Abstract
Secreted protein, acidic and rich in cysteine (SPARC, also known as osteonectin), is a small molecule glycoprotein associated with cell secretions. The purpose of our research is to clarify the clinicopathological and prognostic significance of SPARC expression in breast cancer. In this study, we performed a meta-analysis and bioinformatics analysis using the PubMed, Web of Science, Wanfang Data, and CNKI databases. The meta-analysis showed that SPARC expression was elevated in breast cancer tissue, compared with normal tissue, while SPARC expression in tumor stromal cells was higher than that of tumor cells. The expression of SPARC was positively correlated with histological grade and TNM staging. The Kaplan-Meier plotter showed that low SPARC expression was negatively correlated with the overall, postprogression, and distant metastasis survival rates of patients. According to Oncomine database, SPARC expression was upregulated in breast cancer than normal tissues. In TCGA database, univariate analysis showed that lymph node metastasis, distant metastasis, and TNM staging were negatively correlated with patient prognosis in breast cancers. Cox multivariate analysis showed that age, lymph node metastasis, distant metastasis, and TNM staging were important factors affecting the survival time of breast cancer patients. SPARC expression can be employed as a good indicator of prognosis of breast cancer patients, which will provide new methods and ideas of preventive treatment.
1. Introduction
Secreted protein, acidic and rich in cysteine (SPARC, also known as osteonectin), is a small molecule glycoprotein associated with cell secretions [1]. The SPARC gene is located on human chromosome Sq31.3-q32 and contains 10 exons, while the protein contains 298-304 amino acids. SPARC contains three highly conserved domains: the amino-terminal acidic calcium ion domain, the copper ion region homologous to the follicular dormancy hormone, and the extracellular calcium ion region [2, 3]. Osteopontin (SPARC) is involved in embryonic development, tissue repair, and cell regeneration. SPARC can regulate cell adhesion and cell proliferation through different signaling pathways and is a highly conserved extracellular interstitial protein. Its main functions are to prevent cell adhesion, regulate cell differentiation, prevent the spreading of cells, inhibit cell response to specific growth factors, regulate extracellular matrix and matrix metalloproteinase production, and influence neovascularization [4, 5]. Many of the biological functions of SPARC are stimulated by interactions with other proteins. Interactions with different proteins can produce a range of functional activities leading to diverse SPARC functions [6]. For example, SPARC participates in the regulation of the extracellular matrix. Its interaction with collagen affects the remodeling of connective tissue.
Additionally, glycoprotein and hyaluronectin contain the same expression site as SPARC, but the two proteins produce opposite effects on cell adhesion and are also associated with tissue remodeling [7]. SPARC can directly bind to vascular endothelial growth factor (VEGF) to inhibit the vascular endothelial growth factor pathway, preventing vascular endothelial growth factor and its receptor from binding to each other [8]. At the same time, SPARC can also bind to platelet-derived growth factor PDGF to indirectly inhibit angiogenesis by downregulating matrix metalloproteinases (MMPs) and transforming growth factor β1 antibodies (TGF-β1), which in turn inhibits tumor invasion and metastasis [9, 10]. Abnormal methylation of the CpG island of the promoter region of the SPARC gene can inhibit SPARC expression [11].
Abnormal methylation of the SPARC gene promoter region that leads to gene expression silencing has been observed in primary pancreatic cancer. SPARC mRNA is expressed in nonneoplastic pancreatic ductal epithelial cells but is not found in pancreatic cancer cell lines, which indirectly indicates that the silencing of the SPARC gene can lead to the development of pancreatic cancer [12, 13]. These findings suggest that the abnormal methylation of the CpG 2 region may be a suitable marker that can be used for the preliminary screening of early pancreatic cancer. SPARC increases the level of phosphorylation of AKT in gliomas through the PI3K/AKT pathway, significantly inhibiting EGF activity in ovarian cancer [14], and can activate GSK3β targets in adipocytes [15]. In mesangial cells, SPARC can enhance the activity of TGF-β, which leads to an increase in JNK activation and c-Jun phosphorylation [16]. In the Wnt pathway, SPARC can activate ILK, thereby phosphorylating its downstream in GSK-3B target. Phosphorylation of this target can lead to β-catenin aggregation and ultimately TCF4 activation. This pathway can also inhibit the expression of laminin in melanocytes [17, 18].
Previous research has shown that SPARC is closely associated with tumor development and plays a vital role in tumor invasion and metastasis [19]. SPARC expression is elevated in melanoma, glioma, meningioma, kidney cancer, and prostate cancer [20–23]. High level of SPARC expression enhanced tumor invasion and metastasis, leading to a poor prognosis of patients. In our study, we performed a meta-analysis and bioinformatics analysis to confirm the relationship between SPARC mRNA expression and the clinicopathological factors of breast cancer.
2. Materials and Methods
2.1. Static Search and Data Extraction
Articles were searched in PubMed, Web of Science, Wanfang Data, and CNKI databases (May 2020) using the key words: SPARC and breast and cancer or carcinoma or tumor. Inclusion criteria for studies included (1) breast cancer patients; (2) expression of SPARC was detected by immunohistochemistry; (3) articles contain SPARC expression and clinicopathological parameters; (4) all patients did not receive chemotherapy or radiotherapy before surgery. Exclusion criteria included (1) abstracts, case reports, reviews, and meeting notes; (2) repeat publications; (3) unclear diagnosis.
2.2. Data Extraction and Quality Assessment
As shown in Table 1, the information of eligible publications was extracted by two reviewers (Shi S and Zhang ZG) and included name of the first author, year of publication, patients' country, antibody company, number of cases and controls, risks for cancer, and follow-up outcomes. According to the Newcastle Ottawa Oncomine Scale (NOS; ohri.ca/programs/clinical_epidemiology/oxford.htm), the quality of the studies was independently assessed by two reviewers. The methods consists sample selection, comparability, and ascertainment of outcomes.
Table 1.
Main characteristics of eligible studies.
| First author | Year | Country | Ethnicity | Antibody supplier | Cases | Ctr | Risk to cancer | Outcome | Quality | Reference |
|---|---|---|---|---|---|---|---|---|---|---|
| Cui K | 2017 | China | 65 | 72 | Increased | 8 | 24 | |||
| Xu XD | 2014 | China | UK | Abcam | 255 | Negative | 7 | 25 | ||
| Zhou QF | 2020 | China | UK | Abcam | 150 | 7 | 26 | |||
| Chen F | 2017 | China | USA | Cell Signaling | 122 | Negative | 7 | 27 | ||
| Yan C | 2016 | China | 63 | 31 | Increased | 8 | 28 | |||
| Chen Y | 2018 | China | China | Bioss | 70 | 20 | Increased | Negative | 8 | 29 |
| Gao LL | 2015 | China | China | Bioss | 60 | 15 | Increased | 8 | 30 | |
| Zhang XM | 2008 | China | USA | Santa | 61 | 32 | Increased | 8 | 31 | |
| Lindner JL | 2014 | German | UK | Novocastra | 667 | 8 | 32 | |||
| Ma JJ | 2017 | China | USA | Cell Signaling | 7 | 33 | ||||
| Zhu AJ | 2016 | China | USA | Thermo | 211 | 7 | 34 | |||
| Guo W | 2017 | China | UK | Abcam | 88 | 8 | 35 | |||
| Witkiewicz AK | 2010 | USA | Denmark | Dako | 7 | 36 | ||||
| Watkins G | 2005 | UK | USA | Santa | Negative | 7 | 37 | |||
| Barth PJ | 2005 | German | UK | Novocastra | 25 | 25 | Increased | 8 | 38 | |
| Sun XY | 2015 | China | China | Bioss | 70 | 20 | Increased | 8 | 39 | |
| Liu XM | 2012 | China | China | Bioss | 65 | 20 | Increased | 8 | 40 | |
| Zhang SQ | 2016 | China | China | Bioss | 92 | 30 | Increased | Negative | 8 | 41 |
| Sun XY | 2014 | China | China | Bioss | 70 | 20 | Increased | 8 | 42 |
2.3. Bioinformatics Analysis
The prognostic value of SPARC mRNA expression in breast cancer was analyzed using a Kaplan-Meier plotter (http://www.kmplot.com). Expression of SPARC was associated with overall survival (OS), relapse-free survival (RFS), distant metastasis-free survival (DMFS), and postprogression survival (PPS) for all patients. The expression of SPARC was associated with clinicopathological features. SPARC gene expression was analyzed using the Oncomine database (http://www.oncomine.org), an extensive database of tumor chip data, including gene chip and gene expression data. The database can be used to analyze gene expression differences and classify the clinical information of tumor patients. Differences in SPARC expression at mRNA level were compared between carcinoma and normal tissues. Data on gene expression and the clinical pathology of SPARC were downloaded from the cancer genome atlas (TCGA, http://www.cancer.gov) database using the TCGA-assembler of R software. The letter code of breast cancer is BRCA. We organized the data and analyzed the mRNA expression of SPARC in breast cancer. At the same time, we analyzed the clinicopathological data and prognosis of tumor patients. Cox risk regression models were used to conduct univariate and multivariate analyses. This model analyzed the effect of risk factors, the hazard ratio (HR), and 95% confidence interval (CI).
2.4. Statistical Analysis
Revman version 5.3 was used for the data analysis. The results of the comparison between the case group and the control group were expressed as an odds ratio (OR) and 95% CI. I2 statistics were used to determine the heterogeneity between the research results. If a significant level of heterogeneity was found, a fixed-effect model (I2 < 50%, P > 0.10, Mantel-Haenszel method) was used; otherwise, a random effect model (I2 ≥ 50%, P ≤ 0.10, Der Simonian and Laird method) was used. Publication bias was evaluated using a funnel plot, and funnel plot asymmetry was quantified using Begg's test and Egger's test. Cox risk regression models were used for the univariate and multivariate analyses. This model analyzed the effect of risk factors, the hazard ratio, and 95% CI. A P value of <0.05 was considered to indicate a statistically significant difference. All data analyses were conducted using SPSS 19.0 software.
3. Results
3.1. Study Selection and Characteristics
As shown in Figure 1 and Table 1, a total of 20 articles that analyzed the relationship between SPARC expression and the clinicopathological characteristics of breast cancer were identified [24–44]. However, only 10 of these articles contained an analysis of normal breast tissues [24, 28–31, 38–42]. Data on the clinicopathological characteristics of breast cancer included histological grade, TNM staging, lymph node metastasis, menopausal status, tumor size, and the presence of ER, PR, and HER2 (Table 2). Finally, only 4 articles were found to include the prognostic features of SPARC expression and its relationship with breast cancer [25, 27, 29, 37].
Figure 1.
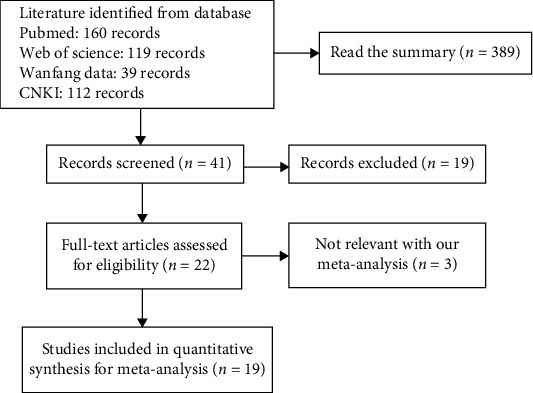
Flow diagram of article selection.
Table 2.
Results of meta-analysis of the correlation between SPARC expression and clinical pathological features of breast cancer.
| Clinicopathological features | Heterogeneity | Test for overall effect | ||
|---|---|---|---|---|
| I 2 (%) | P value | Odds ratio (95% CI) | P value | |
| Histological grade | 45 | 0.08 | 0.66 (0.43-1.00) | 0.05∗ |
| TNM staging | 61 | <0.01 | 0.47 (0.31-0.71) | <0.01∗ |
| Lymph node metastasis | 85 | <0.01 | 0.52 (0.25-1.05) | 0.07 |
| Menopausal status | 0 | 0.49 | 1.03 (0.76-1.40) | 0.85 |
| Size | 0 | 0.92 | 0.86 (0.67-1.12) | 0.27 |
| ER | 67 | <0.01 | 0.98 (0.59-1.63) | 0.94 |
| PR | 27 | 0.17 | 0.78 (0.60-1.02) | 0.07 |
| HER2 | 0 | 0.45 | 1.08 (0.84-1.37) | 0.56 |
| Overall survival | 63 | 0.05 | 1.27 (0.86-1.89) | 0.23 |
| SPARC tumor cell | 74 | <0.01 | 8.74 (4.11-18.58) | <0.01∗ |
| SPARC stromal cell | 65 | 0.02 | 0.18 (0.10-0.33) | <0.01∗ |
TNM: tumor node metastasis; ER: estrogen receptor; PR: progesterone receptor; HER2: human epidermal growth factor receptor-2.
3.2. Forest Plot of OR for the Association between SPARC Expression and the Clinicopathological Characteristics of Breast Cancer
A total of 10 articles that included data on 571 breast cancer patients and 265 normal controls were found. The expression of SPARC was upregulated in breast cancer tissue compared with normal tissues (Figure 2). Our meta-analysis showed that SPARC expression was associated with TNM staging and histological grade (Table 2). The expression of SPARC was also upregulated in breast stromal cells, compared with tumor cells (Table 2).
Figure 2.
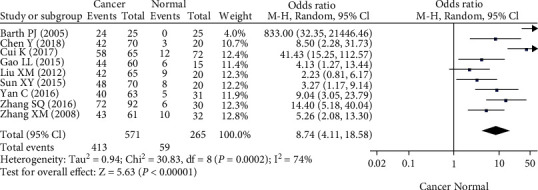
Forest plot of the expression of SPARC in breast cancer. Plots of the association between cancer and normal mucosa.
3.3. Publication Bias
As shown in Figure 3, the heterogeneity between studies was tested using funnel diagrams. Each study was removed from the pooled analysis to assess the impact of each individual study on the aggregated results using a sensitivity analysis. Egger's test results showed that there was no apparent publication bias in this meta-analysis.
Figure 3.
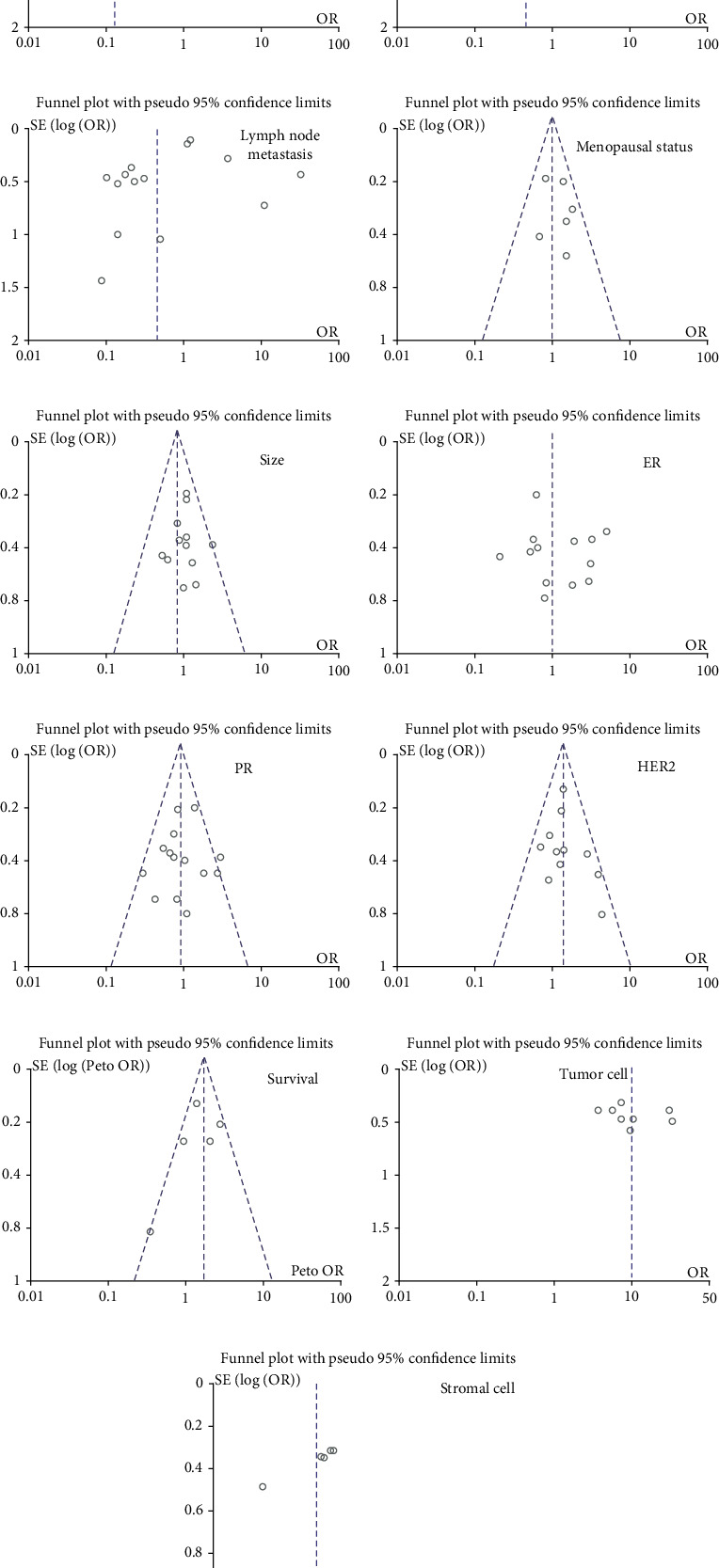
Funnel plot for testing publication bias between SPARC expression and breast cancer. Publication bias was also tested between SPARC expression and clinicopathological features of breast cancer, including (a) histological grade, (b) TNM staging, (c) lymph node metastasis, (d) Menopausal status, (e) size, (f) ER, (g) PR, (h) HER2, and (i) survival. Additionally, publication bias was analyzed based on risk degrees of SPARC expression in (a) tumor cell and (b) stromal cell.
3.4. The Relationship between SPARC Expression and the Bioinformatics Features of Breast Cancer
The Kaplan-Meier plotter was used to find that lower SPARC expression was negatively correlated with the overall survival rate of grade I/II, Her2+, luminal A, wild type patients, the postprogression survival rate of LN+, wild type patients, and the distant metastasis survival rate of wild-type patients (Figure 4, P < 0.05). Elevated SPARC expression was positively correlated with the relapse-free survival rate of patients, even when stratified as grade I/II and luminal A patients, but an opposite result was obtained when stratified as Her2+, ER patients. ER, PR, or luminal B patients and elevated SPARC expression produced a shorter distant metastasis survival rate, compared with a lower expression level (Figure 4, P < 0.05). Based on the TCGA analysis, as well as the databases published by Ma, Radvanyi, Zhao, Curtis, Richardson, Turashvil, Final, and Karnoub, we found that SPARC expression was lower in breast tissues than in invasive or ductal breast carcinoma, invasive lobular, ductal or mixed breast carcinoma, and breast phyllodes tumors. Elevated SPARC expression was found in invasive ductal or lobular breast carcinomas, compared with ductal or lobular breast carcinomas (Figure 5, P < 0.05). The Cox univariate analysis of TCGA data showed that age, TNM staging, lymph node metastasis, and distant metastasis were negatively correlated with patient prognosis (Table 3, P < 0.05). The Cox multivariate analysis showed that age, TNM staging, lymph node metastasis, and distant metastasis found to be risk factors that for breast cancer patient prognosis (Table 4, P < 0.05).
Figure 4.
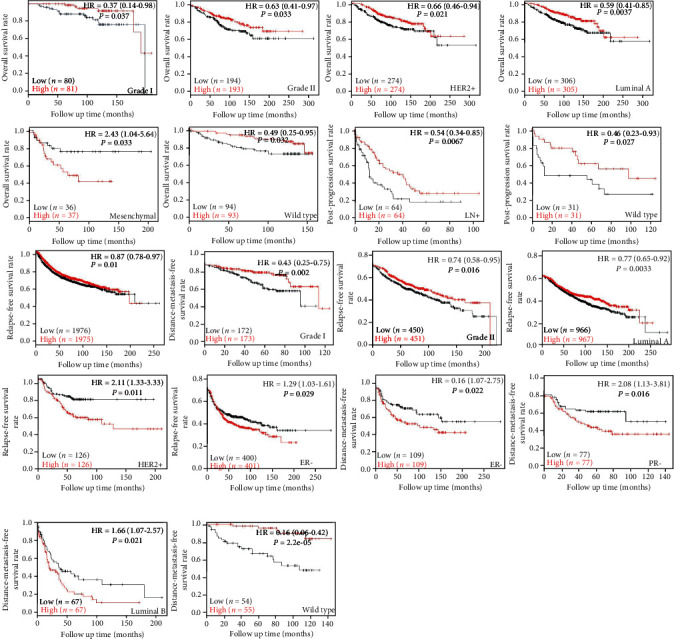
Prognostic value of SPARC mRNA expression in breast cancer patients according to KM-plotter (http://www.kmplot.com).
Figure 5.
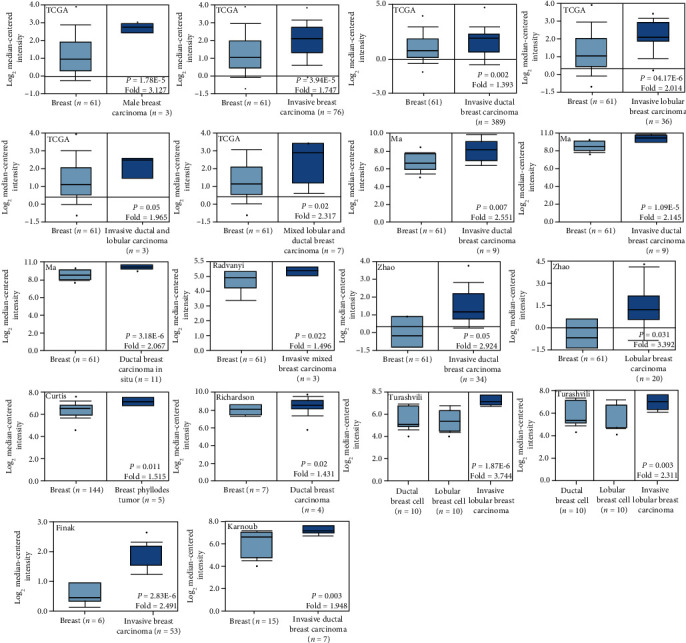
Prognostic value of SPARC mRNA expression in breast cancer patients according to Oncomine database (http://www.oncomine.org).
Table 3.
Univariate analysis of prognostic risk factors in the patients with breast cancer.
| Characteristics | Patients (%) | Relative risk (95% CI) | P value |
|---|---|---|---|
| Sex | |||
| Female | 1065 (98.9) | 0.852 (0.119-6.102) | 0.873 |
| Male | 12 (1.1) | ||
| Age(years) | |||
| <60 | 599 (56.0) | 0.516 (0.371-0.719) | <0.001∗ |
| ≥60 | 470 (44.0) | ||
| TNM staging | |||
| I-II | 792 (73.4) | 0.384 (0.272-0.543) | <0.001∗ |
| III-IV | 259 (24.6) | ||
| Depth of invasion | |||
| - | 281 (26.2) | 0.734 (0.497-1.084) | 0.120 |
| + | 792 (73.8) | ||
| Lymph node metastasis | |||
| - | 504 (47.6) | 0.468 (0.352-0.672) | <0.001∗ |
| + | 555 (52.4) | ||
| Distant metastasis | |||
| - | 893 (97.6) | 0.208 (0.124-0.349) | <0.001∗ |
| + | 22 (2.4) |
CI: confidence interval; TNM: tumor node metastasis.
Table 4.
Multivariate analysis of clinicopathological variables for the survival of the patients with breast cancer.
| Clinicopathological parameters | Relative risk (95% CI) | P |
|---|---|---|
| SPARC expression (+) | 0.855 (0.597-1.223) | 0.390 |
| Age (≥60 years) | 2.070 (1.425-3.007) | <0.001∗ |
| Sex (female) | 1.753 (0.242-12.705) | 0.578 |
| Depth of invasion (T2-4) | 1.123 (0.709-1.778) | 0.622 |
| Lymph node metastasis (+) | 1.622 (1.026-2.563) | 0.038∗ |
| Distant metastasis (+) | 2.547 (1.310-4.950) | 0.006∗ |
| TNM staging (III–IV) | 1.707 (1.063-2.742) | 0.027∗ |
CI: confidence interval; TNM: tumor node metastasis.
4. Discussion
SPARC acts as an antiadhesion protein to regulate growth factors and matrix proteases. SPARC can counteract the effect of β-FGF in promoting cell proliferation, migration, and mediating angiogenesis, while it can also inhibit β-FGF receptor autophosphorylation and ERK 1/2 activation [43]. Additionally, SPARC can inhibit VEGF-mediated endothelial cell proliferation and directly bind to PDGF-B and interfere with its binding to fibroblast receptors [44, 45]. TGF-β can mediate the production of SPARC proteins. With low levels of TGF-β, expression levels have been found in the glomerular mesangial cells of SPARC knockout mice [3]. SPARC can mediate the expression of MMP-1 and MMP-9 in peripheral blood monocytes and the expression of MMP-1, MMP-3, and MMP-9 in fibroblasts [46].
Studies have found that SPARC is mainly expressed in mesenchymal cells in gastric cancer tissue. The expression of SPARC was negatively correlated with differentiation, Lauren classification, lymph node metastasis, and clinical stage, while lymph node metastasis was an independent prognostic factor for patients with gastric cancer [47–49]. Sato et al. found that SPARC expression at mRNA level in cancer tissues was significantly higher than that of normal adjacent tissues [50]. Previous research has shown that SPARC methylation occurs at a high rate in gastric cancer tissues and that promoter DNA methylation can inhibit SPARC expression in gastric cancer cells [51]. SPARC was also highly expressed in esophageal and liver cancer tissues and was closely related to the degree of malignancy, but its expression was low in pancreatic and colon cancer tissues [13, 15, 52, 53]. SPARC expression was significantly lower in ovarian cancer tissues than in normal tissues and in patients with a poorly differentiated and larger omentum [54]. SPARC expression could inhibit the production of interleukin-6 in ovarian cancer tissues and decrease levels of peritoneal metastasis caused by ovarian cancer. SPARC could also block the transformation of vascular endothelial cells from the G1 phase to the S phase and induce the apoptosis and migration of vascular endothelial cells [55, 56]. Similar results were observed in endometrial cancer but not in cervical cancer [57, 58]. SPARC expression was also higher in lung squamous cell carcinoma than in lung adenocarcinoma. SPARC was found to be synthesized and secreted by tumor stromal cells [59], and its expression was associated with an acidic environment and the necrosis of tumor tissues, as its expression levels were higher in tumor necrosis areas [60]. The results of multivariate and univariate analyses demonstrated the prognostic value of SPARC expression in determining the overall survival rate [59].
SPARC protein expression was significantly associated with interstitial remodeling, the loss of CD34, and α-SMA expression in invasive ductal carcinoma and interfered with TGF-β1 signaling, which allowed it to play a role in tumor progression [38]. SPARC was highly expressed in breast cancer tissues and was associated with TNM staging and lymph node metastasis. The Cox analysis showed that TNM staging and lymph node metastasis were risk factors that affected the prognosis of patients. RT-PCR results showed that SPARC was highly expressed at the mRNA level in breast cancer tissues [61, 62]. Our research results also elevated that high SPARC expression was associated with TNM staging and histological grade. The univariate analysis showed that age, TNM staging, lymph node metastasis, and distant metastasis were associated with a poor prognosis in breast cancer patients. The analysis conducted using the Cox proportional hazard regression model showed that age, TNM staging, lymph node metastasis, and distant metastasis are essential factors that affect the survival time of breast cancer patients.
SPARC expression at protein and mRNA levels showed opposite trends in breast cancer. The mRNA level expression of a particular gene does not necessarily have a linear relationship with the expression level of its translated product protein due to several reasons. First, gene expression is regulated at various levels, and regulation at the transcription level is only an intermediate link. Second, posttranscriptional translation and posttranslational regulation all contribute to the expression of the final protein. Finally, the mRNA degradation, protein degradation, and modified folding may cause inconsistencies between mRNA and protein expression levels of a given protein.
5. Conclusion
SPARC plays a complex role in tumorigenesis and development. At the same time, SPARC expression is upregulated in breast cancer patients. SPARC is positively related with TNM staging and histological grade of breast cancer patients. SPARC expression can be employed as a good marker for the prognosis of patients with cancers, which will provide new methods and ideas for preventive treatment.
Conflicts of Interest
The authors declare that they have no competing interests.
References
- 1.Termine J. D., Kleinman H. K., Whitson S. W., Conn K. M., McGarvey M. L., Martin G. R. Osteonectin, a bone-specific protein linking mineral to collagen. Cell . 1981;26(1):99–105. doi: 10.1016/0092-8674(81)90037-4. [DOI] [PubMed] [Google Scholar]
- 2.Chlenski A., Cohn S. L. Modulation of matrix remodeling by SPARC in neoplastic progression. Seminars in Cell & Developmental Biology . 2010;21(1):55–65. doi: 10.1016/j.semcdb.2009.11.018. [DOI] [PubMed] [Google Scholar]
- 3.Brune K., Hong S. M., Li A., et al. Genetic and epigenetic alterations of familial pancreatic cancers. Cancer Epidemiology and Prevention Biomarkers . 2008;17(12):3536–3542. doi: 10.1158/1055-9965.EPI-08-0630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang W. J., Mei C. L. Research progress of SPARC. Chinese Journal of Clinical Medicine . 2004;5:65–68. [Google Scholar]
- 5.Schellings M. W. M., Vanhoutte D., Swinnen M., et al. Absence of SPARC results in increased cardiac rupture and dysfunction after acute myocardial infarction. Journal of Experimental Medicine . 2009;206(1):113–123. doi: 10.1084/jem.20081244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gaillard O., Lebon P., Delattre J. Bidirectional signaling between the cytoskeleton and integrins. Current Opinion in Cell Biology . 1999;11(2):274–286. doi: 10.1016/S0955-0674(99)80037-4. [DOI] [PubMed] [Google Scholar]
- 7.Yan Q., Sage E. H. SPARC a matricellular glycoprotein with important biological functions. Journal of Histochemistry & Cytochemistry . 1999;47(12):1495–1505. doi: 10.1177/002215549904701201. [DOI] [PubMed] [Google Scholar]
- 8.Bradshaw A. D. Diverse biological functions of the SPARC family of proteins. International Journal of Biochemistry and Cell Biology . 2012;44(3):480–488. doi: 10.1016/j.biocel.2011.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Raines E. W., Lane T. F., Iruela-Arispe M. L., Ross R., Sage E. H. The extracellular glycoprotein SPARC interacts with platelet-derived growth factor (PDGF)-AB and -BB and inhibits the binding of PDGF to its receptors. Proceedings of the National Academy of Sciences . 1992;89(4):1281–1285. doi: 10.1073/pnas.89.4.1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lau C., Poon R., Cheung S., Yu W. C., Fan S. T. SPARC and Hevin expression correlate with tumour angiogenesis in hepatocellular carcinoma. Journal of Pathology . 2006;210(4):459–468. doi: 10.1002/path.2068. [DOI] [PubMed] [Google Scholar]
- 11.Nagaraju G. P., EI-Rayes B. F. SPARC and DNA methylation: possible diagnostic and therapeutic implications in gastrointestinal cancers. Cancer Letters . 2013;328(1):10–17. doi: 10.1016/j.canlet.2012.08.028. [DOI] [PubMed] [Google Scholar]
- 12.Gao A., Zuo X., Liu Q. G., Lu X., Guo W., Tian L. Methylation of PARP-1 promoter involved in the regulation of benzene-induced decrease of PARP-1 mRNA expression. Toxicology Letters . 2010;195(2-3):114–118. doi: 10.1016/j.toxlet.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 13.Sato N., Fukushima N., Maehara N., et al. SPARC/osteonectin is a frequent target for aberrant methylation in pancreatic adenocarcinoma and a mediator of tumor-stromal interactions. Oncogene . 2003;22(32):5021–5030. doi: 10.1038/sj.onc.1206807. [DOI] [PubMed] [Google Scholar]
- 14.Nie J., Chang B., Traktuev D. O., et al. IFATS collection: combinatorial peptides identify α5β1 integrin as a receptor for the matricellular protein SPARC on adipose stromal cells. Stem Cells . 2008;26(10):2735–2745. doi: 10.1634/stemcells.2008-0212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang E., Kang H. J., Koh K. H., Rhee H., Kim N. K., Kim H. Frequent inactivation of SPARC by promoter hypermethylation in colon cancers. International Journal of Cancer . 2007;121(3):567–575. doi: 10.1002/ijc.22706. [DOI] [PubMed] [Google Scholar]
- 16.Tang M. J., Tai I. T. A novel interaction between procaspase 8 and SPARC enhances apoptosis and potentiates chemotherapy sensitivity in colorectal cancers. Journal of Biological Chemistry . 2007;282(47):34457–34467. doi: 10.1074/jbc.M704459200. [DOI] [PubMed] [Google Scholar]
- 17.Cheetham S., Tang M. J., Mesak F., Kennecke H., Owen D., Tai I. T. SPARC promoter hypermethylation in colorectal cancers can be reversed by 5-Aza-2′deoxycytidine to increase SPARC expression and improve therapy response. British Journal of Cancer . 2008;98(11):1810–1819. doi: 10.1038/sj.bjc.6604377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Prada F., Benedetti L. G., Bravo A. I., Alvarez M. J., Carbone C., Podhajcer O. L. SPARC endogenous level, rather than fibroblast-produced SPARC or stroma reorganization induced by SPARC, is responsible for melanoma cell growth. Journal of Investigative Dermatology . 2007;127(11):2618–2628. doi: 10.1038/sj.jid.5700962. [DOI] [PubMed] [Google Scholar]
- 19.Massi D., Franchi A., Borgognoni L., Reali U. M., Santucci M. Osteonectin expression correlates with clinical outcome in thin cutaneous malignant melanomas. Human Pathology . 1999;30(3):339–344. doi: 10.1016/S0046-8177(99)90014-X. [DOI] [PubMed] [Google Scholar]
- 20.Schultz C., Lemke N., Ge S. Secreted protein acidic and rich in cysteine promotes glioma invasion and delays tumor growth in vivo. Cancer Research . 2002;62:6270–6277. [PubMed] [Google Scholar]
- 21.Rempel S. A., Ge S. G., Gutierrez J. A. SPARC: a potential diagnostic marker of invasive meningiomas. Clinical Cancer Research . 1999;5(2):237–241. [PubMed] [Google Scholar]
- 22.Nishie A., Masuda K., Otsubo M., et al. High expression of the Cap 43 gene in infiltrating macrophages of human renal cell carcinomas. Clinical cancer research . 2001;7(7):2145–2151. [PubMed] [Google Scholar]
- 23.Thomas R., True L. D., Bassuk J. A., Lange P. H., Vessella R. L. Differential expression of osteonectin/SPARC during human prostate cancer progression. Clinical cancer research an official journal of the american association for cancer research. 2000;6(3):1140–1149. [PubMed] [Google Scholar]
- 24.Cui K., Li B. Y. The relationship between the expression level of SPARC and the occurrence, development, invasion and metastasis of breast cancer. Journal of Hunan Normal University . 2017;14:57–60. [Google Scholar]
- 25.Xu X. D., Xu L., Li Y. J., Li Z. H., Li Z., Teng Y. E. Expression and clinical significance of SPARC protein in breast cancer. Journal of China Medical University . 2014;43:493–498. [Google Scholar]
- 26.Zhou Q. F., Yue S. L., Qi S. Q., Zhao Z. Z., Su Y., Lin Y. Effects of secreted acidic protein and androgen receptor rich in cysteine on the prognosis of patients with triple negative breast cancer. Modern Practical Medicine . 2020;32:180–182. [Google Scholar]
- 27.Chen F., Zhu L., Chen H., Chen S. Z., Xu Y. H. Clinical significance of secreted protein acidic and rich in cysteine expression in breast cancer tissue. The Chinese Journal of Clinical Pharmacology . 2017;33:18–20. [Google Scholar]
- 28.Yan C., Hong W. Observation of SPARC protein expression in breast cancer. Shandong Medical Journal . 2016;56:63–64. [Google Scholar]
- 29.Chen Y., Liu S. Z., Zhang P. The expression of SPARC and Notch-1 in breast cancer and their clinical significanceS. Journal of Hubei University for Nationalities·Medical Edition . 2018;35:14–18. [Google Scholar]
- 30.Gao L. L., Yu G. H., Zhang J. M. Expression and significance of SIRT1 and SPARC in breast invasive ductal carcinoma tissues. China Medical Herald . 2015;12:16–18. [Google Scholar]
- 31.Zhang X. M., Chen J. W., Hu H. H., Lu G. Z., Yang Z. R. Expression of SPARC in invasive ductal carcinoma of breast. Journal of Shanghai Jiaotong University . 2008;28:1445–1448. [Google Scholar]
- 32.Lindner J. L., Loibl S., Denkert C., et al. Expression of secreted protein acidic and rich in cysteine (SPARC) in breast cancer and response to neoadjuvant chemotherapy†. Annals of Oncology . 2015;26(1):95–100. doi: 10.1093/annonc/mdu487. [DOI] [PubMed] [Google Scholar]
- 33.Ma J. J., Gao S., Xie X. J., et al. SPARC inhibits breast cancer bone metastasis and may be a clinical therapeutic target. Oncology Letters . 2017;14(5):5876–5882. doi: 10.3892/ol.2017.6925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhu A. J., Yuan P., Du F., Hong R. X., Ding X. Y., Shi X. Q. SPARC overexpression in primary tumors correlates with disease recurrence and overall survival in patients with triple negative breast cancer. Oncotarget . 2016;7(47):76628–76634. doi: 10.18632/oncotarget.10532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guo W., Zhang M., Chen Y., Gao S. Y. The clinical significance of secreted protein acidic and rich in cysteine expression in breast cancer tissue and its association with prognosis. Journal of Cancer Research & Therapeutics . 2017;13(5):833–836. doi: 10.4103/jcrt.JCRT_424_17. [DOI] [PubMed] [Google Scholar]
- 36.Witkiewicz A. K., Freydin B., Chervoneva I., et al. Stromal CD10 and SPARC expression in ductal carcinoma in situ (DCIS) patients predicts disease recurrence. Cancer Biology & Therapy . 2010;10(4):391–396. doi: 10.4161/cbt.10.4.12449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Watkins G., Douglas-Jones A., Bryce R., Mansel R. E., Jiang W. G. Increased levels of SPARC (osteonectin) in human breast cancer tissues and its association with clinical outcomes. Prostaglandins leukotrienes & essential fatty acids . 2005;72(4):267–272. doi: 10.1016/j.plefa.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 38.Barth P. J., Moll R., Ramaswamy A. Stromal remodeling and SPARC (secreted protein acid rich in cysteine) expression in invasive ductal carcinomas of the breast. Virchows Archiv . 2005;446(5):532–536. doi: 10.1007/s00428-005-1256-9. [DOI] [PubMed] [Google Scholar]
- 39.Sun X. Y., Yu G. H., Zhang J. M. Correlation between SPARC and MMP-2 expression in breast cancer tissues. Chinese Journal of Cancer Prevention and Treatment . 2015;22:674–677. [Google Scholar]
- 40.Liu X. M., Yu G. H., Zhang J. M., Liu S. Z., Gao Y. F., Su F. Expression and significance of SPARC and VEGF in breast invasive ductal carcinoma tissues. Chinese Journal of Cancer Prevention and Treatment . 2012;19:1061–1065. [Google Scholar]
- 41.Zhang S. Q., Ma W. Expression of cysteine-rich secreted protein in breast cancer and its clinical significance. Maternal and Child Health Care of China . 2016;31:5157–5159. [Google Scholar]
- 42.Sun X. Y., Yu G. H., Zhang J. M. SPARC and Her-2's expression in breast cancer tissue. China Medicine and Pharmacy . 2014;4:18–21. [Google Scholar]
- 43.Socha M. J., Said N., Dai Y., et al. Aberrant promoter methylation of _Sparc_ in ovarian cancer. Neoplasia . 2009;11(2):p. 126-IN1. doi: 10.1593/neo.81146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Said N., Socha M. J., Olearczyk J. J., Elmarakby A. A., Imig J. D., Motamed K. Normalization of the ovarian cancer microenvironment by SPARC. Molecular Cancer Research . 2007;5(10):1015–1030. doi: 10.1158/1541-7786.MCR-07-0001. [DOI] [PubMed] [Google Scholar]
- 45.Mantoni T. S., Schendel R. R. E., Rödel F., et al. Stromal SPARC expression and patient survival after chemoradiation for non-resectable pancreatic adenocarcinoma. Cancer Biology & Therapy . 2008;7(11):1806–1815. doi: 10.4161/cbt.7.11.6846. [DOI] [PubMed] [Google Scholar]
- 46.Arnold S., Mira E., Muneer S., et al. Forced expression of MMP9 rescues the loss of angiogenesis and abrogates metastasis of pancreatic tumors triggered by the absence of host SPARC. Experimental Biology & Medicine . 2008;233(7):860–873. doi: 10.3181/0801-RM-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li Y., Wu J. F., Zhao W. D. Expression and significance of SPARC and MMP-9 in gastric cancer. Shandong Medical Journal . 2015;55:48–50. [Google Scholar]
- 48.Dong M. X., Yang Y. H., Yu J. J. Expression of SPARC in gastric cancer tissues and its significance. QILU YIXUE ZAZHI . 2011;26:105–110. [Google Scholar]
- 49.Yang M. L., Zhai L. L., Ma L. H. Relationship between expression of SPARC and VEGF with tumor angiogenesis in gastric carcinoma. Chinese Journal of Diagnostic Patholog . 2012;19:52–55. [Google Scholar]
- 50.Sato T., Oshima T., Yamamoto N., et al. Clinical significance of SPARC gene expression in patients with gastric cancer. Journal of Surgical Oncology . 2013;108(6):364–368. doi: 10.1002/jso.23425. [DOI] [PubMed] [Google Scholar]
- 51.Chen Z. Y., Zhang J. L., Yao H. X., et al. Aberrant methylation of the _SPARC_ gene promoter and its clinical implication in gastric cancer. Scientific Reports . 2015;4(1):p. 7035. doi: 10.1038/srep07035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Porte H., Triboulet J. P., Kotelevets L., et al. Overexpression of stromelysin-3, BM-40/SPARC, and MET genes in human esophageal carcinoma: implications for prognosis. Clinical Cancer Research . 1998;4(6):1375–1382. [PubMed] [Google Scholar]
- 53.Le B. B., Faouzi S., Boussarie L. Osteonectin/SPARC is overexpressed in human hepatocellular carcinoma. The Journal of Pathology . 1999;189(1):46–52. doi: 10.1002/(SICI)1096-9896(199909)189:1<46::AID-PATH392>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 54.Yan L. L., Cui Z. M., Zheng Y. Expression and significance of SPARC in epithelial ovarian tumors. Shandong Medical Journal . 2008;48:35–37. [Google Scholar]
- 55.Said N. A., Najwer I., Socha M. J., Fulton D. J., Mok S. C., Motamed K. SPARC inhibits LPA-mediated mesothelial--ovarian cancer cell crosstalk. Neoplasia . 2007;9(1):23–35. doi: 10.1593/neo.06658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chlenski A., Liu S. Q., Crawford S. E. SPARC is a key Schwannian-derived inhibitor controlling neuroblastoma tumor angiogenesis. Cancer Research . 2003;62:7357–7363. [PubMed] [Google Scholar]
- 57.Deng T., Zhou Q. Expression of SPARC in the squamous cervical carcinoma and its clinic significance. Journal of Chongqing Medical University . 2011;36:60–64. [Google Scholar]
- 58.Wang L., Cui Z. M., Zheng Y. Expression and significance of the SPARC protein in endometrial carcinoma. Progess in modern biomedicine . 2011;11:905–908. [Google Scholar]
- 59.Huang Y., Zhang J., Zhao Y.-Y., et al. SPARC expression and prognostic value in non-small cell lung cancer. Chinese Journal of Cancer . 2012;31(11):541–548. doi: 10.5732/cjc.012.10212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Koukourakis M. I., Giatromanolaki A., Brekken R. A., et al. Enhanced expression of SPARC/osteonectin in the tumor-associated stroma of non-small cell lung cancer is correlated with markers of hypoxia/acidity and with poor prognosis of patients. Cancer Research . 2003;63(17):5376–5380. [PubMed] [Google Scholar]
- 61.Chen Y., Liu S. Z., Zhang P. Expressions of SPARC and Notch-1 in breast cancer and their clinical significance. Journal of Hubei University for Nationalities . 2018;35:17–21. [Google Scholar]
- 62.Che Z. Q., Wang H., Qi J. Expression of SPARC and clinical significance in breast cancer. The Practical Journal of Cancer . 2005;20:120–122. [Google Scholar]


