Abstract
A high-output stoma (HOS) or fistula is when small bowel output causes water, sodium and often magnesium depletion. This tends to occur when the output is >1.5 -2.0 L/24 hours though varies according to the amount of food/drink taken orally. An HOS occurs in up to 31% of small bowel stomas. A high-output enterocutaneous fistula may, if from the proximal small bowel, behave in the same way and its fluid management will be the same as for an HOS.
The clinical assessment consists of excluding causes other than a short bowel and treating them (especially partial or intermittent obstruction). A contrast follow through study gives an approximate measurement of residual small intestinal length (if not known from surgery) and may show the quality of the remaining small bowel.
If HOS is due to a short bowel, the first step is to rehydrate the patient so stopping severe thirst. When thirst has resolved and renal function returned to normal, oral hypotonic fluid is restricted and a glucose-saline solution is sipped. Medication to slow transit (loperamide often in high dose) or to reduce secretions (omeprazole for gastric acid) may be helpful. Subcutaneous fluid (usually saline with added magnesium) may be given before intravenous fluids though can take 10–12 hours to infuse. Generally parenteral support is needed when less than 100 cm of functioning jejunum remains. If there is defunctioned bowel in situ, consideration should be given to bringing it back into continuity.
Keywords: short bowel syndrome, IBD Surgery, malabsorption, nutritional support, surgical complications
Key points.
Exclude and treat causes other than a short bowel (eg, intermittent/partial small bowel obstruction).
Look at the stoma and output volume, colour and consistency. The sodium content is about 100 mmol/L.
Rehydrate and thus treat thirst.
Restrict hypotonic fluid (tea, coffee, water, juices, etc).
Sip an oral glucose/saline solution (sodium concentration 90–120 mmol/L) and if hypomagnesaemia give magnesium supplements.
If an oral/enteral liquid feed is given, it aims to be iso-osmolar (300 mOsm/kg) and have a sodium concentration of 90–120 mmol/L.
Loperamide (4–24 mg four times a day) may be given to slow transit and increase absorption. Codeine phosphate may be added but is addictive and care is needed in the elderly.
Omeprazole (especially in those with a net ‘secretory’ output) will reduce stomal output and if the dose is adequate will increase the stomal fluid pH to greater than 5.
If dehydration persists, subcutaneous or parenteral saline with added magnesium may be given.
Monitor serum urea, electrolytes, magnesium and a random urine sodium concentration.
Bring colon (or other small bowel) back into circuit (if present and possible).
Introduction
A normal ileostomy may function within the first day of surgery depending on whether an ileus occurs (often due to opiates and excessive intravenous saline). The stomal output from an ileostomy may reduce over several months as adaptation occurs; however, patients with a jejunostomy (less than 200 cm small bowel remaining) do not generally show any improvement in absorption with time. The normal ileostomy output, when established, is 600–1200 mL/24 hours.
A high-output stoma (HOS) (often called ileostomy diarrhoea) is when the output is enough to cause ‘dehydration’ (water and sodium depletion). In general, this occurs with an output of greater than 1.5–2.0 L / 24 hours. However, this depends on the oral intake. A 2 L output for someone taking in 4.0 L will cause no problems but if only an intake of 0.5 L it will result in dehydration.1
Patients with an output greater than the oral intake are termed net ‘secretors’ and will need parenteral support, while those with an output less than the oral intake are termed net ‘absorbers’ and can be managed on an oral regimen.1 This patient classification can be difficult unless the total (solid and liquid) oral intake and the output are measured over 24 hours in a careful balance study.
An HOS occurred early in 16% patients (within 3 weeks of a stoma being formed) and late (more than 3 weeks) in 4% in whom this was a persistent problem.2 Other studies show similar rates 16%–31% following surgery.3–5 Problems are more common in patients with a loop ileostomy or after an ileal resection. There are rarely any problems of HOS when more than half the colon remains in continuity and there is more than 50 cm functioning small bowel present.25
Evidence that many patients with an ileostomy are salt and water depleted comes from the observation that plasma renin and aldosterone levels are high in ileostomy patients6 and 13% have a urine sodium concentration of less than 10 mmol/L.7 Unrecognised, chronic dehydration in these patients can lead to end stage renal failure, so the occurrence of a chronic HOS needs to be detected early and managed well with regular monitoring. If the management of the HOS is not well addressed and a renal transplant is performed it is unlikely to be successful. Diuretics given to patients with an ileostomy (especially if they have had problems of HOS) may precipitate renal failure and generally should be avoided. Ideally a specialist local service should monitor these patients; currently, this is often a nutrition support team.
Causes of an HOS
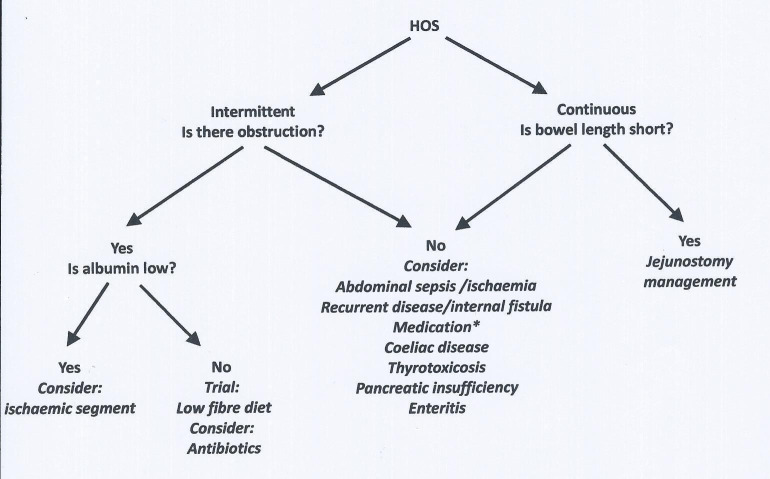
Causes of an HOS other than a short bowel (jejunostomy <200 cm) should be sought. This is a common group who may have a normal length of small intestine (figure 1, box 1). An early HOS is most commonly due to sepsis (a raised white bllood cell count () on day 1 is a clue8 and may be why an early HOS is more common in diabetics.4 One explanation for sepsis causing an HOS is that it leads to hypoalbuminaemia and oedema of the stoma leading to outlet obstruction. The other common causes of an early HOS are medication related; this can be because of a prokinetic drug (eg, metoclopramide) or the sudden usually accidental withdrawal of one (eg, opiates or cortisol). Clostridium difficile can affect the small bowel and cause an HOS.9 A chronically HOS is most commonly due to a short bowel (jejunostomy). However, intermittent/partial obstruction due to small bowel strictures is common (with associated bacterial overgrowth), a stenosis is most commonly at the stoma.5 Recurrent disease (including ischaemia), internal fistula, small bowel diverticula, coeliac disease and thyrotoxicosis can all contribute and if treated the HOS may resolve. If the HOS is due to strictures and there is a low serum albumin it may be that a section of chronically/critically ischaemic bowel remains in situ and the problem will only resolve with surgical resection.
Figure 1.
Management of high-output stoma (HOS). Intermittent is taken as less than one episode of HOS/month and continuous as more than one episode of HOS/month.
Box 1. High-output stoma.
Early (<3 weeks of formation)
Abdominal sepsis/ileus.
-
Drug related
Prokinetic drugs (eg, metoclopramide).
Low cortisol.
Opiate withdrawal (eg, codeine phosphate).
Enteritis (Clostridium difficile)
Late (chronic more than 3 weeks)
Short bowel—jejunostomy <200 cm
Intermittent/partial obstruction (strictures).
Other less common causes:
Recurrent disease.
Internal fistula.
Small bowel diverticula.
Coeliac disease.
Thyrotoxicosis.
Reasons for an HOS in patients with a short bowel (jejunostomy)
Normal small intestinal length measured at surgery, radiologically or at autopsy, is very variable and ranges from 275 to 1049 cm measured from the duodeno-jejunal flexure.10–12 Due to this wide range of normal bowel length, it is most important to know the length of bowel remaining rather than the length removed. Problems of hydration due to a short length of remaining bowel (and a colectomy) tend to occur when less than 200 cm jejunum remain. Often a patient is not known to have a short bowel, but their starting bowel length may have been short, and hence after a minor resection they develop the problems associated with a short bowel.13 A short bowel is the most common reason for a late/chronic HOS though is often not recognised because small bowel length has not been measured at surgery.
The physiological reasons for an HOS in patients with a short bowel and jejunostomy are: loss of the normal daily secretions produced in response to food, hypotonic fluid drunk (with excessive thirst), gastric acid hypersecretion and rapid gastrointestinal transit.
Loss of normal daily intestinal secretions
Daily secretions amount to about 4 L/24 hours (0.5 L saliva, 2 L gastric acid, 1.5 L pancreaticobiliary secretions) and are produced in response to the food and drink consumed (about 2 L/24 hours) and cannot all be absorbed in a short remaining bowel (less than 100 cm) so are lost through the stoma. These stomal losses are large and the sodium concentration is about 100 mmol/L (range 80–140 mmol/L),14 so a 4 L output will contain about 400 mmol of sodium.
In most normal subjects, about 6 L of chyme pass the duodenojejunal flexure daily and this only starts to be less dilute than that consumed after about 100 cm jejunum. This length is the approximate transition length between a net ‘secretor’ and a net ‘absorber’. Even in the fasting state there is an obligatory loss of intestinal secretions produced with the migrating myoelectric complex.15
Hypotonic fluid and thirst
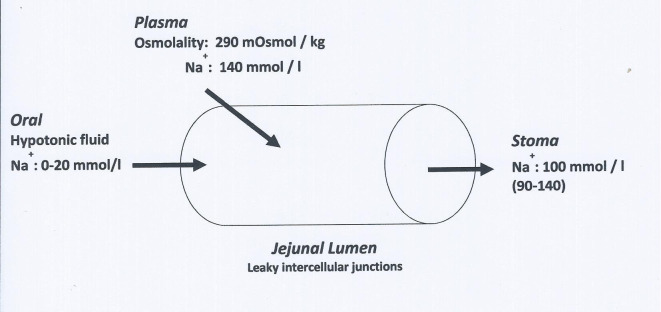
Jejunal mucosa is ‘leaky’ and rapid sodium fluxes occur across it. If water or any solution with a sodium concentration of less than 90 mmol/L is drunk there is a net efflux of sodium from the plasma into the bowel lumen16 until a luminal sodium concentration of 90–100 mmol/L is reached. In a patient with a jejunostomy, this fluid is then lost in the stomal output (100 mmol/L sodium) (figure 2). Patients, who are water and sodium depleted, are often very thirsty and so may drink an increasing amount of hypotonic fluid (often containing no sodium) and the effect is to increase the stomal output and increase the sodium losses and so further increasing the thirst.7 16–19
Figure 2.
Diagram to show sodium movement into the jejunal lumen when hypotonic fluid is drunk (upper gastrointestinal secretions not shown).
Gastric acid hypersecretion
Hypergastrinaemia is observed after a small bowel resection in humans20 21 and this could result in gastric acid hypersecretion and thus contribute to the high output from a jejunostomy. In humans, gastric acid hypersecretion has only been demonstrated in the immediate postoperative period in patients with a retained colon.22 It is unclear whether this phenomenon persists beyond the first weeks.
Rapid gastrointestinal transit
Rapid gastric emptying of liquid occurs and may increase the stomal output.23 The gastric emptying rate is fastest in those with the shortest lengths of residual jejunum.23 Small bowel transit time for liquid and solid is also very rapid.23 Both of these effects may be due to low serum levels of peptide YY (PYY)21 and, to a lesser extent, low levels of glucagon-like peptide 2 (GLP-2).24
Reasons for hypomagnesaemia
Hypomagnesaemis is estimated to occur in 78% of patient with a jejunostomy.25 While it may cause fatigue, depression, irritability, muscle weakness, tremor, tetany if there is associated hypocalcaemia, and, if very severe, convulsions; it is often asymptomatic even at very low serum levels (eg, 0.2 mmol/L). The reasons for hypomagnesaemia include secondary hyperaldosteronism,26 27 removal of ileum/colon which are key areas in the gut for absorption, free fatty acid malabsorption (so complexing with Ca and Mg)28 29 and taking proton pump inhibitor (PPIs) drugs.30 In the long-term hypomagnesaemia will lead to a loss of bone density with a risk of fractures and chondrocalcinosis.31
Assessment of a patient with an HOS
The assessment starts with looking for a cause of an HOS (figure 1, box 1) other than a short bowel. A history of colicky abdominal pain, loud bowel sounds (borborygmi); a stoma ceasing to work for a time is suggestive of an obstructive cause. The HOS occurs during recovery from the obstruction and at this time the patient may have no symptoms other than those of dehydration. Such patients often present for medical care episodically (every few months or even years). Radiological contrast examinations do not always show the stricture(s) and a trial of a low fibre/residue diet can be used both as a treatment and as a diagnostic test. If there are strictures bacterial overgrowth may be occurring and a trial of oral antibiotics (eg, coamoxyclav or rifaximin) may be tried and if successful given in rotation (eg, changing every 6 weeks). If pancreatic malabsorption is thought to contribute to an HOS then a trial of pancreatic enzyme replacement may be given. A stomal elastase measurement is unlikely to be reliable due to dilution by secretions and oral fluid intake.
The symptoms from water and sodium loss through the stoma are of thirst, cramps (may also relate to hypomagnesaemia) and faintness. The patient may complain of frequent emptying of their stoma bag especially at night, difficult skin care often due to leakage and the need to find a toilet quickly.
The physical examination includes looking for rapid weight loss (negative fluid balance), a postural blood pressure fall (>10 mm Hg), oliguria (less than 800 mL/24 hours) and an assessment of the patient’s nutritional status (this is usually good unless the remaining small bowel length is less than 100 cm). The stoma effluent volume, colour and consistency should be inspected (a yellow/green colour in an established stoma suggests a short length of remaining bowel). A finger should be inserted gently into the stoma to determine if there is a stenosis. However, an obstruction at the stoma may not be felt if it is a functional obstruction, due to oedema or the thickness of the abdominal wall, and a trial of a wide bore catheter placed into the stoma may be tried to determine if the output reduces.
Biochemistry will include measurement of the serum urea, creatinine, magnesium and measurement of a random urine sodium concentration (<10 mmol/L is significant). Only when dehydration is severe will the urea/creatinine rise. The creatinine may be low if there is reduced muscle mass. Urinary electrolytes are usually more useful than serum measurements because the normal physiological homeostatic mechanisms preserve serum electrolyte concentrations until the late stages of depletion. When interpreting a urinary sodium result it is important to check that the patient is not receiving diuretics or intravenous/subcutaneous saline or has renal impairment/tubular damage (eg, from resolving acute kidney injury) when the result may be falsely normal. In addition a urinary sodium concentration can be low if the patient has hypovolaemia due to a low plasma oncotic pressure (eg, due to a low serum albumin).
Citrulline is an amino acid produced by functioning small bowel mucosa, fasting levels do correlate with residual small bowel length. Although clinically used to assess the progress of small bowel function after a small bowel transplant or when the colon is brought into continuity, it has not been widely adopted as a marker of functioning small bowel.32
A radiological contrast follow through examination is usually performed to show the length of the remaining bowel and its health; it may detect recurrent disease/obstruction.33
Treatment
A patient presenting with an HOS and renal failure will need urgent rehydration and in most cases the progression to irreversible or chronic renal failure can be prevented. The replacement fluid needs to contain 100–150 mmol sodium/L for example, intravenous normal saline, 2–4 L/day. During this time, the patient may be kept ‘nil by mouth’ to reduce the stomal output. In general, dialysis is avoided as the removal of any more fluid can worsen the renal failure which may become permanent. Great care must be taken not to give too much fluid as this will readily cause oedema, partly due to the high circulating aldosterone levels.6 7 34 35 Cramps can be rapidly helped by oral or intravenous sodium chloride, and/or by magnesium supplementation.
Once renal failure has been corrected and thirst relieved, usually over 2–3 days, an attempt is made to reduce stomal output, even in patients with a jejunostomy requiring parenteral nutrition, as this may well reduce the amount or frequency of intravenous fluid replacement and the social difficulties in managing the stoma. If there is a cause for the HOS this must be treated, if one cannot be found and the bowel length is apparently normal the same regimen as for a short bowel will be followed.
Sometimes, admitting patients with a chronic HOS, giving intravenous saline and keeping them ‘nil by mouth’ will demonstrate to them that their output is mostly driven by their oral intake. These patients are dependent on their treatment regimen and if missed/stopped for a day may result in dehydration and a hospital admission for rehydration
The oral treatment to reduce an HOS and its consequences of dehydration starts with restricting oral hypotonic fluids and giving a glucose saline solution (or in mild cases extra oral salt) to sip. If this alone is not successful then oral medications to reduce gut motility and/or secretions may be tried.
Restrict oral fluids
Treatment for the high output from a jejunostomy, ileostomy or high fistula starts with the patient restricting the total amount of oral hypotonic fluid (water, tea, coffee, fruit juices, alcohol or dilute salt solutions) to 0.5–1.0 L/24 hours. To make up the rest of the fluid requirement the patient is encouraged to drink a glucose–saline rehydration solution. Many patients at home with a marginally high stomal output (1–1.5 L) will be helped by a combination of mild oral fluid restriction (less than 1.5 L per day) and the addition of salt to their diet.
Patients are often advised to take liquids and solids at different times (no liquid for half an hour before and after food), however, there is no published evidence that this reduces stomal output or increases absorption of macronutrients or micronutrients.36
Patients must never be advised to ‘drink as much as possible’ either to quench their thirst or keep up with their stomal output as this will increase stomal sodium losses, worsen dehydration and increase thirst.
Drink oral glucose–saline solution
Patients with stomal losses of less than 1200 mL daily can usually maintain sodium balance by adding extra salt to the limit of palatability at the table and when cooking. When stoma losses are in the range 1200–2000 mL, or sometimes more, it is possible for a patient to maintain sodium balance by taking a glucose–saline solution or salt capsules.18 In hot weather, patients with a stoma are more likely to have problems of dehydration because of water and sodium loss in sweat.
As the sodium content of jejunostomy (or ileostomy) effluent is relatively constant at about 90 mmol/L and as there is coupled absorption of sodium and glucose in the jejunum,37–39 patients are advised to sip a glucose–saline solution with a sodium concentration of at least 90 mmol/L throughout the day. The first WHO cholera solution has a sodium concentration of 90 mmol/L40 and is still commonly used (without the potassium chloride) (also referred to as the St Mark’s solution) (table 1). Patients can prepare this solution at home using simple measuring scoops. There is no evidence that the sodium bicarbonate adds to the effectiveness of this solution39 and it may be more palatable if sodium bicarbonate is replaced by sodium citrate. Indeed a pure sodium citrate solution (sodium concentration 120 mmol/L) was successful.41 If the sodium concentration is increased further (eg, to 136 mmol/L), absorption of sodium and water is improved.42 Although taste perception changes in patients who are depleted in salt and water, they may find this solution, which tastes like ‘sweet seawater’, too salty to drink. Double strength Dioralyte is often given (table 1). It does contain potassium and so serum potassium measurements may need to be made more frequently than 3 monthly, especially if renal impairment occurs.
Table 1.
Oral rehydration solutions
| Modified WHO cholera solution ‘St Mark’s solution’* | Dioralyte strength | Sodium citrate solution | ||
| Single | Double† | |||
| Volume (litres) | 1 | 1 | 1 | 1 |
| Na+ (mmol) | 90 | 60 | 120 | 120 |
| K+ (mmol) | 0 | 20 | 40 | 0 |
| Cl- (mmol) | 90 | 60 | 120 | 0 |
| Citrate (mmol) | 0 | 10 | 20 | 120 |
| Glucose (mmol) | 80 | 90 | 180 | 80 |
A stronger solution that can be used is is sodium chloride 7 g (120 mmol), glucose (8 g) (44 mmol) and tap water 1 L.
*Sodium chloride 3.5 g (60 mmol), sodium bicarbonate 2.5 g (30 mmol) or sodium citrate 2.9 g (30 mmol), glucose 20 g (110 mmol) and 1 L tap water.
†10 sachets.
A glucose-polymer (55 g Maxijul) may be substituted for glucose to increase the energy intake by a mean of 115 kcal/day.18 The glucose-polymer (or even a rice-based solution) can be especially useful in diabetic patients as it causes less extreme changes in blood glucose than a glucose-based solution.
The patient should be encouraged to sip a total of 1 L or more of one of these solutions in small quantities at intervals throughout the day. They should make up the majority of the oral fluid intake. As compliance is often a major problem, patients need to understand the need for the solution and can make it more palatable by chilling and/or flavouring with fruit juice. Compliance with the regimen is vital as if 1 day of fluid restriction/glucose saline solution consumption is omitted the patient may be admitted to hospital dehydrated. It is important to note that solutions with a sodium content of less than 90 mmol/L such as single strength Dioralyte or commercial preparations used to treat infective or traveller’s diarrhoea or in sport’s drinks sports are not adequate.
Sodium chloride capsules (500 mg each) are effective when taken in large amounts (14/24 hour), but can cause some patients to feel sick and even vomit.18 If an enteral feed is given, sodium chloride needs to be added to make the total sodium concentration of the feed 100 mmol/L while keeping the osmolality near to 300 mOsm/kg. A hyperosmolar solution/feed (eg, of amino acids) will cause increase stomal water losses.
Some patients cannot be maintained with an oral regimen (usually if jejunal length is less than 100 cm) and regular subcutaneous or parenteral saline supplements are needed. Subcutaneous saline can be slow to run (eg, a litre usually containing 4–8 mmol magnesium sulphate that takes 10–12 hours to infuse), it may cause swelling of a limb; however, it is relatively simple and quick to start with few risks of infection. It is most appropriate if the additional fluid is only needed 1–4 days a week. Patients with less than 100 cm jejunum remaining may need oral or parenteral nutritional supplements (see table 2), but a few need, no nutritional supplements, only 1 or 2 L of parenteral saline daily, usually with added magnesium sulphate (4 mmol/L). This may be given as a regular infusion at home.
Table 2.
Jejunostomy length and the type of nutritional/fluid support needed
| Jejunum (cm) | Nutrition | Fluid |
| 0–50 | Parenteral | Saline |
| 51–100 | Parenteral* | Saline |
| 101–150 | Oral/enteral | OGS |
| 151–200 | None | OGS |
*At 85–100 cm may need parenteral saline only.
OGS, oral (or enteral) glucose/saline solution.
Drug therapy for an HOS (jejunostomy)
If restricting oral fluids and giving a glucose–saline solution to drink are not adequate treatment, drugs may be needed. The intestinal output, especially in net ‘secretors’ rises after meals (figure 3), and it is therefore important to give the drugs before food. Drugs used to reduce jejunostomy output act to reduce either intestinal motility or secretions.
Figure 3.
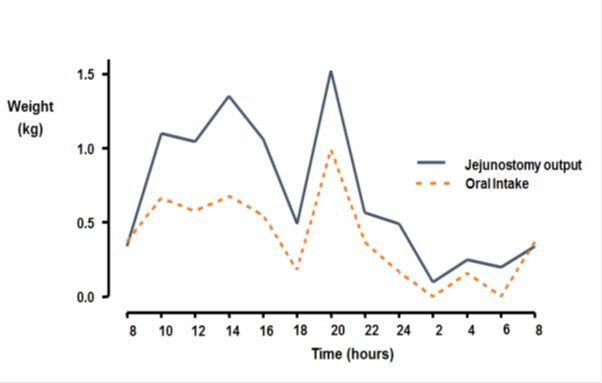
Jejunostomy output and oral intake in a patient with 30 cm jejunum.1
Antimotility (antidiarrhoeal) drugs
Opiate drugs such as tincture of opium (laudanum) or codeine phosphate have been used for many years to treat diarrhoea but are sedative and, in the long term, addictive. Synthetic drugs were manufactured with the aim that they should be free of opiate-like activity on the central nervous system. Diphenoxylate (Lomotil) was the first to be used in clinical practice but has largely been replaced by loperamide (Imodium) which has no central nervous system effects. Loperamide is preferred to codeine phosphate as it does not sedate and is not addictive. Codeine phosphate increases the output of stomal fat43 44; loperamide does not44 45 although it reduces the pancreaticobiliery secretions.46
Loperamide and codeine phosphate reduce intestinal motility and thus decrease water and sodium output from an ileostomy by about 20%–30%.43–45 47 48 Oral loperamide, 4 mg taken four times a day, was more effective in reducing the weight and sodium content of ileostomy fluid than codeine phosphate 60 mg taken four times a day,44 but the effect of both together may be greater.49 Loperamide circulates through the entero-hepatic circulation, but this is severely disrupted in these patients, and small bowel transit may be rapid. Thus, high doses of loperamide (eg, 12–24 mg) at a time) may be needed, as in patients who have had a vagotomy and pyloroplasty.50 One case series suggested even higher doses (40 mg five times a day, 30 mg three times a day and 100 mg four times a day) were effective.51
In 2017, the UK Medicines and Healthcare products Regulatory Agency issued an alert about serious cardiovascular events (QT prolongation, torsades de pointes and cardiac arrest/deaths) associated with high or very high doses of loperamide when used as a drug of abuse or for self-treatment of opioid withdrawal. The British Intestinal Failure Alliance advice about this included performing an ECG in all patients with an HOS/fistula before starting high-dose loperamide (more than 4 mg four times a day) and the QT interval being measured. It was suggested that the ECG should be repeated after starting the high dose and then every 3 years. The total daily dose of loperamide should be below 80 mg, however, if exceeded serum loperamide levels should be measured. Loperamide toxicity should be considered in any patient with fainting episodes not accounted for by dehydration or other drugs and if there is QT prolongation or a ventricular arrhythmia including torsades de pointes or if a cardiac arrest has occurred.52
Loperamide and codeine phosphate are effective in most patients with a jejunostomy,53 particularly net ‘absorbers’. A combination of them taken traditionally 15–30 min before food, a glucose–saline solution and other fluid restriction can liberate some patients from dependence on parenteral saline supplements.49
Antisecretory drugs
Food and drink are diluted by digestive juices, thus the volume of stomal effluent can be reduced in ‘secretors’ by drugs that reduce the secretions from the stomach, liver and pancreas. Drugs that reduce gastric acid secretion, such as the H2 antagonists or PPIs or the somatostatin analogue octreotide, are most commonly used. These drugs may not be effective in net ‘absorbers’ and should only be continued if there is a measureable reduction in stomal output with their use. They should not be used routinely (especially PPIs).
H2 antagonists/PPIs
H2 antagonists (cimetidine,54 55 ranitidine1) and PPIs (omeprazole)56 57 are effective in reducing the secretions in net ‘secretors’ in whom the stomal output usually exceeds 2 L/24 hours. This beneficial effect is likely to be due to the reduction in normal daily gastric acid secretion and a reduction in gastric acid hypersecretion. Omeprazole is readily absorbed in the duodenum and upper small bowel, but if less than 50 cm of jejunum remains it may need to be given intravenously. Giving omeprazole orally dissolved in bicarbonate may improve its absorption. Omeprazole usually has little beneficial effect in patients who are net ‘absorbers’. They do not change the absorption of energy, carbohydrate, lipid, nitrogen and divalent cations54–57 and do not reduce jejunostomy output sufficiently to prevent the need for parenteral fluid and electrolyte replacement.
The PPIs have been associated with Cl difficile infection, abnormal liver function tests, osteopenia/osteoporosis and increased risk of fractures, myocardial infarction and renal impairment.58 When used (eg, omeprazole 40–80 mg daily) the dose can be titrated such that fresh stomal fluid has a pH greater than 5.
Somatostatin and octreotide
Somatostatin and octreotide reduce salivary, gastric and pancreaticobiliary secretions, slow small bowel transit, and may delay gastric emptying; for these reasons they reduce the intestinal output from a jejunostomy in both net ‘secretors’ and ‘absorbers’. Somatostatin has a serum half-life of 3 min so is given by continuous infusion,59 whereas that of octreotide is 90 min so it is usually given as regular (two or three times daily) subcutaneous injections before food.
Studies in adults have shown octreotide to reduce ileostomy diarrhoea and large-volume jejunostomy outputs.1 14 60–66 The greatest reductions in intestinal output have occurred in net ‘secretors’, and many patients have been able to reduce the volume of parenteral support needed.63 66 Although some patients have achieved positive intestinal fluid balance, they have rarely been able to stop parenteral fluids completely.63 66 All studies have shown a reduction in sodium output which parallels that of the intestinal output.1 14 60–66 The reduction in output in net ‘absorbers’ may be none or very small. In one study in which all patients had mild ileostomy diarrhoea (0.8–1.3 kg/24 hours the output reduced by only 0.3 kg/24 hours.61 In three patients, an intravenous dose of 50 µg octreotide twice a day was as effective in reducing the intestinal output as 100 µg three times a day.63 Magnesium balance has not been changed by octreotide62 64 and it does does not significantly change total energy63 65 66 or nitrogen absorption.60 62 64–66 As pancreaticobiliary secretion is reduced, it would be expected that fat absorption would be reduced61; however, it is usually unchanged.64–66
As there is little intestinal adaptation in patients with a jejunostomy,15 the risk (based on some animal studies with short bowel and colon in continuity) of octreotide inhibiting intestinal adaptation is unlikely to be important. In addition the effect of octreotide is maintained in the long term.60 62–64 66 After a year’s continuous therapy with 50 µg intravenous octreotide two times per day, the reduction in stomal output was the same as at the start of treatment.63 66
A subcutaneous injection of octreotide may be painful, especially in the very thin, while an intravenous injection may cause flushing, nausea and headache.63 Blood glucose generally remains within the normal range.64 Patients with a jejunostomy have a very high prevalence of gallstones (45%),25 and long-term octreotide therapy may further increase this.67 Although hypoglycaemia may occur,64 there is no evidence that octreotide causes diabetes or hypothyroidism after prolonged usage. Increasing the consistency of the small bowel contents could increase the risk of developing small bowel obstruction if there are adhesions.
Long-acting octreotide 20 mg68 and lanreotide 120 mg69 have both been used to treat HOS with deep subcutaneous/intramuscular injections every 4 weeks.
Octreotide is not commonly used because oral omeprazole (40 mg once daily) is equally effective. It gave an equivalent reduction in stomal output to intravenous octreotide 50 µg two times per day in two patients.1 56
Mineralocorticoids and desmopressin
The distal ileum, with its tight intracellular junctions, can concentrate the intraluminal contents. This ability develops from 2 to 16 weeks after the formation of an ileostomy.70 71 This capacity for sodium absorption may partly relate to high aldosterone levels6 34 and can be induced by mineralocorticoids72–74 or high-dose hydrocortisone.75 Although intraluminal hydrocortisone does increase jejunal water, sodium and glucose absorption in normal subjects,76 mineralocorticoids do not usually reduce ileostomy output. Corticosteroids are not recommended (unless correcting a deficiency) and mineralocorticoids are unlikely to be successful as there are high circulating aldosterone levels so sodium absorption may already be maximised.
Desmopressin, an analogue of antidiuretic hormone, has no effect on ileal fluid or electrolyte loss in man.77
Cholylsarcosine
A synthetic bile acid resistant to bacterial deconjugation and dehydroxylation, cholylsarcosine improved fat and calcium absorption but did not affect the volume of stomal output.78 79
Clonidine
Clonidine is an α2-adrenergic agonist that prolongs gastrointestinal transit and has been used to treat chronic diarrhoea. A 0.3 mg clonidine patch to eight jejunostomy patients receiving parenteral nutrition resulted in a reduction in stomal output of 0.44 kg/day (39 mmol sodium) without affecting energy, fat or xylose absorption.80 It is rarely used but may (if available) be a treatment for those who are not responding to other conventional treatments.
Peptide hormones (including growth factors)
Patients with a jejunostomy have low circulating levels of PYY (slows transit) and GLP-2.21 24 A GLP-2 agonist teduglutide, which stimulates small bowel mucosal growth and increases absorption of salt, water and nutrients, may be used as a treatment (though is expensive and in the UK is only prescribed by specialist home parenteral nutrition/intestinal failure centres for patients receiving parenteral support).83 While in studies teduglutide may reduce parenteral requirements by 20% and may occasionally allow a patient to stop parenteral nutrition.84–87 There are other longer-acting GLP-2 agonists being developed for clinical use (eg, apraglutide and glepaglutide). A GLP-1 agonist (liraglutide) which primarily slows upper gastrointestinal transit has been used with some success.87 There may be a future role for using combinations of peptide hormone analogues.
Treatment of hypomagnesaemia
The first step in treatment is to correct dehydration and sodium depletion which cause secondary hyperaldosteronism and hence renal magnesium loss. A diet relatively low in fat may be given so preventing the chelation of magnesium in the gut lumen with free-fatty acids so making the magnesium unavailable for absorption.28
Serum magnesium levels can usually be improved by oral supplements, however, the data about the magnesium absorption from different preparations are often derived from normal volunteer studies and studies of patients with a short bowel and retained functioning colon. Tablet dissolution and magnesium availability may be very different in patients with a jejunostomy.
Many oral magnesium salts, which are generally poorly absorbed, have been given as a treatment and include magnesium sulphate, chloride, hydroxide, acetate, carbonate, gluconate, lactate, citrate, aspartate, pyroglutamate, oxide and diglycinate.88 89 In clinical practice in the UK, magnesium oxide, glycerophosphate or aspartate are most commonly given. Magnesium oxide may be given to a total of 12–24 mmol daily and is often given at night when intestinal transit is assumed to be slowest and hence there is more time for absorption. This regimen increases magnesium absorption and does not appear to increase stomal output.
A topical magnesium chloride spray may help those with magnesium depletion who do not adequately absorb magnesium preparations from their gut90 and may offer a mode of correcting serum levels and helping symptoms that may be related hypomagnesaemia. PPI drugs can reduce serum magnesium levels and a trial of stopping these may be beneficial.30
If oral magnesium supplements do not bring the magnesium level into the normal range, oral 1α-hydroxycholecalciferol in a gradually increasing dose (every 2–4 weeks) of 1–9 µg daily has been shown to improve magnesium balance in patients with a retained colon.91 92 This action occurs by increasing both intestinal and renal magnesium absorption.92 Hypomagnesaemia will cause both a failure of parathormone release and a resistance to its action so that 1α-hydroxycholecalciferol cannot be made in the kidney in adequate amounts; thus it is important that the 1α preparation of vitamin D is given.
Magnesium can occasionally be given as: a subcutaneous injection (patients usually have jejunal length of 85–150 cm) of 4 mmol magnesium sulphate every two or more days, but this can cause skin ulceration; an intramuscular injection of 10 mmol/L, but this is painful; or a regular intravenous infusion of 12 or more mmol, usually in a litre of saline over 1–2 hours, though this can cause a flushing sensation. A 4–8 mmol of magnesium sulphate can infused subcutaneously in a litre of saline over 10–12 hours 1–3 times a week in some patients.
Nutritional treatment
Need for enteral or parenteral nutrition
Patients with an HOS may be malnourished if their gut length is short (table 2). Most patients with less than 75 cm of jejunum remaining need long-term parenteral nutrition; most in the range 75–100 cm need parenteral saline (sometimes with added magnesium) (table 2) but manage to maintain nutritional status with an enteral regimen even though they may only absorb about 50%–60% of their oral energy intake.
All patients wish to eat food so as to feel normal and to maintain social relationships. In patients maintained on parenteral nutrition, an oral intake is detrimental as it increases jejunostomy losses. Patients taking an oral regimen need to consume more energy than a normal person to compensate for malabsorption. This malabsorption factor must be taken into account if giving oral/enteral feeds. Most patients can achieve this by eating more high-energy food. Oral sip feeds may be given in addition to food, preferably taken between meals and at bedtime. By these means, a patient may increase energy intake by at least 1000 kcal/day. If oral sip feeds during the day fail to achieve weight gain or maintain nutrition, a nasogastric or gastrostomy tube may be inserted and a feed given at night so that the short residual length of intestine is used at a time when it is usually inactive.
Once weight is regained, the daily energy requirement may decrease so that a nocturnal feed can be reduced or stopped and sip-feeds during the day may become adequate. Only if these measures fail and the patient continues to lose weight, or fails to regain lost weight, is parenteral nutrition given.
Oral/enteral nutrition/food
Patients with a jejunostomy absorb a constant though reduced proportion of the nitrogen, energy and fat from their diet.28 93 94 Increasing fat in the diet raises fat excretion but does not usually increase stomal output, nor make the output offensive.28 93 94
Increasing the fat in the diet does (as expected) increase the loss of the divalent cations (Mg and Ca),28 but this is not always the case.93 A diet of small molecules (eg, an elemental diet) is not advised as it causes a feed to be hyperosmolar91 and usually contains little sodium, so increasing the losses of water and sodium from the stoma. A peptide feed still has the problem of a relatively high osmolality, and thus can increase stomal output but nitrogen absorption is increased.95 Little advantage comes from taking a diet of water-soluble medium-chain triglycerides in place of normal fat.96 The addition of glutamine, 15 g, to a litre of rehydration solution in patients with a jejunostomy resulted in no additional benefit in terms of water or sodium absorption.97 The fibre content of the diet plays only a minor role in determining jejunal output93 but if reduced will reduce episodes of HOS if there are adhesions and so is often advised.
Thus jejunostomy patients need a large total oral energy intake of a polymeric, iso-osmolar (300 mOsm/kg) diet that is relatively high in fat with added salt (sodium concentration 100 mmol/L). The volume of the stomal output may become so high with a normal diet or with extra feeding that it is a major social disability. If this is the case, parenteral feeding may be needed to enable oral intake to be reduced.
Predicting drug absorption
Many drugs are incompletely absorbed by patients with a short bowel and may be needed in much higher amounts than usual (eg, thyroxine, warfarin and digoxin)98 or may need to be given intravenously. An attempt to predict the absorption of a medication in patients with a short bowel can be made by using the time to peak levels and the biopharmaceutical classification of drugs. A drug with a short time to peak plasma levels is likely to be absorbed in the upper gut and so be absorbed in patients with a short bowel; this will not be the case if there is a long time to peak plasma levels. The biopharmaceutical classification of drugs is based on drug aqueous solubility and intestinal permeability.99 100 A drug with high solubility and high permeability (class 1) is likely to be well absorbed in a short length of gut but this will not be the case for one with poor solubility and permeability.
Changes in jejunostomy output with time
Patients with a normal terminal ileostomy experience a decrease in stomal output from about day 5 to 16 weeks after its formation.101 Hill et al showed, in patients with an ‘ileostomy’ following an ileal resection, that there was no decrease in ileostomy water, sodium and potassium losses from 11 days after the resection to 6 months.102 There is no structural change in distal duodenal mucosa in patients with an established jejunostomy.103 Thus there is no evidence for any structural or functional adaptive changes occurring in patients with a jejunostomy. The fluid and nutrients needed change very little with time and are likely to be the same for as long as the jejunostomy remains.25
Surgical options
If there is small or large bowel out of circuit then if this is brought back into continuity absorption may improve and problems of an HOS resolved. This is well shown when patients after a mesenteric infarction have continuity restored and 77% were able to stop parenteral nutrition within 5 years.104 The reversal of a 10 cm segment of small bowel has been reported to be successful in increasing absorption in some patients with a short bowel with few complications reported.105 The Serial Transverse Enteroplasty Procedure (STEP) is being performed if the small bowel is sufficiently dilated and has mainly been performed in children with a colon in continuity.106 Rarely small bowel transplantation can be required mainly for complications related to intestinal failure/parenteral nutrition (eg, liver disease or failing venous access).
Patient support
Patients with a stoma and a high output may need psychosocial support and the help of local stoma nurses and patient support groups (eg, ileostomy association or PINNT in the UK) and advice leaflets.
Monitoring
Accurate daily measurements of body weight, fluid balance (especially stomal effluent) and postural blood pressure are important. Serum electrolyte (creatinine, potassium and magnesium) and urinary sodium estimation may be done every 1–3 days initially but once or twice weekly when the patient is stable in hospital. The aims are to maintain hydration and body weight and a daily urine volume of at least 800 mL with a sodium concentration greater than 20 mmol/L. At home, if stable, measurements of weight, urine sodium concentration and serum magnesium are done every 3 months.
Footnotes
Collaborators: None.
Contributors: JMDN has written all of this article based upon clinical experience, research and literature reviews.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: Chairman of the Adjudication committee for a phase III multicentre, double blind, randomised, placebo-controlled, parallel-group, efficacy and safety trial of Apraglutide (VectivBio AG).
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
References
- 1. Nightingale JMD, Lennard-Jones JE, Walker ER, et al. Jejunal efflux in short bowel syndrome. The Lancet 1990;336:765–8. 10.1016/0140-6736(90)93238-K [DOI] [PubMed] [Google Scholar]
- 2. Baker ML, Williams RN, Nightingale JMD. Causes and management of a high-output stoma. Colorectal Disease 2011;13:191–7. 10.1111/j.1463-1318.2009.02107.x [DOI] [PubMed] [Google Scholar]
- 3. Arenas Villafranca JJ, López-Rodríguez C, Abilés J, et al. Protocol for the detection and nutritional management of high-output stomas. Nutr J 2015;14:1. 10.1186/s12937-015-0034-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Takeda M, Takahashi H, Haraguchi N, et al. Factors predictive of high-output ileostomy: a retrospective single-center comparative study. Surg Today 2019;49:482–7. 10.1007/s00595-018-1756-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hara Y, Miura T, Sakamoto Y, et al. Organ/space infection is a common cause of high output stoma and outlet obstruction in diverting ileostomy. BMC Surg 2020;20:83. 10.1186/s12893-020-00734-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kennedy HJ, Al-Dujaili EA, Edwards CR, et al. Water and electrolyte balance in subjects with a permanent ileostomy. Gut 1983;24:702–5. 10.1136/gut.24.8.702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Newton CR, Drury P, Gonvers JJ. Incidence and treatment of sodium depletion in ileostomists. Scan J Gastroenterol 1982;74:159–60. [PubMed] [Google Scholar]
- 8. Fujino S, Miyoshi N, Ohue M, et al. Prediction model and treatment of high-output ileostomy in colorectal cancer surgery. Mol Clin Oncol 2017;7:468–72. 10.3892/mco.2017.1336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Williams RN, Hemingway D, Miller AS. Enteral Clostridium difficile, an emerging cause for high-output ileostomy. J Clin Pathol 2009;62:951–3. 10.1136/jcp.2008.062901 [DOI] [PubMed] [Google Scholar]
- 10. Nightingale JMD, Spiller RC. Normal intestinal anatomy and physiology. In: Failure I, Nightingale JMD, eds. Greenwich medical media limited, 2001: 15–36. [Google Scholar]
- 11. Teitelbaum EN, Vaziri K, Zettervall S, et al. Intraoperative small bowel length measurements and analysis of demographic predictors of increased length. Clin Anat 2013;26:27–32. 10.1002/ca.22238 [DOI] [PubMed] [Google Scholar]
- 12. Tacchino RM. Bowel length: measurement, predictors, and impact on bariatric and metabolic surgery. Surg Obes Relat Dis 2015;11:328–34. 10.1016/j.soard.2014.09.016 [DOI] [PubMed] [Google Scholar]
- 13. Nightingale JMD, Lennard-Jones JE. Adult patients with a short bowel due to Crohn??s disease often start with a short normal bowel. Eur J Gastroenterol Hepatol 1995;7:989–91. 10.1097/00042737-199510000-00015 [DOI] [PubMed] [Google Scholar]
- 14. Nightingale JM. The Sir David Cuthbertson medal lecture. clinical problems of a short bowel and their treatment. Proc Nutr Soc 1994;53:373–91. 10.1079/pns19940043 [DOI] [PubMed] [Google Scholar]
- 15. Nightingale JMD, Woodward J. And small bowel/Nutrition Committee of Bsg. guidelines for the management of patients with a short bowel. Gut 2006;55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Newton CR, Gonvers JJ, McIntyre PB, et al. Effect of different drinks on fluid and electrolyte losses from a jejunostomy. J R Soc Med 1985;78:27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Griffin GE, Fagan EF, Hodgson HJ, et al. Enteral therapy in the management of massive gut resection complicated by chronic fluid and electrolyte depletion. Dig Dis Sci 1982;27:902–8. 10.1007/BF01316574 [DOI] [PubMed] [Google Scholar]
- 18. Nightingale JM, Lennard-Jones JE, Walker ER, et al. Oral salt supplements to compensate for jejunostomy losses: comparison of sodium chloride capsules, glucose electrolyte solution, and glucose polymer electrolyte solution. Gut 1992;33:759–61. 10.1136/gut.33.6.759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rodrigues CA, Lennard-Jones JE, Thompson DG, et al. What is the ideal sodium concentration of oral rehydration solutions (ORS) for short bowel patients? Clin Sci 1988;74:69. 10.1042/cs074069Pa [DOI] [Google Scholar]
- 20. Buxton B. Small bowel resection and gastric acid hypersecretion. Gut 1974;15:229–38. 10.1136/gut.15.3.229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nightingale JM, Kamm MA, van der Sijp JR, et al. Gastrointestinal hormones in short bowel syndrome. Peptide YY may be the ‘colonic brake’ to gastric emptying. Gut 1996;39:267–72. 10.1136/gut.39.2.267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Windsor CWO, Fejfar J, Woodward DAK. Gastric secretion after massive small bowel resection. Gut 1969;10:779–86. 10.1136/gut.10.10.779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nightingale JM, Kamm MA, van der Sijp JR, et al. Disturbed gastric emptying in the short bowel syndrome. Evidence for a ‘colonic brake’. Gut 1993;34:1171–6. 10.1136/gut.34.9.1171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jeppesen PB, Hartmann B, Hansen BS, et al. Impaired meal stimulated glucagon-like peptide 2 response in ileal resected short bowel patients with intestinal failure. Gut 1999;45:559–63. 10.1136/gut.45.4.559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nightingale JM, Lennard-Jones JE, Gertner DJ, et al. Colonic preservation reduces need for parenteral therapy, increases incidence of renal stones, but does not change high prevalence of gall stones in patients with a short bowel. Gut 1992;33:1493–7. 10.1136/gut.33.11.1493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hanna S, Macintyre I. The influence of aldosterone on magnesium metabolism. The Lancet 1960;276:348–50. 10.1016/S0140-6736(60)91487-2 [DOI] [PubMed] [Google Scholar]
- 27. Horton R, Biglieri EG. Effect of aldosterone on the metabolism of magnesium. J Clin Endocrinol Metab 1962;22:1187–92. [DOI] [PubMed] [Google Scholar]
- 28. Ovesen L, Chu R, Howard L. The influence of dietary fat on jejunostomy output in patients with severe short bowel syndrome. Am J Clin Nutr 1983;38:270–7. 10.1093/ajcn/38.2.270 [DOI] [PubMed] [Google Scholar]
- 29. Hessov I, Andersson H, Isaksson B. Effects of a low-fat diet on mineral absorption in small-bowel disease. Scan J Gastroenterol 1983;18:551–4. 10.3109/00365528309181636 [DOI] [PubMed] [Google Scholar]
- 30. Pisani LF, Filippi E, Vavassori S, et al. Effect of proton pump inhibitors on magnesium balance: is there a link to cardiovascular risk? Magnesium Research 2016;29:1–10. 10.1684/mrh.2016.0397 [DOI] [PubMed] [Google Scholar]
- 31. Richette P, Ayoub G, Lahalle S, et al. Hypomagnesemia associated with chondrocalcinosis: a cross-sectional study. Arthritis Rheum 2007;57:1496–501. 10.1002/art.23106 [DOI] [PubMed] [Google Scholar]
- 32. Fragkos KC, Forbes A. Citrulline as a marker of intestinal function and absorption in clinical settings: a systematic review and meta-analysis. United European Gastroenterol J 2018;6:181–91. 10.1177/2050640617737632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nightingale JMD, Bartram CI, Lennard-Jones JE. Length of residual small bowel after partial resection: correlation between radiographic and surgical measurements. Gastrointest Radiol 1991;16:305–6. 10.1007/BF01887374 [DOI] [PubMed] [Google Scholar]
- 34. Ladefoged K, ØLgaard K. Fluid and electrolyte absorption and renin-angiotensin-aldosterone axis in patients with severe short-bowel syndrome. Scand J Gastroenterol 1979;14:729–35. 10.3109/00365527909181945 [DOI] [PubMed] [Google Scholar]
- 35. Ladefoged K, Ølgaard K. Sodium homeostasis after small-bowel resection. Scand J Gastroenterol 1985;20:361–9. 10.3109/00365528509091665 [DOI] [PubMed] [Google Scholar]
- 36. Woolf GM, Miller C, Kurian R. Nutritional absorption in short bowel syndrome. evaluation of fluid, calorie and divalent cation requirements. Dig Dis Sci 1987;32:8–15. [DOI] [PubMed] [Google Scholar]
- 37. Olsen WA, Ingelfinger FJ. The role of sodium in intestinal glucose absorption in man. J Clin Invest 1968;47:1133–42. 10.1172/JCI105802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sladen GE, Dawson AM. Interrelationships between the absorptions of glucose, sodium and water by the normal human jejunum. Clin Sci 1969;36:119–32. [PubMed] [Google Scholar]
- 39. Fordtran JS. Stimulation of active and passive sodium absorption by sugars in the human jejunum. J Clin Invest 1975;55:728–37. 10.1172/JCI107983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Avery ME, Snyder JD. Oral therapy for acute diarrhoea. The underused simple solution. N Engl J Med 1990;323:891–4. [DOI] [PubMed] [Google Scholar]
- 41. Culkin A, Gabe SM, Nightingale JM. PP070-SUN: outstanding Abstract: a randomised controlled crossover trial to investigate the efficacy of a new oral rehydration solution for patients with a high output stoma. Clin Nutr Suppl 2014;33:S45. 10.1016/S0261-5614(14)50112-4 [DOI] [Google Scholar]
- 42. Beaugerie L, Cosnes J, Verwaerde F, et al. Isotonic high-sodium oral rehydration solution for increasing sodium absorption in patients with short-bowel syndrome. Am J Clin Nutr 1991;53:769–72. 10.1093/ajcn/53.3.769 [DOI] [PubMed] [Google Scholar]
- 43. Newton CR. Effect of codeine phosphate, Lomotil, and Isogel on ileostomy function. Gut 1978;19:377–83. 10.1136/gut.19.5.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. King RF, Norton T, Hill GL. A double-blind crossover study of the effect of loperamide hydrochloride and codeine phosphate on ileostomy output. Aust N Z J Surg 1982;52:121–4. 10.1111/j.1445-2197.1982.tb06083.x [DOI] [PubMed] [Google Scholar]
- 45. Tytgat GN, Huibregtse K, Dagevos J, et al. Effect of loperamide on fecal output and composition in well-established ileostomy and ileorectal anastomosis. Am J Dig Dis 1977;22:669–76. 10.1007/BF01078345 [DOI] [PubMed] [Google Scholar]
- 46. Remington M, Fleming CR, Malagelada JR. Inhibition of postprandial pancreatic and biliary secretion by loperamide in patients with short bowel syndrome. Gut 1982;23:98–101. 10.1136/gut.23.2.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Tytgat GN, Huibregtse K. Loperamide and ileostomy output--placebo-controled double-blind crossover study. Br Med J 1975;2:667–8. 10.1136/bmj.2.5972.667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kristensen K, Qvist N. The acute effect of loperamide on ileostomy output: a randomized, double-blinded, placebo-controlled, crossover study. Basic Clin Pharmacol Toxicol 2017;121:493–8. 10.1111/bcpt.12830 [DOI] [PubMed] [Google Scholar]
- 49. Nightingale JMD, Lennard-Jones JE, Walker ER. A patient with jejunostomy liberated from home intravenous therapy after 14 years; contribution of balance studies. Clinical Nutrition 1992;11:101–5. 10.1016/0261-5614(92)90019-M [DOI] [PubMed] [Google Scholar]
- 50. O'Brien JD, Thompson DG, McIntyre A, et al. Effect of codeine and loperamide on upper intestinal transit and absorption in normal subjects and patients with postvagotomy diarrhoea. Gut 1988;29:312–8. 10.1136/gut.29.3.312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Mackowski A, Chen H-K, Levitt M. Successful management of chronic high-output ileostomy with high dose loperamide. BMJ Case Rep 2015;2015. 10.1136/bcr-2015-209411. [Epub ahead of print: 22 Apr 2015]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Meade U. the BIFA Committee. Nightingale J. British intestinal failure alliance (BIFA) position statement the use of high dose loperamide in patients with intestinal failure, 2018. Available: https://www.bapen.org.uk/pdfs/bifa/position-statements/use-of-loperamide-in-patients-with-intestinal-failure.pdf
- 53. Rodrigues CA, Lennard-Jones JE, Walker ER. The effects of octreotide, soy polysaccharide, codeine and loperamide on nutrient, fluid and electrolyte absorption in the short-bowel syndrome. Aliment Pharmacol Ther 1989;3:159–69. 10.1111/j.1365-2036.1989.tb00202.x [DOI] [PubMed] [Google Scholar]
- 54. Aly A, Bárány F, Kollberg B, et al. Effect of an H2-Receptor Blocking Agent on Diarrhoeas after Extensive Small Bowel Resection in Crohn’s Disease. Acta Med Scand 1980;207:119–22. 10.1111/j.0954-6820.1980.tb09688.x [DOI] [PubMed] [Google Scholar]
- 55. Jacobsen O, Ladefoged K, Stage JG, et al. Effects of cimetidine on jejunostomy effluents in patients with severe short-bowel syndrome. Scand J Gastroenterol 1986;21:824–8. 10.3109/00365528609011125 [DOI] [PubMed] [Google Scholar]
- 56. Nightingale JMD, Walker ER, Farthing MJG, et al. Effect of omeprazole on intestinal output in the short bowel syndrome. Aliment Pharmacol Ther 1991;5:405–12. [DOI] [PubMed] [Google Scholar]
- 57. Jeppesen PB, Staun M, Tjellesen L, et al. Effect of intravenous ranitidine and omeprazole on intestinal absorption of water, sodium, and macronutrients in patients with intestinal resection. Gut 1998;43:763–9. 10.1136/gut.43.6.763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. NICE . British National formulary (BNF). Available: https://bnf.nice.org.uk/drug-class/proton-pump-inhibitors-2.html#sideEffects
- 59. Dharmsathaphorn K, Gorelick FS, Sherwin RS, et al. Somatostatin decreases diarrhea in patients with the short-bowel syndrome. J Clin Gastroenterol 1982;4:521–4. 10.1097/00004836-198212000-00008 [DOI] [PubMed] [Google Scholar]
- 60. Cooper JC, Williams NS, King RF, et al. Effects of a long-acting somatostatin analogue in patients with severe ileostomy diarrhoea. Br J Surg 1986;73:128–31. 10.1002/bjs.1800730219 [DOI] [PubMed] [Google Scholar]
- 61. Kusuhara K, Kusunoki M, Okamoto T, et al. Reduction of the effluent volume in high-output ileostomy patients by a somatostatin analogue, SMS 201-995. Int J Colorectal Dis 1992;7:202–5. 10.1007/BF00341221 [DOI] [PubMed] [Google Scholar]
- 62. Shaffer JL, O’Hanrahan T, Rowntree S. Does somatostatin analogue (201-995) reduce high output stoma effluent? A controlled trial. Gut 1988;29:A1432–3. [Google Scholar]
- 63. Nightingale JM, Walker ER, Burnham WR, et al. Octreotide (a somatostatin analogue) improves the quality of life in some patients with a short intestine. Aliment Pharmacol Ther 1989;3:367–73. 10.1111/j.1365-2036.1989.tb00223.x [DOI] [PubMed] [Google Scholar]
- 64. Ladefoged K, Christensen KC, Hegnhoj J, et al. Effect of a long acting somatostatin analogue SMS 201-995 on jejunostomy effluents in patients with severe short bowel syndrome. Gut 1989;30:943–9. 10.1136/gut.30.7.943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Lémann M, de Montigny S, Mahé S. Effect of octreotide on water and electrolytes losses, nutrient absorption and transit in short bowel syndrome. Eur J Gastroenterol Hepatol 1993;5:817–22. [Google Scholar]
- 66. O'Keefe SJ, Peterson ME, Fleming CR. Octreotide as an adjunct to home parenteral nutrition in the management of permanent end-jejunostomy syndrome. JPEN J Parenter Enteral Nutr 1994;18:26–34. 10.1177/014860719401800102 [DOI] [PubMed] [Google Scholar]
- 67. Dowling RH, Hussaini SH, Murphy GM, et al. Gallstones during octreotide therapy. Digestion 1993;54:107–20. 10.1159/000201088 [DOI] [PubMed] [Google Scholar]
- 68. Nehra V, Camilleri M, Burton D, et al. An open trial of octreotide long-acting release in the management of short bowel syndrome. Am J Gastroenterol 2001;96:1494–8. 10.1111/j.1572-0241.2001.03803.x [DOI] [PubMed] [Google Scholar]
- 69. Mesli Y, Holterbach L, Delhorme J-B. Is lanreotide really useful in high output stoma? comparison between lanreotide to conventional antidiarrheal treatment alone. J Invest Surg 2020;4:1–5. [DOI] [PubMed] [Google Scholar]
- 70. Wright HK, Cleveland JC, Tilson MD, et al. Morphology and absorptive capacity of the ileum after ileostomy in man. Am J Surg 1969;117:242–5. 10.1016/0002-9610(69)90310-9 [DOI] [PubMed] [Google Scholar]
- 71. Ladas SD, Isaacs PE, Murphy GM, et al. Fasting and postprandial ileal function in adapted ileostomates and normal subjects. Gut 1986;27:906–12. 10.1136/gut.27.8.906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Goulston K, Harrison DD, Skyring AP. Effect of mineralocorticoids on the sodium/potassium ratio of human ileostomy fluid. Lancet 1963;282:541–2. 10.1016/S0140-6736(63)92640-0 [DOI] [PubMed] [Google Scholar]
- 73. Levitan R, Goulston K. Water and electrolyte content of human ileostomy fluid after d-aldosterone administration. Gastroenterology 1967;52:510–2. 10.1016/S0016-5085(67)80178-1 [DOI] [PubMed] [Google Scholar]
- 74. Kramer P, Levitan R. Effect of 9-α-Fluorohydrocortisone on the ileal excreta of Ileostomized subjects. Gastroenterology 1972;62:235–41. 10.1016/S0016-5085(72)80174-4 [DOI] [PubMed] [Google Scholar]
- 75. Feretis CB, Vyssoulis GP, Pararas BN. The influence of corticosteroids on ileostomy discharge of patients operated for ulcerative colitis. Am Surg 1984;50:433–6. [PubMed] [Google Scholar]
- 76. Sandle GI, Keir MJ, Record CO. The effect of hydrocortisone on the transport of water, sodium, and glucose in the jejunum. perfusion studies in normal subjects and patients with coeliac disease. Scand J Gastroenterol 1981;16:667–71. 10.3109/00365528109182028 [DOI] [PubMed] [Google Scholar]
- 77. Sutters M, Carmichael DJ, Unwin RJ, et al. ‘Low sodium’ diuresis and ileal loss in patients with ileostomies: effect of desmopressin. Gut 1991;32:649–53. 10.1136/gut.32.6.649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Gruy-Kapral C, Little KH, Fordtran JS, et al. Conjugated bile acid replacement therapy for short-bowel syndrome. Gastroenterology 1999;116:15–21. 10.1016/S0016-5085(99)70223-4 [DOI] [PubMed] [Google Scholar]
- 79. Heydorn S, Jeppesen PB M. Bile acid replacement therapy with cholylsarcosine for short bowel syndrome. Scan J Gastroenterol 1999;34:818–23. [DOI] [PubMed] [Google Scholar]
- 80. Buchman AL, Fryer J, Wallin A, et al. Clonidine reduces diarrhea and sodium loss in patients with proximal jejunostomy: a controlled study. JPEN J Parenter Enteral Nutr 2006;30:487–91. 10.1177/0148607106030006487 [DOI] [PubMed] [Google Scholar]
- 81. Nightingale JM, Kamm MA, van der Sijp JR, et al. Gastrointestinal hormones in short bowel syndrome. PYY may be the ‘colonic brake’ to gastric emptying. Gut 1996;39:267–72. 10.1136/gut.39.2.267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Jeppesen PB, Hartmann B, Hansen BS, et al. Impaired meal stimulated glucagon-like peptide 2 response in ileal resected short bowel patients with intestinal failure. Gut 1999;45:559–63. 10.1136/gut.45.4.559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Oke S, Nightingale J, Palle Jeppesen and the BIFA committee . British intestinal failure alliance (BIFA) position statement. Use of peptide growth factors for adult patients with intestinal failure, 2018. Available: www.bapen.org.uk/pdfs/bifa/position-statements/use-of-peptide-growth-factors-for-adult-patients-with-intestinal-failure.pdf
- 84. Jeppesen PB, Gilroy R, Pertkiewicz M, et al. Randomised placebo-controlled trial of teduglutide in reducing parenteral nutrition and/or intravenous fluid requirements in patients with short bowel syndrome. Gut 2011;60:902–14. 10.1136/gut.2010.218271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Jeppesen PB, Pertkiewicz M, Messing B, et al. Teduglutide reduces need for parenteral support among patients with short bowel syndrome with intestinal failure. Gastroenterology 2012;143:1473–81. 10.1053/j.gastro.2012.09.007 [DOI] [PubMed] [Google Scholar]
- 86. Schwartz LK, O'Keefe SJD, Fujioka K, et al. Long-Term Teduglutide for the treatment of patients with intestinal failure associated with short bowel syndrome. Clin Transl Gastroenterol 2016;7:e142. 10.1038/ctg.2015.69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Hvistendahl M, Brandt CF, Tribler S. Effect of liraglutide treatment on jejunostomy output in patients with short bowel syndrome: an open-label pilot study. J Parenter Enteral Nutr 2018;42:112–21. [DOI] [PubMed] [Google Scholar]
- 88. Kaufman SS, Loseke CA, Anderson JB, et al. Magnesium acetate vs. magnesium gluconate supplementation in short bowel syndrome. J Pediatr Gastroenterol Nutr 1993;16:104–5. 10.1097/00005176-199301000-00025 [DOI] [PubMed] [Google Scholar]
- 89. Schuette SA, Lashner BA, Janghorbani M. Bioavailability of magnesium diglycinate vs magnesium oxide in patients with ileal resection. JPEN J Parenter Enteral Nutr 1994;18:430–5. 10.1177/0148607194018005430 [DOI] [PubMed] [Google Scholar]
- 90. Kass L, Rosanoff A, Tanner A, et al. Effect of transdermal magnesium cream on serum and urinary magnesium levels in humans: a pilot study. PLoS One 2017;12:e0174817. 10.1371/journal.pone.0174817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Selby PL, Peacock M, Bambach CP. Hypomagnesaemia after small bowel resection: treatment with 1 α-hydroxylated vitamin D metabolites. Br J Surg 1984;71:334–7. 10.1002/bjs.1800710504 [DOI] [PubMed] [Google Scholar]
- 92. Fukumoto S, Matsumoto T, Tanaka Y, et al. Renal Magnesium Wasting in a Patient with Short Bowel Syndrome with Magnesium Deficiency: Effect of 1 α -Hydroxyvitamin D Treatment*. The Journal of Metab 1987;65:1301–4. 10.1210/jcem-65-6-1301 [DOI] [PubMed] [Google Scholar]
- 93. McIntyre PB, Fitchew M, Lennard-Jones JE. Patients with a high jejunostomy do not need a special diet. Gastroenterology 1986;91:25–33. 10.1016/0016-5085(86)90434-8 [DOI] [PubMed] [Google Scholar]
- 94. Nordgaard I, Hansen BS, Mortensen PB. Colon as a digestive organ in patients with short bowel. Lancet 1994;343:373–6. 10.1016/S0140-6736(94)91220-3 [DOI] [PubMed] [Google Scholar]
- 95. Cosnes J, Evard D, Beaugerie L, et al. Improvement in protein absorption with a small-peptide-based diet in patients with high jejunostomy. Nutrition 1992;8:406–11. [PubMed] [Google Scholar]
- 96. Jeppesen PB, Mortensen PB. The influence of a preserved colon on the absorption of medium chain fat in patients with small bowel resection. Gut 1998;43:478–83. 10.1136/gut.43.4.478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Beaugerie L, Carbonnel F, Hecketsweiler B, et al. Effects of an isotonic oral rehydration solution, enriched with glutamine, on fluid and sodium absorption in patients with short-bowel syndrome. Aliment Pharmacol Ther 1997;11:741–6. 10.1046/j.1365-2036.1997.t01-1-00201.x [DOI] [PubMed] [Google Scholar]
- 98. Ehrenpreis ED, Guerriero S, Nogueras JJ, et al. Malabsorption of digoxin tablets, gel caps, and elixir in a patient with an end jejunostomy. Ann Pharmacother 1994;28:1239–40. 10.1177/106002809402801104 [DOI] [PubMed] [Google Scholar]
- 99. Amidon GL, Lennernäs H, Shah VP, et al. A theoretical basis for a biopharmaceutic drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm Res 1995;12:413–20. 10.1023/A:1016212804288 [DOI] [PubMed] [Google Scholar]
- 100. Lindenberg M, Kopp S, Dressman JB. Classification of orally administered drugs on the world Health organization model list of essential medicines according to the biopharmaceutics classification system. Eur J Pharm Biopharm 2004;58:265–78. 10.1016/j.ejpb.2004.03.001 [DOI] [PubMed] [Google Scholar]
- 101. Crawford N, Brooke BN. Ileostomy chemistry. Lancet 1957;1:864–7. [DOI] [PubMed] [Google Scholar]
- 102. Hill GL, Mair WS, Goligher JC. Impairment of 'ileostomy adaptation' in patients after ileal resection. Gut 1974;15:982–7. 10.1136/gut.15.12.982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. O'Keefe SJ, Haymond MW, Bennet WM, et al. Long-Acting somatostatin analogue therapy and protein metabolism in patients with jejunostomies. Gastroenterology 1994;107:379–88. 10.1016/0016-5085(94)90162-7 [DOI] [PubMed] [Google Scholar]
- 104. Adaba F, Rajendran A, Patel A, et al. Mesenteric infarction: clinical outcomes after restoration of bowel continuity. Ann Surg 2015;262:1059–64. 10.1097/SLA.0000000000001100 [DOI] [PubMed] [Google Scholar]
- 105. Beyer-Berjot L, Joly F, Maggiori L, et al. Segmental reversal of the small bowel can end permanent parenteral nutrition dependency: an experience of 38 adults with short bowel syndrome. Ann Surg 2012;256:739–44. discussion 744-5. 10.1097/SLA.0b013e31827387f5 [DOI] [PubMed] [Google Scholar]
- 106. Yannam GR, Sudan DL, Grant W, et al. Intestinal lengthening in adult patients with short bowel syndrome. J Gastrointest Surg 2010;14:1931–6. 10.1007/s11605-010-1291-y [DOI] [PubMed] [Google Scholar]