ABSTRACT
Background
Data on renal replacement therapy (RRT) for end-stage renal disease were collected by the European Renal Association (ERA) Registry via national and regional renal registries in Europe and countries bordering the Mediterranean Sea. This article provides a summary of the 2019 ERA Registry Annual Report, including data from 34 countries and additional age comparisons.
Methods
Individual patient data for 2019 were provided by 35 registries and aggregated data by 17 registries. Using these data, the incidence and prevalence of RRT, the kidney transplantation activity and the survival probabilities were calculated.
Results
In 2019, a general population of 680.8 million people was covered by the ERA Registry. Overall, the incidence of RRT was 132 per million population (p.m.p.). Of these patients, 62% were men, 54% were ≥65 years of age and 21% had diabetes mellitus as primary renal disease (PRD), and 84% had haemodialysis (HD), 11% had peritoneal dialysis (PD) and 5% had pre-emptive kidney transplantation as an initial treatment modality. The overall prevalence of RRT on 31 December 2019 was 893 p.m.p., with 58% of patients on HD, 5% on PD and 37% living with a kidney transplant. The overall kidney transplant rate was 35 p.m.p. and 29% of the kidney grafts were from a living donor. The unadjusted 5-year survival probability was 42.3% for patients commencing dialysis, 86.6% for recipients of deceased donor grafts and 94.4% for recipients of living donor grafts in the period 2010–14. When comparing age categories, there were substantial differences in the distribution of PRD, treatment modality and kidney donor type, and in the survival probabilities.
Keywords: dialysis, epidemiology, ESRD, graft survival, kidney transplantation, patient survival
INTRODUCTION
This article provides a summary of the European Renal Association (ERA) Registry's 2019 Annual Report (Supplementary data), which presents the latest data on the epidemiology of renal replacement therapy (RRT) for end-stage renal disease (ESRD) in Europe and countries bordering the Mediterranean Sea. Data were provided to the ERA Registry by a total of 52 national or regional registries from 34 countries; 35 registries provided individual patient data and 17 renal registries provided aggregated data (Appendix 1). Compared with the 2018 Annual Report, this year data from Poland could be included, while data from Bulgaria could not be included. In addition, this year for the first time, individual patient data from the Spanish region La Rioja were included. The coverage of the general population was 680.3 million people for the incidence calculations and 680.8 million people for the prevalence calculations, the discrepancy resulting from a difference in coverage of the general population in the Netherlands. When excluding Israel, the remaining countries cover a general population of 672 million people, representing 78.0% of the 2019 European general population. This coverage is higher than the 74.2% covered in the 2018 Annual Report [1].
The 2019 incidence and prevalence of RRT, kidney transplantation activity and both patient and graft survival in Europe are presented in this article. In addition, this year's annual report contains additional age comparisons that are also presented in this article. Further details on the methodology used for analysis, as well as the complete results, can be found in the ERA Registry 2019 Annual Report (Supplementary data).
RESULTS
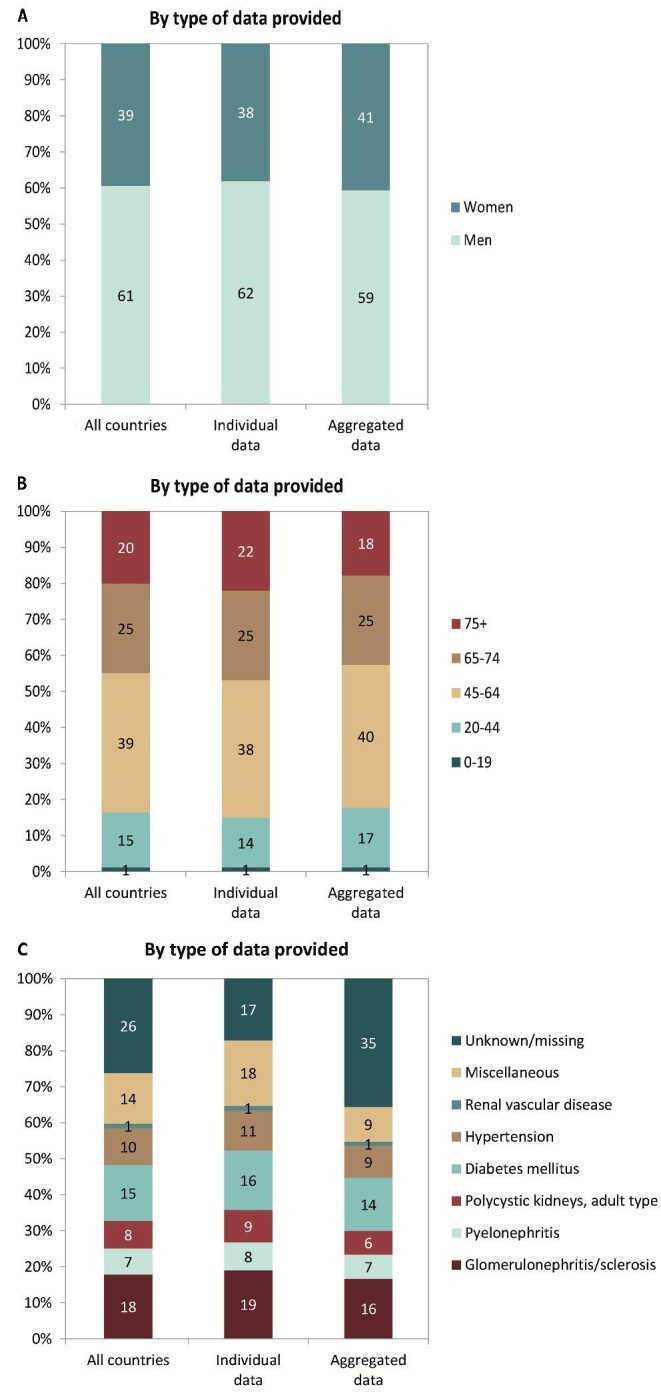
Incidence of RRT
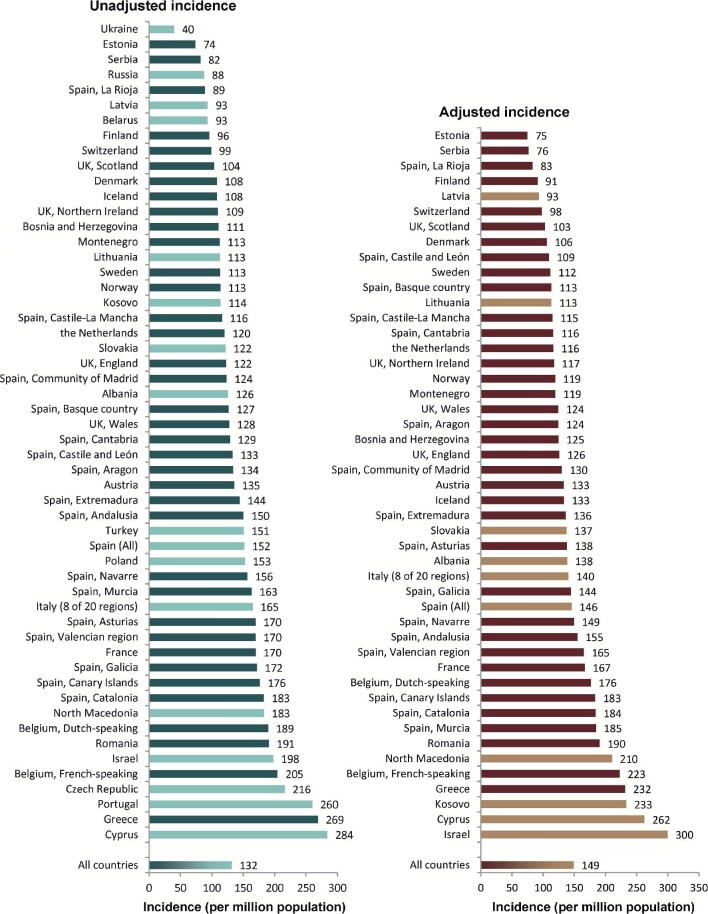
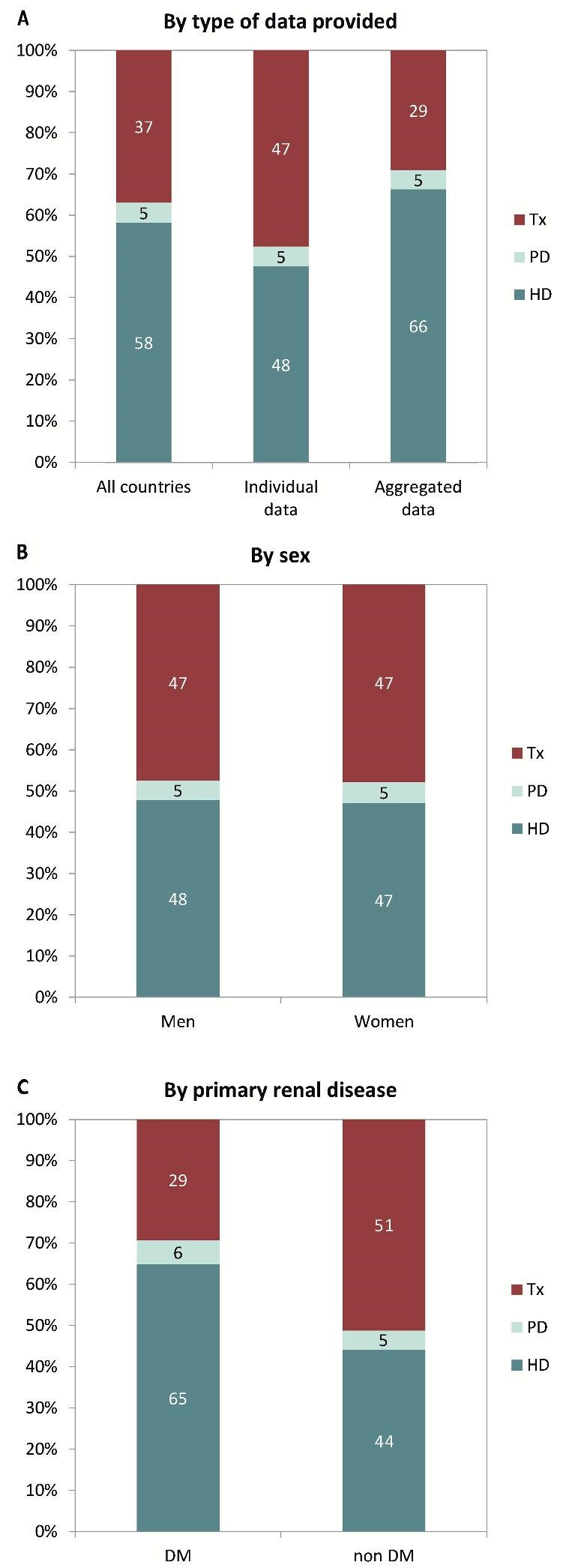
In 2019, 89 579 individuals out of a population of 680.3 million people initiated RRT for ESRD, corresponding to around 1 per every 7500 Europeans [132 per million population (p.m.p.); Table 1]. The unadjusted incidence ranged from around 1 per 25 000 inhabitants (40 p.m.p.) in Ukraine and 1 per 13 500 inhabitants (74 p.m.p.) in Estonia to around 1 per 3500 inhabitants (269 p.m.p. and 284 p.m.p.) in Greece and Cyprus (Table 1 and Figures 1 and 2). The adjusted incidence rate [standardized to the age and sex distribution of the European Union 28 (EU-28) countries’ population in 2015] [2] was available for 27 countries and ranged between 1 per 13 500 inhabitants (75 p.m.p.) in Estonia and 1 per 3500 inhabitants (300 p.m.p.) in Israel (Figure 2). For patients with diabetes mellitus (DM) as primary renal disease (PRD), the unadjusted incidence of RRT was 28 p.m.p, ranging from 8 and 10 p.m.p. in Iceland and Ukraine, respectively, to 92 and 120 p.m.p. in Israel and Cyprus, respectively (Table 1). The median age of patients starting RRT was 67.9 years, but this differed by 20 years between Ukraine (54.0 years) and Greece (74.4 years; Table 1). Of the total group of patients commencing RRT, 62% were men, 54% were aged ≥65 years and 21% had DM as PRD (Figure 3). When initiating RRT, the majority (84%) of patients started on haemodialysis (HD), 11% started on peritoneal dialysis (PD) and 5% of patients received a pre-emptive kidney transplant (Figure 4). The distribution of initial treatment modalities was similar for men and women (Figure 4). Patients with DM as PRD more often started RRT on HD compared with those without DM (86% versus 80%) and less frequently received a pre-emptive kidney transplant (2% versus 6%). On Day 91 after the start of RRT, 82% of incident patients were receiving HD, 13% were receiving PD and 5% were living with a functioning kidney transplant (Figure 5).
Table 1.
Incidence of RRT (as count and p.m.p.) in 2019 on Day 1, by country or region, unadjusted and the mean and median age at the start of RRT and the incidence of RRT for patients with DM as primary renal disease (as count and p.m.p.)
| Incidence of RRT in 2019, at Day 1 | |||||||
|---|---|---|---|---|---|---|---|
| Country/region | General population covered by the registry in thousands | All (n) | All (p.m.p.) | Mean age (years) | Median age (years) | DM (n) | DM (p.m.p.) |
| Albania | 2833 | 356 | 126 | 60.0 | 62.5 | 73 | 26 |
| Austriaa | 8859 | 1200 | 135 | 65.5 | 68.9 | 284 | 32 |
| Belarusb | 9466 | 883 | 93 | 187 | 20 | ||
| Belgium, Dutch-speakingc | 6618 | 1254 | 189 | 70.6 | 73.5 | 234 | 35 |
| Belgium, French-speakingc | 4871 | 997 | 205 | 67.3 | 69.4 | 227 | 47 |
| Bosnia and Herzegovina | 3531 | 391 | 111 | 63.5 | 64.9 | 114 | 32 |
| Cyprus | 888 | 252 | 284 | 69.0 | 73.0 | 107 | 120 |
| Czech Republicd | 10 480 | 2267 | 216 | ||||
| Denmark | 5871 | 634 | 108 | 62.0 | 66.1 | 168 | 29 |
| Estonia | 1327 | 98 | 74 | 59.2 | 62.8 | 21 | 16 |
| Finland | 5522 | 530 | 96 | 62.2 | 66.0 | 158 | 29 |
| France | 67 249 | 11 417 | 170 | 67.8 | 70.6 | 2674 | 40 |
| Greece | 10 722 | 2883 | 269 | 71.7 | 74.4 | 749 | 70 |
| Iceland | 361 | 39 | 108 | 63.1 | 66.3 | 3 | 8 |
| Israel | 9053 | 1790 | 198 | 66.1 | 69.4 | 836 | 92 |
| Italy (8 of 20 regions) | 22 431 | 3703 | 165 | 69.5 | 72.3 | 568 | 25 |
| Kosovo | 1688 | 192 | 114 | 59.5 | 61.5 | 71 | 42 |
| Latvia | 1297 | 121 | 93 | 62.1 | 65.0 | 32 | 25 |
| Lithuania | 2794 | 315 | 113 | 65.1 | 64.0 | 62 | 22 |
| Montenegroc | 622 | 70 | 113 | 61.3 | 64.7 | 17 | 27 |
| North Macedonia | 2076 | 380 | 183 | 64.9 | 66.0 | 94 | 45 |
| Norway | 5348 | 606 | 113 | 63.7 | 68.0 | 113 | 21 |
| Poland | 38 383 | 5865 | 153 | 1840 | 48 | ||
| Portugale | 10 277 | 2673 | 260 | 872 | 85 | ||
| Romania | 19 100 | 3643 | 191 | 62.9 | 65.0 | 432 | 23 |
| Russiad | 143 814 | 12 602 | 88 | 2837 | 20 | ||
| Serbia | 6251 | 511 | 82 | 61.8 | 64.8 | 130 | 21 |
| Slovakiad | 4644 | 566 | 122 | 64.2 | 66.0 | 174 | 37 |
| Spain (All) | 47 026 | 7133 | 152 | 63.4 | 67.9 | 1740 | 37 |
| Spain, Andalusia | 8453 | 1272 | 150 | 63.9 | 66.9 | 344 | 41 |
| Spain, Aragon | 1325 | 177 | 134 | 65.2 | 68.9 | 49 | 37 |
| Spain, Asturias | 1021 | 173 | 170 | 68.0 | 69.0 | 44 | 43 |
| Spain, Basque country | 2184 | 277 | 127 | 64.6 | 68.4 | 66 | 30 |
| Spain, Canary Islands | 2222 | 392 | 176 | 64.7 | 67.0 | 128 | 58 |
| Spain, Cantabriac | 582 | 75 | 129 | 66.1 | 67.9 | 20 | 34 |
| Spain, Castile and Leónc | 2400 | 319 | 133 | 68.1 | 69.9 | 85 | 35 |
| Spain, Castile-La Manchac | 2040 | 237 | 116 | 66.4 | 69.4 | 73 | 36 |
| Spain, Catalonia | 7675 | 1403 | 183 | 65.9 | 69.5 | 236 | 31 |
| Spain, Community of Madrid | 6663 | 823 | 124 | 64.4 | 67.4 | 215 | 32 |
| Spain, Extremadura | 1068 | 154 | 144 | 65.2 | 67.0 | 37 | 35 |
| Spain, Galicia | 2702 | 464 | 172 | 65.7 | 67.8 | 125 | 46 |
| Spain, La Rioja | 315 | 28 | 89 | 66.7 | 72.1 | 9 | 29 |
| Spain, Murcia | 1494 | 244 | 163 | 65.5 | 68.9 | 61 | 41 |
| Spain, Navarrec | 653 | 102 | 156 | 68.4 | 71.5 | 24 | 37 |
| Spain, Valencian region | 5004 | 849 | 170 | 66.2 | 69.0 | 194 | 39 |
| Sweden | 10 279 | 1164 | 113 | 64.0 | 68.1 | 271 | 26 |
| Switzerland | 8575 | 848 | 99 | 66.1 | 69.3 | 171 | 20 |
| The Netherlands | 16 131 | 1939 | 120 | 63.7 | 67.2 | 363 | 23 |
| Turkeyf | 83 155 | 12 518 | 151 | 560 | 56 | ||
| UK, England | 56 287 | 6889 | 122 | 61.1 | 64.1 | 1815 | 32 |
| UK, Northern Ireland | 1894 | 207 | 109 | 61.0 | 63.0 | 42 | 22 |
| UK, Scotland | 5463 | 566 | 104 | 58.3 | 60.8 | 166 | 30 |
| UK, Wales | 3153 | 402 | 128 | 62.0 | 65.4 | 144 | 46 |
| Ukraineb | 41 984 | 1675 | 40 | 52.9 | 54.0 | 399 | 10 |
| All countries | 680 322 | 89 579 | 132 | 64.9 | 67.9 | 18 748 | 28 |
When cells are left empty, the data are unavailable and could not be used for the calculation of the summary data.
The incidence is underestimated by approximately 1% due to one haemodialysis centre not submitting data.
Patients younger than 18 years of age are not reported.
Patients younger than 20 years of age are not reported: the true incidence counts are therefore slightly higher than the counts reported here.
Data include dialysis patients only.
Data on the incidence of primary renal disease are available for dialysis patients only (98.8%, total n = 2673).
Data on the incidence of primary renal disease (DM) is based on 1498 dialysis patients (12.0% of total).
RRT, renal replacement therapy; DM, diabetes mellitus as primary renal disease.
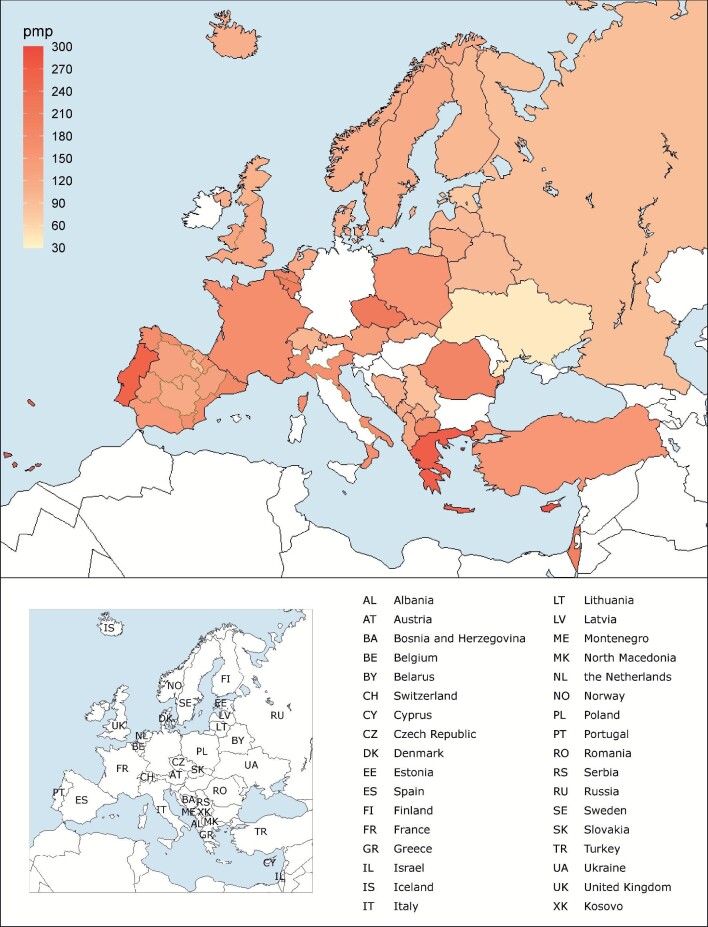
FIGURE 1:
Incidence of RRT (p.m.p.) in 2019, on Day 1, by country or region, unadjusted. The incidence for Czech Republic, Russia and Slovakia only includes patients receiving dialysis.
FIGURE 2:
Unadjusted (left panel) and adjusted (right panel) incidence of RRT p.m.p. in 2019, on Day 1, by country or region. Registries providing individual patient data are shown as dark-coloured bars and registries providing aggregated data as light-coloured bars. Age- and sex-adjusted incidence was calculated by standardization to the age and sex distribution of the EU-28 population. The incidence for Czech Republic, Russia and Slovakia only includes patients receiving dialysis.
FIGURE 3:
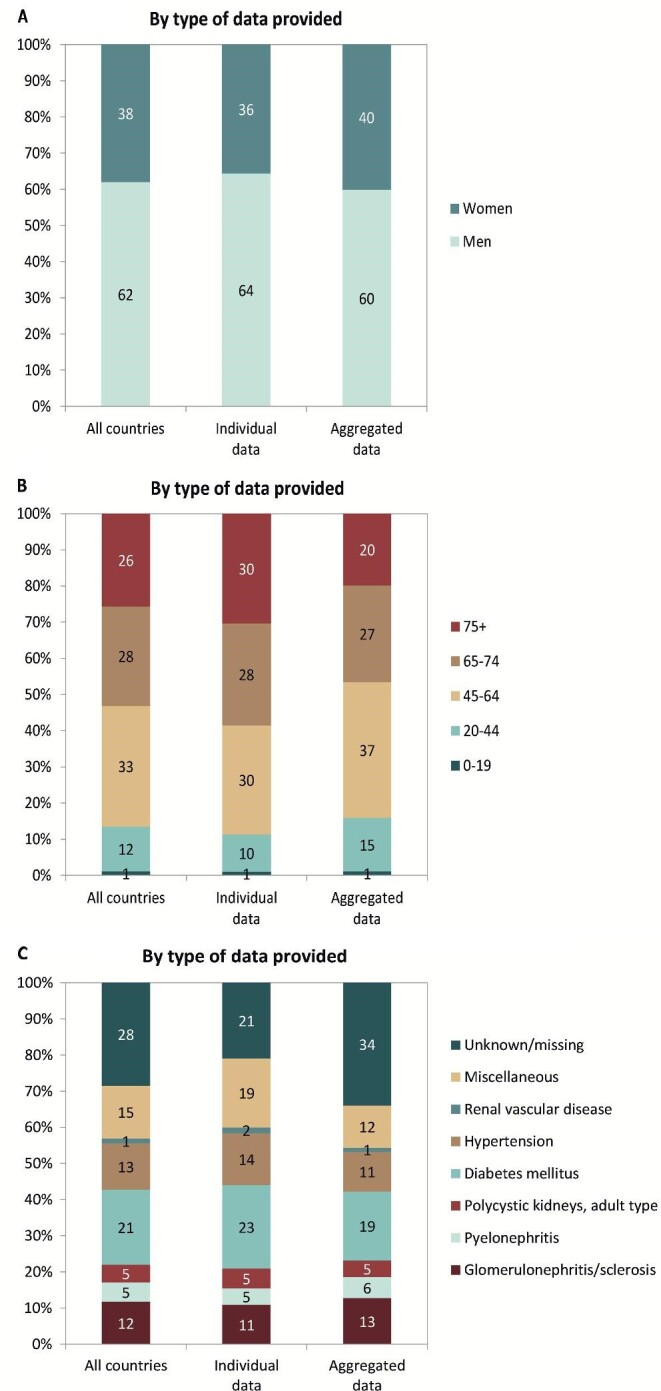
(A) Sex, (B) age and (C) primary renal disease distribution by type of data provided for incident patients accepted for RRT in 2019, on Day 1. See Appendix 1 for a list of countries and regions providing individual patient data or aggregated data.
FIGURE 4:
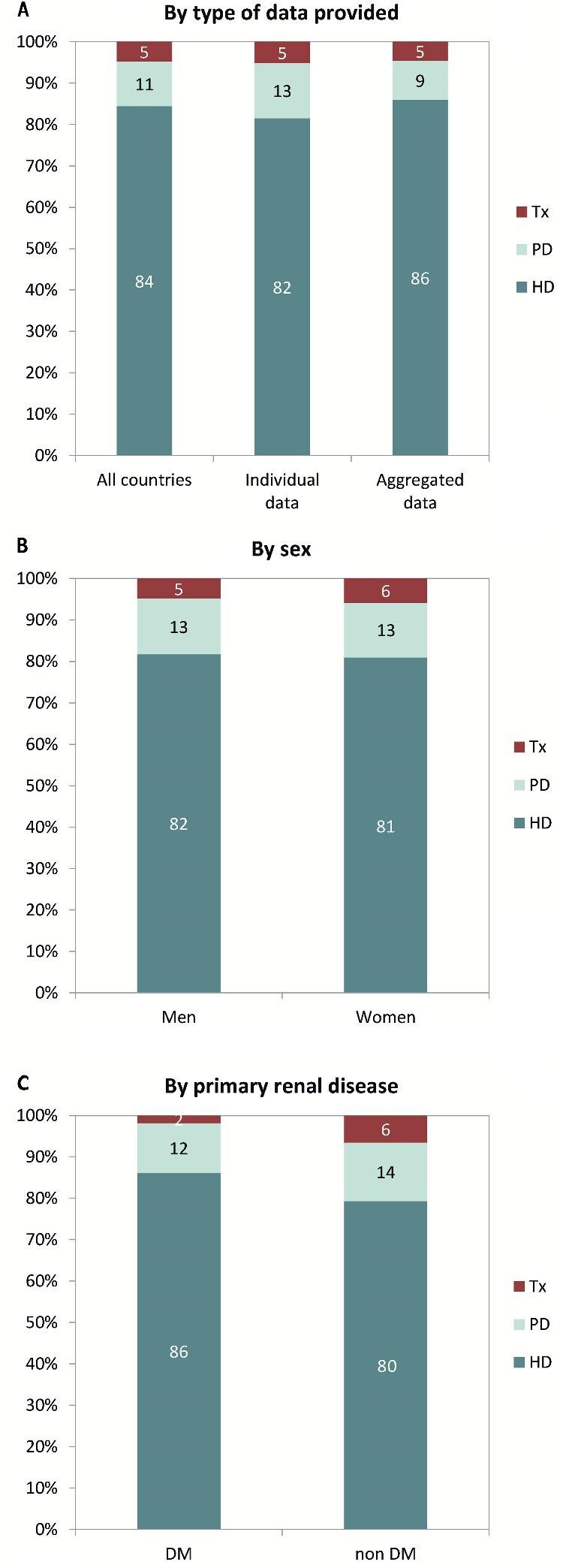
Treatment modality distribution, on Day 1, by (A) type of data provided, (B) sex and (C) primary renal disease (DM and non-DM) for incident patients accepted for RRT in 2019. Panels (B) and (C) are only based on the data from registries providing individual patient data. See Appendix 1 for a list of countries and regions providing individual patient data or aggregated data. DM, diabetes mellitus; HD, haemodialysis; PD, peritoneal dialysis; Tx, kidney transplant.
FIGURE 5:
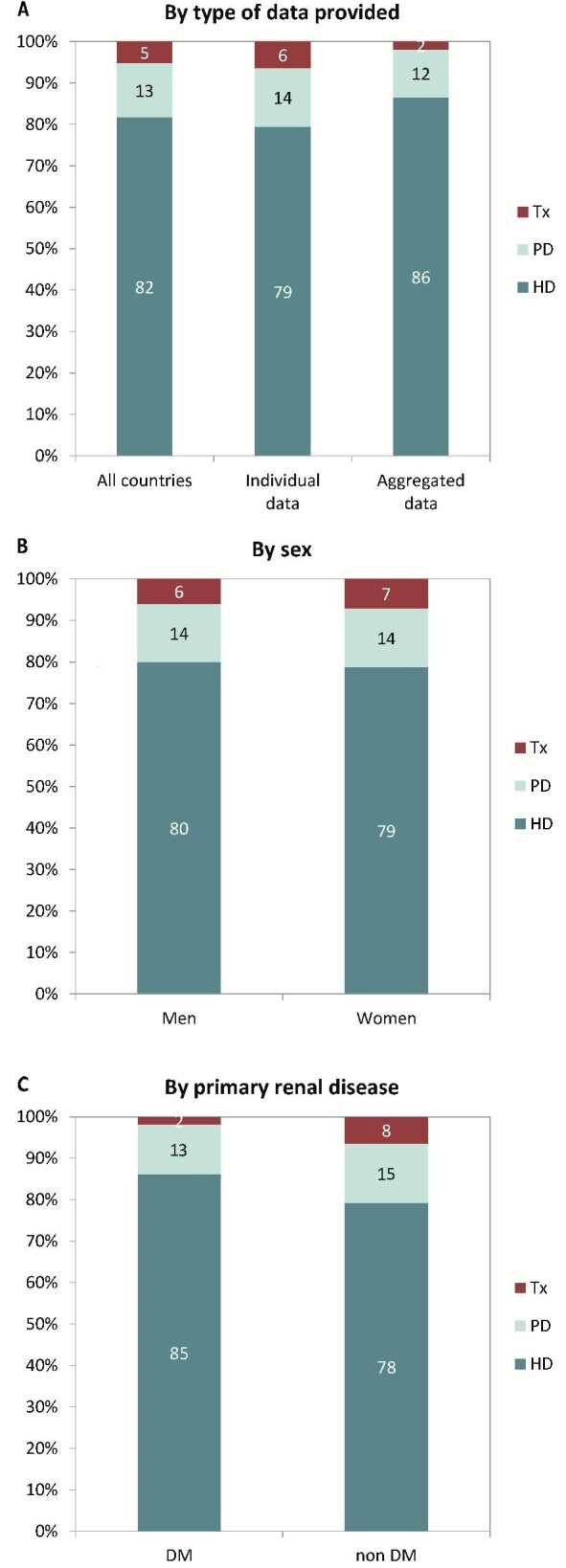
Treatment modality distribution, on Day 91, by (A) type of data provided, (B) sex and (C) primary renal disease (DM and non-DM) for incident patients accepted for RRT in 2019. Parts (B) and (C) are only based on the data from registries providing individual patient data. See Appendix 1 for a list of countries and regions providing individual patient data or aggregated data. DM, diabetes mellitus; HD, haemodialysis; PD, peritoneal dialysis; Tx, kidney transplant.
Prevalence of RRT
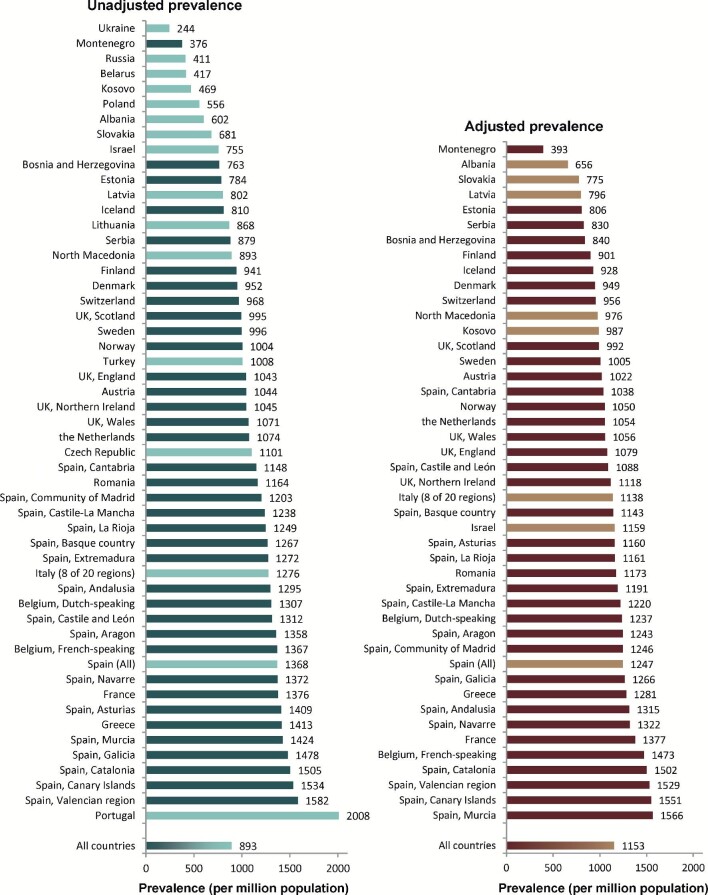
On 31 December 2019, 607 320 patients were receiving RRT for ESRD, corresponding to around 1 per every 1000 Europeans (893 p.m.p.; Table 2). Within individual countries or regions, the unadjusted prevalence ranged from 1 per 4000 inhabitants (244 p.m.p.) in Ukraine and 1 per 2500 inhabitants (376 p.m.p.) in Montenegro to 1 per 650 inhabitants (1582 p.m.p.) in the Valencian region (Spain) and 1 per 500 inhabitants (2008 p.m.p.) in Portugal (Table 2 and Figures 6 and 7). The adjusted prevalence rate was available for 25 countries and ranged from 1 per 2500 inhabitants (393 p.m.p.) in Montenegro to 1 per 650 inhabitants (1566 p.m.p.) in Murcia (Spain; Figure 7). The prevalence of patients with DM as PRD was 154 p.m.p. and ranged from 38 p.m.p. in Ukraine to 425 p.m.p. in Canary Islands (Spain). Prevalent patients receiving RRT had a median age of 60.5 years, which ranged from 53.0 years in Albania to 69.0 years in Israel (Table 2). Among the prevalent patients, 61% were men, 45% were aged ≥65 years and 15% had DM as PRD (Figure 8). Furthermore, 58% of the prevalent patients were receiving HD, while 5% were receiving PD and a further 37% were living with a kidney transplant (Figure 9). Patients with DM as PRD were less likely to be living with a functioning kidney transplant compared with patients with a PRD other than DM (29% versus 51%).
Table 2.
Prevalence of RRT (as count and p.m.p.) on 31 December 2019, by country or region, unadjusted and the mean and median age on 31 December 2019 and the prevalence of RRT for patients DM as primary renal disease (as count and p.m.p.)
| Prevalent patients on RRT in 2019 | |||||||
|---|---|---|---|---|---|---|---|
| Country/region | General population covered by the registry in thousands | All (n) | All (p.m.p.) | Mean age (years) | Median age (years) | DM (n) | DM (p.m.p.) |
| Albania | 2833 | 1706 | 602 | 51.9 | 53.0 | 352 | 124 |
| Austriaa | 8859 | 9250 | 1044 | 62.4 | 63.7 | 1407 | 159 |
| Belarusb | 9466 | 3948 | 417 | 515 | 54 | ||
| Belgium, Dutch-speakingc | 6618 | 8648 | 1307 | 66.6 | 68.5 | 1431 | 216 |
| Belgium, French-speakingc | 4871 | 6658 | 1367 | 65.3 | 67.0 | 1194 | 245 |
| Bosnia and Herzegovina | 3531 | 2695 | 763 | 60.2 | 62.0 | 543 | 154 |
| Cyprus | 888 | ||||||
| Czech Republic | 10 480 | 11 543 | 1101 | ||||
| Denmark | 5871 | 5591 | 952 | 59.1 | 60.5 | 943 | 161 |
| Estonia | 1327 | 1040 | 784 | 58.8 | 59.5 | 195 | 147 |
| Finland | 5522 | 5198 | 941 | 59.9 | 62.4 | 1300 | 235 |
| France | 67 249 | 92 512 | 1376 | 63.4 | 65.5 | 15 299 | 227 |
| Greece | 10 722 | 15 153 | 1413 | 65.8 | 68.0 | 2903 | 271 |
| Iceland | 361 | 292 | 810 | 57.4 | 58.8 | 32 | 89 |
| Israeld | 9053 | 6839 | 755 | 67.0 | 69.0 | 3239 | 358 |
| Italy (8 of 20 regions) | 22 431 | 28 622 | 1276 | 63.3 | 65.4 | 2992 | 133 |
| Kosovo | 1688 | 792 | 469 | 60.1 | 61.0 | 248 | 147 |
| Latvia | 1297 | 1040 | 802 | 56.1 | 58.0 | 119 | 92 |
| Lithuania | 2794 | 2424 | 868 | ||||
| Montenegroc | 622 | 234 | 376 | 58.5 | 60.5 | 41 | 66 |
| North Macedonia | 2076 | 1853 | 893 | 59.8 | 61.0 | 329 | 158 |
| Norway | 5348 | 5369 | 1004 | 60.2 | 62.5 | 746 | 139 |
| Polandd | 38 383 | 21 339 | 556 | 6211 | 162 | ||
| Portugale,f | 10 277 | 20 640 | 2008 | 67.5 | 3694 | 359 | |
| Romania | 19 100 | 22 236 | 1164 | 63.2 | 65.0 | 2222 | 116 |
| Russia | 143 814 | 59 106 | 411 | 10 752 | 75 | ||
| Serbia | 6251 | 5495 | 879 | 60.5 | 62.9 | 956 | 153 |
| Slovakiad | 4644 | 3161 | 681 | 64.7 | 67.0 | 904 | 195 |
| Spain (All) | 47 026 | 64 311 | 1368 | 60.7 | 64.0 | 10 566 | 225 |
| Spain, Andalusia | 8453 | 10 943 | 1295 | 61.2 | 62.5 | 1793 | 212 |
| Spain, Aragon | 1325 | 1800 | 1358 | 64.4 | 66.1 | 322 | 243 |
| Spain, Asturias | 1021 | 1438 | 1409 | 64.4 | 65.6 | 255 | 250 |
| Spain, Basque country | 2184 | 2767 | 1267 | 62.2 | 64.4 | 342 | 157 |
| Spain, Canary Islands | 2222 | 3409 | 1534 | 62.5 | 63.6 | 944 | 425 |
| Spain, Cantabriac | 582 | 668 | 1148 | 63.3 | 64.8 | 102 | 175 |
| Spain, Castile and Leónc | 2400 | 3149 | 1312 | 65.5 | 66.5 | 552 | 230 |
| Spain, Castile-La Manchac | 2040 | 2526 | 1238 | 63.6 | 64.5 | 424 | 208 |
| Spain, Catalonia | 7675 | 11 551 | 1505 | 63.4 | 65.1 | 1630 | 212 |
| Spain, Community of Madrid | 6663 | 8017 | 1203 | 62.5 | 63.9 | 1439 | 216 |
| Spain, Extremadura | 1068 | 1358 | 1272 | 62.7 | 63.2 | 213 | 199 |
| Spain, Galicia | 2702 | 3994 | 1478 | 63.5 | 64.9 | 699 | 259 |
| Spain, La Rioja | 315 | 393 | 1249 | 62.4 | 64.7 | 47 | 149 |
| Spain, Murcia | 1494 | 2128 | 1424 | 62.6 | 63.7 | 320 | 214 |
| Spain, Navarre c | 653 | 896 | 1372 | 63.8 | 65.7 | 138 | 211 |
| Spain, Valencian region | 5004 | 7914 | 1582 | 63.8 | 65.8 | 1160 | 232 |
| Sweden | 10 279 | 10 240 | 996 | 60.3 | 62.4 | 1786 | 174 |
| Switzerland | 8575 | 8298 | 968 | 62.8 | 64.7 | 1259 | 147 |
| The Netherlands | 16 651 | 17 886 | 1074 | 61.1 | 63.1 | 2386 | 143 |
| Turkeyg | 83 155 | 83 783 | 1008 | 2381 | 371 | ||
| UK, England | 56 287 | 58 406 | 1043 | 58.2 | 59.3 | 10 242 | 183 |
| UK, Northern Ireland | 1894 | 1966 | 1045 | 58.2 | 59.0 | 282 | 150 |
| UK, Scotland | 5463 | 5435 | 995 | 57.2 | 58.5 | 942 | 172 |
| UK, Wales | 3153 | 3361 | 1071 | 58.9 | 60.5 | 607 | 193 |
| Ukraineb | 41 984 | 10 250 | 244 | 53.4 | 55.0 | 1614 | 38 |
| All countries | 680 842 | 607 320 | 893 | 61.8 | 60.5 | 90 633 | 154 |
When cells are left empty, the data are unavailable and could not be used for the calculation of the summary data.
The prevalence is underestimated by approximately 1% due to one haemodialysis centre not submitting data.
Patients younger than 18 years of age are not reported.
Patients younger than 20 years of age are not reported. The true prevalent counts are therefore slightly higher than the counts reported here.
Data on prevalence include dialysis patients only.
Data on mean age include dialysis patients only.
Data on primary renal disease are available for dialysis patients only (64.8%, total n = 20 640).
Data on the prevalence of primary renal disease (DM) is based on 6460 dialysis patients (7.6% of total).
RRT, renal replacement therapy; DM, diabetes mellitus as primary renal disease.
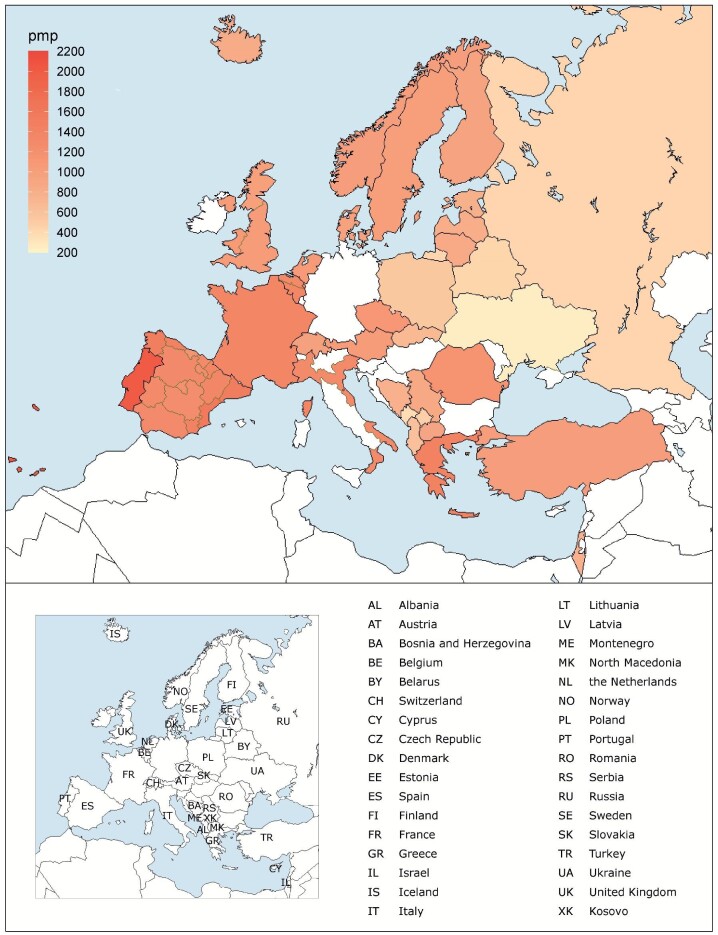
FIGURE 6:
Prevalence of RRT (p.m.p.) on 31 December 2019 by country or region. The prevalence for Israel, Poland and Slovakia only includes patients receiving dialysis.
FIGURE 7:
Unadjusted (left panel) and adjusted (right panel) prevalence (p.m.p.) of RRT on 31 December 2019 by country or region. Registries providing individual patient data are shown as dark-coloured bars and registries providing aggregated data as light-coloured bars. Age- and sex-adjusted prevalence was calculated by standardization to the age and sex distribution of the EU-28 population. The prevalence for Israel, Poland and Slovakia only includes patients receiving dialysis.
FIGURE 8:
(A) Sex, (B) age and (C) primary renal disease distribution, by type of data provided for prevalent patients on RRT on 31 December 2019. See Appendix 1 for a list of countries and regions providing individual patient data or aggregated data.
FIGURE 9:
Treatment modality distribution by (A) type of data provided, (B) sex and (C) primary renal disease (DM and non-DM) for prevalent patients on RRT on 31 December 2019. Parts (B) and (C) are only based on the data from registries providing individual patient data. See Appendix 1 for a list of countries and regions providing individual patient data or aggregated data. DM, diabetes mellitus; HD, haemodialysis; PD, peritoneal dialysis; Tx, kidney transplant.
Kidney transplantation
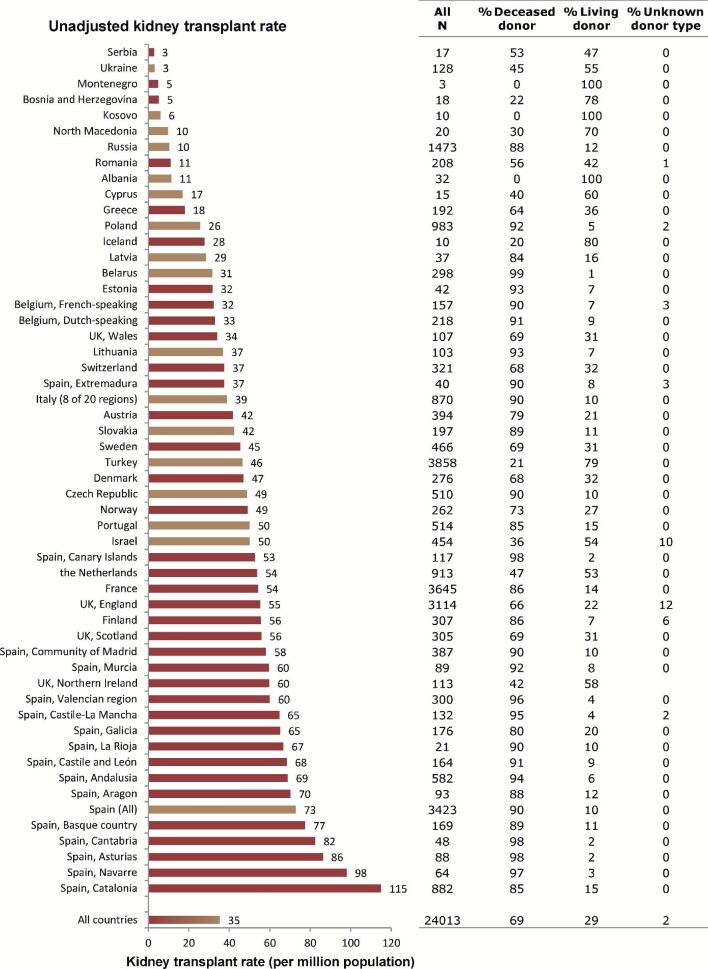
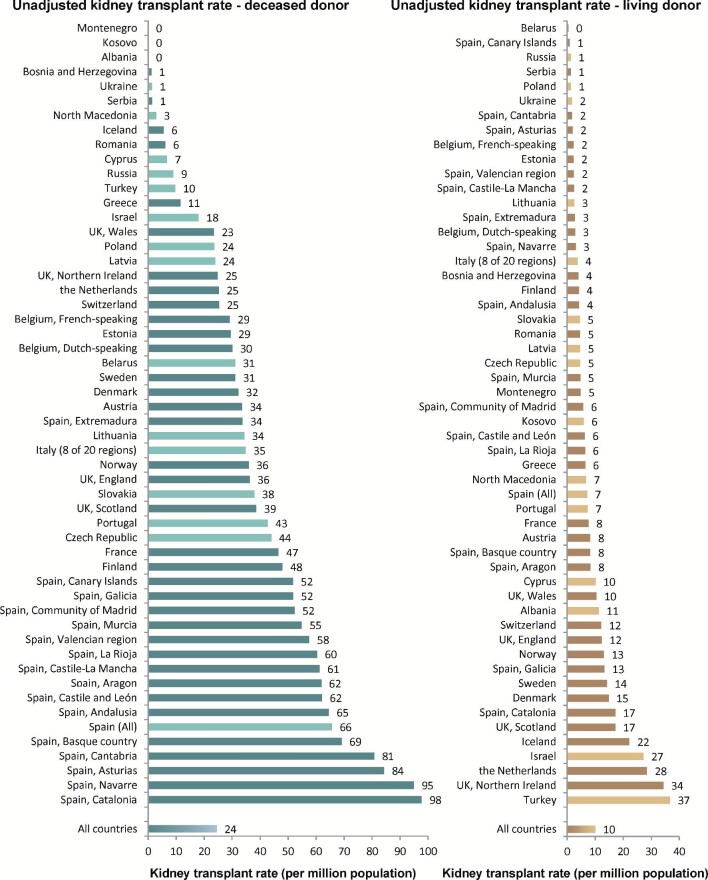
A total of 24 013 kidney transplantations were carried out in 2019, resulting in an overall unadjusted transplant rate of around 1 per 28 500 Europeans (35 p.m.p.; Figure 10). In the individual countries or regions, the unadjusted kidney transplant rates ranged from 1 per 350 000 inhabitants (3 p.m.p.) in Serbia and Ukraine to 1 per 10 000 inhabitants (98 p.m.p.) in Navarre (Spain) and 1 per 8500 inhabitants (115 p.m.p.) in Catalonia (Spain). Altogether, the unadjusted deceased donor kidney transplant rate was more than twice that of living donor transplants (69% versus 29%; 24 p.m.p. versus 10 p.m.p.; Figures 11 and 12). The highest unadjusted rates of deceased donor kidney transplants were found in some Spanish regions [more than 1 per 12 500 inhabitants (>80 p.m.p.); Figure 12], while the highest unadjusted rates of living donor transplants were observed in Northern Ireland [1 per 29 500 inhabitants (34 p.m.p.)] and Turkey [1 per 27 000 inhabitants (37 p.m.p.); Figure 12].
FIGURE 10:
Kidney transplants performed in 2019, presented as counts and p.m.p., by country or region, unadjusted. Registries providing individual patient data are shown as red-coloured bars and registries providing aggregated data as orange-coloured bars. The total count for Austria is based on residents and non-residents. For Romania, Serbia and the Netherlands, the overall kidney transplant rate is underestimated by 30%, 15% and 2%, respectively.
FIGURE 11:
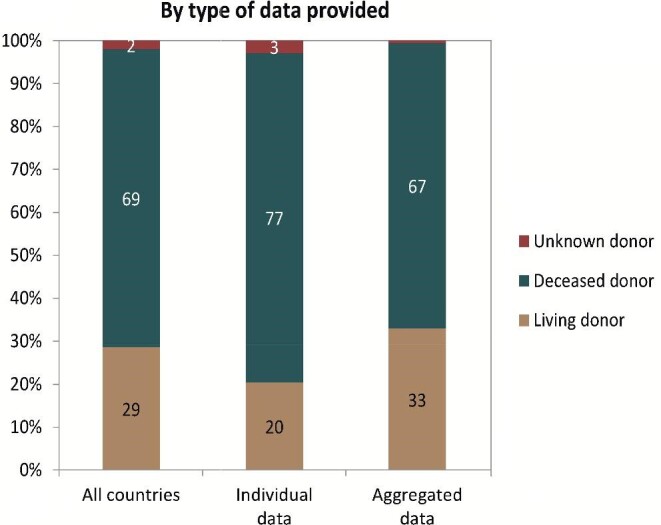
Donor-type distribution for kidney transplants performed in 2019, by type of data provided. See Appendix 1 for a list of countries and regions providing individual patient data or aggregated data.
FIGURE 12:
Deceased donor (left panel) and living donor (right panel) kidney transplants performed in 2019 p.m.p., by country or region, unadjusted. Registries providing individual patient data are shown as dark-coloured bars and registries providing aggregated data as light-coloured bars. The total count for Austria is based on residents and non-residents. For Romania and the Netherlands, the kidney transplant rate is underestimated by 30% and 2%, respectively. For Serbia, the transplant rate is underestimated by 16% for deceased donor transplants and by 12% for living donor transplants.
Survival of patients receiving RRT
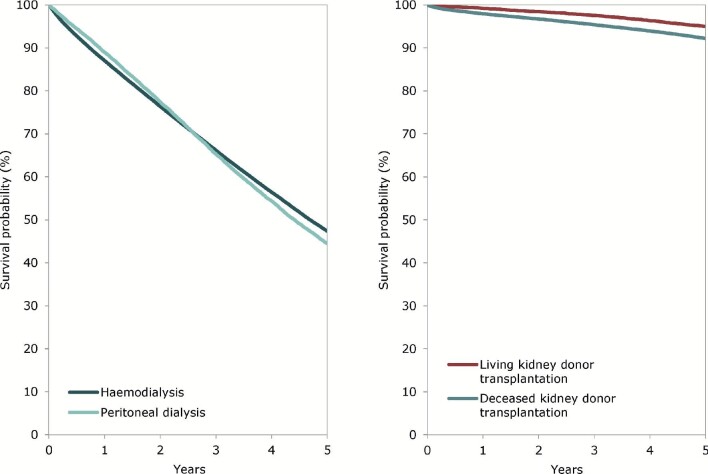
During the period 2010–14, the 5-year unadjusted patient survival probability for patients commencing RRT was 51.9% [95% confidence interval (95% CI) 51.6–52.1 Table 3]. Patients starting RRT on dialysis in this period had an observed unadjusted 5-year patient survival probability of 42.3% (95% CI 42.1–42.6). Higher survival probabilities in the first 2 years for those receiving PD were identified through an adjusted analysis focusing on HD and PD (Figure 13). Among patients receiving a kidney transplant in the period 2010–14, living donor transplant recipients experienced a higher adjusted 5-year patient survival than recipients of deceased donor transplants, 95.1% (95% CI 94.7–95.6) versus 92.3% (95% CI 92.0–92.6; Figure 13 and Table 3). Living donor transplant recipients also had a higher adjusted 5-year graft survival compared with deceased donor transplants, 87.9% (95% CI 87.3–88.5) versus 81.6% (95% CI 81.2–82.0; Table 3). A description of the adjustments made and the countries and regions included in these analyses can be found in Table 3.
Table 3.
Survival probabilities at 1, 2 and 5 years by treatment modality and cohort, from Day 1 of the start of RRT or dialysis, or from the day of first kidney transplantation
| Survival probabilities as percentage (95% CIs) | |||||
|---|---|---|---|---|---|
| Cohort 2010–14 | Cohort 2013–17 | ||||
| Survival type | 1 year | 2 years | 5 years | 1 year | 2 years |
| Patient survival on RRT | |||||
| Unadjusted | 84.5 (84.4–84.7) | 74.5 (74.3–74.8) | 51.9 (51.6–52.1) | 85.6 (85.4–85.7) | 76.0 (75.8–76.2) |
| Adjusteda | 87.3 (87.2–87.5) | 78.2 (78.0–78.4) | 54.1 (53.8–54.3) | 88.1 (87.9–88.2) | 79.3 (79.1–79.5) |
| Patient survival on dialysis | |||||
| Unadjusted | 83.5 (83.3–83.6) | 72.0 (71.8–72.2) | 42.3 (42.1–42.6) | 84.5 (84.3–84.7) | 73.4 (73.2–73.6) |
| Adjusteda | 85.7 (85.6–85.9) | 75.5 (75.2–75.7) | 47.4 (47.1–47.7) | 86.9 (86.7–87.1) | 77.1 (76.9–77.3) |
| Patient survival after first kidney transplantation (deceased donor) | |||||
| Unadjusted | 96.2 (96.0–96.4) | 94.0 (93.8–94.3) | 86.6 (86.3–87.0) | 96.3 (96.1–96.5) | 94.2 (94.0–94.5) |
| Adjustedb | 98.0 (97.8–98.1) | 96.7 (96.6–96.9) | 92.3 (92.0–92.6) | 98.0 (97.9–98.2) | 96.9 (96.7–97.1) |
| Graft survival after first kidney transplantation (deceased donor) | |||||
| Unadjusted | 90.7 (90.4–91.0) | 87.6 (87.3–88.0) | 77.7 (77.3–78.1) | 91.3 (91.0–91.6) | 88.3 (88.0–88.6) |
| Adjustedb | 92.6 (92.3–92.9) | 90.0 (89.7–90.4) | 81.6 (81.2–82.0) | 93.2 (92.9–93.4) | 90.7 (90.4–91.0) |
| Patient survival after first kidney transplantation (living donor) | |||||
| Unadjusted | 99.1 (98.9–99.2) | 98.1 (97.9–98.4) | 94.4 (93.9–94.8) | 98.9 (98.7–99.0) | 98.1 (97.8–98.3) |
| Adjustedb | 99.2 (99.1–99.4) | 98.4 (98.2–98.7) | 95.1 (94.7–95.6) | 99.1 (98.9–99.2) | 98.4 (98.2–98.7) |
| Graft survival after first kidney transplantation (living donor) | |||||
| Unadjusted | 96.8 (96.4–97.1) | 95.1 (94.6–95.4) | 88.6 (88.0–89.1) | 96.7 (96.4–97.0) | 95.3 (94.9–95.7) |
| Adjustedb | 96.6 (96.2–96.9) | 94.8 (94.3–95.2) | 87.9 (87.3–88.5) | 96.5 (96.2–96.8) | 95.0 (94.6–95.4) |
The findings are based on data from the following renal registries providing individual patient data: Austria, Belgium (Dutch-speaking), Belgium (French-speaking), Bosnia and Herzegovina, Denmark, Finland, France, Greece, Iceland, Norway, Spain (Andalusia), Spain (Aragon), Spain (Asturias), Spain (Basque country), Spain (Cantabria), Spain (Castile and León), Spain (Castile-La Mancha), Spain (Catalonia), Spain (Community of Madrid), Spain (Extremadura), Spain (Galicia), Spain (Murcia), Spain (Valencian Region), Sweden, the Netherlands, the UK (England/Northern Ireland/Wales) and the UK (Scotland).
Unadjusted survival probabilities were calculated using the Kaplan–Meier method, and adjusted survival probabilities using the Cox regression model.
Analyses were adjusted using fixed values: age (67 years), sex (63% men) and primary renal disease (24% diabetes mellitus, 19% hypertension/renal vascular disease, 11% glomerulonephritis and 46% other causes).
Analyses were adjusted using fixed values: age (50 years), sex (63% men) and primary renal disease (14% diabetes mellitus, 10% hypertension/renal vascular disease, 23% glomerulonephritis and 53% other causes).
FIGURE 13:
Survival of patients starting HD and PD between 2010 and 2014 from Day 91 (left panel) and patients receiving a first kidney transplant from a living or deceased donor between 2010 and 2014 (right panel). Survival on dialysis was censored for kidney transplantation and adjusted using fixed values for age (67 years), sex (63% men) and primary renal disease (24% diabetes mellitus, 19% hypertension/renal vascular disease, 11% glomerulonephritis and 46% other causes). Survival after kidney transplantation was adjusted using fixed values for age (50 years), sex (63% men) and primary renal disease (14% diabetes mellitus, 10% hypertension/renal vascular disease, 23% glomerulonephritis and 53% other causes). These figures are based on the data from the following registries providing individual patient data: Austria, Belgium (Dutch-speaking), Belgium (French-speaking), Bosnia and Herzegovina, Denmark, Finland, France, Greece, Iceland, Norway, Spain (Andalusia), Spain (Aragon), Spain (Asturias), Spain (Basque country), Spain (Cantabria), Spain (Castile and León), Spain (Castile-La Mancha), Spain (Catalonia), Spain (Community of Madrid), Spain (Extremadura), Spain (Galicia), Spain (Murcia), Spain (Valencian Region), Sweden, the Netherlands, the UK (England/Northern Ireland/Wales) and the UK (Scotland).
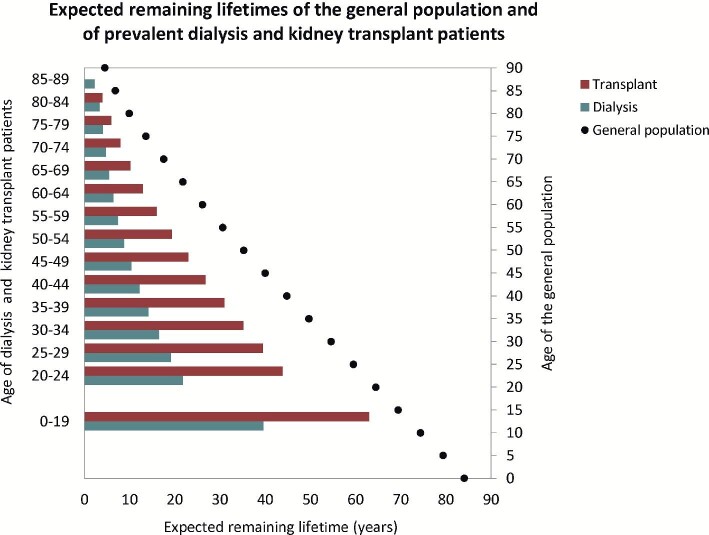
Expected remaining lifetime
Based on data from the period 2015 to 2019, patients receiving dialysis are expected to live only around half of the estimated remaining lifetime of patients living with a functioning kidney transplant (Figure 14). The life expectancy of patients on dialysis was about 70% shorter than that in the general population. For kidney transplant recipients, life expectancy was approximately 40% shorter than that of the general population.
FIGURE 14:
Expected remaining lifetime of prevalent dialysis and kidney transplant patients (cohort 2015–19) and the general population (cohort 2015–19), by age. This figure is based on data from the following registries providing individual patient data: Austria, Belgium (Dutch-speaking), Belgium (French-speaking), Bosnia and Herzegovina, Denmark, Finland, France, Greece, Iceland, Norway, Spain (Andalusia), Spain (Aragon), Spain (Asturias), Spain (Basque country), Spain (Cantabria), Spain (Castille and León), Spain (Castille-La Mancha), Spain (Catalonia), Spain (Community of Madrid), Spain (Extremadura), Spain (Galicia), Spain (Murcia), Spain (Valencian Region), Sweden, the Netherlands, the UK (England/Northern Ireland/Wales) and the UK (Scotland).
Age comparisons
Figures 15–21 show the comparisons of age groups using data from 35 national or regional renal registries in 18 countries providing individual patient data. In 2019, the incidence of RRT ranged from around 1 per 170 000 persons aged 0–19 years [6 per million age-related population (p.m.a.r.p.)] to around 1 per 1900 persons aged ≥75 years (539 p.m.a.r.p.; Figure 15). The proportion of women was higher in patients aged 0–19 years (43%) than in older age groups (34–38%). In addition, there were considerable differences in the PRD distribution (Figure 16). Especially in the youngest age category, a high proportion of patients with ESRD due to miscellaneous causes was observed, likely resulting from hereditary and congenital diseases being included in this PRD category (Appendix 2). On the other hand, the proportion of patients with DM or hypertension as PRD increased with age. In addition, the distribution of initial treatment modalities differed between age groups, with decreasing proportions of patients receiving either PD or a pre-emptive transplant with advancing age (Figure 16).
FIGURE 15:
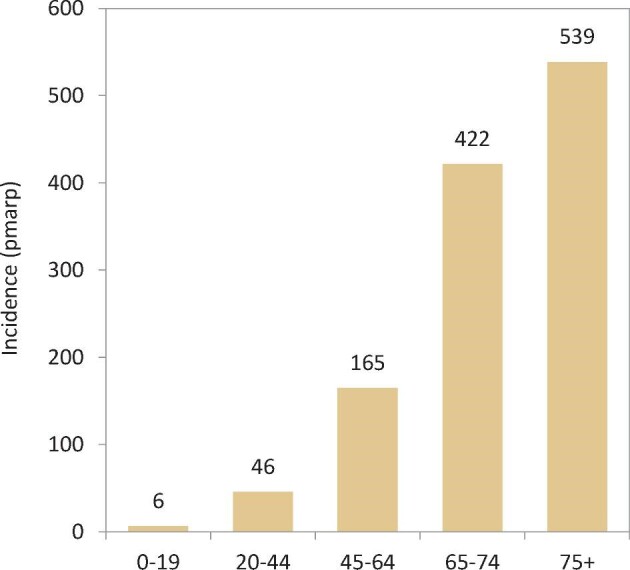
Incidence of RRT per million age-related population (p.m.a.r.p.) in 2019, on Day 1, by age, unadjusted. Results are based on data from registries providing individual patient data.
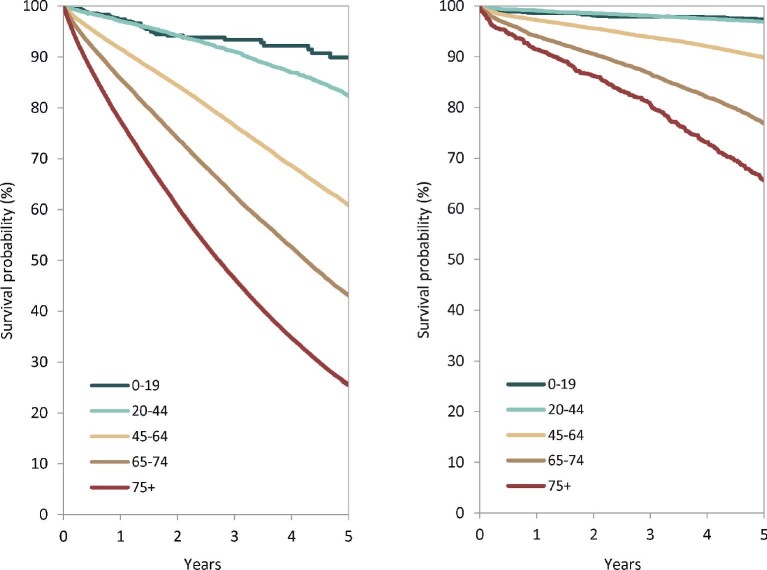
FIGURE 21:
Patient survival probability by age for incident dialysis patients from Day 91 (left panel) and for patients receiving a first kidney transplant from the day of transplantation (right panel), adjusted for sex and primary renal disease. Results are based on data from registries providing individual patient data.
FIGURE 16:
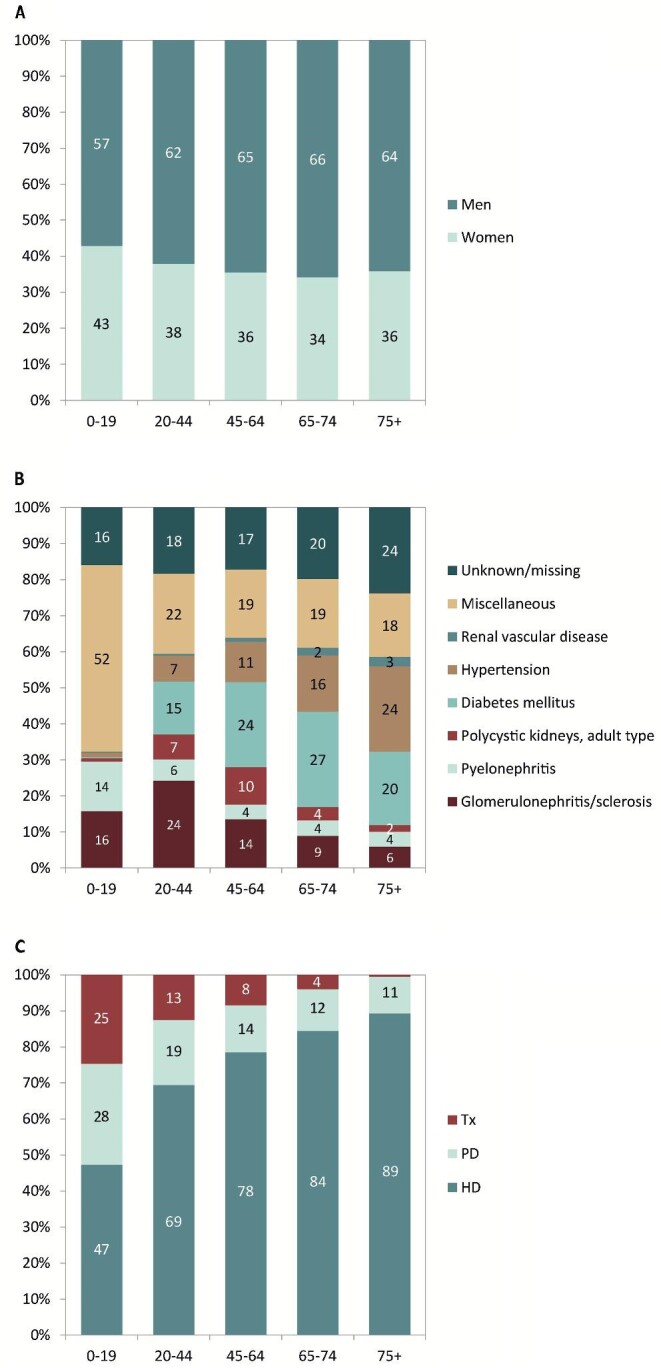
(A) Sex, (B) primary renal disease and (C) treatment modality distribution by age in incident patients accepted for RRT in 2019, on Day 1, unadjusted. Results are based on data from registries providing individual patient data. HD, haemodialysis; PD, peritoneal dialysis; Tx, kidney transplant.
On 31 December 2019, the unadjusted prevalence of RRT ranged from around 1 per 19 000 persons aged 0–19 years (53 p.m.a.r.p.) to 1 per 300 persons aged ≥75 years (3154 p.m.a.r.p.; Figure 17). The distribution of men and women was similar among all age groups, with approximately 38% being women (Figure 18). A total of 60% of RRT patients aged 0–19 years had miscellaneous PRD (Figure 18). The distribution of treatment modalities differed largely between age groups, with 78% of patients aged 0–19 years living with a functioning kidney graft compared with 18% of patients aged ≥75 years (Figure 18).
FIGURE 17:
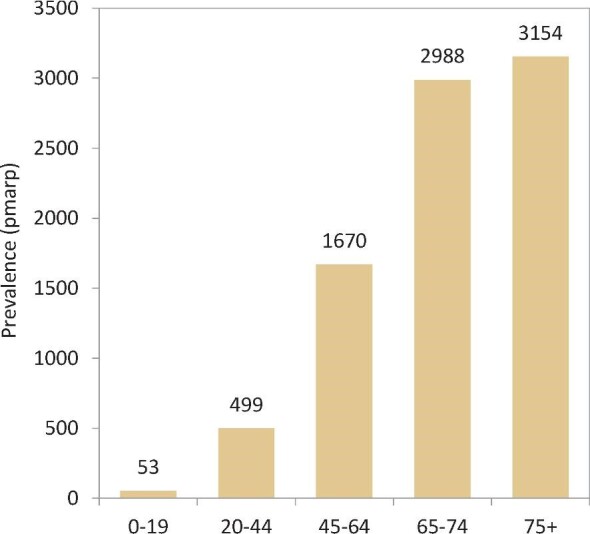
Prevalence of RRT per million age-related population (p.m.a.r.p.) on 31 December 2019, by age, unadjusted. Results are based on data from registries providing individual patient data.
FIGURE 18:
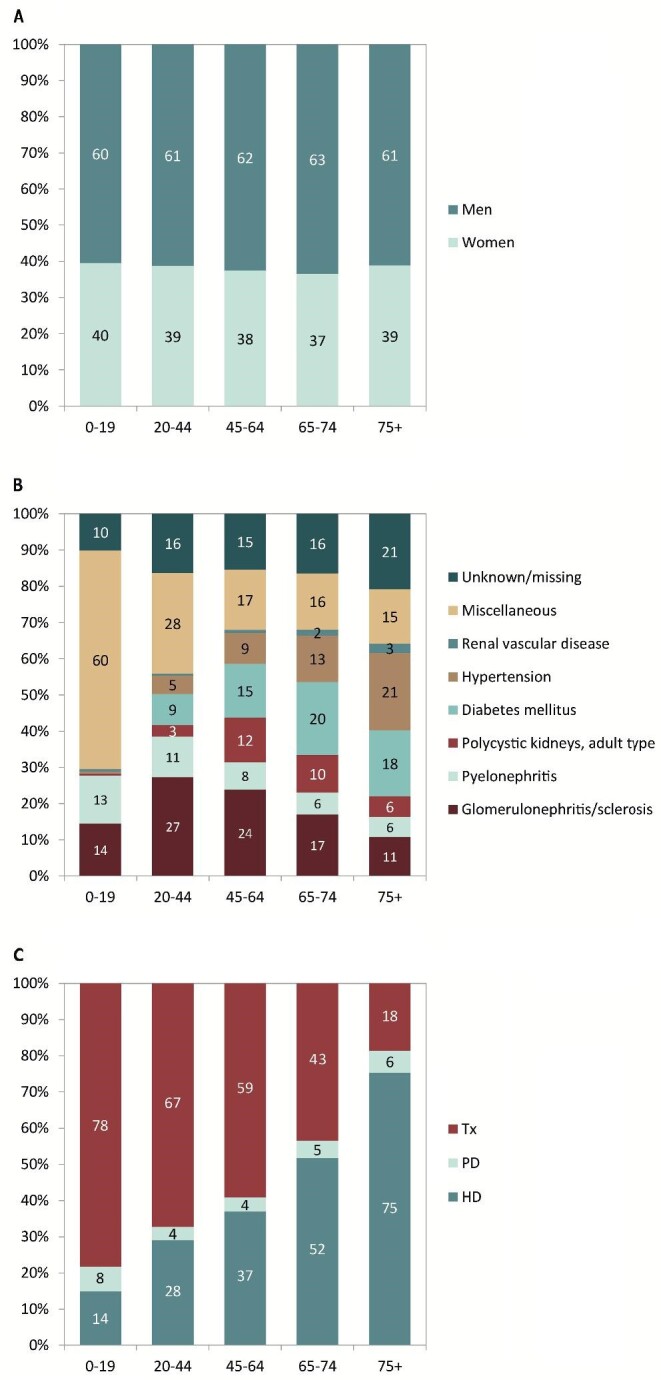
(A) Sex, (B) primary renal disease and (C) treatment modality distribution by age in prevalent patients on 31 December 2019, unadjusted. Results are based on data from registries providing individual patient data. HD, haemodialysis; PD, peritoneal dialysis; Tx, kidney transplant.
Figure 19 shows the number of kidney transplants in each recipient age group. The group of recipients aged 45–64 years received the highest number of kidney transplants, representing 47% of the total number of kidneys transplanted in 2019. In total, 77% of kidney transplantations were performed using deceased donor grafts. However, this proportion differed between the age groups, ranging from 63% deceased donor grafts in patients aged 0–19 years to 93% in patients aged ≥75 years (Figure 20).
FIGURE 19:
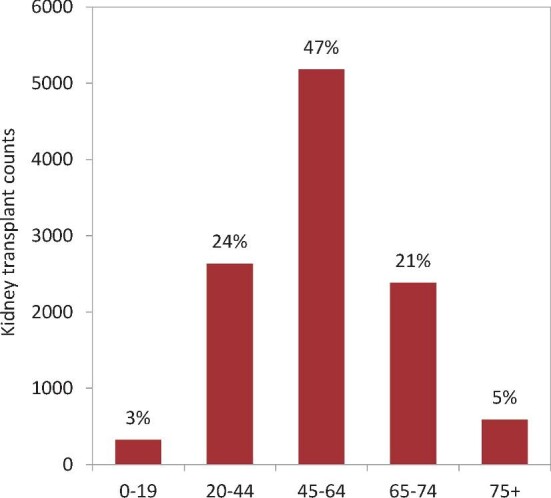
Kidney transplant counts and percentages by recipient age in 2019, unadjusted. Results are based on data from registries providing individual patient data. The percentages in this figure sum up to 100% for all age groups together.
FIGURE 20:
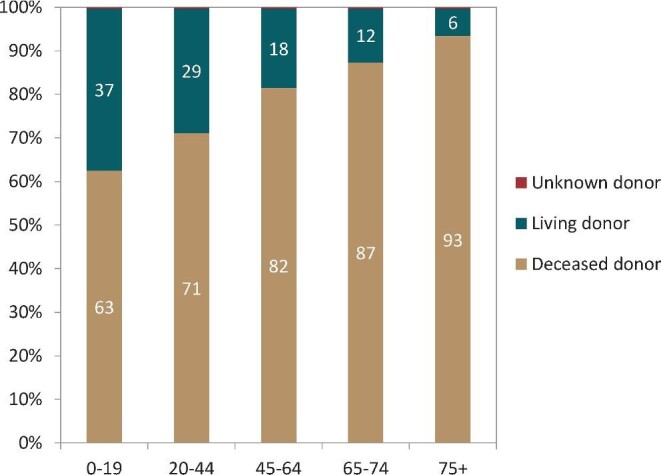
Donor type distribution by age in kidney transplant recipients, unadjusted. Results are based on data from registries providing individual patient data.
Figure 21 shows the adjusted patient survival probabilities by age category for patients on dialysis or recipients of a first kidney transplantation. In dialysis patients, the 5-year patient survival ranged from 90% in patients aged 0–19 years to 25% in patients aged ≥75 years. For kidney transplant recipients, the 5-year patient survival after first kidney transplantation ranged from 97% in patients aged 0–19 years to 66% in patients aged ≥75 years.
AFFILIATED REGISTRIES
Albanian Renal Registry (A. Idrizi, M. Rroji and E. Likaj); Austrian Dialysis and Transplant Registry (OEDTR) (F. Engler, R. Kramar, G. Mayer and the Austrian Society of Nephrology); Belarus Renal Registry (K.S. Komissarov and K.S. Kamisarau); Dutch speaking Belgian Society of Nephrology (NBVN) (M. Couttenye and F. Schroven); French speaking Belgian Society of Nephrology (GNFB) (J.M. des Grottes and F. Collart); Renal Registry Bosnia and Herzegovina; Cyprus Renal Registry (A. Pastelli and L. Yioukas); Czech Republic: Registry of Dialysis Patients (RDP) (I. Rychlík and J. Potucek); Danish Nephrology Registry (DNS); Estonian Society of Nephrology (Ü. Pechter and K. Lilienthal); Finnish Registry for Kidney Diseases (J. Helve and H. Niemelä); France: The Epidemiology and Information Network in Nephrology (REIN) (C. Couchoud); Hellenic Renal Registry (G. Moustakas); Icelandic End-Stage Renal Disease Registry; Montenegro Renal Registry (M. Ratkovic and F. Tomović); Israel National Registry of Renal Replacement Therapy (L. Keinan-Boker and R. Dichtiar); Italian Registry of Dialysis and Transplantation (RIDT) (A. Limido, M. Nordio and M. Postorino); Kosovo Renal Registry (S. Selmani and M. Tolaj-Avdiu); Latvian Renal Registry (V. Kuzema, A. Popovam and A. Pētersons); Lithuanian Renal Registry (V. Vainauskas, I. Nedzelskiene and E. Žiginskiené); North Macedonian Renal Registry (O. Stojceva and R.I. Bushljetik); Norwegian Renal Registry (A.V. Reisæter); Portuguese Renal Registry (A. Ferreira); Romanian Renal Registry (RRR) (G. Mircescu, L. Garneata and E. Podgoreanu); Russian Renal Registry (A. Andrusev, H. Zakharova and N. Tomilina); Renal Registry in Serbia (M. Lausevic, R. Naumovic, all of the Serbian renal units and the Serbian Society of Nephrology); Slovakian Renal Registry (I. Lajdová, V. Spustová and M.J. Rosenberger); Spain Renal Registry (B. Mahillo Durán and M.O. Valentín Muñoz); Swedish Renal Registry (SRR) (K.G. Prütz, M. Evans, S. Schön, T. Lundgren, H. Rydell and M. Segelmark); Swiss Dialysis Registry (P. Ambühl and R. Guidotti); Dutch Renal Registry (RENINE) (L. Heuveling, S. Vogelaar and M. ten Dam); Registry of the Nephrology, Dialysis and Transplantation in Turkey (TSNNR) (K. Ateş and G. Süleymanlar); Ukrainian Renal Data System (URDS) (M. Kolesnyk, O. Razvazhaieva and N. Kozliuk); UK Renal Registry (all the staff of the UK Renal Registry and of the renal units submitting data); Scottish Renal Registry (SRR) (all of the Scottish renal units); and the regional registries of Andalusia (SICATA), Aragon (F. Arribas Monzón), Asturias (P. Beltrán, J.R. Quirós and RERCA Working Group), Basque country (UNIPAR) (Á. Magaz, J. Aranzabal, M. Rodrigo and I. Moina), Canary Islands (I. Santana Gil and C. Torres Medina), Cantabria, Castile and León (M.A. Palencia García), Castile-La Mancha (G. Gutiérrez Ávila and I. Moreno Alía), Catalonia (RMRC) (J. Comas and J. Tort), Community of Madrid (F. Tornero Molina), Extremadura [all the renal units (Nephrology and Dialysis)], Galicia, La Rioja (E. Huarte Loza and H. Hernández Vargas), Murcia (I. Marín Sánchez), Navarre (J. Manrique Escola and J. Arteaga Coloma) and Valencian region (O.L. Rodríguez-Arévalo).
ERA REGISTRY COMMITTEE MEMBERS
C. Wanner, Germany (ERA President); A. Ortiz, Spain (Chairman); P. Ambühl, Switzerland; M. Arici, Turkey; M. Arnol, Slovenia; P.M. Ferraro, Italy; J. Harambat, France; J. Helve, Finland; J.E. Sánchez-Alvarez, Spain; M. Segelmark, Sweden; S.S. Sørensen, Denmark and E. Vidal, Italy.
ERA REGISTRY OFFICE STAFF
K.J. Jager (Managing Director), M.E. Astely, M. Bonthuis, R. Bonenink, R. Cornet, G. Guggenheim, J.A. Huijben, A. Kramer, V.S. Stel and A.J. Weerstra.
Supplementary Material
ACKNOWLEDGEMENTS
The ERA Registry would like to thank the patients and staff of all the dialysis and transplant units who have contributed data via their national and regional renal registries. In addition, we would like to thank the persons and organizations listed in the paragraph ‘Affiliated Registries’ for their contribution to the work of the ERA Registry.
Appendix 1.
Countries or regions providing individual patient data to the ERA Registry: Austria, Dutch-speaking Belgium, French-speaking Belgium, Bosnia and Herzegovina, Denmark, Estonia, Finland, France, Greece, Iceland, Montenegro, Norway, Romania, Serbia, Sweden, Switzerland, the Netherlands, the UK, England/Northern Ireland/Wales and the UK, Scotland, and the Spanish regions of Andalusia, Aragon, Asturias, Basque country, Canary Islands, Cantabria, Castile and León, Castile-La Mancha, Catalonia, Community of Madrid, Extremadura, Galicia, La Rioja, Murcia, Navarre and Valencian region.
Countries or regions providing aggregated data to the ERA Registry: Albania, Belarus, Cyprus, Czech Republic, Israel, Italy, Kosovo, Latvia, Lithuania, North Macedonia, Poland, Portugal, Russia, Slovakia, Spain, Turkey and Ukraine.
Countries not providing data to the ERA Registry: Andorra, Armenia, Azerbaijan, Bulgaria, Croatia, Georgia, Germany, Hungary, Ireland, Liechtenstein, Luxembourg, Malta, Moldova, Monaco, San Marino and Slovenia.
Countries part of the European Union (EU-28) population in 2015 (used as reference population): Austria, Belgium, Bulgaria, Czech Republic, Croatia, Cyprus, Denmark, Germany, Estonia, Greece, Finland, France, Italy, Ireland, Latvia, Lithuania, Luxembourg, Hungary, Malta, the Netherlands, Poland, Portugal, Romania, Slovenia, Slovakia, Spain, Sweden and the UK.
Appendix 2.
Miscellaneous primary renal disease: Nephropathy (interstitial) due to analgesic drugs, nephropathy (interstitial) due to cis-platinum, nephropathy (interstitial) due to cyclosporin A, lead-induced nephropathy (interstitial), drug-induced nephropathy (interstitial) not mentioned above, cystic kidney disease—type unspecified, polycystic kidneys; infantile (recessive), medullary cystic disease; including nephronophtisis, cystic kidney disease—other specified type, hereditary/familial nephropathy—type unspecified, hereditary nephritis with nerve deafness (Alport's Syndrome), cystinosis, primary oxalosis, Fabry's disease, hereditary nephropathy—other specified type, renal hypoplasia (congenital)—type unspecified, oligomeganephronic hypoplasia, congenital renal dysplasia with or without urinary tract malformation, syndrome of agenesis of abdominal muscles (prune belly syndrome), renal vascular disease due to polyarteritis, Wegener's granulomatosis, ischaemic renal disease/cholesterol embolism, glomerulonephritis related to liver cirrhosis, cryoglobulinaemic glomerulonephritis, myelomatosis/light chain deposit disease, amyloidosis, lupus erythematosus, Henoch–Schoenlein purpura, Goodpasture's Syndrome, systemic sclerosis (scleroderma), haemolytic uraemic syndrome (including Moschcowitz syndrome), multi-system disease—other (not mentioned above), tubular necrosis (irreversible) or cortical necrosis (different from 88), tuberculosis, gout, nephrocalcinosis and hypercalcaemic nephropathy, Balkan nephropathy, kidney tumour, traumatic or surgical loss of kidney and other identified renal disorders.
Contributor Information
Rianne Boenink, ERA Registry, Department of Medical Informatics, Amsterdam UMC, University of Amsterdam, Amsterdam Public Health research institute, Amsterdam, The Netherlands.
Megan E Astley, ERA Registry, Department of Medical Informatics, Amsterdam UMC, University of Amsterdam, Amsterdam Public Health research institute, Amsterdam, The Netherlands.
Jilske A Huijben, ERA Registry, Department of Medical Informatics, Amsterdam UMC, University of Amsterdam, Amsterdam Public Health research institute, Amsterdam, The Netherlands.
Vianda S Stel, ERA Registry, Department of Medical Informatics, Amsterdam UMC, University of Amsterdam, Amsterdam Public Health research institute, Amsterdam, The Netherlands.
Julia Kerschbaum, Austrian Dialysis and Transplant Registry, Department of Internal Medicine IV—Nephrology and Hypertension, Medical University Innsbruck, Innsbruck, Austria.
Mai Ots-Rosenberg, Department of Internal Medicine of Tartu University and Tartu University Hospital, Tartu, Estonia.
Anders A Åsberg, The Norwegian Renal Registry, Oslo University Hospital—Rikshospitalet, Oslo, Norway; Department of Transplantation Medicine, Oslo University Hospital—Rikshospitalet, Oslo, Norway.
Frantisek Lopot, Department of Medicine, General University Hospital, Prague—Strahov, Czech Republic.
Eliezer Golan, Israel Renal Registry, Ramat Gan, Israel.
Pablo Castro de la Nuez, SICATA: Information System of the Autonomous Coordination of Transplants of Andalusia, Seville, Andalucia, Spain.
Marta Rodríguez Camblor, RERCA, Public Health Directorate, Asturias, Spain.
Sara Trujillo-Alemán, Health Quality Assessment and Information System Service, Dirección General de Programas Asistenciales, Servicio Canario de la Salud, Canary Islands, Spain.
Juan Carlos Ruiz San Millan, Department of Nephrology, Valdecilla Hospital, IDIVAL, University of Cantabria, Santander, Cantabria, Spain.
Pablo Ucio Mingo, Coordinación Autonómica de Trasplantes de Castilla y León, Dirección General de Planificación y Asistencia Sanitaria, Valladolid, Castilla y León, Spain.
Juan Manuel Díaz, Servei Nefrologia, Fundació Puigvert, Barcelona, Catalonia, Spain.
M Encarnación Bouzas-Caamaño, Regional Transplant Coordination of Galicia, Galician Health Service, Santiago de Compostela, Galicia, Spain.
Marta Artamendi, Nephrology Department, Hospital San Pedro, Logroño, La Rioja, Spain.
Manuel I Aparicio Madre, Oficina Regional de Coordinación de Trasplantes, Madrid Region, Spain.
Carmen Santiuste de Pablos, Murcia Renal Registry, Department of Epidemiology, Murcia Regional Health Council, IMIB-Arrixaca, Murcia, Spain; CIBERESP (Spanish Consortium for Biomedical Research in Epidemiology and Public Health), Madrid, Spain.
María Fernanda Slon Roblero, Complejo Hospitalario de Navarra, Pamplona, Navarra, Spain.
Oscar Zurriaga, CIBERESP (Spanish Consortium for Biomedical Research in Epidemiology and Public Health), Madrid, Spain; Valencian Region Renal Registry, Valencia Regional Health Authority, Generalitat Valenciana, Spain; Universitat de Valencia, Valencia, Spain.
Maria E Stendahl, Swedish Renal Registry, Department of Internal Medicine, Jonkoping Regional Hospital, Jonkoping, Sweden.
Samira Bell, Division of Population Health and Genomics, School of Medicine, University of Dundee, Dundee, UK; The Scottish Renal Registry, Scottish Health Audits, Public Health Scotland, Meridian Court, Glasgow, UK.
Alma Idrizi, Service of Nephrology, UHC Mother Teresa, Tirana, Albania.
Kyriakos Ioannou, Cyprus Renal Registry, Nicosia, Cyprus; Nephrology Department, American Medical Center, Nicosia, Cyprus.
Alicja Debska-Slizien, Department of Nephrology, Transplantology and Internal Medicine, Gdansk Medical University, Gdansk, Poland.
Ana A Galvão, Portuguese Society of Nephrology, Coimbra, Portugal.
Johan M De Meester, Department of Nephrology, Dialysis and Hypertension, Dutch-speaking Belgian Renal Registry (NBVN), Sint-Niklaas, Belgium.
Halima Resić, Society of Nephrology and Dialysis of Bosnia and Herzegovina, Sarajevo, Bosnia and Herzegovina.
Kristine Hommel, Department of Medicine, Holbaek Hospital, Holbaek, Denmark.
Danilo Radunovic, Clinical Center of Montenegro, Clinic for Nephrology, Podgorica, Montenegro.
Runolfur Pálsson, Division of Nephrology, Landspitali–The National University Hospital of Iceland, Reykjavik, Iceland; Faculty of Medicine, School of Health Sciences, University of Iceland, Reykjavik, Iceland.
Mathilde Lassalle, REIN Registry, Agence de la Biomédecine, Saint-Denis La Plaine, France.
Patrik Finne, Department of Nephrology, University of Helsinki and Helsinki University Hospital, Helsinki, Finland; Finnish Registry for Kidney Diseases, Helsinki, Finland.
María De los Ángeles-Garcia Bazaga, Dirección General de Salud Pública, Servicio Extremeño de Salud, Consejería de Sanidad y Políticas Sociales, Junta de Extremadura, Spain.
Nikola Gjorgjievski, University Hospital of Nephrology, Skopje, North Macedonia; Faculty of Medicine, University SS “Cyril and Methodius”, Skopje, North Macedonia.
Nurhan Seyahi, Department of Nephrology, Cerrahpaşa Medical Faculty, Istanbul University-Cerrahpaşa, Istanbul, Turkey.
Marjolein Bonthuis, ERA Registry, Department of Medical Informatics, Amsterdam UMC, University of Amsterdam, Amsterdam Public Health research institute, Amsterdam, The Netherlands; ESPN/ERA Registry, Department of Medical Informatics, Amsterdam UMC, University of Amsterdam, Amsterdam Public Health Research Institute, Amsterdam, The Netherlands.
Alberto Ortiz, Department of Nephrology and Hypertension, IIS-Fundacion Jimenez Diaz UAM, Madrid, Spain; Department of Medicine, Universidad Autonoma de Madrid, Madrid, Spain.
Kitty J Jager, ERA Registry, Department of Medical Informatics, Amsterdam UMC, University of Amsterdam, Amsterdam Public Health research institute, Amsterdam, The Netherlands.
Anneke Kramer, ERA Registry, Department of Medical Informatics, Amsterdam UMC, University of Amsterdam, Amsterdam Public Health research institute, Amsterdam, The Netherlands.
FUNDING
The ERA Registry is funded by the ERA. This article was written by R. Boenink et al. on behalf of the ERA Registry, which is an official body of the ERA. In addition, S.B. reports personal fees from AstraZeneca, outside the submitted work; A.D.-S. reports personal fees from Astellas and Fresenius, outside the submitted work; F.L. reports personal fees from MeditesPharma, outside the submitted work; R.P. reports grants from The Iceland Centre for Research, Landspitali University Hospital Research Fund and University of Iceland Research Fund, outside the submitted work; P.F. reports grants from Finska läkaresällskapet and Liv och Hälsa, outside the submitted work; M.F.S.R. reports personal fees from Baxter and Fresenius, outside the submitted work; A.O. reports grants from Sanofi, and personal fees from Astellas, AstraZeneca, Amicus, Bayes, Fresenius Medical Care and Idorsia, outside the submitted work; and K.J.J. reports grants from ERA, during the conduct of the study.
CONFLICT OF INTEREST STATEMENT
A.O. is the CKJ Editor-in-Chief.
REFERENCES
- 1. Kramer A, Boenink R, Stel VSet al. The ERA-EDTA Registry Annual Report 2018: a summary. Clin Kidney J 2021; 14: 107–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Eurostat . Demography, Population Stock and Balance-Population National Level. https://ec.europa.eu/eurostat/web/main/data/database (August 2021, date last accessed) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.