Abstract
Introduction:
The annual economic burden of chronic homelessness in the U.S. is estimated to be as high as $3.4 billion. The Permanent Supportive Housing with Housing First (Housing First) program, implemented to address the problem, has been shown to be effective. This paper examines the economic cost and benefit of Housing First programs.
Methods:
The search of peer-reviewed and gray literature from inception of databases through November 2019 yielded 20 evaluation studies of Housing First programs, 17 from the U.S. and 3 from Canada. All analyses were conducted during March 2019 through July 2020. Monetary values are reported in 2019 U.S. dollars.
Results:
Evidence from studies conducted in the U.S. was separated from those conducted in Canada. The median intervention cost per person per year for U.S. studies was $16,479 and for all studies, including those for Canada, it was $16,336. The median total benefit for the U.S. studies was $18,247 per person per year and $17,751 for all studies including those for Canada. The benefit-to-cost ratio for U.S. studies was 1.80:1, and for all studies including those for Canada it was 1.06:1.
Discussion:
The evidence from this review shows economic benefits exceed the cost of Housing First programs in the U.S. There were too few studies to determine cost–benefit in the Canadian context.
INTRODUCTION
Chronic homelessness is a public health concern. The U.S. Department of Housing and Urban Development (HUD) defines the chronically homeless as individuals with disability who have been continuously homeless for ≥1 year, or have experienced ≥4 episodes of homelessness totaling ≥12 months over the past 3 years.1 Disability may include substance use disorder (SUD), serious mental illness, developmental disability, post-traumatic stress disorder, cognitive impairment from brain injury, or chronic physical illness including HIV.1 The 1988 Institute of Medicine report on homelessness noted that health and homelessness interact in a 3-step process.2 First, people enter homelessness as a result of financial hardship,3–5 adverse childhood experiences,6,7 or poor mental health and SUD.8–11 Second, the experience of homelessness and exposure to attendant risk factors contribute to worsening health as well as new health issues,12,13 with the lack of preventive care exacerbating chronic diseases.14–16
Third, cumulated effects of homelessness experienced by the chronically homeless result in their very poor physical and mental health which, in turn, increase the risk of mortality and likelihood of remaining in or returning to homelessness.17,18 The lack of support or access to social safety net services at the outset of the journey of many chronically homeless people continues to deplete them of personal resources and income and, once homeless, causes them to consume extensive resources through social programs.19–24
The number of people classified as chronically homeless by HUD was 119,813 in 2007, 77,486 in 2016, and 96,141 in 2019.25 These estimates are counts from field surveys conducted during a single night in January of each year, a method that may lead to an underestimate in cold climates. The states of California, New York, Washington, Oregon, Pennsylvania, and Florida had the highest number of homeless individuals and highest rate of homelessness.25 Based on a reported annual societal cost per person experiencing homelessness of >$35,500,26 and the approximately 96,000 people in HUD’s 2019 count of the chronically homeless,25 the annual societal cost is as high as $3.4 billion.
One program to address chronic homelessness is permanent supportive housing with housing first (Housing First Programs).27 Housing First provides regular, subsidized, permanent housing offering supportive services to people with disabilities experiencing homelessness, without requiring that clients undergo treatment for their disability or maintain sobriety in the case of those with SUD. Housing First is distinguished from what was the traditional approach called the Continuum of Care, which specified a stepwise process that required compliance with psychiatric treatment and encouraged sobriety as clients started in short-term emergency housing such as shelters and then moved to transitional residential programs to prepare and ready them for independent living within permanent supportive housing.28
In 2019, the Community Preventive Services Task Force (CPSTF), an independent, non-federal panel of population health experts,29 recommended Housing First Programs30 based on a systematic review of evidence. The evidence showed the programs decreased homelessness, increased housing stability, and improved the quality of life for people who are experiencing homelessness and have a disabling condition.31 Homelessness was measured as the duration or proportion of time spent homeless and housing stability was measured in a variety of ways in the included studies. Physical and mental health scores were similar across study groups and mixed for alcohol and substance use. Quality of life and community integration scores improved and the number of emergency department visits and inpatient stays were reduced.31
Regarding the economics of Housing First Programs, a recent review found mixed evidence whether societal benefits exceed the cost of intervention.32 An earlier review was similarly inconclusive and identified several deficiencies in the literature at the time and called for better-designed studies.19 On the other hand, CPSTF found that the economic benefits exceeded the cost of Housing First Programs in the U.S. based on a systematic review of the economic evidence completed in 2020.30 The present study describes the process, results, and conclusions of the systematic economic review. The following are the research questions:
What is the intervention cost to implement Housing First Programs?
What are the economic benefits (costs averted) of Housing First Programs?
How do intervention costs compare to economic benefits (costs averted) for Housing First Programs?
Are Housing First Programs cost effective? What is the cost per quality-adjusted life year (QALY) saved ≤ $50,000?33 What is the Cost per disability adjusted life year (DALY) averted ≤ per capita gross domestic product (GDP)?34
METHODS
This study was conducted using established methods for systematic economic reviews developed by scientists at the Centers for Disease Control and Prevention and approved by CPSTF.35 The review team included subject matter experts on homelessness from various agencies, organizations, and academic institutions; members of CPSTF; and experts in systematic economic reviews from the Community Guide Office at the Centers for Disease Control and Prevention. Two reviewers independently screened the search yield, abstracted information from included studies, computed economic estimates, and quality scored each estimate. Disagreements were resolved through discussions with the larger review team. Community Guide scientists have a mean >10 years of experience conducting systematic reviews of evidence for public health interventions.36 Reviewers undergo didactic and on-the-job training, which includes mastering the methods in published papers and internal handbooks and piloting with sample sets of studies at the outset of each review project.
The following steps are integral to Community Guide systematic economic review methods: constitute the review team, develop intervention definition, develop analytic framework identify the pathways of intervention effectiveness and outcomes of interest, specify parameters of evidence search and inclusion criteria, abstract outcomes and other relevant information from included studies, assess quality of estimates, summarize economic outcomes, and draw conclusions. The key steps for the present review are described here, beginning with the search strategy and inclusion criteria.
Search strategy.
Peer-reviewed and gray literature were searched with the following criteria for inclusion: met the definition of the program, conducted in a high-income country,37 written in English, and reported ≥1 economic outcomes in the research questions. The searches were conducted in PubMed, MEDLINE, Embase, PsycINFO, Sociological Abstracts, ERIC, CINAHL, Scopus, Cochrane, EconLit, Campbell, and NTIS (including HUD) from inception of databases to November 2019.38 Reference lists from included studies were screened and subject matter experts were consulted for additional studies.
Intervention definition.
Housing First Programs provide regular, subsidized, time-unlimited housing to individuals and families experiencing homelessness in which the head of household has a disabling condition, which may include mental health disorders or SUD, difficulties in independent working and living, or HIV infection. Clients are not required to be “housing ready,” (i.e., substance free or in treatment). Services to support housing stability include ≥1 of: health care, mental health services, treatment for SUD, peer support, occupational therapy, employment counseling, initial furnishing expenses, and training in money management.30
Analytic framework.
The framework in Figure 1 postulates that Housing First Programs delivered to people with disabling conditions experiencing homelessness will improve and sustain their housing stability and health. The framework identifies housing locator services, rent subsidies, and support for healthcare services (i.e., physical and mental health, substance abuse) as drivers of intervention cost. Other components of intervention cost may include assistance with furnishings or move-in, landlord relations, assistance with integration into the community, employment search and training, and assistance in maintaining stable housing. The framework postulates that the economic benefits of Housing First Programs are derived from improved health and wellness of previously homeless clients and the averted costs of: health care, temporary housing services such as shelters, judicial and police services, welfare and disability transfers, and unemployment. The framework considers all these components of benefits to be drivers except for unemployment. It is postulated that improvements in health lead to increased quality and quantity of years lived. The framework conceptualizes summary economic outcomes as cost–benefit or cost effectiveness. Cost–benefit is the ratio of benefits or averted costs to intervention cost, and is favorable if benefits exceed cost. Cost effectiveness is net cost per additional QALY gained or DALY averted, and is favorable if the former is <$50,00033 or the latter is less than per capita GDP.34
Figure 1.
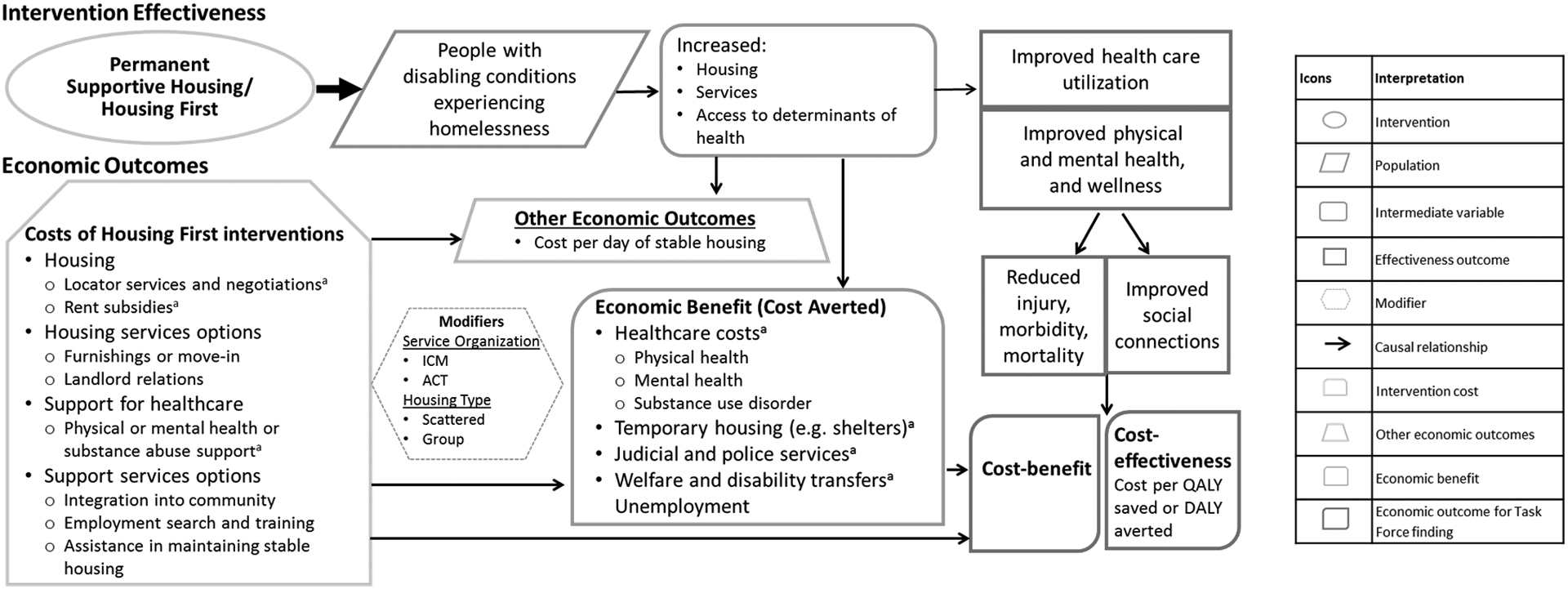
Pathways to economic costs and benefits.
aCost Drivers; ICM, Intensive Case Management; ACT, Assertive Community Treatment; QALY, Quality Adjusted Life Year; DALY, Disability Adjusted Life Year
Quality assessment.
Quality assessment was conducted for each estimate that contributed to the economic outcomes of interest: intervention cost, intervention benefit, and the composite cost–benefit. A quality assessment tool developed for the scope and objective of the present review along with with full process description is in the Appendix (available online). Quality of capture was assessed as good, fair, or limited for each estimate for how well it captured the components that are deemed to be drivers of magnitude. Quality of measurement was assessed as good, fair, or limited for each estimate for the appropriateness of design and statistical and analytic methods used to derive the estimates. The overall quality of an estimate was the lower of the quality assigned for capture and the quality assigned for measurement. Limited quality estimates were removed from the review. Finally, the quality assigned to estimates that were a combination of other estimates such as benefit–cost ratios was the lower of the quality assigned to total benefit and intervention cost components.
Quality based on capture of drivers was assigned to each estimate as good, fair, or limited as it included most, some, or almost none of the components considered to be drivers, respectively. The drivers of intervention cost, seen earlier in the analytic framework, were housing rent subsidies and locator services, other housing assistance such as move-in costs, healthcare support for physical or mental health, and any additional supports provided to participants. The drivers of postulated benefits, again from the analytic framework, were healthcare cost averted and averted costs of multiple other social services related to temporary housing, judicial, and welfare services. Next, quality of measurement was assessed for each estimate of intervention cost and benefit based on limitation points for failing to follow appropriate measurement and statistical methods. Quality based on measurement was assigned to each estimate as good, fair, or limited as the number of limitations points were few, some, or many, respectively. The criteria for assessing limitation points were broadly classified into the domains of appropriate: population, analytic horizon, study or experiment design, data sources, and valuation. Thus, limitation points for measurement were assigned for small sample size, populations that were not chronically homeless or had a disability, time horizons that were too short to plausibly capture intervention effects, study designs that did not have an appropriate comparison group, and outcomes based on self-reports rather than drawn from records of servicing agencies.
Summarizing outcomes.
All monetary values are in 2019 U.S. dollars, adjusted for inflation using the Consumer Price Index,39 and converted from foreign currency denominations using purchasing power parities.40 Estimates are reported in per patient per year (PPPY) terms, wherever possible. Summaries of estimates are reported as medians with interquartile intervals (IQI), when n≥4. All analyses were conducted during March 2019 through July 2020.
Review decisions.
Results are presented separately for studies from the U.S. followed by overall results. The rationale for the separation was that the homeless populations in the U.S. are different from other high-income countries owing to existence of racial and ethnic disparities, the difference in availability of social services in the U.S. compared with other high-income countries, and presence of universal health insurance in other high-income countries.
RESULTS
The economic review included 20 studies: 17 studies41–57 for the U.S. and 3 studies58–60 for Canada. No studies for other high-income countries met the inclusion criteria. Table 1 shows one study for the U.S.49 and another for Canada60 modeled the economic benefits and the remaining were based on observed changes. The median sample size was 279 (IQI=113–1,158; 19 studies).41,43–60 The median mean age of participants was 45 years (IQI=42–48 years; 9 studies),41,44–48,50,53,56 and a median of 30% were women (IQI=29%–40%; 13 studies).41,44–50,52,54,56,58,59 Among studies reporting race and ethnicity, participants were White (median=31%; 8 studies),41,44,46,47,50,52,54,56 African American (median=47%; 10 studies),41,44,46,47,49,50,52–54,56 Hispanic (median=9%; 8 studies),41,44,46,47,50,52,54,56 and American Indian or Alaska Native (14% and 28%; 2 studies).50,56
Table 1.
Study and Population Characteristics
| Study author (year) Location |
Design Intervention sample size |
Type of disability | Mean age | Percent female | Race and ethnicity |
|---|---|---|---|---|---|
| Basu (2012)41 Chicago, IL |
RCT 201 |
Group a: All Group b: Chronically homeless Group c: Persons living with HIV |
47 years | 26% | White 7%, Black 81%, Hispanic 8%, Other 4% |
| Byrne (2014)42 Nationwide, U.S. |
PPC NR |
MH or SUD | NR | NR | NR |
| Culhane (2002)43 New York, NY |
PPMC 4,679 |
MH | NR | NR | NR |
| Flaming (2009)54 Los Angeles, CA |
PPMC 279 |
Group a: All Group b: MH Group c: SUD Group d: HIV |
Age ≥46 years 70% | 30% | White 15%, Black 65%, Hispanic 10%, Other 10% |
| Flaming (2013)44 Los Angeles, CA |
WLC 89 |
High need and high utilizers | 48 years | 29% | White 23%, Black 43%, Hispanic 15%, Other 7% |
| Gilmer (2009)46 San Diego, CA |
PPMC 177 |
MH | 42 years | 60% | White 60%, Black 22%, Hispanic 9%, Other 9% |
| Gilmer (2010)47 San Diego, CA |
PPMC 209 |
MH | 44 years | 37% | White 61%, Black 26%, Hispanic 9%, Other 4% |
| Gilmer (2014)48 Statewide, CA |
PPMC 10,231 |
MH | 42 years | 46% | White 31%, Black 10%, Hispanic10%, Unclassified 49% |
| Gilmer (2016)45 Statewide, CA |
PPMC 2,609 |
MH | 21 years | 49% | White 31%, Black 11%, Hispanic22%, Unclassified 37% |
| Holtgrave (2013)49 Baltimore, MD; Chicago, IL; Los Angeles, CA |
RCT 315 |
HIV | Age ≥50 years 64% and Age 30‒39 years 24% | 29% | Black 78%, Other 22% |
| Larimer (2009)50 Seattle, WA |
WLC 95 |
SUD and high utilizers | 48 years | 6% | White 39%, Black 10%, Hispanic 6%, Native American 28% Other 13% |
| Lim (2018)52 New York, NY |
PPC 737 |
MH or dual MH-SUD | Age 35‒54 years 67% and Age 18‒34 years 15% | 29% | White 15%, Black 51%, Hispanic 28%, Other 6% |
| Rosenheck (2003)53 San Francisco, CA; San Diego, CA; New Orleans, LA; Cleveland, OH |
RCT 182 |
MH or SUD | 42 years | NR | Black 64%, Other 36% |
| Schinka (1998)55 Tampa, FL |
PPC 36 |
SUD | NR | NR | NR |
| Seligson (2013)51 New York, NY |
PPMC 1695 |
Group a: MH or dual MH-SUD Group b: Head of household with MH or dual MH-SUD Group c: Head of household with SUD, disability or HIV Group d: Youth leaving foster care Group e: Serious MH, SUD, or HIV |
NR | NR | NR |
| Srebnik (2013)56 Seattle, WA |
PPC 29 |
MH or PH and high utilizers | 51 years | 28% | White 62%, Black 17%, Hispanic 7%, Native American 14% |
| Toros (2012)57 Los Angeles, CA |
PPC 50 |
MH or SUD | NR | NR | NR |
| Goering (2014)a58 Vancouver, Montreal, Toronto, Moncton |
RCT 1,158 |
Group a: Severe disability or disease and high utilizers Group b: Moderate disability or disease and moderate utilizers |
NR | 32% | NR |
| Latimer (2019)59 Vancouver, Montreal, Winnipeg, Toronto |
RCT 689 |
MH or SUD | Age <30 years 7.1%, Age 30‒49 years 57.8%, Age ≥50 years 25.1% | 65% | NR |
| Patterson (2008)a,b,c60 British Columbia |
Modeled 18,759; 11,750; 7,009 |
Group a: All Group b: Chronically homeless Group c: At risk or moderately homeless |
NR | NR | NR |
| Summary Median (IQI) |
Intervention sample size 279 (IQI: 113 to 1,158) |
— | 45.5years (IQI: 42 to 48) | 30% (IQI: 29% to 40%) | Median White 31%, Black 47%, Hispanic 9% |
PPMC, pre post with matched control; PPC, pre post with control; WLC, wait list control; MH, mental health disorders; SUD, substance use disorders; PH, chronic physical health conditions; NR, not reported.
Table 2 shows that 15 studies41,43,44,47,49–51,53–60 reported intervention cost and 15 studies41,43–48,50–52,54,56,57,59,60 studies reported economic benefits from averted healthcare cost. Benefits from other sources were: averted emergency housing (4 studies),43,50,51,59 averted judicial and police services (12 studies),41,43,44,46,47,50,51,54,56,57,59,60 averted welfare and disability transfers (4 studies),44,51,54,59 and increased employment income (1 study).59 Two studies50,58 provided the aggregate and not separate estimates for healthcare and non-healthcare costs averted.
Table 2.
Intervention Cost of Program and Program Benefits: Components, and Quality of Estimates
| Study author (year) | Design | Intervention cost per PPPY | Quality of intervention cost estimate | Components included in intervention cost estimate | Healthcare cost averted PPPY (A) | Components included in non-healthcare cost averted estimate | Non-healthcare cost averted PPPY (B) | Total benefits from averted costs PPPY (A+B) | Quality of total benefit estimate |
|---|---|---|---|---|---|---|---|---|---|
| Basu (2012)a41 | RCT | $4,368 | G | R, S | ‒$11,248 | J | ‒$1,376 | ‒12,624 | F |
| Basu (2012)b41 | RCT | $4,177 | G | R, S | ‒16,381 | J | ‒635 | ‒$17,016 | G |
| Basu (2012)c41 | RCT | $5,525 | G | R, S | ‒$12,315 | J | ‒1,878 | ‒$14,193 | F |
| Culhane (2002)43 | PPMC | $20,830 | G | R, S | ‒$13,462 | Hs, J | ‒$5,178 | ‒$18,640 | G |
| Flaming (2009)a54 | PPMC | $15,737 | F | R | ‒$29,731 | W, J | ‒$2,985 | ‒$32,716 | G |
| Flaming (2009)b54 | PPMC | $15,651 | F | R | ‒$32,730 | W, J | ‒$3,284 | ‒$36,014 | G |
| Flaming (2009)c54 | PPMC | $15,951 | F | R | ‒31,402 | W, J | ‒3,156 | ‒$34,558 | G |
| Flaming (2009)d54 | PPMC | $16,051 | F | R | ‒$40,555 | W, J | ‒4,070 | ‒44,625 | G |
| Flaming (2013)44 | WLC | $32,955 | G | R, S | ‒$47,289 | W, J | ‒4,904 | ‒52,193 | G |
| Gilmer (2009)46 | PPMC | NR | NA | NA | $666 | J | ‒$385 | $281 | F |
| Gilmer (2010)47 | PPMC | $3,921 | G | R, Sa | $711 | J | ‒$2,023 | ‒$1,312 | F |
| Gilmer (2014)48 | PPMC | NR | NA | NA | $14,865 | None | NR | $14,865 | F |
| Gilmer (2016)45 | PPMC | NR | NA | NA | $16,445 | None | NR | $16,445 | F |
| Holtgrave (2013)49 | RCT | $16,085 | G | R, S | NR | None | NR | NA | |
| Larimer (2009)50 | WLC | $17,069 | G | R, S | NR | NR | NR | ‒$54,392b | G |
| Lim (2018)52 | PPC | NR | NA | NA | ‒$5,301 | None | NR | ‒$5,301 | F |
| Rosenheck (2003)53 | RCT | $3,213 | G | R, Sa | NR | None | NR | NR | NA |
| Schinka (1998)55 | PPC | $70,122 | F | R, S | NR | None | NR | NR | NA |
| Seligson (2013)a51 | PPMC | $16,873 | G | R, S | ‒4,906 | Hs, W, J | ‒12,948 | ‒$17,854 | G |
| Seligson (2013)b51 | PPMC | $29,105 | G | R, S | ‒$5,329 | Hs, W, J | ‒$32,301 | ‒$37,630 | G |
| Seligson (2013)c51 | PPMC | $29,154 | G | R, S | $315 | Hs, W, J | ‒$29,044 | ‒$28,729 | G |
| Seligson (2013)d51 | PPMC | $25,567 | G | R, S | ‒$10,441 | Hs, W, J | ‒$1,903 | ‒12,344 | G |
| Seligson (2013)e51 | PPMC | NR | NA | NA | $2,903 | Hs, W, J | ‒$8,817 | ‒$5,914 | G |
| Srebnik (2013)56 | PPC | $20,274 | G | R, L, Sa | ‒$36,429 | J | $724 | ‒$35,705 | G |
| Toros (2012)57 | PPC | $34,104 | G | R, S | ‒14,566 | J | ‒$12,341 | ‒$26,907 | F |
| Goering (2014)a58 | RCT | $20,143 | G | R, S | NR | NR | NR | ‒$19,344b | G |
| Goering (2014)b58 | RCT | $12,830 | G | R, S | NR | NR | NR | ‒$4,388b | F |
| Latimer (2019)59 | RCT | $11,553 | G | R, S | $475 | Hs, W, J, E | ‒$2,468 | ‒$1,993 | F |
| Patterson (2008)a60 | Modeled | $16,586 | F | R, S | ‒$16,657 | J | ‒$1,094 | ‒$17,751 | F |
| Patterson (2008)b60 | Modeled | $14,994 | F | R, S | ‒$16,657 | J | ‒$1,094 | ‒$17,751 | F |
| Patterson (2008)c60 | Modeled | $19,249 | F | R, S | ‒$16,657 | J | ‒$1,094 | ‒$17,751 | F |
| U.S. studies Median (IQI) | — | $16,479 (IQI: $13,120 to $26,452) | — | — | ‒$11,248 (‒$29,731 to $315) | — | ‒$3,220 (‒$7,907 to ‒$1,884) | $18,247 (IQI: $7,522 to $35,418) | — |
| U.S. studies with good quality estimates Median (IQI) | — | $17,069 (IQI: $4,947 to $27,336) | — | — | — | — | — | $33,637 (IQI: $18,051 to $37,227) | — |
| All estimates Median (IQI) | — | $16,336 (IQI: $13,371 to $20,691) | — | — | ‒$12,315 (‒$16,657 to $315) | — | ‒$2,727 (‒$5,110 to ‒$1,165) | $17,751 (IQI: $5,761 to $33,177) | — |
Does not include management and overhead costs.
Does not provide separate healthcare and non-healthcare benefits estimates.
PPMC, pre post with matched control; PPC, pre post with control; WLC, wait list control; PPPY, per person per year; NA, not applicable; NR, not reported; G, good; F, fair; R, rent subsidies; L, housing locator services and negotiations; S, healthcare support services; H, healthcare; Hs, Temporary housing; J, Judicial and police; W, Welfare and disability transfers; E, Employment income; IQI, interquartile interval.
A total of twelve studies shown in Table 3 reported both intervention cost and program benefit that produced cost–benefit evidence, 9 studies41,43,44,47,50,51,54,56,57 for the U.S. and 3 studies58–60 for Canada. Four studies42,49,53,55 met the program definition but did not provide cost–benefit or cost-effectiveness outcomes of interest to the economic review. Three of these42,53,55 were conducted by the Department of Veterans Affairs and compared Housing First programs to other homeless programs offered by the Department of Veterans Affairs. One study49 for homeless people with HIV considered treatment costs of averted partner infections as benefit. Therefore, intervention cost estimates from these studies were included in the present review but benefit estimates were excluded.
Table 3.
Cost-Benefit Estimates and Quality
| Study author (year) | Design | Intervention cost PPPY (A) | Total benefit PPPY (B) | Benefit to cost ratio (B/A) | Quality of benefit to cost ratio estimate |
|---|---|---|---|---|---|
| Basu (2012)a41 | RCT | $4,368 | $12,624 | 2.9 | F |
| Basu (2012)b41 | RCT | $4,177 | $17,016 | 4.1 | G |
| Basu (2012)c41 | RCT | $5,525 | $14,193 | 2.6 | F |
| Culhane (2002)43 | PPMC | $20,830 | $18,640 | 0.9 | G |
| Flaming (2009)a54 | PPMC | $15,737 | $32,715 | 2.1 | F |
| Flaming (2009)b54 | PPMC | $15,651 | $36,014 | 2.3 | F |
| Flaming (2009)c54 | PPMC | $15,951 | $34,558 | 2.2 | F |
| Flaming (2009)d54 | PPMC | $16,051 | $44,625 | 2.8 | F |
| Flaming (2013)44 | WLC | $32,955 | $52,193 | 1.6 | G |
| Gilmer (2010)47 | PPMC | $3,921a | $1,312 | 0.3 | F |
| Larimer (2009)50 | WLC | $17,069 | $54,392 | 3.2 | G |
| Seligson (2013)a51 | PPMC | $16,873 | $17,854 | 1.1 | G |
| Seligson (2013)b51 | PPMC | $29,105 | $37,630 | 1.3 | G |
| Seligson (2013)c51 | PPMC | $29,154 | $28,729 | 1.0 | G |
| Seligson (2013)d51 | PPMC | $25,567 | $12,344 | 0.5 | G |
| Srebnik (2013)56 | PPC | $20,274a | $35,705 | 1.8 | G |
| Toros (2012)57 | PPC | $34,104 | $26,907 | 0.8 | F |
| Goering (2014)a58 | RCT | $20,143 | $19,344 | 1.0 | G |
| Goering (2014)b58 | RCT | $12,830 | $4,388 | 0.3 | F |
| Latimer (2019)59 | RCT | $11,553 | $1,993 | 0.2 | F |
| Patterson (2008)a60 | Modeled | $16,586 | $17,750 | 1.1 | F |
| Patterson (2008)b60 | Modeled | $14,994 | $17,750 | 1.2 | F |
| Patterson (2008)c60 | Modeled | $19,249 | $17,750 | 0.9 | F |
| Summary Median (IQI) | — | U.S. studies $16,873 (IQI: $15,651 to $25,567) U.S. studies with good quality $20,830 (IQI: $17,069 to $29,105) All studies $16,586 (IQI: $13,912 to $20,552) |
U.S. studies $28,729 (IQI: $17,016 to $36,014) U.S. studies with good quality $28,729 (IQI: $17,854 to $37,630) All studies $18,640 (IQI: $15,605 to $35,132) |
U.S. studies 1.80 (IQI: 1.00 to 2.60) U.S. studies with good quality $1.3 (IQI: $1.0 to $1.8) All studies 1.06 (IQI: 0.87 to 1.84) |
— |
Does not include management and overhead costs.
PPMC, pre post with matched control; PPC, pre post with control; WLC, wait list control; PPPY, per person per year; NR, not reported; NA, not applicable; PPPY, per person per year; G, good; F, fair; IQI, interquartile interval.
Of the 23 intervention cost estimates, 18 (12 studies)41,43,47,49–51,53,54,56–59 were of good quality and the remaining 5 (3 studies)44,55,60 were of fair quality. The most frequent limitations were small sample size and valuation based on sources external to the study. Of the 25 economic benefit estimates, 12 (8 studies)41,43,44,50,51,54,56,58 were of good quality and 13 (10 studies)41,45–48,52,57–60 were of fair quality. The most frequent limitations were inappropriate comparison group and valuation based on sources external to the study.
Intervention Cost
Table 2 shows the median cost PPPY for U.S. studies was $16,479 (IQI=$13,120–$26,452; 12 studies).41,43,44,47,49–51,53–57 For U.S. studies with good-quality estimates, the median was $17,069 (IQI=$4,947–$27,336; 10 studies).41,43,44,47,49–51,53,56,57 The magnitude of intervention cost for U.S. studies was not substantially different between good quality estimates and all estimates. The median PPPY for all studies was $16,336 (IQI=$13,371–$20,691; 15 studies).41,43,44,47,49–51,53–60
For the U.S. studies, the intervention cost per person did not necessarily decrease with larger trials; the median for trials with 29–209 people was $11,29741,44,47,50,53,55–57 and for trials with 279–4,679 people the median was $16,479.43,49,51,54 The median intervention cost of $29,105 for U.S. studies of individuals with mental health or SUD51,53,57 was much higher than that of people with only mental health disorders (median=$17,963)43,47,54,56 or only SUD (median=$17,069).50,54,55 A total of three studies47,53,56 likely underestimated intervention cost because they did not include management and overheads.
Economic Benefit
Table 2 shows the median total benefit PPPY for U.S. studies was $18,247 (IQI=$7,522–$35,418; 13 studies).41,43–48,50–52,54,56,57 Note that 3 of these estimates45,46,48 indicated costs were increasing. Considering the U.S studies with good-quality estimates, the median total benefit was $33,637 (IQI=$18,051–$37,227; 7 studies).41,43,44,50,51,54,56 The magnitude of benefit was substantially larger for good-quality estimates from U.S studies. The median total benefit PPPY for all studies was $17,751 (IQI=$5,761–$33,177; 16 studies).41,43–48,50–52,54,56–60
For the U.S. studies, the median healthcare cost averted was −$11,248 (IQI= −29,731–$315; 12 studies),41,43–48,51,52,54,56,57 where a negative sign indicates healthcare cost decreased. All but 6 of the 21 estimates from 5 studies45–48,51 indicated that healthcare cost decreased. Three of the U.S. studdies45,48,52 did not provide estimates of averted cost beyond healthcare cost.
For U.S. studies where averted costs were from healthcare or the judicial system, the median averted cost PPPY was −$14,193 (IQI= −$21,962 to −$6,968; 5 studies).41,46,47,56,57 Adding those studies that also included changes in other welfare assistance or housing assistance, the averted cost grew to a median of −$26,907 (IQI= −$35,705 to −$12,624; 9 studies).41,43,44,46,47,51,54,56,57 It is clear that averted cost estimates reported by studies increase the more comprehensive they are in capturing the effects of the program on other social services.
The median averted cost PPPY of −$22,381 for U.S. studies of people that have mental health disorders or SUD51,52,57 was much higher than the median of −$1,312 for individuals with only mental health disorders.43,45–48,54,56 It is worth noting that programs for the homeless groups that represented >1 disabling condition such as mental health disorders had higher intervention cost while also averting greater societal costs.
Benefit-to-Cost Ratio
Table 3 shows the median benefit-to-cost ratio for U.S. studies was 1.80 (IQI=1.00–2.60; 9 studies).19,41,44,47,50,51,54,56,57 The median benefit-to-cost ratio for good-quality estimates from the U.S. studies was 1.30 (IQI=1.00–1.80; 6 studies).19,41,44,50,51,56 Further exclusion of U.S studies with wait list44,50 or convenience56 comparison groups and those that selected participants from among high utilizers of services44,50,56 produced a median benefit-to-cost ratio of 1.05 (IQI=0.93–1.25; 3 studies).41,43,51 These subgroup analyses for the U.S studies indicate the favorable summary for cost–benefit estimates is robust under stricter standards for evidence. The median benefit-to-cost ratio was 1.06 (IQI=0.87–1.84; 12 studies)19,41,44,47,50,51,54,56–60 for all studies combined, including the studies in Canada.
Looking more closely at the U.S. cost–benefit estimates that were of good quality19,41,44,50,51,56 versus good or fair,19,41,44,47,50,51,54,56,57 the median of the intervention cost component was $20,830 (IQI=$17,069–$29,105) versus $16,873 (IQI=$16,651–$25,567) and the median of the benefits component was $28,729 (IQI=$17,854–$37,630) versus $28,729 (IQI=$17,016–$36,014). Management and overhead cost were not included in 2 studies,47,56 likely underestimating the intervention cost. It may be surmised that intervention cost is underestimated, and benefits are appropriately estimated in the literature that reported cost–benefit.
DISCUSSION
Two recent reviews of the evidence for Housing First programs could not reach conclusions about the economic merits of the programs. Aubry et al.32 found mixed evidence whether the averted societal costs exceeded the cost to implement. The National Academy61 review found the evidence did not demonstrate a favorable net cost. There is substantial concordance between the set of studies included in the Aubry and colleagues32 review and those in the present review, whereas the earlier National Academy61 review included only RCTs or quasi-experimental designs that assessed only healthcare cost impacts. The present review distinguishes itself from the Aubry et al.32 review by focusing on U.S. studies in keeping with the mission of CPSTF and the exclusion of 4 studies42,49,53,55 that did not provide the final cost–benefit or cost-effectiveness outcomes of interest to the CPSTF.
A recent study from Canada62 that was published after the end of search period of the present review found the averted societal costs of Housing First programs designed to support participants with serious mental illness covered about 69% of the cost to implement the program. This is in line with the included studies from Canada that reported cost–benefit estimates <1.
With the caveat in mind that there were only a handful of studies from Canada, the cost to implement was comparable between the U.S and Canadian studies but the averted costs were far greater in the U.S studies (Table 2). Some explanations for the difference are explored here. Averted cost of healthcare was a far larger contributor to the overall costs averted in U.S studies than in the few Canadian studies that reported the information. It is well known that the U.S expenditures on health care are higher than other high-income countries.63 Focusing on acute care, U.S spending was 10% higher than other high-income countries in 1960, 21% higher in 1980, and 55% higher in 2007.64 Comparing hospital care and physician services in 2002 between the U.S and Canada, the per capita (per 1,000 population) cost in the U.S was $2,870 in the U.S and $1,281 in Canada, a difference of $1,598.65
An alternative approach to understanding the differences in averted costs found in U.S versus Canadian implementations of Housing First programs is to take an ecological perspective that recognizes the different social and policy milieu experienced by the homeless in the 2 countries. Studies that report cost of homelessness can provide an estimate for the maximum avertable social cost that a program to reduce homelessness can potentially produce. One study23 in Philadelphia reported $10,800 PPPY in utilization of social services by people experiencing chronic homelessness in 2002 and another study43 in New York City reported $62,000 PPPY for individuals with severe mental health disabilities. A Canadian study66 reported utilization of social services by homeless individuals in British Columbia, Canada ranged between $4,700 and $93,600 during the late 1990s. Although these do not constitute a systematic review of the evidence, the estimates from the cited studies are indicative of the large potential for averted costs in both the U.S. and Canada.
One can also compare the safety net provided by countries through their social programs that may ameliorate or prevent the circumstances that precede homelessness. Among the statistics published by the Organisation for Economic Co-operation and Development are public social expenditures (excluding income effects of tax policy) as a percentage of GDP.67 For family support, public social expenditures in 1990 were 0.5% in the U.S. and 0.6% in Canada and in 2018 they were 0.6% and 1.6%. For housing support, public social expenditures in 1990 were 0.3% in the U.S. and 0.6% in Canada and in 2018 they were 0.2% and 0.3%. For other social policy areas such as food subsidies, public social expenditures in 1990 were 0.4% in the U.S. and 2.4% in Canada and in 2018 they were 0.7% and 2.3%.67 These Organisation for Economic Co-operation and Development statistics indicate Canada spent a larger share of GDP on public social expenditures. A recent examination of historic trends in social safety net expenditures in the U.S. found that although public social expenditures as a percentage of GDP showed a consistently increasing trend, the gross statistics hide disparate trends along the spectrum of income level and family type.68 From the 1980s through 2005, there were redistributions of supports away from non-elderly and nondisabled families to older adults and families with disabilities; away from non-elderly, nondisabled single-parent families to married-parent families; and away from the poorest single-parent and married-parent families to those just below or just above the federal poverty threshold. Between 1984 and 2004, the reduction in government transfers in real terms were 35% for single-parent families and 31% for married-parent families.68 The Great Recession of 2008 interrupted the negative trend for those in the lowest income levels below the poverty line with increased social expenditures which were sustained post-recession; however, the disparate treatment in favor of those just above or just below the poverty line continued.69 The smaller overall safety net and the recent trends disparately affecting the poorest groups in the U.S. are potential contributors to greater economic hardships that foster and sustain homelessness in the U.S compared with Canada.
Limitations
No included studies examined the economics of Housing First Programs in rural communities. Some cost–benefit studies were incomplete in their capture of components known a priori to be drivers of intervention cost such as the cost of supportive healthcare services54 or drivers of benefits such as averted cost of shelters.41,47,54,56,57 The focus of the latter studies appeared to be on benefits from averted healthcare cost and averted cost of crime and policing.
It can be argued61 a better measure of the economic merits of programs whose objective is to reduce homelessness among people living with disabling chronic conditions may be cost per QALY or cost per DALY studies because the QALY/DALY accounts for improved health. However, none were found in the search. This said, benefit-to-cost ratios are useful information for potential implementers and funders by identifying what it costs to implement a program strategy and what types of societal costs may be expected to be recouped owing to its success.
Evidence from this systematic economic review shows the economic benefits exceed the intervention cost for Housing First Programs in the U.S. The conclusion is based on the weight of evidence summarized in the median and IQI for the ratio of benefit to cost for Housing First programs implemented in the U.S. There were too few studies to determine the cost–benefit of Housing First programs in the Canadian context.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank members of our coordination team from the Centers for Disease Control and Prevention and from partner organizations. The authors acknowledge Yolanda Strayhorn, MLIS from the Office of Library Science at the Centers for Disease Control and Prevention for her assistance in library research.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Homeless Emergency Assistance and Rapid Transition to Housing: Defining “Chronically Homeless”. Department of Housing and Urban Development. 80 FR 75791. https://www.federalregister.gov/documents/2015/12/04/2015-30473/homeless-emergency-assistance-and-rapid-transition-to-housing-defining-chronically-homeless. Published 2015. Accessed September 16, 2021. [Google Scholar]
- 2.Institute of Medicine, Committee on Health Care for Homeless People. Homelessness, health, and human needs. Washington, DC: National Academies Press; 1988. [Google Scholar]
- 3.Chamberlain C, Johnson G. Pathways into adult homelessness. J Sociol (Melb). 2013;49(1):60–77. 10.1177/1440783311422458. [DOI] [Google Scholar]
- 4.Thompson RG Jr, Wall MM, Greenstein E, Grant BF, Hasin DS. Substance-use disorders and poverty as prospective predictors of first-time homelessness in the United States. Am J Public Health. 2013;103(suppl 2):S282–S288. 10.2105/ajph.2013.301302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Laere IR, de Wit MA, Klazinga NS. Pathways into homelessness: recently homeless adults problems and service use before and after becoming homeless in Amsterdam. BMC Public Health. 2009;9:3. 10.1186/1471-2458-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Montgomery AE, Cutuli J, Evans-Chase M, Treglia D, Culhane DP. Relationship among adverse childhood experiences, history of active military service, and adult outcomes: homelessness, mental health, and physical health. Am J Public Health. 2013;103(suppl 2):S262–S268. 10.2105/ajph.2013.301474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roos LE, Mota N, Afifi TO, Katz LY, Distasio J, Sareen J. Relationship between adverse childhood experiences and homelessness and the impact of axis I and II disorders. Am J Public Health. 2013;103(suppl 2):S275–S281. 10.2105/ajph.2013.301323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown RT, Goodman L, Guzman D, Tieu L, Ponath C, Kushel MB. Pathways to homelessness among older homeless adults: results from the HOPE HOME Study. PLoS One. 2016;11(5):e0155065. 10.1371/journal.pone.0155065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Piat M, Polvere L, Kirst M, et al. Pathways into homelessness: understanding how both individual and structural factors contribute to and sustain homelessness in Canada. Urban Stud. 2015;52(13):2366–2382. 10.1177/0042098014548138. [DOI] [Google Scholar]
- 10.Tsai J Lifetime and 1-year prevalence of homelessness in the US population: results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. J Public Health (Oxf). 2018;40(1):65–74. 10.1093/pubmed/fdx034. [DOI] [PubMed] [Google Scholar]
- 11.Tsai J, Rosenheck RA. Risk factors for homelessness among US veterans. Epidemiol Rev. 2015;37(1):177–195. 10.1093/epirev/mxu004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fazel S, Geddes JR, Kushel M. The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 2014;384(9953):1529–1540. 10.1016/s0140-6736(14)61132-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson G, Chamberlain C. Homelessness and substance abuse: which comes first? Australian Social Work. 2008;61(4):342–356. 10.1080/03124070802428191. [DOI] [Google Scholar]
- 14.Lebrun‐Harris LA, Baggett TP, Jenkins DM, et al. Health status and health care experiences among homeless patients in federally supported health centers: findings from the 2009 patient survey. Health Serv Res. 2013;48(3):992–1017. 10.1111/1475-6773.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lewer D, Aldridge RW, Menezes D, et al. Health-related quality of life and prevalence of six chronic diseases in homeless and housed people: a cross-sectional study in London and Birmingham, England. BMJ Open. 2019;9(4):e025192. 10.1136/bmjopen-2018-025192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martens W A review of physical and mental health in homeless persons. Public Health Rev. 2001;29(1):13–33. [PubMed] [Google Scholar]
- 17.Caton CL, Dominguez B, Schanzer B, et al. Risk factors for long-term homelessness: findings from a longitudinal study of first-time homeless single adults. Am J Public Health. 2005;95(10):1753–1759. 10.2105/ajph.2005.063321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caton CL, Wilkins C, Anderson J. People who experience long-term homelessness: characteristics and interventions. In: Toward Understanding Homelessness: The 2007 National Symposium on Homelessness Research. HHS, U.S. Department of Housing and Urban Development; 2007. [Google Scholar]
- 19.Culhane DP. The cost of homelessness: a perspective from the United States. Eur J Homelessness. 2008;2(1):97–114. [Google Scholar]
- 20.Fuehrlein BS, Cowell AJ, Pollio DE, Cupps LY, Balfour ME, North CS. Deriving costs of service use among an urban homeless population. J Subst Abuse Treat. 2014;46(4):491–497. 10.1016/j.jsat.2013.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Latimer EA, Rabouin D, Cao Z, et al. Costs of services for homeless people with mental illness in 5 Canadian cities: a large prospective follow-up study. CMAJ Open. 2017;5(3):E576–E585. 10.9778/cmajo.20170018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parsell C, Petersen M, Culhane D. Cost offsets of supportive housing: evidence for social work. Br J Soc Work. 2017;47(5):1534–1553. 10.1093/bjsw/bcw115. [DOI] [Google Scholar]
- 23.Poulin SR, Maguire M, Metraux S, Culhane DP. Service use and costs for persons experiencing chronic homelessness in Philadelphia: a population-based study. Psychiatr. Serv 2010;61(11):1093–1098. 10.1176/ps.2010.61.11.1093. [DOI] [PubMed] [Google Scholar]
- 24.Wu F, Stevens M. The Services Homeless Single Adults Use and their Associated Costs. https://homeless.lacounty.gov/wp-content/uploads/2019/02/homeless-costs-final.pdf. Published 2016. Accessed May 23, 2020.
- 25.Henry M, Watt R, Mahathey A, Ouellette J, Sitler A. The 2019 Annual Homeless Assessment Report (AHAR) to Congress. Part 1: point-in-time estimates of homelessness. https://www.hudexchange.info/resource/5948/2019-ahar-part-1-pit-estimates-of-homelessness-in-the-us/. Published 2020. Accessed July 31, 2020.
- 26.National Alliance to End Homelessness. Ending chronic homelessness saves taxpayers money. http://endhomelessness.org/wp-content/uploads/2017/06/Cost-Savings-from-PSH.pdf. Published 2015. Accessed May 23, 2020.
- 27.Housing and Urban Development. Housing First in Permanent Supportive Housing. https://files.hudexchange.info/resources/documents/Housing-First-Permanent-Supportive-Housing-Brief.pdf. Published 2014. Accessed May 10, 2021.
- 28.Tsemberis S, Gulcur L, Nakae M. Housing first, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am J Public Health. 2004;94(4):651–656. 10.2105/ajph.94.4.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.The Guide to Community Preventive Services (the Community Guide). About the Community Preventive Services Task Force. https://www.thecommunityguide.org/task-force/about-community-preventive-services-task-force. Accessed September 16, 2021.
- 30.The Guide to Community Preventive Services (the Community Guide). Health Equity: Permanent Supportive Housing with Housing First (Housing First Programs). Snapshot. https://www.thecommunityguide.org/findings/health-equity-housing-first-programs. Accessed September 16, 2021.
- 31.Peng Y, Hahn RA, Finnie RK, et al. Permanent supportive housing with housing first to reduce homelessness and promote health among homeless populations with disability: a Community Guide Systematic Review. J Public Health Manag Pract. 2020;26(5):404–411. 10.1097/phh.0000000000001219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aubry T, Bloch G, Brcic V, et al. Effectiveness of permanent supportive housing and income assistance interventions for homeless individuals in high-income countries: a systematic review. Lancet Public Health. 2020;5(6):e342–e360. 10.1016/s2468-2667(20)30055-4. [DOI] [PubMed] [Google Scholar]
- 33.Eichler HG, Kong SX, Gerth WC, Mavros P, Jönsson B. Use of cost‐effectiveness analysis in health‐care resource allocation decision‐making: how are cost‐effectiveness thresholds expected to emerge? Value Health. 2004;7(5):518–528. 10.1111/j.1524-4733.2004.75003.x. [DOI] [PubMed] [Google Scholar]
- 34.WHO. Macroeconomics and health: investing in health for economic development: report of the Commission on Macroeconomics and Health. Macroeconomics and health: investing in health for economic development: report of the commission on macroeconomics and health. https://apps.who.int/iris/bitstream/handle/10665/42435/924154550X.pdf;sequence=1. Published 2001. Accessed September 16, 2021.
- 35.The Guide to Community Preventive Services (the Community Guide). Methods Manual - Part 2: Economic Review Process. https://www.thecommunityguide.org/methods-manual/economic-review-methods. Accessed September 22, 2021.
- 36.The Guide to Community Preventive Services (the Community Guide). The Community Guide Staff. https://www.thecommunityguide.org/about/community-guide-staff. Accessed June 15, 2021.
- 37.The World Bank. World Bank Country and Lending Groups. https://data.worldbank.org/about/country-and-lending-groups. Accessed September 16, 2021.
- 38.The Guide to Community Preventive Services (the Community Guide). Health Equity: Permanent Supportive Housing with Housing First (Housing First Programs). Supporting materials: Search Strategies – Economic Review. https://www.thecommunityguide.org/findings/health-equity-housing-first-programs. Accessed September 16, 2021.
- 39.Bureau of Labor Statistics. Databases, Tables & Calculators by Subject: CPI for All Urban Consumers (CPI-U). https://data.bls.gov/timeseries/CUUR0000SA0?output_view=pct_1mth. Accessed September 16, 2021.
- 40.The World Bank. Purchasing Power Parities. PPP conversion factor, private consumption. https://data.worldbank.org/indicator/PA.NUS.PRVT.PP. Accessed September 16, 2021.
- 41.Basu A, Kee R, Buchanan D, Sadowski LS. Comparative cost analysis of housing and case management program for chronically ill homeless adults compared to usual care. Health Serv Res. 2012;47(1 Pt 2):523–543. 10.1111/j.1475-6773.2011.01350.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Byrne T, Roberts CB, Culhane DP, Kane V. Estimating cost savings associated with HUD-VASH placement. Research Brief, National Center on Homelessness among Veterans, U.S. Department of Veterans Affairs; 2014. https://www.va.gov/HOMELESS/Estimating_Cost_Savings_Associated_With_HUD_VASH_Placement.pdf. Accessed September 16, 2021. [Google Scholar]
- 43.Culhane DP, Metraux S, Hadley TR. The impact of supportive housing for homeless people with severe mental illness on the utilization of the public health, corrections, and emergency shelter systems: the New York-New York Initiative. Hous Policy Debate. 2002;13(1):107–163. 10.1080/10511482.2002.9521437. [DOI] [Google Scholar]
- 44.Flaming D, Lee S, Burns P, Sumner G. Getting home: Outcomes from housing high cost homeless hospital patients [preprint]. SSRN. Posted May 2, 2016. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2772242. Accessed May 25, 2020.
- 45.Gilmer TP. Permanent supportive housing for transition-age youths: service costs and fidelity to the housing first model. Psychiatr Serv. 2016;67(6):615–621. 10.1176/appi.ps.201500200. [DOI] [PubMed] [Google Scholar]
- 46.Gilmer TP, Manning WG, Ettner SL. A cost analysis of San Diego County’s REACH program for homeless persons. Psychiatr Serv. 2009;60(4):445–450. 10.1176/ps.2009.60.4.445. [DOI] [PubMed] [Google Scholar]
- 47.Gilmer TP, Stefancic A, Ettner SL, Manning WG, Tsemberis S. Effect of full-service partnerships on homelessness, use and costs of mental health services, and quality of life among adults with serious mental illness. Arch Gen Psychiatry. 2010;67(6):645–652. 10.1001/archgenpsychiatry.2010.56. [DOI] [PubMed] [Google Scholar]
- 48.Gilmer TP, Stefancic A, Tsemberis S, Ettner SL. Full-service partnerships among adults with serious mental illness in California: impact on utilization and costs. Psychiatr Serv. 2014;65(9):1120–1125. 10.1176/appi.ps.201300380. [DOI] [PubMed] [Google Scholar]
- 49.Holtgrave DR, Wolitski RJ, Pals SL, et al. Cost-utility analysis of the housing and health intervention for homeless and unstably housed persons living with HIV. AIDS Behav. 2013;17(5):1626–1631. 10.1007/s10461-012-0204-3. [DOI] [PubMed] [Google Scholar]
- 50.Larimer ME, Malone DK, Garner MD, et al. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA. 2009;301(13):1349–1357. 10.1001/jama.2009.414. [DOI] [PubMed] [Google Scholar]
- 51.Levanon Seligson A, Lim S, Singh T, et al. New York/New York III Supportive housing evaluation: interim utilization and cost analysis. A report from the New York City Department of Health and Mental Hygiene in collaboration with the New York City Human Resources Administration and the New York State Office of Mental Health. https://shnny.org/images/uploads/NY-NY-III-Interim-Report.pdf. Published 2013. Accessed April 10, 2020. [Google Scholar]
- 52.Lim S, Gao Q, Stazesky E, Singh TP, Harris TG, Levanon Seligson A. Impact of a New York City supportive housing program on Medicaid expenditure patterns among people with serious mental illness and chronic homelessness. BMC Health Serv Res. 2018;18:15. 10.1186/s12913-017-2816-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rosenheck R, Kasprow W, Frisman L, Liu-Mares W. Cost-effectiveness of supported housing for homeless persons with mental illness. Arch Gen Psychiatry. 2003;60(9):940–951. 10.1001/archpsyc.60.9.940. [DOI] [PubMed] [Google Scholar]
- 54.Flaming D, Burns P, Matsunaga M. Where we sleep. Costs when homeless and housed in Los Angeles [preprint]. SSRN. Posted May 2, 2016. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2772796. Accessed September 16, 2021. [Google Scholar]
- 55.Schinka JA, Francis E, Hughes P, LaLone L, Flynn C. Comparative outcomes and costs of inpatient care and supportive housing for substance-dependent veterans. Psychiatr Serv. 1998;49(7):946–950. 10.1176/ps.49.7.946. [DOI] [PubMed] [Google Scholar]
- 56.Srebnik D, Connor T, Sylla L. A pilot study of the impact of housing first-supported housing for intensive users of medical hospitalization and sobering services. Am J Public Health. 2013;103(2):316–321. 10.2105/ajph.2012.300867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Toros H, Stevens M, Moreno M. Project 50: The cost effectiveness of the permanent supportive housing model in the skid row section of Los Angeles County. http://zevyaroslavsky.org/wp-content/uploads/Project-50-Cost-Effectiveness-report-FINAL-6-6-12.pdf. Published 2012. Accessed May 24, 2020.
- 58.Goering P, Veldhuizen S, Watson A, et al. National Final Report. Cross-site at Home/Chez Soi Project (Calgary, AB: Mental Health Commission of Canada; ). https://www.mentalhealthcommission.ca/sites/default/files/mhcc_at_home_report_national_cross-site_eng_2_0.pdf. Published 2014. Accessed April 15, 2020. [Google Scholar]
- 59.Latimer EA, Rabouin D, Cao Z, et al. Cost-effectiveness of housing first intervention with intensive case management compared with treatment as usual for homeless adults with mental illness: secondary analysis of a randomized clinical trial. JAMA Netw Open. 2019;2(8):e199782. 10.1001/jamanetworkopen.2019.9782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Patterson M, Somers J, McIntosh K, Shiell A, Frankish CJ. Housing and support for adults with severe addictions and/or mental illness in British Columbia. https://www.health.gov.bc.ca/library/publications/year/2007/Housing_Support_for_MHA_Adults.pdf. Published 2007. Accessed April 10, 2020.
- 61.National Academies of Sciences, Engineering, and Medicine. Permanent supportive housing: evaluating the evidence for improving health outcomes among people experiencing chronic homelessness. Washington, DC: The National Academies Press; 2018. 10.17226/25133. [DOI] [PubMed] [Google Scholar]
- 62.Latimer EA, Rabouin D, Cao Z, et al. Cost-effectiveness of housing first with assertive community treatment: results from the Canadian At Home/Chez Soi Trial. Psychiatr Serv. 2020;71(10):1020–1030. 10.1176/appi.ps.202000029. [DOI] [PubMed] [Google Scholar]
- 63.Fernandes A Health at a Glance 2019. Paris, France: OECD Publishing; 2019. [Google Scholar]
- 64.Cutler DM, Ly DP. The (paper) work of medicine: understanding international medical costs. J Econ Perspect. 2011;25(2):3–25. 10.1257/jep.25.2.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pozen A, Cutler DM. Medical spending differences in the United States and Canada: the role of prices, procedures, and administrative expense5s. Inquiry. 2010;47(2):124–134. 10.5034/inquiryjrnl_47.02.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Eberle MP. Homelessness, Causes & Effects, Vol. 3: The Costs of Homelessness in British Columbia. Ministry of Social Development & Economic Security; 2001. http://www.urbancentre.utoronto.ca/pdfs/researchassociates/4_vol_report/Vol3.pdf. Accessed September 16, 2021.
- 67.OECD. Social Expenditures Database (SOCX). Published 2019.
- 68.Moffitt RA. The deserving poor, the family, and the US welfare system. Demography. 2015;52(3):729–749. 10.1007/s13524-015-0395-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Moffitt RA, Pauley G. Trends in the distribution of social safety net support after the Great Recession. Palo Alto, CA: Stanford Center on Poverty and Inequality; 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


