ABSTRACT
Objective
To assess the effects of mobilization with movement (MWM) on pain, range of motion (ROM), and disability in the management of shoulder musculoskeletal disorders.
Methods
Six databases and Scopus, were searched for randomized control trials. The ROB 2.0 tool was used to determine risk-of-bias and GRADE used for quality of evidence. Meta-analyses were performed for the sub-category of frozen shoulder and shoulder pain with movement dysfunction to evaluate the effect of MWM in isolation or in addition to exercise therapy and/or electrotherapy when compared with other conservative interventions.
Results
Out of 25 studies, 21 were included in eight separate meta-analyses for pain, ROM, and disability in the two sub-categories. For frozen shoulder, the addition of MWM significantly improved pain (SMD −1.23, 95% CI −1.96, −0.51)), flexion ROM (MD −11.73, 95% CI −17.83, −5.64), abduction ROM (mean difference −13.14, 95% CI −19.42, −6.87), and disability (SMD −1.50, 95% CI (−2.30, −0.7). For shoulder pain with movement dysfunction, the addition of MWM significantly improved pain (SMD −1.07, 95% CI −1.87, −0.26), flexion ROM (mean difference −18.48, 95% CI- 32.43, −4.54), abduction ROM (MD −32.46, 95% CI – 69.76, 4.84), and disability (SMD −0.88, 95% CI −2.18, 0.43). The majority of studies were found to have a high risk of bias.
Discussion
MWM is associated with improved pain, mobility, and function in patients with a range of shoulder musculoskeletal disorders and the effects clinically meaningful. However, these findings need to be interpreted with caution due to the high levels of heterogeneity and risk of bias.
Level of Evidence
Treatment, level 1a.
KEYWORDS: Mulligan’s mobilization with movement, manual therapy, systematic review, shoulder dysfunction
Introduction
Demand for effective conservative management of shoulder conditions reflects its prevalence as the third most common musculoskeletal (MSK) condition seen in United Kingdom (UK) [1] with one-year prevalence among a global survey reported to be between 4.7 and 46.7% [2]. Clinicians may be challenged by the scope of possible structural diagnoses, the changing nomenclature used to describe the experience of pain, distress and loss of function, and the application of recommended management strategies [3].
Current guidelines for the conservative management of shoulder conditions include exercise, patient education, manual therapy, activity modification, non-steroidal anti-inflammatory drugs, and corticosteroid injections [4,5]. The hierarchy in the priority of these strategies suggests exercise as the first in line for management [6]. Multimodal care has also been promoted [7], as having strong recommendations for exercise combined with manual therapy in a recent literature review [6].
The application of effective manual therapy is ambiguous due to the variety of techniques, dosage, duration of affect, progressions, and rational for its usage [6]. In systematic reviews, all varieties of manual therapy are synthesized [6–9], which often does not allow discrimination between techniques or help guide clinicians. Mobilization with movement (MWM) is one specific form of manual therapy gaining increasing popularity with a number of studies showing treatment benefit for a range of shoulder conditions [9–12]. MWM involves the application of sustained gliding force (passive mobilization component) with a concurrent active movement performed by the patient (active movement component). The application of MWM, when precisely indicated, has beneficial effects on painful movement and thereby function is immediately improved. Thus, MWM can be distinguished from passive, practitioner-applied manual therapy which is based on a test-treat-retest model of application [13]. The immediate symptom modification feature of MWM may allow greater clarity to allow clinicians to discriminate between manual therapy selections.
Previous systematic reviews evaluating the effectiveness of MWM lack the precise work on shoulder [14] and excluded many studies focused on a shoulder-specific population [15]. Although a recent systematic review for shoulder conditions has been undertaken [16], the current review is indicated as the previous work lacked robustness due to, identification and exclusion of studies selected, the presence of new studies since its release, and no pre-registration of its proposal. Therefore, we undertook a systematic review with meta-analysis to determine the additional benefits of MWM when compared to other non-surgical forms of management, including other forms of manual therapy, electrotherapy, placebo, sham, or no treatment for shoulder musculoskeletal disorders in two categories: frozen shoulder or shoulder pain with movement dysfunction. Frozen shoulder is a readily identifiable syndrome, but the diagnosis of other shoulder-specific disorders is problematic. Hence, we chose to separate frozen shoulder from other unknown shoulder disorders.
Methods
This review was conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The systematic review was prospectively registered on PROSPERO: CRD42020210618.
Data sources and searches
The following databases were searched: PubMed (MEDLINE), CINAHL, SPORTDiscus, PEDro, Cochrane library, and Scopus, from inception to January 2021 (appendix 1). Appropriate search and MeSH terms were adapted and applied to each database. To supplement the initial database searches, a manual search of the references listed in identified systematic reviews was also conducted.
Eligibility criteria
We included randomized-controlled trials (RCTs) and randomized cross-over studies evaluating the effects of MWM or self-MWM on shoulder conditions, either alone or in combination with other interventions. The comparator group comprised no intervention, any other form of conservative intervention including ‘wait and see’, usual care, standard care, sham, or placebo but not including MWM intervention. Studies were considered if they included adults aged 18 years and above of either gender and used outcome measures of pain severity, range of motion (ROM), and disability scores.
Studies were excluded if the full text was not available and if the language was not English.
Duplicate studies identified as a result of searching multiple databases were removed using EndNoteX8 software. The titles and abstracts were screened by two assessors independently (KS and GM), according to predetermined eligibility criteria. Full-text articles were assessed and, if there was uncertainty over the inclusion of a study, a third reviewer (SR) was consulted until consensus was reached.
Quality assessment and data extraction
Each study’s risk of bias was assessed using the ROB 2.0 tool [17]. This tool evaluates the risk of bias across five domains: the randomization process, deviations from intended interventions, missing outcome data, measurement of outcomes, and selection of reported results. The tool includes algorithms that map responses to signaling questions onto a proposed risk-of-bias judgment for each domain, leading reviewers to make a judgment of ‘Low risk of bias’, ‘Some concerns’, or ‘High risk of bias’ both for each domain and as an overall risk-of-bias judgment for each study. Two reviewers (KS, GM) independently performed risk of bias assessments on all studies and any discrepancies were resolved by consensus discussion.
The approach proposed by the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) Working Group for rating the quality of the best available evidence and developing health care recommendations [18] was used to rate the quality of the evidence and grade the certainty of outcomes in the meta-analysis. Using the GRADE approach, the quality of evidence was rated independently by two reviewers (KS and GM) according to four levels ranging from high to very low (Box 1).
Box 1.
Quality of evidence ratings using the GRADE approach
| High | We are very confident that the true effect lies close to that of the estimate of the effect. |
| Moderate | We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different |
| Low | Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. |
| Very Low | We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect |
Two independent reviewers extracted data using a data extraction form. Other review members were consulted if necessary. If all information was not readily available in the studies, numerical data were requested from author groups.
Data synthesis
A narrative synthesis of aggregate data was provided within the review by describing the population characteristics, methodology, and results of included studies.
The trials were compared for homogeneity through visual examination (Tables 1 and 2). If trials were sufficiently homogenous and could be grouped according to outcome measures, that is, range of motion, pain, and disability scores, a meta-analysis was performed to provide a quantitative synthesis of aggregate data from the included studies. If only one study was available in the grouping, meta-analysis could not be performed and the statistics from that single study were reported. Review Manager 5.3 (Cochrane Collaboration) software was used for the statistical analysis. If all included trials used the same outcome measure, a summary of intervention effects was reported as a weighted mean difference with 95% confidence intervals and p-value. If the included trials used different outcome measures, a summary of intervention effects was reported as a standardized mean difference with 95% confidence intervals and p-value. A fixed-effect model was used when there was no evidence of heterogeneity between studies, otherwise, a random-effects model was applied. Clinical variation and heterogeneity between studies were examined and evaluated using Q statistic and I2 tests. Forest plots were used to illustrate the outcomes of meta-analysis. The I2 statistic, an expression of inconsistency of studies’ results, describes the percentage of variation across studies because of heterogeneity rather than by chance. A high values of I2 (>50%) and P < .05 indicate statistically significant heterogeneity among the studies for an outcome. The reasons for high heterogeneity were explored. The interpretations for trivial, small, medium, and large effect sizes (≤0.2 trivial effect, 0.2–0.49 small effect; 0.5–0.79 medium effect; ≥0.8, large effect) were chosen [19].
Table 1.
Characteristics of included studies (frozen shoulder sub-category)
| Study(Author, Year, Design,) |
Participants (n, M:F, Age) | Experimental Intervention |
Comparator intervention |
Dose | Outcome measures and Time points | Main Findings |
|---|---|---|---|---|---|---|
| Boruah et al. 2015, RCT | Exp: n = 25, 7:18, 49.76 (3.49) | MWM + Exercise + Heat therapy | Scapular Mobilization + Exercise + Heat | 5 per week X 3 weeks | ROM, SPADI- pain. Baseline, 3 weeks | Significant improvement in all outcomes for MWM group compared to control group |
| Con: n = 25, 11:14, 50.04 (3.34) | ||||||
| Dilip et al. 2016, RCT | Exp: n = 20, 9:11, 53.55 (7.57) | MWM+ Exercise | Gong’s Mobilization + Exercise | 5 per week X 2 weeks | ROM, Pain intensity. Baseline, 2 weeks |
Significant improvement in pain intensity for Gong’s mobilization and in ROM for MWM |
| Con: n = 20, 9:11, 51.00 (6.82) | ||||||
| Goyal et al. 2013, RCT | Exp: n = 10, 6:4, 50.40 (5.85) | MWM + Exercise | 1. End range Mobilization + Exercise 2. End range Mobilization + MWM + Exercise |
2 per week X 3 weeks | ROM, SPADI. Baseline, 3 weeks |
Significant improvement in all outcomes for MWM + End range Mobilization group + Exercises compared to other groups |
| 1. Con: n = 10, 6:4, 48.60 (5.37) 2. | ||||||
| Con: n = 10, 4:6, 47.90 (4.35) | ||||||
| Khyathi et al. 2015, RCT | Exp: n = 20, 12:8, 50.40 (5.42) | MWM + Exercise | Spencer technique + Exercise | 5 per week X 1 week | ROM, Pain intensity, SPADI. Baseline, 5 sessions (1 week) | Significant improvement in ROM and SPADI but not pain intensity for MWM group compared to Spencer technique group |
| Con: n = 20, 11:9, 50.85 (5.14) | ||||||
| Minerva et al. 2016, RC | Exp: n = 30, NA,NA | MWM + Exercise | Maitland Mobilization + Exercise | 3 per week X 4 weeks | ROM, SPADI. Base line, 4 weeks |
Significant improvement in all outcomes for MWM group compared to Maitland Mobilization group |
| Con: n = 30, NA, NA | ||||||
| Rathod et al. 2019, RCT | Exp: n = 20, NA,NA | MWM + Heat | Kaltenborn Mobilization + Heat | 10 sessions X 3 weeks | ROM, Pain intensity, SPADI. Baseline, 10 sessions | Significant improvement in all outcomes for MWM group compared to Kaltenborn Mobilization group |
| Con: n = 20, NA,NA | ||||||
| Shrivastava et al. 2011, RCT | Exp: n = 20, 12:8, 59.2 (7.18) | MWM + Exercise | Maitland Mobilization + Exercise | 6 per week x 2 weeks, | ROM, Pain intensity, SPADI. Baseline, 4 weeks | Significant improvement in pain intensity for MWM group compared to Maitland group |
| Con: n = 20, 7:13, 51.15 (8.53) | ||||||
| Doner et al. 2012, RCT | Exp: n = 20, 7:13, 59.25 (9.17) | MWM + Heat + TENS | Heat + Exercise +TENS | 5 per week X 3 weeks | ROM, Pain intensity, Constant score, Shoulder Disability Questionnaire Baseline, 3 weeks, 3 months | Significant improvement in all outcomes for MWM group compared to control group |
| Con: n = 20, 2:18, 58.55 (8.57) | ||||||
| Sai et al. 2015, RCT | Exp: n = 30, 14:20, 50.5 (5.9) | MWM + Exercise | Exercise | 2 per week x 12 weeks | ROM, Pain intensity, DASH. Baseline, 3 weeks, 6 weeks, 3 months |
Significant improvement in all outcomes for MWM group compared to control group |
| Con: n = 30, 15:19, 51.0 (7.7) | ||||||
| Ranjana et al. 2017, RCT | Exp: n = 15, NA,NA | MWM + Exercise | 1. Maitland Mobilization + Exercise 2. Exercise |
3 per week x 4 weeks | ROM, Pain intensity, SPADI. Baseline, 4 weeks, 6 weeks | Significant improvement in all outcomes except external rotation ROM for MWM group compared to Maitland and only exercise group |
| 1. Con: n = 15, NA,NA | ||||||
| 2. Con: n = 15, NA,NA | ||||||
| Arshad et al. 2015, RCT | Exp: n = 50, NA,NA | MWM + Exercise + Ultrasound + TENS + Home Exercise | Maitland Mobilization + Ultrasound + TENS + Home Exercise | 2 per week X 2 months | ROM, Pain intensity. Baseline, 2 months |
No significant difference in any outcome for MWM group compared to Maitland group |
| Con: n = 50, NA,NA | ||||||
| Haider et al. 2014, RCT | Exp: n = 30, 10:20, 47 (9.21) | MWM | Maitland Mobilization | NA | ROM Baseline, 2 weeks, 4 weeks, 6 weeks |
Significant improvement in all outcomes for MWM group compared to Maitland group |
| Con: n = 30, 7:23, 46.23 (9.71) | ||||||
| Yeole et al. 2017, RCT | Exp: n = 15, NA,NA | MWM + Exercise | Exercise | 7 sessions | ROM, Pain intensity, SPADI. Baseline, 1 week |
Significant improvement in all outcomes for MWM group compared to control group |
| Con: n = 15, NA,NA | ||||||
| Youssef et al. 2015, RCT | Exp: n = 15, NA, 54.8 (5.85) | MWM + Exercise | Maitland Mobilization + Exercise | 3 per week X 6 weeks | ROM, SPADI. Baseline, 6 weeks |
Significant improvement in all outcomes for MWM group compared to Maitland group |
| Con: n = 15, NA, 53.4 (5.23) |
Exp: Experimental group, Con: Control group, RCT: Randomized clinical trial, MWM: Mobilization with movement, ROM: range of motion, SPADI: Shoulder Pain and Disability Index, TENS: transcutaneous electrical nerve stimulation, DASH: Disability of Arm Shoulder and Hand, NA: Not available, US: Ultrasound, VAS: Visual analogue scale
Table 2.
Characteristics of included studies (Shoulder pain with movement dysfunction sub-category)
| Study(Author,Year, Design) | Participants (n, M:F, Age) | Experimental intervention |
Comparator intervention |
Dose | Outcome measures and Time points | Main Findings |
|---|---|---|---|---|---|---|
| Kachingwe 2008, Pilot RCT | Exp: n = 9, 5:4, 48.9 (13.7) | MWM + Exercise | 1. Kaltenborn mobilization + Exercise 2. Exercise 3. Control |
1 per week x 6 weeks | ROM, Pain intensity, SPADI. Baseline, 3 weeks | No significant difference in any outcome between the groups post intervention |
| 1. Con: n = 9, 4:5, 43.4 (14.7) | ||||||
| 2. Con: n = 8, 4:4, 47.3 (20.1) | ||||||
| 3. Con: n = 7, 4:3 45.6 (13.0) | ||||||
| Djordjevic 2012, RCT | Exp: n = 10, 4:6, 51.80 (5.3) | MWM + kinesiotaping | Exercise | 10 sessions | ROM. Baseline, 5 & 10 days |
Significant improvement in ROM for MWM + kinesiotaping group compared to control group |
| Con: n = 10, 3:7, 54.10 (6.8) | ||||||
| Srivastava 2018, RCT | Exp: n = 11, NA, 50.09 (11.36) | MWM + Exercise | Cryotherapy + Exercise | 6 sessions | ROM, Pain intensity, SPADI. Baseline, after 1st and 6th intervention | No significant difference in any outcome for MWM group compared to Cryotherapy group |
| Con: n = 11, NA, 41.91 (11.22) | ||||||
| Delgado 2015, RCT | Exp: n = 21, 4:17, 55.4 (7.8) | MWM | Sham | 2per week X 2 weeks | ROM, Pain intensity. Baseline, 2 weeks |
Significant improvement in all outcomes for MWM group compared to sham group |
| Con: n = 21, 4:17, 54.3 (10) | ||||||
| Guimarães 2016, Crossover RCT | Exp: n = 14, 6:8, NA | MWM | Sham | 4 x sessions to crossover 48 hours apart | ROM, Pain intensity, SPADI, DASH, Muscle strength. Baseline, after 4x sessions (around 8–10 days) | No significant difference in any outcome for MWM group compared to sham group |
| Con: n = 13, 6:7, NA | ||||||
| Teys 2006, Crossover RCT | n = 24,11:3, 46.1 (9.86) | MWM | Sham control |
3 sessions | ROM, pressure pain threshold. Baseline – 3 sessions with 24 hr interval | Significant improvement in all outcomes for MWM group compared to sham and control group |
| Exp: n = 15, 11:4, 40.23 (10.55) | ||||||
| Neelapala 2016, RCT | Con: n = 16, 12:4, 42.41 (10.38) | MWM + Exercise | Exercise | 3 sessions | Pain, muscle strength, Scapular upward rotation. Baseline, after 3 sessions |
Significant improvement in pain and external rotation strength for MWM group compared to control group |
| Romero 2015, Pilot RCT | Exp: n = 22, 11:11, 84.7 (8.7) | MWM + postural advice + Exercise | Postural advice + Exercise | 3 per week x 2 weeks | Baseline, 2 weeks, 1 and 3 months | No significant between and within groups differences in any outcome |
| Con: n = 22, 11:11, 83.1 (7.8) | ||||||
| Satpute 2015, RCT | Exp: n = 22, 10:12, 53.41 (7.08) | MWM+ Exercise + Heat | Exercise + Heat | 3 per week X 3 weeks | ROM, Pain intensity, SPADI, Baseline, 3 weeks | Significant improvement in all outcomes for MWM group compared to control group |
| Con: n = 22,15:7, 52.41 (7.06) | ||||||
| Subhash 2020, RCT | Exp: n = 16, NA, 30.87 (9.37) | MWM + Exercise + Heat | Exercise + Heat | 6 sessions over 2 weeks | ROM, Pain intensity, SPADI, Baseline, 2 weeks | Significant improvement in pain intensity and flexion ROM for MWM group compared to control group. No significant difference between groups for any other outcomes |
| Con: n = 16, NA, 32.37 (9.74) | ||||||
| Menek 2019, RCT | Exp: n = 15, 8:7, 51.73 (6.64) | MWM+ Exercise + Cryotherapy + TENS+US | Exercise + Cryotherapy + TENS+US | 5 per week X 6 weeks | ROM, Pain intensity, DASH, SF-36 Base line, 6 weeks |
Significant improvement in all outcomes for MWM group compared to control group |
| Con: n = 15, 10:5, 50.26 (4.28) |
Exp: Experimental group, Con: Control group, RCT: Randomized clinical trial, MWM: Mobilization with movement, ROM: range of motion, SPADI: Shoulder Pain and Disability Index, TENS: Transcutaneous electrical nerve stimulation, DASH: Disability of Arm Shoulder and Hand, NA: Not available, US: Ultrasound, VAS: Visual analogue scale, SF-36: Short Form-36.
Results
Results of the literature search
A literature search was conducted in six databases from inception to January 2021 and identified a total of 1956 studies (Appendix 1). After removing duplicates 1620 studies remained for title and abstract screening. Seventeen additional studies were identified through hand searching reference lists. Thus, the title and abstract of 1637 studies were screened. From these, 31 potentially eligible studies for full-text assessment were identified, and 25 [10–12,20–41] studies were included based on the inclusion and exclusion criteria (Figure 1).
Figure 1.
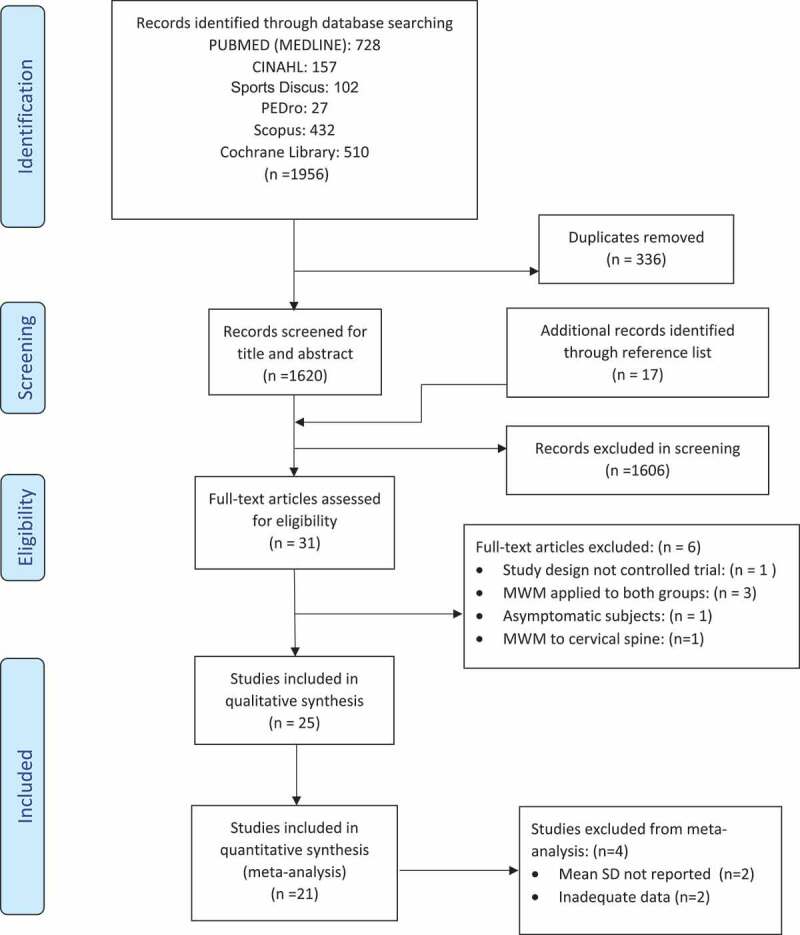
Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram.
The characteristics of included studies are summarized in Table 1 (frozen shoulder sub-category) and Table 2 (shoulder pain and movement dysfunction sub-category).
Qualitative synthesis
All included studies were RCTs. Two of the RCT’s were a crossover design [25,39] and two were pilot studies [10,27]. Only six studies were registered with a clinical trial registry [10,12,23,25,35,37]. In the evaluated studies, there were a total of 1014 participants. Fourteen studies evaluated 665 patients with frozen shoulder and 11 studies evaluated 349 patients with shoulder pain and movement dysfunction. Among the frozen shoulder sub-category, all studies except two [11,33] evaluated MWM in combination with exercise therapy. MWM was compared with other manual therapy techniques including Maitland mobilization (seven studies) and Kaltenborn mobilization (two studies). All studies included patients with unilateral stage-II frozen shoulder except three studies, where the stage of frozen shoulder was not reported [24,26,40]. Three studies included patients with frozen shoulder who had a history of diabetes mellitus [20,34,41]. In the shoulder pain and movement dysfunction sub-category, three studies evaluated MWM in isolation which was compared with a sham intervention [12,25,39]. In seven studies, MWM was used in conjunction with electrotherapeutic modalities such as the heat therapy, cryotherapy, therapeutic ultrasound, and transcutaneous electrical nerve stimulation (TENS). There was wide variability in the MWM treatment dosage such as the number of treatment sessions utilized during the study period, which ranged from a minimum of three sessions to a maximum of 24 sessions. MWM intervention was applied for a minimum of 1 week and a maximum of 2 months and only three studies followed patients over a longer time course, with a maximum of 3-months follow-up [10,11,34]. None of the studies followed the Mulligan Concept treatment guidelines of only applying MWM in patients who had a beneficial effect following a trial MWM. The most commonly reported MWM technique was a postero-lateral glide combined with active arm elevation. Only two studies evaluated an inferior glide, which was combined with movement of hand behind back [22,35]. One study evaluated scapulothoracic MWM in a weight-bearing position [38].
Risk of bias assessment
The results of the risk of bias assessment are seen in Figure 2. Of the 25 studies assessed, three were rated as an overall risk of bias of ‘low risk’, four were rated as ‘some concerns’ and 18 were rated as having ‘high risk’. The most common methodological problems in the included studies resulting in a high risk of bias were a lack of concealed allocation (14 studies) and failure to blind outcome assessors (13 studies). As most studies were not registered prospectively, there was often no study protocol, leading to a decision of ‘some concerns’ for domain two and domain five for most studies.
Figure 2.
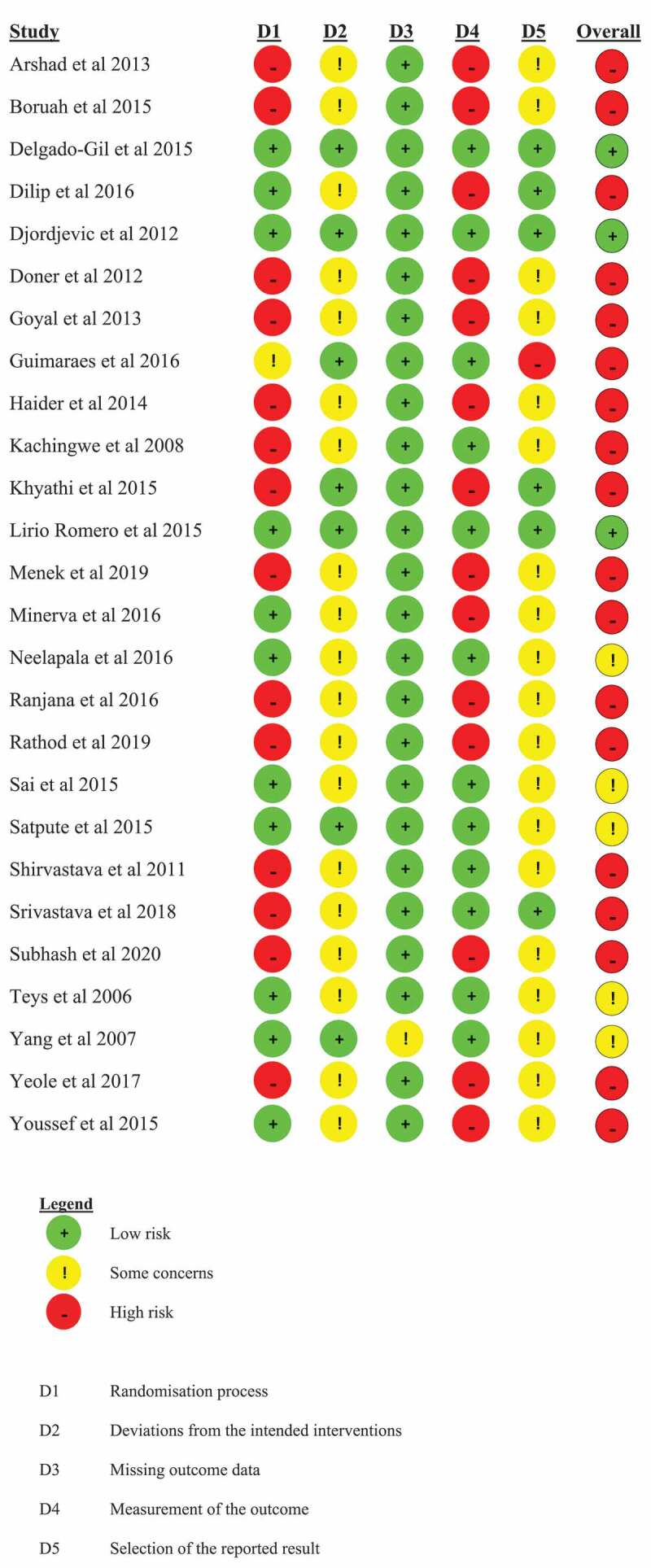
ROB 2.0 judgements according to domain and overall risk of bias for each study
Meta-analysis
Meta-analysis was carried out on the results from 21 studies using the post-intervention scores for experimental and control groups. For studies comparing MWM with more than one control group, control groups were combined into a single group. Analyzed studies displayed high levels of heterogeneity (I2 > 75%); hence, the results are presented based on the random effects model. Meta-analysis was not possible in four studies for the following reasons: mean values and SD were not reported [10,27]; or inadequate data were available [30,36]. Authors of studies with missing data were contacted but no response was received except for Romero et al [10] where data were not available.
Meta-analyses were performed for the sub-category of frozen shoulder (12 studies available) and for the sub-category shoulder pain with movement dysfunction (nine studies available) to assess the immediate effects of MWM on pain, flexion, and abduction ROM, as well as disability up to 2-month post-intervention. For both sub-categories, meta-analyses were performed to evaluate the effect of MWM, either in addition to exercise therapy and/or electrotherapy or MWM alone (experimental group) when compared to either exercise therapy and electrotherapy alone or other type of manual therapy (control group). The random effects model was chosen as a conservative measure to account for heterogeneity among included studies. Standardized mean differences (SMD) with 95% confidence intervals (CIs) were calculated for pain and disability. Mean differences (MD) with 95% confidence intervals (CIs) were calculated separately for flexion and abduction ROM.
Frozen shoulder
Pooled data from eight studies with 345 participants were combined for analysis of the effects of MWM on pain. Statistically significant improvement was present post-intervention favoring MWM (SMD [95% CI]: −1.23 [−1.96, −0.51] Z = 3.35 (P = 0.0008) with high levels of heterogeneity (I2 = 89%) (Figure 3(A)). Pooled data from nine studies with 430 participants were grouped for analysis of the effects of MWM on flexion ROM. Statistically significant improvement was present post-intervention favoring MWM (mean difference [95% CI]: −11.73 [−17.83, −5.64] Z = 3.77 (P = 0.0002) with high levels of heterogeneity (I2 = 82%) (Figure 3(B)). Pooled data from nine studies with 465 participants were grouped for analysis of the effects of MWM on abduction ROM. Statistically significant improvement was present post-intervention favoring MWM (mean difference [95% CI]: −13.14 [−19.42, −6.87] Z = 4.10 (P < 0.0001) with high levels of heterogeneity (I2 = 85%) (Figure 3(C)). Pooled data from eight studies with 305 participants were grouped for analysis of the effects of MWM on disability. Statistically significant improvement was present post-intervention favoring MWM (SMD [95% CI]: −1.50 [−2.30, −0.71] Z = 3.69 (P = 0.0002) with high levels of heterogeneity (I2 = 89%) (Figure 3(D)).
Figure 3.
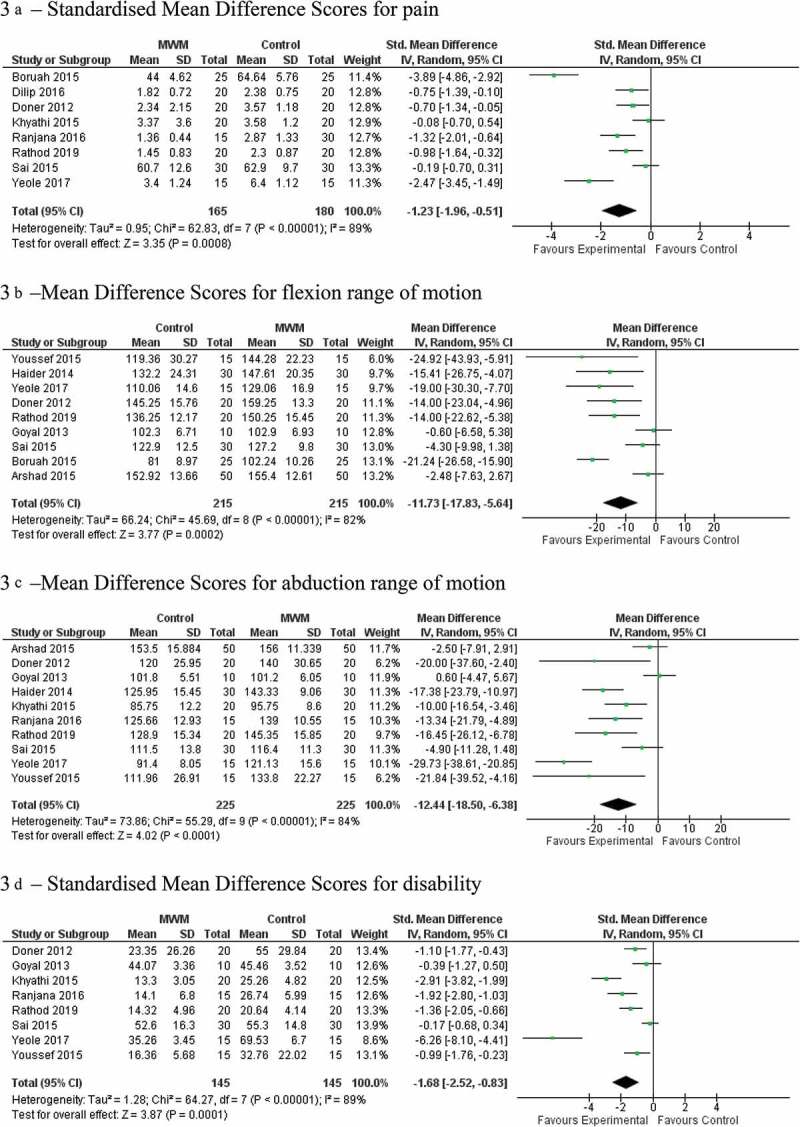
Forest plots for frozen shoulder sub category (a) Standardized Mean Difference Scores for pain. (b) Mean Difference Scores for flexion range of motion. (c) Mean Difference Scores for abduction range of motion. (d) Standardized Mean Difference Scores for disability.
Shoulder pain with movement dysfunction
Pooled data from seven studies with 228 participants were grouped for analysis of the effects of MWM on pain. Statistically significant improvement was present post-intervention favoring MWM (SMD [95% CI]: −1.07 [−1.87, −0.26] Z = 2.61 (P = 0.009) with high levels of heterogeneity (I2 = 86%) (Figure 4(A)). Pooled data from seven studies with 173 participants were grouped for analysis of the effects of MWM on flexion ROM. Statistically significant improvement was present post-intervention favoring MWM (mean difference [95% CI]: −18.48 [−32.43, −4.54] Z = 2.60 (P = 0.009) with high levels of heterogeneity (I2 = 90%) (Figure 4(B)). Pooled data from five studies with 151 participants were grouped for analysis of the effects of MWM on abduction ROM. Statistically significant improvement was present post-intervention favoring MWM (mean difference [95% CI]: −32.46 [−69.76, 4.84] Z = 1.71 (P = 0.09) with high levels of heterogeneity (I2 = 97%) (Figure 4(C)). Pooled data from five studies with 155 participants were grouped for analysis of the effects of MWM on disability. Statistically significant improvement was present post-intervention favoring MWM (SMD [95% CI]: −0.88 [−2.18, 0.43] Z = 1.32 (P = 0.19) with high levels of heterogeneity (I2 = 92%) (Figure 4(D)). Improvement in shoulder flexion and abduction ROM in both sub-categories is clinically relevant, as improvement was greater than the reported MDC of 11ο for patients with shoulder pathologies [42].
Figure 4.
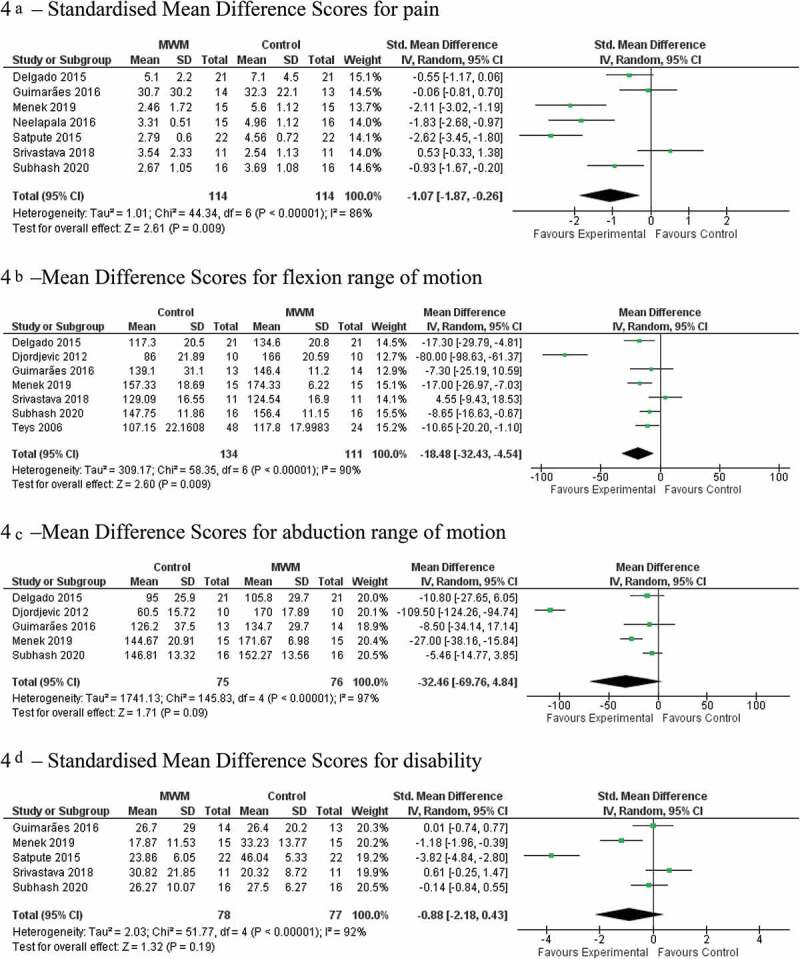
Forest plots for shoulder pain with movement dysfunction sub-category. (a) Standardized Mean Difference Scores for pain. (b) Mean Difference Scores for flexion range of motion. (c) Mean Difference Scores for abduction range of motion. (d) Standardized Mean Difference Scores for disability.
GRADE analysis for frozen shoulder sub-category
For the frozen shoulder sub-group, the certainty of the effect estimate was rated as very low for all four variables analyzed in the meta-analysis (Table 3). For the shoulder pain with movement dysfunction sub-group, the certainty of the effect estimate was rated as very low for all four variables analyzed in the meta-analysis (Table 4).
Table 3.
GRADE assessment for the frozen shoulder sub-category
| Certainty assessment |
№ of patients |
Effect |
Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| № of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | MWM | other interventions or no intervention | Relative(95% CI) | Absolute(95% CI) | ||
| Pain (assessed with: VAS, NPRS or SPADI-Pain) | ||||||||||||
| 8 | randomized trials | very serious a | serious b | not serious | serious c | none | 165 | 180 | - | SMD 1.23 lower(1.96 lower to 0.51 lower) | ⨁◯◯◯VERY LOW | |
| Flexion ROM (assessed with: degrees) | ||||||||||||
| 9 | randomized trials | very serious d | serious b | not serious | serious e | none | 215 | 215 | - | MD 11.73 lower(17.81 lower to 5.64 lower) | ⨁◯◯◯VERY LOW | |
| Abduction ROM (assessed with: degrees) | ||||||||||||
| 10 | randomized trials | very serious f | serious b | not serious | serious e | none | 240 | 225 | - | MD 13.14 lower(19.42 lower to 6.87 lower) | ⨁◯◯◯VERY LOW | |
| Disability (assessed with: DASH, SPADI, Shoulder Constant) | ||||||||||||
| 8 | randomized trials | very serious a | serious b | not serious | serious c | none | 145 | 160 | - | SMD 1.5 lower(2.3 lower to 0.71 lower) | ⨁◯◯◯VERY LOW | |
GRADE: Grading of Recommendations Assessment, Development and Evaluation, CI: Confidence interval; SMD: Standardized mean difference; MD: Mean difference, VAS: Visual analogue scale, NPRS: Numeric pain rating scale, SPADI: Shoulder Pain and Disability Index
Explanations
a. Of the eight studies included in the analysis, seven were scored as a high risk of bias when using the ROB 2.0 tool. Most studies did not have concealed allocation, blinded assessors or a pre-published protocol.
b. Considerable heterogeneity was evident as measured by an I squared score of > 80%.
c. Total sample size for pain and disability is fewer than the recommended number of 400 for analyses using the standardized mean difference.
d. Of the nine studies included in the analysis, eight were scored as a high risk of bias when using the ROB 2.0 tool. Most studies did not have concealed allocation, blinded assessors or a pre-published protocol.
e. The lower boundary of the 95% confidence interval does not exceed the minimal clinically important difference of 12 degrees.
f. Of the ten studies included in the analysis, nine were scored as a high risk of bias when using the ROB 2.0 tool. Most studies did not have concealed allocation, blinded assessors or a pre-published protocol.
Table 4.
GRADE assessment for the shoulder pain with movement dysfunction sub-category
| Certainty assessment |
№ of patients |
Effect |
Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| № of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | MWM | other interventions or no interventions | Relative(95% CI) | Absolute(95% CI) | ||
| Pain (assessed with: VAS or NPRS) | ||||||||||||
| 7 | randomized trials | serious a | serious b | not serious | serious c | none | 114 | 114 | - | SMD 1.07 lower(1.87 lower to 0.26 lower) | ⨁◯◯◯VERY LOW | |
| Flexion ROM (assessed with: goniometry (degrees)) | ||||||||||||
| 7 | randomized trials | serious d | serious b | not serious | serious e | none | 134 | 111 | - | MD 18.48 lower(32.43 lower to 4.54 lower) | ⨁◯◯◯VERY LOW | |
| Abduction ROM (assessed with: goniometry (degrees)) | ||||||||||||
| 5 | randomized trials | serious f | serious b | not serious | serious e | none | 75 | 76 | - | MD 32.46 lower(69.76 lower to 4.84 higher) | ⨁◯◯◯VERY LOW | |
| Disability (assessed with: DASH or SPADI) | ||||||||||||
| 5 | randomized trials | very serious g | serious b | not serious | serious h | none | 78 | 77 | - | SMD 0.88 lower(2.18 lower to 0.43 higher) | ⨁◯◯◯VERY LOW | |
GRADE: Grading of Recommendations Assessment, Development and Evaluation, CI: Confidence interval; SMD: Standardized mean difference; MD: Mean difference, DASH: Disabilities of the Arm, Shoulder and Hand, SPADI: shoulder Pain and Disability Index,
Explanations
a. Of the seven studies included in the analysis, four were scored as a high risk of bias and two were scored as some concerns when using the ROB 2.0 tool. Three studies failed to have concealed allocation and two studies failed to have blinded outcome assessors while there were concerns with selection of the reported result with one study.
b. Considerable heterogeneity was evident as measured by an I2 score of >85%
c. Total sample size for pain and disability is fewer than the recommended number of 400 for analyses using the standardized mean difference
d. Of the seven studies included in the analysis, four were scored as a high risk of bias and one was scored as some concerns when using the ROB 2.0 tool. Three studies failed to have concealed allocation, two studies failed to have blinded outcome assessors while there were concerns with selection of the reported result with one study.
e. The lower boundary of the 95% confidence interval does not exceed the minimal clinically important difference of 12 degrees
f. Of the five studies included in the analysis, two were scored as a high risk of bias and one was scored as some concerns when using the ROB 2.0 tool. One study failed to have concealed allocation and there were concerns with selection of the reported result in one study.
g. Of the five studies included in the analysis, four were scored as a high risk of bias and one was scored as some concerns when using the ROB 2.0 tool. Three studies failed to have concealed allocation and two studies failed to have blinded outcome assessors while there were concerns with selection of the reported result in one study.
h. Total sample size for pain and disability is fewer than the recommended number of 400 for analyses using the standardized mean difference.
Discussion
The objective of this systematic review and meta-analysis was to determine the additional benefits of MWM in terms of pain, flexion, and abduction ROM, as well as disability when compared to other non-surgical forms of management, including other forms of manual therapy, electrotherapy, placebo, sham, or no treatment for shoulder musculoskeletal disorders in two categories: frozen shoulder or shoulder pain with movement dysfunction.
Findings
Our results indicate important benefits of MWM for all variables in each category, although caution is required in interpretation due to high levels of heterogeneity and risk of bias.
This is the first systematic review with meta-analysis to evaluate the clinical effectiveness of MWM in isolation or in addition to other physiotherapeutic modalities on pain, ROM and disability for commonly encountered shoulder conditions in clinical practice. The only other systematic review of MWM for shoulder did not include meta-analysis. Most of the included studies in our review evaluated MWM techniques designed to increase shoulder flexion and abduction ROM, thus studies that evaluated these movements were considered for meta-analysis. MWM demonstrated statistically significant and clinically relevant benefits in patients with stage-II frozen shoulder when compared to exercise, passive manual therapy or electrotherapy. Similarly, for patients with shoulder pain and movement dysfunction, MWM demonstrated statistically significant and clinically relevant benefits when compared to exercise alone, electrotherapy, or sham interventions. In addition to ROM, MWM conferred a statistically significant improvement in pain intensity over a control condition in both frozen shoulder and shoulder pain and movement dysfunction sub-categories.
The SMD score was −1.23 (95% CI −1.96, −0.51) in patients with frozen shoulder, and −1.07 (95% CI −1.87, −0.26) in patients with shoulder pain and movement dysfunction. Improvement in pain was statistically significant and favored MWM even when the control group included other passive joint mobilization techniques or sham interventions. This would suggest that pain relief with MWM may be attributed more to neurophysiological effects rather than biomechanical effects of stretching local articular structures [43] since MWM is applied with minimal force, being always pain-free.
In patients with frozen shoulder, flexion ROM improved significantly more following MWM than the control condition (including Maitland, Kaltenborn, and Spencer techniques among others shown in Table 1) with mean difference of −11.73 (95% CI −17.83, −5.64). For abduction, the mean difference was −13.14 (95% CI −19.42, −6.87). In patients with shoulder pain and movement dysfunction, the mean difference in flexion and abduction ROM was −18.48 (95% CI −32.43, −4.54) and −32.46 (95% CI −69.76, 4.84), respectively. These effects were not only statistically significant but also clinically relevant as the improvements in ROM were greater than the MCID of 11° for these two measures [42]. Similar to pain, improvement in ROM was statistically significant even when the control group included other passive joint mobilization techniques. MWM is likely to involve less force than other forms of manual therapy. Again this suggests that improvements in ROM after MWM may be related to neurophysiological effects rather than a mechanical influence on capsular and ligamentous extensibility.
Disability improved significantly more following MWM than the control condition (Table 1) with a SMD of −1.50 (95% CI −2.30, −0.71) and SMD of −0.88 (95% CI −2.18, 0.43) in the category’s frozen shoulder and shoulder pain and movement dysfunction, respectively. Direct comparisons with the MCID are not possible due to the standardization of the disability measures used in the studies included in meta-analysis. The effect sizes for all outcomes were large (> 0.8) for both sub-categories [19]. However, the studies included in meta-analysis displayed high levels of heterogeneity (I2 > 75%), and the GRADE certainty of effect estimate was rated as very low for all variables in both categories, challenging the strength of these results [44] . Pain relief and clinically relevant improvement in shoulder ROM may allow patients to exercises more effectively during their rehabilitation and could explain the significant improvement seen in disability.
The results are in accordance with previous systematic reviews reporting on the efficacy of MWM for peripheral joint disorders including the shoulder, in terms of pain [15,16,45] and ROM [14–16]. However, there was disagreement with respect to disability. Our analysis compared MWM to any other intervention including sham as well as other forms of manual therapy. A previous review of MWM for peripheral joints found no effect on disability when comparing MWM with other forms of manual therapy [45]. In any case, both reviews found high levels of heterogeneity, so we should be cautious about the results.
Heterogeneity displayed in the results of included trials could be explained by the choice of outcomes. It follows that the outcome measure of ROM is very valid for a patient with significant functional stiffness seen in a type-II frozen shoulder, but would be of little value in a patient presenting with subacromial pain syndrome, where pain intensity with load, disability, or other measures are more meaningful [46].
Divergent methods of application of MWM are also suggested in accounting for heterogeneity in results. It is recommended MWM is both an assessment tool and treatment artifact. Its use as a treatment should only follow when an immediate positive modification to a patient’s affected movement or function occurs [46,47]. If a trial MWM proves ineffective, varying the weight-bearing status of the patient using different functional positions, or trialing the use of other forms of MWM are attempted until all avenues are exhausted. The studies found applied RCT and RCT crossover models, assessing standardized adjuncts alone, which lack the finesse to adopt the above guideline. This can be viewed as antithetical to the clinical setting. Interestingly, RCTs evaluating the effects of MWM for lumbar radiculopathy [48] and post ankle sprain [49] using the advised guidelines have been untaken. In Nguyen’s work, despite the fact that there was an overall 84% positive response rate to MWM for ankle sprain, not all patients responded to the first applied MWM technique. The authors postulate this to be a likely outcome in the shoulder, where MWM’s for the scapulothoracic joint, glenohumeral joint, acromioclavicular joint, and spine can be attempted. It is suggested that each patient may require a different approach that is clinically reasoned, patient-centered, and modifiable to achieve the best outcome for the patient [50]. This resonates with guidelines emphasizing the importance of individualized care within a holistic package of multi-modal management in musculoskeletal conditions [4,6] and is useful to the clinician as it represents a truer reflection of the treatment interaction.
Strength and limitations
A strength of this systematic review is that more studies were included than a recent systematic review with similar inclusion criteria evaluating the effect of MWM on shoulder conditions [16]. The additional studies were identified by searching reference lists and non-indexed journals. Additionally, our review provides statistical pooling of data through meta-analysis, which is generally considered to be more precise [51]. In addition, the GRADE approach was used to assess the quality of results. A weakness of this review is that most of the included studies only evaluated the effects of MWM post-intervention, thus it was not possible to report on the long-term effects. Included studies demonstrated significant clinical, methodological, and statistical heterogeneity and most of the included studies showed high risk of bias due to their methodological weaknesses; hence, improvements observed in all outcomes cannot be solely attributed to MWM intervention and caution is required when considering the results.
Future research scope
The authors recommend future studies follow a more pragmatic clinically reasoned and patient-centered approach to the use of the MWM with long-term follow-up. More detailed description of the MWM technique used in clinical trials, and effects of trial MWM’s with details of positive responders are advised. Progression of MWM to include greater load, potentially with over-pressure, should be considered, as should the use of self-MWM and the application of tape, especially within the context of effective patient communication, building patient resilience and providing self-management strategies. As found with exercise in the management of shoulder conditions, the type, dosage, duration, and application of manual therapy in shoulder conditions is ambiguous [6]. By distinguishing between passive manual therapy and MWM, clinicians may be aided in their selection and application of techniques, whereas synthesizing data for manual therapy as a whole is likely to only give insight into the impact of physical touch in the therapeutic relationship. The authors recommend future systematic reviews into shoulder manual therapy make this division.
Conclusion
This systematic review revealed that MWM in isolation or in addition to exercise therapy and/or electrotherapy is superior in improving pain, ROM, and disability in patients with shoulder dysfunction when compared with either exercise therapy and electrotherapy alone or other type of manual therapy. However, the evidence is of low quality owing to high levels of heterogeneity among included studies and inclusion of studies with high risk of bias.
Supplementary Material
Biographies
Kiran Satpute
holds postgraduate qualification in Musculoskeletal Physiotherapy. He is Associate Professor and Head of the Musculoskeletal Department at Smt. Kashibai Navale College of Physiotherapy, India. He is currently a PhD Scholar at Sancheti College of Physiotherapy, India.
Dr Sue Reid
has been a titledmusculoskeletal physiotherapist for 30 years, and is a Certified Mulligan Practitioner and Honorary Member of the Mulligan Concept Teachers Association. She is currently a senior lecturer at the Australian Catholic University, prior to which she taught at the University of Newcastle in Australia for 14 years. Her clinical and research interests include the treatment of cervical spine dysfunction, headaches, tempero-manibular pain, concussion and dizziness. She has an extensive publication list, presented her research at several international conferences, and run numerous workshops on concussion management internationally.
Thomas Mitchell
is a wrist and hand specialist, First Contact Practitioner clinical supervisor and private practitioner in Sheffield UK.
Grant Mackay
is an Australian Physiotherapy Association titled Musculoskeletal Physiotherapist and works in clinical practice in Wollongong, Australia. He completed his Bachelor of Applied Science (Physiotherapy) with honours at the University of Sydney and his Master of Clinical Physiotherapy (Manipulative Therapy) at Curtin University. As a teaching member of the Mulligan Concept Teacher Association, Grant provides postgraduate training courses in the Mulligan Concept. Grant is a faculty staff member of Manual Concepts.
Toby Hall
is a Specialist Musculoskeletal Physiotherapist, Adjunct Associate Professor at Curtin University, and director of Manual Concepts. He graduated as a physiotherapist in the UK in 1985, completing an MSc in 1996 and a PhD in 2010. He has published more than 20 book chapters and more than 140 peer-reviewed articles. He has co-authored 3 books “Mobilisation with Movement, The Art and the Science” & The Mulligan Concept of Manual Therapy: Textbook of Techniques” in 1st & 2nd Edn. He regularly reviews for many journals, is on the international advisory panel of the Journal Musculoskeletal Science & Practice, and is an Associate Editor for the Journal of Manual and Manipulative Therapy.
Appendix 1. The following databases were searched: PubMed (MEDLINE), CINAHL, SPORTDiscus, PEDro, Cochrane library, and Scopus, from inception to 8 January 2021
| Database (n) | Search terms |
|---|---|
| Pubmed (MEDLINE) 728 |
‘Shoulder’[All Fields] OR ‘Acromion’[All Fields] OR ‘Rotator Cuff’[All Fields] OR ‘Acromioclavicular Joint’[All Fields] AND ‘Shoulder Impingement Syndrome’[All Fields] OR ‘Rotator Cuff Injuries’[All Fields] OR ‘Rotator Cuff Tear Arthropathy’[All Fields] OR ‘Bursitis’[All Fields] OR ‘Tendinopathy’[All Fields] OR ‘Osteoarthritis’[All Fields] OR ‘shoulder pain’[MeSH Terms] OR ‘Shoulder’[All Fields] AND ‘pain’[All Fields] OR ‘shoulder pain’[All Fields] AND ‘movement’[MeSH Terms] OR ‘movement’[All Fields] OR ‘movements’[All Fields] OR ‘movement s’[All Fields] AND ‘impair’[All Fields] OR ‘impaired’[All Fields] OR ‘impairment’[All Fields] OR ‘impairments’[All Fields] OR ‘impairing’[All Fields] OR ‘impairment’[All Fields] OR ‘impairments’[All Fields] OR ‘impairs’[All Fields] OR ‘stiff’[All Fields] OR ‘stiffness’[All Fields] OR ‘stiffnesses’[All Fields] AND ‘Exercise Movement Techniques’[All Fields] AND ‘Musculoskeletal Manipulations’[All Fields] OR ‘MWM’[All Fields] OR ‘Mobilisation with movement’[All Fields] OR ‘mobilization with movement’[All Fields] OR ‘Mulligan concept’[All Fields] OR ‘Manual therapies’ [All Fields] OR ‘Manual therapy’[All Fields] AND (‘clinical trial’[Publication Type] OR ‘randomized controlled trial’[Publication Type]) |
|
CINAHL 157 |
|
| Sports Discus: 102 |
AND
AND
AND
|
| PEDro 27 | Mobilization with Movement and shoulder |
| Scopus – 432 | (shoulder) OR (acromion) OR (rotator AND cuff) OR (acromioclavicular AND joint) AND (”Shoulder Impingement Syndrome”) OR (”Rotator Cuff Injuries”) OR (”Rotator Cuff Tear Arthropathy”) OR (bursitis) OR (tendinopathy) OR (osteoarthritis) OR (”Shoulder pain with movement impairment”) OR (stiffness) AND (exercise AND movement AND techniques) AND (musculoskeletal AND manipulations) OR (MWM) OR (”Mobilization with movement”) OR (”mobilization with movement”) OR (”Mulligan concept”) AND (LIMIT-TO (DOCTYPE, ”ar”)) AND (LIMIT-TO (LANGUAGE, ”English”)) |
| Cochrane Library – 510 | #1 Shoulder OR Acromion OR rotator cuff OR Acromioclavicular Joint #2 Shoulder Impingement Syndrome OR Rotator Cuff Injuries OR Rotator Cuff Tear Arthropathy OR Bursitis OR Tendinopathy OR Osteoarthritis OR shoulder pain OR Shoulder AND pain OR shoulder pain AND movement OR movement OR movements AND impair OR impaired OR impairment OR impairments OR impairing OR impairment OR impairments OR impairs OR stiff OR stiffness OR stiffness 3# Exercise Movement Techniques AND Musculoskeletal Manipulations OR MWM OR Mobilization with movement OR mobilization with movement OR Mulligan concept OR Manual therapies OR Manual therapy #1 AND #2 AND #3 |
Supplemental Material
Supplemental data for this article can be accessed here.
Disclosure statement
Kiran Satpute, Grant Mackay, Thomas Mitchell, and Toby Hall teach the Mulligan Concept on postgraduate physiotherapy courses, for which they receive a teaching fee.
References
- [1].Urwin M, Symmons D, Allison T, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis. 1998. Nov;57(11):649–655. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Luime JJ, Koes BW, Hendriksen IJM, et al. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol. 2004;33(2):73–81. . [DOI] [PubMed] [Google Scholar]
- [3].Littlewood C, Bateman M, Connor C, et al. Physiotherapists’ recommendations for examination and treatment of rotator cuff related shoulder pain: a consensus exercise. Physiother Pract Res. 2019;40(2):87–94. . [Google Scholar]
- [4].NICE guidelines ‘Management of shoulder pain’ 2017. [accessed 2021 Mar 01]. Available from: https://cks.nice.org.uk/topics/shoulder-pain/management/initial-management/#initial-management.
- [5].sitecore\lewis.ashman@rcseng.ac.uk. Subacromial Shoulder Pain - Commissioning Guide [Internet]. Royal College of Surgeons. [accessed 2021 Mar 01]. Available from : https://www.rcseng.ac.uk/library-and-publications/rcs-publications/docs/subacromial-shoulder-pain/
- [6].Pieters L, Lewis J, Kuppens K, et al. An update of systematic reviews examining the effectiveness of conservative physical therapy interventions for subacromial shoulder pain. J Orthop Sports Phys Ther. 2020. Mar;50(3):131–141. . [DOI] [PubMed] [Google Scholar]
- [7].Littlewood C, May S, Walters S.. A review of systematic reviews of the effectiveness of conservative interventions for rotator cuff tendinopathy. Shoulder Elbow. 2013;5(3):151–167. [Google Scholar]
- [8].Cliona JM, Hill JC, Hay EM, et al. Identifying potential moderators of first-line treatment effect in patients with musculoskeletal shoulder pain: a systematic review. Eur J Physiother. 2020;1–15. [Google Scholar]
- [9].Lowe CM, Barrett E, McCreesh K, et al. Clinical effectiveness of non-surgical interventions for primary frozen shoulder: a systematic review. J Rehabil Med. 2019;51(8):539–556. [DOI] [PubMed] [Google Scholar]
- [10].Lirio Romero C, Torres Lacomba M, Castilla Montoro Y, et al. Mobilization with movement for shoulder dysfunction in older adults: a pilot trial. J Chiropr Med. 2015;14(4):249–258. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Doner G, Guven Z, Atalay A, et al. Evalution of Mulligan’s technique for adhesive capsulitis of the shoulder. J Rehabil Med. 2013. Jan;45(1):87–91. [DOI] [PubMed] [Google Scholar]
- [12].Delgado-Gil JA, Prado-Robles E, Rodrigues-de-Souza DP, et al. Effects of mobilization with movement on pain and range of motion in patients with unilateral shoulder impingement syndrome: a randomized controlled trial. J Manipulative Physiol Ther. 2015;38(4):245–252. [DOI] [PubMed] [Google Scholar]
- [13].Hing W, Hall T, Mulligan B.. The Mulligan Concept of Manual Therapy. 2nd ed. 2019. Chatswood, Australia: Elsevier. [Google Scholar]
- [14].Stathopoulos N, Dimitriadis Z, Koumantakis GA. Effectiveness of Mulligan’s mobilization with movement techniques on range of motion in peripheral joint pathologies: a systematic review with meta-analysis between 2008 and 2018. J Manipulative Physiol Ther. 2019;42(6):439–449. [DOI] [PubMed] [Google Scholar]
- [15].Westad K, Tjoestolvsen F, Hebron C. The effectiveness of Mulligan’s mobilisation with movement (MWM) on peripheral joints in musculoskeletal (MSK) conditions: a systematic review. Musculoskeletal Sci Pract. 2019;39:157–163. [DOI] [PubMed] [Google Scholar]
- [16].Varghese MV, George J. Effectiveness of Mulligans mobilisation with movement on shoulder dysfunction: a systematic review. Journal of Clinical and Diagnostic Research. 2020;14(10):1–5. [Google Scholar]
- [17].Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- [18].GRADE handbook [Internet]. [cited 2021 Mar 15]. Available from: https://gdt.gradepro.org/app/handbook/handbook.html
- [19].Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York: Academic Press; 2013. p. 459. [Google Scholar]
- [20].Arshad HS, Shah IH, Nasir RH. Comparison of Mulligan mobilization with movement and end-range mobilization following Maitland techniques in patients with frozen shoulder in improving range of motion. International Journal of Science and Research. 2013;4(4):7. [Google Scholar]
- [21].Boruah L, Dutta A, Deka P, et al. To study the effect of scapular mobilization versus mobilization with movement to reduce pain and improve gleno-humeral range of motion in adhesive capsulitis of shoulder: a comparative study. Int J Physiother. 2015;2(5). DOI: 10.15621/ijphy/2015/v2i5/78239 [DOI] [Google Scholar]
- [22].Dilip JR. Effect of Gong’s mobilization versus Mulligan’s mobilization on shoulder pain and shoulder medial rotation mobility in frozen shoulder. Int J Physiother. 2016;3(1). DOI: 10.15621/ijphy/2016/v3i1/88928 [DOI] [Google Scholar]
- [23].Djordjevic OC, Vukicevic D, Katunac L, et al. Mobilization with movement and kinesiotaping compared with a supervised exercise program for painful shoulder: results of a clinical trial. J Manipulative Physiol Ther. 2012. Jul;35(6):454–463. [DOI] [PubMed] [Google Scholar]
- [24].Goyal R, Jindal P, Khurana G. A comparison of granisetron and nitroglycerine for attenuating rocuronium pain: a double-blinded randomized, placebo controlled trial. Saudi J Anaesth. 2014;8(1):83‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Guimarães JF, Salvini TF, Siqueira ALJ, et al. Effects of mobilization with movement vs Sham technique on range of motion, strength, and function in patients with shoulder impingement syndrome: randomized clinical trial. J Manipulative Physiol Ther. 2016;39(9):605–615. [DOI] [PubMed] [Google Scholar]
- [26].Haider R, Bashir MS, Adeel M, et al. Comparison of conservative exercise therapy with and without Maitland Thoracic Manipulative therapy in patients with subacromial pain: clinical trial. J Pak Med Assoc. 2018;68(3):381–387. [PubMed] [Google Scholar]
- [27].Kachingwe AF, Phillips B, Sletten E, et al. Comparison of manual therapy techniques with therapeutic exercise in the treatment of shoulder impingement: a randomized controlled pilot clinical trial. J Man Manip Ther. 2008;16(4):238–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Khyathi P, Babu KV, Kumar NSDA. Comparative effect of spencer technique versus mulligans technique for subjects with frozen shoulder a single blind study. Int J Physiother. 2015;2(2):448–458. [Google Scholar]
- [29].Menek B, Tarakci D, Algun ZC. The effect of Mulligan mobilization on pain and life quality of patients with Rotator cuff syndrome: a randomized controlled trial. J Back Musculoskelet Rehabil. 2019;32(1):171–178. [DOI] [PubMed] [Google Scholar]
- [30].Minerva RK, Alagingi NK, Apparao P. To Compare the effectiveness of Maitland versus Mulligan mobilisation in idiopathic adhesive capsulitis of shoulder. Int J Health Sci (Qassim). 2016;2:9. [Google Scholar]
- [31].Neelapala YVR, Reddy YRS, Danait R. Effect of Mulligan’s posterolateral glide on shoulder rotator strength, scapular upward rotation in shoulder pain subjects - a randomized controlled trial. J Musculoskeletal Res. 2016;19(3):1. . [Google Scholar]
- [32].Ranjana SP, Banerjee D, Bhushan V, et al. Long term efficacy of Maitland mobilization versus Mulligan mobilization in idiopathic adhesive capsulitis of shoulder: a randomized controlled trial. Indian J Physiother Occup Ther. 2016;10(4):91–97. [Google Scholar]
- [33].Rathod D, Priyanka G, Palkar A. Comparative study of Kaltenborn mobilisation versus Mulligan mobilisation in patients with frozen shoulder. Int J Health Sci (Qassim). 2019;9(9):320–324. [Google Scholar]
- [34].Sai KV, Kumar JNS. Effects of Mulligan’s mobilisation with movement on pain and range of motion in diabetic frozen shoulder a randomized clinical trail. Indian J Physiother Occup Ther. 2015;9(4):187–193. [Google Scholar]
- [35].Satpute KH, Bhandari P, Hall T. Efficacy of hand behind back mobilization with movement for acute shoulder pain and movement impairment: a randomized controlled trial. J Manipulative Physiol Ther. 2015;38(5):324–334. [DOI] [PubMed] [Google Scholar]
- [36].Shrivastava A, Shyam AK, Sabnis S, et al. Randomised controlled study of Mulligan’s Vs. Maitland’s mobilization technique in adhesive capsulitis of shoulder joint. Indian J Physiother Occup Ther. 2011;5(4):12–15. [Google Scholar]
- [37].Srivastava N, Joshi S. Comparision between the Effectiveness of Mobilization with Movement and End Range Mobilization along with Conventional Therapy for Management of Frozen Shoulder. Indian J Physiother Occup Ther. 2017;11(4):176‐179. [Google Scholar]
- [38].Subhash R, Makhija M. Effectiveness of mobilization with movement in weight bearing position on pain, shoulder range of motion and function in patients with shoulder dysfunction. Indian J Public Health Res Dev. 2020;11(6):912‐916. [Google Scholar]
- [39].Teys P, Bisset L, Vicenzino B. The initial effects of a Mulligan’s mobilization with movement technique on range of movement and pressure pain threshold in pain-limited shoulders. Man Ther. 2008;13(1):37–42. [DOI] [PubMed] [Google Scholar]
- [40].Yeole U, DrP D, Gharote G, et al. Effectiveness of movement with mobilization in adhesive capsulitis of shoulder: randomized controlled trial. Indian Journal of Medical Research and Pharmaceutical Sciences. 2017;4(2):1–8. [Google Scholar]
- [41].Youssef AR, Ibrahim AMA, Ayad KE. Mulligan mobilization is more effective in treating diabetic frozen shoulder than the Maitland technique. Int J Physiother. 2015;804–810. [Google Scholar]
- [42].Mullaney MJ, McHugh MP, Johnson CP, et al. Reliability of shoulder range of motion comparing a goniometer to a digital level. Physiother Theory Pract. 2010;26(5):327–333. [DOI] [PubMed] [Google Scholar]
- [43].Bialosky J, Beneciuk J, Bishop M, et al. Unraveling the mechanisms of manual therapy: modeling an approach. Journal of Orthopaedic and Sports Physical Therapy. 2018;48(1):8–18. [DOI] [PubMed] [Google Scholar]
- [44].Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003. Sep 6;327(7414):557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Stathopoulos N, Dimitriadis Z, Koumantakis GA. Effectiveness of Mulligan’s mobilization with movement techniques on pain and disability of peripheral joints: a systematic review with meta-analysis between 2008-2017. Physiotherapy. 2019;105(1):1–9. [DOI] [PubMed] [Google Scholar]
- [46].Vicenzino B, Hing W, Rivett D, et al. Mobilisation with Movement The Art and the Science. 1st ed. 2011. Chatswood, Australia: Elsevier. [Google Scholar]
- [47].Lehman GJ. The role and value of symptom-modification approaches in musculoskeletal practice. J Orthop Sports Phys Ther. 2018;48(6):430–435. [DOI] [PubMed] [Google Scholar]
- [48].Satpute K, Hall T, Bisen R, et al. The effect of spinal mobilization with leg movement in patients with lumbar radiculopathy-a double-blind randomized controlled trial. Arch Phys Med Rehabil. 2019;100(5):828–836. [DOI] [PubMed] [Google Scholar]
- [49].Nguyen AP, Pitance L, Mahaudens P, et al. Effects of Mulligan mobilization with movement in subacute lateral ankle sprains: a pragmatic randomized trial. J Man Manip Ther. 2021;1–12. doi: 10.1080/10669817.2021.1889165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Zeppieri Jr G, Bialosky J, George SZ. Importance of outcome domain for patients with musculoskeletal pain: characterizing subgroups and their response to treatment. Phys Ther. 2020;100(5):829–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Bartolucci AA, Hillegass WB. Overview, Strengths, and Limitations of Systematic Reviews and Meta-Analyses. In: Chiappelli F, editor. Evidence-Based Practice: toward Optimizing Clinical Outcomes. Berlin, Heidelberg: Springer; 2010; 251–252. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


