Abstract
Background
We aimed to investigate the prevalence trends and explore the influencing factors of post-stroke depression based on the National Health and Nutrition Examination Survey (NHANES) database, including data from 2005 to 2018.
Material/Methods
A total of 1298 patients with stroke were included in this study. Multivariate logistic regression analysis was performed to select influencing factors. Subgroup analysis was conducted based on different populations. The odds ratio (OR) and 95% confidence interval (CI) were calculated.
Results
The prevalence of post-stroke depression was 16.35% in 2005 and 23.29% in 2018, and presented a linear upward trend by year (F=195.00, P<0.001) from 2005 to 2018. Age (≥60 years vs <60 years; OR=0.40; 95% CI, 0.30–0.54), sex (female vs male; OR=1.37; 95% CI, 1.02–1.84), education level (junior middle school or below vs college or above; OR=0.64; 95% CI, 0.46–0.90), annual household income (≥$20,000 vs <$20,000; OR=0.60; 95% CI, 0.45–0.80), and sleep disorders (sleep disorders vs no sleep disorders; OR=4.07; 95% CI, 3.01–5.49) were associated with the risk of post-stroke depression. The age-based subgroup analysis showed that sex and education level were not influencing factors of post-stroke depression in patients ≥60 years, and education level was not related to the risk of post-stroke depression among men in the sex-based analysis.
Conclusions
Stroke patients with sleep disorders, age <60 years, and female sex may have an increased risk of post-stroke depression.
Keywords: Depression, Nutrition Surveys, Prevalence, Stroke
Background
Stroke, an acute cerebrovascular disease, is a group of cerebral injury diseases caused by the sudden rupture of blood vessels in the brain or the blockage of blood vessels that prevents blood from flowing to the brain [1]. It is a leading cause of death and disability in Chinese adults, with a high risk of morbidity, mortality, and disability [2], which increases the burden on individuals and families. Epidemiological data show there are about 610 000 newly diagnosed strokes and 185 000 recurrent cases annually in United States [3]. Because of the unknown trajectory of strokes and the lack of effective treatments, the recurrence of stroke affects the daily life of the whole family, thereby leading to a situational crisis that causes several mental health disorders, such as anxiety and depression [4,5]. Therefore, paying attention to the mental status of people with a chronic illness is especially important in preventing the progression of the disease.
Depression, a common neuropsychiatric symptom, is a major condition that influences the health of over 3 billion people worldwide [6]. It is estimated that nearly 10% to 25% of women and 7% to 12% of men suffer from depression at least once in their lives [7]. Studies reported that approximately 33.3% of stroke survivors have depression, which is a frequent manifestation that is easily overlooked in the progression of stroke [8,9]. Multiple studies have shown that post-stroke depression is connected with adverse functional outcomes, including disability, sleeping disorders, cognitive impairment, and impaired social interaction [10,11]. Some researchers have suggested that post-stroke depression can increase the death risk of individuals with stroke by influencing their behavior, such as lifestyle habits and the use of preventive medications for stroke recurrence [12–14]. Hence, it is necessary to focus on the occurrence of depression after stroke to improve the functional outcomes among patients with stroke.
To the best of our knowledge, the epidemic trends of depression in individuals with stroke have been rarely reported. In the present study, we investigated the prevalence trends and explored the influencing factors of post-stroke depression based on the National Health and Nutrition Examination Survey (NHANES) database, including data from 2005 to 2018.
Material and Methods
Patients
Data in this study were extracted for years 2005 to 2018 from the NHANES database, which is a cross-sectional survey for health and nutritional status of the US civilian and non-institutionalized population conducted by the National Center of Health Statistics and Centers for Disease Control and Prevention. Participants were randomly screened based on a complex, stratified, and multi-stage cluster sampling design. The information collection was carried out by interviews, and corresponding examinations and assessments were conducted in a mobile examination center. Additional information is available at http://www.cdc.gov/nchs/nhanes.htm. The NHANES database (2005–2018) included 39 748 participants, of which 1591 (4.00%) participants had had a stroke. After excluding patients who did not meet the requirements, a total of 1298 patients with stroke were included in this study. This study did not need to be approved by the Institutional Review Board of Beijing Shijitan Hospital because the data used were accessed from a publicly available database.
Study Variables
The demographic and clinical data of participants were extracted and included age, sex, body mass index (BMI, kg/m2), marital status, ethnicity, education level, annual household income ($), diabetes mellitus, sleeping status, systolic blood pressure (mmHg), diastolic blood pressure (mmHg), total cholesterol (mg/dL), high-density lipoprotein (mg/dL), low-density lipoprotein (mg/dL), blood lead (μg/L), and the Patient Health Questionnaire (PHQ-9).
Definitions
The PHQ-9 was used to measure current depression and the frequency of depression in the past 2 weeks. Each response of the 9 items was assigned a score from 0 to 3 as follows: never, 0; several days, 1; ≥50% of the days, 2; and almost daily, 3. The questions of the PHQ-9 were asked at the mobile examination center by trained interviewers. The definition of depressive symptomology was identified according to the continuous distribution of a parameter. Current depression was confirmed with an aggregate score ≥10 [15]. The question “Has a doctor or other health professional ever told you that you had a stroke” was used to determine a history of stroke.
Statistical Analysis
All statistical analyses were performed using 2-sided tests (SAS software), and a P value <0.05 was considered statistically significant. Continuous variables were tested by the t test or the Mann-Whitney test; variables with normal distribution were described as mean±SD, and continuous variables with a non-normal distribution were described by M (Q1, Q5). Categorical variables were tested by the chi-squared (χ2) test or the Fisher’s test and described as number and percentage. The variables with statistical significance in univariate analysis were incorporated into multivariate logistic regression analysis to explore the influencing factors of post-stroke depression. The odds ratio (OR) and 95% confidence interval (CI) were calculated.
Results
Baseline Characteristics of Patients with Stroke
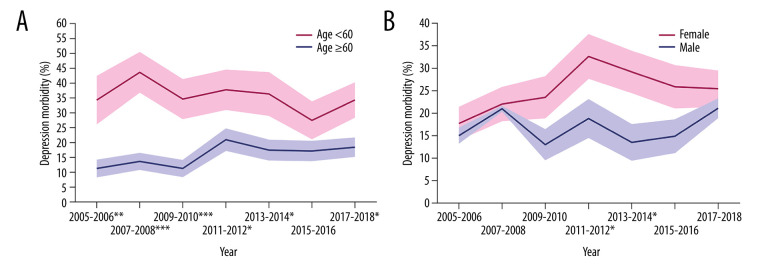
A total of 1298 patients with stroke were included in this study (Figure 1), including 642 (49.46%) men and 656 (50.54%) women. Of these patients, 357 (27.50%) were <60 years, and 941 (72.5%) were ≥60 years. Among them, 612 (47.15%) were married, 166 (12.79%) were unmarried, 272 (20.96%) were widowed, and 248 (19.11%) were divorced or separated. In terms of educational levels, 432 (33.28%) patients had a junior-middle-school level or below, 358 (27.58%) had a high-school level or a GED, and 508 (39.14%) had a college level or above. In addition, 787 (60.63%) patients had an annual household income ≥$20,000, 468 (36.06%) had diabetes, 555 (42.76%) had sleep disorders, and 275 (21.19%) were depressed.
Figure 1.
Selection of study sample.
Comparison on the Characteristics of Depression and Non-Depression Groups
The proportion of age ≥60 years (χ2=61.050, P<0.001) and annual household income ≥$20,000 (χ2=18.262, P<0.001) were lower in the depression group than in the non-depression group. In addition, patients with depression had a lower education level (Z=−1.998, P=0.046). Compared with the non-depression group, BMI (t=−3.360, P<0.001), diastolic blood pressure (t=−4.040, P<0.001), total cholesterol (t=−2.830, P=0.005), blood lead (Z=−3.074, P=0.002), proportion of females (χ2=13.473, P<0.001), and sleep disorders (χ2=112.976, P<0.001) were higher in the depression group. The distribution of marital status between the depression and non-depression groups was also statistically significant (χ2=24.819, P<0.001) (Table 1).
Table 1.
Comparison on the characteristics of the depression and non-depression groups.
| Variables | Total | Non-depression (n=1,023) | Depression (n=275) | Statistic | P |
|---|---|---|---|---|---|
| Age (years), n (%) | χ2=61.050 | <0.001 | |||
| <60 | 357 (27.50) | 230 (22.48) | 127 (46.18) | ||
| ≥60 | 941 (72.50) | 793 (77.52) | 148 (53.82) | ||
| BMI (kg/m2), mean±SD | 29.97±6.75 | 29.60±6.39 | 31.32±7.80 | t=−3.360 | <0.001 |
| Gender, n (%) | χ2=13.473 | <0.001 | |||
| Male | 642 (49.46) | 533 (52.10) | 109 (39.64) | ||
| Female | 656 (50.54) | 490 (47.90) | 166 (60.36) | ||
| Ethnicity, n (%) | χ2=3.250 | 0.517 | |||
| Mexican American | 116 (8.94) | 90 (8.80) | 26 (9.45) | ||
| Hispanic American | 77 (5.93) | 55 (5.38) | 22 (8.00) | ||
| White | 653 (50.31) | 515 (50.34) | 138 (50.18) | ||
| Black | 363 (27.97) | 291 (28.45) | 72 (26.18) | ||
| Other | 89 (6.86) | 72 (7.04) | 17 (6.18) | ||
| Marital status, n (%) | χ2=24.819 | <0.001 | |||
| Married | 612 (47.15) | 509 (49.76) | 103 (37.45) | ||
| Widowed | 272 (20.96) | 220 (21.51) | 52 (18.91) | ||
| Divorced or separated | 248 (19.11) | 182 (17.79) | 66 (24.00) | ||
| Unmarried, n (%) | 166 (12.79) | 112 (10.95) | 54 (19.64) | ||
| Education, n (%) | Z=−1.998 | 0.046 | |||
| Junior middle schools or below | 432 (33.28) | 327 (31.96) | 105 (38.18) | ||
| Senior high schools or GED | 358 (27.58) | 284 (27.76) | 74 (26.91) | ||
| Colleges or above | 508 (39.14) | 412 (40.27) | 96 (34.91) | ||
| Annual household income, n (%) | χ2=18.262 | <0.001 | |||
| <20,000$ | 511 (39.37) | 372 (36.36) | 139 (50.55) | ||
| ≥20,000$ | 787 (60.63) | 651 (63.64) | 136 (49.45) | ||
| Diabetes, n (%) | χ2=0.470 | 0.493 | |||
| No | 830 (63.94) | 659 (64.42) | 171 (62.18) | ||
| Yes | 468 (36.06) | 364 (35.58) | 104 (37.82) | ||
| Sleep disorders, n (%) | χ2=112.976 | <0.001 | |||
| No | 743 (57.24) | 663 (64.81) | 80 (29.09) | ||
| Yes | 555 (42.76) | 360 (35.19) | 195 (70.91) | ||
| SBP (mmHg), mean±SD | 134.33±22.91 | 134.69±23.01 | 133.02±22.53 | t=1.070 | 0.284 |
| DBP (mmHg), mean±SD | 69.53±13.82 | 68.74±13.85 | 72.50±13.30 | t=−4.040 | <0.001 |
| TC (mg/dL), mean±SD | 184.31±46.89 | 182.30±45.75 | 191.78±50.29 | t=−2.830 | 0.005 |
| HDL (mg/dL), mean±SD | 51.50±16.60 | 51.72±16.53 | 50.66±16.85 | t=0.940 | 0.347 |
| LDL (mg/dL), M (Q1, Q3) | 102.00 (77.00,132.00) | 101.00 (78.00,129.00) | 105.00 (76.00,138.00) | Z=1.573 | 0.116 |
| Lead (μg/L), M (Q1, Q3) | 1.63 (1.10, 2.61) | 1.70 (1.14, 2.71) | 1.44 (1.01, 2.39) | Z=−3.074 | 0.002 |
Prevalence Trends of Post-Stroke Depression from 2005 to 2018
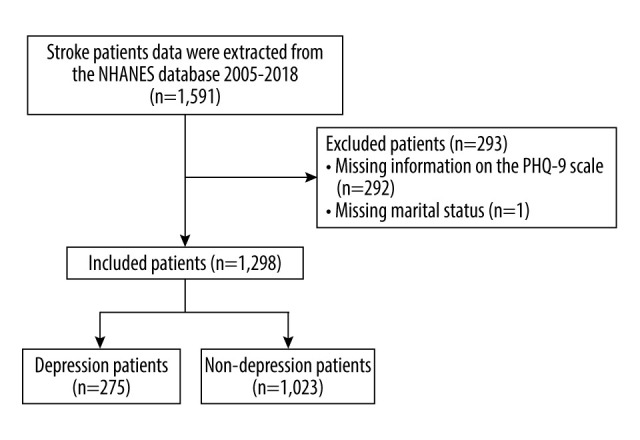
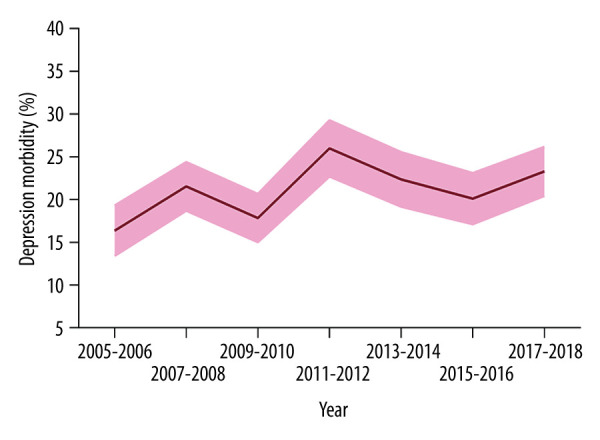
The prevalence of post-stroke depression was 16.35% in 2005 and 23.29% in 2018. The prevalence of depression in patients with stroke from 2005 to 2018 showed a linear upward trend by year (F=195.00, P<0.001) (Figure 2). In different populations, the prevalence of post-stroke depression in patients <60 years was always higher than that in patients ≥60 years, and the prevalence of post-stroke depression in women was always higher than that in men (Figure 3). However, there was no significant difference of post-stroke depression prevalence by age subgroups (≥60 years vs <60 years, P>0.05) and sex subgroups (women vs men, P>0.05).
Figure 2.
The prevalence trends of post-stroke depression based on National Health and Nutrition Examination Survey database from 2005 to 2018.
Figure 3.
The prevalence trends of post-stroke depression based on age and sex. (A) Trends of prevalence in patients ≥60 years and <60 years; (B) trends of prevalence in men and women. * P<0.05, ** P<0.01, *** P<0.001, indicates that the chi-square test is statistically significant between the two groups.
Influencing Factors of Post-Stroke Depression
The multivariate logistic regression analysis showed that age, sex, education level, annual household income, and sleep disorders were the influencing factors of post-stroke depression. The risk of depression for patients ≥60 years was 0.40 times that of patients <60 years (OR=0.40; 95% CI, 0.30–0.54). The risk of depression in women was 1.37 times that in men (OR=1.37; 95% CI, 1.02–1.84). Compared with the risk of depression in the education level junior-middle-school or below group, the risk of depression in the senior-high-school or GED group (OR=0.74; 95% CI, 0.51–1.07) and college or above group (OR=0.64; 95% CI, 0.46–0.90) were lower. The risk of depression for patients with an annual household income ≥$20,000 was 0.60 times higher than that of patients with an annual household income <$20,000 (OR=0.60; 95% CI, 0.45–0.80). Furthermore, patients with sleep disorders were at a higher risk of depression (OR=4.07; 95% CI, 3.01–5.49) (Figure 4).
Figure 4.
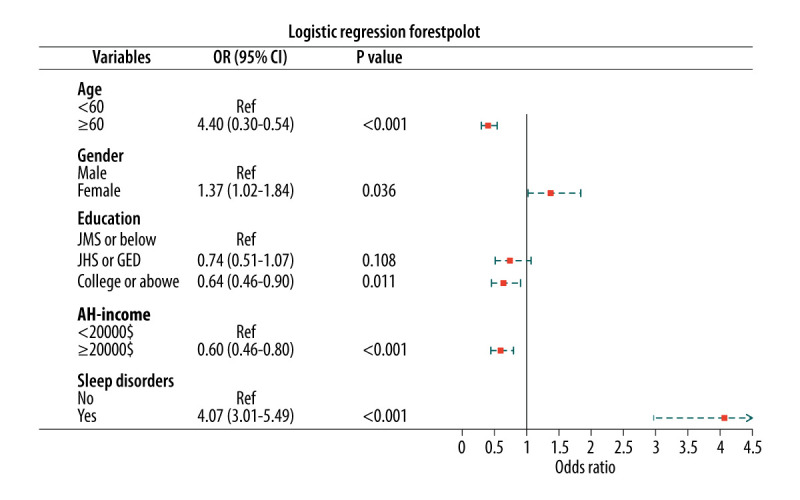
The influencing factors of post-stroke depression.
Influencing Factors of Post-Stroke Depression in Different Ages and Sexes
The influencing factors of post-stroke depression in patients <60 years had statistically significant differences in sex, education level, annual household income, and sleep disorders (P<0.05). In patients ≥60 years, the influencing factors of post-stroke depression were annual household income and sleep disorders (P<0.05), while sex and education level were not influencing factors (P>0.05) (Table 2). In men, the influencing factors of post-stroke depression were age, annual household income, and sleep disorders (P<0.05), but not education level (P>0.05). Furthermore, the influencing factors of post-stroke depression in women were age, education level, annual household income, and sleep disorders (P<0.05) (Table 3).
Table 2.
Analysis of influencing factors of post-stroke depression based on age.
| Characteristics | Age <60 | Age ≥60 | ||||
|---|---|---|---|---|---|---|
| β | OR (95% CI) | P | β | OR (95% CI) | P | |
| Gender | ||||||
| Male | Ref | Ref | ||||
| Female | 0.562 | 1.76 (1.06–2.92) | 0.030 | 0.207 | 1.23 (0.85–1.77) | 0.269 |
| Education | ||||||
| JMS or below | Ref | Ref | ||||
| JHS or GED | −0.492 | 0.61 (0.33–1.15) | 0.127 | −0.247 | 0.78 (0.49–1.24) | 0.290 |
| College or above | −0.662 | 0.52 (0.29–0.93) | 0.028 | −0.354 | 0.70 (0.46–1.08) | 0.107 |
| Annual household income | ||||||
| <20,000$ | Ref | Ref | ||||
| ≥20,000$ | −0.642 | 0.53 (0.32–0.86) | 0.010 | −0.472 | 0.62 (0.43–0.90) | 0.012 |
| Sleep disorders | ||||||
| No | Ref | Ref | ||||
| Yes | 1.839 | 6.29 (3.69–10.71) | <0.001 | 1.185 | 3.27 (2.26–4.73) | <0.001 |
JMS – junior middle schools; JHS – senior high schools; OR – odd ratio
Table 3.
Analysis of influencing factors of post-stroke depression based on sex.
| Characteristics | Male | Female | ||||
|---|---|---|---|---|---|---|
| β | OR (95% CI) | P | β | OR (95% CI) | P | |
| Gender | ||||||
| Male | Ref | Ref | ||||
| Female | −0.687 | 0.50 (0.31–0.81) | 0.004 | −1.062 | 0.35 (0.24–0.51) | <0.001 |
| Education | ||||||
| JMS or below | Ref | Ref | ||||
| JHS or GED | −0.173 | 0.84 (0.49–1.45) | 0.535 | −0.419 | 0.66 (0.40–1.08) | 0.099 |
| College or above | −0.432 | 0.65 (0.38–1.12) | 0.118 | −0.473 | 0.62 (0.40–0.98) | 0.040 |
| Annual household income | ||||||
| <20,000$ | Ref | Ref | ||||
| ≥20,000$ | −0.577 | 0.56 (0.36–0.89) | 0.013 | −0.492 | 0.61 (0.42–0.89) | 0.011 |
| Sleep disorders | ||||||
| No | Ref | Ref | ||||
| Yes | 1.636 | 5.13 (3.24–8.13) | <0.001 | 1.229 | 3.42 (2.30–5.08) | <0.001 |
JMS – junior middle schools; JHS – senior high schools; OR – odd ratio
Discussion
In this study, we analyzed the epidemic trends of post-stroke depression and explored the influencing factors of depression in patients with stroke, based on the NHANES database. The results showed that the prevalence of post-stroke depression in 2011 to 2018 was higher than that in 2005 to 2010. Age ≥60 years, higher education level, and higher annual household income were related to a reduced risk of post-stroke depression, while female sex and sleep disorders were associated with an increased risk of post-stroke depression.
Approximately one-third of stroke survivors have post-stroke depression [16]. Previous studies have shown that post-stroke depression is the most important and common complication of stroke [16,17]. The etiology of post-stroke depression is multi-factorial, comprising biological and psycho-social factors. It has been reported that biological factors are the main factors associated with post-stroke depression [18], including age, sex, inflammation, response to ischemia, genetic susceptibility, alterations of neurogenesis in neurotrophic factors lesion location, neurogenesis, and activation of the hypothalamic-pituitary-adrenal axis [19]. The psycho-social factors include post-stroke cognitive and functional deficits, past psychiatric history, pre-morbid neurotic personality traits, and social isolation [20]. Our results showed that from 2005 to 2018, the prevalence of depression in patients with stroke had an upward trend by year. In different populations, patients with stroke who are <60 years old and female sex accounted for a higher proportion of post-stroke depression. A possible explanation is that patients under 60 years old are the mainstay of the family, and they are more likely to experience depression due to economic, family, and health-related pressures after stroke [21]. The high proportion of post-stroke depression among women may be due to poor psychological endurance, which may affect their endocrine and neurotransmitter production from stressful events [22,23]. In addition, the composition of the population can also contribute to an increase in post-stroke depression. Dong et al indicated that the prevalence of post-stroke depression in Mexican Americans was 1.69 times that of non-Hispanic whites [24].
A multivariate logistic regression analysis was used to explore influencing factors of post-stroke depression in this study. The results showed that the influencing factors of post-stroke depression were age, sex, education level, annual household income, and sleep disorders. Age and sex are the most frequently studied risk factors in post-stroke depression and exhibit the most controversial results [25]. A meta-analysis showed that age (<70 years) was one of the most significant risk factors in post-stroke depression [9]. The proportion of patients <65 years of age has increased significantly, especially in low- and middle-income countries [26], which can pose a huge challenge of post-stroke depression. Female sex has also been shown to be a risk factor for post-stroke depression [9,27]. Our results revealed that the risk of post-stroke depression in women was 1.37 times that in men. Furthermore, patients with a higher education level and higher annual household income had a lower risk of post-stroke depression. A cohort prospective study indicated that education level was a protective factor for post-stroke depression [28]. Jiang et al showed that lower income was one of the risk factors for depression in patients with acute stroke [29]. Sleep disorders cause neuroendocrine and circadian rhythm abnormalities that increase the risk for depression [30]. Dong et al indicated that sleep disorders are associated with a significantly increased risk of post-stroke depression [31]. In addition, we conducted a further analysis based on age and sex to explore the influencing factors of post-stroke depression in different populations. The results showed that sex and education level were not the influencing factors of post-stroke depression in patients ≥60 years, and education level was not an influencing factor of post-stroke depression in men.
The strength of our study was the analysis of prevalence trends of post-stroke depression based on the NHANES database from 2005 to 2018. The influencing factors of post-stroke depression were also explored, and further analysis was performed to assess the influencing factors of post-stroke depression in different populations. However, this study has some limitations. First, some biological factors (such as cytokines) can play an important role in the occurrence of post-stroke depression, but they were not analyzed owing to a data deficiency in the NHANES database. Second, this study mainly analyzed the biological factors of post-stroke depression, but the psycho-social factors were not assessed owing to the limitations of the NHANES database. For example, the social support data included only years 2003 to 2008, the physical activity data included only years 1999 to 2006, and no past psychiatric history data was found. Further studies should pay more attention to the psycho-social factors for post-stroke depression. Third, the PHQ-9 was used to classify current depression and may have underestimated clinical depression. However, a PHQ-9 score ≥10 had a sensitivity of 88% and a specificity of 88% in identifying depression, indicating that there may be relatively few misclassifications of depression [32].
Conclusions
From 2005 to 2018, the prevalence of depression in patients with stroke was on an upward trend by year. Age <60 years and female sex accounted for a higher proportion of patients with post-stroke depression. Sleep disorders and female sex were related to an increased risk of post-stroke depression. Age ≥60 years, higher education level, and higher annual household income were associated with a reduced risk of post-stroke depression. Clinicians should intervene early in patients with factors that may increase the risk of post-stroke depression. Future studies should explore the influence of psycho-social factors on post-stroke depression.
Footnotes
Conflict of interest: None declared
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors, who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Financial support: None declared
References
- 1.Campbell BCV, Khatri P. Stroke. Lancet. 2020;396:129–42. doi: 10.1016/S0140-6736(20)31179-X. [DOI] [PubMed] [Google Scholar]
- 2.Wang W, Jiang B, Sun H, et al. Prevalence, incidence, and mortality of stroke in China: Results from a nationwide population-based survey of 480–687 adults. Circulation. 2017;135:759–71. doi: 10.1161/CIRCULATIONAHA.116.025250. [DOI] [PubMed] [Google Scholar]
- 3.Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: A report from the American Heart Association. Circulation. 2017;135:e146–603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raju RS, Sarma PS, Pandian JD. Psychosocial problems, quality of life, and functional independence among Indian stroke survivors. Stroke. 2010;41:2932–37. doi: 10.1161/STROKEAHA.110.596817. [DOI] [PubMed] [Google Scholar]
- 5.Kapoor A, Si K, Yu AYX, et al. Younger age and depressive symptoms predict high risk of generalized anxiety after stroke and transient ischemic attack. Stroke. 2019;50:2359–63. doi: 10.1161/STROKEAHA.119.025464. [DOI] [PubMed] [Google Scholar]
- 6.Herrman H, Kieling C, McGorry P, et al. Reducing the global burden of depression: A Lancet-World Psychiatric Association Commission. Lancet. 2019;393:e42–43. doi: 10.1016/S0140-6736(18)32408-5. [DOI] [PubMed] [Google Scholar]
- 7.Driscoll KA, Johnson SB, Barker D, et al. Risk factors associated with depressive symptoms in caregivers of children with type 1 diabetes or cystic fibrosis. J Pediatr Psychol. 2010;35:814–22. doi: 10.1093/jpepsy/jsp138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dong JY, Zhang YH, Tong J, Qin LQ. Depression and risk of stroke: A meta-analysis of prospective studies. Stroke. 2012;43:32–37. doi: 10.1161/STROKEAHA.111.630871. [DOI] [PubMed] [Google Scholar]
- 9.Shi Y, Yang D, Zeng Y, Wu W. Risk factors for post-stroke depression: A meta-analysis. Front Aging Neurosci. 2017;9:218. doi: 10.3389/fnagi.2017.00218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pohjasvaara T, Vataja R, Leppävuori A, et al. Depression is an independent predictor of poor long-term functional outcome post-stroke. Eur J Neurol. 2001;8:315–19. doi: 10.1046/j.1468-1331.2001.00182.x. [DOI] [PubMed] [Google Scholar]
- 11.Goodwin RD, Devanand DP. Stroke, depression, and functional health outcomes among adults in the community. J Geriatr Psychiatry Neurol. 2008;21:41–46. doi: 10.1177/0891988707311041. [DOI] [PubMed] [Google Scholar]
- 12.Ayerbe L, Ayis S, Crichton S, et al. The long-term outcomes of depression up to 10 years after stroke: The South London Stroke Register. J Neurol Neurosurg Psychiatry. 2014;85:514–21. doi: 10.1136/jnnp-2013-306448. [DOI] [PubMed] [Google Scholar]
- 13.Jorge RE, Robinson RG, Arndt S, Starkstein S. Mortality and poststroke depression: A placebo-controlled trial of antidepressants. Am J Psychiatry. 2003;160:1823–29. doi: 10.1176/appi.ajp.160.10.1823. [DOI] [PubMed] [Google Scholar]
- 14.Bartoli F, Di Brita C, Crocamo C, et al. Early post-stroke depression and mortality: meta-analysis and meta-regression. Front Psychiatry. 2018;9:530. doi: 10.3389/fpsyt.2018.00530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jorgensen D, White GE, Sekikawa A, Gianaros P. Higher dietary inflammation is associated with increased odds of depression independent of Framingham Risk Score in the National Health and Nutrition Examination Survey. Nutr Res. 2018;54:23–32. doi: 10.1016/j.nutres.2018.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ayerbe L, Ayis S, Wolfe CD, Rudd AG. Natural history, predictors and outcomes of depression after stroke: Systematic review and meta-analysis. Br J Psychiatry. 2013;202:14–21. doi: 10.1192/bjp.bp.111.107664. [DOI] [PubMed] [Google Scholar]
- 17.Hackett ML, Anderson CS. Predictors of depression after stroke: A systematic review of observational studies. Stroke. 2005;36:2296–301. doi: 10.1161/01.STR.0000183622.75135.a4. [DOI] [PubMed] [Google Scholar]
- 18.Villa RF, Ferrari F, Moretti A. Post-stroke depression: Mechanisms and pharmacological treatment. Pharmacol Ther. 2018;184:131–44. doi: 10.1016/j.pharmthera.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 19.Loubinoux I, Kronenberg G, Endres M, Schumann-Bard P, et al. Post-stroke depression: Mechanisms, translation and therapy. J Cell Mol Med. 2012;16:1961–69. doi: 10.1111/j.1582-4934.2012.01555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whyte EM, Mulsant BH. Post stroke depression: Epidemiology, pathophysiology, and biological treatment. Biol Psychiatry. 2002;52:253–64. doi: 10.1016/s0006-3223(02)01424-5. [DOI] [PubMed] [Google Scholar]
- 21.McCarthy MJ, Sucharew HJ, Alwell K, et al. Age, subjective stress, and depression after ischemic stroke. J Behav Med. 2016;39:55–64. doi: 10.1007/s10865-015-9663-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Poynter B, Shuman M, Diaz-Granados N, et al. Sex differences in the prevalence of post-stroke depression: A systematic review. Psychosomatics. 2009;50:563–69. doi: 10.1176/appi.psy.50.6.563. [DOI] [PubMed] [Google Scholar]
- 23.Robinson RG, Jorge RE. Post-stroke depression: A review. Am J Psychiatry. 2016;173:221–31. doi: 10.1176/appi.ajp.2015.15030363. [DOI] [PubMed] [Google Scholar]
- 24.Dong L, Sánchez BN, Skolarus LE, et al. Ethnic differences in prevalence of post-stroke depression. Circ Cardiovasc Qual Outcomes. 2018;11:e004222. doi: 10.1161/CIRCOUTCOMES.117.004222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Das J, Rajanigant GK. Post stroke depression: The sequelae of cerebral stroke. Neurosci Biobehav Rev. 2018;90:104–14. doi: 10.1016/j.neubiorev.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 26.Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990–2010: Findings from the Global Burden of Disease Study 2010. Lancet. 2014;383:245–54. doi: 10.1016/s0140-6736(13)61953-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.De Ryck A, Brouns R, Geurden M, et al. Risk factors for poststroke depression: Identification of inconsistencies based on a systematic review. J Geriatr Psychiatry Neurol. 2014;27:147–58. doi: 10.1177/0891988714527514. [DOI] [PubMed] [Google Scholar]
- 28.Wang Z, Zhu M, Su Z, et al. Post-stroke depression: Different characteristics based on follow-up stage and gender – a cohort perspective study from Mainland China. Neurol Res. 2017;39:996–1005. doi: 10.1080/01616412.2017.1364514. [DOI] [PubMed] [Google Scholar]
- 29.Jiang XG, Lin Y, Li YS. Correlative study on risk factors of depression among acute stroke patients. Eur Rev Med Pharmacol Sci. 2014;18:1315–23. [PubMed] [Google Scholar]
- 30.Tsuno N, Besset A, Ritchie K. Sleep and depression. J Clin Psychiatry. 2005;66:1254–69. doi: 10.4088/jcp.v66n1008. [DOI] [PubMed] [Google Scholar]
- 31.Dong L, Brown DL, Chervin RD, et al. Pre-stroke sleep duration and post-stroke depression. Sleep Med. 2021;77:325–29. doi: 10.1016/j.sleep.2020.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]