Abstract
Chronic kidney disease (CKD) is a silent and poorly known killer. The current concept of CKD is relatively young and uptake by the public, physicians and health authorities is not widespread. Physicians still confuse CKD with chronic kidney insufficiency or failure. For the wider public and health authorities, CKD evokes kidney replacement therapy (KRT). In Spain, the prevalence of KRT is 0.13%. Thus health authorities may consider CKD a non-issue: very few persons eventually need KRT and, for those in whom kidneys fail, the problem is ‘solved’ by dialysis or kidney transplantation. However, KRT is the tip of the iceberg in the burden of CKD. The main burden of CKD is accelerated ageing and premature death. The cut-off points for kidney function and kidney damage indexes that define CKD also mark an increased risk for all-cause premature death. CKD is the most prevalent risk factor for lethal coronavirus disease 2019 (COVID-19) and the factor that most increases the risk of death in COVID-19, after old age. Men and women undergoing KRT still have an annual mortality that is 10- to 100-fold higher than similar-age peers, and life expectancy is shortened by ~40 years for young persons on dialysis and by 15 years for young persons with a functioning kidney graft. CKD is expected to become the fifth greatest global cause of death by 2040 and the second greatest cause of death in Spain before the end of the century, a time when one in four Spaniards will have CKD. However, by 2022, CKD will become the only top-15 global predicted cause of death that is not supported by a dedicated well-funded Centres for Biomedical Research (CIBER) network structure in Spain. Realizing the underestimation of the CKD burden of disease by health authorities, the Decade of the Kidney initiative for 2020–2030 was launched by the American Association of Kidney Patients and the European Kidney Health Alliance. Leading Spanish kidney researchers grouped in the kidney collaborative research network Red de Investigación Renal have now applied for the Redes de Investigación Cooperativa Orientadas a Resultados en Salud (RICORS) call for collaborative research in Spain with the support of the Spanish Society of Nephrology, Federación Nacional de Asociaciones para la Lucha Contra las Enfermedades del Riñón and ONT: RICORS2040 aims to prevent the dire predictions for the global 2040 burden of CKD from becoming true.
Keywords: accelerated ageing, burden of disease, chronic kidney disease, COVID-19, decade of the kidney, kidney failure, kidney transplantation, research funding
CHRONIC KIDNEY DISEASE: AN EVOLVING CONCEPT IN NEED OF UPDATING
The Kidney Disease: Improving Global Outcomes consensus defines chronic kidney disease (CKD) as abnormalities of kidney structure or function present for >3 months with implications for health [1]. Just one criterion identifying abnormal kidney structure or function allows the diagnosis of CKD. Criteria include a low glomerular filtration rate (GFR; <60 mL/min/1.73 m2) or evidence of kidney damage such as pathological albuminuria [urinary albumin:creatinine ratio (UACR) ≥30 mg/g]; abnormal urine sediment, histology or imaging; abnormalities due to tubular disorders or kidney transplantation. In clinical practice, this means that diagnosing CKD when GFR is ≥60 mL/min/1.73 m2 requires urinalysis or kidney imaging. A recent conceptual manuscript summarized the key features of CKD for non-nephrologists, as there is ongoing confusion, even in high-quality journals, such as the New England Journal of Medicine [2].
A CKD diagnosis implies an increased risk of progressing to require kidney replacement therapy (KRT), of all-cause and cardiovascular death and of acute kidney injury (AKI) [1, 3–5]. There is a bidirectional relationship between CKD and AKI. CKD is the main risk factor for AKI and AKI may accelerate CKD [6]. AKI has a high mortality and increases the risk of death for >1 year after the episode [6]. AKI is also common, as ~5% of hospitalized patients develop in-hospital AKI [7]. More recently, CKD has been identified as the most prevalent risk factor for lethal coronavirus disease 2019 (COVID-19) and as the factor that most increased the risk of death in COVID-19 after older age [8–10] (Figure 1). AKI is also common in COVID-19 and a key risk factor for death [8].
FIGURE 1:
CKD is the most prevalent risk factor for severe COVID-19 and also the risk factor for severe COVID-19 that is associated with the highest risk of death, after old age. (A) CKD as a percentage of persons at risk of severe COVID-19 on a global scale. Data from Clark et al. [10]. (B) Risk of death associated with pre-existent conditions in patients with COVID-19 in an adjusted analysis. Data from Williamson et al. [9]. Reproduced from ERA-EDTA Council and ERACODA Working Group [8].
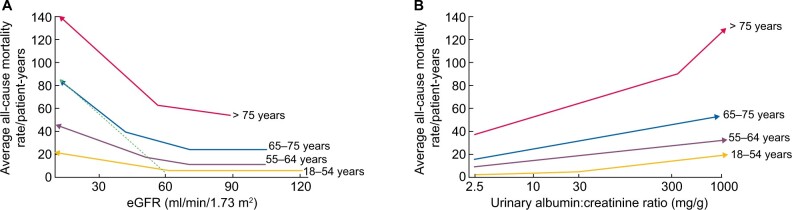
Correct CKD diagnoses require indicating cause and G (GFR: G1–G5) and A (albuminuria: A1–A3) categories. Increasing CKD categories are associated with an increased risk of all-cause and cardiovascular death, even in the elderly (Figure 2A and B). The G1 (GFR ≥90 mL/min/1.73 m2) and A1 (UACR <30 mg/g) categories are not diagnostic of CKD by themselves. Persons in category G1A1 must fulfil an additional criterion to be diagnosed with CKD, such as imaging diagnostics of polycystic kidney disease (PKD) [1, 2]. The autosomal dominant PKD paradigm illustrates the way to go: a diagnostic test (sonography) allows the diagnosis of CKD decades before patients fulfil any other criterion to diagnose CKD, including the most commonly used ones such as GFR and UACR thresholds [11]. Similar diagnostic tools are needed for other forms of CKD, as by the time GFR falls to 60 mL/min/1.73 m2, CKD has progressed unnoticed (potentially over years and even decades) to destroy >50% of the functioning kidney mass. Similarly, albuminuria as low as >2.5 mg/g is already associated with an increased risk of premature death (Figure 2B). Again, the current albuminuria threshold used to diagnose CKD is a late event. There is a clear margin for earlier diagnosis and therapy of CKD. Additional future criteria to diagnose CKD may be envisioned, such as genetic tests disclosing clearly pathogenic gene variants or urinary biomarkers beyond UACR, including urinary peptidomics [12, 13].
FIGURE 2:
CKD is associated with an increased risk of death even in the very elderly. All-cause mortality rate (absolute risk) for different (A) eGFR and (B) UACR values by age categories based on weighted average across cohorts, adjusted for covariates. A steeper slope at an older age indicates a higher absolute risk difference associated with low eGFR as compared with younger age categories: the discontinuous green line represents the overlay of the risk for the very elderly on top of the risk line for the younger age range. Similar trends were observed for albuminuria. Conceptual representation of data presented in Hallan et al. [4]. In panel A, an increase in the risk of death observed in patients >55 years of age with higher eGFR values is not shown, as this is thought to be an artefact depending on lower muscle mass of patients who were sicker at baseline.
Kidney failure (end-stage kidney disease, G5, GFR <15 mL/min/1.73 m2) is probably the only form of kidney disease well known to the wider public, non-nephrologists and healthcare authorities. Non-experts usually equate the burden of CKD with the burden of KRT for kidney failure. Despite care for KRT patients representing a disproportionate percentage of the healthcare budget (the roughly 64 292 persons on KRT in Spain consume 2.5–5.0% of the healthcare budget), the bulk of the health burden of CKD is not represented by KRT but by accelerated ageing and premature death, as clearly quantified by Global Burden of Disease (GBD) data discussed below [14]. However, there are no registries in Spain for persons with CKD not on KRT as is the case for many other countries.
KRT: A SUCCESS STORY OR A STORY OF FAILURE?
KRT has been hailed as one of the success stories of healthcare that allows survival when a vital organ has failed. Counterintuitively, this reflects only a partial view of the facts. Rather, KRT should be considered a failure of CKD management, as the expected remaining lifetime is severely reduced—by ~70% (40 years less) and by 25% (15 years less) for a 20-year-old on dialysis or with a functioning kidney graft, respectively [15, 16]. The absolute reduction in the expected remaining lifetime is less at older ages, but the relative reduction in life expectancy remains constant up to age 89 years (Figure 3A). The fact that the mortality of kidney failure remains high, up to 100-fold higher in patients on KRT than for similar-aged controls [5], is not well known by health authorities and may hinder funding for CKD research. Indeed, the 5-year survival of patients on dialysis is lower than for all forms of cancer combined [17] (Figure 3B).
FIGURE 3:
Severely limited survival in persons on KRT. (A) Expected remaining lifetimes of the general population and of dialysis and kidney transplant patients in the ERA-EDTA Registry. Arrows and numbers depict relative and absolute reductions in life expectancy for young adults on KRT, either on dialysis (burgundy) or with a functioning kidney graft (orange) [15, 16]. (B) Percentage 5-year survival of KRT modalities (red bars) (haemodialysis, peritoneal dialysis, transplantation after deceased donation and transplantation after living donation) or after the diagnosis of cancer (blue bars). Only malignancies with an incidence >3% of all cancers are illustrated. Orange bar: all cancers aggregated. Based on 2016 data. Source: Vanholder et al. [17].
THE MOST COMMON CAUSE OF CKD IS UNKNOWN: THE NEED TO REDEFINE THE CKD AETIOLOGY LANDSCAPE
The most common cause of KRT in Spain is diabetes (25% of persons initiating KRT), followed by unknown (15%), ‘vascular’, glomerulonephritis (14%) and inherited kidney disease [15, 16, 18]. The magnitude of the inherited category is difficult to assess as it is usually divided into PKD and others. Others are usually dumped into a ‘miscellaneous’ category or misdiagnosed as glomerular or interstitial CKD. Recent analysis of the Madrid and Catalonian KRT registries has disclosed that inherited kidney disease is as frequent as glomerulonephritis [19]. Inherited kidney diseases are frequently overlooked by physicians as illustrated by whole-exome sequencing findings of monogenic kidney diseases in 9% of adult CKD and in 17–34% of those with CKD of unknown cause [20, 21].
‘Vascular’ mainly means hypertension, and it is labelled as hypertension in the European Renal Association–European Dialysis and Transplant Association (ERA-EDTA) Registry [15, 16, 18]. In clinical practice, hypertension is usually listed as a cause when there is no other obvious aetiology, following expert recommendation [22]. This practice has been criticized, as it may replace an inadequate aetiologic workup, likely downplaying the incidence of other causes of CKD while falsely boosting hypertension as a cause (rather than as consequence) of CKD [23, 24]. Thus there is no relationship between the prevalence of hypertension and hypertensive CKD in different countries [23]. In African Americans, hypertensive nephropathy has long been shown to represent a familial predisposition to CKD triggered by different causes, i.e. it would be better classified as inherited kidney disease accelerated by triggers such as human immunodeficiency virus or severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection [25].
The ERA-EDTA Registry provides more elaborate data (Spanish data are made public on websites but not regularly published in journals by themselves) and a European-wide perspective [15, 16]. In ERA-EDTA Registry data for all countries, the most common cause of incident KRT was unknown (27%, increasing to 39% if we add hypertension) followed by diabetes (20%), glomerulonephritis (11%) and PKD (5%). For prevalent KRT, the ranking is unknown (27%, increasing to 35% by adding hypertension) followed by glomerulonephritis (19%), diabetes (15%) and PKD (8%). This identifies a major issue in CKD. A significant percentage of persons lack an aetiological diagnosis, which precludes aetiology-targeted therapy and early prevention campaigns. Among the fastest-growing segment of CKD patients (those ≥65 years of age), unknown and hypertension accounted for 43% of incident KRT patients, highlighting the need to define cause in the elderly. We propose that accelerated kidney ageing may be a key contributor to CKD, including in the elderly, and are currently devising a working definition for accelerated kidney ageing that spurs research in this field.
THE GROWING BURDEN OF CKD
Globally, ~850 million persons have CKD [26]. The GBD study has generated data on the global and local burden of CKD, while Spanish epidemiological studies provide information on the local prevalence of CKD and the epidemiology of KRT.
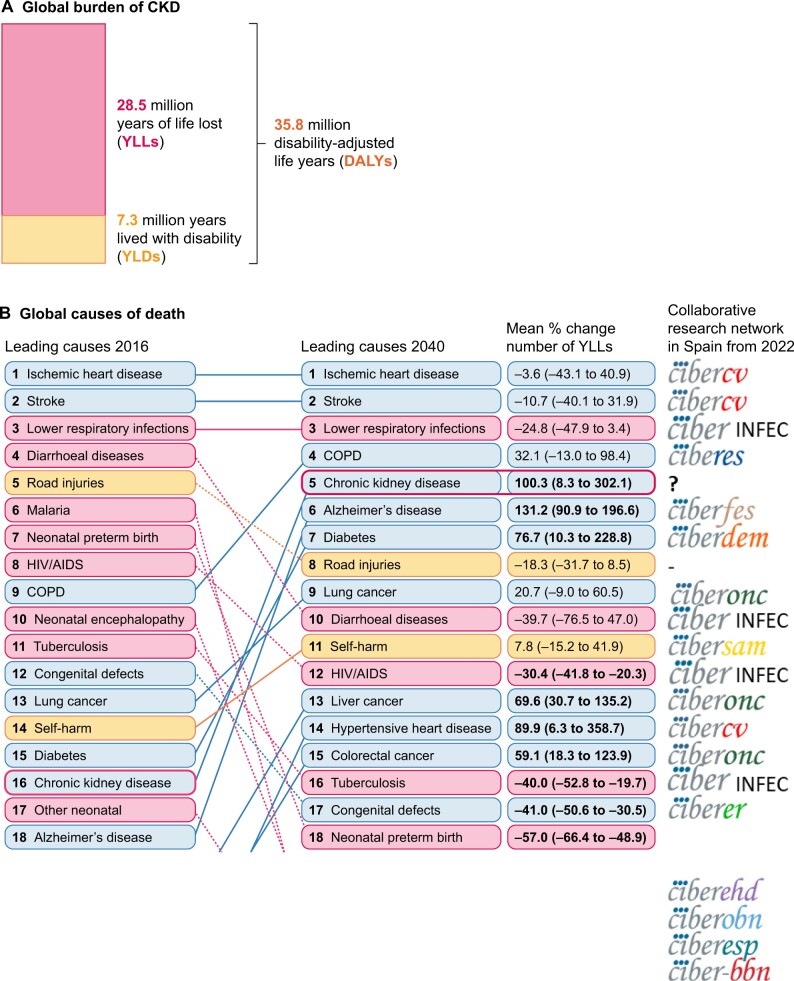
In 2017, 1.2 million people died from CKD globally and CKD resulted in 35.8 million disability-adjusted life years (DALYs), most of them (>70%) not due to diabetic kidney disease (DKD), as well as in 7.3 million years lived with disability (YLD) and 28.5 million years of life lost (YLL) [27] (Figure 4A). Considerable global variation was noted in CKD burden. Age-standardized CKD DALY rates varied >15-fold between countries, a variability also evident within Spain and even within Spain autonomous communities [15, 27]. This illustrates the need for interregional collaborative research to identify and correct the drivers of a higher burden in certain regions.
FIGURE 4:
Global burden of CKD, according to the GDB study. (A) 2017 global DALYs, YLD and YLL due to CKD [27]. (B) Major global causes of death in 2016 and predicted for 2040 according to the GBD study, ranked by YLL [14]. CKD is marked by empty rectangles. Logos to the right correspond to ISCIII-funded collaborative research networks in Spain that will address each cause from 2022. At the time of this writing, the status of kidney research in 2022 is still unclear. An infectious disease CIBER will be created in 2022, but at this point we are unaware of the logo. Thus, the CIBER logo was used and the word ‘INFEC’ was added.
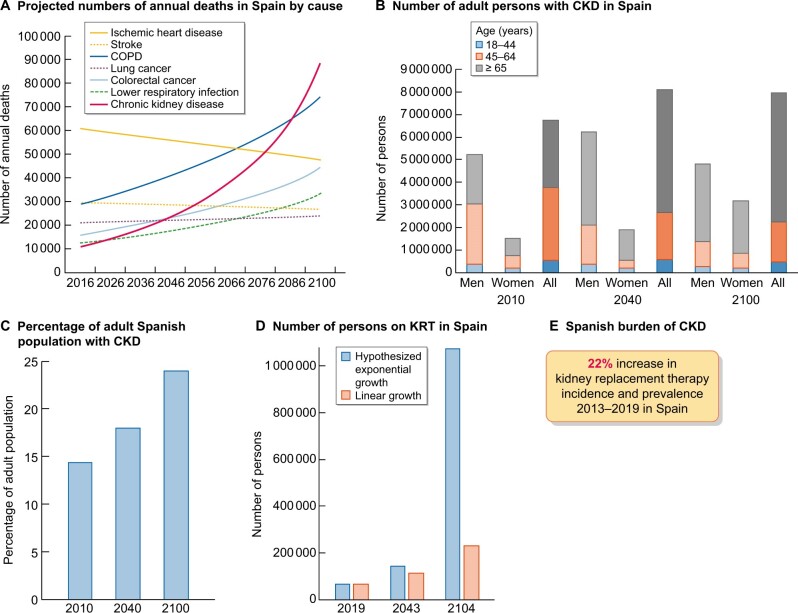
The GBD projected that CKD will become the fifth greatest global cause of death by 2040 [14] (Figure 4B). YLL due to CKD are expected to double by 2040, the fastest increase among major causes of death after Alzheimer’s. In contrast, the burden of other major causes of death is projected to decrease (e.g. ischaemic heart disease −3.6% or stroke −10.7%). Interestingly, CKD growth as a global cause of death outpaces diabetes, illustrating the need to address non-diabetic causes of CKD and protect the kidneys in persons with diabetes. Spain GBD data identified CKD as the eighth greatest cause of death, representing the largest departure from official Instituto Nacional de Estadistica (INE) data among causes of death in Spain. The INE underestimated the burden of CKD, likely due to low awareness of the condition [28, 29]. Spain’s GBD identified CKD as the second fastest-growing cause of death, the sixth fastest-growing cause of YLD and the seventh fastest-growing cause of DALYs among the top 25 causes for each category [28, 29]. Projecting into the future, the recent rate of increase of CKD in Spain’s GBD, CKD will become the second leading cause of death, after Alzheimer’s, before the end of the century [29] (Figure 5A). This is likely an underestimation, as the progressive change in the age pyramid over the next few decades was not considered. Spanish projections may also apply to other countries with long life expectancies.
FIGURE 5:
CKD burden and epidemiology in Spain. (A) Projected numbers of annual deaths in Spain by cause. Alzheimer’s not shown but it is projected to become the leading cause of death before the end of the century, well above the others. Past growth according to the GBD 2016 for Spain was projected into the future [29]. The projection did not consider the progressive ageing of the Spanish population. Thus it represents an underestimation of CKD-related deaths. (B) Number of adults with CKD in Spain, by gender and overall, according to the ERICA study from 2010 and projection into the future assuming the same prevalence of CKD by age category and considering changes in the Spanish population age pyramid according to the WHO predictions [30–32]. Since the increasing mean age within each age category was not considered, this projection represents an underestimation [30, 31]. For each selected year, data for men, women and all are shown. (C) Percentage of Spanish adults with CKD in the ERICA study (2010) and projection into the future [30–32]. (D) Number of prevalent persons on KRT in Spain in 2019 and projection into the future based on the 22% (12 000 persons) growth from 2013 to 2019 [18]. In blue, estimates according to hypothesized exponential growth; in orange, estimates according to linear growth. The progressive ageing of the population was not accounted for, potentially underestimating the results. (E) Increase in the incidence and prevalence of KRT from 2013 to 2019 in Spain.
FIGURE 6:
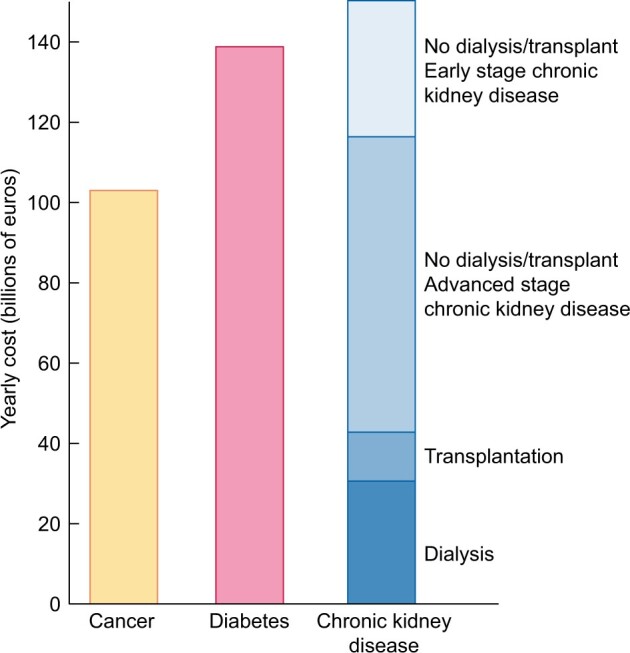
The economic burden of CKD. Comparison of aggregated annual healthcare costs for Europe of cancer (yellow), diabetes mellitus (red) and CKD (different shades of blue). Costs of CKD are a composite of early CKD (stages/categories G1–G2 in native or transplant kidneys, in light blue), more advanced stages of CKD (stages/categories G3–G5 not on dialysis in native or transplant kidneys), transplantation and dialysis (dark blue). Source: Vanholder et al. [17].
The population of Spain is projected to peak in the present decade and to become progressively older and decrease to ~23–33 million by 2100 [30, 31]. The most recent estimate of the number of persons with CKD dates from 2010, when 14% of Spanish adults (6.7 million) had CKD [32]. CKD was more common in men than in women and a majority of persons with CKD were in the 45- to 64-year age range. Projecting these numbers into the future in the absence of changes to the current standard of care, assuming a constant prevalence of CKD within each age range and gender group and using World Health Organization (WHO) population prediction estimates, results in at least 8.12 million persons with CKD by 2040 and 7.96 million by 2100, which will represent 18% and 24% of the Spanish population, respectively (Figure 5B and C). This is an underestimation, as progressive ageing of the population (persons ≥65 years of age are estimated to increase from 17% in 2010 to 32% by 2040 and 35% by 2100) will also occur within the same age range category, and this would be associated with an increased prevalence of CKD within age categories. Additionally, by 2040, most persons with CKD will be ≥65 years old.
The prevalence of KRT in Spain is also increasing. It increased 38% from 2007 to 2019 [985 to 1367 per million population (pmp)] and the rate appears to be accelerating (it increased 14% from 2007 to 2013 and 22% from 2013 to 2019). At this rate of growth, the number of persons on KRT will hit 0.23–1.00 million by the end of the century, i.e. ~1–4% of the projected population of Spain at that time (Figure 5D). The incidence of KRT also increased by 22% from 2013 to 2019 (125–152 pmp) [18] (Figure 5E). A majority of persons on KRT in Spain (55%) have a functioning kidney graft. Thus improving kidney and person outcomes in kidney graft recipients is a major aim in kidney research. As for CKD, KRT is also more common in men than in women. Therefore studies on CKD or KRT that do not split by gender may reflect the disease in men and studies addressing risk stratification, diagnosis and therapeutic approaches independently for men and women are required. Furthermore, there are large regional differences (range of incident KRT is 85–197 pmp and of prevalent KRT is 740–1567 pmp for different Spanish regions), which are also observed within regions (e.g. in Madrid, the range of incident KRT is 50–200 pmp and of prevalent KRT is 980–1700 pmp for different healthcare catchment areas). The causes of these differences are not fully understood, but it is critically important to define them in order to identify and target factors that generate CKD hotspots or benchmark potential healthcare contributors [33].
The burden of CKD is also economic. The extrapolated annual cost of all CKD is at least as high as that for cancer or diabetes and estimated at >€140 billion annually in Europe and >$130 billion in the USA [17, 34] (Figure 6).
THE RATIONALE FOR RICORS2040
From 2022, the Instituto de Salud Carlos III (ISCIII, a Spanish government agency that funds health research) will fund the Redes de Investigación Cooperativa Orientadas a Resultados en Salud (RICORS; Cooperative Research Networks Focused on Results in Health) programme of network research. This will replace the prior ISCIII-funded programme of network research called RETICS (Network for Cooperative Research in Health). The Spanish kidney research community, represented by the research groups integrated into the Kidney Research Network RETIC (RETIC REDINREN) and by several working groups of the Spanish Society of Nephrology [Sociedad Española de Nefrología (SEN)], such as GLOSEN (glomerular disease working group) and GEENDIAB (diabetes working group), has submitted the RICORS2040 proposal to the RICORS call. RICORS2040 is supported by the Sociedad Española de Nefrología (SENEFRO), the ERA-EDTA, Federación Nacional de Asociaciones para la Lucha Contra las Enfermedades del Riñón (Spanish Kidney Patients Association) and Organización Nacional de Trasplantes (ONT). RICORS2040 is focused on kidney diseases within one of the four thematic areas of the RICORS call: ‘inflammation and immunopathology of organs and systems’ [35]. This thematic area includes kidney diseases and also other topics, including non-transmissible immune system diseases, allergic diseases, multiple sclerosis and eye diseases. Thus RICORS2040 complies with guidance indicating that proposals should address one of the four thematic areas and may refer to one or more topics within a thematic area [35].
CKD as a chronic inflammatory disease
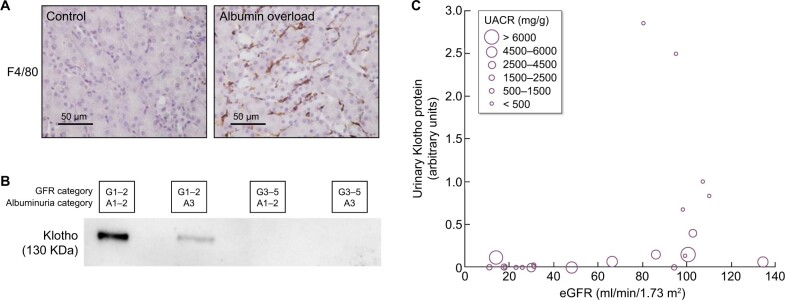
CKD can be characterized as a local inflammatory disease that becomes a systemic inflammatory disease as it progresses. Indeed, activation of the master regulator of inflammation [nuclear factor (NF)-κB], local expression of inflammatory cytokines and immune cell infiltrates are already observed in the early stages of CKD and can be triggered by albuminuria, hyperglycaemia and genetic defects, among others [36, 37] (Figure 7A). Kidneys have multiple functions and GFR, which is usually estimated (not measured) in routine clinical care, is just one of them. There is increasing evidence that production of the anti-ageing and anti-inflammatory factor Klotho is a key function of kidney tubules that is lost very early in the course of CKD (GFR category G1, i.e. normal kidney function) partly in response to local inflammation and/or albuminuria [38–40] (Figure 7B). Loss of anti-inflammatory molecules and accumulation of uraemic toxins leads to systemic inflammation, which is a key predictor of cardiovascular events and death in CKD, likely contributing to the accelerated biological ageing that characterizes CKD [41, 42]. The immune response also causes native kidney injury and is a leading cause of chronic graft injury.
FIGURE 7:
CKD as a local and systemic inflammatory disease leading to accelerated biological ageing. (A) Albuminuria itself may trigger kidney inflammation as illustrated by the albumin overload model in mice: pathological albuminuria triggered interstitial macrophage (F4/80-positive cells) infiltration (data shown) while kidney function was preserved (data not shown) [37]. Thus albuminuria induces the loss of a key kidney function (production of the anti-inflammatory, anti-fibrosis and anti-ageing protein Klotho) well before the kidney function assessed in routine clinical care (GFR) is lost. (B) Decreased urinary Klotho in persons with CKD G1/G2 (i.e. higher eGFR levels that per se are not diagnostic of CKD) with pathological albuminuria (consistent with cell culture and in vivo preclinical models in which inflammatory cytokines or albumin/albuminuria decreased tubular cell Klotho production by healthy tubular cells) and also in persons with CKD G3–5 (i.e. reduced eGFR, diagnostic, by itself, of CKD). In CKD G3–5 the decrease in Klotho is likely the consequence, in part, of decreased tubular cell mass. (C) Decreased urinary Klotho in persons with pathological albuminuria and preserved eGFR and also in persons with decreased eGFR irrespective of albuminuria. Vertical axis reflects urinary Klotho, horizontal axis reflects eGFR and diameter of circles reflects the magnitude of albuminuria [37].
Current versus future burden: the decade of the kidney
We strongly believe that current research should be guided by future projections of disease burden rather than by past statistics. Predictions for the global impact of CKD are dire. RICORS2040 derives its name from its aim to prove wrong the projections that CKD will become the fifth leading global cause of death by 2040. In this regard, RICORS2040 is fully aligned with the Decade of the Kidney concept first established by the American Association of Kidney Patients for 2020–2030, given the realization that CKD care lags other major causes of death in terms of current outcomes, predicted outcomes in the next decades and research funding [43]. This was followed by the Advancing American Kidney Health (AAKH) initiative of the USA government that is expected to become a catalyst for investment in kidney disease clinical trials and precision medicine [44]. The Decade of the Kidney is supported by the European Kidney Health Alliance (EKHA) and by patient associations across Europe that have launched a European movement for 2021–2030 [17, 43]. The RICORS2040 leadership is actively contributing to EKHA efforts.
Emphasis on prevention
RICORS2040 is focused on preservation of native and graft kidney function and improving outcomes in persons with CKD by preventing systemic consequences of CKD, collectively grouped into the concept of accelerated biological ageing, including consequences of kidney transplantation and its therapy (Figure 8), as a majority of persons on KRT in Spain have a kidney graft. Thus, preventing the need for KRT in men and women with native kidneys or kidney grafts and improving kidney and patient outcomes in kidney graft recipients are major aims of RICORS2040. Risk stratification and optimization of therapeutic approaches to improve quality of life and life expectancy in the dialysis population are also addressed.
FIGURE 8:
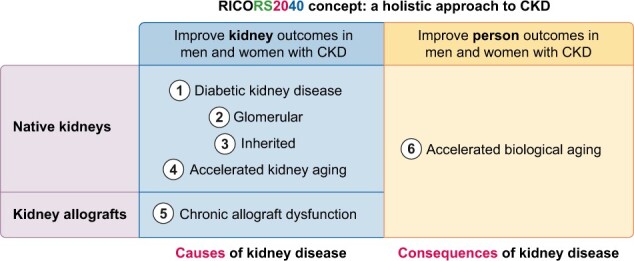
RICORS2040 concept and overall structure and research aims. RICORS2040 aims at improving kidney and person outcomes in both men and women with CKD. There are two sets of aims. The first set aims at improving the diagnosis and management of the most common causes of CKD to prevent or delay CKD progression. For this, the main causes of native kidney CKD (diabetes, glomerular, inherited/genetic) will be addressed and the accelerated kidney ageing concept will be explored as a final common pathway of CKD progression and as a potential cause of CKD in persons in whom no other cause is identified. Since the life expectancy of kidney allografts is markedly shorter than for native kidneys, chronic allograft dysfunction will also be explored. The second set aims to improve person outcomes by optimizing the diagnosis and management of the consequences of CKD (or of kidney transplantation therapy) on other organs and systems, what we have collectively called the accelerated biological ageing of CKD. Please note that Aim 4 is focused on accelerated kidney ageing as a cause of CKD and on kidney events, while Aim 6 is focused on the impact of CKD on other organs and systems, i.e. on accelerated biological ageing of diverse organs and systems occurring as a consequence of CKD. Care will be taken to identify and optimize the management of gender-related issues and provide clinical guidance with specific information for men and for women.
Men and women
There is mounting evidence that course and complications of CKD are not the same in men and women and even the cut-off points to define CKD may differ [45]. However, we still use the same metric and the same cut-off points to diagnose CKD and for risk stratification in men and women, even knowing that creatinine excretion differs and therefore the denominator for UACR differs for men and for women. RICORS2040 will address the factors behind the gender gap in CKD burden and aims to provide clinical guidance for both men and women and to identify information gaps that preclude a gender-conscious approach to the diagnosis, risk stratification and treatment of CKD.
Addressing regional inequality
RICORS2040 will also address the factors behind geographical differences in CKD burden as it incorporates multiple centres from all over Spain. Specifically, kidney research and care centres from 12 of the 17 Spanish regions (autonomous communities) encompassing 90% of the Spanish population are integrated into RICORS2040.
Clinical guidance should be implemented
A key issue hampering the achievement of health outcome targets is the poor implementation of clinical guidance documents. In this regard, clinical guidance documents are rarely validated in real-world clinical practice to assess potential shortcomings or barriers to implementation. RICORS2040 will use continuous improvement approaches to generate, validate and improve clinical guidance documents for different causes of CKD as well as for assessing and slowing the progression of CKD and the associated accelerated biological ageing of organs and systems in men and women with native kidneys or with kidney grafts. Testing the implementation of clinical guidance documents in a large number of centres from different regional health systems under real-world conditions will allow identification and correction of most shortcomings and feasibility issues.
In summary, RICORS2040 is focused on decreasing the need for KRT by improving prevention, diagnosis and therapy for major causes of CKD (diabetic, glomerular, inherited and accelerated kidney ageing; the latter is a concept that RICORS2040 is developing) in native kidneys and of chronic allograft nephropathy as well as on improving outcomes of men and women with CKD by preventing, identifying and treating major consequences of CKD or its therapy that contribute to the burden of accelerated ageing and premature death (Table 1). This will be achieved through systematization of prior knowledge generated by its antecessor REDINREN and the international community into gender-conscious clinical guidance documents, novel research to address gaps of knowledge and monitoring of clinical guidance implementation to generate updated clinical guidance documents as output of RICORS2040.
Table 1.
Aims of RICORS2040
| The general aim of RICORS2040 is to improve kidney and person outcomes in men and women with CKD or at high risk of CKD. The name derives from the aim to prove wrong the dire predictions regarding the global burden of CKD by 2040, which closely reflects those for Spain: the GBD collaboration predicts that CKD will become the fifth leading global cause of death by 2040. |
| Specific aims: |
| 1. Improve kidney outcomes in men and women with diabetes or DKD |
| Improve risk stratification in DKD to foster precision nephrology |
| Evaluate novel strategies for kidney protection through therapeutic drug repositioning |
| Develop, evaluate and update the Spanish Clinical Practice Guideline for detection and management of DKD |
| 2. Improve kidney outcomes in men and women with primary glomerular disease |
| Improve risk stratification in glomerular disease to foster precision nephrology |
| Evaluate novel kidney protective approaches in primary glomerular disease |
| Develop, evaluate and update clinical guidance documents |
| 3. Improve kidney outcomes in men and women with inherited kidney disease |
| Increase awareness of inherited kidney disease with special focus on glomerular and tubular kidney disease |
| Improve risk stratification in inherited glomerular disease to foster precision nephrology |
| Identify genetic predictors of CKD progression |
| Develop, evaluate and update clinical guidance documents |
| 4. Define accelerated kidney ageing as a cause of CKD and slow the loss of GFR in men and women |
| Develop a working definition of accelerated kidney ageing |
| Develop tools to predict and assess rapid CKD progression |
| Test novel therapeutic approaches to kidney protection |
| Develop, evaluate and update clinical guidance documents |
| 5. Improve kidney allograft outcomes and improve the outcomes in men and women with a functioning kidney graft |
| Improve the outcome of chronic allograft nephropathy, decreasing graft loss |
| Limit the negative impact of immunosuppressive therapies on comorbidities and life-threatening complications |
| Develop, evaluate and update clinical guidance documents for precision immunosuppression |
| 6. Improve the outcomes of men and women with CKD by targeting the accelerated biological ageing that is a consequence of CKD |
| Develop novel risk stratification tools for cardiovascular disease and CKD–mineral and bone disorder (MBD) to foster precision nephrology. |
| Improve the recognition and outcome of frailty |
| Evaluate the long-term safety and efficacy of SARS-CoV-2 vaccines in persons with advanced CKD |
| Develop, evaluate and update clinical guidance documents on key consequences of CKD, such as cardiovascular disease, CKD-MBD, frailty and susceptibility to severe SARS-CoV-2 infection |
RICORS2040 WITHIN THE WIDER MOVEMENT TOWARDS ADDRESSING THE PLIGHT OF PERSONS WITH KIDNEY DISEASE
RICORS2040 addresses CKD, the predicted fifth leading global cause of death by 2040. Currently there is no confirmed funded research network on CKD for 2022 in Spain, as the current RETIC REDINREN expires in 2021. RICORS2040 will build upon knowledge, resources and collaborations developed by REDINREN. RICORS2040 is aligned with a major international movement to improve the outcomes of persons with kidney disease through investment in kidney research. In this regard, RICORS2040 follows the plea of Vanholder et al. representing major European scientific and patient associations, nephrology professionals, patients and their families, caregivers and kidney health advocacy organizations to draw the attention of authorities to realize changes in understanding, research and treatment of kidney disease during the Decade of the Kidney (2020–2030) [17, 46]. It is also aligned with the AAKH initiative, the American National Kidney Foundation and the American Society of Nephrology, which advocate for increased funding for the National Institute of Diabetes and Digestive and Kidney Diseases [34, 44]. The long-term goal is to reduce the burden of kidney disease and improve the quality of life of persons living with kidney disease. Kidney research is in dire need of research funding support, and this would be best achieved through the collaboration of all major stakeholders, from patient and scientific organizations to pharmaceutical companies to international, national and public funders.
MAJOR SHORTCOMINGS IN SPAIN’S HEALTH RESEARCH FUNDING STRUCTURE
The ISCIII is the main funder of health research in Spain and has long fostered successful collaborative research structures through dedicated research centres [e.g. Spanish National Cancer Research Centre (CNIO) and Spanish National Cardiovascular Research Centre (CNIC)]. Additionally, the ISCIII currently funds research networks for most major predicted 2040 global causes of death [14]: ischaemic heart disease (CIBERCV), stroke (CIBERCV and from 2022, stroke RICORS), infection (CIBER from 2022) and chronic obstructive pulmonary disease. The ISCIII research networks also fund projected 2040 causes of death ranked below CKD (e.g. CIBERONC for cancer and CIBERDEM for diabetes). In fact, in 2022, CKD will become the only top-15 predicted worldwide cause of death that is not supported by the ISCIII CIBER programme (Figure 4B). This represents a major, correctable gap in Spain’s health research funding structure since there is also no dedicated research centre for kidney research. In this environment, the success of RICORS2040 would be critical for the survival of collaborative kidney research in Spain, although the ultimate aim would not be survival, but expansion according to the projected global burden of CKD.
Supplementary Material
APPENDIX
Asociación para la información y la investigación de las enfermedades renales genéticas (AIRG-E)
Marta RogerPresidenta
Víctor Martínez JiménezHospital Virgen de la Arrixaca de Murcia
José Carlos Rodríguez PerezHospital Universitario de Gran Canaria Dr. Negrin
Mónica FurlanoFundació Puigvert
Laia Sans AtxerParc De Salut Mar
Federación Europea de Pacientes Renales (EKPF)
Daniel Gallego Zurro
Asociación para la lucha Contra las Enfermedades Renales (ALCER):
Carlos María Romeo Casabona
Daniel Gallego Zurro
Clemente Gómez Gómez
Pilar Pérez Bermúdez
Manuel Arellano Armisen
Santiago Albaladejo López
Inmaculada Gutiérrez Porras
Josefa Gómez Ruiz
José Manuel Martin Orgaz
Marta Moreno Barón
Sociedad Española de Nefrología (SENEFRO) council:
Patricia de Sequera OrtizHospital Universitario Infanta Leonor
Gabriel de Arriba de la FuenteHospital Universitario de Guadalajara
Borja Quiroga GiliHospital Universitario de la Princesa
Gema Fernández FresnedoHospital Universitario Marqués de Valdecilla
Sagrario Soriano CabreraHospital Universitario Reina Sofía de Córdoba
Javier Pérez ContrerasHospital General Universitario de Alicante
Miquel Blasco PelicanoHospital Clinic de Barcelona
Auxiliadora Mazuecos BlancaHospital Puerta del Mar
Mariano Rodríguez PortilloHospital Universitario Reina Sofía de Córdoba
J. Emilio Sánchez ÁlvarezHospital Universitario de Cabueñes
María José Soler RomeoHospital Universitario General Vall d'Hebrón
Manuel Gorostidi PérezHospital Universitario Central de Asturias
Marian Goicoechea DiezhandinoHospital General Universitario Gregorio Marañón
Sociedad Española de Trasplante (SET) council,
Domingo Hernández MarreroTrasplante Renal. Hospital Regional Universitario de Málaga
Constantino Fondevila CampoTrasplante Hepático. Hospital Clinic de Barcelona
EduardoMiñambres GarcíaCoordinación Trasplantes. Hospital Universitario Marqués de Valdecilla
DoloresGarcía- Cosío CarmonaTrasplante Cardiaco. Hospital 12 de Octubre
Armando Torres RamírezTrasplante Renal. Hospital Universitario de Canarias
Luis Muñoz BellvisCirugía HBP. Complejo Asistencial Universitario de Salamanca
Marina Berenguer HaymTrasplante Hepático. Hospital Universitario y Politécnico de la Fe
Manuel Barrera GómezTrasplante Hepático. Hospital Universitario Nuestra Señora de la Candelaria
José Manuel Cifrián MartínezGrupo de Trasplante Pulmonar. Hospital Universitario Marqués de Valdecilla
Josep María Cruzado GarritTrasplante Renal. Hospital Universitario de Bellvitge
Rafael San Juan GarridoEspecialidad en Enfermedades Infecciosas. Hospital 12 de Octubre
Javier Briceño DelgadoAsociación Española de Cirugía. Hospital Universitario Reina Sofía de Córdoba
Marta Bodro MarimontGrupo de Estudio de la Infección en el Trasplante (GESITRA)/Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica (SEIMC). Hospital Clinic de Barcelona
María O. Valentín MuñozOrganización Nacional de Trasplantes (ONT)
José Miguel Pérez VillaresSociedad Española de Medicina Intensiva Critica y Unidades Coronarias (SEMICYUC). Hospital Universitario Virgen de las Nieves
Ángel Salvatierra VelázquezGrupo de Trasplante de Pulmón de la Sociedad Española de Neumología y Cirugía Torácica (SEPAR). Hospital Universitario Reina Sofía de Córdoba
Luis Almenar BonetSección Trasplante Cardíaco de la Sociedad Española de Cardiología. Hospital Universitario y Politécnico de la Fe de Valencia
Miguel Ángel Gómez BravoSociedad Andaluza de Trasplantes. Hospital Virgen del Rocío
Francesc J. Moreso MateosSociedad Catalana de Trasplantes. Hospital Universitario Vall d`Hebrón
Manuel Muro AmadorSociedad Española de InmunologíaMurcia.Hospital Virgen de la Arrixaca
Auxiliadora Mazuecos BlancaSociedad Española de Nefrología. Hospital del Mar
José A. Pons MiñanoSociedad Española de Trasplante Hepático. Hospital Virgen de la Arrixaca
Amado Andrés BelmonteSociedad Madrileña de Trasplantes. Hospital 12 de Octubre
Amparo Solé JoverSociedad Valenciana de Trasplante. Hospital Universitario y Politécnico de La Fe
Daniel Casanova RituertoEuropean Union of Medical Specialists (UEMS) Committe Board. Hospital Universitario Marqués de Valdecilla
Fernando Pardo Sánchez UEMS Committe Board. Clínica Universidad de Navarra.
Fundación Renal Íñigo Álvarez de Toledo:
María Dolores Arenas MD PhD
Roberto Martin Hernández MD
Blanca Miranda Serrano MD PhD
RICORS2040/REDINREN:
Alberto Ortiz ArduanFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Ana B SanzFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Adrian M RamosFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Gina Córdoba-DavidFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Jorge García-JiménezFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Miguel Fontecha-Barriuso Fundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Juan Guerrero-MauvecinFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Ana M. Lopez-DíazFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
María Dolores Sánchez-NiñoFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Lara Valiño-RivasFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Leticia CuarentalFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Marta RibagordaFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Aranzazu Pintor-ChocanoFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Chiara FaveroFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Gloria Alvarez-LlamasFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Martín Cleary CatalinaFundación Jiménez Díaz
Beatriz Fernández-FernándezFundación Jiménez Díaz
María Vanessa Pérez-GómezFundación Jiménez Díaz
Emma Raquel Alegre de MontanerFundación Jiménez Díaz
Raúl Fernández PradoFundación Jiménez Díaz
Jorge Rojas RiveraFundación Jiménez Díaz
Ana María Ramos VerdeFundación Jiménez Díaz
Sergio Luis-LimaFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Jinny Sánchez-RodríguezFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Soledad Pizarro SánchezHospital Universitario Rey Juan Carlos
Marta Ruiz OrtegaUniversidad Autónoma de Madrid
Emilio González ParraFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Sandra Rayego MateosUniversidad Autónoma de Madrid
Pablo Javier Cannata OrtizFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Laura Márquez ExpósitoUniversidad Autónoma de Madrid
Antonio Tejera-MuñozFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Vanessa MarchantUniversidad Autónoma de Madrid
Lucia Tejedor-SantamariaFundación Instituto de Investigación Sanitaria Fundación Jiménez Díaz
Matilde Alique AgilarUniversidad de Alcalá de Henares
Fritz DiekmannFundación Privada Clínic. Hospital Clínic de Barcelona. Institut D'investigacions Biomèdiques August Pi I Sunyer (IDIBAPS)
Beatriz Bayes GenisHospital Clínic de Barcelona
Federico Oppenheimer SalinasHospital Clínic de Barcelona. Institut D'investigacions Biomèdiques August Pi I Sunyer (IDIBAPS)
María José Ramírez BajoFundació Privada Clínic
Elisenda Bañon ManeusFundació Privada Clínic. Institut D'investigacions Biomèdiques August Pi I Sunyer (IDIBAPS)
Marta Arias GuillenHospital Clínic de Barcelona
Jordi Rovira JuárezInstitut D'investigacions Biomèdiques August Pi I Sunyer (IDIBAPS)
Marta Lazo RodríguezFundació Privada Clínic
Ignacio Revuelta VicenteHospital Clínic de Barcelona. Institut D'investigacions Biomèdiques August Pi I Sunyer (IDIBAPS)
Josep Miquel Blasco PelicanoHospital Clínic de Barcelona
Luis Fernando Quintana PorrasHospital Clínic de Barcelona. Institut D'investigacions Biomèdiques August Pi I Sunyer (IDIBAPS)
Pedro Ventura Abreu AguiarHospital Clínic de Barcelona. Institut D'investigacions Biomèdiques August Pi I Sunyer (IDIBAPS)
Marc Xipell FontInstitut D'investigacions Biomèdiques August Pi I Sunyer (IDIBAPS)
Alicia Molina AndujarHospital Clínic de Barcelona
David CucchiariHospital Clínic de Barcelona. Institut D'investigacions Biomèdiques August Pi I Sunyer (IDIBAPS)
Enrique Montagud MarrahHospital Clínic de Barcelona
Josep MCampistol Plana Hospital Clínic de Barcelona. Institut D'investigacions Biomèdiques August Pi I Sunyer (IDIBAPS)
Gastón Julio PiñeiroHospital Clínic de Barcelona
Carlos Martínez SalgadoFundación Instituto de Estudios de Ciencias de la Salud de Castilla y León (IECSCYL). Institute of Biomedical Research of Salamanca (IBSAL)
Ana I. Morales MartínInstitute of Biomedical Research of Salamanca (IBSAL)
Francisco J.López HernándezInstitute of Biomedical Research of Salamanca (IBSAL)
Nélida Eleno BalboaInstitute of Biomedical Research of Salamanca (IBSAL)
Marta Prieto VicenteInstitute of Biomedical Research of Salamanca (IBSAL)
Isabel Fuentes CalvoInstitute of Biomedical Research of Salamanca (IBSAL)
Laura Ramudo GonzálezInstitute of Biomedical Research of Salamanca (IBSAL)
Laura Vicente VicenteInstitute of Biomedical Research of Salamanca (IBSAL)
Sandra M. Sancho MartínezInstitute of Biomedical Research of Salamanca (IBSAL)
Alfredo G. Casanova PasoInstitute of Biomedical Research of Salamanca (IBSAL)
Moisés Pescador GarrielInstitute of Biomedical Research of Salamanca (IBSAL)
Juan José Vaquero LópezUniversidad de Alcalá
Ana María Cuadro PalaciosUniversidad de Alcalá
David Sucunza SaénzUniversidad de Alcalá
Patricia García GarcíaUniversidad de Alcalá
José Luis Aceña BonillaUniversidad de Alcalá
Manuel A. Fernández RodríguezUniversidad de Alcalá
Alberto Domingo GalánUniversidad de Alcalá
Estíbaliz Merino MarcosUniversidad de Alcalá
Javier Carreras Pérez-AradrosUniversidad de Alcalá
Rubén Manzano San JoséUniversidad de Alcalá
Francisco Maqueda ZelayaUniversidad de Alcalá
Ester Sans PanadésUniversidad de Alcalá
Álvaro González MolinaUniversidad de Alcalá
Julia Atarejos SalidoUniversidad de Alcalá
Roser Torra BalcellsFundació Puigvert
Elisabet Ars CriachFundació Puigvert
Montserrat Díaz EncarnaciónFundació Puigvert
Lluis Guirado PerichFundació Puigvert
Monica FurlanoFundació Puigvert
Cristina Canal GirolFundació Puigvert
Yolanda Arce TerrobaFundació Puigvert
Marc Pybus OliverasFundació Puigvert
Laia Ejarque VilaFundació Puigvert
Nuria Serra CabañasFundació Puigvert
Carme Facundo MolasFundació Puigvert
Irene Silva TorresFundació Puigvert
Santiago Lamas PelaezCentro de Biología Molecular Severo Ochoa
Carlos Rey SerraCentro de Biología Molecular Severo Ochoa
Carolina Castillo TorresHospital Príncipe de Asturias
Jessica Paola Tituaña FajardoCentro de Biología Molecular Severo Ochoa
José Ignacio Herrero LahuertaCentro de Biología Molecular Severo Ochoa
Verónica Miguel HerranzCentro de Biología Molecular Severo Ochoa
Mariano Rodriguez PortilloHospital Reina Sofía
Alejandro Martin MaloHospital Reina Sofía
Sagrario Soriano CabreraHospital Reina Sofía
Juan Rafael Muñoz CastañedaInstituto Maimonides de Investigación Biomédica de Córdoba (IMIBIC)
María Encarnación Rodríguez OrtizInstituto Maimonides de Investigación Biomédica de Córdoba (IMIBIC)
Julio Manuel Martínez MorenoInstituto Maimonides de Investigación Biomédica de Córdoba (IMIBIC)
Ana Isabel Raya BermúdezInstituto Maimonides de Investigación Biomédica de Córdoba (IMIBIC)
Rafael Santamaría OlmoHospital Reina Sofía
Fátima Guerrero PavónInstituto Maimonides de Investigación Biomédica de Córdoba (IMIBIC)
Cayetana Moyano PeregrinHospital Reina Sofía
Escolástico Aguilera TejeroInstituto Maimonides de Investigación Biomédica de Córdoba (IMIBIC)
Ignacio Lopez VillalbaInstituto Maimonides de Investigación Biomédica de Córdoba (IMIBIC)
Andrés Carmona MuñozInstituto Maimonides de Investigación Biomédica de Córdoba (IMIBIC)
María Victoria Pendon Ruiz De MierHospital Reina Sofía
Carmen María Pineda MartosInstituto Maimonides de Investigación Biomédica de Córdoba (IMIBIC)
Rodrigo López BaltanasInstituto Maimonides de Investigación Biomédica de Córdoba (IMIBIC)
Cristian Rodelo HaadHospital Reina Sofía
Marcella Franquesa BartoloméFundación Instituto Investigación Germans Trias I Pujol
Ricardo Lauzurica ValdemorosHospital Germans Trias I Pujol
Francisco Enrique Borras SerresFundación Instituto Investigación Germans Trias I Pujol
Maruja Navarro DíazHospital Germans Trias I Pujol
Francisco Javier Juega MariñoHospital Germans Trias I Pujol
Laura Cañas SoleHospital Germans Trias I Pujol
Maria Isabel Troya SaboridoHospital Germans Trias I Pujol
Jordi Soler MajoralHospital Germans Trias I Pujol
Marina López MartínezHospital Germans Trias I Pujol
Emilio Rodrigo CalabiaUniversity Hospital Marqués de Valdecilla/IDIVAL, University of Cantabria
Juan Carlos Ruiz San MillánUniversity Hospital Marqués de Valdecilla/IDIVAL, University of Cantabria
Marcos López-HoyosUniversity Hospital Marqués de Valdecilla/IDIVAL, University of Cantabria
Adalberto Benito-HernándezUniversity Hospital Marqués de Valdecilla/IDIVAL, University of Cantabria
Gema Fernández FresnedoUniversity Hospital Marqués de Valdecilla/IDIVAL, University of Cantabria
David San SegundoUniversity Hospital Marqués de Valdecilla/IDIVAL, University of Cantabria
Rosalía ValeroUniversity Hospital Marqués de Valdecilla/IDIVAL, University of Cantabria
Eliécer Coto GarcíaHospital Universitario Central de Asturias
Juan Gómez De OnaHospital Universitario Central de Asturias
Elias Cuesta LlavonaHospital Universitario Central de Asturias
Fernando Santos RodríguezHospital Universitario Central de Asturias
Rebeca Lorca GutiérrezHospital Universitario Central de Asturias
Helena Gil PeñaHospital Universitario Central de Asturias
Manuel Gorostidi PérezHospital Universitario Central de Asturias
Domingo Hernández MarreroInstituto de Investigación Biomédica de Málaga (IBIMA)
Verónica LópezHospital Regional Universitario de Malaga/IBIMA
Eugenia SolaHospital Regional Universitario de Malaga/IBIMA
Mercedes CabelloHospital Regional Universitario de Malaga/IBIMA
Abelardo CaballeroHospital Regional Universitario de Malaga/IBIMA
Myriam LeónHospital Regional Universitario de Malaga/IBIMA
Pedro RuizHospital Regional Universitario de Malaga/IBIMA
Juana AlonsoHospital Regional Universitario de Malaga/IBIMA
Juan Navarro-GonzálezHospital Nuestra Sra. Candelaria, Tenerife
María Del Carmen Mora-FernándezHospital Universitario Nuestra Señora de Candelaria
Javier Donate-CorreaHospital Universitario Nuestra Señora de Candelaria
Ernesto Martín-NuñezHospital Universitario Nuestra Señora de Candelaria
Nayra Pérez DelgadoHospital Universitario Nuestra Señora de Candelaria
Secundino Gigarrán-GuldrisHospital Da Costa, Burela
José Carlos Rodríguez PérezHospital Universitario Dr. Negrín
José Luis Górriz TeruelHospital Clínico Universitario de Valencia
Alberto Martínez CastelaoHospital Universitario Bellvitge, Hospitalec, Barcelona
José Manuel Valdivielso RevillaInstituto de Investigación Biomédica de Lleida. Fundación Dr. Pifarre (IRBLLEIDA)
Cristina Martínez MartínezInstituto de Investigación Biomédica de Lleida. Fundación Dr. Pifarre (IRBLLEIDA)
Milica Bozic StanojevicInstituto de Investigación Biomédica de Lleida. Fundación Dr. Pifarre (IRBLLEIDA)
Eva Castro BoqueInstituto de Investigación Biomédica de Lleida. Fundación Dr. Pifarre (IRBLLEIDA)
María Nuria Sans RosellInstituto de Investigación Biomédica de Lleida. Fundación Dr. Pifarre (IRBLLEIDA)
Virtudes Maria De LamoInstituto de Investigación Biomédica de Lleida. Fundación Dr. Pifarre (IRBLLEIDA)
Juan Miguel Díaz TocadosInstituto de Investigación Biomédica de Lleida. Fundación Dr. Pifarre (IRBLLEIDA)
Alicia Garcia CarrascoInstituto de Investigación Biomédica de Lleida. Fundación Dr. Pifarre (IRBLLEIDA)
Marcelino Bermúdez LópezInstituto de Investigación Biomédica de Lleida. Fundación Dr. Pifarre (IRBLLEIDA)
Maite Caus EnriquezInstituto de Investigación Biomédica de Lleida. Fundación Dr. Pifarre (IRBLLEIDA)
Ana Martinez BardajiInstituto de Investigación Biomédica de Lleida. Fundación Dr. Pifarre (IRBLLEIDA)
Nuria Dolade MasotInstituto de Investigación Biomédica de Lleida. Fundación Dr. Pifarre (IRBLLEIDA)
Aurora Pérez GómezInstituto de Investigación Biomédica de Lleida. Fundación Dr. Pifarre (IRBLLEIDA)
Auria Eritja SanjuanInstituto de Investigación Biomédica de Lleida. Fundación Dr. Pifarre (IRBLLEIDA)
Antonio Osuna OrtegaHospital Universitario Virgen de las Nieves de Granada
Rosemary Wangensteen FuentesUniversidad de Jaén
Maria del Carmen De Gracia GuindoHospital Universitario Virgen de las Nieves de Granada
Maria del Carmen Ruiz FuentesHospital Universitario Virgen de las Nieves de Granada
Francisco O’Valle RavassaUniversidad de Granada
Mercedes Caba MolinaHospital Universitario San Cecilio
César Luis Ramírez TortosaHospital Universitario San Cecilio
Raimundo García Del Moral GarridoUniversidad de Granada
María José Soler RomeoFundación Instituto de Investigación Valle de Hebrón
Conxita Jacobs-CacháVall D’Hebron Research Institute (VHIR)
Oriol Bestard MatamorosVall D’Hebron Research Institute (VHIR)
Francesc Moreso MateosVall D’Hebron Research Institute (VHIR)
María Antonia Emilia MeneghiniVall D’Hebron Research Institute (VHIR)
Joana Sellares RoigHospital Universitari Vall D´Hebron
Irina Torres BetsabéHospital Universitari Vall D´Hebron
Carlos López LarreaHospital Universitario Central de Asturias. Instituto de Investigación Sanitaria del Principado de Asturias
Beatriz Suarez ÁlvarezInstituto de Investigación Sanitaria del Principado de Asturias
María del Carmen Díaz CorteHospital Universitario Central de Asturias. Instituto de Investigación Sanitaria del Principado de Asturias
Raúl R Rodrigues-DiezInstituto de Investigación Sanitaria del Principado de Asturias
Antonio López VázquezHospital Universitario Central de Asturias. Instituto de Investigación Sanitaria del Principado de Asturias
Segundo González RodríguezUniversidad de Oviedo
José Ramón Vidal CastiñeiraHospital Universitario Central de Asturias. Instituto de Investigación Sanitaria del Principado de Asturias
Cristina Martín MartínInstituto de Investigación Sanitaria del Principado de Asturias
María Laura Saiz ÁlvarezInstituto de Investigación Sanitaria del Principado de Asturias
Viviana Corte IglesiasInstituto de Investigación Sanitaria del Principado de Asturias
Jesús Martínez BorraHospital Universitario Central de Asturias. Instituto de Investigación Sanitaria del Principado de Asturias
María Auxiliadora Bajo RubioHospital Universitario La Paz
Gloria Del Peso GilsanzHospital Universitario La Paz
Manuel López CabreraCentro de Biología Molecular Severo Ochoa
José Antonio Jiménez HeffernanHospital Universitario La Princesa
Marta Ossorio GonzálezHospital Universitario La Paz
Olga Costero GonzálezHospital Universitario La Paz
María Elena González GarcíaHospital Universitario La Paz
Carlos Jiménez MartínHospital Universitario La Paz
Pilar Sandoval CorreaCentro de Biología Molecular Severo Ochoa
Sara Afonso RamosHospital Universitario La Paz
María López OlivaHospital Universitario La Paz
Begoña Rivas BecerraHospital Universitario La Paz
Cristina Vega CabreraHospital Universitario La Paz
Guadalupe Tirma González MateoCentro de Biología Molecular Severo Ochoa
Rafael Sánchez VillanuevaHospital Universitario La Paz
Laura Álvarez GarcíaHospital Universitario La Paz
Jorge B Cannata AndíaHospital Universitario Central de Asturias. Instituto de Investigación Sanitaria del Principado de Asturias
Manuel Naves DíazHospital Universitario Central de Asturias. Instituto de Investigación Sanitaria del Principado de Asturias
José Luis Fernández MartínHospital Universitario Central de Asturias. Instituto de Investigación Sanitaria del Principado de Asturias
Natalia Carrillo LópezInstituto de Investigación Sanitaria del Principado de Asturias
Sara Panizo GarcíaInstituto de Investigación Sanitaria del Principado de Asturias
Cristina Alonso MontesInstituto de Investigación Sanitaria del Principado de Asturias
Minerva Rodríguez GarcíaHospital Universitario Central de Asturias. Instituto de Investigación Sanitaria del Principado de Asturias
Iñigo Lozano Martínez LuengasHospital de Cabueñes
Emilio Sánchez ÁlvarezHospital de Cabueñes
Laura Martínez AriasInstituto de Investigación Sanitaria del Principado de Asturias
Beatriz Martín CarroInstituto de Investigación Sanitaria del Principado de Asturias
Julia Martín VirgalaInstituto de Investigación Sanitaria del Principado de Asturias
Miguel García GonzálezComplejo Hospitalario de Santiago de Compostela (CHUS). Instituto de Investigación Sanitaria (IDIS)
José María Lamas BarreiroComplejo Hospitalario Universitario de Vigo
Miguel Pérez FontanComplejo Hospitalario Universitario A Coruña
Alfonso Otero GonzálezComplejo Hospitalario Universitario de Ourense
Luz María Cuiña BarjaComplejo Hospitalario de Pontevedra
Alejandro Sánchez BarreiroUniversidad de Santiago de Compostela
Beatriz Pazos AriasPoliclínico Vigo S.A.
Ángel Alonso HernándezComplejo Hospitalario Universitario A Coruña
María Pardo PérezInstituto de Investigación Sanitaria de Santiago de Compostela (IDIS)
Jesús Calviño VarelaHospital Lucus Augusti
Jorge Amigo LechugaFundación Pública Gallega de Medicina Genómica
Cándido Díaz RodríguezHospital Clínico Universitario de Santiago
María García MuriasInstituto de Investigación Sanitaria de Santiago de Compostela (IDIS)
Ana María Barcia de la IglesiaInstituto de Investigación Sanitaria de Santiago de Compostela (IDIS)
Pablo Bouza PiñeiroComplejo Hospitalario A. Marcide-Novoa Santos
Álvaro Gil GonzálezUniversidad de Santiago de Compostela
Adrian Cordido EijoInstituto de Investigación Sanitaria de Santiago de Compostela (IDIS)
Noa Carrera CachazaInstituto de Investigación Sanitaria de Santiago de Compostela (IDIS)
Marta Vizoso GonzálezInstituto de Investigación Sanitaria de Santiago de Compostela (IDIS)
Josep Maria Cruzado GarritHospital de Bellvitge
Núria Lloberas BlanchFundación Idibell
Ana Maria Sola MartínezFundación Idibell
Miguel Hueso ValHospital de Bellvitge
Juliana BordignonDraibeHospital de Bellvitge
Edoardo MelilliHospital de Bellvitge
Anna Manonelles MonteroHospital de Bellvitge
Núria Montero PérezHospital de Bellvitge
Xavier Fulladosa OliverasHospital de Bellvitge
Marta Crespo BarrioInstituto Hospital del Mar de Investigaciones Médicas (FIMIM)
Julio Pascual SantosInstituto Hospital del Mar de Investigaciones Médicas (FIMIM)
Clara Barrios BarreraInstituto Hospital del Mar de Investigaciones Médicas (FIMIM)
María José Pérez SáezInstituto Hospital del Mar de Investigaciones Médicas (FIMIM)
María Dolores Redondo PachónInstituto Hospital del Mar de Investigaciones Médicas (FIMIM)
Carlos Arias CabralesInstituto Hospital del Mar de Investigaciones Médicas (FIMIM)
Anna Buxeda PorrasInstituto Hospital del Mar de Investigaciones Médicas (FIMIM)
Eva Rodríguez GarcíaInstituto Hospital del Mar de Investigaciones Médicas (FIMIM)
Laia Sans AtxerInstituto Hospital del Mar de Investigaciones Médicas (FIMIM)
Vanesa Palau GonzálezInstituto Hospital del Mar de Investigaciones Médicas (FIMIM)
Laura Llinàs MallolInstituto Hospital del Mar de Investigaciones Médicas (FIMIM)
Marta Riera OlivaInstituto Hospital del Mar de Investigaciones Médicas (FIMIM)
Diego Rodríguez PuyolFundación Investigación Biomédica. Hospital Príncipe de Asturias
María Piedad Ruiz TorresUniversidad de Alcalá
Susana López OngilFundación Investigación Biomédica. Hospital Príncipe de Asturias
Laura Calleros BasilioUniversidad de Alcalá
Gemma Olmos CenteneraUniversidad de Alcalá
Patricia Martínez de MiguelHospital Universitario Príncipe de Asturias
Loreto Fernández RodríguezHospital Universitario Príncipe de Asturias
Hanane Bouarich NadahHospital Universitario Príncipe de Asturias
María Pérez FernándezHospital Universitario Príncipe de Asturias
Manuel Rafael Ramírez ChamondUniversidad de Alcalá
Patricia Sequera OrtizHospital Universitario Infanta Leonor
Nuria García FernándezInstituto de Investigación Sanitaria de Navarra (IDISNA),
Alberto Benito BoillosUniversidad de Navarra
Nerea Varo CenarruzabeitiaUniversidad de Navarra
María Asunción Fernández SearaUniversidad de Navarra
Inés Díaz Dorronsoro,Universidad de Navarra
Paloma Martin MorenoClínica Universidad de Navarra
Francisco Javier LavillaClínica Universidad de Navarra
Armando TorresHospital Universitario de Canarias. Universidad de La Laguna
Domingo Marrero MirandaHospital Universitario de Canarias
Aurelio Pastor Rodríguez HernándezHospital Universitario de Canarias
Eduardo De Bonis RedondoHospital Universitario de Canarias
Esteban PorriniUniversidad de La Laguna
María de los Ángeles Cobo CasoHospital Universitario de Canarias
María Lourdes Pérez TamajónHospital Universitario de Canarias
Margarita Rufino HernándezHospital Universitario de Canarias
María Sagrario García RebolloHospital Universitario de Canarias
Patricia Delgado MallenHospital Universitario de Canarias
Alejandra Álvarez GonzálezHospital Universitario de Canarias
Ana María González RinneHospital Universitario de Canarias
Rosa Miquel RodríguezHospital Universitario de Canarias
Sara Estupiñan TorresHospital Universitario de Canarias
Diego Álvarez SosaHospital Universitario de Canarias
Beatriz Escamilla CabreraHospital Universitario de Canarias
Nayara Zamora RodríguezHospital Universitario de Canarias
Arminda Fariña HernándezHospital Universitario de Canarias
María José Rodríguez GamboaHospital Universitario de Canarias
Cobo Caso, Maria de Los AngelesHospital Universitario de Canarias
PerezTamajon, Maria LourdesHospital Universitario de Canarias
Rufino Hernandez, MargaritaHospital Universitario de Canarias
Garcia Rebollo, Maria SagrarioHospital Universitario de Canarias
Delgado Mallen, PatriciaHospital Universitario de Canarias
AlvarezGonzalez, AlejandraHospital Universitario de Canarias
Gonzalez Rinne, Ana MariaHospital Universitario de Canarias
Miquel Rodriguez, RosaHospital Universitario de Canarias
Estupiñan Torres, SaraHospital Universitario de Canarias
Alvarez Sosa, DiegoHospital Universitario de Canarias
Escamilla Cabrera, BeatrizHospital Universitario de Canarias
Zamora Rodiguez, NayaraHospital Universitario de Canarias
Fariña Hernandez, ArmindaHospital Universitario de Canarias
Rodriguez Gamboa, MariaJoseHospital Universitario de Canarias
María Laura García BermejoInstituto Ramón y Cajal de Investigación Sanitaria (IRYCIS)
Milagros Fernández LucasHospital Ramón y Cajal
Elisa Conde MorenoInstituto Ramón y Cajal de Investigación Sanitaria (IRYCIS)
Laura Salinas MuñozInstituto Ramón y Cajal de Investigación Sanitaria (IRYCIS)
Silvia Serrano HuertasInstituto Ramón y Cajal de Investigación Sanitaria (IRYCIS)
Esperanza Macarena Rodríguez SerranoInstituto Ramón y Cajal de Investigación Sanitaria (IRYCIS)
Miren Edurne Ramos MuñozInstituto Ramón y Cajal de Investigación Sanitaria (IRYCIS)
Lorena Crespo ToroInstituto Ramón y Cajal de Investigación Sanitaria (IRYCIS)
Carolina Pilar Blanco AgudoInstituto Ramón y Cajal de Investigación Sanitaria (IRYCIS)
Cristina Galeano ÁlvarezInstituto Ramón y Cajal de Investigación Sanitaria (IRYCIS)
José PortolesFundación Investigación Biomédica Hospital Puerta de Hierro
María MarquésFundación Investigación Biomédica Hospital Puerta de Hierro
Esther RubioFundación Investigación Biomédica Hospital Puerta de Hierro
Beatriz Sánchez-SobrinoFundación Investigación Biomédica Hospital Puerta de Hierro
Estefanya García-MenéndezFundación Investigación Biomédica Hospital Puerta de Hierro
Alberto Lázaro FernándezUniversidad Complutense de Madrid
Marian Goicoechea DiezhandinIISGM. Hospital General Universitario Gregorio Marañón
Patrocinio Rodríguez BenítezIISGM. Hospital General Universitario Gregorio Marañón
María Ángeles González-Nicolás GonzálezUniversidad Complutense de Madrid
Meritxell López GallardoUniversidad Complutense de Madrid
Gema María Fernández JuárezHospital Universitario Fundación Alcorcón
Eduardo Gutiérrez MartínezInstituto de Investigación Hospital 12 de Octubre (i+12)
Manuel Praga TerenteInstituto de Investigación Hospital 12 de Octubre (i+12)
Ana Tato RiberaHospital Universitario Fundación Alcorcón
Teresa Cavero EscribanoInstituto de Investigación Hospital 12 de Octubre (i+12)
Fernando Caravaca FontanInstituto de Investigación Hospital 12 de Octubre (i+12)
Amir Shabaka FernándezHospital Universitario Fundación Alcorcón
Nicolás Roberto Robles Pérez - MonteolivaComplejo Hospitalario Universitario de Badajoz
Enrique Luna HuertaComplejo Hospitalario Universitario de Badajoz
Guillermo Gervasini RodríguezFacultad de Medicina de Badajoz
Sergio Barroso HernándezComplejo Hospitalario Universitario de Badajoz
Sonia Mota ZamoranoFacultad de Medicina de Badajoz
Juan Manuel López GómezComplejo Hospitalario Universitario de Badajoz
Román Hernández GallegoComplejo Hospitalario Universitario de Badajoz
Contributor Information
Asociación Información Enfermedades Renales Genéticas (AIRG-E), European Kidney Patients' Federation (EKPF), Federación Nacional de Asociaciones para la Lucha Contra las Enfermedades del Riñón (ALCER), Fundación Renal Íñigo Álvarez de Toledo (FRIAT), Red de Investigación Renal (REDINREN), Resultados en Salud 2040 (RICORS2040), Sociedad Española de Nefrología (SENEFRO) Council, Sociedad Española de Trasplante (SET) Council, Organización Nacional de Trasplantes (ONT):
Marta Roger, Víctor Martínez Jiménez, José Carlos Rodríguez Perez, Mónica Furlano, Laia Sans Atxer, Daniel Gallego Zurro, Carlos María Romeo Casabona, Daniel Gallego Zurro, Clemente Gómez Gómez, Pilar Pérez Bermúdez, Manuel Arellano Armisen, Santiago Albaladejo López, Inmaculada Gutiérrez Porras, Josefa Gómez Ruiz, José Manuel Martin Orgaz, Marta Moreno Barón, Patricia de Sequera Ortiz, Gabriel de Arriba de la Fuente, Borja Quiroga Gili, Gema Fernández Fresnedo, Sagrario Soriano Cabrera, Javier Pérez Contreras, Miquel Blasco Pelicano, Auxiliadora Mazuecos Blanca, Mariano Rodríguez Portillo, J Emilio Sánchez Álvarez, María José Soler Romeo, Manuel Gorostidi Pérez, Marian Goicoechea Diezhandino, Domingo Hernández Marrero, Constantino Fondevila Campo, Eduardo Miñambres García, Dolores García- Cosío Carmona, Armando Torres Ramírez, Luis Muñoz Bellvis, Marina Berenguer Haym, Manuel Barrera Gómez, José Manuel Cifrián Martínez, Josep María Cruzado Garrit, Rafael San Juan Garrido, Javier Briceño Delgado, Marta Bodro Marimont, María O Valentín Muñoz, José Miguel Pérez Villares, Ángel Salvatierra Velázquez, Luis Almenar Bonet, Miguel Ángel Gómez Bravo, Francesc J Moreso Mateos, Manuel Muro Amador, Auxiliadora Mazuecos Blanca, José A Pons Miñano, Amado Andrés Belmonte, Amparo Solé Jover, Daniel Casanova Rituerto, Fernando Pardo Sánchez, María Dolores Arenas, Roberto Martin Hernández, Blanca Miranda Serrano, Alberto Ortiz Arduan, Ana B Sanz, Adrian M Ramos, Gina Córdoba-David, Jorge García-Jiménez, Miguel Fontecha-Barriuso, Juan Guerrero-Mauvecin, Ana M Lopez-Díaz, María Dolores Sánchez-Niño, Lara Valiño-Rivas, Leticia Cuarental, Marta Ribagorda, Aranzazu Pintor-Chocano, Chiara Favero, Gloria Alvarez-Llamas, Martín Cleary Catalina, Beatriz Fernández-Fernández, María Vanessa Pérez-Gómez, Emma Raquel Alegre de Montaner, Raúl Fernández Prado, Jorge Rojas Rivera, Ana María Ramos Verde, Sergio Luis-Lima, Jinny Sánchez-Rodríguez, Soledad Pizarro Sánchez, Marta Ruiz Ortega, Emilio González Parra, Sandra Rayego Mateos, Pablo Javier Cannata Ortiz, Laura Márquez Expósito, Antonio Tejera-Muñoz, Vanessa Marchant, Lucia Tejedor-Santamaria, Matilde Alique Agilar, Fritz Diekmann, Beatriz Bayes Genis, Federico Oppenheimer Salinas, María José Ramírez Bajo, Elisenda Bañon Maneus, Marta Arias Guillen, Jordi Rovira Juárez, Marta Lazo Rodríguez, Ignacio Revuelta Vicente, Josep Miquel Blasco Pelicano, Luis Fernando Quintana Porras, Pedro Ventura Abreu Aguiar, Marc Xipell Font, Alicia Molina Andujar, David Cucchiari, Enrique Montagud Marrah, Josep M, Gastón Julio Piñeiro, Carlos Martínez Salgado, Ana I Morales Martín, Francisco J López Hernández, Nélida Eleno Balboa, Marta Prieto Vicente, Isabel Fuentes Calvo, Laura Ramudo González, Laura Vicente Vicente, Sandra M Sancho Martínez, Alfredo G Casanova Paso, Moisés Pescador Garriel, Juan José Vaquero López, Ana María Cuadro Palacios, David Sucunza Saénz, Patricia García García, José Luis Aceña Bonilla, Manuel A Fernández Rodríguez, Alberto Domingo Galán, Estíbaliz Merino Marcos, Javier Carreras Pérez-Aradros, Rubén Manzano San José, Francisco Maqueda Zelaya, Ester Sans Panadés, Álvaro González Molina, Julia Atarejos Salido, Roser Torra Balcells, Elisabet Ars Criach, Montserrat Díaz Encarnación, Lluis Guirado Perich, Monica Furlano, Cristina Canal Girol, Yolanda Arce Terroba, Marc Pybus Oliveras, Laia Ejarque Vila, Nuria Serra Cabañas, Carme Facundo Molas, Irene Silva Torres, Santiago Lamas Pelaez, Carlos Rey Serra, Carolina Castillo Torres, Jessica Paola Tituaña Fajardo, José Ignacio Herrero Lahuerta, Verónica Miguel Herranz, Mariano Rodriguez Portillo, Alejandro Martin Malo, Sagrario Soriano Cabrera, Juan Rafael Muñoz Castañeda, María Encarnación Rodríguez Ortiz, Julio Manuel Martínez Moreno, Ana Isabel Raya Bermúdez, Rafael Santamaría Olmo, Fátima Guerrero Pavón, Cayetana Moyano Peregrin, Escolástico Aguilera Tejero, Ignacio Lopez Villalba, Andrés Carmona Muñoz, María Victoria Pendon Ruiz De Mier, Carmen María Pineda Martos, Rodrigo López Baltanas, Cristian Rodelo Haad, Marcella Franquesa Bartolomé, Ricardo Lauzurica Valdemoros, Francisco Enrique Borras Serres, Maruja Navarro Díaz, Francisco Javier Juega Mariño, Laura Cañas Sole, Maria Isabel Troya Saborido, Jordi Soler Majoral, Marina López Martínez, Emilio Rodrigo Calabia, Juan Carlos Ruiz San Millán, Marcos López-Hoyos, Adalberto Benito-Hernández, Gema Fernández Fresnedo, David San Segundo, Rosalía Valero, Eliécer Coto García, Juan Gómez De Ona, Elias Cuesta Llavona, Fernando Santos Rodríguez, Rebeca Lorca Gutiérrez, Helena Gil Peña, Manuel Gorostidi Pérez, Domingo Hernández Marrero, Verónica López, Eugenia Sola, Mercedes Cabello, Abelardo Caballero, Myriam León, Pedro Ruiz, Juana Alonso, Juan Navarro-González, María Del Carmen Mora-Fernández, Javier Donate-Correa, Ernesto Martín-Nuñez, Nayra Pérez Delgado, Secundino Gigarrán-Guldris, José Carlos Rodríguez Pérez, José Luis Górriz Teruel, Alberto Martínez Castelao, José Manuel Valdivielso Revilla, Cristina Martínez Martínez, Milica Bozic Stanojevic, Eva Castro Boque, María Nuria Sans Rosell, Virtudes Maria De Lamo, Juan Miguel Díaz Tocados, Alicia Garcia Carrasco, Marcelino Bermúdez López, Maite Caus Enriquez, Ana Martinez Bardaji, Nuria Dolade Masot, Aurora Pérez Gómez, Auria Eritja Sanjuan, Antonio Osuna Ortega, Rosemary Wangensteen Fuentes, Maria del Carmen De Gracia Guindo, Maria del Carmen Ruiz Fuentes, Francisco O'Valle Ravassa, Mercedes Caba Molina, César Luis Ramírez Tortosa, Raimundo García Del Moral Garrido, María José Soler Romeo, Conxita Jacobs-Cachá, Oriol Bestard Matamoros, Francesc Moreso Mateos, María Antonia Emilia Meneghini, Joana Sellares Roig, Irina Torres Betsabé, Carlos López Larrea, Beatriz Suarez Álvarez, María del Carmen Díaz Corte, Raúl R Rodrigues-Diez, Antonio López Vázquez, Segundo González Rodríguez, José Ramón Vidal Castiñeira, Cristina Martín Martín, María Laura Saiz Álvarez, Viviana Corte Iglesias, Jesús Martínez Borra, María Auxiliadora Bajo Rubio, Gloria Del Peso Gilsanz, Manuel López Cabrera, José Antonio Jiménez Heffernan, Marta Ossorio González, Olga Costero González, María Elena González García, Carlos Jiménez Martín, Pilar Sandoval Correa, Sara Afonso Ramos, María López Oliva, Begoña Rivas Becerra, Cristina Vega Cabrera, Guadalupe Tirma González Mateo, Rafael Sánchez Villanueva, Laura Álvarez García, Jorge B Cannata Andía, Manuel Naves Díaz, José Luis Fernández Martín, Natalia Carrillo López, Sara Panizo García, Cristina Alonso Montes, Minerva Rodríguez García, Iñigo Lozano Martínez Luengas, Emilio Sánchez Álvarez, Laura Martínez Arias, Beatriz Martín Carro, Julia Martín Virgala, Miguel García González, José María Lamas Barreiro, Miguel Pérez Fontan, Alfonso Otero González, Luz María Cuiña Barja, Alejandro Sánchez Barreiro, Beatriz Pazos Arias, Ángel Alonso Hernández, María Pardo Pérez, Jesús Calviño Varela, Jorge Amigo Lechuga, Cándido Díaz Rodríguez, María García Murias, Ana María Barcia de la Iglesia, Pablo Bouza Piñeiro, Álvaro Gil González, Adrian Cordido Eijo, Noa Carrera Cachaza, Marta Vizoso González, Josep Maria Cruzado Garrit, Núria Lloberas Blanch, Ana Maria Sola Martínez, Miguel Hueso Val, Juliana BordignonDraibe, Edoardo Melilli, Anna Manonelles Montero, Núria Montero Pérez, Xavier Fulladosa Oliveras, Marta Crespo Barrio, Julio Pascual Santos, Clara Barrios Barrera, María José Pérez Sáez, María Dolores Redondo Pachón, Carlos Arias Cabrales, Anna Buxeda Porras, Eva Rodríguez García, Laia Sans Atxer, Vanesa Palau González, Laura Llinàs Mallol, Marta Riera Oliva, Diego Rodríguez Puyol, María Piedad Ruiz Torres, Susana López Ongil, Laura Calleros Basilio, Gemma Olmos Centenera, Patricia Martínez de Miguel, Loreto Fernández Rodríguez, Hanane Bouarich Nadah, María Pérez Fernández, Manuel Rafael Ramírez Chamond, Patricia Sequera Ortiz, Nuria García Fernández, Alberto Benito Boillos, Nerea Varo Cenarruzabeitia, María Asunción Fernández Seara, Inés Díaz Dorronsoro,, Paloma Martin Moreno, Francisco Javier Lavilla, Armando Torres, Domingo Marrero Miranda, Aurelio Pastor Rodríguez Hernández, Eduardo De Bonis Redondo, Esteban Porrini, María de los Ángeles Cobo Caso, María Lourdes Pérez Tamajón, Margarita Rufino Hernández, María Sagrario García Rebollo, Patricia Delgado Mallen, Alejandra Álvarez González, Ana María González Rinne, Rosa Miquel Rodríguez, Sara Estupiñan Torres, Diego Álvarez Sosa, Beatriz Escamilla Cabrera, Nayara Zamora Rodríguez, Arminda Fariña Hernández, María José Rodríguez Gamboa, Cobo Caso, Maria de Los Angeles, Perez Tamajon, Maria Lourdes, Margarita Rufino Hernandez, Garcia Rebollo, Maria Sagrario, Patricia Delgado Mallen, Alvarez Gonzalez, Alejandra, Gonzalez Rinne, Ana Maria, Rosa Miquel Rodriguez, Sara Estupiñan Torres, Diego Alvarez Sosa, Beatriz Escamilla Cabrera, Nayara Zamora Rodiguez, Arminda Fariña Hernandez, Rodriguez Gamboa, Maria Jose, María Laura García Bermejo, Milagros Fernández Lucas, Elisa Conde Moreno, Laura Salinas Muñoz, Silvia Serrano Huertas, Esperanza Macarena Rodríguez Serrano, Miren Edurne Ramos Muñoz, Lorena Crespo Toro, Carolina Pilar Blanco Agudo, Cristina Galeano Álvarez, José Portoles, María Marqués, Esther Rubio, Beatriz Sánchez-Sobrino, Estefanya García-Menéndez, Alberto Lázaro Fernández, Marian Goicoechea Diezhandin, Patrocinio Rodríguez Benítez, María Ángeles González-Nicolás González, Meritxell López Gallardo, Gema María Fernández Juárez, Eduardo Gutiérrez Martínez, Manuel Praga Terente, Ana Tato Ribera, Teresa Cavero Escribano, Fernando Caravaca Fontan, Amir Shabaka Fernández, Nicolás Roberto Robles Pérez - Monteoliva, Enrique Luna Huerta, Guillermo Gervasini Rodríguez, Sergio Barroso Hernández, Sonia Mota Zamorano, Juan Manuel López Gómez, and Román Hernández Gallego
SUPPLEMENTARY DATA
Supplementary data are available at ckj online.
FUNDING
This study was supported by REDINREN RD16/0009 by the Instituto de Salud Carlos III (ISCIII).
CONFLICT OF INTEREST STATEMENT
Authors are members of scientific and patient associations with an interest in improving the outcomes and quality of life of persons with kidney disease. A.O. is Editor in Chief for Clinical Kidney Journal, Maria Jose Soler is Associate Editor and Editor in Chief elect for Clinical Kidney Journal and Roser Torra and Jose Maria Cruzado are Associate Editors for Clinical Kidney Journal.
REFERENCES
- 1. Kidney Disease: Improving Global Outcomes CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 2013; 3: 1–150. [DOI] [PubMed] [Google Scholar]
- 2. Perez-Gomez MV, Bartsch LA, Castillo-Rodriguez E. et al. Clarifying the concept of chronic kidney disease for non-nephrologists. Clin Kidney J 2019; 12: 258–226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Matsushita K, Coresh J, Sang Y. et al. Estimated glomerular filtration rate and albuminuria for prediction of cardiovascular outcomes: a collaborative meta-analysis of individual participant data. Lancet Diabetes Endocrinol 2015; 3: 514–525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hallan SI, Matsushita K, Sang Y. et al. Age and association of kidney measures with mortality and end-stage renal disease. JAMA 2012; 308: 2349–2360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ortiz A, Covic A, Fliser D. et al. Epidemiology, contributors to, and clinical trials of mortality risk in chronic kidney failure. Lancet 2014; 383: 1831–1843 [DOI] [PubMed] [Google Scholar]
- 6. Chawla LS, Eggers PW, Star RA. et al. Acute kidney injury and chronic kidney disease as interconnected syndromes. N Engl J Med 2014; 371: 58–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Martin-Cleary C, Molinero-Casares LM, Ortiz A. et al. Development and internal validation of a prediction model for hospital-acquired acute kidney injury. Clin Kidney J 2021; 14: 309–316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. ERA-EDTA Council, ERACODA Working Group. Chronic kidney disease is a key risk factor for severe COVID-19: a call to action by the ERA-EDTA. Nephrol Dial Transplant 2021; 36: 87–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Williamson EJ, Walker AJ, Bhaskaran K. et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020; 584: 430–436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Clark A, Jit M, Warren-Gash C. et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health 2020; 8: e1003–e1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sanchez-Niño MD, Sanz AB, Ramos AM. et al. Clinical proteomics in kidney disease as an exponential technology: heading towards the disruptive phase. Clin Kidney J 2017; 10: 188–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tofte N, Lindhardt M, Adamova K. et al. Early detection of diabetic kidney disease by urinary proteomics and subsequent intervention with spironolactone to delay progression (PRIORITY): a prospective observational study and embedded randomised placebo-controlled trial. Lancet Diabetes Endocrinol 2020; 8: 301–312 [DOI] [PubMed] [Google Scholar]
- 13. Rodríguez-Ortiz ME, Pontillo C, Rodríguez M. et al. Novel urinary biomarkers for improved prediction of progressive eGFR loss in early chronic kidney disease stages and in high risk individuals without chronic kidney disease. Sci Rep 2018; 8: 15940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Foreman KJ, Marquez N, Dolgert A. et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016-40 for 195 countries and territories. Lancet 2018; 392: 2052–2090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.ERA-EDTA Registry. ERA-EDTA Registry Annual Report 2018. Amsterdam: Amsterdam UMC, location AMC, Department of Medical Informatics, 2020. https://www.era-edta.org/registry/AnnRep2018.pdf (1 May 2021, date last accessed)
- 16. Kramer A, Boenink R, Noordzij M. et al. The ERA-EDTA Registry Annual Report 2017: a summary. Clin Kidney J 2020; 13: 693–709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vanholder R, Annemans L, Bello AK. et al. Fighting the unbearable lightness of neglecting kidney health: the decade of the kidney. Clin Kidney J 2021; 14: 1719–1730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Organización Nacional de Trasplantes. Registro Español de Enfermos Renales. http://www.ont.es/infesp/Paginas/RegistroEnfermosRenales.aspx (1 May 2021, date last accessed)
- 19. Torra R, Furlano M, Ortiz A. et al. Genetic kidney diseases as an underrecognized cause of chronic kidney disease: the key role of international registry reports. Clin Kidney J 2021; 14: 1879–1885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Groopman EE, Marasa M, Cameron-Christie S. et al. Diagnostic utility of exome sequencing for kidney disease. N Engl J Med 2019; 380: 142–151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Connaughton DM, Bukhari S, Conlon P. et al. The Irish kidney gene project–prevalence of family history in patients with kidney disease in Ireland. Nephron 2015; 130: 293–301 [DOI] [PubMed] [Google Scholar]
- 22. Mann JFE, Hilgers KF.. Clinical features, diagnosis, and treatment of hypertensive nephrosclerosis. https://www.uptodate.com/contents/clinical-features-diagnosis-and-treatment-of-hypertensive-nephrosclerosis?_escaped_fragment_= (9 July 2020, date last accessed) [Google Scholar]
- 23. Carriazo S, Vanessa Perez-Gomez M, Ortiz A.. Hypertensive nephropathy: a major roadblock hindering the advance of precision nephrology. Clin Kidney J 2020; 13: 504–509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Freedman BI, Sedor JR.. Hypertension-associated kidney disease: perhaps no more. J Am Soc Nephrol 2008; 19: 2047–2051 [DOI] [PubMed] [Google Scholar]
- 25. Friedman DJ. COVID-19 and APOL1: understanding disease mechanisms through clinical observation. J Am Soc Nephrol 2021; 32: 1–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jager KJ, Kovesdy C, Langham R. et al. A single number for advocacy and communication-worldwide more than 850 million individuals have kidney diseases. Kidney Int 2019; 96: 1048–1050 [DOI] [PubMed] [Google Scholar]
- 27. GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020; 395: 709–733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Soriano JB, Rojas-Rueda D, Alonso J. et al. The burden of disease in Spain: results from the Global Burden of Disease 2016. Med Clin (Barc) 2018; 151: 171–190 [DOI] [PubMed] [Google Scholar]
- 29. Ortiz A, Sanchez-Niño MD, Crespo-Barrio M. et al. The Spanish Society of Nephrology (SENEFRO) commentary to the Spain GBD 2016 report: keeping chronic kidney disease out of sight of health authorities will only magnify the problem. Nefrologia 2019; 39: 29–34 [DOI] [PubMed] [Google Scholar]
- 30. Vollset SE, Goren E, Yuan CW. et al. Fertility, mortality, migration, and population scenarios for 195 countries and territories from 2017 to 2100: a forecasting analysis for the Global Burden of Disease Study. Lancet 2020; 396: 1285–1306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.United Nations. Department of Economic and Social Affairs.Population dynamics. https://population.un.org/wpp/Graphs/DemographicProfiles/Pyramid/724 (1 May 2021, date last accessed)
- 32. Gorostidi M, Sánchez-Martínez M, Ruilope LM. et al. Chronic kidney disease in Spain: prevalence and impact of accumulation of cardiovascular risk factors. Nefrologia 2018; 38: 606–615 [DOI] [PubMed] [Google Scholar]
- 33. Martín-Cleary C, Ortiz A.. CKD hotspots around the world: where, why and what the lessons are. A CKJ review series. Clin Kidney J 2014; 7: 519–523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Murray R, Zimmerman T, Agarwal A. et al. Kidney-related research in the United States: a position statement from the National Kidney Foundation and the American Society of Nephrology. Am J Kidney Dis 2021; 78: 161–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. https://www.isciii.es/QueHacemos/Financiacion/Documents/RD21/FAQs_RD_2021.pdf (1 March 2021, date last accessed)
- 36. Sanz AB, Sanchez-Niño MD, Ramos AM. et al. NF-kappaB in renal inflammation. J Am Soc Nephrol 2010; 21: 1254–1262 [DOI] [PubMed] [Google Scholar]
- 37. Fernandez-Fernandez B, Izquierdo MC, Valiño-Rivas L. et al. Albumin downregulates Klotho in tubular cells. Nephrol Dial Transplant 2018; 33: 1712–1722 [DOI] [PubMed] [Google Scholar]
- 38. Hu MC, Shi M, Zhang J. et al. Klotho deficiency causes vascular calcification in chronic kidney disease. J Am Soc Nephrol 2011; 22: 124–136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Moreno JA, Izquierdo MC, Sanchez-Niño MD. et al. The inflammatory cytokines TWEAK and TNFα reduce renal klotho expression through NFκB. J Am Soc Nephrol 2011; 22: 1315–1325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sanchis P, Ho CY, Liu Y. et al. Arterial "inflammaging" drives vascular calcification in children on dialysis. Kidney Int 2019; 95: 958–972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kooman JP, Kotanko P, Schols AM. et al. Chronic kidney disease and premature ageing. Nat Rev Nephrol 2014; 10: 732–742 [DOI] [PubMed] [Google Scholar]
- 42. Wanner C, Tonelli M,. Kidney Disease: Improving Global Outcomes Lipid Guideline Development Work Group Members. KDIGO Clinical Practice Guideline for Lipid Management in CKD: summary of recommendation statements and clinical approach to the patient. Kidney Int 2014; 85: 1303–1309 [DOI] [PubMed] [Google Scholar]
- 43.European Kidney Health Alliance. Resolve the unmet needs of kidney patients in “The Decade of the Kidney”. http://ekha.eu/wp-content/uploads/200910_EKHA_postion_EU_new_farma_strategy.pdf (1 May 2021, date last accessed)
- 44. Fowler KJ. Advancing American Kidney Health (AAKH): catalyst for investment in kidney diseases clinical trials and precision medicine: an opportunity to advance upstream interventions and the importance of nephrology. Clin J Am Soc Nephrol 2020; 15: 1689–1691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Fernandez-Fernandez B, Mahillo I, Sanchez-Rodriguez J. et al. Gender, albuminuria and chronic kidney disease progression in treated diabetic kidney disease. J Clin Med 2020; 9: 161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.European Kidney Health Alliance. The Decade of the Kidney™. http://ekha.eu/the-decade-of-the-kidney/ (1 June 2021, date last accessed)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.