Abstract
Background:
Exacerbation of asthma symptoms increases the likelihood of emergency department (ED) visits and hospitalizations. Because the ED is an important healthcare resource for immediate asthma care with acute exacerbations, we identify those populations most likely to seek ED treatment for asthma and describe the asthma burden for post-ED visit hospitalizations and critical care units.
Methods:
We examined the characteristics of asthma-related ED visits and hospital admissions and assessed the association between them using multivariable logistic regression models by analyzing data from the National Hospital Ambulatory Medical Care Survey (NHAMCS) during 2010–2015.
Results:
Of all ED visits, 1.32% were asthma-related; of all ED visits that resulted in hospitalization, 1.12% were asthma-related and, of all ED visits that resulted in admission to a critical care unit, 1.20% were asthma related. The percentages of asthma-related ED visits and post-ED hospitalizations (H) were greater among children (adjusted prevalence ratio: ED: 2.28 [1.96.29–2.65]; H: 8.75 [5.93–12.92]) than among adults and greater for blacks (ED: (2.26 [1.97–2.60]; H: 3.25 [2.07–5.12]) and Hispanics (ED: (1.74 [1.47–2.08]; H: 2.424 [1.46–4.00]) than for whites. The percentage of ED visits was also greater for those covered by Medicaid or the Children’s Health Insurance Program (CHIP) than by private insurance.
Conclusions:
Both asthma-related ED visits and post-ED hospitalizations were greater for children, blacks, and Hispics. ED visits were also greater for Medicaid/CHIP. These findings might help prompt future studies on identifying additional potential risk factors for frequent ED visits among disproportionally affected subpopulations.
Keywords: Healthcare use, demographics, hospitalization, critical care unit, source of payment
Introduction
In 2016, asthma affected approximately 20 million adults and 6 million children in the United States (1). Approximately half of children (54%) and adults (45%) with current asthma had at least one asthma attack in the past 12 months (1). Exacerbation of asthma symptoms increases the risk for emergency department (ED) visits and hospitalizations, especially among children (2,3). The ED is an important healthcare resource for immediate asthma care for people with acute exacerbations, especially for those who might not have a primary care physician or usual place for primary care (4). Children with asthma use healthcare resources significantly more than do children without asthma. Greater healthcare resource use (e.g.ED visits, hospitalizations, stays in critical care facilities) is associated with higher treatment costs (5,6).
During 2015, ED visits for all causes in the United States totaled 137 million (7). Of those, about 0.1% (195,000) died in the ED and 9% (12 million) resulted in hospital admissions. Of those hospitalized, 1.1% (1.5 million) were admitted to a critical care unit (7). Considering ED visits for all causes, adults aged ≥65 years were more likely to be hospitalized after an ED visit than were younger adults. Of all-cause ED visits, 1.7 million ED visits were asthma-related (7). During 2014–2015, 9.5% of all-cause ED visits in the U.S. were made by patients with documentation in the medical record of a diagnosis of asthma, regardless of the diagnosis for the current visit (8). The percent-age was highest for children aged 5–17 years (13.6%), compared with 6.6% for children aged 0–4 years, 9.9% for adults aged 18–64 years, and 6.5% for those aged ≥65 years. Among those aged 0–4 years, boys were more likely than girls to have an ED visit with asthma diagnosis in their medical record (8). Conversely, women were more likely than men to have an ED visit with asthma diagnosis among adults (ages ≥18 years).
Considering the higher cost of ED visits and hospitalizations (5,6), identifying characteristics of patients who were frequent healthcare resource users for asthma exacerbations could lead to targeted interventions that could reduce the economic burden to patients and the healthcare system. We examined characteristics of asthma-related ED visits, asthma-related post-ED hospital, and critical care unit admissions by analyzing 6 years of nationally representative ED data from the National Hospital Ambulatory Medical Care Survey (NHAMCS). Thereby, the study adds contributions to the existing body of knowledge about asthma-related healthcare use.
Our objective for this study was to identify characteristics of those populations most likely to seek ED treatment for asthma and to describe the asthma burden for post-ED visit-related hospitalizations and critical care units. Although the percentages of ED visits and hospitalization after an ED visit for all causes were greater for older adults (7), we hypothesized that the percentages of asthma-related ED visits and hospitalization would be higher for children given that asthma prevalence is higher among children (aged 0–7 years) (1,2,9) and that they are more vulnerable to environmental allergens and irritants (e.g.mold, pollens, house dust mites, cockroaches, rodents, animal allergens, environmental tobacco smoking [ETS], and other ambient air pollutants such as particulate matters (PM 2.5, ozone, sulfur dioxide, and nitrogen oxides) (10–12) that exacerbate asthma symptoms, and thereby increasing the likelihood of emergency department (ED) visits and hospitalizations.
Methods
Survey data description
Our analyses included 2010–2015 data from the ED public use data file of the National Hospital Ambulatory Medical Care Survey (NHAMCS). NHAMCS is a national probability sample survey of visits to hospital outpatient departments, EDs, and hospital-based ambulatory surgery centers, conducted by the National Center for Health Statistics (13). We included all ED visits, even if the same person had more than one visit (unit of analysis is the visit). Detailed information on the survey design and analytic methods is provided in the NHAMCS public use data file documentation for each year (14). ED data from 2010 to 2015 were combined to achieve a sufficient sample size for reliable estimates on the use and provision of ambulatory care services in hospital EDs. Asthma-related visits were selected based on an ICD-9-CM code of 493.0. The 2016 NHAMCS data were not included in the analysis because coding changed from ICD-9-CM in 2015 to ICD-10-CM in 2016. The hospital sampling response rate was around 70% in 2015, but the rate varied each year (14).
The ED survey form asks the provider to list up to 5 causes of an ED visit in sequence (from primary cause to 5th cause). For this study, an ED visit was defined as asthma-related if the primary diagnosis for the visit was asthma (ICD-9-CM code 493.0). We analyzed asthma-related emergency department (ED) visits and post-ED visit hospital and critical care admissions. We examined the distribution of ED visits and post-ED visit hospital admissions by selected patient characteristics. However, because of few (n = 29) asthma-related ED visits that resulted in a critical care admission, we were unable to do sub-group analysis focusing on critical care admissions.
Those characteristics included sex (male, female), children (ages 0–17 years) vs. adults (ages ≥18 years), age group (0–4, 5–17, 18–34, 35–64, and ≥65 years), and race/ethnicity (non-Hispanic white, non-Hispanic black, non-Hispanic other, and Hispanic or Latino). We also considered hospital location by U.S. Census region (Northeast, Midwest, South, and West) and the primary expected source of payment (private insurance, Medicare, Medicaid, Children’s Health Insurance Program [CHIP], or other [workers’ compensation, no charge, charity, self-pay, or other]). Missing values for age, sex, and race/ethnicity variables were imputed and imputed variables were included in the dataset. We used the imputed age, sex, and race/ethnicity variables for the analyses (14).
Statistical methods
All statistical procedures were conducted using SAS software version 9.4 and SAS-Callable SUDAAN version 11.0.1 to account for complex sampling design (14). Patient visit weights were used to produce unbiased national annual estimates from sample data. We examined the distribution of ED visits and ED visits resulting in hospitalization with asthma as primary diagnosis by the selected characteristics (sex, age, race/ethnicity, U.S. Census regions for hospital locations, and primary expected source of payment). We used chi-square tests to determine statistically significance differences in ED visit distribution between subgroups. Multi-variable logistic regression models were used to examine the association between the dichotomous outcome variable(s) (i.e.asthma-related ED visits and hospitalizations after an ED visit) and covariates (age, sex, race/ethnicity, U.S. Census region for hospital location, and expected source of payment). Considering that this is a secondary data analysis of a cross-sectional dataset with complex survey design, usual variable selection techniques (e.g.step-wise, forward, or backward selection) cannot be applied to select covariates for the statistical models used in this study. Authors used prior knowledge drawn from previous publications to identify variables that were associated with healthcare use (1–3,8,9). We created two age variables including five-age group (0–4, 5–17, 18–34, 35–64, and 65 years and over) and two-age group (children vs. adults) variables. For each outcome variable, we used two separate models including only one of the two age variables as a covariate with all other covariates to calculate adjusted prevalence ratios and 95% confidence intervals.
NHAMCS collected data on ED and outpatient department visits by sampling hospitals (e.g. hospital outpatient departments, EDs, and hospital-based ambulatory surgery centers). Therefore, sampling survey design variables (strata and primary sampling unit) were based on both ED and outpatient department (OPD) components of NHAMCS. NHAMCS recommends that if only ED data, without the accompanying OPD data are analyzed, testing for significant differences should be at the alpha = 0.01 level, rather than the more commonly used alpha = 0.05, to decrease the possibility of a Type I error. For this study, we only analyzed ED data because OPD public-use data were not available for the years studied. An estimate was considered unreliable if it had a relative standard error (RSE) >30% or was based on fewer than 30 records, regardless of the magnitude of the RSE (14).
Results
During 2010–2015, about 134,287,679 (SE = 3,498,708) ED visits for all causes in the United States were reported in NHAMCS. About 10.38% of ED visits for all causes resulted in hospital admission and 13.01% of ED visits resulting in hospital admissions were admitted to critical care units. About 1.20% of all ED visits that resulted in an admission to a critical care unit were asthma-related (primary diagnosis for the admission was asthma (ICD-9-CM code of 493.0) (Figure 1, Table 1).
Figure 1.
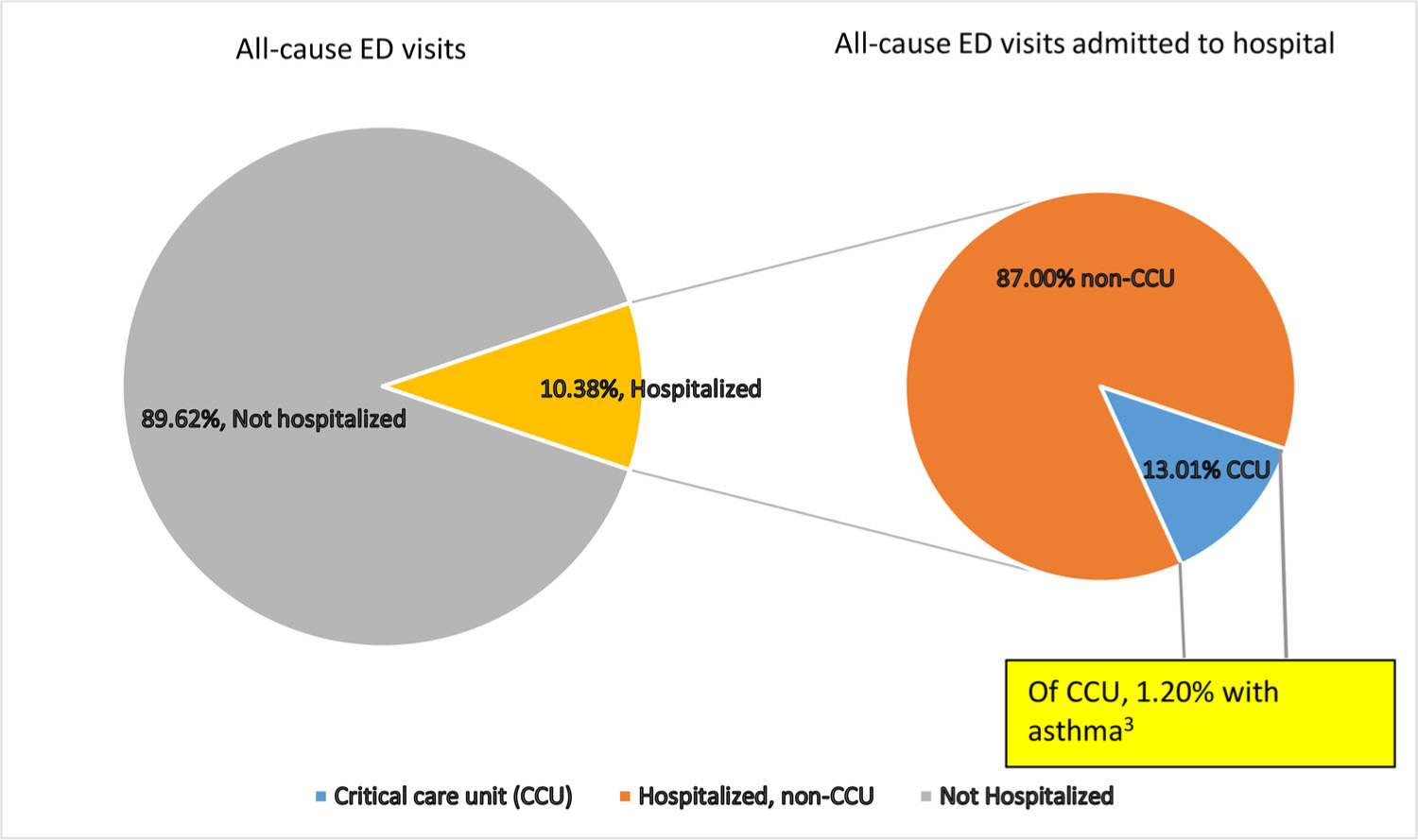
Percentagea of emergency department (ED) visitsb for asthmac admitted to a critical care unit (CCU)—National Hospital Ambulatory Medical Care Survey, United States, 2010–2015.
aPercentage of emergency department (ED) visits with asthma as the primary diagnosis that were admitted to a critical care unit (CCU).
bBased on a sample of visits to EDs in noninstitutional general and short-stay hospitals, exclusive of federal, military, and Veterans administration hospitals, located in the 50 states and the District of Columbia.
cDefined as ED visits with a diagnosis of asthma (ICD-9-CM 493.0) as the primary diagnosis for the current visit.
Table 1.
Percentage of emergency department (ED) visits with asthma as primary diagnosis by healthcare facility—National Hospital Ambulatory Medical Care Survey, United States, 2010–2015.
| All-cause emergency department (ED) visits |
Asthma-related ED visitsa |
||||||
|---|---|---|---|---|---|---|---|
| Number of visits | Weighted number of visits | SE of weighted number | Number of visits | Weighted number of visits | SE of weighted number | Percent (95% CI) | |
| Total | 165,155 | 134,287,679 | 3,498,708 | 2,271 | 1,770,769 | 80,155 | 1.32 (1.22–1.42) |
| Admitted to this hospital after an ED visit | 18,150 | 13,934,424 | 487,859 | 203 | 155,891 | 15,797 | 1.12 (0.92–1.36) |
| Admitted to a critical care unit | 2,238 | 1,812,453 | 92,278 | 29 | 21,783 | 4,941 | 1.20 (0.77–1.86) |
Abbreviations: ED, emergency department; SE, standard error; CI, confidence interval.
Primary diagnosis for ED visit was asthma (ICD-9-CM code of 493.0).
Asthma-related ED visits among all-cause ED visits
Overall, 1.32% (n = 1,770,769) of all ED visits were asthma-related. Among all ED visits, the percentage of asthma-related visits was similar for males (1.41%) and females (1.24%) but differed by age, race/ethnicity, geographic location of the hospital, and source of payment (Table 2).
Table 2.
Asthma-relateda emergency department (ED) visits among all-cause ED visits by selected characteristics—National Hospital Ambulatory Medical Care Survey, United States, 2010–2015.
| All-cause ED visits |
Asthma-related ED visits |
||||||
|---|---|---|---|---|---|---|---|
| Characteristics | Number of visits | Weighted number (SE) | Number of visits | Weighted number (SE) | Percent (95% CI) | p-valueb,c | PR (95% CI) |
| Total | 165,155 | 134,287,679 (3,498,708) | 2,271 | 1,770,769 (80,155) | 1.32 (1.22–1.42) | ||
| Sex | 0.044b | ||||||
| Male | 74,597 | 60,078,909 (1,573,624) | 1,067 | 848,319 (52,605) | 1.41 (1.27–1.57) | Referent | |
| Female | 90,558 | 74,208,769 (1,966,669) | 1,204 | 922,449 (43,292) | 1.24 (1.14–1.35) | 0.90 (0.80–1.02) | |
| Age group (years) | <0.001 b | ||||||
| Children (0–17) | 36,469 | 29,876,705 (1,112,132) | 964 | 786,212 (57,873) | 2.63 (2.37–2.93) | 2.28 (1.96–2.65) | |
| Adults (18 and over) | 128,686 | 104,410,973 (2,765,896) | 1,307 | 984,556 (46,678) | 0.94 (0.87–1.02) | Referent | |
| Age group (years) | 165,155 | <0.001 b,c | |||||
| 0–4 | 16,031 | 13,335,725 (582,455) | 338 | 266,879 (29,634) | 2.00 (1.66–2.40) | 1.71 (1.36–2.16) | |
| 5–17 | 20,438 | 16,540,981 (579,475) | 626 | 519,333 (42,462) | 3.14 (2.76–3.57) | 2.88 (2.40–3.45) | |
| 18–34 | 43,569 | 35,829,093 (1,054,497) | 490 | 368,491 (26,845) | 1.03 (0.90–1.17) | Referent | |
| 35–64 | 59,676 | 47,829,630 (1,282,992) | 693 | 534,114 (31,078) | 1.12 (1.00–1.24) | 1.12 (0.95–1.32) | |
| 65 and over | 25,441 | 20,752,251 (575,956) | 124 | 81,952 (10,582) | 0.39 (0.31–0.51) | 0.50 (0.34–0.74) | |
| Race and ethnicity | 165,155 | <0.001 b,c | |||||
| Non-Hispanic white | 96,636 | 79,509,137 (2,217,107) | 850 | 674,593 (37,146) | 0.85 (0.77–0.94) | Referent | |
| Non-Hispanic black | 36,501 | 30,021,697 (1,386,297) | 866 | 652,671 (45,637) | 2.17 (1.96–2.42) | 2.26 (1.97–2.60) | |
| Non-Hispanic other | 5,929 | 3,938,685 (243,748) | 79 | 55,767 (8,774) | 1.42 (1.06–1.90) | 1.54 (1.09–2.17) | |
| Hispanic | 26,089 | 20,818,160 (961,951) | 476 | 387,738 (37,742) | 1.86 (1.60–2.17) | 1.74 (1.47–2.08) | |
| U.S. Census regiond | <0.001 b,c | ||||||
| Northeast | 35,187 | 23,476,254 (1,234,567) | 631 | 432,429 (37,815) | 1.84 (1.58–2.14) | 1.60 (1.30–1.97) | |
| Midwest | 39,601 | 31,181,053 (1,889,944) | 546 | 397,954 (39,624) | 1.28 (1.08–1.51) | 1.04 (0.83–1.31) | |
| South | 57,163 | 51,721,461 (2,126,536) | 704 | 632,957 (48,849) | 1.22 (1.09–1.38) | 0.97 (0.79–1.19) | |
| West | 33,204 | 27,908,911 (1,620,627) | 390 | 307,429 (32,230) | 1.10 (0.93–1.31) | Referent | |
| Expected source of payment | <0.001 b,c | ||||||
| Private insurance | 46,954 | 38,357,531 (1,241,363) | 593 | 464,381 (31,812) | 1.21 (1.07–1.38) | Referent | |
| Medicare | 29,943 | 24,432,959 (691,397) | 197 | 145,328 (17,331) | 0.59 (0.47–0.75) | 0.95 (0.66–1.36) | |
| Medicaid/CHIP | 47,968 | 37,978,873 (1,252,502) | 1,002 | 772,275 (50,435) | 2.03 (1.84–2.25) | 1.23 (1.05–1.43) | |
| Othere | 28,360 | 23,627,118 (771,937) | 315 | 246,920 (21,593) | 1.05 (0.89–1.23) | 0.90 (0.74–1.09) | |
Abbreviations: ED, emergency department; SE, standard error; CI, confidence interval; χ2, chi-square test for independence; PR, prevalence ratios adjusted for all independent variables in the multi-variable logistic regression models; CHIP, Children’s Health Insurance Program.
Primary diagnosis for ED visit was asthma (ICD-9-CM code 493.0).
p-Value of < 0.01 is used to determine statistically significant association between two categorical variables using chi-square test.
Using t-test (two-tailed) at alpha = 0.01, the percentage of asthma-related ED visits were significantly different between 0–4 years and aged 5–17 years (p < 0.001), between aged 65 years and older and aged 18–34 years (p < 0.001); between Non–Hispanic (NH) whites; between NH whites and NH Blacks (p < 0.001), between NH whites and NH other race (p = 0.009), and between NH whites and Hispanics (p < 0.001); between Northeast and Midwest (p < 0.001), between Northeast and. South (p < 0.001), between Northeast and West (p < 0.001); and between private insurance coverage and Medicare (p < 0.001), and between private insurance coverage and Medicaid/CHIP (p < 0.001), and between Medicare and Medicaid/CHIP (p < 0.001).
U.S. nation’s four main regions as defined by the Census Bureau: the Northeast, Midwest, South, and West.
Includes worker’s compensation, no charge, charity, self-pay, or other.
The percentage of asthma-related visits among children (2.63%) was significantly greater than the percentage among adults (0.94%) (adjusted prevalence ratio [PR]: 2.28 [1.96–2.65]). In addition, the percentage of asthma-related ED visits was greater for children aged 5–17 years (3.14%) than for children aged 0–4 years (2.00%). Among adults, the percentage of asthma-related ED visits was similar for adults aged 18–34 years and 35–64 years but lower for aged ≥65 years (18–34 years, 1.03%; 35–64 years, 1.12%; ≥65 years, 0.39%) (Table 2). The percentage of asthma-related ED visits for non-Hispanic blacks (2.17%; PR: 2.26 [1.97–2.60]), non-Hispanic other race (1.42%; PR: 1.54 [1.09–2.17]), and Hispanics (1.86%; PR: 1.74 [1.47–2.08]) were greater than for non-Hispanic whites (0.85%). A greater percentage of asthma-related ED visits was reported from hospitals in the Northeast (1.84%; PR: 1.60 [1.30–1.97]) than the West (1.10%). Among source of payment groups, reported ED visits was lower for those covered by Medicare (0.59%), higher for those covered by Medicaid/CHIP (2.03%), and in between for those covered by private insurance (1.21%). However, after adjusting for covariates, differences in reported ED visits remained significant only between those covered by Medicaid/CHIP (2.03%; PR: 1.23[1.05–1.43]) and those covered by private source of payment (1.21%) (Table 2).
Asthma-related hospital admissions among all-cause hospital admissions after an ED visit
About 10.38% (13.9 million) of ED visits from all causes resulted in admission to a treating hospital (Figure 1, Table 3). Of those admissions, 1.12% (n = 155,891) was asthma-related. Among all ED visits resulted in a hospital admission, the percentage of asthma-related admissions was greater among children (6.92%; PR: 8.75 [5.93–12.92]) than among adults (0.76%).
Table 3.
Asthma-relateda hospital admission among all-cause hospital admissions after emergency department (ED) visits by selected characteristics—National Hospital Ambulatory Medical Care Survey, United States, 2010–2015.
| All-cause hospital admissions after an ED visit |
Percentage of asthma-related hospital admission after an ED visit |
||||||
|---|---|---|---|---|---|---|---|
| Characteristics | Number of visits | Weighted number (SE) | Number of visits | Weighted number (SE) | Percent (95% CI) | p-valueb,c | PR (95% CI) |
| Total | 18,150 | 13,934,424 (487,859) | 203 | 155,891 (15,797) | 1.12 (0.92–1.36) | ||
| Sex | 0.074b | ||||||
| Male | 8,484 | 6,589,622 (240,983) | 85 | 60,716 (9,824) | 0.92 (0.67–1.26) | Referent | |
| Female | 9,666 | 7,344,802 (266,365) | 118 | 95,175 (11,828) | 1.30 (1.02–1.64) | 1.60 (1.08–2.36) | |
| Age group (years) | < 0.001 b | ||||||
| Children (0–17) | 1,112 | 816,957 (68,163) | 69 | 56,521 (10,752) | 6.92 (5.03–9.45) | 8.75 (5.93–12.92) | |
| Adults (≥18) | 17,038 | 13,117,467 (464,956) | 134 | 99,370 (11,665) | 0.76 (0.61–0.95) | Referent | |
| Age group (years) | <0.001 b,c | ||||||
| 0–4 | 530 | 390,303 (41,336) | 34 | 28,546 (7,629) | 7.31 (4.70–11.22) | 6.64 (3.45–12.75) | |
| 5–17 | 582 | 426,654 (35,338) | 35 | 27,975 (7,104) | 6.56 (4.05–10.44) | 6.44 (3.18–13.02) | |
| 18–34 | 2,336 | 1,511,103 (69,525) | 24 | 17,980 (4,332) | 1.19 (0.74–1.90) | Referent | |
| 35–64 | 7,140 | 5,507,718 (216,099) | 75 | 56,986 (8,658) | 1.03 (0.77–1.39) | 1.02 (0.54–1.90) | |
| ≥65 | 7,562 | 6,098,646 (230,378) | 35 | 24,405 (5,752) | 0.40 (0.25–0.63) | 0.76 (0.31–1.88) | |
| Race and ethnicity | <0.001 b,c | ||||||
| Non-Hispanic white | 11,880 | 9,468,292 (363,802) | 73 | 52,796 (8,458) | 0.56 (0.41–0.76) | Referent | |
| Non-Hispanic black | 3,190 | 2,410,347 (141,638) | 76 | 59,269 (8,988) | 2.46 (1.87–3.22) | 3.25 (2.07–5.12) | |
| Non-Hispanic othere | 764 | 435,438 (42,864) | 8–e | –e | –e | –e | |
| Hispanic | 2,316 | 1,620,347 (101,740) | 46 | 38,150 (7,619) | 2.35 (1.62–3.40) | 2.42 (1.46–4.00) | |
| U.S. Census region | 0.469b,c | ||||||
| Northeast | 4,574 | 2,990,590 (212,254) | 53 | 36,117 (7,011) | 1.21 (0.83–1.76) | 1.06 (0.60–1.90) | |
| Midwest | 4,377 | 3,371,954 (253,766) | 48 | 29,224 (5,704) | 0.87 (0.60–1.26) | 0.87 (0.48–1.60) | |
| South | 5,764 | 5,020,189 (312,406) | 66 | 62,584 (11,172) | 1.25 (0.89–1.74) | 0.86 (0.47–1.57) | |
| West | 3,435 | 2,551,691 (176,262) | 36 | 27,965 (6,560) | 1.10 (0.70–1.72) | Referent | |
| Expected source of payment | <0.001 b,c | ||||||
| Private insurance | 4,078 | 3,180,669 (144,181) | 45 | 41,701 (8,446) | 1.31 (0.88–1.94) | Referent | |
| Medicare | 7,948 | 6,404,121 (253,706) | 43 | 26,572 (5,395) | 0.41 (0.28–0.62) | 0.54 (0.26–1.11) | |
| Medicaid/CHIP | 3,364 | 2,305,918 (110,217) | 85 | 59,642 (9,213) | 2.59 (1.95–3.43) | 1.01 (0.64–1.59) | |
| Othere,f | 1,694 | 1,273,741 (70,302) | 16–e | –e | –e | –e | |
Abbreviations: ED, emergency department; SE, standard error; CI, confidence interval; χ2, chi-square test for independence; PR, prevalence ratios adjusted for all independent variables in the multi-variable logistic regression models; CHIP, Children’s Health Insurance Program.
Primary diagnosis for ED visit was asthma (ICD-9-CM code 493.0).
p-Value of <0.01 is used to determine statistically significant association between two categorical variables using chi-square (χ2) test.
Using t-test (two-tailed) at alpha = 0.01, the percentage of asthma-related hospital admissions were significantly different between adults aged 65 years and older and aged 18–34 years (0.008); between non-Hispanic blacks and non-Hispanic whites (<0.001), between non-Hispanic whites and Hispanics (<0.001); and between those with private insurance and Medicare (0.001), between private insurance and Medicaid/CHIP (0.003), between Medicare and Medicaid/CHIP (p<0.001).
U.S. nation’s four main regions as defined by the Census Bureau: the Northeast, Midwest, South, and West.
Relative standard error of the estimate is greater than 30% or number of visits is less than 30; estimate is unstable.
Includes worker’s compensation, no charge, charity, self-pay, or other
The percentage of asthma-related hospital admission was similar for children ages 0–4 years and 5–17 years. However, among adults, the percentage of asthma-related ED visits resulting in a hospital admission decreased as age increased (18–34 years, 1.19%; 35–64 years, 1.03%, and ≥65 years, 0.40%) (Table 3). The percentage of asthma-related ED visits resulting in hospital admission was significantly higher among females (1.30%; PR: 1.60 [1.08–2.36]), non-Hispanic blacks (2.46%; PR: 3.25 [2.072–5.12]), and Hispanics (2.35%; PR: 2.42 [1.46–4.00]) than the corresponding references (percentage among males (0.92%) and non-Hispanic whites (0.56%), respectively). The percentage of asthma-related ED visits resulting in hospital admission did not differ by hospital’s geographic location and source of payment (Table 3).
Discussion
The findings in this study are based on large samples of nationally representative ED visits from the National Hospital Ambulatory Medical Care Survey (NHAMCS) (13). About 10.38% of all ED visits resulted in a hospital admission of which 1.12% were asthma-related. About 13.01% of hospital admissions resulted in an admission to a critical care unit, of which 1.20% were asthma-related. The low percentage of critical care unit admissions may reflect the nature of asthma: asthma exacerbations are episodic and reversible by appropriate treatment and management (10).
Of all ED visits, the percentages of asthma-related ED visits and asthma-related hospital admission were greater for children than adults and for blacks and Hispanics than whites, non-Hispanic. These findings are similar those reported in the literature. For example, children with asthma have higher healthcare resource use (5), especially those who might not have a primary care physician or usual place for primary care (4). The percentage of all-cause ED visits by patients with asthma was the highest for children aged 5–17 years compared with all other age groups, including adults (8). Black children with asthma from low-income families were more likely to return to the ED within 12 months than were white children with asthma. Among families whose primary language was not English, Hispanic and Asian/Pacific Islanders with asthma were more likely to be hospitalized at the first ED visit (15). In this study, we could not assess other risk factors for asthma-related ED visits or hospitalizations because related information was not available in the database, such as those factors identified by other studies. Stanford and colleagues (16) showed that the risk for a recurrent asthma-related ED visit or inpatient stay increases as the time to initiate an asthma controller medication increased. Children of lower income families were more likely to have ED re-visits, and younger children and those with severe asthma were more likely to have ED re-visits and hospitalizations (17).
These study findings also reveal that the percentage of asthma-related ED visits was higher in hospitals located in the Northeast than the West. Identifying reasons for higher asthma-related ED visits in hospitals located in the Northeast is beyond the scope of this study, although asthma prevalence is usually higher in the Northeast (9). In addition, percentage of asthma-related ED visits were higher for persons with Medicaid or CHIP healthcare coverage than for persons with private healthcare coverage. This might partly be explained by characteristics of enrollees, given that Medicaid or CHIP enrollees are more likely to be poor, less educated, and minorities (18), and they are more likely to have high healthcare resource use because of asthma (4,5,15–17).
These findings are based on large samples of nationally representative ED visits from National Hospital Ambulatory Medical Care Survey (NHAMCS). By analyzing the data, we were able to obtain reliable estimates for asthma-related ED visits and hospital admission after an ED visit by demo-graphic characteristics, hospital locations, and primary source of payments. A limitation, however, is that the data are cross-sectional: information is not on patients but on visits, which could include more than one visit per patient. The database also has limited information on most of the possible risk factors for ED visits and hospital admissions after an ED visit. However, these limitations should not affect the accuracy of the study findings, which describe the distribution of asthma-related ED visits and ED visits resulting in hospitalization by selected characteristics. These characteristics may serve as a proxy for the other possible risk factors for healthcare use that were not assessed (e.g.environmental triggers, low income, appropriate medical care including medication adherence, and access to primary care and specialty care), because of lack of related information in the database (2–4,11,12,15–18). Finally, because our study focused on ED visits and hospitalizations for which asthma was listed as the primary diagnosis and excluded all other none-primary asthma diagnoses, our results suggest an underestimate of asthma-related visits in ambulatory care settings.
Conclusions
The percentages of asthma-related ED visits and hospital admissions after an ED visit were higher for children than for adults, and higher for blacks and Hispanics than for whites. These findings might prompt future studies on identifying additional potential risk factors for frequent ED visits among disproportionally affected subpopulations and promoting targeted public health strategies to reduce preventable asthma-related ED visits. Additional investigation about asthma-related admissions to critical care units from post-ED visits could inform healthcare providers about the overall burden of asthma.
Funding
The authors received no financial support for the research, authorship, or publication of this article.
Footnotes
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- 1.Centers for Disease Control and Prevention. Asthma. Data, statistics, and surveillance, National Health Interview Survey (NHIS) data [accessed 2019 Mar 4]. https://www.cdc.gov/asthma/nhis/default.htm.
- 2.Zahran HS, Bailey CM, Damon SA, Garbe PL, Breysse PN. Vital signs: asthma in children—United States, 2001–2016. MMWR Morb Mortal Wkly Rep 2018;67(5):149–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suruki RY, Daugherty JB, Boudiaf N, Albers FC. The frequency of asthma exacerbations and healthcare utilization in patients with asthma from the UK and USA. BMC Pulm Med 2017;17(1):74. doi: 10.1186/s12890-017-0409-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pourat N, Davis AC, Chen X, Vrungos S, Kominski GF. In California, primary care continuity was associated with reduced emergency department use and fewer hospitalizations. Health Aff 2015;34(7): 1113–1120. doi: 10.1377/hlthaff.2014.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perry R, Braileanu G, Palmer T, Stevens P. The economic burden of pediatric asthma in the United States: literature review of current evidence. Pharmacoeconomics 2019;37(2):155–167. doi: 10.1007/s40273-018-0726-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pearson WS, Goates SA, Harrykissoon SD, Miller SA. State-based Medicaid costs for pediatric asthma emergency department visits. Prev Chronic Dis 2014;11: E108. doi: 10.5888/pcd11.140139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rui P, Kang K. National Hospital Ambulatory Medical Care Survey: 2015 emergency department summary tables [accessed 2019 Jun 13]. http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2015_ed_web_tables.pdf.
- 8.Centers for Disease Control and Prevention. QuickStats: percentage of all emergency department (ED) visits made by patients with asthma, by sex and age group—National Hospital Ambulatory Medical Care Survey, United States 2014–2015. MMWR Morb Mortal Wkly Rep 2018;67:167. doi: 10.15585/mmwr.mm6705a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moorman JE, Akinbami LJ, Bailey CM, Zahran HS, King ME, Johnson CA, Liu X. National surveillance of asthma: United States, 2001–2010. National Center for Health Statistics. Vital Health Stat 3 2012;35:1–58. [accessed 2019 Jun 13]. https://www.cdc.gov/nchs/data/series/sr_03/sr03_035.pdf. [PubMed] [Google Scholar]
- 10.National Heart, Lung, and Blood Institute. Expert panel report 3: guidelines for the diagnosis and management of asthma. NIH pub no 07–4051 Bethesda (MD): National Institutes of Health; 2007. [accessed 2019 Jun 13]. https://www.nhlbi.nih.gov/health-topics/guidelines-for-diagnosis-management-of-asthma. [Google Scholar]
- 11.Institute of Medicine Committee on the Assessment of Asthma and Indoor Air, Division of Health Promotion and Disease Prevention. “Front matter.” Clearing the air: asthma and indoor air exposures Washington, DC: The National Academies Press; 2000. [Google Scholar]
- 12.Hannaway PJ. Asthma—an emerging epidemic: a manual for patients with asthma, parents of children with asthma, asthma educators, health-care providers, school nurses and coaches Marblehead (MA): Lighthouse Press; 2002. [Google Scholar]
- 13.Centers for Disease Control and Prevention. About the ambulatory health care surveys [accessed 2019 Mar 1]. https://www.cdc.gov/nchs/ahcd/about_ahcd.htm.
- 14.Centers for Disease Control and Prevention. National Hospital Ambulatory Medical Care Survey. Ambulatory health care data. Datasets and documentation. Downloadable documentation, NHAMCS, 1992–2016 [accessed 2019 Jun 13]. https://www.cdc.gov/nchs/ahcd/datasets_documentation_related.htm.
- 15.Aratani Y, Nguyen HA, Sharma V. Asthma-related emergency department visits among low-income families with young children by race/ethnicity and primary language. Pediatr Emerg Care 2019. doi: 10.1097/PEC.0000000000001430. [DOI] [PubMed] [Google Scholar]
- 16.Stanford RH, Buikema AR, Riedel AA, Camargo CA Jr, Rey GG, Chapman KR. Asthma controller delay and recurrence risk after an emergency department visit or hospitalization. Respir Med 2012;106(12): 1631–1638. doi: 10.1016/j.rmed.2012.08.017. [DOI] [PubMed] [Google Scholar]
- 17.Li P, To T, Guttmann A. Follow-up care after an emergency department visit for asthma and subse-quent healthcare utilization in a universal-access healthcare system. J Pediatr 2012;161(2):208–313.e1. doi: 10.1016/j.jpeds.2012.02.038. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. National Health Interview Survey. Summary health statistics: health insurance coverage; Table P-11a 2018. [accessed 2019 Jun 13]. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2017_SHS_Table_P-11.pdf.


