Abstract
Background:
Currently, evidence-based learning systems to increase knowledge and evidence level of wound care are unavailable to wound care nurses in Denmark, which means that they need to learn about diabetic foot ulcers from experience and peer-to-peer training, or by asking experienced colleagues. Interactive evidence-based learning systems built on case-based reasoning (CBR) have the potential to increase wound care nurses’ diabetic foot ulcer knowledge and evidence levels.
Method:
A prototype of a CBR-interactive, evidence-based algorithm-operated learning system calculates a dissimilarity score (DS) that gives a quantitative measure of similarity between a new case and cases stored in a case base in relation to six variables: necrosis, wound size, granulation, fibrin, dry skin, and age. Based on the DS, cases are selected by matching the six variables with the best predictive power and by weighing the impact of each variable according to its contribution to the prediction. The cases are ranked, and the six cases with the lowest DS are visualized in the system.
Results:
Conventional education, that is, evidence-based learning material such as books and lectures, may be less motivating and pedagogical than peer-to-peer training, which is, however, often less evidence-based. The CBR interactive learning systems presented in this study may bridge the two approaches. Showing wound care nurses how individual variables affect outcomes may help them achieve greater insights into pathophysiological processes.
Conclusion:
A prototype of a CBR-interactive, evidence-based learning system that is centered on diabetic foot ulcers and related treatments bridges the gap between traditional evidence-based learning and more motivating and interactive learning approaches.
Keywords: case-based reasoning, diabetic foot ulcers, wound care nurses, dissimilarity score, variables, education, knowledge level, evidence, interactive learning system
Introduction
Diabetic foot ulcers are a late diabetic complication that often leads to amputations such as minor lower-extremity amputation, for example, of a toe, and/or major lower-extremity amputation, for example, of a limb.1-3 Approximately one quarter of diabetic foot ulcers end in amputations. 3 If wound care nurses’ diabetic foot ulcer knowledge and evidence level increased, some of these amputations might be possible to avoid or at least postpone.4-6 Ideally, providing wound care to diabetic foot ulcers should be a multidisciplinary task, which should involve, for example, podiatrists, endocrinologists, vascular and orthopedic surgeons, microbiologists, and specialized nurses. In Denmark, however, the majority of the diabetic foot ulcer care is provided by community nurses with specialization within wounds. 7 Currently, evidence-based learning systems used to increase wound care nurses’ knowledge and evidence level are not available. Therefore, wound care nurses need to learn about diabetic foot ulcers and related treatments from experience and peer-to-peer training, or by asking experienced colleagues.8,9 Unfortunately, this means that wound care nurses as a group may hold on to inexpedient habits and practices instead of increasing their knowledge and evidence level.4,10
Building a meaningful learning system based on evidence requires good quality evidence. Systematic reviews of randomized controlled trials conclude that studies comparing different diabetic foot ulcer treatments have low evidence levels.11-19 Therefore, this type of study cannot be used to draw conclusions or make summaries that can be implemented into future learning systems. Even though they rank lower in the evidence hierarchy, 20 retrospective cohort study designs may pose another means of generating evidence. A newly published retrospective cohort study showed how variables in the form of on-site wound characteristics or easily accessible information collected during wound care consultations are highly informative when it comes to predicting whether a diabetic foot ulcer will heal or not. 21 The data and principles used in that study could provide the basis of an evidence-based learning system.
Case-based reasoning (CBR) is a well-established artificial intelligence technique that has been practiced in different scientific areas, not only as a problem-solving methodology but also as a learning methodology.22,23 It is an intuitive, transparent, and relevant technique when previously successful solutions have been recorded, as is the case in the healthcare sector. The overall idea behind CBR is to apply experience and knowledge from previously solved cases to solve new problems. A case refers to a problematic situation. In classic CBR, the system, when confronted with a new case, retrieves a set of similar cases, reuses previous solutions to the problem by revising them in the context of the current case, before retaining the “solved” case for future use in the CBR system.24,25 One domain where the CBR methodology has been particularly appropriate is within the medical domain.26,27 Overviews show that in the medical domain, CBR has been applied to psychiatry, oncology, audiology, intensive care, heart failure treatments, dyspnea management, hypertension treatment, and diabetes management.28,29 Most CBR systems have been applied to classification and treatment choice such as diagnosis and decision support systems, others have been used as planning systems, and a few have been used as tutoring or learning systems.26,28-30 The aim of this study was to use the CBR methodology and CBR data as well as principles from the retrospective cohort study 21 to build a prototype of an interactive pedagogical tool for evidence-based diabetic foot ulcer care for nurses.
Case-Based Reasoning System
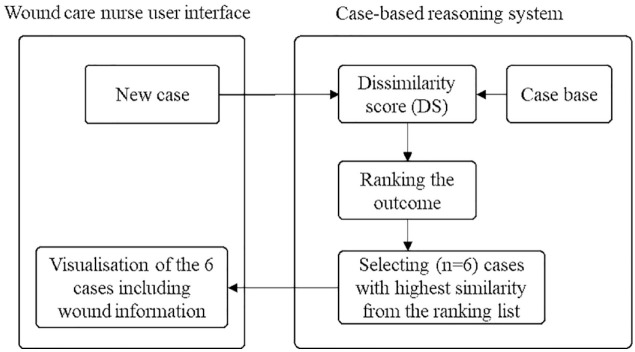
When operating the prototype of the CBR interactive, evidence-based learning system, the wound care nurse starts by entering characteristics of a new case whereupon the system provides him or her with a selection of six cases similar to the new case. For each of the selected cases, the wound care nurse will get access to one or more images of the foot ulcer, the quantitative characteristics of the foot ulcer, how the foot ulcer was treated, and information regarding whether the foot ulcer healed. Figure 1 outlines the architecture of the prototype of the pedagogical tool for evidence-based diabetic foot ulcer care for nurses.
Figure 1.
Outline of the CBR-interactive, evidence-based learning system.
The prototype of the CBR interactive learning system operates by an algorithm that calculates a dissimilarity score (DS) giving a quantitative measure of the similarity between the new case and each of the cases stored in a prototype case base with respect to the six variables necrosis, wound size, granulation, fibrin, dry skin, and age. A DS of zero corresponds to no dissimilarity, that is, complete similarity. Based on the DS, the cases are organized and ranked, and the six cases with the lowest DS are selected. It should be noted that the six selected variables are those shown to be the best outcome predictors of a given treatment. 21 In other words, if the purpose, for example, had been to find visually similar cases, other variables would probably have been selected.
The case-based reasoning system is operated in three phases: (i) the case base is built; (ii) cases are retrieved from the case base, and (iii) each new case is retained by adding it to the case base as described in more detail below.
Case Base Building
Six variables were included in the study as depicted in Table 1, which also reports the log odds ratios (β), coefficients from a logistic regression model as reported in a previous study. 21 The evidence for choosing these six variables (Table 1) has been published in a study by Bender et al. 21 The study by Bender et al. showed that the combination of these predictor variables lead to an area under the curve of 0.77.
Table 1.
Variables Included in The Learning System. Variable = Name of the Predictor Variable; Type = Variable’s Type; Values = Values that each Variable May Assume; Log Odds Ratio (β). A Change in a Variable by One Unit (Or, in Case of Nominal Variables, a Change from “No” to “Yes”) Increases the Log Odds Ratio by the Value of the Corresponding Weight, β. 21
| Variable | Type | Values | Log odds ratio (β) |
|---|---|---|---|
| Necrosis | Nominal | [yes, no] | −1,4286 |
| Wound size (cm2) | Continuous | (0,+∞ ) | 0.0294 |
| Granulation | Nominal | [yes, no] | 0.1789 |
| Fibrin | Nominal | [yes, no] | −0.7640 |
| Dry skin | Nominal | [yes, no] | −0.7041 |
| Age (years) | Integer | (0,+∞ ) | −0.0464 |
In the prototype version of the system, the case base contained a fixed number of diabetic foot ulcer cases (N = 162), where a case refers to the quantitative characteristics of treatments and outcome (healed/not healed) of a specific diabetic foot ulcer. The cases were selected from a larger database using the inclusion criteria: observation period between 14 and 30 days, minimum wound size corresponding to 0.5 m2, and at least two registrations of the wound size, as described in a previous study. 21 The data comes from a Danish database, named Pleje.net. Wound care community nurses working in the home nursing care, who treat chronic ulcers in the patients’ homes, including diabetic foot ulcers, enter this data. This information is validated by wound specialists working at Danish hospitals specialized in diabetic foot ulcers. Most conventional facilities probably do not practice evidence based methodology. The wound care specialist validation in Pleje.net is evidence-based, which means that the database has a high validity when using it in case-based learning. A more detailed description of the selection process and its rationale can be found in Bender et al. 21
Case Retrieval
In order to retrieve cases, the prototype of the CBR-interactive, evidence-based learning system assessed the similarity of a new case with respect to all cases from the case base. For each of the cases in the case base, B, the DS was calculated using the equation:
where N are the coefficients (observed values) of the new case, Bj are the coefficients (observed values) of the jth entry in the case base, and βi is the log odds ratio corresponding to the ith variable (Table 1). Based on the DS, cases are ranked, and the six cases with the lowest DS are selected for visualization. It should be noted that by using this DS, cases are selected not only by matching the six variables with the best predictive power, but also by weighing the impact of each variable according to its contribution to the prediction.
Wound Care Nurse User Interface
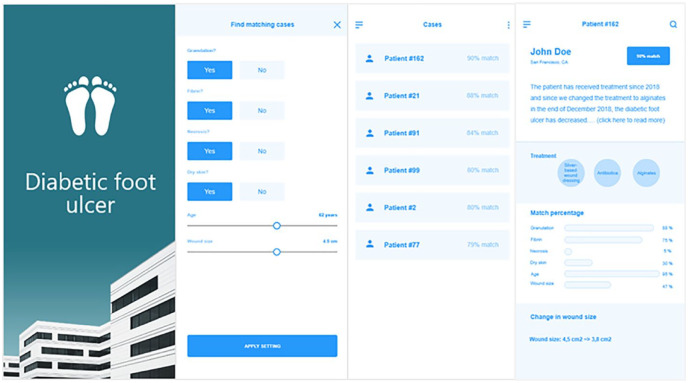
The interface of the prototype of the interactive pedagogical nurse tool prototype is illustrated in Figures 2a–2d. When tapping the icon for the case-based reasoning tool in the patient record system running on the nurse’s mobile phone, the start page is shown for a second or two, as shown in Figure 2a.
Figure 2.
(Consists of four sub-figures, 2a–2d). A visualization of the prototype system.
In the prototype system, the first step for the wound care nurse involves entering the characteristics of the diabetic foot ulcer, as illustrated in Figure 2b (information on age is retrieved from the patient health record, but it can be changed manually by the nurse). The wound care nurse enters information on the six characteristics: granulation, fibrin, necrosis, dry skin, age, and wound size. The first four binary characteristics are answered by tapping ‘yes’ or ‘no’. The last two continuous characteristics, age, and wound size, are answered using an adjustment bar. When all six characteristics are entered, the wound care nurses can press “apply settings”.
After entering the wound characteristics, the six best matching cases are listed, as illustrated in Figure 2c. The list contains the patient identification number, as used in the case base, and the match between the listed cases and the new case. Since the DS used in the case-based reasoning system may be hard for some nurses to interpret, the score is converted into a match percentage, calculated by the following formula:
After tapping one of the cases in the list, the details for this case are shown, as illustrated in Figure 2d. From top to bottom, the following information is given: (1) A short description of the patient and/or other relevant information regarding the patient is outlined and the match percentage is shown. For example, for patient#162, John Doe, there is a 90% match. (2) A bar chart showing the match of each of the six variables multiplied by the corresponding weighing. In this case, there is a match for variables 1, 2, 4, 5 and 6, but no match for variable 3. (3) An overview of the treatment for this patient. (4) An overview of the treatment outcome measured by change in wound size. When having questions, for example regarding why one of the matching patients in the CBR-prototype system has been chosen for comparison with the current patient, the nurse can enter an interactive chat function by double tapping the relevant matching patient and thereby get in contact with the hospital-based wound specialists. After having selected the matching patient in question, the nurse can, if it is more convenient, phone the hospital-based wound specialists as he or she is used to when having questions to the treatment of a specific patient.
Discussion
CBR has been used in several studies centered on diabetes management for purposes such as supporting physicians in providing appropriate treatment for maintaining blood glucose control, supporting patient education, and for insulin pump therapy and other types of diabetes management.31-36 To our knowledge, none of these studies have focused on diabetic foot ulcers. In our study, a pedagogical prototype tool for nurses has been presented with the aim of increasing wound care nurses’ diabetic foot ulcer knowledge and evidence level.
In a study by Marling et al., a case-based decision support system to assist patients with Type 1 diabetes in handling insulin pump therapy was developed. 34 Even though this system was oriented toward insulin pump therapy and designed to support patients, whereas the present system focuses on diabetic foot ulcers supporting wound care nurses, the two systems do share several similarities. In the study by Marling et al., 18 variables were selected among 140 different variables as the most relevant. 34 In the present study, six variables were selected among the 60 variables available. 21 In both studies, health professionals collected data as part of their daily routine with patients. Both studies compared cases using similarity calculus: Marling et al. used a nearest neighbor approach, whereas the present study used a dissimilarity score based on logistic regression coefficients. It should be noted that several similarity calculus methods are reported in the literature: rule-based reasoning, neural network, fuzzy logic, Euclidian distance, similarity function, genetic algorithms, weight set ranked by decision tree, probabilistic, cluster, similarity measurements, and nearest neighborhood.26,34,37-43 Some systems combined two or more methods43,44 such as the system presented by Montani et al., 37 where CBR and rule-based reasoning were integrated into the same system to help physicians with therapy planning.
In a survey mapping the use of CBR in medicine published by Choudhury and Begum, the authors identified 76 systems which fell into two groups: 23 using only CBR and 53 using CBR in combination with another technique. 28 The authors of the survey did not describe the reasons for using more than one technique. It should be noted that in most of the 53 system, combining two or more techniques that involved moving from using one technique to two or more techniques is reflected in the publication of separate papers, such as in the work of Montani et al. 37
Holt et al. divided CBR systems into four groups, most of which were diagnosis and decision support systems, a smaller part were classification systems, another smaller part were categorized as planning systems, and only a few were categorized as tutoring systems. 27 The last mentioned category includes systems that involve no particular interaction with the user. The present system is interactive and therefore does not seem to fall in the tutoring systems category or any of the other three categories. The categorization could be expanded with a fifth category, interactive learning systems, or the fourth category could alternatively be further divided into two sub-categories, tutoring systems and interactive learning systems, and given a more generic label, for example pedagogical systems.
As mentioned, CBR is very similar to human cognitive thinking and reasoning when it comes to learning and solving problems. In our perspective, there is large pedagogical potential in applying interactive learning systems. Conventional education, i.e. evidence-based learning material such as books and other written material and lectures, may be less motivating and pedagogical than peer-to-peer training, which is, however, often less evidence-based. CBR-interactive, evidence-based learning systems such as the one suggested in the present study may therefore be able to bridge the two approaches; that is, CBR-interactive learning systems may offer an evidence-based, motivating and more pedagogical approach to learning; for example, showing the wound care nurses how individual variables influence the outcome may help them to achieve better insights into pathophysiological processes and, ideally, the rationale behind various treatments. It should be noted that, when the CBR-interactive learning system is taken into routine use, the decision on how to treat a wound should continue to be based on the clinical skills of the wound care community nurse and, in case of any doubt, the wound care community nurse should continue to consult the specialist call center.
CBR methods may have some limitations. One limitation is the large processing time involved in searching for similar cases in the case base. One should be aware of this limitation, as it might affect the usability of a final learning system. Another limitation relates to the large storage space used in CBR. A general limitation in the study is that the analysis is based on the variables that are routinely registered by the wound care community nurses in Denmark and, therefore, variables such as neuropathy, ischemia, and wound depth were not included in the logistic regression analysis. 21 The potential benefit of adding more variables to the routinely registered variables should be analyzed in future work.
Conclusion
The present CBR prototype is, to our knowledge, the first CBR-interactive, evidence-based learning system centered on diabetic foot ulcers and related treatment. The present prototype illustrates a CBR-interactive learning system that shows how to bridge the gap between traditional evidence-based learning and more motivating and interactive approaches to learning.
Future work should include further development of the CBR-interactive, evidence-based learning system that involve heuristic evaluation and user tests. To demonstrate pedagogical effects in a clinical setting, relatively inexperienced wound care nurses should also be studied by assessing their competence level at baseline and after having used the system for a period. A conventional RCT should be applied to demonstrate clinical effect.
Footnotes
Abbreviations: CBR, Case-based reasoning; DS, Dissimilarity score.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Clara Bender  https://orcid.org/0000-0002-4278-0397
https://orcid.org/0000-0002-4278-0397
Simon Lebech Cichosz  https://orcid.org/0000-0002-3484-7571
https://orcid.org/0000-0002-3484-7571
References
- 1. Tennvall GR, Apelqvist J, Eneroth M. Costs of deep foot infections in patients with diabetes mellitus. Pharmacoeconomics. 2000;18(3):225-238. [DOI] [PubMed] [Google Scholar]
- 2. Boulton AJ, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet. 2005;366(9498):1719-1724. [DOI] [PubMed] [Google Scholar]
- 3. Johannesson A, Larsson G-U, Ramstrand N, Turkiewicz A, Wiréhn A-B, Atroshi I. Incidence of lower-limb amputation in the diabetic and nondiabetic general population: a 10-year population-based cohort study of initial unilateral and contralateral amputations and reamputations. Diabetes Care. 2009;32(2):275-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Haram R, Ribu E, Rustøen T. The views of district nurses on their level of knowledge about the treatment of leg and foot ulcers. J Wound Ostomy Continence Nurs. 2003;30(1):25-32. [DOI] [PubMed] [Google Scholar]
- 5. Gottrup F. Education in wound management in Europe with a special focus on the Danish model. Adv Wound Care (New Rochelle). 2012;1(3):133-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Redmond C, Davies C, Cornally D, Fegan M, O’Toole M. Teaching and learning in the biosciences: the development of an educational programme to assist student nurses in their assessment and management of patients with wounds. J Clin Nurs. 2016;25(17-18):2706-2712. [DOI] [PubMed] [Google Scholar]
- 7. Jørgensen SF, Nygaard R, Posnett J. Meeting the challenges of wound care in Danish home care. J Wound Care. 2013;22(10):540-545. [DOI] [PubMed] [Google Scholar]
- 8. Schaarup C, Pape-Haugaard LB, Hejlesen OK. Models used in clinical decision support systems supporting healthcare professionals treating chronic wounds: systematic literature review. JMIR Diabetes. 2018;3(2):e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zary N, Car J, Carlstedt-Duke J, et al. Digital education for health professions: methods for overarching evidence syntheses (Preprint). J Med Internet Res. 2019;21(2):1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Welsh L. Wound care evidence, knowledge and education amongst nurses: a semi-systematic literature review. Int Wound J. 2018;15(1):53-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dumville JC, O’Meara S, Deshpande S, Speak K. Alginate dressings for healing diabetic foot ulcers. Cochrane Database Syst Rev. 2013;2013(6):CD009110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Edwards J, Stapley S. Debridement of diabetic foot ulcers. Cochrane Database Syst Rev. 2012:CD003556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Selva Olid A, Solà I, Barajas-Nava LA, et al. Systemic antibiotics for treating diabetic foot infections. Cochrane Database Syst Rev. 2015;9:CD009061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dumville JC, Deshpande S, O’Meara S, Speak K. Foam dressings for healing diabetic foot ulcers. Cochrane Database Syst Rev. 2011;9:CD009111. [DOI] [PubMed] [Google Scholar]
- 15. Cruciani M, Lipsky BA, Mengoli C, de Lalla F. Granulocyte-colony stimulating factors as adjunctive therapy for diabetic foot infections. Cochrane Database Syst Rev. 2013;8:CD006810. [DOI] [PubMed] [Google Scholar]
- 16. Martí-Carvajal AJ, Gluud C, Nicola S, et al. Growth factors for treating diabetic foot ulcers. Cochrane Database Syst Rev. 2015;10:CD008548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lewis J, Lipp A. Pressure-relieving interventions for treating diabetic foot ulcers. Cochrane Database Syst Rev. 2013;1:CD002302. [DOI] [PubMed] [Google Scholar]
- 18. Bergin SM, Wraight P. Silver based wound dressings and topical agents for treating diabetic foot ulcers. Cochrane Database Syst Rev. 2006;1:CD005082. [DOI] [PubMed] [Google Scholar]
- 19. Santema TB, Poyck PPC, Ubbink DT. Skin grafting and tissue replacement for treating foot ulcers in people with diabetes. Cochrane Database Syst Rev. 2016;2(2):CD011255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Burns PB, Rohrich RJ, Chung KC. The levels of evidence and their role in evidence-based medicine. Plast Reconstr Surg. 2015;128(1):305-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bender C, Cichosz SL, Pape-Haugaard L, et al. Assessment of simple bedside wound characteristics for a prediction model for diabetic foot ulcer outcomes. J Diabetes Sci Technol. Published online July 22, 2020. doi: 10.1177/1932296820942307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Richter MM, Weber RO. Basic CBR Elements in Case-Based Reasoning. Berlin, Heidelberg: Springer; 2013. [Google Scholar]
- 23. Recio-García JA, González-Calero PA, Díaz-Agudo B. Jcolibri2: a framework for building case-based reasoning systems. Sci Comput Program. 2014;79:126-145. [Google Scholar]
- 24. Aamodt A, Plaza E. Case based reasoning: foundational issues, methodological variations, and system approaches. AI Commun. 1994;7(1):39-59. [Google Scholar]
- 25. Kolodner J. Case-Based Reasoning. San Mateo, CA: Morgan Kaufmann Publishers; 1993. [Google Scholar]
- 26. Blanco X, Rodríguez S, Corchado JM, Zato C. Case-based reasoning applied to medical diagnosis and treatment. Adv Intell Syst Comput. 2012;151:137-46. [Google Scholar]
- 27. Holt A, Bichindaritz I, Schmidt R, Perner P. Medical applications in case-based reasoning. Knoweledge Eng Rev. 2005;20(3):289-292. [Google Scholar]
- 28. Choudhury N, Begum SA. A survey on case-based reasoning in medicine. Int J Adv Comput Sci Appl. 2016;7(8):136-144. [Google Scholar]
- 29. Bichindaritz I, Montani S. Advances in case-based reasoning in the health sciences. Artif Intell Med. 2011;51(2):75-79. [DOI] [PubMed] [Google Scholar]
- 30. Bichindaritz I. Case-based reasoning in the health sciences. Artif Intell Med. 2006;36(2):121-125. [DOI] [PubMed] [Google Scholar]
- 31. Schmidt R, Montani S, Bellazzi R, Portinale L, Gierl L. Cased-based reasoning for medical knowledge-based systems. Int J Med Inform. 2001;64(2-3):355-367. [DOI] [PubMed] [Google Scholar]
- 32. Bellazzi R, Larizza C, Montani S, et al. A telemedicine support for diabetes management: the T-IDDM project. Comput Methods Programs Biomed. 2002;69(2):147-161. [DOI] [PubMed] [Google Scholar]
- 33. Montani S, Portinale L, Leonardo G, Bellazzi R. Applying case-based retrieval to hemodialysis treatment. In: Ashley KD, Bridge DG, eds. Workshop: Proceedings of the Fifth International Conference on Case-Based Reasoning (ICCBR) Held in Trondheim, Norway, 23-26 June, 2003. Springer; 2003:1-734. [Google Scholar]
- 34. Marling C, Shubrook J, Schwartz F. Toward case-based reasoning for diabetes management: a preliminary clinical study and decision support system prototype. Comput Intell 2009;25(3):165-179. [Google Scholar]
- 35. Pesl P, Herrero P, Reddy M, et al. Case-based reasoning for insulin bolus advice: evaluation of case parameters in a six-week pilot study. J Diabetes Sci Technol. 2017;11(1):37-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Herrero P, Pesl P, Reddy M, Oliver N, Georgiou P, Toumazou C. Advanced insulin bolus advisor based on run-to-run control and case-based reasoning. IEEE J Biomed Health Inform. 2015;19(3):1087-1096. [DOI] [PubMed] [Google Scholar]
- 37. Montani S, Bellazzi R, Portinale L, Stefanelli M. A multi-modal reasoning methodology for managing IDDM patients. Int J Med Inform. 2000;58-59:243-256. [DOI] [PubMed] [Google Scholar]
- 38. Chuang C-L. Case-based reasoning support for liver disease diagnosis. Artif Intell Med 2011;53(1):15-23. [DOI] [PubMed] [Google Scholar]
- 39. Petrovic S, Mishra N, Sundar S. A novel case based reasoning approach to radiotherapy planning. Expert Syst Appl. 2011;38(9):10759-10769. [Google Scholar]
- 40. Ahn H, Kim KJ. Global optimization of case-based reasoning for breast cytology diagnosis. Expert Syst Appl. 2009;36(1):724-734. [Google Scholar]
- 41. Ocampo E, MacEiras M, Herrera S, Maurente C, Rodríguez D, Sicilia MA. Comparing Bayesian inference and case-based reasoning as support techniques in the diagnosis of acute bacterial meningitis. Expert Syst Appl. 2011;38(8):10343-10354. [Google Scholar]
- 42. Hsu KH, Chiu C, Chiu NH, et al. A case-based classifier for hypertension detection. Knowledge-Based Syst. 2011;24(1):33-39. [Google Scholar]
- 43. Huang M-L, Hung Y-H, Lee W-M, Li RK, Wang T-H. Usage of case-based reasoning, neural network and adaptive neuro-fuzzy inference system classification techniques in breast cancer dataset classification diagnosis. J Med Syst. 2012;36(2):407-414. [DOI] [PubMed] [Google Scholar]
- 44. Schmidt R, Montani S, Bellazzi R, Portinale L, Gierl L. Cased-based reasoning for medical knowledge-based systems. Int J Med Inform. 2001;64(2-3):355-367. [DOI] [PubMed] [Google Scholar]