Abstract
Positive patient identification (PPID) is an integral step to ensure the correct patient identity prior to a healthcare delivery event. Following implementation of a new EHR in November 2017, Vanderbilt University Medical Center (VUMC) experienced frequent and inconsistent failure of barcode scanners which impacted the electronic PPID (ePPID) and blood verification processes. Following multiple iterations of troubleshooting, vendor engagement, and device upgrades, we developed a clinical decision support (CDS) tool as a visual reminder to perform ePPID. If ePPID was initially bypassed, the clinician received a passive alert which remained visible throughout the procedure or until ePPID was completed successfully. We conducted a retrospective observational study using an interrupted time series analysis and analysis of variance pre-and post-CDS intervention. Following CDS intervention, we observed an immediate 20.8% increase in successful ePPID (p < 0.001). The mean success rate of ePPID attempts increased from 62.0% pre-intervention to 94.4% post-intervention (p < 0.001). There were 108 providers who had less than 80.0% success in the six-months prior to CDS intervention, of whom all improved to an average of 95.9% success. Our CDS approach highlights the utility of non-interruptive but continually visible alerts to improve patient safety workflows. By making errors clearly visible to users and their peers, performance improved to only 5.6% of alerts bypassed.
Keywords: Clinical Decision Support, Patient Safety, Electronic Health Records, Implementation Science
Introduction
Preventable medical errors are estimated to be the third leading cause of death in the United States [1]. Patient and specimen misidentification has garnered considerable evidence as a particular source of preventable harm to patients, including medication errors, diagnostic errors, incorrect procedures, and death [2–4]. Positive patient identification (PPID) is an approach to avoid these misidentification errors by ensuring that healthcare delivery events are provided to the correct patient and the correct time using the correct means of administration [5]. Ensuring accurate PPID has been recognized as an approach to improve the quality and safety patient care [6, 7]. Consistent and accurate PPID using two different patient identifiers is a Joint Commission National Patient Safety Goal [8].
Electronic PPID (ePPID) technology, often deployed as a barcode scanning system, is widely operational across healthcare environments. These systems provide integration with the electronic health record (EHR) system to verify the correct patient, their medical history, and their therapeutic regimens. The barcode scanning-based ePPID system consists of patient wristbands with a printed barcode that contains identifying information. Prior to a healthcare delivery event, the clinician confirms a patient’s identity by scanning the wristband barcode and scanning a separate barcode on a specimen, medication, or the EHR screen to verify the correct patient and correct therapy. This technology has greatly improved the PPID workflow, with extensive research highlighting its improvements to patient safety across clinical environments [9, 10].
Vanderbilt University Medical Center (VUMC) in November 2017 migrated from a locally-developed EHR to the Epic system. VUMC implemented barcode scanning of patient wristbands to enable ePPID. Following the EHR migration, VUMC experienced frequent and inconsistent barcode scanning failures across perioperative and other procedural areas, which impacted electronic PPID and blood verification processes. As a result, some providers frequently bypassed ePPID documentation and manually selected patients rather than performing the necessary troubleshooting steps, which led to patient safety concerns. Following numerous problem management approaches, we developed a passive, conditionally visible, clinical decision support (CDS) tool to encourage accurate ePPID following initial documentation bypass. We highlight the steps by which we designed and developed the CDS tool and present statistics to describe its efficacy in improving ePPID.
Methods
The work was conducted as quality improvement and was exempt from institutional review board review.
Study site
The Vanderbilt University Medical Center is a large academic medical center located in middle Tennessee. VUMC includes the 864-bed Vanderbilt University Hospital, which performs nearly 40,000 yearly surgical procedures [11]. The perioperative environment supports both anesthesiology and surgery trainees. The anesthesiology services are staffed by faculty members, residents, certified registered nurse anesthetists, and student nurse anesthetists. Barcode scanners are used by anesthesia providers to verify that the correct patient and correct patient chart are open prior to delivering the anesthetic. Following a patient’s entry into the operating room and initiation of an anesthesia event, the patient and encounter identification are scanned from the patient’s armband. If the appropriate information is not scanned, there is a hard stop until an override reason is entered.
Barcode scanner troubleshooting and problem management
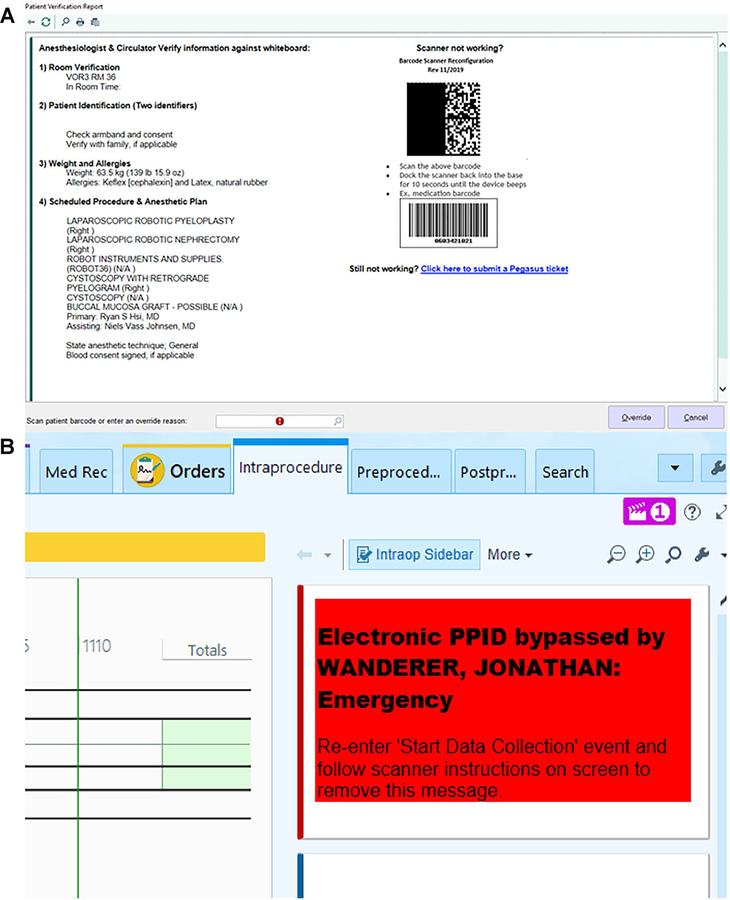
Beginning April 2019, VUMC began receiving a series of incident tickets related to barcode scanner issues. In subsequent months, Information Technology support and Periprocedural IT governance teams conducted a series of troubleshooting steps and applied device and firmware upgrades. After it was determined that the barcode scanners required frequent resetting, we added a barcode scanner configuration page and troubleshooting steps within the existing anesthesia workflow in the EHR to aid in reconfiguring disconnected scanners (Fig. 1a) and ultimate engaged the barcode scanner vendor. By October 2020, scanner issues remained prevalent causing limited success of ePPID, leading to the development of our CDS alert.
Fig. 1.
(a) Begin Anesthesia Page with Barcode Scanner Troubleshooting and (b) Passive CDS Alert for Bypassed ePPID. © Epic Systems Corporation
The timeline of key troubleshooting and problem management steps is included as supplementary material.
Passive clinical decision support alert
We developed a passive, conditionally visible, reminder to encourage clinicians to perform ePPID if that step had been bypassed (Fig. 1b). On the anesthesia data collection screen, the clinician was prompted to scan the patient’s armband for identity verification. This screen also contained a set of troubleshooting steps to quickly reconfigure and reconnect the scanning device in case of malfunction. If the provider chose to manually bypass a failed verification attempt rather than perform scanner troubleshooting and successfully document ePPID, the alert would appear on the right side of the EHR screen. The alert remained visible to the provider and their peers throughout the procedure or until the ePPID was completed. We rolled out the intervention across VUMC on October 7, 2020. The alert was active for all providers during anesthesia administration.
Alert efficacy evaluation
To assess the efficacy of our CDS approach, we conducted a retrospective observational study using autoregressive interrupted time series (ITS) analysis and analysis of variance (ANOVA) to test differences in perioperative ePPID success pre- and post-CDS intervention. For our institutional level comparison, we evaluated trends between October 1, 2019 and April 28, 2021. We assessed provider-level ePPID compliance between April 7, 2020 and April 7, 2021 corresponding to six-months before and after the CDS intervention was implemented in our EHR.
Results
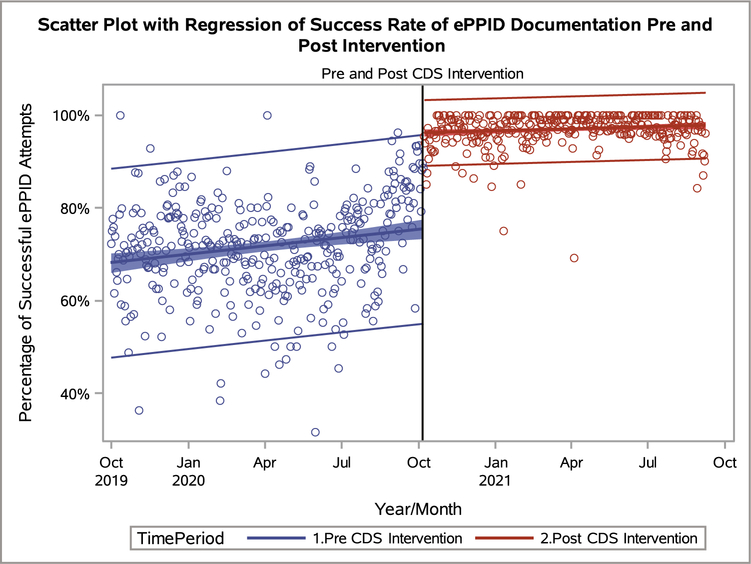
Between October 1, 2019 and April 28, 2021, there were 537 anesthesia providers who performed a total of 40,829 ePPID attempts, of which 30,459 (74.6%) were successful. As shown in Fig. 2, there was an immediate increase of 20.8% in the success rate of ePPID attempts following CDS implementation (p < 0.001). Prior to the CDS intervention, among all providers, 62.0% of attempts were successful. There were 28.2% of bypasses that were noted as scanner malfunction. Following implementation of the CDS alert, 94.4% of all attempts were successful and 3.1% of bypasses were due to scanner malfunction. There were 221 (90.9%) providers who maintained or improved their ePPID success in the six-months following CDS intervention. 108 of these providers had less than 80.0% successful attempts in the six-months prior to CDS intervention, of whom all improved to an average of 95.9% success in the following six-months.
Fig. 2.
Daily ePPID Success Pre- and Post-CDS Intervention. Each point represents the percentage of successful ePPID attempts
Discussion
Our CDS initiative to improve ePPID documentation highlights the utility of non-interruptive but continually visible alerts in improving clinician compliance to key safety workflows. Prior to our CDS intervention, the patient verification interface in the EHR required manual override to bypass ePPID. Despite troubleshooting steps presented on the verification interface, only 62.0% of attempts were completed successfully. Following CDS implementation, ePPID verification improved to 94.4% success. There have been numerous prior approaches to utilize CDS to improve compliance to safety workflows, but these alerts are often interruptive in nature and require a hard-stop intervention before the clinician can continue their healthcare delivery [12]. These active alerts are integral to intervening in events that can cause immediate harm, but lead to alert fatigue when used too frequently or in non-urgent situations [13, 14]. Our results highlight the opportunity to apply passive alerts that encourage behavior change during non-critical events without directly inhibiting existing workflow.
The non-interruptive approach to our clinical decision support was enabled by an alert that was always visible to the clinician and their peers in the respective operating room until ePPID was performed successfully. In developing the alert, we hypothesized that incorporating an element of peer visibility to failed safety workflows would encourage clinicians to self-correct the initially unsuccessful process. By making these errors clearly visible to users and their peers, only 3.1% of alerts were bypassed due to scanner malfunction. Further, providers who had low rates of ePPID documentation prior to CDS intervention had greatly improved post-intervention performance. Prior work has highlighted peer influence within clinical environments as a significant contributor to behavior change [15]. The marked improvement in ePPID success immediately following CDS intervention and in the months thereafter suggest that our non-interruptive approach was effective in improving potentially unsafe behavior.
It is important to consider the results from this work in light of several key limitations. We conducted this work at a single academic medical center. Our CDS intervention was developed by a team of trained clinicians with substantial informatics background, EHR builders, and Health Information Technology staff, but we did not formal evaluate usability prior to implementation. However, the alert was developed in consideration of Epic standards and current CDS literature and implemented such that it did not directly interrupt existing workflow. Finally, it is important to recognize that our CDS approach was developed to improve clinician behavior, but it is not intended as a replacement to ensuring operational hardware and software solutions. Nonetheless, our results suggest that our approach is effective in encouraging clinician involvement in troubleshooting minor technical problems when they inhibit key safety workflows.
Conclusions
Barcode scanner malfunctions inhibit key patient safety workflows. Coupled with iterative troubleshooting and device repair, our non-interruptive, conditionally-visible, CDS alert substantial improved the success of perioperative ePPID documentation at our institution.
Supplementary Material
Acknowledgements
GL and REF receive ongoing support from the National Heart, Lung, and Blood Institute (K23HL148640). BDS and AW were supported by R01AG062499 from the National Institute on Aging.
Footnotes
Competing Interests GL reports owning stock in Johnson and Johnson. All other authors have no competing interests to declare that are relevant to the content of this article.
This article is part of the Topical Collection on Clinical Systems
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s10916-022-01801-7.
Declarations
Ethics Approval This study was performed in compliance with the World Medical Association Declaration of Helsinki on Ethics Principles for Medical Research Involving Human Subjects. The work was conducted as quality improvement and was exempt from institutional review board review.
Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affliations.
References
- 1.Makary MA, Daniel M. Medical error-the third leading cause of death in the US. BMJ 2016;353:i2139–5. 10.1136/bmj.i2139. [DOI] [PubMed] [Google Scholar]
- 2.Snydman LK, Harubin B, Kumar S, Chen J, Lopez RE, Salem DN. Voluntary electronic reporting of laboratory errors: an analysis of 37,532 laboratory event reports from 30 health care organizations. American Journal of Medical Quality 2012;27:147–53. 10.1177/1062860611413567. [DOI] [PubMed] [Google Scholar]
- 3.Nakhleh RE, Idowu MO, Souers RJ, Meier FA, Bekeris LG. Mislabeling of cases, specimens, blocks, and slides: a college of american pathologists study of 136 institutions. Archives of Pathology & Laboratory Medicine 2011;135:969–74. 10.5858/2010-0726-cpr. [DOI] [PubMed] [Google Scholar]
- 4.Rubio EI, Hogan L. Time-Out: It’s Radiology’s Turn--Incidence of Wrong-Patient or Wrong-Study Errors. AJR American Journal of Roentgenology 2015;205:941–6. 10.2214/ajr.15.14720. [DOI] [PubMed] [Google Scholar]
- 5.Grissinger M The Five Rights. Pharmacy and Therapeutics 2010;10:542. [Google Scholar]
- 6.Seiden SC, Barach P. Wrong-side/wrong-site, wrong-procedure, and wrong-patient adverse events: Are they preventable? JAMA Surgery 2006. 10.1001/archsurg.141.9.931. [DOI] [PubMed] [Google Scholar]
- 7.Borchard A, Schwappach DLB, Barbir A, Bezzola P. A Systematic Review of the Effectiveness, Compliance, and Critical Factors for Implementation of Safety Checklists in Surgery. Annals of Surgery 2012;256:925–33. 10.1097/sla.0b013e3182682f27. [DOI] [PubMed] [Google Scholar]
- 8.Two Patient Identifiers - Understanding the Requirements 2020. https://www.jointcommission.org/standards/standard-faqs/homecare/national-patient-safety-goals-npsg/000001545/.
- 9.Riplinger L, Piera-Jiménez J, Dooling JP. Patient Identification Techniques - Approaches, Implications, and Findings. Yearbook of Medical Informatics 2020;29:81–6. 10.1055/s0040-1701984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Askeland RW, McGrane S, Levitt JS, Dane SK, Greene DL, VandeBerg JA, et al. Improving transfusion safety: implementation of a comprehensive computerized bar code–based tracking system for detecting and preventing errors. Transfusion 2008;48:1308–17. 10.1111/j.1537-2995.2008.01668.x. [DOI] [PubMed] [Google Scholar]
- 11.Vanderbilt University Medical Center Factsheet. 2019.
- 12.Co Z, Holmgren AJ, Classen DC, Newmark L, Seger DL, Danforth M, et al. The tradeofs between safety and alert fatigue: Data from a national evaluation of hospital medication-related clinical decision support. J Am Med Inform Assn 2020;27:1252–8. 10.1093/jamia/ocaa098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sittig DF, Wright A, Oshero? JA, Middleton B, Teich JM, Ash JS, et al. Grand challenges in clinical decision support. Journal of Biomedical Informatics 2008;41:387–92. 10.1016/j.jbi.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Powers EM, Shiffman RN, Melnick ER, Hickner A, Sharifi M. Efficacy and unintended consequences of hard-stop alerts in electronic health record systems: a systematic review. J Am Med Inform Assn 2018;25:1556–66. 10.1093/jamia/ocy112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eisenberg JM. Sociologic influences on decision-making by clinicians. Annals of Internal Medicine 1AD;90:957–64. 10.7326/0003-4819-90-6-957. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.