Abstract
Objective:
The objective of this review is to discuss a compilation of the currently available literature regarding the impact of diabetic neuropathy (DN) on activities of daily living (ADL), postural stability, and risk of falls.
Methods:
A systematic electronic search strategy was conducted on PubMed/MEDLINE database, Cochrane Library, and Embase in March 2020. This narrative review included clinical cross-sectional studies assessing ADL, postural balance, and falls in adults with DN. All studies underwent a quality assessment based on the Newcastle Ottawa scale developed to assess cross-sectional studies.
Results:
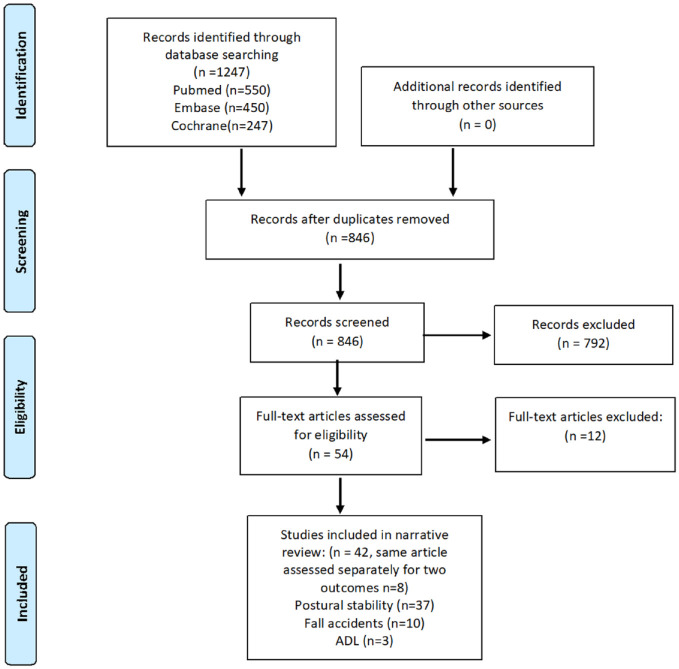
Forty-two studies were identified. A total of 37 studies evaluated postural stability in DN, 10 studies assessed fall accidents, and three studies assessed ADL in individuals with DN. Seven studies assessed both postural stability and fall accidents, and one study assessed postural stability and ADL. Each of the studied outcome variables was assessed separately. Based on a quality assessment, eight studies were excluded resulting in an evaluation of 34 studies.
Conclusions:
Diabetic neuropathy has a negative impact on postural balance and gait kinematics combined with an increased fall risk. Because of the few number of studies available, we were unable to evaluate the impact of DN on ADL. Our findings are in concordance with previous reviews, supporting the evidence for DN as a critical measure negatively impacting postural stability and fall risk in individuals with diabetes. Further clinical investigative studies are needed.
Keywords: activities of daily living, diabetic neuropathy, falls, postural stability
Introduction
Journal of Diabetes Science and Technology’s special section on Diabetic Neuropathy.
Diabetic neuropathy (DN) is a common complication of diabetes that may negatively affect physical activity and independence. 1 DN has been reported to lead to postural instability, increased risk of falling, and inability to perform activities of daily living (ADL). Several studies have assessed ADL, postural stability, and fall risk in individuals with DN. Because of large variabilities in the study populations and designs, outcome measures, and definitions of DN, there is a substantial lack of knowledge and evidence. No previous review has comprehensively assessed these factors.
Therefore,in our review, we will present and discuss an updated compilation of the currently available literature on the impact of DN on activities of daily living, postural stability, and risk of falls.
Methods and Design
Our methodology for the systematic literature search aimed to identify studies that assessed individuals with DN regarding fall accidents, postural balance, or activities of daily living. Two independent reviewers assessed the inclusion and exclusion criteria (KSK, HA). Only investigational clinical studies concerning humans with DN written in English were included. We applied the PRISMA guidelines for this review (Supplementary Material). The defined PICO-statements were defined as follows: Population (P): Adults (age >18 y) with diabetes mellitus; Phenomenon of Interest (I): Impact of Diabetic neuropathy; Context (C): in diabetic neuropathy; Outcome (O): The outcome variables were accidental falls, postural balance, and activities of daily living.
Exclusion criteria: Studies reported as abstracts only. Abstracts that did not mention the inclusion of individuals with diabetic neuropathy. Abstracts that did not include any of the outcome measures, studies that enrolled less than 10 individuals with DN included neuropathies due to other causes than diabetes, intervention trials on drugs, study protocols, case reports, other reviews, studies that included treatment interventions, or studies used to validate assessment instruments were excluded. Studies were excluded if they did not specify how DN was diagnosed or only included subgroups of DN (e.g. painful DN).
Search Strategy
An electronic search was conducted on PubMed/MEDLINE database, Cochrane Library, and Embase in March 2020. The search had no set start date criteria. The reviewers assessed the inclusion and exclusion criteria. The search strategy on PubMed/MEDLINE was as follows and was modified for other search databases: Search ((((((“Diabetic Neuropathies”[Mesh]) OR “Diabetic Neuropathies”) OR “Diabetic Neuropathy”) OR “Diabetic Polyneuropathies”) OR “Diabetic Polyneuropathy”)) AND (((((((((((((“Postural Balance”[Mesh]) OR “Postural Balance”) OR “Postural Balances”) OR “Body Equilibrium”) OR “Accidental Falls”[Mesh]) OR “Accidental Falls”) OR “Accidental Fall”) OR “Falling”) OR “Activities of Daily Living”[Mesh]) OR “Activities of Daily Living”) OR “Activity of Daily Living”) OR “Daily Life Activities”) OR “Daily Life Activity”) Filters: Humans
Data Collection and Selection of Studies
Collection and selection of studies were performed through an online reference management system (Mendeley) to assess database hits and remove duplicates. First articles were screened by abstract and title, and full-text articles were screened only if the inclusion criteria for the review were met or if the eligibility could not be assessed based on the abstract or title.
Quality evaluation of included studies
All studies included were assessed for quality by the Newcastle-Ottawa Quality Assessment Scale (NOAS) for cross-sectional studies. 2 This scale consists of three major components: (1) selection, (2) comparability, (3) outcome and encompasses eight criteria. Study quality is scored on a scale from 0 to 10, a higher score indicating higher methodological quality. To be included in our narrative review, studies had to have a score of ≥5. Studies were assessed separately for the three outcomes: postural balance, fall accidents, and ADLs. If a study assessed two or more variables, the study was reassessed for each variable within each category.
Diabetic neuropathy
Only studies including clinical assessment of individuals with diabetes and DN were included. If a study was based solely on questionnaires or registry data, the study was not included.
Postural balance
Several factors can affect balance in DN, including impairment of the sensory system, muscle weakness, impaired mobility, and structural and functional alterations of the foot. 3 Both static and dynamic postural stability has been shown to be impaired in DN. In individuals with DN the gait is characterized by longer stance phases, shorter steps, 4 and slower gait velocity. Several different tools have been identified and used for the measurement of balance. All clinical studies were included in this review, assessing both static and dynamic postural stability by the use of computer-assisted tools such as posturography or kinematic gait analysis tools or clinical tests.
Accidental falls
All clinical studies evaluating individuals with DN and the frequency or risk of falling prospectively and/or retrospectively and or by registry data were included. Several recently published studies have assessed falling based on a risk estimation using the Berg Balance Scale or other clinical assessment. However, as actual falling was not assessed, these studies were not included.
Activities of daily living
“Activities of daily living” are defined as activities in the performance of the basic activities of self-care, such as feeding, dressing, toileting, washing, and ambulation. Other more extensive tasks are included within the definition, such as the use of public transportation, shopping for groceries, meal preparation, and doing household chores. Only studies that included an actual assessment of ADL were included.
Results
Our systematic search identified 1247 articles. After removing duplicates, titles and abstracts were screened, resulting in 54 full-text articles. These articles were assessed for eligibility, out of which 42 were included (Figure 1, Table S1). After quality assessment of the cross-sectional studies according to the NOAS (Table S2.), further eight studies were excluded due to poor quality. One study described postural stability and ADL in DN. 5 Seven studies assessed both fall accidents and postural stability in individuals with DN; however, one of these studies was included for the postural stability assessment but did not fulfill the criteria for risk of falls description. 3 None of the included studies assessed all three outcome variables of interest.
Figure 1.
PRISMA flow chart for study selection.
A total of 37 studies examining the impact of DN on postural stability were identified. After quality assessment, eight studies were excluded and 29 studies, of which 14 studies, were good quality studies. Several of the included studies described a correlation between postural instability and altered gait kinematics in individuals with DN.3,6-16 Two studies described the correlation between poor postural stability and the severity of DN.17,18 Additionally, two studies accentuated the finding by also performing nerve conduction velocities.19,20 Slower walking speed8,21 and altered gait pattern10,22 reduced muscle strength, and/or reduced joint torques of the lower limbs while walking in DN, were described in several studies.23-26 However, three studies suggested that DN may not be the only cause of postural instability reported in this population, suggesting diabetes may itself negatively affect postural control 27 through impaired neurocognitive functions 28 or poor glycemic control. 13
Ten studies evaluating fall accidents in DN were identified, of which, one study had to be excluded due to an unsatisfactory score. This resulted in inclusion of nine studies with a satisfactory score. However, none of the studies included qualified for a “good” or “very good” category.
Out of the nine studies assessing falls in DN, six studies showed an increased frequency of falling in the DN population,13,16,26,28,29 whereas one study showed no difference between the reporting of falls between individuals with and without DN. Cavanaugh described that individuals with DN had a 15 times increased risk of suffering from a fall-related injury. 30 However, this study did not only evaluate fall accidents as other injuries such as fall-related fractures, sprains, and cuts were also included within the same category.
Only three studies were identified evaluating ADL in DN, all of which were qualified as “good” or “very good.” All three studies found a correlation between decreased ADL and DN. Vileikyte et al. suggested ADL restrictions in DN were associated with depressive symptoms and neuropathic pain. 31
Discussion
Based on the results of the present systematic review of 34 studies, it can be concluded that individuals with DN suffer from postural instability, impaired gait, and report an increased incidence of falling. Only three studies assessed activities of daily living, and therefore, we can only infer that impaired balance and decreased gait kinematics in DN can increase the incidence of falling and impact ADL.
Diabetic Neuropathy and Postural Stability
Based on literature search, the majority of the studies identified reported DN to impair postural stability and alter gait kinematics (gait velocity, stride length, forefoot displacement, plantarflexion, and the proprioceptive threshold of the ankle). Several of the studies were of high quality; however, most studies included a convenience sample, and only two studies included a random sample of individuals with DN/and or diabetes representing the average diabetes population.13,32
Three of the studies describing postural stability included a power sample size calculation.13,17,32 Most of the studies included, compared, and described the results in a control group, and 15 studies compared the results to individuals without DN and healthy controls, adjusting for the impact of diabetes per se. All studies included a clinical evaluation of postural stability. Only four studies described the use of an objective and validated instrument for the evaluation of postural stability.14,22,28,33 By not using validated evaluation methods, other studies might have inaccurately evaluated postural instability. Several of the studies described postural stability based on functional reach test (FRT), or the one-legged stand test.11,16,32,34 Although these tests are validated, they are not objective as compared to computer-assisted posturography. Compensatory movements during the test such as truncal shift, are not taken into account in FRT, which may influence the test to a higher degree than the displacement of center of pressure, which is evaluated during computer-assisted posturography. 35
Several of the studies of postural stability did not adjust for confounders such as age and gender, which might have skewed the findings,10,12,18,23,27,36 as older age is known to be associated with postural instability. Based on our review of the currently existing literature, we found an association between DN and postural instability as 29 studies confirmed the association, and only three studies disproved it.
Diabetic Neuropathy and Falls
Only few included studies assessed the frequency of falling in DN, most of which were of low quality. In most studies, the results were compared to a control group and result concerning non-responders were presented. Four studies assessed falling prospectively,28-30,37 whereas the other studies were retrospective using recall assessment of falling based on different time frames (3, 6, or 12 mo). Assessing fall accidents during different time frames limits the ability to compare the results from the different studies, as longer time frames might introduce recall bias, whereas shorter time frames have to take seasonal changes into account. Assessment of fall accidents is challenging as multiple factors such as external forces and seasonal changes can impact the frequency. In this review, we evaluated if other risk factors were taken into consideration, such as age and gender. However, we did not grade the studies according to the adjustment of other factors that may affect the risk of falls and or postural stability. Maintenance of postural balance and the ability to recover from a fall depends on several factors, including the normal function of; visual, vestibular, somatosensory, and the musculoskeletal system, all of which can be impaired in diabetes. Other factors, such as decreased cognitive functions, depression, orthostatic hypotension, and hypoglycemic episodes, have also shown to increase fall risk. Several of the studies included did not incorporate a multifactorial assessment for fall risk with little or no evaluation of confounding factors, not allowing for an accurate assessment of the impact of DN on falls. Furthermore, most studies identified did not consist of a random sample, were lacking a clear definition of falling, or provided little or no explanation of the time frame used for fall assessment. Only one study included a random sample of individuals with sample size calculation. 13
In spite of several weaknesses, all of the included studies, except one, described an association between increased fall risk and DN. Therefore we conclude that there is an increased risk of falls in DN.
Diabetic Neuropathy and Activities of Daily Living
Four studies assessed both postural stability and falling in individuals with DN,13,15,28 and one of these studies 3 was excluded due to low quality under the fall outcome category assessment; however, this study was included in the postural stability assessment.
As balance and gait can have a great impact on activities of daily living, multiple studies suggest an association. Remarkably, only few studies assessed the impact of DN on activities of daily living using scales or questionnaires. Therefore, we may conclude that the impact of DN on ADL remains unknown and future clinical studies should include tools assessing ADL.
Technology
Studies included in our search were based on individuals with DN. However, the technologies used in the assessment of DN differed in the included studies basing the diagnosis of DN on: vibration perception thresholds, monofilament testing, nerve conductive studies and different clinical scales such as: Toronto Clinical Neuropathy Score, Utah Early Neuropathy Scale, modified Neuropathy Disability Score, Diabetic Neuropathy Examination Score, and Michigan Neuropathy Screening Instrument. In the past, clinical testing and diagnosis of DN have been challenging because of low reproducibility and a lack of consensus concerning the definition of DN. However, over the past decades, multiple clinical scales, questionnaires, and scoring systems have been developed and validated to aid in recognition of clinical manifestations and complaints in DN. This has led to recommendations of performing more than one test, with more than one abnormality to confirm the diagnosis of DN. In 2009, the criteria were defined and described by Tesfaye et al. on behalf of the Toronto Diabetic Neuropathy Expert Group. 38 Studies included in this review were not differentiated or excluded based on the diagnostic criteria of DN (Table S1). However, studies were included pending inclusion of a description and evaluation of DN. This may be a weakness due to the uncertainty to what degree individuals suffered from DN. Only six studies included in our review performed both clinical assessment and nerve conductive studies, which are included in the Toronto criteria of confirmed DN.
There is a clear need for clinical studies assessing the causation of falling in diabetes by applying a multifactorial assessment and including DN, which has a great impact on postural stability, fall risk, and may lead to impaired activities of daily living. In individuals with DN, clinicians should consider examination of postural stability and fall risk as part of fall prevention programs to improve ADL and ultimately quality of life.
Conclusions
Based on this review we conclude that DN has a negative impact on postural balance. Furthermore, DN causes impaired gait and leads to an increased fall risk. Because of a very few number of studies, it was not possible to assess the impact of DN on ADL. Our findings are in concordance with previous reviews, supporting the evidence for DN as a critical measure negatively impacting fall risk, postural instability in individuals with diabetes. There is a clear need for high quality controlled clinical studies focusing on the functional consequences of DN.
Supplemental Material
Supplemental material, sj-pdf-1-dst-10.1177_1932296821997921 for The Impact of Diabetic Neuropathy on Activities of Daily Living, Postural Balance and Risk of Falls - A Systematic Review by Karolina Snopek Khan and Henning Andersen in Journal of Diabetes Science and Technology
Supplemental material, sj-pdf-2-dst-10.1177_1932296821997921 for The Impact of Diabetic Neuropathy on Activities of Daily Living, Postural Balance and Risk of Falls - A Systematic Review by Karolina Snopek Khan and Henning Andersen in Journal of Diabetes Science and Technology
Supplemental material, sj-pdf-3-dst-10.1177_1932296821997921 for The Impact of Diabetic Neuropathy on Activities of Daily Living, Postural Balance and Risk of Falls - A Systematic Review by Karolina Snopek Khan and Henning Andersen in Journal of Diabetes Science and Technology
Footnotes
Abbreviations: ADL, activities of daily living; DN, diabetic neuropathy; NOAS, Newcastle-Ottawa Quality Assessment Scale.
Author contributions: Khan KS: Study design, data collection, interpretation of data and writing of first manuscript draft.
Andersen H: Study design, data collection, interpretation of data, writing and revision of manuscript.
Both authors approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this publication is part of the International Diabetic Neuropathy Consortium (IDNC) research program, which is supported by a Novo Nordisk Foundation Challenge Program grant (Grant number NNF14OC0011633) and Aarhus University. Aarhus University, receives funding for other studies from companies in the form of research grants to (and administered by) Aarhus University. None of these studies has any relation to the present study.
ORCID iD: Karolina Snopek Khan  https://orcid.org/0000-0003-1288-6227
https://orcid.org/0000-0003-1288-6227
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Pop-Busui R, Boulton AJM, Feldman EL, et al. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care. 2017;40:136-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ottawa Hospital Research Institute n.d. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 3. Vaz MM, Costa GC, Reis JG, Junior WM, Albuquerque de, Paula FJ, Abreu DC. Postural control and functional strength in patients with type 2 diabetes mellitus with and without peripheral neuropathy. Arch Phys Med Rehabil. 2013;94:2465-2470. [DOI] [PubMed] [Google Scholar]
- 4. Melai T, Schaper NC, Ijzerman TH, et al. Increased forefoot loading is associated with an increased plantar flexion moment. Hum Mov Sci. 2013;32:785-793. [DOI] [PubMed] [Google Scholar]
- 5. Riandini T, Wee HL, Khoo EY, et al. Functional status mediates the association between peripheral neuropathy and health-related quality of life in individuals with diabetes. Acta Diabetol. 2018;55:155-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lalli P, Chan A, Garven A, et al. Increased gait variability in diabetes mellitus patients with neuropathic pain. J Diabetes Complications. 2013;27:248-254. [DOI] [PubMed] [Google Scholar]
- 7. Simoneau GG, Ulbrecht JS, Derr JA, et al. Postural instability in patients with diabetic sensory neuropathy. Diabetes Care. 1994;17:1411-1421. [DOI] [PubMed] [Google Scholar]
- 8. Resnick HE, Stansberry KB, Harris TB, et al. Diabetes, peripheral neuropathy, and old age disability. Muscle Nerve. 2002;25:43-50. [DOI] [PubMed] [Google Scholar]
- 9. Dingwell JB, Ulbrecht JS, Boch J, et al. Neuropathic gait shows only trends towards increased variability of sagittal plane kinematics during treadmill locomotion. Gait Posture. 1999;10:21-29. [DOI] [PubMed] [Google Scholar]
- 10. Menz HB, Lord SR, St George R, et al. Walking stability and sensorimotor function in older people with diabetic peripheral neuropathy. Arch Phys Med Rehabil. 2004;85:245-252. [DOI] [PubMed] [Google Scholar]
- 11. Cimbiz A, Cakir O. Evaluation of balance and physical fitness in diabetic neuropathic patients. J Diabetes Complications. 2005;19:160-164. [DOI] [PubMed] [Google Scholar]
- 12. Schilling RJ, Bollt EM, Fulk GD, et al. A quiet standing index for testing the postural sway of healthy and diabetic adults across a range of ages. IEEE Trans Biomed Eng. 2009;56:292-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Emam AA, Gad AM, Ahmed MM, Assal HS, Mousa SG. Quantitative assessment of posture stability using computerised dynamic posturography in type 2 diabetic patients with neuropathy and its relation to glycaemic control. Singapore Med J. 2009;50:614-618. [PubMed] [Google Scholar]
- 14. Fahmy IM, Ramzy GM, Salem NA, Ahmed GM, Mohammed AA. Balance disturbance in patients with diabetic sensory polyneuropathy. Egypt J Neurol Psychiatry Neurosurg. 2014;51:21-29. [Google Scholar]
- 15. Toosizadeh N, Mohler J, Armstrong DG, et al. The influence of diabetic peripheral neuropathy on local postural muscle and central sensory feedback balance control. PLoS One. 2015;10:e0135255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bokan-Mirković V, Škarić-Karanikić Ž, Nejkov S, et al. Diabetic polyneuropathy and risk of falls: fear of falling and other factors. Acta Clin Croat. 2017;56:721-727. [DOI] [PubMed] [Google Scholar]
- 17. Corriveau H, Prince F, Hebert R, et al. Evaluation of postural stability in elderly with diabetic neuropathy. Diabetes Care. 2000;23:1187-1191. [DOI] [PubMed] [Google Scholar]
- 18. Ghanavati T, Yazdi MJ, Goharpey S, Arastoo AA. Functional balance in elderly with diabetic neuropathy. Diabetes Res Clin Pract. 2011;11:24-28. [DOI] [PubMed] [Google Scholar]
- 19. Uccioli L, Giacomini PG, Monticone G, et al. Body sway in diabetic neuropathy. Diabetes Care. 1995;18:339-144. [DOI] [PubMed] [Google Scholar]
- 20. Yamamoto R, Kinoshita T, Momoki T, et al. Postural sway and diabetic peripheral neuropathy. Pain. 2011;52:213-221. [DOI] [PubMed] [Google Scholar]
- 21. Handsaker JC, Brown SJ, Bowling FL, et al. Contributory factors to unsteadiness during walking up and down stairs in patients with diabetic peripheral neuropathy. Diabetes Care. 2014;37:3047-3053. [DOI] [PubMed] [Google Scholar]
- 22. Brown SJ, Handsaker JC, Bowling FL, Boulton AJ, Reeves ND. Diabetic peripheral neuropathy compromises balance during daily activities. Diabetes Care. 2015;38:1116-1122. [DOI] [PubMed] [Google Scholar]
- 23. Onodera AN, Gomes AA, Pripas D, et al. Lower limb electromygraphy and kinematics of neuropathic diabetic patients during real-life activities: stair negotiation. Muscle Nerve. 2011;44:269-277. [DOI] [PubMed] [Google Scholar]
- 24. Allet L, Kim H, Ashton-Miller J, et al. Frontal plane hip and ankle sensorimotor function, not age, predicts unipedal stance time. Muscle Nerve. 2012;45:578-585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Brown SJ, Handsaker JC, Bowling FL, et al. Do patients with diabetic neuropathy use a higher proportion of their maximum strength when walking? J Biomech. 2014;47:3639-3644. [DOI] [PubMed] [Google Scholar]
- 26. Allet L, Kim H, Ashton-Miller J, De Mott T, Richardson JK. Step length after discrete perturbation predicts accidental falls and fall-related injury in elderly people with a range of peripheral neuropathy. J Diabetes Complications. 2014;28:79-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fulk GD, Robinson CJ, Mondal S, Storey CM, Hollister AM. The effects of diabetes and/or peripheral neuropathy in detecting short postural perturbations in mature adults. J Neuroeng Rehabil. 2010;7:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Richardson JK, Eckner JT, Allet L, et al. Complex and simple clinical reaction times are associated with gait, balance, and major fall injury in older subjects with diabetic peripheral neuropathy. Am J Phys Med Rehabil. 2017;96:8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zurales K, DeMott TK, Kim H, Allet L, Ashton-Miller JA, Richardson JK. Gait efficiency on an uneven surface is associated with falls and injury in older subjects with a spectrum of lower limb neuromuscular function: a prospective study. Am J Phys Med Rehabil. 2016;95:83-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cavanagh PR, Derr JA, Ulbrecht JS, Maser RE, Orchard TJ. Problems with gait and posture in neuropathic patients with insulin-dependent diabetes mellitus. Diabet Med. 1992;9:469-474. [DOI] [PubMed] [Google Scholar]
- 31. Vileikyte L, Leventhal H, Gonzalez JS, et al. Diabetic peripheral neuropathy and depressive symptoms: the association revisited. Diabetes Care. 2005;28:2378-2383. [DOI] [PubMed] [Google Scholar]
- 32. Timar B, Timar R, Gaiță L, et al. The impact of diabetic neuropathy on balance and on the risk of falls in patients with type 2 diabetes mellitus: a cross-sectional study. PLoS One. 2016;11:e0154654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Palma FH, Antigual DU, Martínez SF, Monrroy MA, Gajardo RE. Static balance in patients presenting diabetes mellitus type 2 with and without diabetic polyneuropathy. Arq Bras Endocrinol Metabol. 2013;57:722-726. [DOI] [PubMed] [Google Scholar]
- 34. Camargo MR, Barela JA, Nozabieli AJL, et al. Balance and ankle muscle strength predict spatiotemporal gait parameters in individuals with diabetic peripheral neuropathy. Diabetes Metab Syndr Clin Res Rev. 2015;9:79-84. [DOI] [PubMed] [Google Scholar]
- 35. Johnsson E, Henriksson M, Hirschfeld H. Does the functional reach test reflect stability limits in elderly people? J Rehabil Med. 2003;35:26-30. [DOI] [PubMed] [Google Scholar]
- 36. Kelly C, Fleischer A, Yalla S, et al. Fear of falling is prevalent in older adults with diabetes mellitus but is unrelated to level of neuropathy. J Am Podiatr Med Assoc. 2013;103:480-488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Richardson JK, Demott T, Allet L, Kim H, Ashton-Miller JA. Hip strength: ankle proprioceptive threshold ratio predicts falls and injury in diabetic neuropathy. Muscle Nerve. 2014;50:437-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Tesfaye S, Vileikyte L, Rayman G, et al. Painful diabetic peripheral neuropathy: consensus recommendations on diagnosis, assessment and management. Diabetes Metab Res Rev. 2011;27:629-638. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-dst-10.1177_1932296821997921 for The Impact of Diabetic Neuropathy on Activities of Daily Living, Postural Balance and Risk of Falls - A Systematic Review by Karolina Snopek Khan and Henning Andersen in Journal of Diabetes Science and Technology
Supplemental material, sj-pdf-2-dst-10.1177_1932296821997921 for The Impact of Diabetic Neuropathy on Activities of Daily Living, Postural Balance and Risk of Falls - A Systematic Review by Karolina Snopek Khan and Henning Andersen in Journal of Diabetes Science and Technology
Supplemental material, sj-pdf-3-dst-10.1177_1932296821997921 for The Impact of Diabetic Neuropathy on Activities of Daily Living, Postural Balance and Risk of Falls - A Systematic Review by Karolina Snopek Khan and Henning Andersen in Journal of Diabetes Science and Technology