sensitivity threshold value (favors ARIAS up to [or down to]) |
|---|---|---|
| Baseline utility | 0.88 | 0.68 |
| Utility after development of SVL | 0.60 | 0.816 |
| Cost of ARIAS screening (camera, maintenance, labor, software) ($) | 31.02 | 161.14 |
| Ranibizumab per-injection medication cost ($) | 2114.06 | 80.26 |
| Probability referred after ARIAS screening (%) | 50.8 | 69.8 |
| Probability adherent in the current practice group (%) | 11.50 | 71.5 |
| Probability of having vtDR after a positive ARIAS screening (%) | 10.0 | 17.3 |
| Probability of progressing to SVL among non-adherent patients (%) | 7.4 | 3.0 |
| Probability of vtDR in the current practice group (%) | 7.5 | 3.2 |
| Notable variables that do not alter model favorability of ARIAS | ||
| Cost of treatment for DME only (year one or years two to five) ($) | 2512.59 | N/A |
| Cost of treatment for PDR with DME (year one or years two to five) ($) | 2416.30 | N/A |
| Cost of treatment for PDR without DME (year one or years two to five) ($) | 1473.82 | N/A |
| Cost of eye examination ($) | 143.08 | N/A |
| Probability of having vtDR at baseline in the refer everyone group | 7.46 | N/A |
| Probability adherent in the ARIAS group (%) | 54.9 | N/A |
| Probability of progressing to SVL among adherent patients (%) | 2.0 | N/A |
ARIAS, Automated Retinal Image Analysis System; DME, diabetic macular edema; DR, diabetic retinopathy; NPDR, nonproliferative DR; PDR, proliferative DR; SVL, severe vision loss; vtDR, vision-threatening DR.
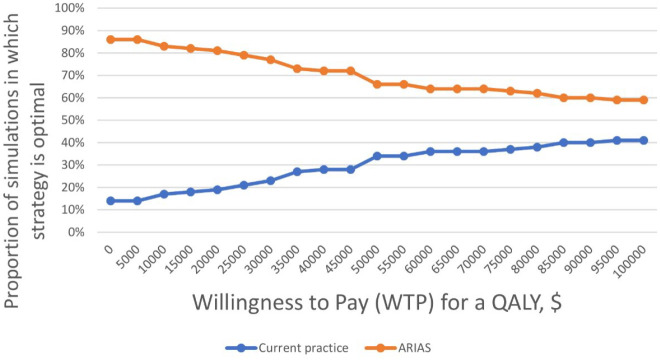
Following one-way sensitivity testing, each variable was converted from a point estimate to a distribution in the Markov model. This permitted probabilistic sensitivity analysis which identified the proportion of iterations favoring ARIAS versus standard of care at varying willingness to pay thresholds. As illustrated in Figure 3, at a willingness to pay of $50 000, the model favored ARIAS in 66% of samples, whereas at a willingness to pay of $100 000, the model favored ARIAS in 59% of instances.
Figure 3.
Cost-effectiveness acceptability curve. Acceptability curve for DR screening using ARIAS in a primary care setting (orange line) compared against rates for the standard of care, in which all individuals with diabetes are referred for dilated retinal examination (blue line). ARIAS, Automated Retinal Image Analysis System; DR, diabetic retinopathy.
Similar to findings in other cost-effectiveness studies, the per-patient price of 0.5-mg ranibizumab accounts for the greatest proportion of the annual cost for any vtDR (Figure 2A). 13 As illustrated in Figure 2B with the medication cost of 0.5-mg ranibizumab removed, the second largest per-patient cost was the expense of ongoing clinic visits (eye examination with optical coherence tomography).
Secondary Outcome Measures
Compared with current practice, our five-year decision tree simulation showed that implementation of ARIAS increased the proportion of all patients with vtDR who were adherent with eye examination referral from 33.8% in the reference group to 59.4% in the ARIAS group. In this model, ARIAS also decreased the incidence of SVL from 3.1% to 1.1% (Table 10). These proportions were calculated from the decision tree in a deterministic fashion, precluding the use of “random walk” simulations, as we performed for primary outcome measures. Subsequently, we could not conduct statistical testing or sensitivity analyses to further analyze these estimates.
Table 10.
Secondary Outcomes of ARIAS Implementation after Five Years.
| Current practice | ARIAS | Percentage of increase or decrease | |
|---|---|---|---|
| Percentage of all vtDR patients adherent | 33.8 | 59.4 | 75.7 |
| Percentage of patients who develop SVL | 3.1 | 1.1 | 64.4 |
ARIAS, Automated Retinal Image Analysis System; SVL, severe vision loss; vtDR, vision-threatening diabetic retinopathy.
Discussion
Five-year economic modeling based on our preliminary data of low-income patients with diabetes suggests that primary care-based ARIAS implementation for DR screening is cost-effective. The calculated ICUR of $258 721.81 comparing the current practice to ARIAS screening is well beyond the willingness-to-pay threshold of $100 000.13,14 ARIAS screening is not associated with greater short-term utility but is substantially less expensive than our institution’s historical practice of referring all patients with diabetes for annual for an in-office screening eye examinations (Table 8). The cost-effectiveness of ARIAS likely derives from the reduction in unnecessary referrals in patients without evidence of DR, the increase in adherence to follow-up ophthalmic care recommendations in patients who have evidence of vtDR as determined by ARIAS technology, and subsequent reduction in incident SVL due to identification and treatment of vtDR (Table 10). Future studies should explore the long-term costs and benefits of ARIAS implementation among low-income primary care patients with diabetes.
While ARIAS screening demonstrated its cost-effectiveness primarily by its reductions in costs, five-year QALY gains were comparable in both the ARIAS and current practice groups. This may be due to the short time frame of our economic modeling as well as the fact that there were relatively few incident cases of SVL in either screening arm (Table 10). Another finding worth greater exploration is that one-way sensitivity analysis demonstrated a change in the cost-effectiveness model once the per-injection medication price of ranibizumab dropped below $80.26 (Table 9). As a one-way sensitivity testing result, it is limited by the fact that all other model variables are held constant. However, it is substantially below the value tested using a distribution wherein the 0.5-mg ranibizumab price was modeled at $2114.06 with an SD of $528.51 (Table 7); if the price of ranibizumab changes dramatically in the United States, repeat modeling with variable distributions and probability sensitivity analyses may be necessary.
This study is limited by the fact that our model analyzes cost-effectiveness over a relatively short time period, a time period chosen primarily due to the follow-up data available via the Protocol I and S studies tracking vtDR treatment and complication rates and visual acuity outcomes. Longer-term studies should be conducted to evaluate differences in cost or QALY. Second, because our modeled treatment relied on the Protocol I and S study results, any limitations in these studies could affect our results as well. This includes evaluating the cost-effectiveness of DR treatment using 0.5-mg ranibizumab, as an economic analysis, including 0.3-mg ranibizumab, aflibercept, or bevacizumab may yield different results, as discussed above. As for why our model used 0.5-mg ranibizumab for modeling purposes, there were several reasons: treating DME with bevacizumab is still off-label, using 0.5-mg ranibizumab for DR treatment cost-effectiveness modeling is commonplace in the published literature,12-14 and in real-life clinical practice, there is still significant use of ranibizumab/aflibercept as first-line treatment for DME, especially for patients with moderate vision loss from DME at baseline (<20/50).31,32 These considerations were the driving factors for our decision to use 0.5-mg ranibizumab as the standard-of-care treatment for patients with DME in our economic model, as it was the modeled treatment paradigm most valid for current recommended practices across all organizations.
A further limitation of our study includes converting visual acuity to QALY figures–QALYis an imperfect measure of a patient’s quality of life. Nevertheless, it is well established in the health economics literature and does provide for a means of comparing competing management strategies of varying costs. As our model was built on the local data obtained from prospective analysis of ARIAS implementation, 15 any limitations to that study, including confounding factors that influenced patient adherence differently between the ARIAS and current practice groups, could impact our cost-effectiveness outcomes as well. However, as detailed in that study, although small demographic differences between the pre-ARIAS and post-ARIAS cohorts were found, it was the post-ARIAS group that had features traditionally associated with nonadherence to medical advice (ie, higher glycated hemoglobin index). Lastly, our model only included direct costs of screening and treatment from the payor’s perspective and did not account for indirect costs to patients such as missed work for appointments or transportation costs—costs that would have likely made ARIAS even more cost-effective, especially among low-income patients that are particularly impacted by cost and transportation barriers.
The cost-effectiveness of telemedicine-based digital retinal imaging (TMDRI) systems, which are distinguished from ARIAS by the involvement of human graders, is well established despite their poor uptake in the United States health care system at large. 33 Current estimates suggest that between 80% and 85% of ophthalmology practices in the United States do not currently employ any form of teleophthalmology or automated retinal screening systems. 34 The lack of such systems exposed weaknesses in health care systems brought on by stressors such as the ongoing COVID-19 pandemic. As all fields in medicine move toward methods to reduce patient risk to nosocomial disease, TMDRI or ARIAS systems offer highly effective and cost-saving methods of screening, as indicated by the results of our analyses and many others. Although assessment of the relative cost-effectiveness of TMDRI and ARIAS is beyond the scope of the current study, such a comparison could be important for many health systems that are currently not employing such screening tools.
A final important point is that the analysis in our study took into consideration screening for DR only, not several other ocular comorbidities for which low-income patients are at high risk. Although EyeArt 2.0 can potentially flag ocular abnormalities such as visually significant cataracts or retinal detachments, 15 the software was designed for the singular purpose of detecting DR. A limitation to our analysis is that the impact of missed screening for ocular comorbidities, such as glaucoma, in patients with diabetes was not taken into consideration. Indeed, this concern points to the potential dangers of allowing an AI platform to “clear” patients from annual dilated ophthalmic examinations by a trained human. However, as noted in numerous epidemiologic studies, many—if not most—patients with diabetes do not currently follow guidelines for annual screening examinations. Such adherence rates can be as low as 10%-30% in especially vulnerable populations.4,35 ARIAS, as a point-of-care test, effectively removes a major barrier for achieving eye care screening adherence, namely, the burden of an additional medical visit in a population that heavily skews toward being low-income and actively employed and in which time away from work demands can be difficult to arrange. Moreover, the algorithms driving ARIAS screening are already being modified to allow for the detection of many ocular conditions, including optic disc edema, glaucoma, and macular degeneration.36-38 Therefore, we anticipate that AI-based screening will not only improve eye screening in populations that typically do not seek eye care but also eventually provide comprehensive screening for many common causes of blindness.
Conclusion
When modeled over five years, primary care-based ARIAS screening among low-income patients with diabetes is substantially less costly and equally as effective as the more traditional practice of referring all patients for annual dilated eye examination. The cost-effectiveness of ARIAS may result from the reduction in unnecessary referrals for annual dilated eye examination, increased rates of adherence to follow-up ophthalmic care recommendations among patients with evidence of vtDR, and the resulting reduction in incident development of SVL. These findings provide support for the financial viability and sustainable use of ARIAS screening systems in the primary care setting.
Footnotes
Abbreviations: ARIAS, automated retinal image analysis system; CPT, current procedural terminology; DME, diabetic macular edema; DR, diabetic retinopathy; DRCR, Diabetic Retinopathy Clinical Research Network; ICUR, incremental cost-utility ratio; NPDR, non-proliferative diabetic retinopathy; PRP, panretinal photocoagulation; PDR, proliferative diabetic retinopathy; QALY, quality-adjusted life years; SVL, severe vision loss; vtDR, vision threatening diabetic retinopathy.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: the screening software described in this study was provided by Eyenuk, Inc. Additional funding was provided to Dr. Rajagopal by a Research to Prevent Blindness Career Development Award, and to Dr. Fuller by the Mentors in Medicine Program, Department of Medicine at Washington University School of Medicine in St. Louis.
ORCID iDs: Spencer D. Fuller  https://orcid.org/0000-0001-9371-1140
https://orcid.org/0000-0001-9371-1140
Martin Gregory  https://orcid.org/0000-0002-6656-9828
https://orcid.org/0000-0002-6656-9828
Jessica Kuo  https://orcid.org/0000-0003-3591-442X
https://orcid.org/0000-0003-3591-442X
References
- 1. Wong TY, Sun J, Kawasaki R, et al. Guidelines on diabetic eye care: the international council of ophthalmology recommendations for screening, follow-up, referral, and treatment based on resource settings. Ophthalmology. 2018;125(10):1608-1622. [DOI] [PubMed] [Google Scholar]
- 2. Sabanayagam C, Yip W, Ting DSW, Tan G, Wong TY. Ten emerging trends in the epidemiology of diabetic retinopathy. Ophthalmic Epidemiol. 2016;23(4):209-222. [DOI] [PubMed] [Google Scholar]
- 3. Klein R, Klein BEK. Screening for diabetic retinopathy, revisited. Am J Ophthalmol. 2002;134(2):261-263. [DOI] [PubMed] [Google Scholar]
- 4. Daskivich LP, Vasquez C, Martinez C, Tseng C-H, Mangione CM. Implementation and evaluation of a large-scale teleretinal diabetic retinopathy screening program in the Los Angeles County Department of Health Services. JAMA Intern Med. 2017;177(5):642-649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tufail A, Rudisill C, Egan C, et al. Automated diabetic retinopathy image assessment software: diagnostic accuracy and cost-effectiveness compared with human graders. Ophthalmology. 2017;124(3):343-351. [DOI] [PubMed] [Google Scholar]
- 6. Soto-Pedre E, Navea A, Millan S, et al. Evaluation of automated image analysis software for the detection of diabetic retinopathy to reduce the ophthalmologists’ workload. Acta Ophthalmol (Copenh). 2015;93(1):e52-e56. [DOI] [PubMed] [Google Scholar]
- 7. Welikala RA, Fraz MM, Foster PJ, et al. Automated retinal image quality assessment on the UK Biobank dataset for epidemiological studies. Comput Biol Med. 2016;71:67-76. [DOI] [PubMed] [Google Scholar]
- 8. Ting DSW, Cheung CY-L, Lim G, et al. Development and validation of a deep learning system for diabetic retinopathy and related eye diseases using retinal images from multiethnic populations with diabetes. JAMA. 2017;318(22):2211-2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nielsen KB, Lautrup ML, Andersen JKH, Savarimuthu TR, Grauslund J. Deep learning–based algorithms in screening of diabetic retinopathy: a systematic review of diagnostic performance [published online ahead of print November 3, 2018]. Ophthalmol Retina. doi: 10.1016/j.oret.2018.10.014 [DOI] [PubMed] [Google Scholar]
- 10. IDx. Homepage. Available at: https://www.eyediagnosis.net/. Accessed November 21, 2019.
- 11. Bhaskaranand M, Ramachandra C, Bhat S, et al. Automated diabetic retinopathy screening and monitoring using retinal fundus image analysis. J Diabetes Sci Technol. 2016;10(2):254-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dewan V, Lambert D, Edler J, Kymes S, Apte RS. Cost-effectiveness analysis of ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2012;119(8):1679-1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ross EL, Hutton DW, Stein JD, Bressler NM, Jampol LM, Glassman AR. Cost-effectiveness of aflibercept, bevacizumab, and ranibizumab for diabetic macular edema treatment: analysis From the Diabetic Retinopathy Clinical Research Network comparative effectiveness trial. JAMA Ophthalmol. 2016;134(8):888-896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hutton DW, Stein JD, Bressler NM, Jampol LM, Browning D, Glassman AR. Cost-effectiveness of intravitreous ranibizumab compared with panretinal photocoagulation for proliferative diabetic retinopathy: secondary analysis from a diabetic retinopathy clinical research network randomized clinical trial. JAMA Ophthalmol. 2017;135(6):576-584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liu J, Gibson E, Ramchal S, Shankar V, Rajagopal R. Diabetic retinopathy screening in a primary care clinic with automated retinal image analysis improves adherence to follow-up ophthalmic care [published online ahead of print June 2020]. Ophthalmol Retina. doi: 10.1016/j.oret.2020.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Varma R, Bressler NM, Doan QV, et al. Prevalence of and risk factors for diabetic macular edema in the United States. JAMA Ophthalmol. 2014;132(11):1334-1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zhang X, Saaddine JB, Chou C-F, et al. Prevalence of diabetic retinopathy in the United States, 2005-2008. JAMA. 2010;304(6):649-656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gross JG, Glassman AR, Jampol LM, et al. Panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA. 2015;314(20):2137-2146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Elman MJ, Aiello LP, Beck RW, et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010;117(6):1064-1077.e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gross JG, Glassman AR, Liu D, et al. Five-year outcomes of panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA Ophthalmol. 2018;136(10):1138-1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Elman MJ, Bressler NM, Qin H, et al. Expanded 2-year follow-up of ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2011;118(4):609-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bressler SB, Glassman AR, Almukhtar T, et al. Five-year outcomes of ranibizumab with prompt or deferred laser versus laser or triamcinolone plus deferred ranibizumab for diabetic macular edema. Am J Ophthalmol. 2016;164:57-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wong TY, Mwamburi M, Klein R, et al. Rates of progression in diabetic retinopathy during different time periods: a systematic review and meta-analysis. Diabetes Care. 2009;32(12):2307-2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Qin H. Intravitreal ranibizumab for diabetic macular edema with prompt vs deferred laser treatment: 3-year randomized trial results. Ophthalmology. 2012;119(11):2312-2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Medicare Coverage Download Database. https://www.cms.gov/medicare-coverage-database/downloads/downloadable-databases.aspx. Accessed October 17, 2019.
- 26. Schmier JK, Hulme-Lowe CK, Covert DW, Lau EC. An updated estimate of costs of endophthalmitis following cataract surgery among Medicare patients: 2010-2014. Clin Ophthalmol Auckl NZ. 2016;10:2121-2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Li EY, Tham CC, Chi SC, Lam DS. Cost-effectiveness of treating normal tension glaucoma. Invest Ophthalmol Vis Sci. 2013;54(5):3394-3399. [DOI] [PubMed] [Google Scholar]
- 28. Sharma S, Brown GC, Brown MM, Hollands H, Shah GK. The cost-effectiveness of photodynamic therapy for fellow eyes with subfoveal choroidal neovascularization secondary to age-related macular degeneration. Ophthalmology. 2001;108(11):2051-2059. [DOI] [PubMed] [Google Scholar]
- 29. Detsky AS. A clinician’s guide to cost-effectiveness analysis. Ann Intern Med. 1990;113(2):147. [DOI] [PubMed] [Google Scholar]
- 30. Brown MM, Brown GC, Sharma S, Landy J. Health care economic analyses and value-based medicine. Surv Ophthalmol. 2003;48(2):204-223. [DOI] [PubMed] [Google Scholar]
- 31. Wells JA, Glassman AR, Ayala AR, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema: two-year results from a comparative effectiveness randomized clinical trial. Ophthalmology. 2016;123(6):1351-1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Baker CW, Glassman AR, Beaulieu WT, et al. Effect of initial management with aflibercept vs laser photocoagulation vs observation on vision loss among patients with diabetic macular edema involving the center of the macula and good visual acuity: a randomized clinical trial. JAMA. 2019;321(19):1880-1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Whited JD, Datta SK, Aiello LM, et al. A modeled economic analysis of a digital teleophthalmology system as used by three federal healthcare agencies for detecting proliferative diabetic retinopathy. Telemed E-Health. 2005;11(6):641-651. [DOI] [PubMed] [Google Scholar]
- 34. Starr MR, Israilevich R, Zhitnitsky M, et al. Practice patterns and responsiveness to simulated common ocular complaints among US ophthalmology centers during the COVID-19 pandemic. JAMA Ophthalmol. 2020;138(9):981-988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kuo J, Liu J, Gibson E, et al. Factors associated with adherence to screening guidelines for diabetic retinopathy among low-income metropolitan patients. Mo Med. 2020;117(3):258-264. [PMC free article] [PubMed] [Google Scholar]
- 36. Milea D, Najjar RP, Jiang Z, et al. Artificial intelligence to detect papilledema from ocular fundus photographs. N Engl J Med. 2020;382(18):1687-1695. [DOI] [PubMed] [Google Scholar]
- 37. Zheng C, Johnson TV, Garg A, Boland MV. Artificial intelligence in glaucoma. Curr Opin Ophthalmol. 2019;30(2):97-103. [DOI] [PubMed] [Google Scholar]
- 38. Pead E, Megaw R, Cameron J, et al. Automated detection of age-related macular degeneration in color fundus photography: a systematic review. Surv Ophthalmol. 2019;64(4):498-511. [DOI] [PMC free article] [PubMed] [Google Scholar]