Abstract
Background
Emergency obstetric care training, using Advances in Labour and Risk Management (ALARM) International Program (AIP) was implemented in Ukraine, a country with universal access to skilled perinatal and obstetric care but restricted resources. A total of 577 providers (65.5% of total) from 28 maternal clinics attended a 5-day training session focused on the five main causes of maternal mortality, with hands-on skill workshops, pre- and post- tests, and an objective structured clinical examination. The effects of this emergency obstetric care training on maternal outcomes is the subject of this paper.
Methods
A non-randomized controlled trial was conducted. The pilot areas where the training was implemented consisted of 64 maternity clinics of which 28 were considered as cases and 36 non-participating clinics were the referents. Data on maternal outcomes were collected for a 2-year span (2004-2005) prior to the trainings, which took place 2006-2007 and again after implementation of the trainings, from 2008 to 2009. Information was collected from 189,852 deliveries. Outcomes for the study were incidences of operative delivery and postpartum hemorrhage. Non-parametric statistics, meta-analyses, and difference in difference (DID) estimation were used to assess the effect of the AIP on maternal indices.
Results
DID analysis showed that after the training, compared to the referents, the cases had significant reduction of blood transfusions (OR: 0.56; 95%CI: 0.48-0.65), plasma transfusions (OR: 0.70; 95%CI: 0.63-0.78), and uterus explorations (OR: 0.64; 95%CI: 0.59-0.69). We observed a non-significant reduction of postpartum hemorrhage ≥1000 ml (OR: 0.92; 95%CI: 0.81-1.04; P = 0.103). Utilization of vacuum extraction for vaginal delivery increased (OR: 2.86; 95%CI: 1.80-4.57), as well as forceps assisted delivery (OR: 1.80; 95%CI: 1.00-3.25) and cesarean section (OR: 1.11; 95%CI: 1.06-1.17). There was no change in the occurrence of postpartum hysterectomy and maternal mortality.
Conclusions
After one week of Emergency Obstetrics Care training of the obstetric staff in a setting with universal access to perinatal and obstetric care but restricted resources, an association with the reduction of postpartum hemorrhage related interventions was observed. The effects on the use of vacuum extraction and cesarean section were minimal.
Trial registration
Retrospectively registered 071212007807 from 07/12/2012.
Keywords: Emergency obstetric care, Training, Evaluation, Effectiveness, Health outcomes, Postpartum hemorrhage, Vacuum extraction, Ukraine
Background
Training programs in Emergency Obstetrics Care (EmOC) are common, and the results of such trainings are well described [1–7]. There are four levels to assess effectiveness of training in EmOC: first, the reaction of participants, second, the improvement of knowledge, and skills, third, changes in providers’ behavior and practices, and fourthly, EmOC availability and health outcomes [8]. That said, detailed analyses of the effects of a training program on outcome measures, including maternal and perinatal mortality and morbidity, were for the most part, contradictory. Whereas some studies demonstrate improvement in perinatal outcomes [9] and reduction in postpartum hemorrhage (PPH) [10], others show no effect of obstetric skills training on the rate of red blood transfusion for PPH [11], the rate of PPH [12], or the adverse outcome index [13].
The Society of Obstetricians and Gynecologists of Canada established the Advances in Labour and Risk Management (ALARM) International Program (known collectively as AIP) in 1998 to assist in the global reduction of maternal and neonatal mortality and morbidity. AIP was designed to motivate and encourage health professionals to improve the delivery of emergency obstetric care in low and middle income countries [14]. The 5-day AIP course is based on adult learning principles that promote a collaborative, multidisciplinary approach of working and learning together. It focuses on the five main causes of maternal mortality: obstructed labor, hemorrhage, sepsis, hypertensive disorders and complications due to unsafe abortion [14]. Participants are also sensitized to factors that impede women’s access to reproductive health services and information [15].
Despite universal access to perinatal and obstetric care, health outcomes for mothers and infants in Eastern European countries are far less favorable than those reported from Western Europe. In Ukraine, despite nearly all women deliver in hospital, attended by an obstetrician-gynecologist, maternal mortality is still much higher than in Western Europe [16].
From 2006 to 2009, Ukraine was one of eleven project countries within the International Federation of Gynecology and Obstetrics (FIGO), “Saving Mothers and Newborns Initiative”, a program that aimed to contribute to the reduction of maternal and newborn morbidity and mortality in targeted countries. The primary tool to achieve those objectives in Ukraine was the AIP [17].
The AIP program in Ukraine was implemented in two pilot regions, Donetsk and Vinnytsia with Ministry of Health (MOH) support. We hypothesized that AIP training would be followed by a decline in important adverse maternal and perinatal outcomes. The aim of this publication is to evaluate the effect of the AIP on selected maternal outcomes at the pilot facilities.
Methods
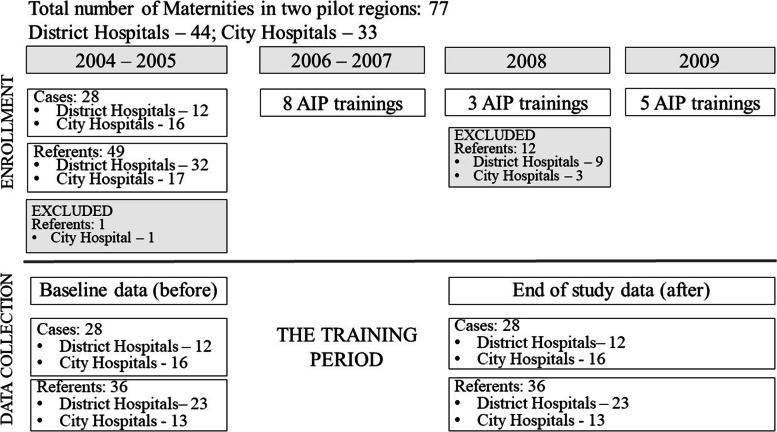
To study the effect of the AIP on maternal and neonatal outcomes, a quasi-experimental design was used. A non-randomized controlled trial was conducted (Fig. 1).
Fig. 1.
Study design to evaluate effectiveness of the emergency obstetric care training in Ukraine
Obstetrical facilities from the pilot area (Donetsk and Vinnytsia regions) included in the ALARM International trainings were considered as cases whereas those that did not participate were the referents
In 2005, the Donetsk region, a highly industrial region in the eastern part of Ukraine, was home to approximately 1.2 million women of reproductive age. The number of deliveries that year was 35,319, cared for in 44 in-patient Maternal Care facilities (17 district hospitals and 27 city hospitals). These facilities were staffed with approximately 1600 midwives and 1300 obstetrician-gynecologists. The second pilot region was Vinnytsia, a rural region in central Ukraine with around 400,000 women of reproductive age. Here, the number of deliveries in 2005 was 14,640, in 33 in-patient Maternal Care facilities (27 district hospitals and 6 city hospitals) staffed by approximately 700 midwives and 400 obstetrician-gynecologists. Approximately half of the providers in both regions were involved in the care of women and neonates during delivery and labor.
Fourteen of 44 facilities in Donetsk and 14 of 33 facilities in Vinnytsia region were designated as project clinics with a total of 881 targeted providers. Those facilities were selected by Regional Public Health Administrations (RPHAs). The 28 facilities from the pilot area included in the AIP training initiative were considered as cases, whereby the remaining 49 facilities served as referents. One city hospital was excluded from the referent group as it was a site used for another project. Each of the 76 facilities was considered as a unit.
During 2006-2007, a total of 28 pilot facilities in the two Ukrainian regions participated in eight AIP training sessions. In 2008, an additional three trainings were conducted. On the request of RPHAs, professionals from 12 referent maternity units were invited to the trainings. Therefore, those 12 units were excluded from the referents. Five AIP training sessions were arranged in 2009. Again, on the request of the RPHAs, an additional 11 facilities from the referent group were invited to the AIP in the second half of 2009. Since those facilities were involved so late in the trainings, no effect on maternal and perinatal outcomes was expected in 2009. Therefore, we decided not to exclude them from the referents. Distribution of facilities by annual number of deliveries is presented in Table 1.
Table 1.
Distribution of facilities involved in the study by number of deliveries per year in 2004
| Number of deliveries per year | Cases, n | Referents, n | Total, n |
|---|---|---|---|
| < 500 | 11 | 21 | 32 |
| 500 - 999 | 7 | 12 | 19 |
| 1000 - 2000 | 9 | 3 | 12 |
| > 2000 | 1 | - | 1 |
| Total | 28 | 36 | 64 |
In total, 342 obstetrician-gynecologists and 235 midwives from the case clinics were trained during 2006-2009 and average coverage for the staff training was 65.5%, varying from 28.6 to 100%. Staff retention rate was close to 100% in all maternity units in the area, during the period under observation.
The AIP training educational environment includes interactive plenary sessions and hands-on skill workshops with obstetrical mannequins, thus allowing all participants the opportunity to address individual learning needs. Sessions were accompanied by pre- and post- tests which measured knowledge and practice skills, including objective structured clinical examinations that required the participant to demonstrate clinical skills [14, 15]. A 2-hour monitoring and refresh session on PPH was conducted in the case units in late 2009.
In Ukraine, statistics are based upon annual reports from the regional departments of medical statistics, which rely upon quarterly hospital reports. No case-based registers were available in the country at the time of the AIP implementation. Hospital reports compiled information from local case records and contained some aggregated data but no personal characteristics of the patients. Before the project was started, a specially designed hospital record form was developed and approved by the RPHAs for collecting hospital data in the suggested project area. Data cannot be linked to any individual patient. These forms were completed by the statisticians in the maternity units from official hospital statistics, since 2001 retrospectively, and since 2005 prospectively. They were checked for consistency by chief-doctors, collected and entered into the database by the investigator.
Information was collected on an annual basis for number of deliveries, live-births, percentage of pre-term births, multiple births, vacuum and forceps delivery, cesarean section (CS), PPH, cases where exploration of uterus was performed, blood or plasma transfusion, postpartum hysterectomy along with Maternal Mortality Ratio per 100,000 live-births (MMR), perinatal deaths (per 1000), and neonatal morbidity (per 1000). PPH was recorded for blood loss 1000 ml or more within 24 h of the birth process, regardless of the route of delivery, and was evaluated by weighing the amount/output [18, 19], according to Ukraine MOH recommendations. To more accurately determine the actual postpartum blood loss and to diminish the effect of amniotic fluid and urine (in vaginal birth) on PPH quantification, after delivery of the placenta, large absorbent pads were changed in vaginal birth and amount of fluid in suction canister was counted for in cesarean section. Irrigation fluid was collected in another canister. All blood-soaked materials and clots as well as fluid volume collected were weighed on a scale in grams. The dry item’s gram weight was subtracted. 1gram weight was considered equal to 1 milliliter of blood loss volume [20]. Total PPH blood loss was recorded after the obstetric team judged that PPH had stopped. Information on 189,852 deliveries was collected.
For this study, data were selected from the database for a 2-year span (2004-2005) prior to trainings and then the 2 years (2008-2009) following the training period at all maternity units of the project area, including both cases and referents. These 2 interim years, 2006-2007 were roll-out periods, defined as transition periods and therefore data for that period were not included in the study. Data for two referent maternity units were collected only for one-year after (2008), since due to the facility closing for renovations 2009 data were not available.
Data obtained for each unit and each year were treated separately as continuous relative indices. As samples for all indices were not normally distributed (Shapiro-Wilk W test), the median with interquartile range (IQR) was calculated prior to and after the training (before, after) in two groups (the cases and the referents). In the univariate analyses, Wilcoxon rank-sum tests were applied. The JMP (SAS Institute, Cary, NC, 1994) program package was used for data-entering and analyses.
Taking into account the large difference in the number of births at the facilities and non-normal distribution of samples, in order to provide a numerical estimate of the overall effect of interest, a meta-analysis was done to calculate the weighted summary proportions under the fixed (Freeman-Tukey transformation (arcsine square root transformation) [21] or random [22] effects model (after test for heterogeneity). A meta-analysis integrates the quantitative findings of maternal indices from each unit and each year for the cases and the referents, the groups before and after the AIP implementation. MedCalc software 20.013 was used to calculate the weighted average indices with 95% CI [23].
Difference-in-differences (DID) analysis was applied to compare outcome changes overtime between the case and the referent groups to evaluate the impact of the AIP on maternal indices by linear regression model [24]. Statistical software EZR v.1.54 (graphical user interface for R statistical software version 4.0.3, R Foundation for Statistical Computing, Vienna, Austria) [25] was used to calculate DID estimators with 95%CI and OR of DID with 95%CI.
The study was approved by the Ethical Committee of the Institute of Medical Problems of Family of the Donetsk National Medical University (DNMU) (Protocol 24, November 7, 2012). The study was retrospectively registered at the DNMU Register, Nu 071212007807 from 07/12/2012.
Results
During the study period there was an increase in the number of births both in the case maternity units (from 47,838 in 2004-2005 to 61,116 in 2008-2009) and in the referents (from 38,032 in 2004-2005 to 42,866 in 2008-2009) with more pronounced increase among the cases.
Non-parametric statistics (Table 2) revealed that at the baseline CS and forceps assisted delivery was more often utilized among the cases. There were no differences in other indices.
Table 2.
Maternal outcomes and some obstetric interventions before and after the training period
| Nu | Indices | Before (2004 – 2005) | After (2008 – 2009) | Before vs After | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases (n=28) | Referents (n=36) | Z1-2 | P 1-2 | Cases (n=28) | Referents (n=36) | Z3-4 | P 3-4 | Cases (n=28) |
Referents (n=36) |
||||||||
| Median | IQR | Median | IQR | Median | IQR | Median | IQR | ||||||||||
| 1 | 2 | 3 | 4 | Z1-3 | P 1-3 | Z2-4 | P 2-4 | ||||||||||
| Number of deliveries | 47 838 | 38 032 | 61 116 | 42 866 | |||||||||||||
| 1 | Vacuum assisted delivery, % | 0 |
0-0 Max 0.77 |
0 |
0-0 Max 1.71 |
0.43 | 0.669 | 0.31 |
0-0.98 Max 4.58 |
0 |
0-0.44 Max 2.53 |
3.59 | 0.000 | -5.64 | < 0.000 | 2.51 | 0.012 |
| 2 | Forceps assisted delivery, % | 0.04 |
0-0.30 Max 2.24 |
0 |
0-0 Max 1.17 |
2.95 | 0.003 | 0 |
0-0 Max 1.40 |
0 |
0-0 Max 0.70 |
1.56 | 0.118 | 3.10 | 0.002 | -1.85 | 0.064 |
| 3 | Cesarean section, % | 11.30 | 8.82-13.09 | 8.33 | 5.79-13.05 | 2.42 | 0.015 | 12.82 | 9.70-15.59 | 10.54 | 7.42 -14.47 | 2.50 | 0.012 | -1.93 | 0.053 | 1.959 | 0.050 |
| 4 | Postpartum hemorrhage, % | 2.24 | 1.22-5.98 | 1.83 | 1.19-4.11 | 1.19 | 0.233 | 1.98 | 0.85-2.70 | 1.72 | 1.01-2.75 | 0.07 | 0.941 | 2.19 | 0.029 | 0.998 | 0.318 |
| 5 | Uterus exploration, % | 5.49 | 1.58-8.88 | 6.12 | 3.16-11.89 | -1.73 | 0.084 | 2.98 | 1.32-4.94 | 4.44 | 2.71-8.09 | -3.25 | 0.001 | 2.46 | 0.014 | -1.94 | 0.053 |
| 6 | Blood transfusion, % | 1.28 | 0.61-2.20 | 1.70 | 0.69-2.49 | -0.84 | 0.399 | 0.84 | 0.36-1.36 | 0.92 | 0.31-1.71 | -0.63 | 0.528 | 2.58 | 0.010 | -2.88 | 0.004 |
| 7 | Plasma transfusion, % | 2.18 | 0.57-4.36 | 1.93 | 1.39-5.90 | -0.96 | 0.337 | 2.05 | 0.70- 3.53 | 1.80 | 0.88-4.30 | -0.41 | 0.684 | 0.32 | 0.746 | -1.23 | 0.219 |
| 8 | Hysterectomy postpartum, % | 0.11 |
0-0.25 Max 2.04 |
0 |
0-0.34 Max 2.17 |
0.003 | 0.998 | 0.15 |
0-0.31 Max 1.74 |
0.18 |
0-0.39 Max 1.09 |
-0.66 | 0.506 | -0.62 | 0.532 | 0.97 | 0.333 |
The median with interquartile range (IQR) is presented. Maximum is added where medians and IQRs were equal to 0. Wilcoxon rank-sum test was used to study difference between the cases and the referents before and after the training period. P-values<0.05 were considered significant (seen in bold). Data on Maternal Mortality Ratio and Maternal Mortality Ratio related to postpartum hemorrhage was excluded from the Table as medians and IQRs for all points were equal to 0
After the training there was a minor increase in vacuum assisted delivery in both groups. Use of forceps assisted delivery declined in both groups, but only for the cases was that decrease significant. CS rate increased from 2004 to 2005 to 2008-2009, yet it was not significant for either the cases or the referents.
PPH with blood loss 1000 ml or more and uterus exploration decreased significantly among the cases, whereas PPH decline among the referents was not significant, neither for the rate of uterus exploration. Blood transfusions were reduced significantly in both groups, but no change in plasma transfusion and postpartum hysterectomy was found after the training, not for the cases nor the referents. No changes in MMR nor MMR related to PPH was observed.
At the end of the study (2008-2009), vacuum assisted delivery was slightly more frequent among the cases. CS rate was still higher among those units involved in the AIP, whereas uterus exploration was less used as compared to the referents.
When meta-analyses were performed, there was no difference between the cases and the referents at the baseline.
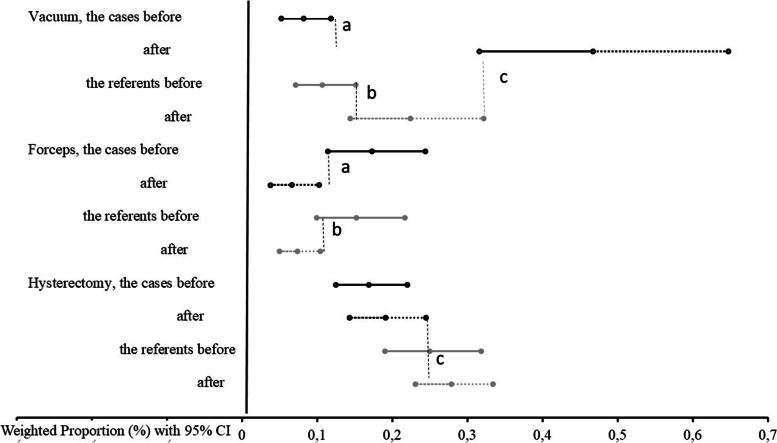
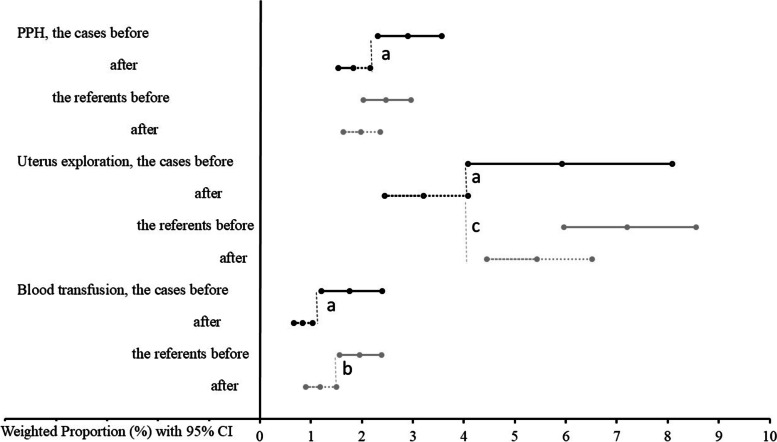
Data on weighted average indices with 95% CI demonstrated significant changes and are presented in Figs. 2 and 3. Among the cases, after the AIP implementation there was a significant increase in vacuum-assisted delivery, and decreases noted in the following: forceps assisted delivery, PPH, uterus exploration and blood transfusion. Also at the referent maternity units, there was a significant increase in vacuum assisted deliveries, a decrease in forceps assisted delivery and in blood transfusions.
Fig. 2.
Effect of the emergency obstetric care training on instrumental vaginal delivery and postpartum hysterectomy rate
Weighted average indices calculated using meta-analyses framework for the cases (n=28) and the referents (n=36) before and after the training with 95%CIs (the whiskers). Black lines represent indices’ values for the cases and grey lines - for the referents. Solid lines indicate groups “before”, dotted lines – “after” the training. P<0.05 for the difference of a the cases before compared with the cases after, b the referents before and after, c the cases and the referents after the training. CI: confidence interval
Fig. 3.
Weighted average rates of postpartum hemorrhage and related activities on regional scale after staff training
Weighted average indices calculated using meta-analyses framework for the cases (n=28) and the referents (n=36), before and after the training with 95%CIs (the whiskers). Black lines represent indices’ values for the cases and grey lines - for the referents. Solid lines indicate groups “before”, dotted lines – “after” the training. P<0.05 for the difference of a the cases before compared with the cases after, b the referents before and after, c the cases and the referents after the training. CI: confidence interval
At the end of the study (2008-2009) vacuum assisted deliveries occurred 2.1 times more often among the cases, whereas uterus exploration was 2.2 times more often and postpartum hysterectomy was 1.5 times more common among the referents.
There were no significant changes in CS rate between the case (11.3; 95% CI: 10.1-12.5 vs. 13.2; 95% CI: 11.7-14.8) and referent maternity units (9.7; 95% CI: 8.3-11.2 vs. 11.2; 95% CI: 9.9-12.7) during the study period.
There were 12 maternal deaths at the baseline and 18 maternal deaths at the end of the study.
Weighted indices showed no difference in MMR per 100,000 live births between the cases and the referents neither before (35.8; 95% CI: 21.0-57.2 vs. 52.2; 95% CI: 31.8-80.7) nor after the training period (37.0; 95% CI: 23.4-55.7 vs. 45.1; 95% CI: 27.3-70.1). The same was true for MMR related to PPH: 28.8; 95% CI: 15.7-48.4 vs. 45.8; 95% CI: 26.9-72.9, and 28.8; 95% CI: 12.5-38.3 vs. 37.1; 95% CI: 21.2-60.3.
Table 3 summarizes the DID analysis’s outcomes.
Table 3.
Effect of the AIP training on maternal indices: difference in difference (DID) estimation
| Outcome variable | Referents, N (%) | Cases, N (%) | DID | p | |||
|---|---|---|---|---|---|---|---|
| Before, n=38,032 |
After, n=42,866 |
Before, n=47,838 |
After, n=61,116 |
DID estimator (95%CI) |
OR (95%CI) | ||
| Postpartum hemorrhage |
905 (2.38) |
747 (1.74) |
1255 (2.62) |
1081 (1.77) |
-0.22 (-0.48 to 0.04) |
0.92 (0.81-1.04) |
0.103 |
| Uterus exploration |
2929 (7.70) |
2521 (5.88) |
3977 (8.31) |
2530 (4.14) |
-2.35 (-2.80 to -1.91) |
0.64 (0.59-0.69) |
<0.001 |
| Blood transfusion |
851 (2.24) |
635 (1.48) |
1008 (2.11) |
476 (0.48) |
-0.57 (-0.80 to -0.35) |
0.56 (0.48-0.65) |
<0.001 |
| Plasma transfusion |
1415 (3.72) |
1120 (2.61) |
2181 (4.56) |
1392 (2.28) |
-1.12 (-1.50 to -0.85) |
0.70 (0.63-0.78) |
<0.001 |
| Hysterectomy postpartum |
101 (0.27) |
109 (0.25) |
75 (0.16) |
109 (0.18) |
0.03 (-0.05 to 0.13) |
1.19 (0.80-1.77) |
0.439 |
| Vacuum assisted delivery |
41 (0.11) |
111 (0.26) |
48 (0.10) |
420 (0.69) |
0.44 (0.33 - 0.54) |
2.86 (1.80-4.57) |
<0.001 |
| Forceps assisted delivery |
80 (0.21) |
23 (0.05) |
80 (0.17) |
47 (0.08) |
0.07 (0.00 - 0.13) |
1.80 (1.00-3.25) |
0.041 |
| Cesarean section |
4706 (12.37) |
5884 (13.73) |
6278 (13.12) |
9734 (15.93) |
1.45 (0.82 - 2.08) |
1.11 (1.06-1.17) |
<0.001 |
N in each box of the second row corresponds to number of deliveries in the groups “before” and “after” the AIP training implementation. Difference in difference (DID) estimator was estimated using linear regression model. DID is presented as estimator (%) with 95% CI, and OR with 95%CI. The P-value is presented for DID estimator. CI: confidence interval; OR: odds ratio
The estimates in the models for the maternal indices suggest that likelihood of uterus exploration, blood transfusion, and plasma transfusion was less for the cases. Reduction was significant. Cases of PPH were non-significant, less after the AIP training. Vacuum assisted, forceps assisted delivery and CSs were more common after the training. The effect of the AIP training on operative delivery was significant. No effect of the AIP training was found on postpartum hysterectomy, MMR, and MMR related to PPH (Table 4).
Table 4.
Effect of the AIP training on maternal death: difference in difference (DID) estimation
| Outcome variable | Referents, N (per 100,000) |
Cases, N (per 100,000) |
DID | p | |||
|---|---|---|---|---|---|---|---|
| Before n=38,076 |
After n=42,872 |
Before n=47,992 |
After n=61,330 |
DID estimator (95%CI) | OR (95%CI) | ||
| Maternal Mortality Ratio |
5 (13.1) |
5 (11.7) |
7 (14.6) |
13 (21.2) |
8.1 (-14.8 to 31.0) |
1.64 (0.35-7.66) |
0.490 |
| Maternal Mortality Ratio related to postpartum hemorrhage |
2 (5.25) |
1 (2.33) |
2 (4.17) |
3 (4.89) |
3.6 (-8.2 to 15.5) |
2.64 (0.13-52.8) |
0.546 |
N in each box of the second row corresponds to number of live-births in the groups “before” and “after” the AIP training implementation. N in boxes related to maternal mortality ratio are numbers of women who died. Index is calculated per 100,000 live-births. Difference in difference (DID) estimator was estimated using linear regression model. DID presented as estimator (per 100,000) with 95% CI, and OR with 95%CI. The P-value is presented for DID estimator. CI: confidence interval; OR: odds ratio
Discussion
Our findings show that implementation of the AIP training at regional level in Ukraine resulted in a significant decline in PPH related interventions, namely uterus exploration (by 36%), blood transfusion (by 44%), and plasma transfusion (by 30%). We observed a non-significant 8% reduction in PPH among the cases. There was a small but significant increase in the use of vacuum (by 186%), forceps assisted delivery (by 80%), and CS (by 11%) after the training. Postpartum hysterectomy, MMR and MMR related to PPH were not affected by the AIP.
This paper represents the first time that the results of the AIP, with emphasis on outcome measures, are described at the regional level in a country with restricted resources but universal access to skilled perinatal and obstetric care.
When the ALARM course was introduced, litigation against those who had taken the course, was shown to decline [26]. Our previous evaluations have reported the experiences of AIP in developing professionals’ responsibility in promoting women’s sexual and reproductive health and rights in Ukraine [27], as well as demonstrated the project’s successes and challenges [17]. A cluster-randomized trial was initiated in Mali and Senegal in 2007 to evaluate effectiveness of complex intervention with AIP training, in reducing maternal mortality [28]. Maternal death review combined with implementation of best practices was effective to reduce hospital base maternal mortality in the first level referral hospitals [29]. The AIP training conducted at a Teaching and Referral Hospital in Kenya with 80% staff coverage demonstrated significant increase in Oxytocin use for active management of the third stage of labor and a decrease in PPH [30].
For more than 30 years, oxytocin has been used routinely after birth in Ukraine to prevent PPH. The data from our training project indicate that AIP training was associated with a downward trend in PPH. Including a quantitative measurement of blood loss during the AIP training could improve the accuracy and reliability of gravimetric technique [31] and may have resulted in a lower threshold for diagnosing PPH [32]. Since there was a significant increase in operative deliveries [32] with increased PPH risk [31] this might lead to less significant PPH reduction after the AIP training. CS increase was significant after the AIP training which is in line with other studies [32]. Vacuum assisted delivery increased in both groups after the training.
Historically, blood transfusion rate is regarded as a more objective and reliable indicator of blood loss [32]. We have found that the AIP training was associated with significant reduction in blood and plasma transfusion. In the referent clinics there was also a significant reduction in blood transfusions. This can probably be explained by the MOH PPH protocol with a strong recommendation to proceed with blood transfusion only if hemoglobin is less than 70 g/l and hematocrit is less than 0.25 l/l (MOH Order 782, 29.12.2005). We can’t exclude effect of that order also in the cases.
Significant reduction in uterus exploration is another indirect measure of PPH decline. If after placenta delivery uterine bleeding does not stop promptly, PPH management protocol is applied [15]. When less invasive measures are not successful (uterotonics, external and bimanual uterus compression) uterus exploration is utilized if doubt exists about the potential for retained products or blood clots.
Our findings may reflect the broad coverage in AIP of many different aspects of PPH prevention / management [33], including partograph use, delayed and obstructed labor management, operative birth, prevention of primary CS, vaginal birth after CS, shoulder dystocia, multiple birth, premature rupture of the membrane, maternal infection, preeclampsia and implementation of the AIP PPH prevention/management evidence-based protocol, which further has been introduced and promoted by FIGO [34]. Therefore, not only training in PPH management as such, but coverage of all risk factors for excessive postpartum bleeding during the training was crucial [15] to improve outcomes. It is not likely that the short PPH monitoring and refresh sessions in late 2009 did effect the results obtained.
The PPH management protocol was introduced in Ukraine by the MOH (Order 676, 31.12.2004), but still there was a difference in the need for PPH related interventions between those who participated in the AIP course and those who did not, clearly related to the AIP training. Items included during the AIP training were: correct active management of the third stage of labor technique with controlled cord traction only with well contracted uterus and after signs of separation of the placenta [34]; uterotonics prescription according to FIGO recommendations; use of external and bimanual uterus compression prior to uterus exploration when examined placenta is complete; aorta compression as an early intervention to stop massive bleeding and reduce blood loss, and intrauterine balloon tamponade with glove to reduce the need for surgical intervention.
Postpartum hysterectomy and maternal death are the most severe PPH related morbidities [35]. Our data showed no changes in postpartum hysterectomy, MMR and MMR related to PPH neither in the maternity units where AIP was implemented nor where it was not, but the sample size was not large enough to demonstrate any change in these rare events. The MMR in the area corresponds to the World Bank estimates of MMR in Ukraine during 2004-2009 [36].
There are many factors related to maternal and perinatal outcomes. Therefore, changes in health outcomes, attributed to training in EmOC, are difficult to measure [8]. During the study period several other activities in the country could affect maternal outcomes. Since 2002, the Maternal and Infant Health Project, an 8-year project implemented by John Snow Inc Research and Training Institute, has worked successfully in the country with the aim to improve the quality of services by implementing evidence-based perinatal technologies [37, 38]. Since 2005 there has been active promotion of the Kiwi Vacuum Assisted Delivery System use in Ukraine. Video with training material from Dr. Aldo Vacca was widely distributed within the country. Still, as demonstrated from our data, vacuum assisted vaginal delivery is uncommon in Ukraine even if it significantly increased after the AIP. This is similar to a study from Mozambique [39].
An acknowledged weakness of our approach is that the project sites were not randomly selected, and it was not possible to stratify facilities by work load at the regional level since project sites selection was the RPHAs decision.
As the AIP Program was the only new Program introduced in the project facilities (cases) since 2006, it is likely that the changes observed in some maternal indices are associated with the AIP training. The observed differences in the maternal indices are subject for many unobserved confounding factors. As data obtained for analysis were only aggregated data it was impossible to adjust DID PPH estimator by other important factors with known effect on PPH. Collection of personalized information could resolve this issue, but was not the case in Ukraine at the time of the study.
Other limitations of the study are that the data used are relatively old and since the study examined the only the Ukrainian population, the effects in other patient populations is unknown.
The main strength of our study is the use of a large dataset to reflect change at regional level and lack of obstetric employee turnover during the study period. There was a constant increase in number of births in Ukraine and also in the project area during 2004-2009 [40]. The number of births increased more in the case clinics.
The experience from this study of a large-scale but time-limited training intervention of obstetric staff indicates that even a short training can significantly decrease the incidence of interventions related to a potentially life-threatening complication such as PPH and demonstrate a downward trend in PPH. The positive effect also seems to be extended for a longer time period. Among the activities necessary to improve obstetric care and maternal and perinatal health, goal-oriented training of staff should be a priority, especially in settings where skilled staff is the most important resource.
Conclusions
Re-training of obstetric staff with focus on EmOC in a setting with universal access to perinatal and obstetric care and restricted resources had positive effects as evidenced by a decrease in the incidence of PPH related interventions and downward trend in PPH.
Acknowledgements
The AIP trainings were the part of the FIGO “Saving Mothers and Newborns Initiative” in Ukraine “The ALARM International Plus (AIP) Program in Ukraine” implemented by Ukrainian Association of Obstetrician and Gynecologists, the Society of Obstetricians and Gynecologists of Canada, the Program for Appropriate Technology in Health and NGO “Ukrainian Medical Project”. Although the project was originally planned for 3.5 years (January 1, 2006 to June 30, 2009), funding was obtained from USAID/Capacity Project for the first 1.5 years only. Subsequent funding was found by FIGO in mid 2008 to continue the roll out of the AIP training as per originally planned in the project proposal. IM was a project leader. Additional training in 2007 was conducted with financial support from the Swiss Cooperation Office in Ukraine.
The authors would like to thank REDe Network and Sustainable Science Institute, for manuscript’s tree of arguments discussion during Scientific Manuscript Writing Workshop, Brazil, 2021.
We are grateful to chief-doctors of all maternities in Donetsk and Vinnytsia Regions for high interest to the AIP and completing specially designed annual hospital’s record forms.
Special appreciation to Chief Obstetrician / Gynecologists of Donetsk and Vinnytsia Regions, Dr. Nikiolay Shpatusko and Dr. Vladimir Boychuk, for support and assistance both in the AIP trainings implementation and data collection.
Abbreviations
- EmOC
Emergency Obstetrics Care
- FIGO
The International Federation of Gynecology and Obstetrics
- ALARM
Advances in Labour and Risk Management
- AIP
ALARM International Program
- PPH
Postpartum Hemorrhage
- MMR
Maternal Mortality Ratio
- CS
Cesarean Section
- MOH
Ministry of Health
- RPHAs
Regional Public Health Administrations
Authors’ contributions
IM contributed to the conception and design of the work, the acquisition, analysis and interpretation of data, drafting the work. VG contributed to the analysis and interpretation of data for the work, revising work critically. GL contributed to the design of the work and interpretation of data for the work, revision critically for important intellectual content. All authors read and approved the final manuscript.
Funding
The author(s) received no financial support for the research.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on request.
Declarations
Ethics approval and consent to participate
This study was carried out according to the Declaration of Helsinki. The study was approved by the Ethical Committee of the Institute of Medical Problems of Family of the Donetsk National Medical University (Protocol 24, November 7, 2012).
With support from the Regional Public Health Administrations data were collected using a specially designed hospital’s record form completed from the official hospital statistics, contained aggregated data but no personal characteristics of the patients. Data cannot be linked to any individual patients. Patients’ informed consent was waived by the Ethical Committee of the Institute of Medical Problems of Family of the Donetsk National Medical University.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Black RS, Brocklehurst P. A systematic review of training in acute obstetric emergencies. BJOG. 2003;110(9):837–41. doi: 10.1111/j.1471-0528.2003.02488.x. [DOI] [PubMed] [Google Scholar]
- 2.Cameron M, Hinshaw K. A systematic review of training in acute obstetric emergencies. BJOG. 2004;111(3):288. doi: 10.1111/j.1471-0528.2004.00084.x. [DOI] [PubMed] [Google Scholar]
- 3.van Lonkhuijzen L, Dijkman A, van Roosmalen J, Zeeman G, Scherpbier A. A systematic review of the effectiveness of training in emergency obstetric care in low-resource environments: Systematic review of training in obstetric emergencies. BJOG. 2010;117(7):777–87. doi: 10.1111/j.1471-0528.2010.02561.x. [DOI] [PubMed] [Google Scholar]
- 4.WKTo W. Training in emergency obstetric skills: is it evidence-based? Hon Kong Med J. 2011;17(2):141–6. [PubMed] [Google Scholar]
- 5.Anderson ER, Black R, Brocklehurst P. Acute obstetric emergency drill in England and Wales: a survey of practice. BJOG. 2005;112(3):372–5. doi: 10.1111/j.1471-0528.2005.00432.x. [DOI] [PubMed] [Google Scholar]
- 6.Crofts JF, Ellis D, Draycott TJ, Winter C, Hunt LP, Akande VA. Change in knowledge of midwives and obstetricians following obstetric emergency training: a randomised controlled trial of local hospital, simulation centre and teamwork training. BJOG. 2007;114(12):1534–41. doi: 10.1111/j.1471-0528.2007.01493.x. [DOI] [PubMed] [Google Scholar]
- 7.Ameh C, Adegoke A, Hofman J, Ismail FM, Ahmed FM, van den Broek N. The impact of emergency obstetric care training in Somaliland, Somalia. Int J Gynaecol Obstet. 2012;117(3):283–7. doi: 10.1016/j.ijgo.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 8.Ameh CA, Mdegela M, White S, van den Broek N. The effectiveness of training in emergency obstetric care: a systematic literature review. Health Policy Plan. 2019;34(4):257–70. doi: 10.1093/heapol/czz028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Draycott T, Sibanda T, Owen L, Akande V, Winter C, Reading S, et al. Does training in obstetric emergencies improve neonatal outcome? BJOG. 2006;113(2):177–82. doi: 10.1111/j.1471-0528.2006.00800.x. [DOI] [PubMed] [Google Scholar]
- 10.Rizvi F, Mackey R, Barrett T, McKenna P, Geary M. Successful reduction of massive postpartum haemorrhage by use of guidelines and staff education. BJOG. 2004;111(5):495–8. doi: 10.1111/j.1471-0528.2004.00103.x. [DOI] [PubMed] [Google Scholar]
- 11.Markova V, Sørensen JL, Holm C, Nørgaard A, Langhoff-Roos J. Evaluation of multi-professional obstetric skills training for postpartum hemorrhage: Obstetric skills and postpartum hemorrhage. Acta Obstet Gynecol Scand. 2012;91(3):346–52. doi: 10.1111/j.1600-0412.2011.01344.x. [DOI] [PubMed] [Google Scholar]
- 12.Strong N, Bianco A, Stone J, Zhenya P, Lambertini L. 631: The impact of postpartum hemorrhage drill training at a single institution. Am J Obstet Gynecol. 2012;206(1):S283. doi: 10.1016/j.ajog.2011.10.649. [DOI] [Google Scholar]
- 13.Nielsen PE, Goldman MB, Mann S, Shapiro DE, Marcus RG, Pratt SD, et al. Effects of teamwork training on adverse outcomes and process of care in labor and delivery: a randomized controlled trial: A randomized controlled trial. Obstet Gynecol. 2007;109(1):48–55. doi: 10.1097/01.AOG.0000250900.53126.c2. [DOI] [PubMed] [Google Scholar]
- 14.Lalonde AB, Beaudoin F, Smith J, Plourde S, Perron L. The ALARM international program: A mobilizing and capacity-building tool to reduce maternal and newborn mortality and morbidity worldwide. J Obstet Gynaecol Can. 2006;28(11):1004–5. doi: 10.1016/S1701-2163(16)32300-3. [DOI] [PubMed] [Google Scholar]
- 15.Advances in labor and risk management [Internet]. Glowm.com. [cited 2021 Mar 14]. Available from: https://www.glowm.com/resource_type/resource/textbook/title/advances-in-labor-and-risk-management/resource_doc/15
- 16.Maternal mortality rate - Country Comparison [Internet]. Indexmundi.com. [cited 2021 Mar 14]. Available from: https://www.indexmundi.com/g/r.aspx?v=2223
- 17.Mogilevkina I, Lalonde A, Perron L, Beaudoin F, Senikas V, Shpatusko N, et al. ALARM International Program in Ukraine: Roll Up Does not Mean End of the Project - Successes and Challenges, International Women’s Health Special Report 2008/ All Committed to Delivering a Better World, SOGC. 2008.
- 18.Diaz V, Abalos E, Carroli G. Methods for blood loss estimation aer vaginal birth (Review). Cochrane Database of Systematic Reviews [Internet]. 2018;(9). Available from: 10.1002/14651858.CD010980.pub2 [DOI] [PMC free article] [PubMed]
- 19.Hancock A, Weeks AD, Lavender DT. Is accurate and reliable blood loss estimation the “crucial step” in early detection of postpartum haemorrhage: an integrative review of the literature. BMC Pregnancy Childbirth [Internet]. 2015;15(230). Available from: 10.1186/s12884-015-0653-6 [DOI] [PMC free article] [PubMed]
- 20.American College of Obstetricians and Gynecologists. Quantitative blood loss in obstetric hemorrhage. ACOG Committee Opinion No. 794. Obstet Gynecol. 2019;134(6). [DOI] [PubMed]
- 21.Freeman MF, Tukey JW. Transformations related to the angular and the square root. ann math stat. 1950;21(4):607–11. doi: 10.1214/aoms/1177729756. [DOI] [Google Scholar]
- 22.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 23.MedCalc Software Ltd, Ostend, Belgium. MedCalc® Statistical Software version 20.013. 2021.
- 24.Gertler PJ, Martinez S, Premand P, Rawlings LB, Vermeersch ChMJ. Impact evaluation in practice. 2nd ed. Washington, D.C.: Inter-American Development Bank and World Bank. World Bank; 2016. 1. Available from: https://openknowledge.worldbank.org/handle/10986/25030.
- 25.Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8. doi: 10.1038/bmt.2012.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Windrim R, Ehman W, Carson GD, Kollesh L, Milne K. The ALARM course: 10 years of continuing professional development in intrapartum care and risk management in Canada. J Obstet Gynaecol Can. 2006;28(7):600–2. doi: 10.1016/S1701-2163(16)32212-5. [DOI] [PubMed] [Google Scholar]
- 27.Mogilevkina I, Shpatusko N, Morozova N, Kulik A, Senikas V, Perron L, et al. Seeking reproductive health care in Ukraine: what we learned from service providers. Entre Nous, The European Magazine for Sexual and Reproductive Health, Issue 70. 2010;18–9.
- 28.Dumont A, Fournier P, Fraser W, Haddad S, Traore M, Diop I, et al. QUARITE (quality of care, risk management and technology in obstetrics): a cluster-randomized trial of a multifaceted intervention to improve emergency obstetric care in Senegal and Mali. Trials. 2009;10(1):85. doi: 10.1186/1745-6215-10-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dumont A, Fournier P, Abrahamowicz M, Traoré M, Haddad S, Fraser WD, et al. Quality of care, risk management, and technology in obstetrics to reduce hospital-based maternal mortality in Senegal and Mali (QUARITE): a cluster-randomised trial. Lancet. 2013;382(9887):146–57. doi: 10.1016/S0140-6736(13)60593-0. [DOI] [PubMed] [Google Scholar]
- 30.Spitzer RF, Steele SJ, Caloia D, Thorne J, Bocking AD, Christoffersen-Deb A, et al. One-year evaluation of the impact of an emergency obstetric and neonatal care training program in Western Kenya. Int J Gynaecol Obstet. 2014;127(2):189–93. doi: 10.1016/j.ijgo.2014.05.023. [DOI] [PubMed] [Google Scholar]
- 31.Bell SF, Watkins A, John M, Macgillivray E, Kitchen TL, James D, et al. Incidence of postpartum haemorrhage defined by quantitative blood loss measurement: a national cohort. BMC Pregnancy Childbirth. 2020;20(1):271. doi: 10.1186/s12884-020-02971-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Egenberg S, Masenga G, Bru LE, Eggebø TM, Mushi C, Massay D, et al. Impact of multi-professional, scenario-based training on postpartum hemorrhage in Tanzania: a quasi-experimental, pre- vs. post-intervention study. BMC Pregnancy Childbirth [Internet]. 2017;17(1). Available from: 10.1186/s12884-017-1478-2 [DOI] [PMC free article] [PubMed]
- 33.Society of Obstetricians and Gynaecologists of Canada . ALARM International: A Program to Reduce Maternal and Neonatal Mortality and Morbidity. 4. Ottawa: SOGC Press; 2008. [Google Scholar]
- 34.Lalonde A. International Federation of Gynecology and Obstetrics. Prevention and treatment of postpartum hemorrhage in low-resource settings. Int J Gynaecol Obstet. 2012;117(2):108–18. doi: 10.1016/j.ijgo.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 35.Katz D, Farber MK. Can measuring blood loss at delivery reduce hemorrhage-related morbidity? Int J Obstet Anesth. 2021;46(102968):102968. doi: 10.1016/j.ijoa.2021.102968. [DOI] [PubMed] [Google Scholar]
- 36.World Bank. Ukraine Maternal Mortality Rate 2000-2021 [Internet]. www.macrotrends.net. 2011 [cited 2021 Nov 2]. Available from: a href=’https://www.macrotrends.net/countries/UKR/ukraine/maternal-mortality-rate’>Ukraine Maternal Mortality Rate 2000-2021
- 37.Nizalova OY, Vyshnya M. Evaluation of the impact of the Mother and Infant Health Project in Ukraine. Health Econ. 2010;19(Suppl(S1):107–25. doi: 10.1002/hec.1609. [DOI] [PubMed] [Google Scholar]
- 38.Berglund A, Lefevre-Cholay H, Bacci A, Blyumina A, Lindmark G. Successful implementation of evidence-based routines in Ukrainian maternities. Acta Obstet Gynecol Scand. 2010;89(2):230–7. doi: 10.3109/00016340903479894. [DOI] [PubMed] [Google Scholar]
- 39.Geelhoed D, de Deus V, Sitoe M, Matsinhe O, Lampião Cardoso M, Manjate C, et al. Improving emergency obstetric care and reversing the underutilisation of vacuum extraction: a qualitative study of implementation in Tete Province, Mozambique. BMC Pregnancy Childbirth 2018,18:266 10.1186/s12884-018-1901-3 [DOI] [PMC free article] [PubMed]
- 40.Center of medical statistics Ministry of Health, Ukraine. Statistical data for 2001-2009 (in Ukrainian) [Internet]. Statistical data. 2011 [cited 2020 Nov 5]. Available from: http://medstat.gov.ua/ukr/statdan.html
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on request.