Abstract
Recognizing that social factors influence patient health outcomes and utilization, health systems have developed interventions to address patients' social needs. Care coordination across the health care and social service sectors is a distinct and important strategy to address social determinants of health, but limited information exists about how care coordination operates in this context. To address this gap, the authors conducted a systematic review of peer-reviewed publications that document the coordination of health care and social services in the United States. After a structured elimination process, 25 publications of 19 programs were synthesized to identify patterns in care coordination implementation. Results indicate that patient needs assessment, in-person patient contact, and standardized care coordination protocols are common across programs that bridge health care and social services. Publications discussing these programs often provide limited detail on other key elements of care coordination, especially the nature of referrals and care coordinator caseload. Additional research is needed to document critical elements of program implementation and to evaluate program impacts.
Keywords: care coordination, social determinants of health, social services, systematic review
Introduction
Social and economic factors impact health outcomes and perpetuate disparities between advantaged and disadvantaged groups.1,2 These nonclinical factors, known as social determinants of health, are often more important than health care in explaining population health outcomes.3–5 To improve patient health and avoid unnecessary utilization and cost, providers and delivery systems are increasingly implementing interventions to address patients' social needs, including assistance with employment, housing, education, food security, and navigating the legal system.6–8 However, long-standing separation of health care and social services poses challenges to effectively linking patients across these sectors for appropriate support. Care coordination is an approach that providers have used for decades to reduce fragmentation in health care,9,10 and represents an important strategy for increasing continuity of health care and social services for patients with complex needs.
Care coordination can be broadly described as the intentional organization of patient care across multiple participants, accompanied by the sharing of relevant information, to improve the safety and effectiveness of services.11,12 Systematic and narrative reviews have summarized a large body of literature on care coordination across health care disciplines including primary care, behavioral health care, and specialty care.9,13–19 However, existing research has not focused on care coordination across the health care and social service sectors. Prior systematic reviews documented clinical interventions to address patients' social needs,6,7 but did not provide details on the specific practice of care coordination within these interventions. Care coordination spanning health care and social services merits special attention because organizations in these sectors often differ in organizational structure, financing, workplace culture, and other factors.20,21 These differences create barriers to effective partnerships that do not exist when coordinating care within the health care system. It is thus plausible that care coordination across health care and social services manifests differently from coordination across specialties within health care. However, no studies have synthesized literature to identify important aspects of this type of care coordination, leaving potential shortfalls in researcher and practitioner understanding.
To inform the implementation and evaluation of cross-sector programs that address both medical and social needs, this article fills a gap in the literature by systematically reviewing research on care coordination across health care and social service sectors. The research team addresses the question: “What program elements are most commonly described in publications regarding care coordination across health care and social services?” In this review, health care is defined as medical care focused on physical health, and excludes coordination that focuses on linking only behavioral health and social services. Social services are defined as any nonmedical services to meet basic social or economic needs, excluding health promotion and education focused solely on health.
Conceptual framework
This systematic review is informed by a conceptual framework (Table 1), which the research team developed based on a review of available frameworks specifying key elements of care coordination.22–27 The team identified 9 key elements hypothesized to influence the effectiveness of care coordination programs, subdivided into 2 categories: processes that occur during care coordination, and infrastructure that provides foundational support for care coordination processes.
Table 1.
Framework of Care Coordination Program Elements
| Category | Program element | Description |
|---|---|---|
| Care Coordination Process | Needs Assessment | Systematic assessment of patient medical, social, and other needs. |
| Care Planning | Development of an individualized care plan to guide care coordination. | |
| Patient Engagement | Nature, frequency, and modes of communication with patient. | |
| Referrals | Nature of referrals to medical, social, and other services (eg, “active” or “warm handoffs”). | |
| Accountability | Mechanisms for ensuring team members effectively coordinate care. | |
| Care Coordination Infrastructure | Staffing | Type of staff involved, training provided to staff, and caseload for care coordination. |
| Information Sharing | Sharing of patient information across relevant providers to support care coordination. | |
| Standard Protocols | Specialized protocols or workflows for care coordination. | |
| Financing | Specialized funding or reimbursement structures for care coordination. |
Five elements of the framework consist of care coordination processes that occur on an ongoing basis to support patients: assessment of patient needs, care planning, patient engagement, referrals across service types, and accountability monitoring. With some differences in terminology, the Agency for Healthcare Research and Quality includes each of these processes as a “mechanism” for achieving care coordination in their Care Coordination Measures Atlas.28 Among these elements, systematic assessment of patient needs and the subsequent development of tailored care plans are 2 of the “Ten Essential Characteristics of Care Coordination” proposed in a recent commentary.29 One systematic review of care coordination measurement instruments found that 59% included assessment of needs and goals, and 44% included creation of a proactive plan of care.24 Another study of 7 programs that linked health care and social services found that all provided baseline health assessments, social needs assessments, and individualized care plans,26 highlighting the importance of these activities. Patient engagement is another process common to high-performing care coordination programs. Effective approaches to patient engagement include a patient-centered approach that supports self-management,24,28 ongoing monitoring and follow-up of patients,26,28 and regular communication with patients and their families or caregivers.29 One study found that care coordination programs successfully reduced hospitalizations when they included frequent in-person contact with patients, at least once a month.30
Referral processes also are central to coordinating care. A multiple case study of programs that bridge across health care and social services found that all referred patients to both social services and medical care.26 Transitions between settings are effective when they are “planned and proactive.”29 For example, one review of literature on linkage to medical and social services for patients with HIV found that “active” referrals, such as helping patients make appointments or even going with patients to obtain services, were more effective than “passive” referrals such as only providing patients with service information.31 Additionally, accountability processes are essential to ensure fidelity of implementation of care coordination elements. Examples include regular interdisciplinary team meetings of providers,27,32 formal partnerships or shared governance structures established between organizations,25 co-location of providers at the same physical site,27,30 and developing a shared vision of patient-centered care.25
The remaining 4 elements of the framework relate to underlying infrastructure elements for supporting care coordination processes: staffing and workforce development, structures for sharing information, standard protocols for care coordination, and financing arrangements. Regarding staffing, one systematic review of care coordination frameworks found that 73% included workforce as a concept.23 Effective care coordination programs build interdisciplinary teams consisting of different types of staff to meet patient needs,27,29 and often provide specialized training in care coordination.26,32 Though research on care coordinator caseloads is limited, one study of care coordination in patient-centered medical homes found that high caseloads pose challenges,33 and research on social worker caseloads indicates that high caseload sizes contribute to staff burnout.34 In addition to strategic staffing, information sharing through electronic systems and other mechanisms is also essential to care coordination,24,25,27–29 though patient privacy and confidentiality require careful consideration prior to integrating data systems.35
Standard procedures or protocols, such as written guidance documents, are another important infrastructure element to support care coordination processes. Weaver et al27 emphasize the importance of plans and rules such as policies, guidelines, and flow diagrams to coordinate care, and prior research has highlighted the example of protocols to guide referral processes.31 However, a multiple case study of programs that link health care and social services found that only 4 of 7 implemented specialized intervention protocols,26 raising questions about the prevalence of standardized procedures in coordination of health care and social services. Finally, financing constitutes another key element of care coordination infrastructure. One study of programs that bridge health care and social services noted flexible financing as a contributor to program success,25 while another identified financing as a challenge to implementing this type of program.26 Despite the importance of understanding the financial structure of care coordination, a systematic review of care coordination frameworks found that only 24% included financing as a concept, indicating that this represents a potentially under-explored care coordination element.23 The research team include financing along with the other 8 elements to organize the results of this systematic review of literature on the coordination of health care and social services.
Methods
Search strategy
This systematic review was written in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Supplementary Table S1, available with the article online).36 A protocol was registered in the PROSPERO registry for systematic reviews (PROSPERO 2019 CRD42019118031). Two investigators developed the search strategy in consultation with a research librarian. In July 2018, the research team searched PubMed, PsycINFO, CINAHL Plus, the Cochrane Database of Systematic Reviews, and the Cochrane Central Register of Controlled Trials (CENTRAL) for relevant publications. The search was limited to English language articles published since 2010 that contained keywords such as care, healthcare, service use, coordinat* (asterisk indicating a wild card for the rest of the word), integrat*, collaborat*, social services, social needs, cross sector, high utilizing, high utilizer, super user, and hot spotter. The research team also identified additional publications by reviewing the references of publications identified in the original search.
Inclusion and exclusion criteria
Publications were included if they described care coordination elements, included adequate empirical detail about program implementation or outcomes, described care coordination across multiple sectors and multiple organizations, focused on non-elderly adults, were located in the United States, and focused on care coordination to address both medical needs and social needs that are not traditionally addressed in the health care system (eg, not solely health insurance enrollment, physical activity promotion, or similar). To identify publications for inclusion and exclusion, the research team engaged in a multistep process of screening titles, abstracts, and full publications. First, team members screened publication titles, and excluded publications that clearly were not relevant. Then, 2 investigators independently reviewed the abstracts of the remaining publications. The abstract reviewers resolved disagreements in partnership with a third reviewer through discussion and consensus. Finally, 2 investigators independently reviewed the full-text versions of the remaining publications, and again resolved disagreements through discussion and consensus. The research team used Endnote software, version X8.2 (Clarivate, Philadelphia, PA) to manage publications during each stage of the review. Additionally, prior to each stage the investigators reviewed a small subset of the publications as a training set to ensure consistency in coding and to refine the inclusion and exclusion criteria.
Data extraction
After the full-text review, members of the research team extracted information from the final publications using a structured web-based form that populated a spreadsheet. The form included both open-ended and closed-ended questions to categorize and describe each included publication. At least 2 members of the research team reviewed the information extracted from each publication to ensure accuracy. This review did not include a risk of bias or study quality assessment because the information extracted from the publications focused on the implementation of the programs that the publications described, and not the empirical findings of the published studies.
Results
Overview of included publications
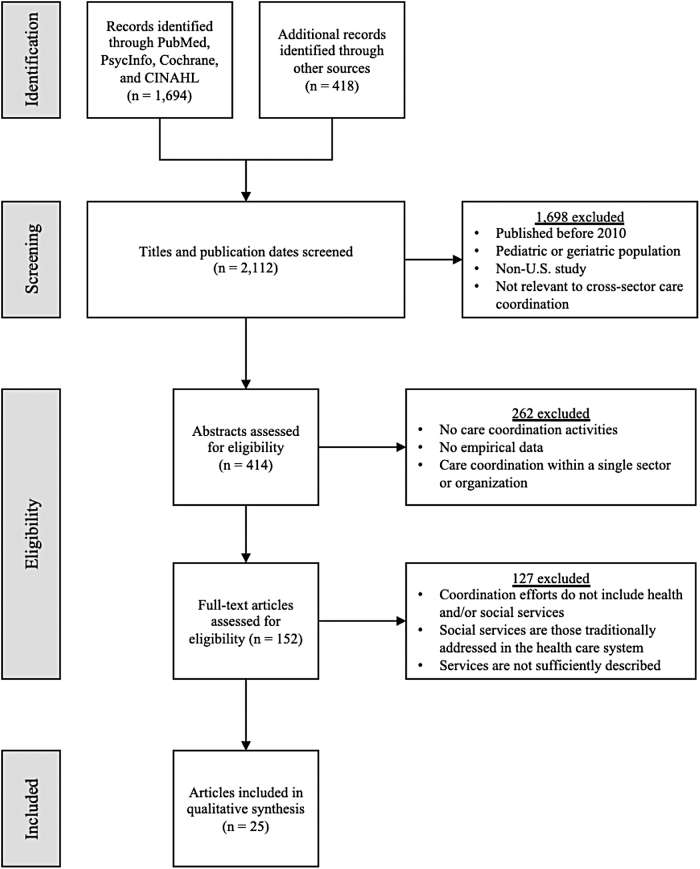
The initial search of research databases resulted in 1694 publications, and an additional 418 were identified through other means including reviewing references of identified publications. After screening for eligibility, 25 publications were included in this review (Figure 1).37–61 Two more publications contained information about multiple programs that coordinated across health care and social services, but were excluded because they provided insufficient detail about each program for the purpose of this review. Additionally, several programs were described in more than 1 publication. As a result, the final set of 25 publications discussed 19 distinct care coordination programs that met criteria for inclusion in analysis. Care coordination programs varied in their target geographic location, type of lead organization, eligible population, and social services addressed (Table 2).
FIG. 1.
Identification of records for inclusion in the study.
Table 2.
Overview of Cross-Sector Care Coordination Programs in Included Publications
| Program | Geographic location | Approximate number of patients or sites | Type of lead organization | Eligible population | Main social services addressed | Primary mode of patient communication | Primary care coordination staff type |
|---|---|---|---|---|---|---|---|
| Camden Coalition of Healthcare Providers37 | Camden, New Jersey | 3 hospitals, 2 FQHCs, and numerous other medical practices and social service agencies | Multidisciplinary coalition | Patients with a high number of hospital admissions | Housing, Benefits assistance | On-site, In the field | Physician or mid-level provider, Social worker |
| Community Health Access Project38 | Richland County, Ohio | 115 patients in the intervention group and 115 controls | Community-based organization | Women at risk of unfavorable birth outcomes | Housing, Education or employment assistance, Benefits assistance, Transportation | In the field | Community health worker or peer coach |
| Emergency Department Care Coordination Intervention39 | Boston, Massachusetts | 36 patients in the intervention group and 36 controls | Emergency department | Patients with high emergency department utilization | Benefits assistance, Transportation | On-site, In the field, Telephonic | Community health worker or peer coach |
| Health Leads Help Desks40–42 | Communities across the United States | More than 100,000 patients at more than 2500 health care institutions from 1996 to 2017 | Health system, Primary care practitioner office or clinic | Patients with unmet basic resource needs | Housing, Education or employment assistance, Benefits assistance, Transportation | On-site, Telephonic | Nonpermanent volunteers |
| Hennepin Health43–46 | Hennepin County, Minnesota | 10,000 patients in 1 Medicaid ACO | Accountable care organization (ACO) | Low-income adults who gained coverage through Medicaid expansion | Housing, Education or employment assistance, Benefits assistance | On-site, In the field, Telephonic | Community health worker or peer coach, Physician or mid-level provider |
| Johns Hopkins Community Health Partnership47 | Baltimore, Maryland | 3000 community-based patients and 40,000 acute care patients | Health system | Adults on Medicaid and Medicare at high risk of hospitalization | Housing, Education or employment assistance, Transportation | On-site, In the field, Telephonic | Community health worker or peer coach, Physician or mid-level provider, Social worker |
| Maryland Medicaid Health Homes48,49 |
Communities in the State of Maryland | 48 health home sites | Behavioral health organization | Adult Medicaid participants with serious mental illness | Housing, Education or employment assistance, Benefits assistance, Transportation | On-site | Physician or mid-level provider |
| Medicaid Opioid Health Homes50 | Three states (Maryland, Rhode Island, and Vermont) | 10,000 patients over 3 states | Behavioral health organization | Medicaid participants with opioid use disorder | Housing, Education or employment assistance, Benefits assistance, Legal assistance, Transportation | On-site | Physician or mid-level provider |
| Medical Student Advocate Program51 | Philadelphia, Pennsylvania | 369 patients in the first 2 years | Primary care practitioner office or clinic | High-risk patients with socioeco-nomic needs | Housing, Education or employment assistance, Benefits assistance, Transportation | On-site, Telephonic | Nonpermanent volunteers |
| New York Health Homes52 | New York State | More than 100,000 individuals over 31 health home sites | Varies | Adults on Medicaid with multiple chronic health conditions, or with HIV/AIDS or serious mental illness | Housing, Benefits assistance, Other social services (not defined) | Not specified | Not specified |
| Pathways to a Healthy Bernalillo County53 | Bernalillo County, New Mexico | 13 collaborating organizations | Health system | At-risk, socially disconnected adults | Housing, Education or employment assistance, Benefits assistance, Legal assistance, Transportation | In the field | Community health worker or peer coach |
| Project Connect54 | New York, New York | 75 patients at 1 urban psychiatric emergency room | Emergency department | Patients with high emergency department utilization | Housing, Education or employment assistance, Benefits assistance | On-site, In the field | Community health worker or peer coach |
| Telephone Care Management Intervention55 | Five Denver-area counties in Colorado | 3540 patients in the intervention group and 1524 controls | Managed care organization | Adults on Medicaid who were blind or disabled | Housing, Transportation | Telephonic | Physician or mid-level provider, Care managers from diverse professions |
| Together4Health56 | Cook County, Illinois | 5000 patients in initial 3 years | Primary care practitioner office or clinic | Adults on Medicaid with multiple health conditions and chronic illnesses | Housing, Other social services (not defined) | On-site, In the field | Community health worker or peer coach, Physician or mid-level provider, Social worker |
| Transitions Clinic57 | San Francisco, California | 185 patients in initial 22 months | Primary care practitioner office or clinic | Adults recently released from jail or prison with chronic medical conditions | Housing, Education or employment assistance, Legal assistance | On-site, In the field, Telephonic | Community health worker or peer coach, Physician or mid-level provider |
| Truman Medical Centers High-Utilization Team Model58 | Kansas City, Missouri | 198 patients enrolled | Health system | Adult patients with high utilization | Housing, Benefits Assistance, Other social services (not defined) | On-site, In the field, Telephonic | Community health worker or peer coach, Physician or mid-level provider, Social worker |
| VA Homeless-Oriented Primary Care Clinic59 | Providence, Rhode Island | 177 patients enrolled | Health system, Primary care practitioner office or clinic | Homeless adult veterans | Housing, Education or employment assistance, Benefits assistance | On-site | Physician or mid-level provider |
| VA Homeless Patient Aligned Care Team60 | Communities across the United States | 18,000 patients at 58 medical facilities in 2015 | Health system, Primary care practitioner office or clinic | Homeless adult veterans | Housing, Education or employment assistance, Benefits assistance, Legal assistance, Transportation | On-site, In the field | Physician or mid-level provider, Social worker |
| Vermont Blueprint for Health61 | Communities in the State of Vermont | 60,000 patients over 3 pilot sites | Primary care practitioner office or clinic | All citizens in the state | Benefits assistance, Transportation | On site | Physician or mid-level provider |
Results include only the program details that were reported in included publications, and may omit details that were not reported.
FQHC, Federally Qualified Health Center; VA, Department of Veterans Affairs.
Of the 25 publications included in the final analysis, 16 (64%) used descriptive study designs that did not include rigorous quantitative comparisons to evaluate the impact of the program discussed. Eight of these 16 descriptive publications provided narrative descriptions of the program with limited empirical data. Four included descriptive quantitative data such as number of people served, frequency and nature of contacts and referrals, patient demographics and needs, patient health care utilization (without rigorous comparison to a control), and patient and provider experiences in the program. Three used qualitative methods, mainly interviews, to report facilitators, barriers, and other themes in program implementation, and one presented a mix of descriptive quantitative data and qualitative interview results. The remaining 9 nondescriptive publications (36%) used observational and randomized study designs to evaluate program impact. Of these, 4 used a nonrandomized pre-post design to evaluate change in outcomes over time with a focus on individual-level clinical health indicators, health care utilization, or cost of care. Three used a nonrandomized cohort design and reported measures including odds ratios for patient health events, and health care utilization rates during set time periods across intervention and comparison groups. Only 2 publications relied on a randomized design; both reported health care utilization as a primary outcome, and one reported health care cost. No publications evaluated program impact on patient socioeconomic status, or social services utilization or cost.
Care coordination program elements
Care coordination program elements are described at the program level (n = 19), rather than the publication level, as some programs were referenced in multiple publications. Publications included in this review contained varying degrees of detail regarding care coordination program implementation (Table 3). Despite variation in target population and setting, all but 2 of the 19 programs (89%) implemented a systematic process to assess patient needs. Though most programs likely conducted a systematic assessment of both medical and social needs, publications provided limited detail on specific social needs assessed or assessment tools used. Twelve programs (63%) developed individualized care plans for patients, though this element may have been underreported as publications on the remaining 7 programs contained inadequate detail to assess the extent of care planning. Ongoing patient engagement was an important element of each program, though information was lacking to assess the frequency or time span of communication with patients in most programs. Eleven programs (58%) clearly used an empowerment-based approach to patient engagement that emphasized patient self-management. According to included publications, all but 1 program (95%) used face-to-face, in-person communication to engage patients either on-site (eg, at clinics or social service offices) or in the field (eg, at home or another location in the community). Eight programs included telephonic support, such as phone calls and text messages; just 1 program was telephonic only.
Table 3.
Care Coordination Program Elements Reported in Included Studies
| Program element | N (%) of programs with dataa | Summary of resultsb |
|---|---|---|
| Care Coordination Processes | ||
| Needs Assessment | . | |
| Systematic assessment of any patient needs | 17 (89%) | 17 programs had a systematic process for evaluating medical, social, or other patient needs. The remaining 2 programs did not have adequate detail on this element. |
| Systematic assessment of social needs | 9 (47%) | 9 programs had a systematic process for evaluating patient social needs. The remaining 10 programs did not have adequate detail on this element. |
| Care Planning | ||
| Development of an individualized plan | 12 (63%) | 12 programs developed individualized care plans for patients. The remaining 7 programs did not have adequate detail on this element. |
| Patient Engagement | ||
| Emphasis on patient-centered care, empowerment, or self-management | 11 (58%) | 11 programs emphasized patient-centered care, empowerment, or self-management. The remaining 8 programs did not have adequate detail on this element. |
| Emphasis on ongoing patient support | 8 (42%) | 8 programs emphasized ongoing patient support rather than episodic or time-limited support. The remaining 11 programs did not have adequate detail on this element. |
| Frequent communication with patient | 6 (32%) | 5 programs expected care coordinators to communicate frequently (at least once per month) with each patient, and 1 required contact every 3 months. This was not discussed in adequate detail to classify many programs. |
| Mode(s) of communication with patient | 18 (95%) | On-site communication: used by 15 programs. Four relied only on on-site communication, and 11 relied on this along with other modes. |
| Field- or community-based communication: used by 11 programs. Two relied only on field-based communication (through home visiting and community-based navigators), and 9 relied on this along with other modes. | ||
| Telephonic communication (phone or text): used by 8 programs. One relied only on telephonic communication, and 7 relied on this along with other modes. | ||
| Referrals | ||
| Used “active” referrals | 10 (53%) | 9 programs used “active” referrals (eg, making appointments) rather than “passive” referrals (eg, only providing information about services). One program did not use active referrals because of reliance on large caseloads and infrequent telephonic communication. The remaining 9 programs did not have adequate detail on this element. |
| Accountability | ||
| Regular meetings of interdisciplinary team | 11 (58%) | 11 programs had regular meetings of an interdisciplinary team to coordinate care. The remaining 8 programs did not have adequate detail on this element. |
| Formal partnerships with other organizations to coordinate care | 7 (37%) | 7 programs had formal partnerships with other organizations to coordinate care (eg, Business Associate Agreements, Memoranda of Understanding, or shared governance structures). The remaining 12 programs did not have adequate detail on this element. |
| Co-location of medical and social services | 7 (37%) | 3 programs co-located medical (physical health) and social services at the same site, and 4 did not co-locate services. The remaining 12 programs did not have adequate detail on this element. |
| Emphasis on shared vision of addressing social determinants of health | 10 (53%) | 10 programs emphasized a shared vision or mission of addressing social determinants of health. The remaining 9 programs did not have adequate detail on this element. |
| Care Coordination Infrastructure | ||
| Staffing | ||
| Primary care coordination staff type | 18 (95%) | Physician or mid-level provider: primary staff for 12 programs. Four relied only on physicians or mid-level providers, and 8 relied on them along with other types of care coordination staff. |
| Community health worker or peer coach: primary staff for 9 programs. Four relied only on community health workers or peer coaches, and 5 relied on them along with other types of care coordination staff. | ||
| Social worker: primary staff for 5 programs, all of which relied on social workers along with other types of care coordination staff. | ||
| Nonpermanent volunteers: primary staff for 2 programs, both of which primarily relied on volunteers without other types of care coordination staff, but with oversight from clinical practitioners. | ||
| Specialized staff training | 14 (74%) | 14 programs provided specialized staff training related to care coordination. The remaining 5 programs did not have adequate detail on this element. |
| Care coordinator caseload | 8 (42%) | Typical caseloads: 2 programs had caseloads up to 20 patients, 2 had caseloads up to 50 patients, and 2 had caseloads up to 100 or 125 patients. This was not discussed in adequate detail to classify many programs. |
| Outlier caseloads: 2 programs had very large caseloads (800 to 20,000) that likely were calculated using a method not comparable to other programs (eg, number of potential patients in the region) | ||
| Information Sharing | ||
| Patient information shared across providers | 8 (42%) | 7 programs shared patient information across providers to support care coordination, and 1 did not because of regulatory limitations on linkage across data systems. The remaining 11 programs did not have adequate detail on this element. |
| Standard Protocols | ||
| Has specialized intervention protocols | 15 (79%) | 15 programs had specialized intervention protocols or workflows for care coordination. The remaining 4 programs did not have adequate detail on this element. |
| Financing | ||
| Specialized funding or reimbursement structure | 10 (53%) | 10 programs had a funding source or reimbursement structure specialized to support care coordination. The remaining 9 programs did not have adequate detail on this element. |
Final results consisted of 25 publications documenting 19 care coordination programs.
Programs were coded as having unavailable data for a program element if included publications did not include adequate information to classify the program as “Yes” or “No” for the element.
Results include only the program elements that were reported in included publications, and may omit elements that were not reported.
By definition, all of the 19 programs in this review referred patients to services that would address identified health and social needs. Nine programs (47%) used active referrals such as helping patients make appointments or attending appointments to provide support. One program used passive referrals and had a structure based on infrequent telephonic contact. Active referrals may be more prevalent than what was extracted from included publications, but it was not possible to ascertain the nature of referrals for many programs based on available information. To ensure implementation of care coordination elements, the majority of programs created processes to hold providers and partner organizations accountable for team-based care, such as team meetings, formal partnerships, and co-location of services. Based on included publications, 11 of the 19 programs held regular meetings of an interdisciplinary care team to coordinate care. Ten emphasized a shared vision or mission to improve social well-being for patients, 7 established formal partnerships across sectors (eg, with Business Associate Agreements or Memoranda of Understanding), and 3 co-located medical and social services in the same physical location. However, these findings likely underreport the prevalence of accountability structures because many publications provided limited detail on this topic.
For staffing, based on available information at least 8 of the 19 programs (42%) distributed responsibility for care coordination across a multidisciplinary team, often including both clinically licensed (eg, nurse) and unlicensed (eg, peer coach) staff. The remaining programs relied primarily on a single type of staff such as community health workers or registered nurses to coordinate care. Taking into account all programs, including those relying on multiple roles, 12 (63%) relied on physicians or other mid-level providers including nurses as care coordinators, 9 (47%) relied on community health workers or peer coaches who typically lacked a clinical license, 5 (26%) relied on social workers, and 2 (11%) relied on nonpermanent volunteers such as medical students. Fourteen of the 19 programs (74%) implemented specialized staff training in care coordination. Trainings included tailored orientation sessions focused on care coordination, ongoing training for staff at regular meetings, and cross-training across disciplines. Approximate care coordinator caseload was available for only 8 programs (42%), and typical caseloads varied significantly across programs, from as low as 5 to as high as 125 patients per care coordinator depending on patient acuity and program structure.
Though exchange of patient information is essential to coordinating care across providers, it was difficult to ascertain the extent of data sharing that occurred in these programs. Though most of the 19 programs reported collecting and storing patient data electronically, insufficient information was provided to determine whether and how these programs exchanged data electronically across different types of staff. The use of standardized protocols to guide care coordination was better documented, with 15 programs (79%) describing specialized intervention protocols or workflows, such as enrollment policies and procedures, distinct pathways of care designed to meet specific needs, and standards for communication across team members. Finally, 10 of the 19 programs (53%) had a specialized funding source or reimbursement structure to support care coordination processes. Financing approaches included sharing costs across insurers, implementing capitation or fixed amounts paid per person enrolled, contributions from partner organizations, grants and private foundation support, and local levy funding. Of the 10 programs with detailed information available about finances, 5 reported financial arrangements or partnership with their state's Medicaid program, highlighting the potentially important role of Medicaid in addressing social determinants of health.
Discussion
Care coordination programs that link patients to health care and social services are an essential component of efforts to address socioeconomic determinants of health outcomes, service utilization, and cost. This study reviewed 25 studies of 19 programs that coordinated health care and social services, with specific attention to implementation of 9 key elements hypothesized to affect the success of these programs (Table 1). Target populations and scope of activities varied significantly across the 19 programs studied (Table 2). For example, Berkowitz et al,47 Frank et al,56 and Miller et al37 described large-scale, complex care coordination interventions that included both clinical and community-based components. By contrast, others focused on a narrower range of target populations and settings, such as O'Toole et al's59 evaluation of a primary care-based intervention for homeless veterans and Wang et al's57 description of a clinic for patients with a history of criminal justice system involvement.
Despite this variation, 3 elements were found to be present in the majority (more than three quarters) of the 19 programs: (1) in-person communication with patients to coordinate care, (2) systematic assessment of patient needs to inform subsequent care plans and interventions, and (3) creation of standard protocols to guide care coordination processes. The research team recommends that future program planning and evaluation efforts include these 3 elements, which may be especially helpful in coordinating across health care and social services. Additional elements were underreported in included publications, making it difficult to assess their prevalence. For example, limited detail was available regarding what types of patient social needs were assessed during intake, frequency and time span of contact with patients, use of warm handoffs or other referral strategies to facilitate service uptake, types of accountability strategies, staff caseload sizes, and approaches to facilitate cross-sector information sharing. These omissions are notable as prior research has identified these factors as critical facilitators and barriers to care coordination success. The team recommends increased consideration of all 9 elements in this proposed framework during the program planning phase, as well as inclusion of information regarding these elements in future publications to guide implementation and evaluation of strategies to coordinate care.
In addition to providing sparse detail on some key care coordination elements, most of the included publications relied on narrative and descriptive methods, leaving a gap in knowledge. Only 2 publications presented results of a randomized design, 7 used a nonrandomized evaluation approach, and the remaining 16 relied on descriptive designs that did not evaluate program impact through rigorous comparisons. When quantitative outcome measures were used, they included individual-level clinical health outcomes, health care utilization, and cost of care. However, no publications evaluated program impact on patient social well-being or social services utilization and cost. Opportunity remains for research to empirically document the effect of coordinating health care and social services on health care and social services utilization, service cost, and patient health and social outcomes.
Limitations
This study was limited by factors associated with the relatively recent emergence of cross-sector care coordination including social services. Many of the publications identified provided narrative descriptions of care coordination programs, with limited or no empirical evidence, thus limiting the review to a narrative approach rather than a more structured review or meta-analysis. Publications did not always contain detailed information on important elements of care coordination implementation, resulting in probable underestimates of how many programs implemented each care coordination element that was analyzed. Even when programs and results were reported in detail, heterogeneity of reporting and program implementation made it difficult to combine all programs into one single narrative review, and some unique program details were omitted to facilitate synthesis. Finally, although this review was comprehensive for the targeted time period, it does not capture the most recent literature on care coordination that has emerged since data were collected for this article, and could be strengthened by a subsequent review.
Conclusions
Leaders and managers should consider all key elements of care coordination when developing programs that link to social services, including systematic patient needs assessment, in-person communication with patients, structured protocols to guide linkages to care, and other processes and underlying infrastructure. Future studies of coordination across health care and social services should document implementation in greater detail, addressing all elements common to care coordination programs, to facilitate comparison across programs. Additional research should consider quasi-experimental and randomized approaches to evaluate program impact on health and social outcomes. It could be beneficial to examine which specific elements of care coordination contribute most to improved outcomes for patients who have complex health and social needs. If well designed, future research can contribute to strategic and efficient coordination of health care and social services to mitigate population health challenges resulting from socioeconomic factors.
Supplementary Material
Authors' Contributions
All authors made substantial contributions to this research. Ms. Albertson made substantial contributions to the acquisition, analysis, and interpretation of data; drafted the manuscript; approved the version to be published; and agreed to be held accountable for the work. Dr. Chuang made substantial contributions to the conception and design of the work, data acquisition, and data analysis and interpretation; provided critical revisions to the manuscript; approved the version to be published; and agreed to be held accountable for the work. Ms. O'Masta made substantial contributions to the conception and design of the work, and data acquisition and analysis; provided critical revisions to the manuscript; approved the version to be published; and agreed to be held accountable for the work. Dr. Miake-Lye made substantial contributions to the conception and design of the work, and data analysis and interpretation; provided critical revisions to the manuscript; approved the version to be published; and agreed to be held accountable for the work. Ms. Haley made substantial contributions to data acquisition and analysis; provided critical revisions to the manuscript; approved the version to be published; and agreed to be held accountable for the work. Dr. Pourat made substantial contributions to the conception and design of the work and interpretation of data; provided critical revisions to the manuscript; and approved the version to be published; and agreed to be held accountable for the work.
Author Disclosure Statement
The authors declare that there are no conflicts of interest.
Funding Information
Funding for this study was provided by the California Department of Health Care Services (DHCS). The views expressed in the article are solely the opinions of the authors and do not necessarily reflect the official policies or endorsement of the DHCS. Ms. Albertson's time was supported in part by the NIH/National Center for Advancing Translational Science (NCATS) UCLA CTSI Grant Number TL1TR001883.
Supplementary Material
References
- 1. Braveman P, Gottlieb L. The social determinants of health: It's time to consider the causes of the causes. Public Health Rep 2014;129(1_suppl2):19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Knighton AJ, Stephenson B, Savitz LA. Measuring the effect of social determinants on patient outcomes: a systematic literature review. J Health Care Poor Underserved 2018;29:81–106. [DOI] [PubMed] [Google Scholar]
- 3. Hood CM, Gennuso KP, Swain GR, Catlin BB. County health rankings: relationships between determinant factors and health outcomes. Am J Prev Med 2016;50:129–135. [DOI] [PubMed] [Google Scholar]
- 4. Woolf SH. Progress in achieving health equity requires attention to root causes. Health Aff 2017;36:984–991. [DOI] [PubMed] [Google Scholar]
- 5. Woolf SH. Necessary but not sufficient: why health care alone cannot improve population health and reduce health inequities. Ann Fam Med 2019;17:196–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gottlieb LM, Garcia K, Wing H, Manchanda R. Clinical interventions addressing nonmedical health determinants in Medicaid managed care. Am J Manag Care 2016;22:370–376. [PubMed] [Google Scholar]
- 7. Gottlieb LM, Wing H, Adler NE. A systematic review of interventions on patients' social and economic needs. Am J Prev Med 2017;53:719–729. [DOI] [PubMed] [Google Scholar]
- 8. Horwitz LI, Chang C, Arcilla HN, Knickman JR. Quantifying health systems' investment in social determinants of health, by sector, 2017–19. Health Aff 2020;39:192–198. [DOI] [PubMed] [Google Scholar]
- 9. Gorin SS, Haggstrom D, Han PKJ, Fairfield KM, Krebs P, Clauser SB. Cancer care coordination: a systematic review and meta-analysis of over 30 years of empirical studies. Ann Behav Med 2017;51:532–546. [DOI] [PubMed] [Google Scholar]
- 10. Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ 2003;327:1219–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Agency for Healthcare Research and Quality. Care coordination. 2018. https://www.ahrq.gov/ncepcr/care/coordination.html Accessed November 21, 2020.
- 12. Schultz EM, McDonald KM. What is care coordination? Int J Care Coord 2014;17:5–24. [Google Scholar]
- 13. De Regge M, De Pourcq K, Meijboom B, Trybou J, Mortier E, Eeckloo K. The role of hospitals in bridging the care continuum: a systematic review of coordination of care and follow-up for adults with chronic conditions. BMC Health Serv Res 2017;17:550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Horvitz-Lennon M, Kilbourne AM, Pincus HA. From silos to bridges: meeting the general health care needs of adults with severe mental illnesses. Health Aff 2006;25:659–669. [DOI] [PubMed] [Google Scholar]
- 15. Ingersoll S, Valente SM, Roper J. Nurse care coordination for diabetes: a literature review and synthesis. J Nurs Care Qual 2005;20:208–214. [DOI] [PubMed] [Google Scholar]
- 16. Katz EB, Carrier ER, Umscheid CA, Pines JM. Comparative effectiveness of care coordination interventions in the emergency department: a systematic review. Ann Emerg Med 2012;60:12–23.e1. [DOI] [PubMed] [Google Scholar]
- 17. Overholser L, Callaway C. Improving care coordination to optimize health outcomes in cancer survivors. J Natl Compr Canc Netw 2019;17:607–610. [DOI] [PubMed] [Google Scholar]
- 18. Tomasone JR, Brouwers MC, Vukmirovic M, et al. Interventions to improve care coordination between primary healthcare and oncology care providers: a systematic review. ESMO Open 2016;1:e000077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tricco AC, Antony J, Ivers NM, et al. Effectiveness of quality improvement strategies for coordination of care to reduce use of health care services: a systematic review and meta-analysis. CMAJ 2014;186:E568–E578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fichtenberg C, Delva J, Minyard K, Gottlieb LM. Health and human services integration: generating sustained health and equity improvements. Health Aff 2020;39:567–573. [DOI] [PubMed] [Google Scholar]
- 21. Petchel S, Gelmon S, Goldberg B. The organizational risks of cross-sector partnerships: a comparison of health and human services perspectives. Health Aff 2020;39:574–581. [DOI] [PubMed] [Google Scholar]
- 22. Chuang E, O'Masta B, Albertson EM, Haley LA, Lu C, Pourat N. Whole person care improves care coordination for many Californians. UCLA Center for Health Policy Research. 2019. https://healthpolicy.ucla.edu/publications/Documents/PDF/2019/wholepersoncare-policybrief-sep2019.pdf Accessed November 21, 2020.
- 23. Peterson K, Anderson J, Bourne D, et al. Health care coordination theoretical frameworks: a systematic scoping review to increase their understanding and use in practice. J Gen Intern Med 2019;34:90–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Schultz EM, Pineda N, Lonhart J, Davies SM, McDonald KM. A systematic review of the care coordination measurement landscape. BMC Health Serv Res 2013;13:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sherry M, Wolff JL, Ballreich J, DuGoff E, Davis K, Anderson G. Bridging the silos of service delivery for high-need, high-cost individuals. Popul Health Manag 2016;19:421–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Shier G, Ginsburg M, Howell J, Volland P, Golden R. Strong social support services, such as transportation and help for caregivers, can lead to lower health care use and costs. Health Aff 2013;32:544–551. [DOI] [PubMed] [Google Scholar]
- 27. Weaver SJ, Che XX, Petersen LA, Hysong SJ. Unpacking care coordination through a multiteam system lens: a conceptual framework and systematic review. Med Care 2018;56:247–259. [DOI] [PubMed] [Google Scholar]
- 28. Agency for Healthcare Research and Quality. Care coordination measures atlas update, chapter 3. Care coordination measurement framework. 2014. https://www.ahrq.gov/ncepcr/care/coordination/atlas/chapter3.html Accessed November 21, 2020.
- 29. Schor EL. Ten essential characteristics of care coordination. JAMA Pediatr 2019;173:5–5. [DOI] [PubMed] [Google Scholar]
- 30. Brown RS, Peikes D, Peterson G, Schore J, Razafindrakoto CM. Six features of Medicare coordinated care demonstration programs that cut hospital admissions of high-risk patients. Health Aff 2012;31:1156–1166. [DOI] [PubMed] [Google Scholar]
- 31. Carter MW, Wu H, Cohen S, Hightow-Weidman L, Lecher SL, Peters PJ. Linkage and referral to HIV and other medical and social services: a focused literature review for sexually transmitted disease prevention and control programs. Sex Transm Dis 2016;43(2 Suppl 1):S76–S82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Press MJ, Michelow MD, MacPhail LH. Care coordination in accountable care organizations: moving beyond structure and incentives. Am J Accountable Care 2012;18:778–780. [PubMed] [Google Scholar]
- 33. Friedman A, Howard J, Shaw EK, Cohen DJ, Shahidi L, Ferrante JM. Facilitators and barriers to care coordination in patient-centered medical homes (PCMHs) from coordinators' perspectives. J Am Board Fam Med 2016;29:90–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Quinn A, Ji P, Nackerud L. Predictors of secondary traumatic stress among social workers: supervision, income, and caseload size. J Social Work 2019;19:504–528. [Google Scholar]
- 35. Reamer FG. Ethical issues in integrated health care: implications for social workers. Health Soc Work 2018;43:118–124. [DOI] [PubMed] [Google Scholar]
- 36. Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Miller A, Cunningham M, Ali N. Bending the cost curve and improving quality of care in America's poorest city. Popul Health Manag 2013;16(S1):S-17. [DOI] [PubMed] [Google Scholar]
- 38. Redding S, Conrey E, Porter K, Paulson J, Hughes K, Redding M. Pathways community care coordination in low birth weight prevention. Matern Child Health J 2015;19:643–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lin MP, Blanchfield BB, Kakoza RM, et al. ED-based care coordination reduces costs for frequent ED users. Am J Manag Care 2017;23:762–766. [PubMed] [Google Scholar]
- 40. Berkowitz SA, Hulberg AC, Hong C, et al. Addressing basic resource needs to improve primary care quality: a community collaboration programme. BMJ Qual Saf 2016;25:164–172. [DOI] [PubMed] [Google Scholar]
- 41. Berkowitz SA, Hulberg AC, Standish S, Reznor G, Atlas SJ. Addressing unmet basic resource needs as part of chronic cardiometabolic disease management. JAMA Intern Med 2017;177:244–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Onie RD, Lavizzo-Mourey R, Lee TH, Marks JS, Perla RJ. Integrating social needs into health care: a twenty-year case study of adaptation and diffusion. Health Aff 2018;37:240–247. [DOI] [PubMed] [Google Scholar]
- 43. Blewett LA, Owen RA. Accountable care for the poor and underserved: Minnesota's Hennepin health model. Am J Public Health 2015;105:622–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Sandberg SF, Erikson C, Owen R, et al. Hennepin health: a safety-net accountable care organization for the expanded Medicaid population. Health Aff 2014;33:1975–1984. [DOI] [PubMed] [Google Scholar]
- 45. Vickery KD, Shippee ND, Menk J, et al. Integrated, accountable care for Medicaid expansion enrollees: a comparative evaluation of Hennepin health. Med Care Res Rev 2018;77:46–59. [DOI] [PubMed] [Google Scholar]
- 46. Vickery KD, Shippee ND, Guzman-Corrales LM, et al. Changes in quality of life among enrollees in Hennepin health: a Medicaid expansion ACO. Med Care Res Rev 2018;77:60–73. [DOI] [PubMed] [Google Scholar]
- 47. Berkowitz SA, Brown P, Brotman DJ, et al. Case study: Johns Hopkins community health partnership: a model for transformation. Healthcare 2016;4:264–270. [DOI] [PubMed] [Google Scholar]
- 48. Kennedy-Hendricks A, Daumit GL, Choksy S, Linden S, McGinty EE. Measuring variation across dimensions of integrated care: The Maryland Medicaid health home model. Adm Policy Ment Health 2018;45:888–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. McGinty EE, Kennedy-Hendricks A, Linden S, Choksy S, Stone E, Daumit GL. An innovative model to coordinate healthcare and social services for people with serious mental illness: A mixed-methods case study of Maryland's Medicaid health home program. Gen Hosp Psychiatry 2018;51:54–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Clemans-Cope L, Wishner JB, Allen EH, Lallemand N, Epstein M, Spillman BC. Experiences of three states implementing the Medicaid health home model to address opioid use disorder—case studies in Maryland, Rhode Island, and Vermont. J Subst Abuse Treat 2017;83:27–35. [DOI] [PubMed] [Google Scholar]
- 51. Onyekere C, Ross S, Namba A, Ross JC, Mann BD. Medical student volunteerism addresses patients' social needs: a novel approach to patient-centered care. Ochsner J 2016;16:45–49. [PMC free article] [PubMed] [Google Scholar]
- 52. Castillo EG, Pincus HA, Smith TE, Miller G, Fish DG. New York state Medicaid reforms: opportunities and challenges to improve the health of those with serious mental illness. J Health Care Poor Underserved 2017;28:839–852. [DOI] [PubMed] [Google Scholar]
- 53. Page-Reeves J, Moffett ML, Steimel L, Smith DT. The evolution of an innovative community-engaged health navigator program to address social determinants of health. Prog Community Health Partnersh 2016;10:603–610. [DOI] [PubMed] [Google Scholar]
- 54. Nossel IR, Lee RJ, Isaacs A, Herman DB, Marcus SM, Essock SM. Use of peer staff in a critical time intervention for frequent users of a psychiatric emergency room. Psychiatr Serv 2016;67:479–481. [DOI] [PubMed] [Google Scholar]
- 55. Kim SE, Michalopoulos C, Kwong RM, Warren A, Manno MS. Telephone care management's effectiveness in coordinating care for Medicaid beneficiaries in managed care: a randomized controlled study. Health Serv Res 2013;48:1730–1749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Frank RG, Riedel L, Barry CL. Together4Health: integrating care for vulnerable populations. Am J Psychiatr Rehabil 2015;18:105–127. [Google Scholar]
- 57. Wang EA, Hong CS, Samuels L, Shavit S, Sanders R, Kushel M. Transitions clinic: creating a community-based model of health care for recently released California prisoners. Public Health Rep 2010;125. https://journals.sagepub.com/doi/pdf/10.1177/003335491012500205 Accessed April 24, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Roberts SR, Crigler J, Ramirez C, Sisco D, Early GL. Working with socially and medically complex patients: when care transitions are circular, overlapping, and continual rather than linear and finite. J Healthc Qual 2015;37:245–265. [DOI] [PubMed] [Google Scholar]
- 59. O'Toole TP, Buckel L, Bourgault C, et al. Applying the chronic care model to homeless veterans: effect of a population approach to primary care on utilization and clinical outcomes. Am J Public Health 2010;100:2493–2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. O'Toole TP, Johnson EE, Aiello R, Kane V, Pape L. Tailoring care to vulnerable populations by incorporating social determinants of health: the Veterans health administration's “homeless patient aligned care team” program. Prev Chronic Dis 2016;13:E44–E44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Bielaszka-DuVernay C. Vermont's blueprint for medical homes, community health teams, and better health at lower cost. Health Aff 2011;30:383–386. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.