Abstract
Vaccine hesitancy is one of the greatest health care challenges of our time, as recently highlighted by the experience with COVID-19 vaccines. It is now clear that several current COVID-19 vaccines are highly effective in preventing severe disease, hospitalization, and death from the disease, but their effectiveness has been greatly undermined by the many unfounded conspiracy theories, active disinformation, and fears (real or imagined) circulating through social media and through society in general, persuading millions of people worldwide not to receive the vaccine. Fortunately, there are numerous practical strategies that physicians and other health care professionals can employ in communicating effectively with vaccine-hesitant individuals, including using humble inquiry, compassionate listening, and storytelling, as well as engaging the entire health care team in providing accurate information. This article summarizes the major points of an IAS-USA-sponsored webinar held on August 3, 2021, titled COVID-19 Vaccine Hesitancy, Crucial Conversations, and Effective Messaging for Patients and Health Care Teams by Marie T. Brown, MD, an expert on adult immunization. The webinar was moderated by Constance A. Benson, MD.
Keywords: COVID-19, vaccine hesitancy, SARS-CoV-2
Last year, a pregnant woman in her second trimester approached one of her physicians and expressed apprehension about receiving the COVID-19 vaccine. She believed in the benefits of the vaccine but was concerned by a lack of data supporting its safety for a fetus, as such data was not yet available in early 2021. The doctor immediately put her at ease. He agreed that there was no published data guaranteeing the safety of the vaccine for pregnant women, but he confirmed that there were tragic examples of pregnant women who did not survive COVID-19 disease. He shared that the obstetricians with whom he worked and the nurses on his staff who were pregnant had all received the vaccine and had no problems.
The doctor told the woman that any potential negative side effects of the vaccine were far, far outweighed by the well-known risks to pregnant women of contracting COVID-19, including pregnancy loss, preterm delivery, poor pregnancy outcomes, extended newborn intensive care unit stays, and more. The doctor also mentioned that his wife had recently received the vaccine and done just fine. The doctor made the woman feel smart for getting vaccinated in her second trimester.
With that confidence, the woman had no further hesitation and was vaccinated. She gave birth to a healthy baby a few months later. After the birth, she and her family were comforted to know that her newborn child now had some passive antibodies and was already somewhat protected against the disease. Months later, she brought the same confidence to her boostershot appointment while breastfeeding her 5-month-old infant.
This true story was shared (with the new mother's permission) by adult vaccination expert Dr Marie Brown during a recent IAS-USA webinar titled COVID-19 Vaccine Hesitancy, Crucial Conversations, and Effective Messaging for Patients and Health Care Teams.
The woman in the story? Dr Brown's daughter.
This experience is an example of one way physicians and health care professionals can address vaccine hesitancy with their patients: by telling stories. For many vaccine-hesitant patients, hearing a story like this from their personal physician is more powerful than facts and statistics. Other important tools that doctors can employ include engaging the entire health care team in the provaccine message, humbly inquiring into patients' fears, compassionately listening to patients' concerns, and avoiding hostility or frustration when presented with misinformation or conspiracy theories.
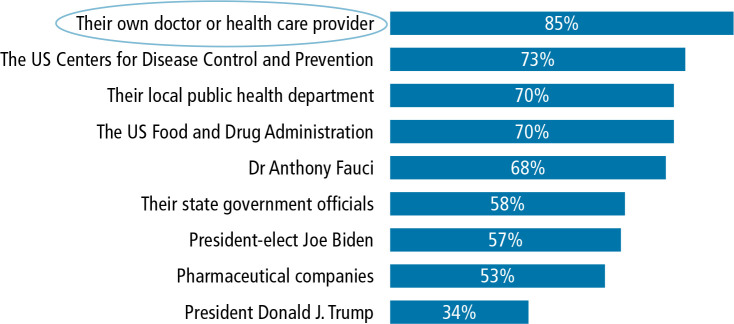
Physicians are in a uniquely advantageous position in the fight against vaccine hesitancy. According to one study, the most influential voice in whether a vaccine-hesitant individual decides to receive the COVID-19 vaccine is not national, state, or local health organizations, but rather that individual's personal physician or health care practitioner (Figure 1).1 It is incumbent on physicians, their teams, and other medical personnel to be on the same page in how they address this crucial public health issue.
Figure 1.
Percentage of Americans in December 2020 who said they had a great deal or a fair amount of trust in each of the presented options to provide reliable information about the COVID-19 vaccine. Adapted from the Kaiser Family Foundation.1
Vaccine hesitancy, social media misinformation, and active disinformation have emerged as some of the greatest health care challenges of this generation. Still, not all the news is dire. Based on surveys conducted during the spring of 2021, about 50% of the wait-and-see group (those individuals who have considered getting the COVID-19 vaccine but who are “waiting to see” its longterm effects) stated that they would strongly consider taking the vaccine once it was fully approved by the US Food and Drug Administration (FDA),2 and on August 24, 2021, the Pfizer vaccine was the first to receive full FDA approval. The United States also recently passed an important milestone: At the time of the webinar, over 50% of those who were in the wait-and-see group in January 2021 had received at least one dose of the vaccine.3 This is encouraging news. However, with only a bit over 70% of eligible Americans having taken at least one dose of the COVID-19 vaccine at this time, there is still much more work to be done and many more difficult conversations to be had with vaccine-hesitant patients.
For many physicians and for others with scientific backgrounds, the knee-jerk reaction when speaking with vaccine-hesitant individuals can often be to confront mistakes and misinformation with cold hard facts. At this point, such an approach is not practical if our goal truly is to convince as many people as possible to choose to be vaccinated. Instead, health care professionals can explore using a host of other communication techniques, such as telling stories, making those stories personal, responding with empathy to people's objections to vaccines and then easing the conversation compassionately in more productive directions, tailoring your message to each patient's concerns, and engaging the entire medical team in provaccine messaging. These are all more practical tactics and much more likely to guide patients in the right direction.
The Roots of Vaccine Hesitancy and the Social Media “Infodemic”
Propaganda, fearmongering, conspiracy theories, and disinformation are likely as old as human society itself. Throughout history, many causes and culprits have coerced large segments of various societies into believing many things that simply are not true, often to highly detrimental ends. Vaccine hesitancy can be seen as just another chapter in that lamentable, ongoing narrative.
Interestingly, though quite discouragingly, modern vaccine hesitancy has its earliest roots in the work of various medical professionals. Large segments of the public readily accepting their dubious claims is disconcerting, but not necessarily surprising. Public confidence in governmental and corporate institutions has never been sacrosanct, often for very good reason. Add to this the American medical industry's more than lamentable historical record; the impact of the long-running Tuskegee Syphilis Study,4 sponsored by the US Public Health Service, and the Puerto Rico Pill Trials5 on communities of color are just 2 of many examples of industrial and governmental malfeasance contributing to public mistrust of the medical establishment.
Sadly, this mistrust, as well as perhaps the notorious shortness of human memory, has led many people to forget one incontestable truth: Second perhaps only to sanitized drinking water, vaccines are arguably the most successful public health achievement in the history of mankind. This statement is not hyperbole. It would be impossible to quantify the number of lives saved and the overall worldwide improvement to quality of life due to, for example, the smallpox, measles, and polio vaccines alone. However, as the hackneyed-but-true expression goes, “Those who cannot remember the past are condemned to repeat it.” Measles was virtually eliminated from the United States decades ago, but in recent years it has seen a resurgence,6 largely due to American parents opting not to vaccinate their children. Polio is poised to make a similar comeback in other parts of the world.7
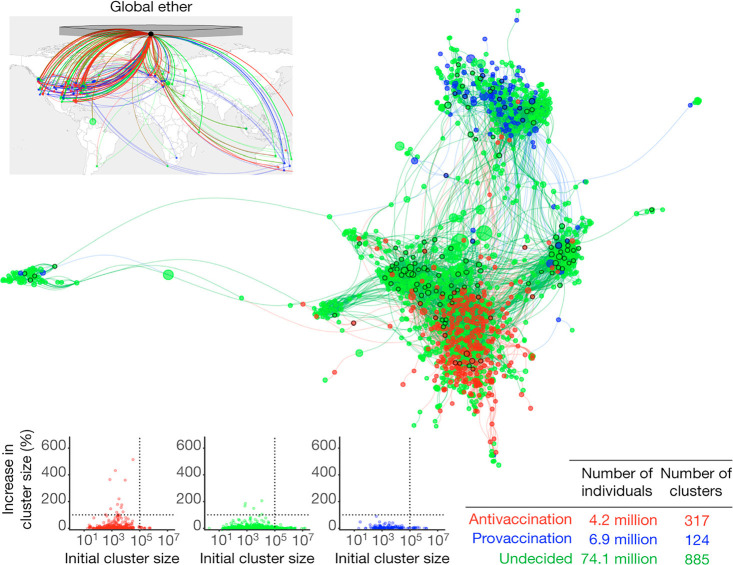
How have we gotten here? There are many, many answers to that question, but one of the most obvious is the influence on American and worldwide culture of the Internet and social media, which have offered the fertile soil in which the antivaccine movement has taken root and flourished. A casual glance at the statistics is startling. Antivaccine tweets are twice as likely to be retweeted as provaccine tweets, and 4 times more likely than neutral tweets.8 One report shows social media platforms realizing $1 billion in annual revenue from antivaccine content alone,9 giving the corporations who own those platforms very little profit motive to stem the antivaccine tide. Another study suggests that if current trends continue, the antivaccine movement could eventually overwhelm provaccine voices online, because anti-vaxxers are heavily entangled with the very large online presence of undecided (or wait-and-see) individuals, and provaccine voices online remain more peripheral, preferring to communicate only with each other (Figure 2).10 Clearly, the online antivaccine movement is entrenched, integrated, and growing stronger every day.
Figure 2.
Entanglement of antivaccine and provaccine advocates with undecided individuals on social media. Antivaccine clusters (red) overlap with a larger number of undecided clusters (green) than do provaccine clusters (blue), indicating the powerful, entrenched reach of antivaccine messaging online. Adapted from Johnson et al.10
This can be difficult to understand, because by any measure there are actually many more provaccine people in America than antivaccine people.10 That does not even take into account the millions of wait-and-see individuals who have already chosen to get the COVID-19 vaccine. Clearly, anti-vaxxers are the minority. However, the Internet and social media (and sometimes the mainstream media) allow small groups of people who hold extreme beliefs but have outsized voices to appear more mainstream, not to mention that the antivaccine movement's highly emotional, anecdotal approach to producing content is very effective on social media, and that the provaccine movement's messaging has floundered at almost every point. Because of this, the antivaccine movement has enjoyed great success online, resulting in what the World Health Organization (WHO) has called an “infodemic,” a rapid, toxic spread online of false information about COVID-19 and the COVID-19 vaccine.9
This infodemic, and the conspiracy theories and misinformation found therein, is wide-ranging in scope. For example, the “plandemic” narrative proposes a decades-long conspiracy between global governments, pharmaceutical companies, the Centers for Disease Control and Prevention (CDC), Google, and other powerful entities to engineer and release COVID-19 for sheer profit-motive purposes.11 Another popular conspiracy theory involves 5G cell phone signals activating microchips embedded in the COVID-19 vaccine to track, and perhaps control, the vaccinated; an early version of this conspiracy even led to the literal burning of 5G phone towers in England in 2020.12 Some anti-vaxxers claim that vaccines were invented to depopulate the Earth or to target certain ethnic or racial groups. The list goes on and on.
Other COVID-19 vaccine myths may seem more “science-based” (and thus more persuasive) at first glance, but they quickly turn out to be equally invalid: that you can catch COVID-19 from taking the COVID-19 vaccine, that COVID-19 vaccines contain fetal cells, that COVID-19 vaccines have been shown to cause infertility, and that COVID-19 vaccines can change your DNA. It is easy for physicians and scientists to dismiss these obviously false myths out of hand. However, all patient-facing medical personnel would do well to at least familiarize themselves with these myths, if only to be prepared when vaccine-hesitant individuals offer them as explanations for their fears.
Though myths abound regarding COVID-19, one thing that is not under debate is that COVID-19 vaccine hesitancy in the United States falls along predictable political and socioeconomic lines: Those in the “definitely not” group are overwhelming Republican, White, and live in rural settings, and those in the “already vaccinated” group are overwhelmingly Democratic and college educated. However, a deeper dive into the numbers reveals some important trends. For example, a large percentage of the wait-and-see group is made up of Black and Hispanic individuals, as well as 18- to 29-year-olds, and the definitely-not group, those who have stated they will never get the COVID-19 vaccine (or any other vaccine) under any circumstances, seems fixed at 15% of the American population, and has been historically fixed at that level since well before COVID-19.
It stands to reason that focusing provaccine messaging on the definitely-not group would not be very fruitful, because they are not likely to be swayed in any case. Instead, the medical establishment can shift its full messaging focus to the very large wait-and-see groups, in the hopes of convincing as many of those individuals as possible to move from being vaccine hesitant to fully vaccinated.
Engaging With Patients
How can that be accomplished? If it is more effective to focus provaccine efforts on vaccine-hesitant (wait-and- see) individuals, what tactics are most useful? Put more simply, how can physicians and medical professionals educate ourselves to communicate more effectively with vaccine-hesitant patients than we have so far?
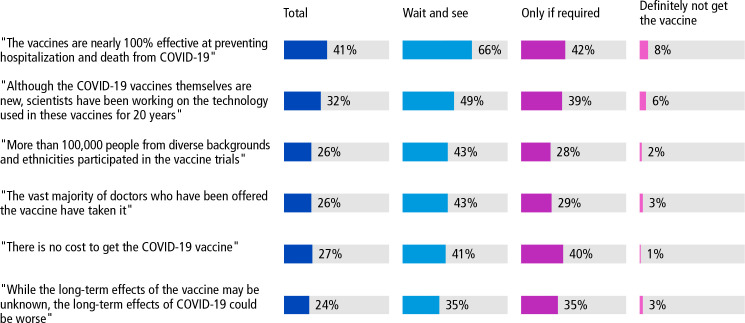
It should be abundantly clear by now that at least one approach will never work: accosting vaccine-hesitant patients with reams of data, no matter how scientifically accurate those data are. However, some fact-based messages do appear to be more effective than others (Figure 3).13 For example, studies have shown that vaccine-hesitant patients are much more likely to opt for the vaccine when they learn that (1) the vaccines are nearly 100% effective at preventing hospitalization and death from COVID-19, or that (2) the technology used to develop the COVID-19 vaccines is not brand new, as seems to be widely believed, but has in fact been in development for nearly 20 years. Patients also seem to respond very strongly when physicians talk about the vaccine helping prevent their loved ones from getting sick.1 Physicians and medical personnel can familiarize themselves with these simple, impactful messages, because doing so goes a long way toward preparing for these difficult conversations.
Figure 3.
Percentage of Americans in March 2021 who said they were most likely to get the COVID-19 vaccine if they heard each of the following messages. Adapted from the Kaiser Family Foundation.13
One of the most powerful tools for engaging with vaccine-hesitant patients is storytelling. Storytelling is hardwired into every human culture and every human brain, so narratives, anecdotes, and metaphors can be very effective ways of breaking down barriers and transmitting life-saving information. Telling emotionally engaging stories is not necessarily a natural skill for many physicians and scientists, but in the current cultural environment, it is a very important skill to foster. With this in mind, think about your own professional and personal experience with COVID-19. Has someone in your family been impacted by the disease? Have you had patients who took the vaccine and had positive outcomes, or patients who did not take the vaccine and had negative outcomes? How did those events affect you personally, make you feel? The more details and emotions you can provide to bring the story to life (while of course maintaining patient privacy), the more effective your message can be. If you know other medical professionals who seem more naturally gifted at telling stories, don't be hesitant to ask them for advice. Often, telling a good story is as simple as remembering a few key bullet points of a narrative, then practicing a few times until telling the story becomes natural.
Another valuable approach involves engaging the entire health care team, not just physicians, in provaccine messaging. Although nearly all practicing physicians in America have chosen to be vaccinated, 3 in 10 health care workers had not been vaccinated for COVID-19 as of March 19, 2021, and 18% of health care workers had not planned to get vaccinated at all.14 This massive disparity within the health care ranks makes it difficult to form a unified front in the messaging battle against COVID-19 vaccine hesitancy; an opportunity is lost every time a patient interacts with a health care worker, including nurses, medical assistants, front desk employees, and many others, and that patient is not addressed about receiving the vaccine. It is crucial to engage with all health care workers on a given team, not only to encourage them to be vaccinated for their own benefit, and not only because they might encourage patients to do the same, but also because those workers can become trusted resources of information about what is happening in the community. Put another way, it is likely much easier to change your team's beliefs than your patients', and the more you do so, the more effective your entire team's unified efforts will be.
Other important advocates to engage with are provaccine community leaders. These can include local celebrities, religious leaders, business leaders, and politicians (although in our current environment, some politicians are the source rather than the solution for vaccine hesitancy). Dr Brown met years ago with the pastor of a large Black church in Chicago, where she practiced internal medicine. During this meeting, the pastor shared with Dr Brown that he had just had a new grandson. This led Dr Brown to inquire if the pastor's tetanus, diphtheria, and pertussis (Tdap)/whooping cough vaccination was up to date. Then, just as the pastor was about to leave the room, he mentioned that his church baptizes more than 10 babies per week, and he asked Dr Brown if his deacons should all get the Tdap vaccine as well. Dr Brown, of course, said yes. “Because he encouraged his deacons, who would have been holding these newborns, and then having an opportunity to talk to their parents, he probably decreased the pertussis rate on the West Side of Chicago singlehandedly,” Dr Brown said.
Even with the help of community advocates and the health care team, physicians will still need to meet directly with vaccine-hesitant patients. Fortunately, numerous websites and online toolkits are available to help prepare medical professionals for these conversations. The free American Medical Association (AMA) STEPS Forward™ toolkit offers useful case studies that walk physicians through various vaccine-related conversations, as well as many patient objections you might encounter.15 Other toolkits aim to help physicians talk with patients, including Black and Latinx patients, about the realities of COVID-19 and the vaccine, as well as providing advice for effective social media use with those communities.16 For some health care organizations, it might also be worth using a physician belief scale to measure you and your team's beliefs about the psychosocial aspects of patient care, which can determine whether you even believe that addressing a patient's personal thoughts or opinions is valuable.17 Using such a tool can offer advice on how to change that mindset for the better.
Another crucial aspect of mindset to consider is your answer (and your patient's answers) to the following question: Do you believe getting the COVID-19 vaccine is a social responsibility, or is it solely a matter of personal choice? Most people on the provaccine side believe the former to be true. However, research shows that the American population is split down the middle on this question.1 Because of this, physicians risk alienating nearly 50% of the population if they push a narrative to vaccine-hesitant patients that they, the patient, have a responsibility to protect others by getting the vaccine, which could conflict with those patients' strong belief in their own personal choice. When interacting with vaccine-hesitant individuals directly, it is not necessary to agree with them on this issue, but it is crucial to respect their beliefs, and not to impose one's own belief system upon them.
Similarly, it is vitally important, when speaking with a vaccine-hesitant patient, not to repeat out loud the myth or conspiracy theory they might have offered you as their reason for not getting vaccinated. Simply hearing the myth spoken out loud, even if the medical professional is debunking it, can in fact reinforce the myth. A better tactic is to genuinely acknowledge that the vaccine-hesitant individual seems invested in learning as much as possible to ensure their own health and the health of others, and then to guide the conversation toward your practical, medically informed advice on how to do that.
On this and many other potential points of disagreement with vaccine-hesitant patients, physicians must do everything in their power to always remain calm and composed, and to allow patients to fully explain their point of view, no matter how much the physician might want to immediately correct them. For example, a patient might ask your opinion of hydroxychloroquine. As a physician with extensive scientific training, you are likely to have very strong opinions about hydroxychloroquine. However, it is not advisable to offer those opinions immediately, and certainly not advisable to offer those opinions in frustration or anger. Instead, a more effective response is to say something with a positive spin, such as: “Oh, I see that you are sincerely worried about this disease, and you are looking for something that will be effective in helping you prevent infection. Is that right?” That type of response opens a conversational door rather than closing it. Although a lengthy conversation will probably take time out of a physician's busy schedule, keeping the patient positively engaged is much more likely to move them toward understanding the incredible benefits of the COVID-19 vaccine.
Other, seemingly more simplistic interventions can also be very effective. Wearing an “I got my COVID shot” button or other similar paraphernalia, and having as many members of the medical team as possible do so as well, sends a clear, unified message to vaccine-hesitant patients (Figure 4). When talking with patients who might claim religious or political reasons for not taking the COVID-19 vaccine, do not be afraid to use your phone to show them online articles from websites they might already use regularly: for example, the 2021 Fox News article18 where former President Donald Trump urged all Americans to get the vaccine and stated that the vaccine is safe and effective, or other stories about how Reverend Franklin Graham and Pope Francis are both publicly in favor of Christians getting the COVID-19 vaccine. Physicians should tailor this approach to the individual patient, and ask first if the patient would like to view some of these news stories. Agreeing to look at these sources of information together could be an effective first step in overcoming their hesitance.
Figure 4.

COVID-19 vaccine pins can help support a provaccine environment.
Finally, the core of any approach to dealing with vaccine-hesitant patients must be humble inquiry. Humble inquiry means sitting down with patients, taking time, asking them sincere questions, listening to them, acknowledging their points of view calmly and compassionately even when one does not agree, and then doing one's best to tailor the most helpful message directly to them. Most people can tell the difference between someone reading from a script and someone really trying to connect emotionally and empathetically. Like storytelling, humble inquiry is not a natural skill for all people, but it is a skill that can be learned and fostered. In this vital struggle against COVID-19 and vaccine hesitancy, we should all consider doing so.
Q&A Session
After the discussion around the numerous tactics for addressing vaccine hesitancy with patients, Dr Brown and Dr Benson engaged in a Question and Answer session with the webinar participants. Following is an abridged transcript of that conversation, edited for brevity and clarity. Again, these discussions were based on the current knowledge as of August 3, 2021, the presentation date of the webinar.
Question:
How can we best address vaccine hesitancy in light of the study in Massachusetts showing that more than 70% of those in the July 2021 outbreak there were people who had been vaccinated? How would you approach the messaging?
Dr Benson:
A lot of the messaging around COVID-19 vaccines has been confusing, largely because the media and even many of our colleagues have not made the distinction between being infected and able to transmit the infection, versus having severe disease, being hospitalized, or having a high risk of dying.
The vaccines that are available to us right now are extremely effective in preventing severe disease, preventing hospitalizations, and preventing deaths.
In our experience in San Diego, of those individuals hospitalized for COVID-19, more than 80% are people who were not vaccinated at all, and the remainder are partially vaccinated or have underlying conditions that interfered with a robust immune response to the vaccine. However, the majority of those hospitalized who had been vaccinated have not required admission to the intensive care unit (ICU). More than 50% of the cases in certain areas and more than 90% in other areas experiencing large surges are with the Delta variant, and although fully vaccinated individuals can be infected with the Delta variant, they are not developing severe disease. With the outbreak of COVID-19 infection in Massachusetts, the majority of individuals had no or mild symptoms and were not hospitalized.
These infections, in fact, are an advertisement for how effective the vaccines are in preventing the majority of those people from getting sick and from being hospitalized and from dying.
Question:
Dr Brown, how did you convince your daughter, who was in the second trimester of pregnancy, to get vaccinated? And as a corollary to that, how do you encourage breastfeeding parents to be vaccinated?
Dr Brown:
That's a great question. I did not need to convince my daughter, who is not in health care but believes strongly in science. She asked her physician, who said, “Get the vaccine. My wife and our staff got it to keep themselves and others healthy.” Understanding that the breast milk may be protective for the newborn, she actually got her third dose while still breastfeeding and feels comforted that she provided the best protection for her baby. Her physician used an anecdote, and that's all she needed. So, it was a trusted person who was caring for her sharing a personal and clear message.
Question:
Why are we calling this “vaccine hesitancy” when people are refusing to be vaccinated? Hesitancy makes it seem like they're not sure if they want the vaccine.
Dr Brown:
In my opinion, “hesitancy” is a good term, because we want to (and often can) move vaccine-hesitant people to vaccine-accepting people. The 10% to 15% of people who refuse the vaccine will always refuse the vaccine. Even back in the smallpox era, the term “conscientious objector” was coined for people who refused to take the smallpox vaccine in London hundreds of years ago. We are not going to change the proportion of those who refuse; it has been consistent throughout history.
What we need to focus on is the vast majority who are hesitant. They want to do the right thing. They need a trusted person to be knowledgeable, to respect their concerns, and to answer their questions.
Question:
How likely are unvaccinated individuals to get infected with SARS-CoV-2? Will 100% of unvaccinated people get COVID-19 if they do not get vaccinated?
Dr Benson:
The answer depends on the level of risk of the person and with whom they are in contact. The current circulating Delta variant is tremendously transmissible. (Update: The Omicron variant is even more transmissible than the Delta variant.) People carrying the Delta (and now Omicron) variant have such high viral loads in the nasal secretions that someone coming into close contact with them in an indoor setting has a high likelihood of becoming infected if they're not vaccinated.
For people who have been vaccinated, however, we do know that breakthrough infections are common, although marginally less common than among those who are unvaccinated. We do know that people at high risk, those who are immunocompromised, for example undergoing cancer chemotherapy or transplant recipients, those who are over the age of 65 years, or who have other underlying conditions that affect immune function may not have as robust an immune response to any vaccine, and may be at some higher risk of infection and of more serious disease.
The point here is not that 100% of people who are fully vaccinated will be protected from infection by the Delta variant, but that the risk of infection may be lower, and the risk of serious disease, hospitalization, and death is substantially lower than for those not vaccinated at all.
Question:
Please address the myth circulating in the media and as stated by a former Nobel laureate that people who have received COVID-19 vaccines would die within 2 years as a result of antibody-dependent enhancement.
Dr Benson:
Antibody-dependent enhancement after vaccination was a very early concern of the scientific community when coronavirus vaccines were first investigated. Some of that was related to (1) the experience with very early coronavirus vaccines in veterinary practices, where animals developed antibody-dependent enhancement and actually got sicker after encountering coronavirus postvaccination; and (2) the experience with dengue vaccine development, which has been hampered by similar antibody-dependent enhancement.
The scientific community has been monitoring this closely since the origin of the first severe acute respiratory syndrome (SARS), SARS-CoV, and Middle East respiratory syndrome (MERS) outbreaks. There is no evidence in any of the human studies with those viruses, or from the data that emerged from the SARS-CoV-2 vaccine trials, that antibody-dependent enhancement has occurred. There has not been a single case reported out of the many millions of people who have now been vaccinated. Thus, there is no evidence that it would occur 2 years after vaccination.
Can we say that with absolute certainty? In my opinion, yes.
Question:
How do you address questions from patients with no absolute answer? How do you address that kind of conversation?
Dr Brown:
I think it is important to pivot quickly to what we do know. If we are trying to get somebody to stop smoking, telling them what bad things can happen, like emphysema or lung cancer, is less effective than highlighting good things, such as being able to play with their grandkids. To encourage vaccination, highlighting its benefits is effective. Do you want to get back to work? Do you want your kids to get out of the house and go back to school? Do you want to be able to hug your parents and see your brothers and sisters? What are you missing now? Maybe they've lost their job.
Pivoting quickly to the benefits of getting the vaccine: It is so safe relative to disease. For example, compare polio and measles vaccination with the encephalitis-associated brain damage that can occur with disease. Share details of the last patient you saw with COVID, without compromising patient confidentiality, to make it more relevant to your patient. Tell them they were a school teacher or a neighbor, whatever the experience was, and how vaccination could have saved them and their family heartache. Make it personal.
The people watching this webinar know the most heart-wrenching story of somebody who died of COVID-19, someone who lost their mother, their sister, or their wife. Share that story. Tell the heart-wrenching story about somebody who could have prevented their death had the vaccine been available. Note how fortunate we are now to have the vaccine. That's how I answer it.
Question:
We get lots of questions about COVID-19 and infertility. How do we respond to that?
Dr Benson:
This is a question that has generally been asked by pregnant women or women anticipating becoming pregnant who are worried about their own fertility. However, there is very strong evidence that with the overexpression of the receptors for coronaviruses in testes, it is far more likely that male infertility will be a complication of COVID disease, not of vaccination. People who get COVID, even if they don't have severe disease, have the potential for SARS-CoV-2 in the testes to decrease sperm count, decrease semen quality, and lower volume. Studies demonstrating short-term infertility in men who have recovered from COVID disease have been published. However, there are no data linking SARS-CoV-2 vaccines to any impact on the male or female reproductive systems or infertility in animal models postvaccination.
All of the infertility data related to COVID stem from this as a complication of COVID itself, not of the vaccines.
Dr Brown:
We should remember that mumps can cause orchitis and infertility, which would make sense to somebody. I think that's a really good message.
Question:
How effective are the current vaccines against variants, and will we need boosters? How durable is the vaccine protection?
Dr Benson:
What we can say, based on our current information, is that each of the vaccines are very effective against the current variants circulating at the time of this webinar in preventing severe disease, preventing hospitalization, and preventing death. We have learned from the experience with the Delta variant that they are not as effective in preventing people who are fully vaccinated from getting infected. There is still the potential with the Delta variant, although maybe not as high a potential as for the unvaccinated, that they could be infected and transmit to another person. (Update: Our understanding with the Omicron variant is that it is even more highly transmissible than the Delta variant, vaccine efficacy in preventing infection among the fully vaccinated is lower, and breakthrough infections are occurring; however, rates of severe disease, hospitalizations, and deaths are lower among those fully vaccinated, and especially among those who have received a booster dose of a vaccine.) This is where we are with understanding vaccine efficacy.
With regard to vaccine boosters, the data from published studies and the messaging from the CDC is that there is a waning of the neutralizing antibody response over time, particularly after 6 to 9 months among those fully vaccinated. For most people with normal immune function, there is still sufficient neutralizing antibody and antibody-mediated cellular immunity to prevent severe disease, hospitalizations, and death at least following exposure to the Delta variant. (Update: A booster dose also further enhances that effect for the Omicron variant.)
However, our current data indicate there are vulnerable populations within the fully vaccinated, such as individuals who are immunosuppressed and individuals who are over 65 years of age. These individuals may have had a less robust early response or a more rapid waning of immunity than what we see in younger, healthier individuals.
(Update: As further data have accumulated, public health officials, the FDA, and the CDC are now in agreement that eligible adults and adolescents who have been previously vaccinated should receive a booster dose of vaccine 5 to 6 months following their initial vaccination. I think we're going to see recommendations from public health officials in the very near future that additional vaccine boosters will be necessary, perhaps every year, as we do with influenza vaccines. Whether it will be necessary to alter or adjust the current vaccines to accommodate current or new variants in the future remains to be established.)
Question:
Is it safe to mix different vaccines?
Dr Benson:
Based on current evidence, the answer is yes. Some countries, like the United Kingdom and Israel, began doing this early on even with the second vaccine dose, particularly when supplies were limited for certain types of vaccines. For example, the adenovirus vector vaccines are now being boosted with the mRNA vaccines in many countries. This appears to be safe in clinical trials, and has been endorsed by the CDC in the United States.
Question:
Do you have particular messages for talking about vaccine hesitancy among your Black or Hispanic populations? Are there tailored messages that you have advice about for those populations?
Dr Brown:
The website I showed, La Conversación,16 has celebrities and trustworthy sources that address some of those concerns. We need to come prepared to these conversations about historical events like the Tuskegee Syphilis Study. We should approach all communities with humility and awareness that, for example, the Tuskegee Study was funded by the US government.
Dr Benson:
You made some very good points about some of the church leaders in African American communities. Making use of representatives of the community is a particularly important message, trying to have a champion, if you will, of vaccination.
There have also been a number of celebrities who can have tremendous influence over Black and Hispanic communities who have had a real handsoff approach to the issue of vaccination. In some instances, this has been misinterpreted as a lack of support for vaccination; however, searching for other celebrity champions more willing to tell their own stories has resulted in some of those messages starting to get out more effectively with people who listen to them.
Dr Brown:
Another myth that has arisen is around documentation required to get the vaccine. Undocumented people hesitate to access a government site that requires documentation, such as a government state-issued ID or social security number. This is where access for the vaccine hesitant is important. Having a mobile station, going to their places of work, and going directly to their worksite are ways to make vaccination easier. Put a mobile station in front of a concert, where you can get in if you get the vaccine. “I really want to see that musician. I'll get the vaccine.”
Improving access to make it more convenient than inconvenient is important, especially when it comes to schools. The American Academy of Pediatrics has a wonderful document for parents to read and sign.19 It asks them to acknowledge statements such as: “If my child does not receive the vaccine(s) according to the medically accepted schedule, the consequences may include: contracting the illness the vaccine is designed to prevent (the outcomes of these illnesses may include one or more of the following: certain types of cancer, pneumonia, illness requiring hospitalization, death, brain damage, paralysis, meningitis, seizures, and deafness; other severe and permanent effects from these vaccine-preventable diseases are possible as well).” That often changes a parent's mind when they have to sign an acknowledgement of the risk.
Question:
Is there any evidence about vaccination-related adverse pregnancy outcomes?
Dr Benson:
The CDC and FDA are following pregnant women who have been vaccinated through the Vaccine Adverse Event Reporting System (VAERS). Based on data they have collected from more than 120,000 pregnant women who reported receiving vaccines during pregnancy, there have been no adverse outcomes among the pregnant women or their infants from data collected as of May 24, 2021. There have been pregnant women who received COVID vaccines who miscarried, but the miscarriage rates among those women are the same as in the general population prior to the pandemic, or in the general population who have not received vaccinations.
Animal toxicity studies are conducted in vaccine development. Numerous animal toxicity studies to date have not shown an adverse effect of current vaccines on embryonic fetal or postnatal development of fetuses born to those animals after receipt of vaccine in early or late gestation. We are pretty comfortable at this point that the vaccines are not associated with adverse pregnancy outcomes.
However, pregnant women who have COVID-19 are at increased risk of more severe illness, increased risk of ICU admission, increased risk of the need for mechanical ventilation, and have a higher mortality rate than nonpregnant women. Infection earlier in pregnancy is also associated with an increased risk of adverse fetal outcomes. And in a meta-analysis that included more than 42 studies involving almost 500,000 pregnant women with COVID, the adverse fetal outcomes that were recognized at higher rates than in the prepandemic era were preeclampsia, preterm birth, and stillbirth.
Question:
Can you comment on the more serious complications of vaccines in young people, including myocarditis?
Dr Benson:
It does appear that the mRNA vaccines are associated with an increased risk of myocarditis. According to the Morbidity and Mortality Weekly Report published by the CDC, the prevalence is about 1 case per 7 million doses, usually occurring after the second dose, is more common in males, and is more common in people under the age of 30 years. The majority of the cases have been self-limited, only a minority of them have required hospitalization, and symptoms have resolved within 5 to 7 days of onset. The symptoms associated with myocarditis have been relatively mild and included chest pain, low-grade fever, and sometimes shortness of breath and pleuritic chest pain. Most have been associated with modest electrocardiogram findings of ST elevations.
In addition to myocarditis, there have been cases of thrombocytopenic purpura that appears to mimic heparin-induced thrombocytopenia in people who have gotten an adenovirus-based vaccine. This adverse reaction appears to have a predilection for women and has been associated with a small number of fatal cases of cavernous sinus thrombosis or other serious thrombosis disorders among younger women who received an adenovirus vector vaccine. It depends on the study one looks at, but this reaction, although rare overall, appears to occur more commonly in women under the age of 30 years. In the United States, the cases are mostly associated with the Johnson & Johnson vaccine. Overall, the rate is approximately 1 in 7 million doses, so it is still a rare complication of vaccination.
Dr Brown:
These numbers, 1 in 7 million, are meaningful to the medical community but may not be as meaningful to the general population. “It's only 1 in 7 million” may not be terribly effective for someone who just came from the local gas station and put $20 down on a 1 in 10 million shot of winning the lottery, given that the average American spends $200 on the lottery each year.
Responding with a narrative related to the person in front of you may be more helpful. To a 20-year-old who is asking you the question, you might respond, “We had a 20-year-old just last week who passed away from COVID after 3 weeks intubated and on a ventilator in the ICU. His girlfriend and parents were devastated, and his family could not be with him during his last frightening days.” Use whatever relatable story that you can share.
Question:
What's your best response to someone who says that vaccine development was rushed, that the vaccines are still experimental, and that they haven't been approved or were only recently approved by the FDA after a long deliberation, so why should I take them or trust them?
Dr Benson:
It is important to note vaccine development for COVID-19 did not involve shortcuts that skipped appropriate steps in the developmental process. All of the same developmental steps were taken, but many were accomplished concurrently rather than consecutively to try and speed the results. By that I mean not only the developmental procedures, but also the manufacturing procedures that needed to be in place to make them available. A massive amount of resources was directed to preclinical development and clinical development in vaccine trials, including investment in sufficient resources to enroll thousands of patients in a few months of time in very large randomized clinical trials.
The logistical setup and implementation of the trials was accelerated, not the developmental process itself. The scientific community completed every single stage of development that we normally would do for a new vaccine including studying them in the laboratory, in animal models, in phase I studies, phase II safety and dose ranging studies, and then in very large phase III randomized trials, each of which was staged to begin when preliminary results from earlier stages indicated it was safe to do so. Rather than, like most vaccines, waiting until they are approved to put together all of the steps for manufacturing, those parts of the process were done in tandem while the clinical trials were being completed. It was understood that money may be spent on a manufacturing process that would never be used, but if we were lucky and any of the candidates were effective, that we would be ready to go when we had the data from the trials.
As Dr Brown said earlier, these vaccine constructs have been in development for more than 20 years. The mRNA construct has been used in Ebola virus vaccine development, as well as early development of vaccines for the first SARS and MERS outbreaks a decade ago. The scientific community was not able to fully test them because those outbreaks stopped before the clinical trials could be completed.
Dr Brown:
I also want to note the important role of employers, especially for younger age groups. Employers are instituting creative strategies for encouraging vaccinations. One organization offered an extra Fourth of July holiday day off if at least 70% of employees were vaccinated. Another offered an additional $20 or $30 into their cafeteria fund. These types of creative strategies have subsequently been followed by local, state, or federal government-instituted vaccine mandates for certain groups, which have been extraordinarily effective in getting more people vaccinated.
Summary
In the maelstrom surrounding the COVID-19 pandemic and the vaccine hesitancy debate, an important point has largely been drowned out: The COVID-19 vaccine is one of the greatest triumphs in the history of medicine. In little over a year, the international medical and scientific establishment produced and rolled out a “magic shot” that has already saved millions of lives. With every passing month, there is more and more evidence of just how effective the COVID-19 vaccines truly are.
When confronted with the arguments, objections, and confusion of vaccine-hesitant patients, it is understandable that some scientists and physicians might feel frustrated when speaking with these individuals. Scientists and physicians rely on cold hard facts, on the evidence in front of them, and on the best research available to make important decisions. This approach is amazingly effective at treating sick patients and developing vaccines. But the majority of individuals do not make decisions in the same way. Instead, they use a combination of rational thinking, personal history, and emotion, among other varied factors. Even the most hardened, by-the-book scientist or physician cannot claim to have made every life decision based solely on facts and evidence.
That is why the techniques discussed in this summary have been shown to be so effective: They are all ways to engage patients emotionally. Sitting down calmly with vaccine-hesitant patients, asking them sincere questions, listening compassionately to their concerns, and telling true and impactful stories: These approaches might seem to be less “scientific,” but they are certainly more human.
Footnotes
This article was based on a webinar presented by Dr Brown and moderated by Dr Benson on August 3, 2021, titled COVID-19 Vaccine Hesitancy, Crucial Conversations, and Effective Messaging for Patients and Health Care Teams. The webinar can be viewed here: https://www.youtube.com/watch?v=Vm0g3L2Hu5g.
Financial affiliations with ineligible companies (formerly named “commercial interests” by the ACCME) in the past 24 months: Dr Brown has no relevant financial affiliations to disclose. (Updated December 20, 2021) Dr Benson has served on advisory and data safety monitoring boards for GlaxoSmithKline/ViiV Healthcare, received research grants awarded to her institution from Gilead Sciences, Inc., and serves as a consultant to NDA Partners, LLC. (Updated December 23, 2021)
Contributor Information
Marie T. Brown, Director of Practice Redesign at the American Medical Association, as well as an internist and Professor in the Department of Internal Medicine at Rush University Medical College in Chicago, Illinois..
Constance A. Benson, Professor of Medicine and Global Public Health, Senior Attending Physician, Vice Chair for Education, and Director of the AntiViral Research Center at the University of California San Diego..
References
- 1. Kaiser Family Foundation. KFF COVID-19 vaccine monitor: December 2020. https://www.kff.org/coronavirus-covid-19/report/kff-covid-19-vaccine-monitor-december-2020/. Published December 2020. Accessed September 21, 2021.
- 2. Kaiser Family Foundation. KFF COVID-19 vaccine monitor: June 2021. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-june-2021/. Published June 2021. Accessed September 21, 2021.
- 3. Kaiser Family Foundation. KFF COVID-19 vaccine monitor: in their own words, six months later. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-in-their-own-words-six-months-later/. Published July 2021. Accessed September 21, 2021.
- 4. Rockwell D, Yobs A, Moore M Jr. The Tuskegee Study of Untreated Syphilis: the 30th year of observation. Arch Intern Med. 1964;114:792–798. [DOI] [PubMed] [Google Scholar]
- 5. Public Broadcasting Service. The Puerto Rico Pill Trials. https://www.pbs.org/wgbh/americanexperience/features/pill-puertorico-pill-trials/. Accessed September 21, 2021.
- 6. Phadke VK, Bednarczyk RA, Omer SB. Vaccine refusal and measles outbreaks in the US. JAMA. 2020;324(13):1344–1345. [DOI] [PubMed] [Google Scholar]
- 7. Beaubien J. The campaign to wipe out polio was going really well… until it wasn't. National Public Radio. Published October 2020. Accessed September 21, 2021.
- 8. Blankenship E, Goff M, Yin J, et al. Sentiment, contents, and retweets: a study of two vaccine-related Twitter datasets. Perm J. 2018;22:17–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Burki T. The online anti-vaccine movement in the age of COVID-19. Lancet Digit Health. 2020;2(10):e504–e505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Johnson N, Velásquez N, Restrepo N, et al. The online competition between pro- and anti-vaccination views. Nature. 2020; 582(7811):230–233. [DOI] [PubMed] [Google Scholar]
- 11. Frenkel S, Decker B, Alba D. How the ‘Plandemic’ movie and its falsehoods spread widely online. New York Times. May 20, 2020.
- 12. Satariano A, Alba D. Burning cell towers, out of baseless fear they spread the virus. New York Times. April 10, 2020.
- 13. Kaiser Family Foundation. KFF COVID-19 vaccine monitor: March 2021. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-march-2021/. Published March 2021. Accessed September 21, 2021.
- 14. Kaiser Family Foundation. KFF/post survey of frontline health care workers finds nearly half remain unvaccinated. https://www.kff.org/coronavirus-covid-19/press-release/kff-post-survey-of-frontline-health-care-workers-finds-nearly-half-remain-unvaccinated/. Published March 2021. Accessed September 21, 2021.
- 15. American Medical Association. STEPS Forward Toolkits. https://edhub.ama-assn.org/steps-forward/module/2702553?resultClick=1&bypassSolrId=J_2702553. Accessed September 21, 2021.
- 16. Greater Than COVID. Greater Than COVID website. https://www.greaterthancovid.org/. Accessed September 21, 2021.
- 17. Ashworth C, Williamson P, Montano D. A scale to measure physician beliefs about psychosocial aspects of patient care. Soc Sci Med. 1984;19(11):1235–1238. [DOI] [PubMed] [Google Scholar]
- 18. Halon Y. Trump urges all Americans to get COVID vaccine: ‘It's a safe vaccine' and it ‘works’. Fox News. March 16, 2021.
- 19. American Academy of Pediatrics. Documenting parental refusal to have their children vaccinated. https://downloads.aap.org/DOPCSP/SOID_RTV_form_01-2019_English.pdf. Accessed August 25, 2021.