Abstract
Purpose:
To identify postpartum depression risk and describe experiences of women in the first 6 weeks after giving birth during the COVID-19 pandemic.
Study Design and Methods:
Using a convergent mixed-methods approach, we recruited a convenience sample of women living in the United States who gave birth March 1, 2020 or later from social media Web sites. Participants completed the Postpartum Depression Screening Scale-Short Form and provided written answers to open-ended questions regarding their experiences at home with their new infant.
Results:
Our 262 participants were on average 32.6 years of age, the majority were White (82%), married or partnered (91.9%), and college educated (87.4%). Mean postpartum depression score was 17.7 (SD = 5.9) with 75% scoring ≥14, indicating significant postpartum depressive symptoms. Qualitative content analysis revealed five themes: Isolation and seclusion continue; Fear, anxiety, and stress filled the days; Grieving the loss of normal: It's just so sad; Complicated by postpartum depression: A dark time; and There is a silver lining. Quantitative and qualitative findings provided a holistic view of women's depressive symptoms and experiences at home with their infants during the COVID-19 pandemic.
Clinical Implications:
Although policies that reduce risk of COVID-19 exposure and infection for patients and the health care team must continue to be implemented, the adverse effects of depressive symptoms on maternal–infant wellbeing within the context of increased isolation due to the pandemic need to be kept at the forefront. Nurses need to be aware of the consequences of women sheltering in place and social distancing on maternal–infant outcomes, particularly on depression and likelihood of breastfeeding.
Key Words: COVID-19, Mixed methods, Pandemic, Postpartum depression, Pregnancy
Women experienced more postpartum depressive symptoms while trying to navigate the challenges of the COVID-19 pandemic than expected, based on prepandemic postpartum depression prevalence data. Seclusion and having minimal help with the new baby were noted to be very stressful for many new mothers. Some mothers expressed positive aspects of COVID-19 related postpartum isolation as being blessings in disguise and a silver lining because they were able to bond with the new baby and their partners while learning parenting together.
Figure.

No caption available.
COVID-19 was declared a pandemic in March 2020 by the World Health Organization. The United States responded by creating social distancing and sheltering in place guidelines to decrease COVID-19 exposure and infection, resulting in rapid changes to obstetric care delivery (American College of Obstetricians and Gynecologists, 2020; Peahl et al., 2020). Pandemics are associated with increased risk of developing mental health problems (Giarratano et al., 2019; Goyal & Selix, 2021) and can increase societal fear which is especially amplified in women with new babies (Dodgson et al., 2010).
Prepandemic postpartum depression (PPD) rates in the United States are estimated between 10% and 15% (Guintivano et al., 2018). A history of depression, poor social support, low socioeconomic status (Guintivano et al.; Pao et al., 2019; Silverman et al., 2017), and cesarean births (Moameri et al., 2019) are associated with developing PPD. Poor maternal quality of life and likelihood of breastfeeding (Dagher et al., 2021) are among the well-documented consequences of untreated PPD. Substantially higher rates of PPD have been observed in women who gave birth in the United States during the COVID-19 pandemic, 36.4% (Liu et al., 2021) as well as worldwide (31%; Basu et al., 2021) and 44.2% (Ostacoli et al., 2020). In a mixed-methods study (Farewell et al., 2020), 12% of perinatal women had higher depression scores during COVID-19 and qualitative themes included uncertainty about perinatal care, maternal–infant risk of COVID-19 exposure, lack of support networks, and inconsistent COVID-19 messaging. Women in Australia described grief from missing out on social events and family support in their posts to an online postpartum support group (Chivers et al., 2020). The COVID-19 pandemic provides a unique opportunity to examine mental health effects during postpartum and can be helpful in providing a framework to guide care during future pandemics.
To gain a holistic understanding of women's experiences during the COVID-19 pandemic, we used a mixed-methods design to answer the following questions about adult women discharged from the hospital and living in the United States: What is the severity of postpartum depressive symptoms among women in the first 6 weeks postpartum during the COVID-19 pandemic and what are the experiences of women at home with their infant(s) in the first 6 weeks after giving birth during the COVID-19 pandemic?
Study Design and Methods
Study approval was obtained from the university-affiliated institutional review board prior to recruitment and data collection. We used a convergent, parallel-mixed methods design for this study that involved simultaneous collection and analysis of qualitative and quantitative data (Creswell & Plano Clark, 2018). We used convenience and snowball sampling to recruit women from the social media site Facebook®. We searched Facebook® for new mothers' groups and sent requests to group administrators to post our study flyers. The study was open from March 1, 2020 through September 30, 2020. Women interested in participating accessed an online Qualtrics® link that included the informed consent statement and two questions to confirm eligibility (18 years of age, given birth to a live infant(s) on or after March 1, 2020). A list of perinatal mental health resources was included at the end of the survey for example, Postpartum Support International and 2020Mom. No compensation was provided for participation. Quantitative and qualitative strands were collected and analyzed independently in a single phase and both strands were equally prioritized. Once analyzed, findings from the quantitative and qualitative strands were merged and the researchers looked for comparisons (convergence) or divergence between them (Creswell & Plano Clark).
Quantitative Strand
To assess current depressive symptoms, we used the 7-item Postpartum Depression Screening Scale-Short Form (PDSS-SF; Beck & Gable, 2002). Questions reflect the following seven dimensions of the full-length 35-item scale: sleeping/eating disturbances, anxiety/insecurity, emotional lability, mental confusion, loss of self, guilt/shame, and suicidal thoughts (Beck & Gable). Items are scored on a 5-point Likert scale and can range from 7 to 35 with scores ≥14 identifying women with significant postpartum depressive symptoms.
The PDSS-SF has demonstrated good sensitivity, specificity, internal consistency, content, construct, and concurrent validity (Beck & Gable, 2002). The PDSS-SF has similar psychometric properties to the long form (Cai et al., 2019), and is accurate for PPD screening (Pereira et al., 2013). Cronbach's alpha for our sample was a = .829. We chose the PDSS-SF for our study given its robust development and psychometric profile and to decrease participant burden in completing the full 35-item scale. A sociodemographic questionnaire was also completed by women that included demographic (age, race-ethnicity, income, education level, marital status), mental health (previous history, current treatment), obstetric (vaginal or cesarean birth), and infant variables (gender, feeding method).
Qualitative Strand
Women were asked to provide written answers to the following statements: Please describe your experiences in the first six weeks at home with your infant(s) during the COVID-19 pandemic, and please describe any concerns you have about COVID-19 over the next few months. Participant's narrative responses helped provide context for the quantitative PDSS-SF scores.
Data Analysis
Quantitative Strand
A cut off score of ≥14 was used to categorize women as either “depressed” or “not depressed” (Depression Category). Descriptive statistics were used to summarize PDSS-SF scores and participant characteristics. One-way ANOVAs were used to identify differences in PDSS-SF scores among certain demographic, obstetric, infant, and mental health-related group factors. Maternal age and number of birth partners were correlated with PDSS-SF scores to identify any significant associations. To see if similar results were found by Depression Category, Chi-Square tests were conducted with Depression Category as the dependent variable, and demographic, obstetric, infant, and mental-health variables as the independent variables. Significant results from these tests were then used as predictor variables in a multiple regression to understand which variables best predict total PDSS-SF scores.
Qualitative Strand
Krippendorff's (2019) content analysis methods were used to analyze participants' experiences during the first 6 weeks postpartum. We chose thematic units as the unit of analysis and defined these units as segments of the women's descriptions of their postpartum experiences during the COVID-19 pandemic. We also used clustering (Krippendorff, 2019), a qualitative method that groups together data that reflect the same qualities as a theme. Dendrograms, treelike diagrams, were developed to aid in visualizing the data. See Figure 1 for an example of a dendrogram for Theme 2, Fear, Anxiety, and Stress Filled the Days.
FIGURE 1.
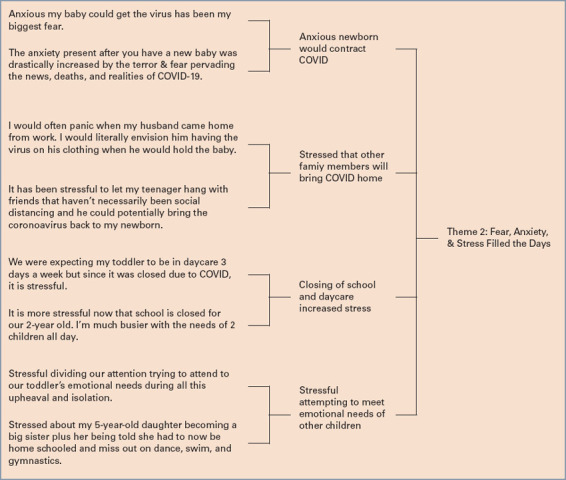
DENDROGRAM FOR THE THEME: FEAR, ANXIETY, AND STRESS FILLED THE DAYS
To ensure trustworthiness of the qualitative findings, the first (DG) and second (CB) authors, both with extensive experience in PPD and qualitative research methods, reviewed all 166 narrative responses individually. Any discrepancies were discussed and resolved together in a subsequent meeting and the data were organized into the five themes.
Results
Sample
Our sample included 262 women aged of 32.6 (SD = 4.3) years. Most participants were White (n = 214, 82%), married or partnered (n = 238; 91.9%), college educated (n = 229; 87.4%), and had an annual income of ≥$75,000 (n = 206, 78.6%). Most women had given birth vaginally (n = 165, 63.5%), and were feeding their infants breastmilk (n = 176, 67.2%). Participants completed study questionnaires between April 2020 and September 2020, with the largest number of participants responding during June 2020 (n = 148, 56.5%; Table 1).
TABLE 1. PARTICIPANT SOCIODEMOGRAPHIC CHARACTERISTICS.
| Characteristic | N (%) | |
|---|---|---|
| Race-ethnicity (n = 261) | ||
| White | 214 (82) | |
| Asian | 22 (8.4) | |
| Hispanic | 16 (6.1) | |
| African American | 2 (0.8) | |
| Other or decline to respond | 7 (2.7) | |
| Relationship status (n = 259) | ||
| Married or partnered | 238 (91.9) | |
| Single or Other | 21 (8.1) | |
| Education level (n = 262) | ||
| College degree | 229 (87.4) | |
| High school diploma or GED | 33 (12.6) | |
| Occupation (n = 250) | ||
| Business | 84 (33.6) | |
| Education | 48 (19.2) | |
| Government | 10 (4) | |
| Health care | 81 (32.4) | |
| Stay-at-home parent or Other | 27 (10.8) | |
| Current employment status (n = 260) | ||
| Employed (full or part time) | 108 (41.6) | |
| Maternity leave | 101 (38.8) | |
| Othera | 51 (15.2) | |
| Annual household income (U.S. dollars; n = 262) | ||
| <$34,999 | 7 (2.7) | |
| $35,000-$74,999 | 43 (16.4) | |
| $75,000-$99,999 | 39 (14.9) | |
| $100,000 or more | 167 (63.7) | |
| Decline to respond | 6 (2.3) | |
| Infant sex (n = 260) | ||
| Female | 133 (51.2) | |
| Male | 126 (48.5) | |
| Twins | 1 (0.4) | |
| Infant feeding (n = 262) | ||
| Breastmilk only | 176 (67.2) | |
| Formula only | 27 (10.3) | |
| Both breastmilk and formula | 59 (22.5) | |
| Type of birth (n = 260) | ||
| Vaginal | 165 (63.5) | |
| Cesarean | 71 (27.3) | |
| Other | 24 (9.2) |
Student, mandatory time off due to COVID-19, other
Postpartum Depression Symptoms
Total PDSS-SF scores ranged between 7 and 32, mean 17.7 (SD = 5.9). Using the suggested cut off score, 66 (25%) scored in the “normal adjustment” range (7-13) and 195 (75%) scored ≥14, indicating significant symptoms of PPD. There were no significant differences in PDSS-SF scores between any obstetric variable groups. Women who were younger tended to have higher PDSS-SF scores (r = -.183, p = .003). There was a significant difference in PDSS-SF scores (F(2, 258) = 4.327, p = .014) between mothers who chose to breastfeed (M = 17.11; SD = 5.88), formula feed (M = 17.63, SD = 6.58), or who used a combination of breastmilk and formula (M = 19.68; SD = 5.87). There was a significant difference in PDSS-SF scores (F(1,259) = 29.92, p = <.001) between women who reported a past history of mental illness (M = 20.46, SD = 6.16), and those without (M = 16.44, SD = 5.26). There was also a significant difference in PDSS-SF scores (F(1,259) = 15.46, p = <.001) between women who were currently receiving treatment for a mental health condition (M = 20.44, SD = 6.29), and those who were not (M = 17.03, SD = 5.55). These findings were confirmed when Depression Category was used as the dependent variable.
Experiences of Postpartum Women During the COVID-19 Pandemic
Of the 262 returned surveys, 166 women (63.6%) provided answers to the open-ended statements, which included short answers and long narratives that resulted in a total of 70 single-spaced pages. Content analysis of the women's postpartum experiences during the COVID-19 pandemic revealed five themes.
Isolation and Seclusion Continue
Women were asked to limit any visitors living outside the home for minimum of 2 weeks with some pediatricians recommending no visitors for 4 weeks postpartum. New mothers stated their husbands or partners were often the only help they had during this quarantine period and described this as such a lonely time. It was really hard having no family or friends to help when I needed it. I felt alone and cried a lot. My husband kept our toddler busy when I was with our newborn. It was the hardest time of my life. We would have had help from family but couldn't because of COVID. They described needing their own mothers with them during the postpartum period. One woman shared that her husband was wonderful helping her but, I needed my mommy! Finally, at five weeks my son had lost weight compared to his two-week checkup. I felt empowered to tell my husband I NEED my mother. She came for two weeks and it stopped the mental and physical health spiral in me and my toddler.
One mother explained, the first six weeks were tough as a new mom. You're already super careful about who comes in contact with your baby so they don't get COVID. Now the only option is complete isolation. They described stocking up on groceries and other supplies before their due date so they would not need to leave the house for 2 weeks and some did not want to risk taking their baby outside in the fresh air for a stroll. It has been so hard and lonely. I want to experience the world with my baby, but I can't.
They reported having to figure out motherhood alone. I was at home with my husband figuring out how to be a first-time mom without the support of my parents or his parents. Mothers described missing out on adult interaction. I'd say the toughest part of this COVID isolation has been not having ‘my village’ minimal family support, not being able to go to support groups for breastfeeding and new moms, not being able to just be around other moms to ask questions and validate normal feelings and experiences.
New mothers reported the isolation they experienced from restricted in-person health care visits during the pandemic. My husband tried his best but nursing [breastfeeding] caused me a lot of distress. It was very hard because the lactation consultants at the hospital were only taking phone calls instead of face-to-face. Another mother recalled, I could not go directly to the lactation nurses because of COVID-19 and all that was available was video chats. It was almost like we were left to decode everything on our own!
One woman who gave birth to twins recounted the lonely month she spent while her twins were in the neonatal intensive care unit (NICU). Once I was discharged from the hospital, my husband was no longer allowed to visit the NICU. We negotiated with the hospital to try and get permission for my husband to visit since we had two babies who were in separate areas of the NICU. After an exhausting and emotional time of trying to negotiate with the hospital, we realized there was no chance for us to get my husband permission to visit. He didn't get to see our babies for over three weeks. It was extremely emotional for both of us.
Fear, Anxiety, and Stress Filled the Days
The COVID-19 pandemic was an emotionally trying time for new mothers with many describing fears and the possibility that their newborn, other children, or themselves could get the virus. Due to this fear, they only left their house with the baby for well-baby checks. Often, only partners would go out to do errands and grocery shop to try and decrease women's anxiety and minimize any exposure to COVID-19. For women with other children at home, the anxiety and stress were often increased. It has been difficult to let my teenager hang with friends that haven't necessarily been social distancing as he [teenager] could potentially bring the coronavirus back to my newborn. Once sheltering in place and social distancing mandates occurred in their communities, other stressors emerged such as school and daycare closures, creating an impossible task of managing home schooling and keeping preschoolers occupied while caring for their newborns. We were expecting my toddler to be in daycare three days a week, but since that wasn't the case, my husband and I have had less time to focus attention on our newborn than we had hoped. Instead, we've been dividing attention trying to attend to our two-year old's emotional needs during all this upheaval and isolation.
They recounted the fear and anxiety during the first 6 weeks at home with their infant. I would often panic when my husband would get home from work. I would literally envision him having the virus on his clothing when he would hold the baby. It was very nerve wracking during those first few weeks. Another mother reported, the constant stress and anxiety about my brand-new baby with exactly zero immune system being born into what feels like a cesspool of a deadly pandemic. It's a wonder I can sleep at all.
Some believed the inability to see a lactation consultant led to other methods to feed their infants. I was unable to successfully breastfeed and couldn't see a lactation consultant because of the virus. Therefore, breastfeeding was unsuccessful, and I have to exclusively pump.
Grieving the Loss of “Normal” It's Just so Sad
The word sad was often used by participants when describing their first 6 weeks at home with their newborn. One new mother describes her sadness from not being able to see family and friends. We were very sad that our friends and family couldn't meet the baby when she was a newborn-that was the hardest part. We video chatted but it's obviously not the same. Family and friends visited through a glass door. Per another, It was emotionally devastating not being able to have any visitors. I feel terrible for our daughter. Every baby deserves to be celebrated when they enter the world. There were no snuggles from family and friends. No joyous meetings. I mourned this loss. They were concerned about lost experiences. We will never get back the opportunity for those early memories with family. COVID really turned a shared family event into a totally isolated blip.
Complicated by Postpartum Depression: A Dark Time
Several women discussed effect of the COVID-19 lockdown on their mental health. It was a dark, terrifying time. Being isolated worsened depressive symptoms. Raising these children mostly by myself as my husband is an essential worker and worked a minimum 40 hours per week, I fell deeper into depression and hormone changes and postpartum depression. I had to increase my medication to feel better and that took a month to start balancing.
They recognized their symptoms and felt they were related to being forced to be alone due to the pandemic. I had severe depression during the first month that was likely exacerbated by being isolated due to COVID-19. I cried multiple times a day. I worried I wasn't good enough for my baby. Per another new mother, the first six weeks at home felt pretty terrible. I was experiencing heavy postpartum depression with intrusive thoughts. I could barely eat, though I was breastfeeding and needed calories.
A history of PPD and being isolated because of COVID-19 contributed to PPD symptoms for one new mother, Untreated PPD. No one to help, no one to bring meals. This was during the initial part of the COVID shutdown and most of my friends were afraid to even drop off food. There were no support groups available virtual or in person and no psychiatrist available within 70 miles. I resumed the SSRIs [antidepressants] I took with my previous pregnancy's postpartum depression. Not having a friend or family support due to quarantine has made the transition very isolating and doesn't help with postpartum depression.
There is a Silver Lining
A few first-time mothers described some of the positive aspects of the COVID-19 pandemic, using phrases, blessing in disguise and silver lining. One woman reported, It was not what I had planned, I had planned on my mother and mother-in-law coming over to help me. Instead, my husband and I had to do everything and figure everything out on our own. The silver lining was that my husband was working from home, so he got to spend extra time with the baby. Enhanced family bonding and family closeness was thought to be related to avoiding visitors to decrease risk of COVID-19 exposure, My husband and I said ‘no’ to having any visitors for two weeks after our baby was born due to COVID. It was hard to not have extra support, but this time together really helped us bond as new family of three. A big part of me is grateful for the closeness COVID meant for our family. One new mother thought she and her husband may have benefited from having to learn parenting on their own and together. It's been challenging not having any support from family since the first two weeks and only having my husband and I to learn how to care for a newborn. On the positive side we have become very good at managing on our own and have benefited from ONLY having each other to figure everything out. Some mothers tried to look at the positive aspects of being alone as new parents. While the prolonged isolation postpartum was emotionally difficult, I also realize that my husband and I had the chance to bond with our baby in a way that we likely never would have been able to under normal circumstances. In that way, this was all a blessing in disguise.
Discussion
We used a mixed-methods approach to identify PPD risk and experiences of women during the first 6 weeks postpartum in the midst of the COVID-19 pandemic. The PPD risk analysis and qualitative themes that were identified help shape a holistic account of women's experiences at home with their new babies during early postpartum.
Three quarters of our participants (75%) scored ≥14 on the PDSS-SF, indicating significant PPD symptoms. The higher rate of PPD symptoms in our sample may be due to the more sensitive and specific PDSS-SF we used to assess depressive symptoms (Cai et al., 2019; Pereira et al., 2013) or to the added stressors of the pandemic (Liu et al., 2021). One third of our participants (34%) reported a previous history of depression and 27.3% reported a cesarean birth which are well-documented risk factors for PPD in nonpandemic times (Moameri et al., 2019; Silverman et al., 2017).
Closer examination of depression scores revealed significantly higher scores in participants who were younger, who were using formula and breastmilk to feed their infants versus breastmilk alone, and participants who had a previous history of mental illness. Younger women are already at an increased risk of PPD (Bauman et al., 2020) as are women with a prior mental health history (Silverman et al., 2017). Participants who wanted to breastfeed their infant described having to supplement formula due to lack of lactation support. Using recommendations from Spatz (2021), nurses should consider other ways to expand in-person breastfeeding assistance opportunities, for example, in the community and in pediatric offices. Qualitative data analysis provided important context to the quantitative strand. Specially, descriptions of isolation, loneliness, limited social support, and concerns of COVID-19 infection that emerged helped to provide context for the high proportion of depressive symptoms in our participants and align with other studies (Chivers et al., 2020; Farewell et al., 2020; Ostacoli et al., 2020).
Limitations
Our findings are limited due to the racial and socioeconomic homogeneity of the sample and reflect continued underrepresentation of Black, Indigenous, and people of color in PPD research. Researchers must strive to diversity study samples to better understand experiences of underserved and women from a larger array of diversity. The anonymous study design prevented us from being able to follow-up with women with elevated PDSS-SF scores. We provided a list of nationwide mental health resources at the end of the survey to address this shortcoming. Written answers to open-ended questions versus face-to-face in-depth interviews also contribute to study limitations. Face-to-face interviews provide an opportunity to observe verbal and nonverbal cues such as facial expression which adds context for answers. Future researchers should include ways to identify long-term PPD symptom trajectories.
Clinical Implications
The first few weeks at home caring for a newborn after being discharged from the hospital are challenging times for any new mother. The added stressors of sheltering in place, social distancing, limited medical appointments, and fear of COVID-19 exposure or infection for family members can be overwhelming. Our findings revealed short- and long-term clinical implications.
Given 75% of our participants had significant PPD symptoms, short-term clinical implications include importance for nurses to advocate for PPD symptom screening and to offer alternative resources such as telehealth, online depression screening, and counseling to women (Peahl et al., 2020). Several new mothers described having limited support from family and friends due to sheltering in place and social distancing. Nurses can help patients identify people in their social networks or social work referral, especially with increased depressive symptoms noted in younger participants.
Others described limited in-person medical appointments. Lactation consultants were scheduling virtual or phone appointments and not making in-person rounds to assist with breastfeeding to maintain social distancing. Nurses can help advocate for safe, social distanced, in-person lactation visits for women, especially first-time mothers or for those desiring in-person assistance. Hospitals should consider setting times for informal chats, following the exemplar “Ask the Educator” established in hospitals at the epicenter of the pandemic that includes live discussion webinars where mothers can receive immediate feedback to their questions (Pasadino et al., 2020).
The continuing COVID-19 pandemic suggests some longer-term implications for clinical practice. As most trusted professionals, nurses can provide patients with evidence-based information. Our data were collected between April 2020 and September 2020, during the first peak of the pandemic, before vaccines were available, a time of inconsistent messaging, and lack of uniformity in guidelines addressing perinatal care during the pandemic (Benski et al., 2020). Recommending resources such as the Centers for Disease Control and Prevention (2021a, 2021b, 2021c) and the American Academy of Pediatrics (2021a, 2021b) to answer questions about COVID-19 exposure-infection risk, breastfeeding, and masking for school-age children at home, COVID-19 vaccines, will help provide consistent messaging and decrease misinformation (Table 2).
TABLE 2. RESOURCES FOR NURSES CARING FOR POSTPARTUM FAMILIES.
| Subject | Agency | URL |
|---|---|---|
| Breastfeeding and caring for newborns if you have COVID-19 | CDC | https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/pregnancy-breastfeeding.html |
| How to protect yourself and others | CDC | https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html |
| Pregnant and recently pregnant people | CDC | https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnant-people.html |
| COVID-19 vaccines in children and adolescents | AAP | COVID-19 Vaccines in Children and Adolescents | American Academy of Pediatrics (aappublications.org) |
| Masks for school age children | AAP | AAP urges in-person learning, masking in updated guidance on safe schools | American Academy of Pediatrics (aappublications.org) |
Note. AAP = Academy of Pediatrics; CDC = Centers for Disease Control and Prevention.
CLINICAL IMPLICATIONS
Nurses should be aware of the increased risk of PPD during times of public health crises such as COVID-19.
Nurses at the bedside are well positioned to identify vulnerabilities, screen for depressive symptoms, and refer women at risk for further evaluation and treatment as needed.
Nurses can help provide support to promote likelihood of breastfeeding.
Nurses must advocate and provide evidence-based education about postpartum depression given the disparities in mental health care screening and access.
New COVID variants and vaccine hesitancy suggest continued disruption for postpartum mothers.
References
- American Academy of Pediatrics. (2021a). AAP urges in-person learning, masking in updated guidance on safe schools. https://www.aappublications.org/news/2021/07/18/schools-071821
- American Academy of Pediatrics. (2021b). COVID-19 vaccines in children and adolescents. https://pediatrics.aappublications.org/content/148/2/e2021052336 [DOI] [PubMed]
- American College of Obstetricians and Gynecologists. (2020). Novel coronavirus 2019 (COVID-19): General information regarding pregnant individuals and COVID-19. https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/03/novel-coronavirus-2019
- Basu A., Kim H. H., Basaldua R., Choi K. W., Charron L., Kelsall N., Hernandez-Diaz S., Wyszynski D. F., Koenen K. C. (2021). A cross-national study of factors associated with women's perinatal mental health and wellbeing during the COVID-19 pandemic. PLoS One, 16(4), e0249780. 10.1371/journal.pone.0249780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauman B. L., Ko J. Y., Cox S., D'Angelo Mph D. V., Warner L., Folger S., Tevendale H. D., Coy K. C., Harrison L., Barfield W. D. (2020). Vital signs: Postpartum depressive symptoms and provider discussions about perinatal depression - United States, 2018. MMWR. Morbidity and Mortality Weekly Report, 69(19), 575–581. 10.15585/mmwr.mm6919a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck C. T., Gable R. K. (2002). Postpartum depression screening scale (PDSS). Western Psychological Services. https://www.wpspublish.com/pdss-postpartum-depression-screening-scale [Google Scholar]
- Benski C., Di Filippo D., Taraschi G., Reich M. R. (2020). Guidelines for pregnancy management during the COVID-19 pandemic: A public health conundrum. International Journal of Environmental Research and Public Health, 17(21), 8277. 10.3390/ijerph17218277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai M., Wang Y., Luo Q., Wei G. (2019). Factor analysis of the prediction of the postpartum depression screening scale. International Journal of Environmental Research and Public Health, 16(24), 5025. 10.3390/ijerph16245025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2021a). Breastfeeding and caring for newborns if You Have COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/pregnancy-breastfeeding.html
- Centers for Disease Control and Prevention. (2021b). How to protect yourself & others. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
- Centers for Disease Control and Prevention. (2021c). Pregnant and recently pregnant people. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnant-people.html
- Chivers B. R., Garad R. M., Boyle J. A., Skouteris H., Teede H. J., Harrison C. L. (2020). Perinatal distress during COVID-19: Thematic analysis of an online parenting forum. Journal of Medical Internet Research, 22(9), e22002–e22002. 10.2196/22002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell J. W., Plano Clark V. L. (2018). Designing and conducting mixed methods research (3rd ed.). Sage. [Google Scholar]
- Dagher R. K., Bruckheim H. E., Colpe L. J., Edwards E., White D. B. (2021). Perinatal depression: Challenges and opportunities. Journal of Women's Health, 30(2), 154–159. 10.1089/jwh.2020.8862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodgson J. E., Tarrant M., Chee Y. O., Watkins A. (2010). New mothers' experiences of social disruption and isolation during the severe acute respiratory syndrome outbreak in Hong Kong. Nursing & Health Sciences, 12(2), 198–204. 10.1111/j.1442-2018.2010.00520.x [DOI] [PubMed] [Google Scholar]
- Farewell C. V., Jewell J., Walls J., Leiferman J. A. (2020). A mixed-methods pilot study of perinatal risk and resilience during COVID-19. Journal of Primary Care & Community Health, 11, 2150132720944074. 10.1177/2150132720944074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giarratano G. P., Barcelona V., Savage J., Harville E. (2019). Mental health and worries of pregnant women living through disaster recovery. Health Care for Women International, 40(3), 259–277. 10.1080/07399332.201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal D., Selix N. W. (2021). Impact of COVID-19 on maternal mental health. MCN. The American Journal of Maternal Child Nursing, 46(2), 103–109. 10.1097/NMC.0000000000000692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guintivano J., Manuck T., Meltzer-Brody S. (2018). Predictors of postpartum depression: A comprehensive review of the last decade of evidence. Clinical Obstetrics and Gynecology, 61(3), 591–603. 10.1097/GRF.0000000000000368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krippendorff K. (2019). Content analysis: An introduction to its methodology (4th ed.). Sage. [Google Scholar]
- Liu C. H., Erdei C., Mittal L. (2021). Risk factors for depression, anxiety, and PTSD symptoms in perinatal women during the COVID-19 Pandemic. Psychiatry Research, 295, 113552. 10.1016/j.psychres.2020.113552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moameri H., Ostadghaderi M., Khatooni E., Doosti-Irani A. (2019). Association of postpartum depression and cesarean section: A systematic review and meta-analysis. Clinical Epidemiology and Global Health, 7(3), 471–480. 10.1016/j.cegh.2019.02.009 [DOI] [Google Scholar]
- Ostacoli L., Cosma S., Bevilacqua F., Berchialla P., Bovetti M., Carosso A. R., Malandrone F., Carletto S., Benedetto C. (2020). Psychosocial factors associated with postpartum psychological distress during the COVID-19 pandemic: A cross-sectional study. BMC Pregnancy and Childbirth, 20(1), 703. 10.1186/s12884-020-03399-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pao C., Guintivano J., Santos H., Meltzer-Brody S. (2019). Postpartum depression and social support in a racially and ethnically diverse population of women. Archives of Women's Mental Health, 22(1), 105–114. 10.1007/s00737-018-0882-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasadino F., DeMarco K., Lampert E. (2020). Connecting with families through virtual perinatal education during the COVID-19 pandemic. MCN. The American Journal of Maternal Child Nursing, 45(6), 364–370. 10.1097/NMC.0000000000000665 [DOI] [PubMed] [Google Scholar]
- Peahl A. F., Smith R. D., Moniz M. H. (2020). Prenatal care redesign: Creating flexible maternity care models through virtual care. American Journal of Obstetrics and Gynecology, 223(3), 389.e1–389.e10. 10.1016/j.ajog.2020.05.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira A. T., Bos S., Marques M., Maia B., Soares M. J., Valente J., Nogueira V., de Azevedo M. H. P., Macedo A. (2013). Short forms of the postpartum depression screening scale: As accurate as the original form. Archives of Women's Mental Health, 16(1), 67–77. 10.1007/s00737-012-0319-6 [DOI] [PubMed] [Google Scholar]
- Silverman M. E., Reichenberg A., Savitz D. A., Cnattingius S., Lichtenstein P., Hultman C. M., Larsson H., Sandin S. (2017). The risk factors for postpartum depression: A population-based study. Depression and Anxiety, 34(2), 178–187. 10.1002/da.22597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spatz D. L. (2021). The COVID-19 pandemic and breastfeeding: Concerns & positive opportunities. MCN. The American Journal of Maternal Child Nursing, 46(4), 238. 10.1097/NMC.0000000000000732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2020). Coronavirus disease (COVID-19) advice for the public. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public


