Abstract
In line with previous instalments of analysis from this ongoing study to monitor ‘Covid Seroprevalence’ among blood donors in South Africa, we report on analysis of 3395 samples obtained from 8 to 12 November 2021 in all provinces of South Africa except the Western Cape. As in our previous analyses, we see no evidence of age and sex dependence of prevalence, but substantial variation by province, and by race within each province, from which we generated provincial total point estimates (EC-74%; FS-75%; GP-68%; ZN-73%; LP-66; MP-73%; NC-63%; NW-81% ) and a ‘South Africa minus Western Cape’ national prevalence estimate of 71% (95%CI 69–74%). We note that sample collection occurred just before the omicron variant driven wave in South Africa, but otherwise present these results without significant interpretation.
Keywords: COVID-19, seroprevalence, anti-SARS-CoV-2 antibodies, blood donors, South Africa
Introduction
We have previously published estimates of the prevalence of anti-SARS-CoV-2 antibodies among blood donors in South Africa, based on specimens collected from January to May 2021 [1,2], as well as estimates of fatality rates, based on these prevalence estimates and publicly available excess deaths estimates [3].
While the interpretation of seroprevalence is increasingly complicated by vaccination coverage and multiple infections of individuals, we understand that seroprevalence is still relevant from the point of view of understanding aspects of transmission and collective immunity that are relevant to ongoing adjustment of anti-transmission measures, policies, and regulation.
Methods
Anticipating that a fourth wave late in 2021 was inevitable (though there was no knowledge of the omicron variant at the time of planning), 3395 specimens were randomly collected from consenting donors from all provinces except the Western Cape (which has its own separate blood service) presenting to donate blood to the South African National Blood Service (SANBS) from 8 to 12 November 2021. This was carried out in accordance with previous arrangements and practices underlying our previous rounds of sampling [1,2], as approved by the SANBS Human Research Ethics Committee (HREC).
For analysis, serology data was linked to basic donor demographic information (age, sex and race) but not to any other underlying data potentially available from the SANBS donor database (donation history, specific locale of donation/residence, donor identifiers etc).
Samples were tested for the presence of antibodies to SARS-CoV-2 nucleocapsid proteins, using the Roche Elecsys platform. These antibodies are typically developed in response to natural infection, but not in response to any vaccine currently available in South Africa. While there is some waning of antibodies, in this context we expect about 95 percent of donors who ever developed antibodies to have detectable levels at the time of testing [4] while a small proportion (we estimate in the range of 5–10 percent) of individuals who experience infection never develop detectable antibodies. [5]
Results
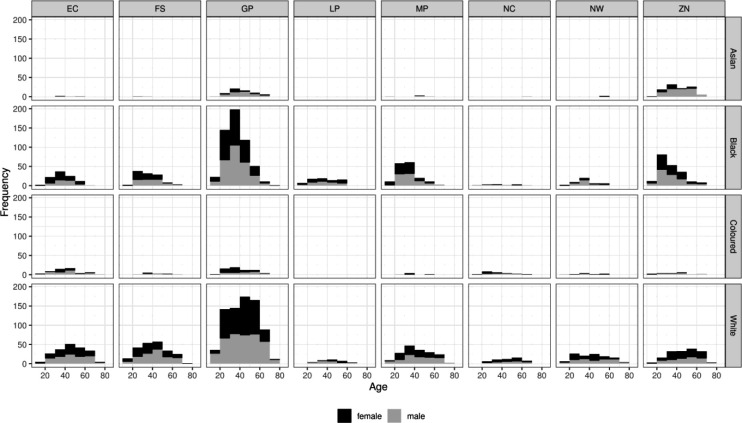
Figure 1 shows the distribution of specimens by age group, race, sex and province. We found no statistically significant dependence of seroprevalence on either age or sex. However, unsurprisingly, there were statistically and epidemiologically significant differences between provinces, and among race groups in each province. Hence:
We report primary results by every combination of province and racial group (Figure 1).
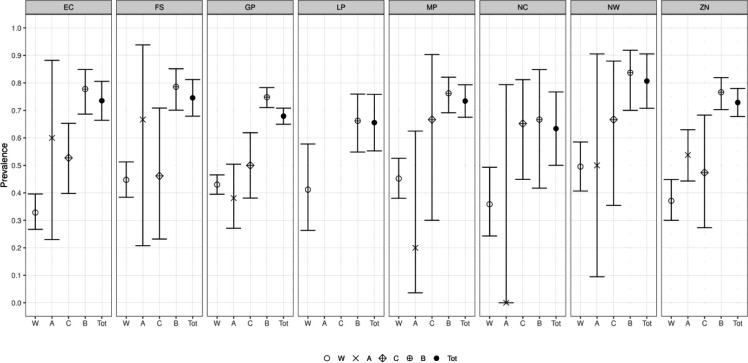
From these, we generated a race-weighted seroprevalence for each province (Figure 2).
From these provincial estimates, we generated a ‘national’ (minus Western Cape) estimate by weighting according to provincial population sizes (Table 1).
Figure 1:
Age distribution of specimens included in the present analysis, further decomposed by race and province.
Figure 2:
Seroprevalence estimates, for each sampled province, by race, and a race weighted provincial total.
Table 1:
The numerical provincial race-weighted seroprevalence values underlying figure 2
| Province | Point Estimate (%) | 95% Confidence Interval Lower bound (%) |
95% Confidence Interval Upper bound (%) |
|---|---|---|---|
| Eastern Cape | 73.5 | 66.0 | 81.0 |
| Free state | 74.6 | 67.5 | 81.6 |
| Gauteng | 67.9 | 64.9 | 70.9 |
| Limpopo | 65.6 | 54.6 | 76.5 |
| Mpumalanga | 73.4 | 67.2 | 79.6 |
| Northern cape | 63.4 | 48.1 | 78.7 |
| North West | 80.7 | 69.9 | 91.5 |
| KwaZulu Natal | 72.9 | 67.5 | 78.2 |
| 8 Province Mean | 71.1 | 68.8 | 73.5 |
Discussion
We note well known caveats about representativeness of donors, and also that at this stage of the epidemic there is an increasing incidence of reinfection. In this study we did not detect antibodies developed due to vaccination.
For the present purposes, we do not offer any substantial interpretation of these results, but trust that they will be of interest and use to modellers, policy makers and others.
More resource intensive surveillance, notably defined by:
More frequent rounds of sampling
Multi-assay testing algorithms to distinguish vaccine induced antibodies from antibodies produced by natural infection
Sequencing
would potentially be significantly more informative.
Acknowledgements
The authors would like to thank the community of South African blood donors, whose voluntary provision of blood daily saves lives, and whose participation in studies enables highly efficient timely research. We also thank many colleagues in the blood services, for their efforts to execute this research in addition to their daily responsibilities, and colleagues at the National Institute of Communicable Diseases, for ongoing discussions which inform the data collection and analysis.
Funding for the operational activities was provided by the South African National Blood Service and in part supported by the South African Medical Research Council with funds received from the Department of Science and Innovation. The time of investigators in the blood services is supported by the blood services. Karin van den Berg and Marion Vermeulen are also supported by the NIH Fogarty International Center training grant 1D43-TW010345. Alex Welte and Laurette Mhlanga are supported by a Centre of Excellence grant from the South African Department of Science and Innovation via the National Research Foundation (Any opinion, finding, and conclusion or recommendation expressed in this material is that of the authors, and the NRF does not accept any liability in this regard). Eduard Grebe is supported by internal funding from Vitalant Research Institute, San Francisco.
Footnotes
Conflicts of Interest
The Authors have no conflicts of interest to declare
References
- 1.Sykes W, Mhlanga L, Swanevelder R, Glatt TN, Grebe E, Coleman C, Pieterson N, Cable R, Welte A, van den Berg K, Vermeulen M Prevalence of anti-SARS-CoV-2 antibodies among blood donors in Northern Cape, KwaZulu-Natal, Eastern Cape, and Free State provinces of South Africa in January 2021 Preprint DOI: 10.21203/rs.3.rs-233375/v1 [DOI] [Google Scholar]
- 2.Vermeulen M, Mhlanga L, Sykes W, Coleman C, Pieterson N, Cable R, Swanevelder R, Glatt TN, Grebe E, Welte A, van den Berg K; Prevalence of anti-SARS-CoV-2 antibodies among blood donors in South Africa during the period January-May 2021. Preprint DOI: 10.21203/rs.3.rs-690372/v2 [DOI] [Google Scholar]
- 3.Mhlanga L, Vermeulen M, Grebe E, Welte A SARS CoV 2 Infection Fatality Rate Estimates for South Africa Preprint DOI: 10.21203/rs.3.rs-707813/v2 [DOI] [Google Scholar]
- 4.Stone M, Grebe E, Sulaeman H, Di Germanio C, Dave H, Kelly K, Biggerstaff B, Crews B O., Tran N, Jerome KR, Denny TN, Hogema B, Destree M, Jones JM, Thornburg N, Simmons G, Krajden M, Kleinman S, Dumont LJ, Busch MP Evaluation of commercially available high-throughput SARS-CoV-2 serological assays for serosurveillance and related applications Preprint DOI: 10.1101/2021.09.04.21262414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Glatt TN, Hilton C, Nyoni C, Swarts A, Swanevelder R, Cowley J, Mmenu C, Moyo-Gwete T, Moore PL, Kutama M, Jaza J, Phayane I, Brits T, Koekemoer J, Jentsch U, Nelson D, van den Berg K, Vermeulen M Rapid and Successful Implementation of a COVID-19 Convalescent Plasma Programme—The South African Experience Viruses 2021, 13, 2050. 10.3390/v13102050 [DOI] [PMC free article] [PubMed] [Google Scholar]