As the COVID-19 pandemic goes on, we continue to identify the long-term complications or symptoms among patients who recovered from this infection, be it mild or severe.1 These complications are collectively recognized as “COVID-19 long-hauler syndrome”.1 It is crucial to understand the factors leading to the development of these long-term sequelae to identify, prevent and manage them using appropriate interventions.
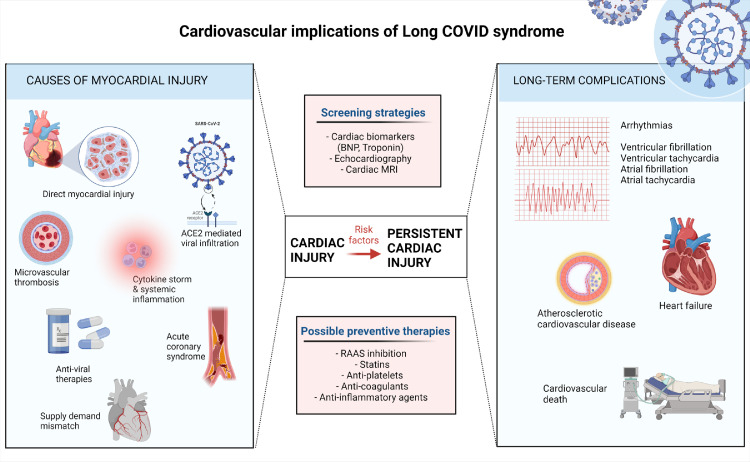
Acute cardiac injury (ACI), marked by elevation of troponin levels in the blood over the 99th percentile, is an important phenomenon shown to occur in nearly 30% of patients admitted to the hospital with COVID-19 infection.2 ACI has been shown to be associated with an elevated risk of critical illness, increased duration of hospital stay and mortality.2,3 Multiple processes, both ischaemic and non-ischaemic, have been shown to contribute to the development of ACI in COVID-19 patients. The most important among them is the direct myocardial injury caused by SARS-CoV-2.4 Tavazzi et al. demonstrated direct viral infection in the interstitial cells of the myocardium on endomyocardial biopsy, accompanied by low-grade inflammation.4 But to date, there has been no demonstration of COVID-19 genome in the cardiac tissue in patients with clinical myocarditis. Other mechanisms postulated to increase myocardial injury include systemic inflammation, vascular endothelial damage, cardiomyocyte apoptosis, abnormal myocardial strain, microthrombi formation and supply-demand mismatch (Figure 1).2 The precise mechanisms of myocardial injury in patients with COVID-19 are still unclear. It is also unknown if the myocardial injury is a direct effect of the virus or a response to systemic inflammation or both.
Figure 1.
Cardiovascular implications of long COVID-19 syndrome. ACE2 – Angiotensin converting enzyme 2. BNP – Brain natriuretic peptide. RAAS – Renin- angiotensin aldosterone system.
Created with BioRender.com.
As we continue to obtain long-term data on COVID-19 survivors, it is imperative to look at how the patients with troponin elevation during their hospital admission fair after discharge. We read with interest the article by Lu et al.5 on the importance of persistent cardiac injury in patients with previous COVID-19 and the factors associated with its development. Among the 673 patients who developed ACI and had a follow-up visit, 371 patients (55.1%) had persistent elevation in troponin levels over a median follow-up of 2.5 months. The authors have made a significant case that COVID-19 is associated with persistent cardiac injury in some patients even after the primary infection has resolved. This highlights the long-term cardiac involvement in patients with COVID-19 in the convalescent period. The clinical relevance of these persistently elevated troponin levels on left ventricular function and other cardiovascular outcomes is still to be determined. A retrospective study from the SWEDEHEART database showed that, among 48,482 COVID 19 patients with elevated cardiac troponin levels (>99 percentile) without a diagnosis of acute coronary syndrome, 7529 patients (15.4%) developed long-term major adverse cardiac events, defined as the composite of all-cause mortality, myocardial infarction, readmission for heart failure, or stroke, over a median follow-up of 4.9 years.6 Kotecha et al. performed cardiac magnetic resonance (CMR) studies in 148 patients with severe COVID-19 and persistent troponin elevation at a median of 68 days post-discharge and observed late gadolinium enhancement and/or ischaemia in 54% of patients.7 Though multiple studies have shown a high frequency of abnormalities on CMR within 1-2 months following SARS-CoV-2 infection, Joy et al. demonstrated that the CMR features are similar in patients with mild COVID-19 illness compared with seronegative healthy individuals, 6 months after SARS-CoV-2 infection.8 However, the long-term CMR abnormalities and their clinical relevance remain to be ascertained.9 Even when the COVID-19 infection has resolved and the individual is no longer infective, he/she might still harbor SARS-CoV-2 RNA in various tissues in the body for up to 230 days.10 This could be one of the mechanisms leading to persistent cardiac injury.10 There are yet major gaps in our understanding of the mechanisms by which SARS-CoV-2 affects the blood vessels and the myocardium, and in turn affects the development of important clinical syndromes like atherosclerosis and heart failure.
Although most of current treatment measures have concentrated on the management of acute illness, multiple trials on the use of various medications and their effects on outcomes in patients with COVID-19 are ongoing.9 Prospective studies are essential to better appreciate the lasting cardiovascular consequences of the long COVID-19 syndrome. It is important to formulate the surveillance guidelines among select groups of patients to identify electrophysiologic, morphologic and functional abnormalities. Consideration should be given for advanced imaging such as CMR, particularly in high-risk patients during follow-up. In that context, whether persistent elevation of troponin points towards a high risk of development of long-term cardiac complications and whether elevated troponin levels is a useful and cost-effective method of screening is to be tested. Optimal screening guidelines for patients after recovery from COVID-19 should be determined to prevent cardiovascular complications in a vast majority of the population.
Contributors
V Chidambaram, A Kumar wrote the first draft and prepared the images. G Calcaterra, J L Mehta edited and revised the final draft.
Declaration of interests
The authors report no existing conflicts of interest.
References
- 1.Nalbandian A., Sehgal K., Gupta A., et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27:601–615. doi: 10.1038/s41591-021-01283-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bavishi C., Bonow R.O., Trivedi V., Abbott J.D., Messerli F.H., Bhatt D. Special article - acute myocardial injury in patients hospitalized with COVID-19 infection: a review. Prog Cardiovasc Dis. 2020;63:682–689. doi: 10.1016/J.PCAD.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chidambaram V., Tun N.L., Haque W.Z., et al. Factors associated with disease severity and mortality among patients with COVID-19: a systematic review and meta-analysis. PLoS One. 2020;15 doi: 10.1371/journal.pone.0241541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tavazzi G., Pellegrini C., Maurelli M., et al. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail. 2020;22:911–915. doi: 10.1002/EJHF.1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lu J.Q., Lu J.Y., Wang W., et al. Clinical predictors of acute cardiac injury and normalization of troponin after hospital discharge from COVID-19. EBioMedicine. 2022 doi: 10.1016/j.ebiom.2022.103821. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eggers K.M., Jernberg T., Lindahl B. Cardiac troponin elevation in patients without a specific diagnosis. J Am Coll Cardiol. 2019;73:1–9. doi: 10.1016/J.JACC.2018.09.082. [DOI] [PubMed] [Google Scholar]
- 7.Kotecha T., Knight D.S., Razvi Y., et al. Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance. Eur Heart J. 2021;42:1866–1878. doi: 10.1093/EURHEARTJ/EHAB075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Joy G., Artico J., Kurdi H., et al. Prospective case-control study of cardiovascular abnormalities 6 months following mild COVID-19 in healthcare workers. JACC Cardiovasc Imaging. 2021;14:2155–2166. doi: 10.1016/J.JCMG.2021.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Satterfield B.A., Bhatt D.L., Gersh B.J. Cardiac involvement in the long-term implications of COVID-19. Nat Rev Cardiol. 2021;2021:1–10. doi: 10.1038/s41569-021-00631-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chertow D, Stein S, Ramelli S. et al. SARS-CoV-2 infection and persistence throughout the human body and brain n.d. 10.21203/rs.3.rs-1139035/v1. [DOI]