Abstract
The human papillomavirus (HPV) vaccine is an important tool for cancer prevention. However, vaccination rates in Alabama, a state with high rates of HPV-related cancers, remain below the national average. Our objective was to develop a comprehensive assessment of HPV vaccination in our state, with the goal to make recommendations for tailored multilevel interventions. A multimodal approach with quantitative and qualitative data was used to determine barriers and facilitators to HPV vaccination in Alabama. This included a survey of pediatric care providers and structured interviews with pediatricians, parents, nurses and community stakeholders. Two separate investigators evaluated the interview transcripts for major themes that occurred in 65% or more interviews. Major barriers included lack of knowledge, concerns about vaccine safety, and the link between the HPV vaccine and sexuality. Qualitative interviews further revealed barriers such as misinformation received from the internet and parental vaccine hesitancy. Opportunities for increasing vaccination include parental education, establishment of a reminder system, increasing access to HPV vaccine providers, and education for providers. Additional facilitators revealed through interviews included: trust in physicians, using the internet or social media to propagate positive messaging, physicians and clinical staff education, utilizing existing technology more effectively, highlighting nurses’ roles as partners in HPV prevention, and the potential of schools as a venue for promotion of the vaccine. Our data are consistent with prior research showing major barriers to HPV vaccination. Several recommendations for optimizing HPV vaccination uptake in Alabama on the patient, provider and system level are given.
Keywords: Human papillomavirus, HPV, HPV vaccine, cervical cancer, cervical cancer prevention, oropharyngeal cancer, qualitative research
Introduction
Over 38,000 new cases of HPV-related cancers are diagnosed annually in the United States, including 12,000 cases of cervical cancer in women and over 15,000 cases of oropharyngeal cancer in men and women.1 Cervical cancer is the most common HPV-related cancer among women, and Southern states have some of the highest cervical cancer incidence and mortality rates. Recent data show that from 2004 to 2013 the cervical cancer incidence in Alabama was 8.5 cases/100,000, compared to the US rate of 7.7/100,000.2,3
Through greater understanding of the link between HPV and cancer, a preventive vaccine was developed with the potential to prevent more than 30,000 cases of HPV-related cancers every year in the US. 4–7 The Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) recommends HPV vaccination for all girls and boys ages 11 to 12, starting as early as 9 years old, 8 Despite overwhelming evidence of the safety and efficacy of this vaccine9, overall rates of vaccine series initiation and completion remain low in the US. In 2016, Alabama ranked 43rd for adolescent HPV vaccination rates.10 In the setting of these low vaccination rates, the University of Alabama at Birmingham Comprehensive Cancer Center obtained a supplement from the National Cancer Institute to identify gaps and opportunities in HPV vaccination. Through this several activities have been completed or are ongoing, including a comprehensive environmental scan to obtain a deeper understanding of barriers, facilitators, and solutions that can guide the development of multi-level public health interventions to promote HPV vaccine uptake. The purpose of this paper is to discuss the results of this assessment and to propose areas of opportunity moving forward.
Methods
Theoretical Framework
Barriers and facilitators to HPV vaccination exist at the system, provider and parent/patient levels.11,12 Therefore, the PRECEDE-PROCEED model was used for data collection, analysis and interpretation,13 with a focus on the PRECEDE (Predisposing, Reinforcing, and Enabling Constructs in Educational/Environmental Diagnosis and Evaluation) phase of the model. Predisposing factors involve the intrapersonal knowledge, beliefs and values that affect an individual’s healthcare decision-making. Enabling factors describe the structural, logistic or policy factors that are involved in HPV vaccination uptake. Reinforcing factors include the interpersonal, family or social influences on healthcare decision making. This model aided our team in performing an epidemiological and environmental assessment of the status of HPV vaccination in Alabama through multiple sources of data: examination of existing HPV vaccine data as well as original quantitative and qualitative data collection with different stakeholders. The PRECEDE-PROCEED model14 and multimodal research approaches15 have previously been used successfully in the development of cancer prevention programs and interventions.
Alabama HPV Vaccine Data
We examined state and national immunization rates from the Centers for Disease Control and Prevention (CDC) annual National Immunization Survey (NIS)-Teen. Additionally, the Alabama Department of Public Health (ADPH) provided data from the Immunization Patient Resources with Integrated Technology system (ImmPRINT) in order to examine rates at the local level, and to compare to CDC data. This system uses provider-level vaccination data to track children and adolescent vaccine doses. Utilization of this system is voluntary, and it is unknown what proportion of providers use it. We also queried physician license records through the Alabama Board of Medical Examiners (ALBME). We requested data on number of physicians licensed in family medicine, pediatrics and obstetrics/gynecology in all 67 Alabama counties.
Provider Survey
Pediatricians and family medicine physicians were contacted through the Alabama chapters of the American Academy of Pediatricians (AAP) and the American Academy of Family Physicians (AAFP) in 2015. AAP members were emailed an online survey and AAFP members were handed surveys at their annual meeting. The 21-item survey included yes/no, Likert-type and open-ended questions focusing on provider HPV vaccination practices, attitudes, and perceived barriers and facilitators to HPV vaccination. The primary purpose of these surveys was to generate preliminary data for development of subsequent qualitative interviews, and they represented a convenience sample of voluntary participants.
Qualitative Interviews
Alabama counties with fewer than 20% HPV vaccination rates based on ImmPRINT data were identified. Among these, three counties (Tuscaloosa, Lee and Shelby) were selected for the study due to their driving distance from Birmingham, as some interviews and recruitment would be done in person. Practicing pediatricians in these counties were recruited via email. Parents and clinical staff members were recruited in-person at the participating pediatrician offices. Clinical staff were included if they were actively involved in patient care and either a registered nurse, licensed practical nurse, or medical assistant. Written informed consent was obtained and the interview conducted on the same day. Parents were included if they were 18 years of age or older, were the primary caregiver of at least one child between the ages of 10 and 13, and were present at the physician’s office for a well-child visit on the day of recruitment. Parental written informed consent was obtained at the physician’s office, and phone interviews scheduled for a time within one week of recruitment. Organizations with a vested interest in HPV vaccination activities in the state were identified a priori, with the goal of recruitment from a variety of perspectives including non-profit, government and payor. A convenience sample of representatives of those organizations were then contacted for participation via email for the stakeholder interviews. Interviews were conducted between March 2016 and April 2017.
A standardized interview topic guide with open-ended questions was developed for each group with overlapping questions to facilitate comparisons. These questions focused on provider HPV vaccination practices and attitudes as well as barriers to and opportunities for vaccination on system, provider and patient levels. Each group of interviews was performed by one investigator to maintain consistency between participants. Participants were reimbursed $50 for their time. Interviews were recorded and transcribed. This research was approved by the UAB Institutional Review Board.
Two investigators independently evaluated the interviews for codes using an iterative sampling approach. Codes were reviewed, revised and agreed upon by both coders at regular intervals during the coding process. These codes were sorted and combined into representative themes. Themes that occurred in the majority (at least 65%) of interviews in one category of participant were considered major themes. Qualitative data was organized and analyzed using NVivo software (QSR International, Australia).
Results
Alabama HPV Vaccine Data
According to CDC data, vaccination rates in Alabama fall below the national average for vaccine initiation and completion among 13–17 year olds.10,16,17 Rates increased from 2014 to 2015, and remained stable from 2015 to 2016. There was a statistically significant increase in vaccination rates for boys from 2014 to 2015, from 16.1% to 30.3% for ≥ two doses, while the rate increase for girls was not statistically significant.17 2016 data demonstrate lower than national average vaccination rates for all adolescents (35.4% vs. 43.4%), boys (24.7% vs. 37.5%) and girls (36.5% vs. 49.5%).10
This differs from data from the state reporting system, ImmPRINT. Examining the number of adolescents receiving three doses of the vaccine with census estimates of number of adolescent children age 13–17 in a county as the denominator, the 2016 overall statewide vaccination rate is only 18%, a decrease of 1% from 2015. County-specific rates ranged from 9% to 38%. When stratified by gender, 14% of boys and 22% of girls had received three doses in 2016. Given that the CDC places this at 24.7% for boys and 36.5% for girls ages 13–17, the ImmPRINT results are likely underestimated.
According to ALBME records, there are 23 counties in Alabama without a pediatrician (34%), 15 without an obstetrician-gynecologist (22%) and three without a family medicine physician (4%). All counties but one have a health department where the HPV vaccine is available. When compared to county-level ImmPRINT data, a higher percentage of vaccine series completion was not correlated with a higher number of pediatricians (ρ=.014, p=0.9) per county, as would be expected.
Provider Survey
The provider survey received 49 responses, 58% from pediatricians and 42% from family medicine physicians. Additional demographics are given in Table 1.
Table 1.
Participant characteristics
| Survey | Qualitative Interviews | ||||
|---|---|---|---|---|---|
|
| |||||
| Variable |
Providersb | Pediatricians | Nurses | Parents | Stakeholders |
| N | 49 | 9 | 6 | 7 | 4 |
| Age range, years (mean) | --- | 41–74 (55) | 26–46 (33) | 28–55 (40) | 33–56 (46) |
| % racial/ethnic minority a | 17% | 22% | 17% | 29% | 50% |
| % female | 74% | 56% | 100% | 100% | 75% |
Includes African American, Hispanic/Latina, Asian
58% pediatricians, 42% family medicine doctors
Of the respondents, 96% recommend HPV vaccination and 92% have the vaccine available at their clinic. The two providers who did not recommend the vaccine were both family medicine physicians. Their written responses for not providing the vaccine included: “Expense, inconvenience, spontaneous clearing of 90% of infections” and “Cost, too expensive, very small pediatric population.” 64% of respondents indicated that they strongly or somewhat agree that “HPV vaccination is not required for school attendance” is a system-level barrier to vaccination. Patient barriers identified included “lack of parental understanding about HPV vaccination” (89%), “parent believes child is not at risk for HPV” (77%), “concern that the vaccine is not safe” (83%) and “reluctance to discuss sexuality and/or STIs” (77%). The two strategies that were most supported for improving HPV vaccination rates included “reminder systems for subsequent doses” (78%) and “guidance for making recommendations for parents in an easy-to-read form” (59%). When asked what would motivate physicians to increase their HPV vaccination coverage, 65% said “expansion of insurance coverage for HPV vaccine” and 63% said “a public education initiative by a professional organization directed at parents.”
Qualitative Interviews
In total, 26 qualitative interviews were performed. The initial goal was to recruit ten pediatricians and eight clinical staff, however saturation was achieved after interviews with nine pediatricians and six clinical staff. Participating clinical staff were all female nurses. Eight parents of adolescents were recruited, however one parent could not be reached by telephone. Six stakeholders were recruited, with two ultimately unable to participate. The participating stakeholders included: a director of a health education non-profit organization, chief medical officer of a health insurance company, health systems manager of a non-profit organization, and state health department employee.
Major Themes
Participants were asked a set of identical questions involving perceived barriers and facilitators to HPV vaccination as well as opportunities for improving HPV vaccination rates at the patient, provider and system levels. Themes that were mentioned by at least 65% of the participants in any group were considered major themes. (Table 2) Figure 1 demonstrates graphical representations of the overlap between groups on the major themes. Additional barriers that were frequently discussed but did not meet criteria for major themes included religion, parental logistics, no school entry requirement, and lack of trust (in pharmaceutical companies or the government).
Table 2.
Major themes and representative quotes
| Theme | Group (%) | Representative Quotes | P/E/Ra Factors | |
|---|---|---|---|---|
| Patient Barriers | Link to sexual activity | Pediatricians (89%) Parents (71%) Nurses (100%) Stakeholders (75%) Ped Survey (77%) |
“Maybe, parents who, I really don’t know how you say it, they may not want their children to have it because they may say, “Well, my child’s not sexually active.” I know that nowadays they are. They’re starting young. I hope my son, I hate to think about that, but a lot of parents, they are, in denial about their children being sexually active.” – 41, female, parent “…then we have stronger ties to religion in the south and especially in Alabama, which means the discussion around sex is way more taboo” – 33, male, stakeholder |
Predisposing |
| Misinformation – from internet or peers | Pediatricians (78%) Parents (71%) Nurses (100%) |
“Then the stuff on Facebook. The untrue articles and that stuff. I even had a mom tell me one day, the same one that told me that it caused her friend’s child to have arthritis, she said, “Well, we’ve all got to die some way.” I was thinking, “Well why did you get any of those other vaccines?” Just untrue stuff. It’s so hard to disprove or talk them into. People just believe everything they read.” – 30, female, nurse | Reinforcing | |
| Lack of knowledge | Pediatricians (67%) Parents (100%) Nurses (83%) Ped Survey (89%) |
“The other that I do not feel like I’m ready to even remotely make a decision is about my son. There definitely needs to be more material out there for that. If that is something that you feel is extremely important for males to receive, that information has got to get out there. Because I had no clue – no clue whatsoever that that was even need and why it was needed.” – 36, female, parent | Predisposing | |
| Concern about vaccine safety | Parents (71%) Nurses (67%) Ped Survey (83%) |
“Well, I’m terrified if my daughter has the vaccination that it’s going to be my fault if something happens to her. I could prevent that from happening by not having her vaccinated. Most people have HPV anyway unless you only have one sexual partner. I don’t know. I just go back and forth with it.” – 41, female, parent | Predisposing | |
| Skeptical parents | Parents (71%) Nurses (67%) | “Just saying I would, I would have to give it a lot more thought with it being such a new vaccine. It’s just, to me, it’s kind of like when there was all that uproar about MMR and it causing, could it be causing autism. I never questioned that because I feel like MMR was, that vaccine has been around since I was a kid.” – 36, female, parent | Predisposing | |
| Infrequent adolescent visits | Pediatricians (67%) | “Then we see the teenagers as they need. We try to get them in for their physicals, but iťs difficult sometimes to get them in. The college students, they come in on an as-needed basis when they're sick or need an excuse for an exam they missed” – 74, male, MD “Well, adolescents I would say often are not coming in as often as little ones so they are not in the office as often” – 45, female, MD |
Enabling | |
| Provider Barriers | Time | Pediatricians (78%) Stakeholders (75%) | “But I also have, like all of us have a limited time to address problems and you have got to – you have to choose your battles. And for me to choose the battle of having a long discussion about this with someone who is against it is frankly a massive waste of my time that I’m not going to do.” – 63, male, MD | Enabling |
| Weak provider recommendation | Stakeholders (75%) | “It’s provider barrier, totally. I’ve heard it from the doctors myself. My own children’s, they’re adults now, but I still interact with her at the AAP and she basically says she asks them do you want school required vaccines or do you want CDC recommended vaccines today?” – 54, female, stakeholder | Enabling/Predisposing | |
| Clinic logistics | Nurses (83%) | “And then, our schedule is not even open six months in advance sometimes. So that’s what makes it even harder. You have to rely more on the mom making a note in her calendar.” – 26, female, nurse | Enabling | |
| Provider uncomfortable discussing sex | Stakeholders (75%) | “I think iťs just all of the providers afraid of what parents may ask, not that the parents actually ask questions.” – 40, female, stakeholder | Predisposing | |
| System Barriers | Insurance/finan cial | Pediatricians (67%) Parents (71%) Stakeholders (75%) |
“I mean it’s an obscenely priced product and the reimbursement – I have a friend that’s in the tractor business and we were playing golf one day and I told him what our margin was on vaccines and he just laughed and he said, “Good thing I don’t do that in the tractor business, we’d be broke”” – 63, male, MD “Well, one for me is I’m not sure that insurance covers this. And that would be a concern.” – 36, female, parent “There’s been some confusion about if you have private insurance whether it’s covered. Different practices may or may not accept Medicaid and they’re charging Blue Cross/Blue Shield patients for the full cost of the vaccination even if they’re participating I think in the VFC program.” 40, female, stakeholder |
Enabling |
| Lack of access to vaccine provider | Stakeholders (100%) | “we have a large number of counties where the only place you can get the shot is the county health department. There are a couple of country health departments that only do shots three hours day. Now all of the sudden the burden for a parent to get this is incredibly high. It’s already something they don’t want to do. Now we’ve made a lot of barriers to them actually getting it” – 33, male, stakeholder “We mostly work with family medicine because we don’t have a lot of pediatricians in our service area so it’s from the family medicine side…We have pediatricians in three out of thirteen counties.” – 40, female, stakeholder |
Enabling | |
| Patient Opportunities | Patient education | Pediatricians (78%) Parents (100%) Nurses (100%) Stakeholders (100%) |
“Just education. Education across the board. A lot of patients do not know why they need it. They do not understand it. There has been so many bad raps against vaccines and autism. They do not want to get anything more than what they have to give.” – 46, female, nurse “It’s not even just education, we educate about it, but providing the right information in the right form to the particular patient we are talking with. There are some patients I can say, “It prevents certain types of cervical cancer,” and they say, “Oh okay, yeah.” Then you tell other people that and they don’t know what a cervix is. It means nothing to them that it prevents cervical cancer. Better tailoring the education, better tailored the demographic you’re dealing with.” – 34, female, nurse |
Predisposing |
| Message of prevention | Pediatricians (100%) Parents (100%) |
“And because, if you think about it, it makes sense. We are all about prevention. If I can prevent with a shot, why in the world not do the shot?” – 62, male, MD | Predisposing | |
| Social media/online | Parents (71%) Stakeholders (75%) Nurses (67%) |
“I think we should utilize social media ads to help fight some of the antivax stuff.” – 33, male, stakeholder “I click on a lot of things at my doctor’s office. They post things on Facebook and I go to a lot of the things that they specifically post.” – 36, female, parent |
Reinforcing | |
| Provider Opportunities | Provider incentives/metrics | Pediatricians (67%) Stakeholders (100%) |
“…provider level feedback reports. So I want to be able to, as part of, again, one of those benefits that you are as an ImmPRINT participating provider, here is your immunization rates as it relates to people that are in your community and as it relates to benchmarks against the state.” – 33, male, stakeholder “Because if you know, and as physicians we’re very competitive. If you knew that your vaccination rates were so much lower than someone else’s, it may help you strive.” – 56, female, stakeholder |
Enabling |
| Staff/provider training or education | Pediatricians (100%) Nurses (83%) Stakeholders (100%) |
“I mean, seriously. Come out and say here are there real numbers. Here is really how we are decreasing cervical cancer, here is really how we are decreasing the number of abnormal Pap smears, here are the real numbers on the VAERS side-effect report. You know” – 41, female, MD “… sometimes we don’t know what we don’t know, so ask questions during a lunch-and-learn and engage the nurses and just wait for us to ask questions because we might not know that we need to ask questions.” – 32, female, nurse “So, again, the key would be to find a way in which to reach those individuals on their grounds or their territory. Meaning can we email you? How can we provide information that would help you improve the quality of care that you’re delivering, i.e. vaccinating more?” – 56, female, stakeholder |
Predisposing/Enabling | |
| Utilize nurses | Pediatricians (100%) Nurses (100%) |
“When they (nurses) are in the room, that’s usually when the first time it comes up, how many shots am I getting today? That’s when the nurse will sometimes tell them if they know, if they anticipate knowing I’m going to say…but that would be good for them to bring up or just say, hey I noticed you haven’t had this.” – 54, female, nurse | Enabling | |
| Utilize technology | Pediatricians (78%) Nurses (83%) |
“-yeah, just pretty much with computer reminders, scheduling, if our templates open a little bit sooner we can probably go ahead and get those scheduled and get them set up to have those automated reminders. That will probably help.” – 32, female, nurse | Enabling | |
| Reminder system | Pediatricians (78%) Parents (86%) |
“You forget. There’s so much other stuff going on, parents forget. Send them a reminder, send them a text, call them” – 41, female, parent | Enabling | |
| Provider counseling | Parents (100%) | “I’d rather him (the doctor) suggest and talk to me about it than to dictate to me, “You need to do this, this, and this,” without any further discussion about it.” – 41, female, parent “Sometimes their language is just too medical, too big, and too broad. It’s easier to kind of break it down and to personalize it. They have so much knowledge, but not everything applies. Does that make sense?” – 28, female, parent |
Predisposing | |
| Doctors are trustworthy | Parents (86%) Nurses (67%) |
“Because like I said before, I know that doctor – that one specific doctor. I know her personally, I trust her. Yeah, things like that from reliable sources, known sources” – 36, female, parent |
Predisposing/Reinforcing | |
| System Opportunities | Promote or educate in schools | Pediatricians (67%) Parents (71%) Nurses (67%) Stakeholders (75%) |
“For the kids, I think to educate kids in a school setting might not be a bad place. Not to try and sway them, but this is the information you should talk to your parents about it. That might be one way to provide the education that you’re going to get a large group in one setting…It’s not like we see a ton of teenagers every day. School setting might be a good place for that.” – 29, female, nurse “As far as like the kids who maybe slip through system, that are not actively being followed by a pediatrician or seeing care every year for the physicals. I guess, you know, if they are actively enrolled in school, I mean maybe we should, you know, promote some of that through school.” – 36, female, parent |
Enabling |
| “Blue card” – policy or mandate | Pediatricians (89%) Nurses (67%) |
“The first dose we generally get them because they have to come for the 11-year-old check-up for the TDAP. That’s the way we get them initially.” – 29, female, nurse | Enabling | |
| Provide or promote in community organizations | Pediatricians (67%) Stakeholders (100%) |
“Yeah, I do believe, especially in the black community, if anything is brought to the church, I think the people would be more receptive to it” – 55, female, parent | Enabling |
P/E/R: Predisposing/Enabling/Reinforcing
Data collected in Alabama from 2015 to 2017
Figure 1a.
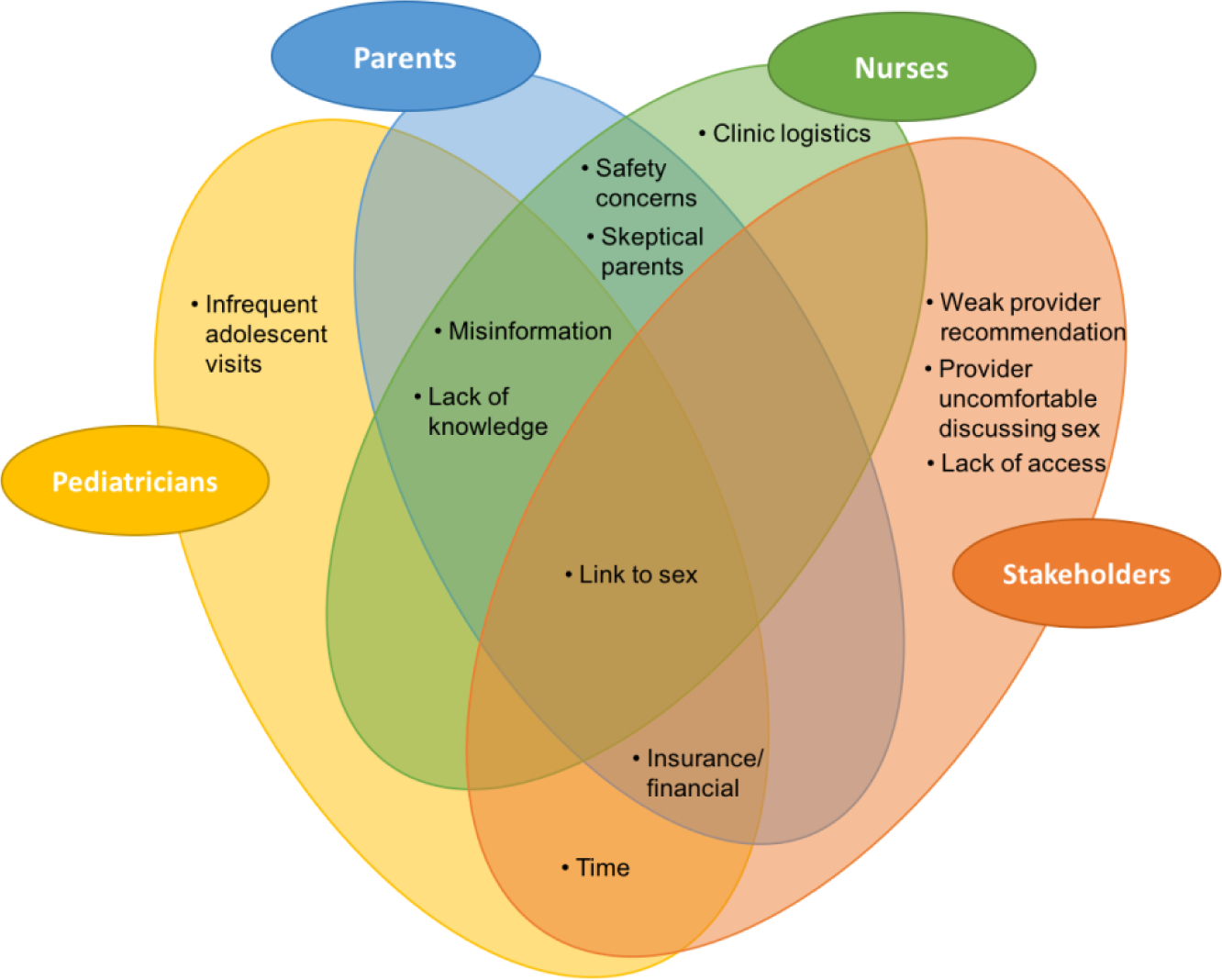
Barriers to HPV Vaccinationa
a. Each oval represents one interview participant group. Themes within overlapping circles represent agreement between those groups.
Overall, pediatricians are in favor of the HPV vaccine, recommend it to their patients, and administer it in their clinics. All of the pediatricians bundle the HPV vaccine with other adolescent vaccines, with some observing this practice more stringently than others. When counseling patients on the HPV vaccine, 100% reported using the message of cancer prevention, and 78% use their own family or personal experiences with the HPV vaccine to motivate parents to vaccinate their children.
All nurses displayed support of patients receiving the HPV vaccine. Most nurses endorsed providing initial basic counseling on the HPV vaccine, with questions or individualized counseling reserved for the physicians. Four out of six nurses exhibited minor gaps in their understanding of the benefits or recommendations for HPV vaccination. For example, several were not aware that HPV causes cancer of organs other than the cervix.
There were varying levels of knowledge among parents, with 86% having misunderstandings about the HPV vaccine. Several parents were not aware that the vaccine prevents disease in males, and one thought that it prevented Hepatitis C. The internet was the most common source of information about the vaccine, with five of seven parents citing websites and social media as resources. Three parents had chosen not to vaccinate their eligible children at the time of the interview for various reasons, including the belief that their child would not be sexually active before marriage, rumors of negative side effects from peers, and not knowing enough about the vaccine to make an informed decision.
Barriers
Patient-level barriers endorsed by 65% of the participants in one or more groups included: link to sexual activity, misinformation received from the internet or peers, lack of knowledge about the vaccine, concern about vaccine safety, skeptical parents, and the infrequency of adolescent medical visits. The link to sexual activity was the only barrier in this category to be endorsed by all four groups. Many participants referenced parents’ belief that their child will not engage in risky sexual behavior, referring to Christian faith or belief in abstinence before marriage.
Lack of time was the most frequently cited provider-level barrier. Stakeholders also cited weak provider recommendation and provider discomfort discussing sex as barriers. Nurses identified clinic logistics such as the doctor forgetting that the patient is due for a vaccine, lack of manpower, the vaccine not being in stock and clinic scheduling.
Pediatricians, parents and stakeholders all identified insurance or financial concerns as perceived system-level barriers. Pediatricians mentioned the vaccine as expensive to carry in their clinic. Participants stated that insurance was a perceived barrier but notably, many parents citing this as a factor were not familiar with the Vaccines for Children (VFC) program that ensures free vaccines to all children without coverage. Finally, stakeholders cited lack of access to a vaccine provider as a major barrier, including the lack of pediatricians in many Alabama counties.
Facilitators
Patient education was discussed by the majority of participants in all four groups. Using a message of cancer prevention was discussed by 100% of parents and pediatricians. The majority of parents discussed their desire for education that is quick and easy to understand. Parents, pediatricians and nurses discussed the popularity of the internet and social media, suggesting this as an avenue to reach parents of adolescent children. In particular, participants discussed the importance of using reliable sources on the internet to combat the misinformation and negativity about the HPV vaccine that exists online.
Both parents and nurses emphasized the trust that parents have in doctors. Furthermore, parents specifically discussed the importance of provider counseling in their decision-making process. Pediatricians and nurses endorsed a need for additional education for clinical staff members in doctors’ offices. Every participant in these groups also identified the importance of utilizing nurses as partners in improving HPV vaccination rates, either through nurse-only visits for subsequent doses, identifying a nurse champion to promote the vaccine within practices, or nurses starting the discussion about vaccination prior to the provider encounter. Nurses, physicians and parents all acknowledged the importance of primary counseling coming from the physician, however all clinicians were favorable towards nurses providing education or taking the lead on improving clinic logistics. Nurses and physicians also emphasized the importance of utilizing technology to their advantage, including the Electronic Medical Record (EMR) and ImmPRINT for tracking vaccinations. Finally, pediatricians and stakeholders mentioned using incentives and metrics to track provider- and practice-level vaccination rates in order to motivate physicians.
All four groups endorsed education about the HPV vaccine in schools as an opportunity to reach parents and adolescents. Suggestions included incorporating lessons into health or sex education, sending memos home with parents, and providing education to parent groups such as Parent-Teacher Organizations. Promoting or providing the vaccine in other community organizations was also discussed. Stakeholders in particular emphasized the potential for collaboration with pharmacies to administer the vaccine. Finally, both pediatricians and nurses discussed the usefulness of the state-mandated vaccination schedule (“blue card”) as an opportunity to bundle adolescent vaccines, as well as a potential opportunity for mandating the HPV vaccine. Several participants mentioned parents’ unwillingness to accept vaccines that are not required, and that the vaccine being on the “blue card” might overcome this barrier.
Predisposing, Enabling and Reinforcing Factors
We then identified predisposing, enabling and reinforcing factors that affect uptake of HPV vaccination, as described in the PRECEDE framework. (Table 2) Predisposing factors that were identified as barriers to HPV vaccination included parental and provider understanding of the HPV vaccine, concern about vaccine safety, beliefs surrounding the link between the vaccine and sexuality, and vaccine hesitancy. Predisposing factors that are facilitators for HPV vaccination uptake include a strong parental and provider desire to prevent cancer and willingness of providers and parents to learn more about the vaccine.
Enabling factors that are barriers include the lack of vaccine providers in some areas of the state, the amount of time it takes providers to counsel patients on the vaccine, the lack of a vaccine requirement for school entry, lack of a fully streamlined vaccine reporting system (ImmPRINT), and vaccine cost. Furthermore, many of the counties that do not have pediatricians are in poor, rural areas of the state. These results parallel recent CDC data that show that adolescents who live outside of metropolitan areas are less likely to initiate HPV vaccination compared to those living in cities (50.4% vs. 65.9%). Walker et al. posit that the lack of pediatricians outside of metropolitan areas may contribute to the disparity in vaccination rates between these populations.10
Enabling factors that are facilitators for vaccine uptake include the existing school Tdap vaccine requirement, the functionality of EMR systems, the potential of schools as a venue for vaccine promotion, and the role of nurses as partners in HPV prevention. While funding mechanisms including private insurance and VFC are a positive enabling factor, many parents in our study saw lack of insurance coverage as a barrier. This demonstrates a lack of knowledge regarding vaccine funding. Reinforcing factors that are barriers include the misinformation found on social media and weak provider recommendations.
Discussion
The multimodal approach of our study allowed us to describe the extent of the HPV vaccination problem in Alabama, identify possible systemic-level barriers to vaccination, and then further explore actionable items at the individual level. In 2016, only 35.4% of adolescents age 13–17 were up to date with the HPV vaccine in Alabama, compared to 43.4% nationwide based on CDC data. According to state-level reporting through ImmPRINT, only 18% of adolescents were up to date during the same time period. Additionally, while 96% of Alabama counties have a practicing family medicine physician, only 66% have a pediatrician. At the individual level, surveyed providers identified barriers to vaccination including the link to sexual activity, parental lack of knowledge, and parental safety concerns. These findings were supported by qualitative interviews with four different groups, with additional barriers and opportunities for vaccination identified. The lack of pediatric providers in some counties found in the analysis of ALBME provider records was supported in qualitative interviews, with participants highlighting the need for vaccine provision and education outside of the pediatrician’s office.
Our findings are consistent with existing research on the barriers to HPV vaccination. A meta-analysis evaluating barriers to HPV vaccination from over 50 articles found similar barriers from the provider and parent perspective. 11 Knowledge gaps and financial concerns were major barriers according to health care providers, while parents included in the meta-analysis most often cited lack of information, lack of provider recommendation, vaccine cost, concerns about vaccine safety and belief that their children are too young to get vaccinated for HPV. Beavis et al.18 analyzed a subset of data from the NIS-TEEN survey which included parents of 12,401 girls between the ages of 13 and 17 who did not have an intention to vaccinate their children, and they demonstrated that the reasons for non-vaccination changed from 2010 to 2014. In 2014, the three most common reasons for not initiating HPV vaccination were the belief that the vaccine is unnecessary, safety or side effect concerns, and lack of knowledge. Safety concerns and lack of knowledge were frequently cited barriers in our data. The authors suggest that the parental concerns related to sexual activity have decreased since 2010. However, our analysis of parents, healthcare providers and public health stakeholders would suggest that the link to sexual activity remains one of the greatest perceived barriers for parents in Alabama. In a 2015 qualitative analysis, caregivers living in rural Appalachian Ohio expressed similar concerns about discussing HPV with adolescents and the connection between the vaccine and sexual activity.19 However, in this same study, caregivers living in a more urban area did not share those concerns.
A strength of our study is the multimodal approach used to examine gaps and opportunities for improving health outcomes in our population. Limitations include the lack of inclusion of family medicine providers in the qualitative interviews. Family medicine providers were included in the survey, but more in-depth input from this group would have added an important perspective and should be considered going forward. The response rate to the survey was low, with only 49 surveys from hundreds of potential respondents. Another limitation was the method of participant sampling. Pediatricians were included in the study if they voluntarily responded to a recruitment email, which may have lead to a selection bias towards providers who are already pro-vaccine. Furthermore, using a convenience sample of nursing staff from these same clinics could also lead to selection bias. Participant opinion should be interpreted carefully, taking context into account and using it as a supplement to the breadth and depth of existing evidence-based recommendations.
Conclusions
A multilevel intervention that focuses on increasing access to vaccine providers, improving patient and parent education, and improving communication between at the provider-patient level using evidence-based strategies can increase uptake of HPV vaccination in Alabama. This is consistent with recommendations from the Community Preventive Services Task Force.20 At the system level, we must improve the statewide reporting system. With a systematic improvement in ImmPRINT reporting, government and nonprofit organizations could identify counties in need. Furthermore, accurate ImmPRINT reporting data can foster provider accountability and may be used to leverage a central reminder system. This could take the onus of dose reminders away from the individual provider and place it a systematic level, potentially giving patients opportunities to obtain doses outside of their typical provider visits. 78% of our surveyed providers supported a reminder system as an opportunity to increase vaccination completion. Next, organizations should reach out to providers in geographic regions with low uptake, particularly in rural counties that do not have a local pediatrician. Provider education interventions regarding vaccine funding mechanisms and evidence-based strategies for vaccine promotion could be tailored to these specific practices. School-based education interventions are a potential avenue for patient and parent education and awareness. The school-based approach has been especially successful outside of the US, and our participants supported the school setting as a venue to provide culturally- and age-appropriate education. 21
Providers should continue to take advantage of the requisite sixth grade school-entry visit. At this visit, consistent messaging with a strong recommendation for the HPV vaccine should be a priority. A recent randomized controlled trial showed that when providers were trained to “announce” the plan for HPV vaccination during a visit there was a an increase in the number of HPV vaccinations given versus standard care.22 While patients express a desire for providers to take the time to provide personalized counseling, the most effective conversations with parents likely do not rely on lengthy explanations of the risks and benefits of the vaccine. Furthermore, lack of provider time is an oft-cited barrier, and quick and easily understandable information is a priority for parents. In our population, the message of cancer prevention is especially important given the strong aversion to discussions surrounding the link to the HPV vaccine and sexual transmission. Nurses should be empowered to support and reiterate this messaging, and can be important allies in implementing clinic-level quality improvement projects. Finally, information could be disseminated through social media and the internet. Specifically, engagement with websites and social media accounts run by physician offices would provide patients with a trusted source.
Alabama is a rural state with high cervical cancer rates and low HPV vaccine uptake rates relative to the rest of the country. Fortunately, significant energy is being put forth to address this problem, with the members of the Alabama HPV Vaccination Coalition leading the charge. Data from this project will be used to develop evidence-based, tailored research and clinical efforts to continue decreasing the burden of HPV-related cancers in Alabama.
Figure 1b.
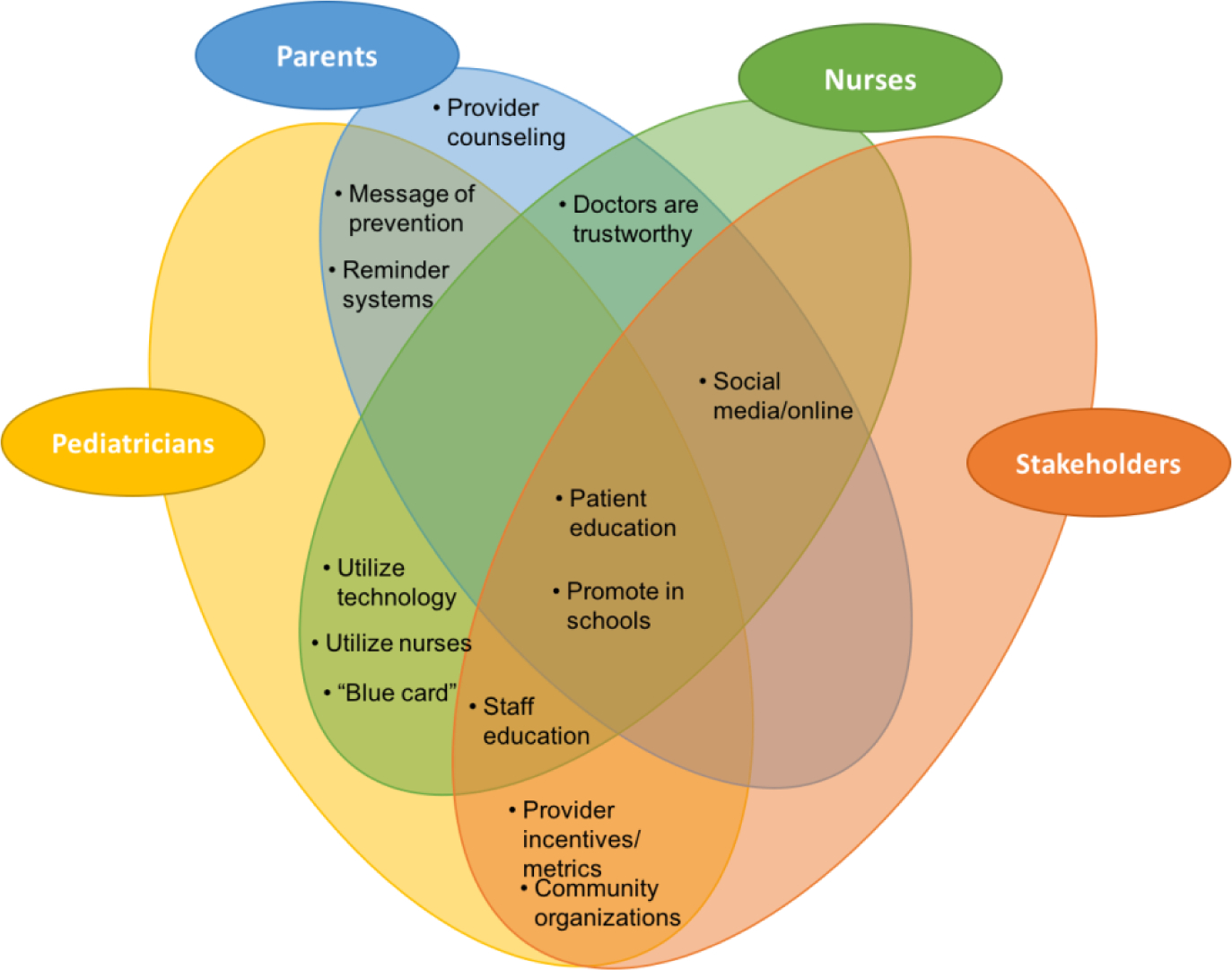
Facilitators to HPV Vaccination
Dilley – Highlights.
A multimodal approach explored poor HPV vaccine uptake in Alabama
Barriers include lack of knowledge and access, safety concerns, link to sex
Suggestions for increasing vaccine uptake on multiple levels are given
Acknowledgements:
Portions of this work were funded by NIH Grant #P30CA013148
Footnotes
Conflict of Interest: Dr. Dilley receives grant funding from Merck that is unrelated to this study. The additional authors declare no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Viens LJ HS, Watson M, Markowitz LE, Thomas CC, Thompson TD, Razzaghi H, Saraiya M. Human Papillomavirus–Associated Cancers — United States, 2008–2012. MMWR Morb Mortal Wkly Rep 2016;26(65):661–666. [DOI] [PubMed] [Google Scholar]
- 2.American Cancer Society I. Alabama Cancer Facts & Figures 2015. In: Health ADoP, ed2016 [Google Scholar]
- 3.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA: A Cancer Journal for Clinicians. 2017;67(1):7–30. [DOI] [PubMed] [Google Scholar]
- 4.Benard VB, Castle PE, Jenison SA, et al. Population-based incidence rates of cervical intraepithelial neoplasia in the human papillomavirus vaccine era. JAMA Oncology. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brotherton JML, Fridman M, May CL, Chappell G, Saville AM, Gertig DM. Early effect of the HPV vaccination programme on cervical abnormalities in Victoria, Australia: an ecological study. The Lancet. 2011;377(9783):2085–2092. [DOI] [PubMed] [Google Scholar]
- 6.Brotherton JML, Malloy M, Budd AC, Saville M, Drennan KT, Gertig DM. Effectiveness of less than three doses of quadrivalent human papillomavirus vaccine against cervical intraepithelial neoplasia when administered using a standard dose spacing schedule: Observational cohort of young women in Australia. Papillomavirus Research. 2015;1:59–73. [Google Scholar]
- 7.Saraiya M, Unger ER, Thompson TD, et al. US Assessment of HPV Types in Cancers: Implications for Current and 9-Valent HPV Vaccines. JNCI Journal of the National Cancer Institute. 2015;107(6):djv086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meites E, Kempe A, Markowitz L. Use of a 2-Dose Schedule for Human Papillomavirus Vaccination — Updated Recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep 2016. 2016;65:1405–1408. [DOI] [PubMed] [Google Scholar]
- 9.Lehtinen M, Paavonen J, Wheeler CM, et al. Overall efficacy of HPV-16/18 AS04-adjuvanted vaccine against grade 3 or greater cervical intraepithelial neoplasia: 4-year end-of-study analysis of the randomised, double-blind PATRICIA trial. The Lancet. Oncology. 2012;13(1):89–99. [DOI] [PubMed] [Google Scholar]
- 10.Walker TY, Elam-Evans LD, Singleton JA, et al. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years - United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66(33):874–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holman DM BV, Roland KB, et al. Barriers to human papillomavirus vaccination among us adolescents: A systematic review of the literature. JAMA Pediatrics. 2014;168(1):76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rambout L, Tashkandi M, Hopkins L, Tricco AC. Self-reported barriers and facilitators to preventive human papillomavirus vaccination among adolescent girls and young women: A systematic review. Preventive Medicine. 2014;58:22–32. [DOI] [PubMed] [Google Scholar]
- 13.Green L, Kreuter M. Health Program Planning: An Educational and Ecological Approach. 4th ed: McGraw-Hill Humanities/Social Sciences/Languages; 2004. [Google Scholar]
- 14.Hiatt RA, Sibley A, Fejerman L, et al. The San Francisco Cancer Initiative: A Community Effort To Reduce The Population Burden Of Cancer. Health Affairs. 2018;37(1):54–61. [DOI] [PubMed] [Google Scholar]
- 15.Dohan D, Schrag D. Using navigators to improve care of underserved patients. Cancer. 2005;104(4):848–855. [DOI] [PubMed] [Google Scholar]
- 16.Reagan-Steiner S YD, Jeyarajah J, Elam-Evans L, Singleton JA, Curtis R, MacNeil J, Markowitz LE, Stokley S. National, regional, and selected local area vaccination coverage among adolescents aged 13–17 years – United States, 2014. Morb Mortal Wkly Rep 2015;64(29):784–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reagan-Steiner S YD, Jeyarajah J, et al. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years — United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:850–858. [DOI] [PubMed] [Google Scholar]
- 18.Beavis A, Krakow M, Levinson K, Rositch A. Reasons for persistent suboptimal rates of HPV vaccination in the US: Shifting the focus from sexuality to education and awareness. Oral Presentation at the SGO Annual Meeting. 2017. [Google Scholar]
- 19.Katz ML, Paskett ED. The Process of Engaging Members From Two Underserved Populations in the Development of Interventions to Promote the Uptake of the HPV Vaccine. Health Promotion Practice. 2015;16(3):443–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Force CPST. Increasing appropriate vaccination. http://www.thecommunityguide.org/vaccines/index.html, 2016.
- 21.Miller K, Dilley SE, Huh WK. Lessons learned from domestic and international human papillomavirus vaccination programs: a review. American Journal of Obstetrics and Gynecology. 2017. [DOI] [PubMed] [Google Scholar]
- 22.Brewer NT, Hall ME, Malo TL, Gilkey MB, Quinn B, Lathren C. Announcements Versus Conversations to Improve HPV Vaccination Coverage: A Randomized Trial. Pediatrics. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]


