ABSTRACT
Study Design
Systematic review.
Background
Physical therapists often use cervicothoracic and thoracic manual techniques to treat musculoskeletal disorders of the upper quarter ,however, the overall effectiveness of this approach remains to be elucidated.
Objective
This systematic review explored studies that examined the short- and long-term effectiveness of manual physical therapy directed at the cervicothoracic and thoracic region in the management of upper quarter musculoskeletal conditions.
Methods
The electronic databases MEDLINE, AMED, CINAHL, and Embase were searched from their inception through 30 October 2020. Eligible clinical trials included those where human subjects treated with cervicothoracic and/or thoracic manual procedures were compared with a control group or other interventions. The methodological quality of individual studies was assessed using the PEDro scale.
Results
The initial search returned 950 individual articles. After the screening of titles and abstracts, full texts were reviewed by two authors, with 14 articles determined to be eligible for inclusion. PEDro scores ranged from 66 to 10 (out of a maximum score of 10). In the immediate to 52-week follow-up period, studies provided limited evidence that cervicothoracic and thoracic manual physical therapy may reduce pain and improve function when compared to control/sham or other treatments.
Conclusions
Evidence provides some support for the short-termeffectiveness of cervicothoracic and thoracic manual physical therapy in reducing pain and improving function in people experiencing upper quarter musculoskeletal disorders. Evidence is lacking for long-term effectiveness as only two studies explored outcomes beyond 26 weeks and this was for patient-perceived improvement.
Prospero ID
CRD42020219456
KEYWORDS: Thoracic spine, Manipulation, Upper quarter
Introduction
Upper extremity musculoskeletal disorders (MSDs) are commonly reported in the general and working populations and usually present as pain and/or tingling in the neck, shoulder, or upper extremity. Upper extremity MSDs typically consists of conditions involving nerves, muscles, and/or joints. These conditions can often be multifactorial and work-related with a reported annual incidence range from 0.08 to 6.3 and prevalence from 0.14 to 14.9 [1,2]. Additionally, a 2006 systematic review suggested that women were significantly more likely to experience an upper extremity MSD than men, and this difference was not attributable to work-related variables. Musculoskeletal disorders have a substantial economic burden on society due to lost work productivity and health care costs [3]. Inpatient and outpatient surgery is the largest contributor to the total amount paid to treat many of these diagnoses and physical therapy services also contribute a portion to the overall care costs, which are estimated to be in the billions of dollars [4].
Physical therapy management of upper extremity (upper quarter) MSDs includes physical agents, therapeutic exercise, thrust or non-thrust manual physical therapy procedures, or a combination of these interventions [5]. Favorable outcomes related to intervention assume diagnosis and classification will determine if symptoms are emanating from the extremity itself or more proximal (such as the spine), thereby directing treatment to that region [6]. The most common upper extremity MSDs in the Truven Health MarketScan database are shoulder pain and rotator cuff tendinopathy, shoulder stiffness, shoulder arthritis, lateral epicondylitis, hand arthritis, trigger finger, wrist pain, and hand pain [6].
A systematic review conducted in 2006 was not able to identify any studies reporting incidence rates for upper quarter MSDs. The authors identified an absence of a universally accepted way of labeling or defining these conditions [3], a challenge which remains to this day. As extremity pain may emanate from the spine, this issue is further confounded. Rosedale and colleagues [7] found over 40% of 369 physical therapy patients with isolated extremity pain, who believed their pain was not originating from the spine, responded positively to spinal intervention, and were thus classified as having a spinal source of symptoms rather than an upper extremity MSD. Similarly, interventions directed only to a particular region, such as the shoulder, do not consider the role of neighboring structures such as the cervicothoracic spine and ribs [8]. Although evidence supports manual physical therapy intervention of the spine in the management of patients with shoulder pain [9–15], the effects of cervicothoracic and thoracic thrust and non-thrust manipulation on individuals with a primary complaint of upper quarter pain remain to be reported in a systematic review. Therefore, the purpose of this systematic review was to determine the effectiveness of manual physical therapy in the treatment of pain and disability in individuals with upper extremity MSDs as outlined above.
Methods
This systematic review was performed following the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines [16]. This study was registered a priori with PROSPERO (ID: CRD42020219456). The included studies were comprised of individuals with a musculoskeletal condition-related pain and/or disability related to the upper quarter. Individuals between the ages of 18 and 80 years of age were included in this systematic review. Studies were excluded if they pertained to post-surgical care.
Search strategy
Eligible studies in this systematic review included randomized clinical or controlled trials of patients with MSDs of the upper quarter treated by a physical therapist with cervicothoracic and/or thoracic thrust/non-thrust manipulation and compared with a control, sham, or other intervention. Randomized trials were included to avoid bias and provide rigor in examining cause-effect relationships between intervention and outcome. Studies were excluded if patients were less than 18 years of age or if the full text was not published in English. The electronic databases PubMed, AMED, SPORTDiscus, CINAHL, and the Cochrane Central register of controlled trials were searched independently by a biomedical librarian. The terms thoracic spine, manipulation, paired with ‘random’, ‘group’, trial” randomized controlled trial,” or ‘controlled clinical trial’ were used to search the electronic databases. Results were limited to human studies. Bibliographic reference lists from identified articles were hand searched for any other potential study not identified during the database searches. Search results are displayed in Appendix A.
After duplicate articles were removed, two independent reviewers (R.S. and J.C.) screened titles and abstracts to determine which studies met the inclusion and exclusion criteria. Studies that appeared to meet the inclusion criteria or whose eligibility could not be determined from the title/abstract screening were retrieved for full-text review by the two independent reviewers (R.S. and J.C.). Disagreements between reviewers were resolved by consulting a third reviewer (M.D.) who was blind to the other reviewers’ decisions on whether the study should be included. Reliability between independent reviewers was calculated for both title/abstract and full-text review using an unweighted kappa.
Data extraction and quality assessment
Data extraction was performed by the primary investigator (R.S.) and was reviewed for accuracy by the senior author (J.C.). Data were then compiled into a standardized data-extraction form and were determined following validation by the two reviewers. Data included sample size, diagnosis, inclusion/exclusion criteria, duration of symptoms, type of manual physical therapy intervention (thrust, non-thrust, massage), main outcomes, and time to an outcome. Data included from extracted studies are found in Table 1 and were determined following validation by the two reviewers.
Table 1.
Data extracted from the included studies
| Study | Study Characteristics |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sample Size | Participants | Diagnosis (Duration) | Intervention group (n) (SD) | Outcome Measure | Comparison group (n) | Follow up | Results | PEDro score | ||
| Kaya et al (2014) | n = 54 | 21 males; 33 females age (30–60) | Subacromial impingement syndrome 6 wk. treatment |
Thoracic manual therapy with exercise (n = 26) Mean age 47.15 (±9.44) |
VAS DASH US of tendon thickness |
Kinesiotape with exercise (n = 28) Mean age 50.85 |
No | Significant differences in pain and DASH within groups; no difference in US thickness | 6 | |
| Land et al (2017) | n = 60 | 30 males; 30 females; age 40–60 | Subacromial shoulder impingement 12 wk. treatment | Upper thoracic mobilization (n = 20) Mean age 51 (±4.4) Shoulder massage, mobilization, stretching (n = 20) Mean age 51 (±4.4) |
AROM shoulder Passive glenohumeral IR Pain Shoulder pain and function disability index Pain (SPADI) |
Ultrasound (control) (n = 20) Mean age 51 (±4.4) |
E-Mail follow up of pain and function (SPADI) Time frame |
Outcomes significantly improved in the groups receiving upper thoracic treatment compared with the active control group and in the posterior shoulder treatment compared with the active control group with no differences detected between the shoulder treatment compared with the thoracic treatment | 10 | |
| Kardouni et al (2015) | n = 45 | 23 females; 22 males; age 18–59 | Subacromial impingement syndrome; 6 techniques during one session | Thoracic SMT (n = 24) Mean age 31.1 (±2.3) | NPRS; Penn shoulder score; GROC | Sham thoracic SMT (n = 21); Mean age 31.2 (±12.1) | No | There were no differences in pain sensitivity between groups. Both groups improved patient rated pain and function within 24–48 hrs. | 9 | |
| Silva et al (2019) | n = 60 | 19 males; 41 females; age 20–70 | Rotator cuff tendinopathy Two treatments |
Thoracic manipulation group (n = 30) Mean age 46.06 (16.11); placebo group (n = 30) Mean age 44.46 (±12.14) | VAS; shoulder flexion, abduction range of motion | Placebo – therapist maintained minimal pressure on thoracic segments with patient in prone | No | Both groups demonstrated a reduction in pain, but there was no clinically significant improvement between groups. Both showed increased shoulder ROM, but only abduction of the painful shoulder in the MG reached the MDC. | 8 | |
| Fernandez-Camero (2011) | n = 18 | 9 females; 8 males; age 18–60 | Lateral epicondylalgia; 1 session | Thoracic manipulation (T5-8) | Pain pressure threshold; pain-free grip strength | Cervical manipulation (C5-6) |
No | Cervical spine manipulation produced a greater increase of PPT in both sides compared with thoracic. For pain-free grip strength, no interaction between group and time existed | 7 | |
| Riley et al (2015) | n = 88 | 54 females; 34 males Age 18–69 |
Patients with shoulder pain; 1 session | Thoracic HVLATM (n = 22); age 52.3 (±8.5): 13 females; nine males Scapular HVLATM (n = 22); age 45.9 (±13.2); 15 females; 7 males |
NPRS; NPRS with impingement testing; SPADI | Thoracic neutral massage (n = 22); age 48.5 (±12.0); 14 females; 8 males Scapular neutral massage (n = 22); age 48.1 (±10.4); 12 females; 10 males |
Outcome measures at 6–9 days post | Patients improved following the interventions. Neither the type of HVLATM nor the message conveyed had a significant effect on patient improvements | 8 | |
| Park et al (2020) | n = 30 | 9 males; 21 females; age | Subacromial impingement syndrome 4 wk treatment, 12 sessions | Thoracic joint mobilization (n = 10); age 49.20 (±9.48) Ex group (n = 10); age 50.90 (±9.10) |
Thoracic kyphosis; pec major and upper trap pain muscle tone and stiffness; affected side PROM; SPADI | Combination group (n = 10); age 50.20(±8.99) | No | All three groups had significant improvements in all variables. The combination group displayed a significant improvement in thoracic kyphosis and upper trapezius muscle tone as well as flexion, medial and lateral rotation ROM and SPADI compared to the mobilization and exercise groups. | 8 | |
| Wright et al (2017) | n = 18 | 8 females; 10 males; >18 yo (mean 43.1) | Subacromial impingement syndrome; treatment 2x/week for 4 weeks | Cervicothoracic thrust/non-thrust plus shoulder manual therapy and exercise (n = 10); 5 males, 5 females; age 46.3 (±15.9) | NPRS; SPADI | Shoulder only manual therapy and exercise (n = 8); 4 males, 4 females; age 39.1 (±15.8) | DC assessment | Both groups showed statistically significant improvements in both pain and function at 2, 4 wks. and DC. Between group differences for changes in pain and physical function were not significant | 7 | |
| Haider et al (2018) | n = 40; | 22 females; 18 males; mean age 49.55 (±9.706) | Subacromial pain; 4 thoracic manipulations over 6 treatment session | Thoracic manual procedures, hot or cold pack, shoulder ROM and strengthening exercises (n = 20) | NPRS; SPADI | Hot or cold pack, shoulder ROM and strengthening exercises (n = 20) |
1 week follow up | Pain intensity and function score improved to a greater extent in the experimental group | 6 | |
| Haik et al (2017) | n = 61 | 38 males; 23 females | Shoulder impingement syndrome; 2 interventions over 1 week | Mid-thoracic manipulation (n = 20); Mean age 32.5(±12.0) |
NPRS; DASH; Western Ontario Rotator Cuff Index | Sham thoracic manipulation group (n = 31); Mean age 31.3(±11.0) | Day 3 follow up | TSM increased scapular upward rotation during arm lowering. Did not influence activity of the scapular muscles and pain, function, scapular tilt and internal rotation were not conclusive | 8 | |
| Bergman et al (2004) | n = 150 | 79 females; 71 males | Shoulder pain; 6 treatments over 12 weeks | Usual medical care plus cervical and thoracic manipulation (n = 79); 42 females, 37 males; mean age 48.4 (±12.4) | Patient-perceived recovery; severity of main complaint; shoulder disability; general health | Usual medical care (n = 71); 37 females, 43 males; mean age 47.8 (±11.8) | 52 weeks follow up 87–94% | More patients from intervention group reported full recovery or very large improvement. The intervention and control groups differed significantly in perceived recovery and patients who reported feeling ‘cured’ at 52 weeks. The outcomes of shoulder pain and disability favored additional manipulative therapy; however, only shoulder disability received a sig difference at 26 wks. | 8 | |
| Vinuesa- Montoya et al (2017) |
n = 41 | 28 males; 13 females | Shoulder impingement syndrome; 10 sessions over 5 weeks (2 session/wk) | Cervicothoracic manipulation plus exercise; (n = 21); 15 males, 6 females; age 46.85(±8.02); 25–57 | VAS; DASH; Shoulder disability questionnaire; Hawkins-Kennedy and Neer test; Shoulder AROM | Home exercise program; (n = 20); 13 males, 7 females; age 51.21(±5.29); 38–58 | no | Between group differences in the DASH. No statistically significant differences for shoulder disability questionnaire and pain intensity. Both groups improved regarding disability and clinical tests for subacromial impingement syndrome | 9 | |
| Grimes et al (2019) | n = 60 | 37 males, 23 females | Shoulder pain syndrome; 2 thoracic manipulative techniques | Seated thoracic manipulation (n = 20); 12 males, 8 females, age 35.6(±14.7) Supine thoracic manipulation (n = 20); 10 males, 10 females; age 37.6(±15.3) |
Self-reported pain; Pain shoulder score; impairment measures | Sham manipulation (n = 20); 15 males, 5 females; age 36.5(±15.5) | no | No differences in pain, satisfaction and function compared to a sham manipulation. Thoracic spine manipulation did not have an immediate effect on the scapular impairments measured. | 8 | |
| Mintken (2016) | n = 140; age 18–65 | 76 females; 64 males | Shoulder pain; 8 sessions of manual therapy with exercise or exercise alone | Thoracic manual therapy plus exercise (n = 70); 40 females, 30 males; age 40.5(±11.7) | SPADI; NPRS; QuickDASH; GROC; PASS | Exercise alone; (n = 70); 36 females, 34 males; age 44.8(±12.9) | 6 mos. follow up | Adding two sessions of high dose cervicothoracic manual therapy to an exercise program did not improve pain or disability in patients with shoulder pain, but did improve patient-perceived success at 4 wks. and 6 mos. and acceptability of symptoms at 4 wks. | 9 | |
The quality of randomized trials were identified through the PEDRO database and were confirmed by two independent reviewers (R.S. and J.C.) using the PEDro (Physiotherapy Evidence Database) quality scale. The PEDro scale is based on 11 criteria, of which 10 contribute to the score, representing internal validity, methodological quality, and risk of bias. The first criterion is not included in the score, as it relates to external validity of the study. Higher scores indicate higher methodological quality. The PEDro scale has been shown to have fair to good interrater reliability, with an intraclass correlation coefficient of 0.55 (95% confidence interval (CI): 0.41, 0.72) [17]. The reviewers’ disagreement was resolved by consulting a third author (M.D.) who was blind to previous assessment scores.
Results
Study selection
Database searches returned a total of 1046 studies. After removing 96 duplicates, 950 titles and abstracts were screened for eligibility. Of these, 26 full-text articles were reviewed. Following full-text review, 14 eligible articles remained and were included in this review. Figure 1 represents the flow diagram of article selection. No articles were identified by hand-searching reference lists of included studies. Inter-rater reliability was good for inclusion/exclusion of articles by the title/abstract and full-text with substantial (k = .63) and almost perfect (k = .93) agreement respectively.
Figure 1.
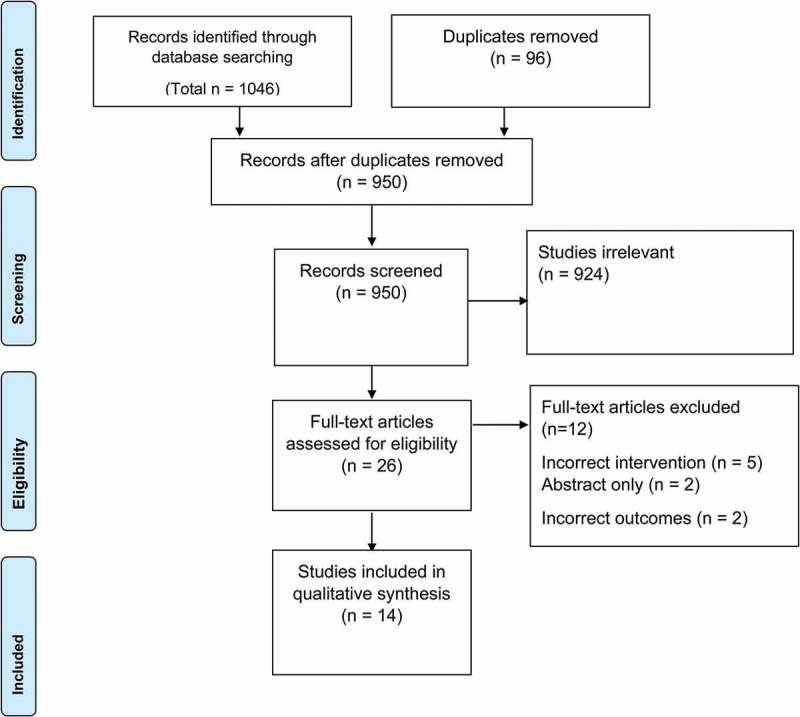
PRISMA flow diagram.
Study Quality
Of the 14 studies selected for this review, the range of PEDro scores was 6–10 and the mean score was 7.92.
Study Characteristics
Fourteen studies met the criteria for inclusion in this systematic review. Twelve of the 14 included studies had a primary intervention of thoracic thrust manipulation [18,19,20,21,22,23,24,25,26,27,28,29], and 2 had a primary intervention of cervicothoracic manipulation [30,31]. Thirteen of the studies included subjects with shoulder diagnoses, and one included a diagnosis related to the elbow [22]. Characteristics of the 14 included studies are included in Table 1.
The 14 included trials in this systematic review included a total of 865 participants. Scores for the quality and risk of bias of the included studies are found in Table 2. PEDro scores for study quality ranged from 6 to 10 (out of a maximum score of 10), with a median score of 7.5 and an interquartile range of 2. Two of the trials (14%) blinded the treating physical therapist [17,19,28,30], and 50% of the trials were blinded subjects using sham or alternative treatment [19–21,26,28–30]. Nine (62%) of the studies included concealed allocation [19–21,23,24,27–29,31]. All 14 of the studies specified eligibility criteria, randomized patients, reported results of between-group statistical comparisons for at least 1 key outcome, and provided point measures and measures of variability for at least 1 key outcome. All 14 of the studies had similar groups at baseline and collected measures of at least 1 key outcome from more than 85% of the subjects initially allocated to groups.
Table 2.
PEDro quality assessment
| Kaya et al.[16] | Land et al[17]. | Silva et al[19]. | Kourdouni et al[18]. | Fernandez-Comero et al[20] | Riley et al[21]. | Park et al[22]. | Wright et al[29]. | Haider et al[23]. | Haik et al[24]. | Bergman et al[25] | Vinuesa-Montoya et al[28] | Grimes et al[26]. | Mintken et al[27]. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PEDro Item | ||||||||||||||
| Eligibility criteria were specified | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Random allocation of subjects | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Allocation concealment | - | + | + | + | - | + | + | + | - | - | + | - | + | + |
| Similar groups at baseline | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Subjects blinded | - | + | + | + | - | - | - | - | - | + | - | + | + | + |
| Therapists administering treatment blinded | - | + | - | - | - | - | - | - | - | - | - | + | - | - |
| Assessors blinded | - | + | - | - | + | + | + | - | - | + | + | + | - | + |
| One key outcome obtained from 85% of subjects initially allocated to groups | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| ‘Intention to treat’ used for analysis of one key outcome | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Between-group statistics for one key outcome reported | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Point measures and measures of variability for one key outcome | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| SCORE | 6 | 10 | 8 | 9 | 7 | 8 | 8 | 7 | 6 | 8 | 8 | 9 | 8 | 9 |
| Internal Validity | F | E | G | E | G | E | E | G | G | E | G | E | E | E |
Six of the studies (43%) included exercise with the manual physical therapy intervention [18,19,25,29–31] and 7 (50%) included manual therapy procedures alone [20–24,26,28]. One study included thoracic manual therapy combined with usual medical care [27]. The comparison groups were varied. Three studies included sham manual interventions [20,26,28] and 1 included a placebo group [21] (Table 1). Physical therapists performed all manual physical therapy procedures and comparison treatments. Six studies included follow-up assessments. Time to follow up varied from 3–9 days in 4 studies [19,23,25,26], 6 months [29] in one study, and one year in one study [27]. Thirteen of the 14 studies assessed both pain and function. Function was assessed with the SPADI in 6 studies [19,23–25,29,31], the DASH in 4 studies [18,26,29,30], and other shoulder disability questionnaires in 4 studies [20,26,27,30]. Pain was assessed using the Numerical Pain Rating Scale (NPRS) in 5 studies [20,23,25,29,31], and the Verbal Analog Pain Scale (VAS) in 3 studies [18,21,30].
Thoracic manual procedures versus control/sham
Five studies [19–21,26,28] examined the short to immediate-term effect of thoracic manual procedures compared to a control or sham. Of the 5 studies, only one showed a significant improvement in pain and function in the treatment group when compared to an active control [19]. There were no significant differences between groups in pain measures or function in two of the studies [20,28]. A statistically significant but not clinically meaningful difference for shoulder pain was found in one study. In this study, only abduction of the painful shoulder reached minimal detectable change [21]. In a trial comparing mid-thoracic manipulation to a sham treatment, manipulation was found to increase scapular upward rotation during arm lowering. However, effects of manipulation on shoulder pain, function, scapular tilt, and internal rotation were inconclusive [26]. The methodological quality of these studies ranged from 7–9 on the PEDro scale.
Cervicothoracic and thoracic manual procedures versus other interventions
Eight studies compared the effects of cervicothoracic or thoracic manual procedures to other interventions [18,22,24,25,27,29–31]. Three of the 8 studies [18,24,30] found significant improvements in pain or function.
The methodological quality of these studies ranged from 7–9 on the PEDro scale.
Long-term effects of thoracic manipulation
Only two studies [27,29] examined the long-term effects of thoracic manipulation. With the addition of thoracic manipulation as a targeted intervention, significant improvement in perceived recovery was found at 52 weeks in one trial [27], and 6-months in the other [29]. The methodological quality of [27] was 8 and [29] was 9 on the PEDro scale, respectively.
Discussion
Results of this systematic review suggest that treatments including cervicothoracic or thoracic manual physical therapy procedures (non-thrust and thrust manipulation) have limited effectiveness in reducing pain and disability for people with upper-quarter MSDs. A PEDro quality assessment found the included studies’ internal validity range from fair to excellent [19–31].
While previous studies [9–15] suggested the effectiveness of thoracic manipulation in the treatment of uppers quarter MSDs, the evidence from this review is less conclusive. Favorable outcomes related to cervicothoracic or thoracic manipulation were found when comparing the intervention to an active control [19], when comparing thoracic manipulation intervention to other interventions [18,24,30], and when assessing patient perception of long-term recovery [27,29]. These results are in line with previous studies that highlight the potential for extremity pain to originate from a spinal source. In a study of extremity pain of spinal source (EXPOSS), 71 people (19%) who had upper extremity complaints were found to have a spinal source of their symptoms [7]. Irrespective of the challenge of diagnosis, the EXPOSS study reported a high proportion of extremity presentations, such as described in this systematic review, that responded to spinal intervention [7]. However, it should be noted that in this review, only one study met the inclusion criteria of an upper quarter disorder other than the shoulder, so it is difficult to generalize the results to disorders of the elbow or wrist/hand [22].
The short-term effectiveness of thoracic manual procedures on painful conditions of the upper quarter is supported by several studies in this review [18–25,27,31]. Short-term effectiveness also appears consistent with a earlier systematic review and meta-analysis that found a significant effect of spinal manipulation on the pain pressure threshold at the remote sites of stimulus application [32]. These results further point to a potential neurophysiological effect rather than a mechanical effect of spinal manipulation [33–36]. Additionally, MSDs, such as those of the upper quarter, may not be limited to the painful area and, additionally, may be mediated by central mechanisms [8,32,37]. This concept has been supported in studies on shoulder [12–15,23–31] and elbow dysfunction [22].
This systematic review includes two studies of the long-term effectiveness of manual procedures directed at the cervicothoracic and thoracic spine by a single health profession (physical therapy) for people with upper-quarter MSDs. These two included studies [27,29] examined the effectiveness of the addition of thoracic manipulation on shoulder dysfunction at 6-months and 52-weeks following the intervention. Both studies did not find a significant improvement in pain or function, but did report an improvement in patient perceived recovery at follow-up.
Limitations
This systematic review has some limitations. The included studies were limited to those investigating manual procedures performed by physical therapists, which may have excluded articles reporting the effects of thrust and non-thrust manipulation on upper quarter MSDs performed by other practitioners. This limitation was intentional, as this review examined evidence specific to physical therapists performing manual procedures. The authors have addressed this concern by limiting the conclusions of the review to only those studies reporting on interventions provided by physical therapists. For this reason, the present findings cannot be generalized to different patient populations treated by different practitioners with varying levels of manipulation training.
Conclusion
Evidence from studies of upper quarter MSDs suggests that manipulation of the cervicothoracic and thoracic spine performed by physical therapists has questionable effectiveness when compared to no treatment, sham, or other interventions for improving pain and function. Further, the limited evidence found in this review for the effectiveness of manipulation directed to the cervicothoracic or thoracic spine for upper quarter MSDs is in relation to short-term outcomes. Further high-quality studies involving other upper quarter MSDs are needed to determine the short-and long-term effectiveness of cervicothoracic and thoracic manipulation in managing these conditions.
Biographies
Ron Schenk PT, PhD, OCS, Dip MDT, FAAOMPT, is a clinical professor and serves as core faculty in the Doctor of Physical Therapy Program at Tufts University School of Medicine where he coordinates and teaches in the musculoskeletal curricular track. His clinical research is in the area of spine pain examination and management. Dr. Schenk received his bachelor's and master's degrees from Ithaca College and his PhD from the University at Buffalo. Ron is a Fellow of the AAOMPT and is a Diplomat in Mechanical Diagnosis and Therapy. He has taught musculoskeletal examination and intervention in professional and post-professional physical therapy programs for 30 years on a full-time basis and his scholarship includes 33 peer-reviewed publications, a book chapter, and 68 professional presentations delivered at national and international conferences. He has received the American Academy of Orthopaedic Manual Physical Therapists’ Freddy Kaltenborn “Teach I Must” Award, the Mike Hage Lecture Award from the Rehabilitation Institute of Chicago, and the McKenzie Institute International Extension Award.
Megan Donaldson PT, PhD, FAAOMPT, serves as the Program Director for the Doctor of Physical Therapy Program at Tufts University School of Medicine. She completed her bachelor’s and master's degrees at D’Youville College and her PhD from Nova Southeastern University and is a Fellow American Academy of Orthopaedic Manual Physical Therapists. She has been a faculty member for 13 years and has 25 peer-reviewed publications, two book chapters, over 50 presentations musculoskeletal health and manual therapy related topics nationally. She serves nationally as the Conference Coordinator/Chair and Executive Board member of the American Academy of Orthopaedic Manual Physical Therapists (AAOMPT), and the American Physical Therapy Association (APTA) as an Ohio Delegate. Dr. Donaldson has earned numerous awards for research, education, and professional service to include being named Ohio Physical Therapy Association Outstanding PT Award, and Chamber of Commerce Award Top 20 under 40.
Jennifer Parent-Nichols, DPT, EdD, is a physical therapist and is certified as a Pediatric Clinical Specialist by the American Board of Physical Therapy Specialties, where she also serves a Council member. She has earned certification as a brain injury specialist and provides educational series for the Brain Injury Association of New Hampshire. She has worked extensively in pediatrics with experience in early intervention, school-based and outpatient therapy, and adolescent sports medicine. Dr. Parent-Nichols has taught in higher education since 2012, is a Clinical Associate Professor, and currently serves as Director of Student Affairs for the Doctor of Physical Therapy Program at Tufts University School of Medicine. Her areas of research include neurology, pediatrics, and education.
Mark Wilhelm PT, DPT, PhD, serves as the Director of Admissions and core faculty in the Doctor of Physical Therapy Program at Tufts University School of Medicine. He completed his Bachelor of Science in Exercise Science from the University of Akron, and his Doctor of Physical Therapy from Walsh University in Ohio. Dr. Wilhelm completed his Doctor of Philosophy in Rehabilitation Sciences from Texas Tech University Health Sciences Center. He received the Dean’s Excellence in Research Award for the School of Health Professions for his clinical musculoskeletal rehabilitation research and support area of clinical biomechanics research. Dr. Wilhelm’s scholarship includes over 20 peer reviewed journal articles and he has co-authored two book chapters.
Alexis A. Wright PT, PhD, DPT, OCS, FAAOMPT, serves as the Director of Curriculum and Assessment and core faculty in the Doctor of Physical Therapy Program at Tufts University School of Medicine. Dr. Wright received her BS in Kinesiology from the University of Illinois at Urbana-Champaign in 2003, a Doctorate of Physical Therapy from Duke University in 2006, and a PhD in physical therapy clinical research from the University of Otago, New Zealand in 2010. Dr. Wright was recognized as a Fellow of the American Academy of Orthopaedic Manual Physical Therapists in 2011 and achieved APTA board certified orthopedic specialization in 2015. Dr. Wright is also a 2019 graduate of the Education Leadership Institute Fellowship through the APTA. Dr. Wright is a frequent research presenter at state, national, and international meetings and a productive author with over 45 peer-reviewed manuscripts in the areas of orthopedics and manual therapy. Dr. Wright currently serves as the Deputy Editor of Physical Therapy Reviews as well as two journal editorial boards and acts as a reviewer for a number of other international and national peer-reviewed journals. Dr. Wright currently serves as a content expert item writer for the Orthopaedic Speciality Council of the American Board of Physical Therapy Specialties. She also currently serves on the APTA Lecture Awards Subcommittee and previous roles included APTA Awards Committee and Nominating Committee Chair of the American Academy of Orthopaedic Manual Physical Therapists. Dr. Wright is a 2007 recipient of the Emerging Leader Award for the American Physical Therapy Association and a 2012 recipient of the Dorothy Briggs Memorial Scientific Inquiry Award for the American Physical Therapy Association.
Josh ClelandPT, PhD, FAAOMPT, FAPTA, serves as the Director of Research and Faculty Development and core faculty in the Doctor of Physical Therapy Program at Tufts University School of Medicine. Dr. Cleland earned a Master of Physical Therapy degree from Notre Dame College and a Doctor of Physical Therapy degree from Creighton University. He received a PhD from Nova Southeastern University. He also received board certification from the American Physical Therapy Association as an Orthopaedic Clinical Specialist and completed a fellowship in manual therapy through Regis University in Denver, CO. Dr. Cleland has received over $700,000 in grant funding for clinical trials investigating the effectiveness of manual physical therapy and exercise in the management of spine and extremities disorders. He has published over 280 manuscripts in peer-reviewed journals and is an Editor for the Journal of Orthopaedic and Sports Physical Therapy. He is currently an author/editor on four textbooks, one of which has been published in nine different languages. Dr. Cleland is a well-known speaker at both the national and international levels and has delivered more than 225 keynote lectures and presentations in over 25 different countries. He is the recipient of numerous awards from the American Physical Therapy Association including the Jack Walker Award, the Eugene Michels New Investigator Award, the Chattanooga Research Award, the Rothstein Golden Pen Award for Scientific Writing, the Dorothy Baethke-Eleanor J. Carlin Award for Excellence in Academic Teaching and the Catherine Worthingham Fellowship Award. Additionally, he also received the 2013, 2014 and 2015 Rose Excellence in Research Award from the Academy of Orthopaedic Physical Therapy.
Appendix A.
Search Strategy Used in the Medline Database
The search strategy included MeSH Terms, keywords, and text words, related to upper quarter musculoskeletal pain treated with manual physical therapy procedures directed at the cervicothoracic and thoracic spine. Search strategies were altered, using data base specific filters, as necessary to complete searches in all data bases.
Articles published in the English language were searched using the above strategies. No publication date limitations were be used. Filters were used when able to restrict article searches to randomized controlled trials, controlled trials, or other trials with an appropriate control group. Hand searches were completed using reference lists of related articles. PubMed, AMED, SPORTDiscus, CINAHL, and the Cochrane Central register of controlled trials were searched with keywords thoracic, manipulation, upper quarter.
PubMed, AMED, SPORTDiscus, CINAHL, Cochrane Central register 1. Randomized controlled trials with or without a true control, sham intervention, or true comparison intervention 2. MeSH descriptor 3. Thoracic 4. Manipulation 5. Upper quarter.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- [1].Da Costa JT, Baptista JS, Vas M.. Incidence and prevalence of upper-limb work related musculoskeletal disorders: a systematic review. Work. 2015;51(4):635–644. [DOI] [PubMed] [Google Scholar]
- [2].Waersted M, Hanvold TN, Veiersted KB.. Computer work and musculoskeletal disorders of the neck and upper extremity: a systematic review. BMC Musculoskelet Disord. 2010;11:79. Published 2010 Apr 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Huisstede B, Bierma-Zeinstra S, Loes BW, et al. Incidence and prevalence of upper-extremity musculoskeletal disorders. A systematic appraisal of the literature. BMC Musculoskelet Disord. 2006;7:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].American Physical Therapy Association . Manual therapy techniques. In; guide to physical therapist practice 3.0. Vol. ch 38. Alexandria, VA: American Physical Therap Association; 2014. [Google Scholar]
- [5].Bokshan SL, DePasse JM, Eltorai AEM, et al. An evidence-based approach to differentiating the cause of shoulder and cervical spine pain. Am J Med. 2016;129(9):913–918. [DOI] [PubMed] [Google Scholar]
- [6].Crijns TJ, Ring D, Valencia V. Factors associated with the cost of care for the most common atraumatic painful upper extremity conditions. J Hand Surg Am. 2019;44(11):989.e1–989e18. [DOI] [PubMed] [Google Scholar]
- [7].Rosedale R, Rastogi R, Kidd J, et al. A study exploring the prevalence of Extremity Pain of Spinal Source (EXPOSS). J Man Manip Ther. 2020;28(4):222–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Wainner RS, Whitman JM, Cleland JA, et al. Regional interdependence: a musculoskeletal examination model whose time has come. J Orthop Sports Phys Ther. 2007;37:658–660. [DOI] [PubMed] [Google Scholar]
- [9].Bang MD, Deyle GD. Comparison of supervised exercise with and without manual physical therapy for patients with shoulder impingement syndrome. J Orthop Sports Phys Ther. 2000;30:126–137. [DOI] [PubMed] [Google Scholar]
- [10].Boyles RE, Flynn TW, Whitman JM. Manipulation following regional interscalene anesthetic block for shoulder adhesive capsulitis: a case series. Man Ther. 2005;10:164–171. [DOI] [PubMed] [Google Scholar]
- [11].Desjardins-Charbonneau A, Roy JS, Dionne CE, et al. The efficacy of manual therapy for rotator cuff tendi- nopathy: a systematic review and meta-analysis. J Orthop Sports Phys Ther. 2015;45:330–350. [DOI] [PubMed] [Google Scholar]
- [12].McDevitt A, Young J, Mintken P, et al. Regional interdependence and manual therapy directed at the thoracic spine. J Man Manip Ther. 2015;23:139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Mintken PE, Cleland JA, Carpenter KJ, et al. Some factors predict successful short-term outcomes in individuals with shoulder pain receiving cervico- thoracic manipulation: a single-arm trial. Phys Ther. 2010;90:26–42. [DOI] [PubMed] [Google Scholar]
- [14].Tate AR, McClure PW, Young IA, et al. Comprehensive impairment-based exercise and manual therapy intervention for patients with subacromial impingement syndrome: a case series. J Orthop Sports Phys Ther. 2010;40:474–493. [DOI] [PubMed] [Google Scholar]
- [15].Wassinger CA, Rich D, Cameron N, et al. Cervical & thoracic manipulations: acute effects upon pain pressure threshold and self-reported pain in experimentally induced shoulder pain. Man Ther. 2016;21:227–232. [DOI] [PubMed] [Google Scholar]
- [16].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Maher CG, Sherrington C, Herbert RD, et al. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–721. [PubMed] [Google Scholar]
- [18].Kaya DO, Baltaci G, Toprak U, et al. The clinical and sonographic effects of kinesiotaping and exercise in comparison with manual therapy and exercise for patients with subacromial impingement syndrome: a preliminary trial. J Manipulative Physiol Ther. 2014;37:422–432. [DOI] [PubMed] [Google Scholar]
- [19].Land H, Gordon S, Watt K. Effect of manual physiotherapy in homogeneous individuals with subacromial shoulder impingement: a randomized controlled trial. Physiother Res Int. 2019. Apr;24(2):e1768. Epub 2019 January 25. [DOI] [PubMed] [Google Scholar]
- [20].Kardouni JR, Shaffer SW, Pidcoe PE, et al. Immediate changes in pressure pain sensitivity after thoracic spinal manipulative therapy in patients with subacromial impingement syndrome: a randomized controlled study. Man Ther. 2015. Aug;20(4):540–546. Epub 2014 December 22. PMID: 25595413. [DOI] [PubMed] [Google Scholar]
- [21].Silva AC, Santos GM, Marques CM, et al. Immediate effects of spinal manipulation on shoulder motion range and pain in individuals with shoulder pain: a randomized trial. J Chiropr Med. 2019;18:19–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Fernández-Carnero J, Cleland JA, Arbizu RL. Examination of motor and hypoalgesic effects of cervical vs thoracic spine manipulation in patients with lateral epicondylalgia: a clinical trial. J Manipulative Physiol Ther. 2011;34(7):432–440. Epub 2011 July 23. PMID: 21875517. [DOI] [PubMed] [Google Scholar]
- [23].Riley SP, Cote MP, Leger RR, et al. Short-term effects of thoracic spinal manipulations and message conveyed by clinicians to patients with musculoskeletal shoulder symptoms: a randomized clinical trial. J Man Manip Ther. 2015;23(1):3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Park SJ, Kim SH, Kim SH. Effects of thoracic mobilization and extension exercise on thoracic alignment and shoulder function in patients with subacromial impingement syndrome: a randomized controlled pilot study. Healthcare. 2020;8:316–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Haider R, Bashir MS, Adeel M, et al. Comparison of conservative exercise therapy with and without Maitland Thoracic Manipulative therapy in patients with subacromial pain: clinical trial. J Pak Med Assoc. 2018;68(3):378–381. [PubMed] [Google Scholar]
- [26].Haik MN, Alburquerque-Sendin F, Camargo PR. Short-term effects of thoracic spine manipulation on shoulder impingement syndrome: a randomized controlled trial. Arch Phys Med Rehabil. 2017;98(8):1594–1605. [DOI] [PubMed] [Google Scholar]
- [27].Bergman GJ, Winters JC, Groenier KH, et al. Manipulative therapy in addition to usual medical care for patients with shoulder dysfunction and pain: a randomized, controlled trial. Ann Intern Med. 2004;141(6):432–439. [DOI] [PubMed] [Google Scholar]
- [28].Grimes JK, Puentedura EJ, Cheng MS, et al. The comparative effects of upper thoracic spine thrust manipulation techniques in individuals with subacromial pain syndrome: a randomized clinical trial. J Orthop Sports Phys Ther. 2019;49(10):716–725. [DOI] [PubMed] [Google Scholar]
- [29].Mintken PE, McDevitt AW, Cleland JA, et al. Cervicothoracic manual therapy plus exercise therapy versus exercise therapy alone in the management of individuals with shoulder pain: a multicenter randomized controlled trial. J Orthop Sports Phys Ther. 2016. Aug;46(8):617–628. PMID: 27477473. [DOI] [PubMed] [Google Scholar]
- [30].Vinuenza-Montoya S, Aguilar-Ferrándiz ME, Matarán-Peñarrocha GA, et al. A preliminary randomized clinical trial on the effect of cervicothoracic manipulation plus supervised exercises vs a home exercise program for the treatment of shoulder impingement. J Chiropr Med. 2017;16:85–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Wright AA, Donaldson M, Wassinger CA, et al. Subacute effects of cervicothoracic spinal thrust/non-thrust in addition to shoulder manual therapy plus exercise intervention in individuals with subacromial impingement syndrome: a prospective, randomized controlled clinical trial pilot study. Int J Sports Phys. 2017;13(1):121–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Sueki DG, Cleland JA, Wainner RS. A regional interdependence model of musculoskeletal dysfunction: research, mechanisms, and clinical implications. J Man Manip Ther. 2013;21(2):90–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Coronado RA, Gay CW, Biolosky JE, et al. Changes in pain sensitivity following spinal manipulation: a systematic review and meta-analysis. J Electromyogr Kinesiol. 2012;22950:752–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Bialosky JE, Beneciuk JM, Bishop MD, et al. Unraveling the mechanisms of manual therapy: modeling an approach. J Orthop Sports Phys Ther. 2018;48(1):8–18. [DOI] [PubMed] [Google Scholar]
- [35].Bialosky JE, Bishop MD, Price DD, et al. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14(5):531–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Bialosky JE, Bishop MD, Penza CW. Placebo mechanisms of manual therapy: a sheep in wolf’s clothing? J Orthop Sports Phys Ther. 2017;47(5):301–304. [DOI] [PubMed] [Google Scholar]
- [37].Ghamkhar L, Arab AM, Nourbakhsh MR, et al. Examination of regional interdependence theory in chronic neck pain: interpretations from correlation of strength measures in cervical and pain-free regions. Pain Med. 2020;21(2):e182–e190. [DOI] [PubMed] [Google Scholar]


