Abstract
This study aims to introduce a new sagittal cephalometric measurement, the sagittal G-triangle analysis, to accurately and reproducibly assess the sagittal jaw relationship. Sagittal G-triangle analysis, which consists of angles AXK and BXK, is based on an equilateral triangle (Bo–X–K) constructed using 5 cephalometric landmarks (Ba, Bo, Po, Or, and G). To test the diagnostic efficiency of this analysis, pretreatment cephalometric radiographs of 120 female and 120 male Chinese patients were randomly selected. For each enlisted subject, angles SNA and SNB as well as angles AXK and BXK were measured and recorded. On the basis of the SNA and SNB results, subjects were categorized into 6 groups: maxillary retrognathism, normal maxilla, maxillary prognathism, mandibular retrognathism, normal mandible, and mandibular prognathism. The diagnostic efficiency of angles AXK and BXK were evaluated using various statistical tests. A high correlation was detected between angles SNA and AXK as well as between angles SNB and BXK. Female patients with angle AXK between −2.255° and 2.860° and male patients with angle AXK between −2.615° and 2.120° were considered to have a normal maxilla position. Female patients with angle BXK between −2.61° and 2.93° and male patients with angle BXK between −2.275° and 0.610° were considered to have a normal mandible position. In conclusion, sagittal G-triangle analysis could be used as an alternative method for the evaluation of the sagittal position of the maxilla and mandible in cephalometric analysis.
Keywords: Cephalometric, nasion, sagittal
Assessment of the sagittal relationship of the maxilla and mandible and quantification of the sagittal changes pre- and post-orthognathic surgery are the 2 primary important aspects in cephalometric analysis in orthognathic diagnosis.1,2 According to the reference plane, the sagittal cephalometric analysis could be divided into 3 groups as follows: 1) those using cranial base as the main reference plane, such as SNA and SNB angle in Steiner analysis3 and N-perpendicular to A-point distance in McNamara analysis;4 2) those using neighboring structure as the main reference plane, such as Condylion to A-point distance in Harvold classic analysis5 and A-point to N-Pog distance in Ricketts analysis;6 and 3) those using the bimaxillary relationship, such as AO–BO distance in Wits appraisal7 and anteroposterior dysplasia indicator in Kim's analysis.8 Theoretically, cephalometric analysis with cranial base reference reveals the actual sagittal position of the maxilla and mandible more precisely. However, there is sometimes a difference between the interpretation of the sagittal cephalometric measurement and actual position of the maxilla and mandible.2
The reason for this is the structure of the anterior cranial base, that is, the sella–nasion plane varies significantly. Not only does the point sella varies but also the position of point nasion is unstable.6,9 As one of the most important landmarks in the anterior cranial base, nasion serves as the cornerstone for current sagittal cephalometric evaluations. Any displacement of nasion, either by cranial growth10,11 or adjacent anatomic structures,12,13 will directly affect the sagittal cephalometric results. During maxillofacial surgery, an ideal position of the maxilla and mandible is essential for a pleasant and harmonic profile of the patient.14 Whether the patient needs one-jaw or two-jaw surgery depends primarily on the clinical experience of the surgeon when sagittal cephalometric analysis is not reliable, even with the help of 3D cephalometric1 or machine learning.15 Thus, a sagittal evaluation that is independent from nasion would be a desirable adjunct in determining the position of the apical base.
After several years of research, our team invented a novel cephalometric analysis using an equilateral triangle as a reference. Constructed on the geometric relationship of the cranial landmarks, this triangle was named the G-triangle. The sagittal, vertical, dental, and soft-tissue cephalometric measurements based on the G-triangle form the G-triangle analysis. Because the G-triangle is independent of nasion, its sagittal evaluation could serve as an alternative evaluation for the previously established sagittal cephalometric parameters. In this paper, with a focus on the sagittal evaluation, we aim to introduce sagittal G-triangle analysis to determine its correlation between the most widely used sagittal cephalometric parameters (SNA and SNB) and to identify its normal ranges using statistic calculation. The results of our study suggested that the sagittal G-triangle analysis, which served as the guide line for the ideal position of the maxilla and mandible, offers an immense help in the treatment planning of maxillofacial surgery.
MATERIALS AND METHODS
Selection of Patients
Pretreatment cephalometric radiographs (120 men and 120 women) were selected randomly from the records of orthodontic patients in the Department of Orthodontics from January 2015 to December 2020. All patients were southern Chinese, and we obtained patient consent to use their clinical records for research purposes before starting their orthodontic treatment. All lateral cephalometric radiographs were obtained using an X550 2D (J. Morita MFG, Kyoto, Japan) machine by the same technician. Patients were positioned in the cephalostat with the sagittal plane at a right angle to the path of the X-rays and the Frankfort Horizontal (FH) plane parallel to the floor. The teeth were in centric occlusion, and the lips were sealed lightly together. The digital radiographs were saved in Joint Photographic Experts Group digital format and calibrated.
We included the lateral cephalometric radiographs of the following patients:
Age range of 18 to 30 years,
No history of orthodontic treatment, trauma, or medical complications,
No pathological lesions of the cranial bone and jaw,
All bilateral anatomical structures showed good superimposition,
Normal-sized frontal sinuses,
Landmarks listed in Supplementary Digital Content, Table 1 were well visualized, and
SN-FH angle between 6.0° and 8.0°.
The G-triangle
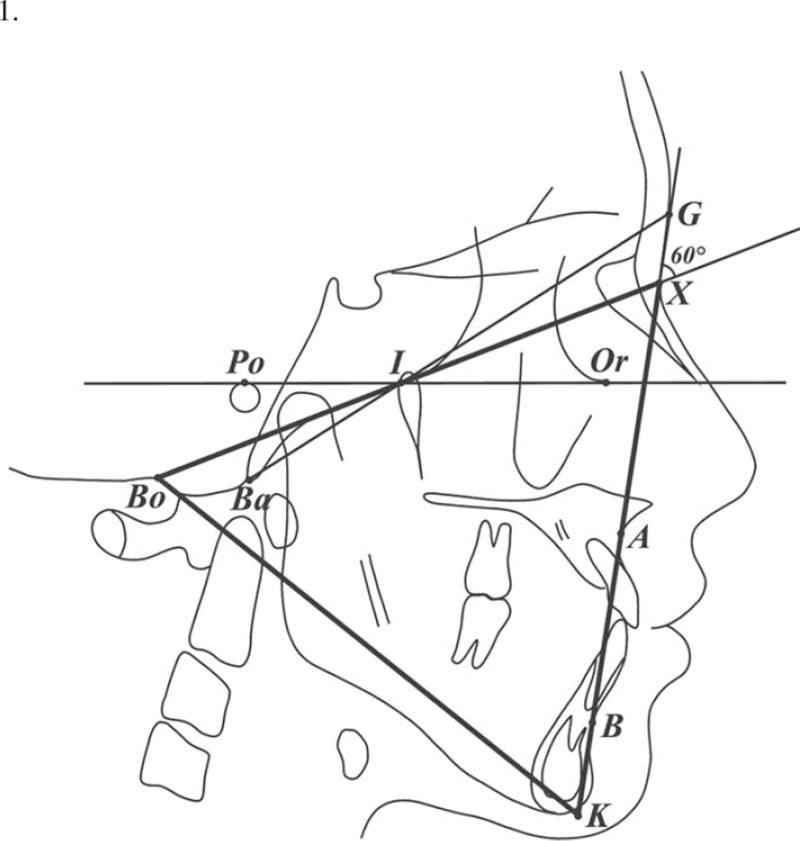
The G-triangle was based on the geometric location of 4 bony landmarks (Bo, Ba, Po, and Or) and 1 soft-tissue landmark (G) and was constructed according to the following steps (Fig. 1):
FIGURE 1.
The frame of G-triangle (the equilateral triangle Bo–X–K).
-
1.
Connect Ba and G, and connect Po and Or. The intersection point of line Ba–G and line Po–Or (FH plane) is defined as point I.
-
2.
Draw a half line from Bo to I.
-
3.
Draw a line passing G to form a 60° angle with line Bo–I. Their intersection point is defined as point X.
-
4.
Draw an inverted equilateral triangle using line segment Bo–X as one of its sides. The third vertex of this triangle is defined as point K.
-
5.
The equilateral triangle Bo–X–K is named the G-triangle.
Measurement Procedure
For the sagittal G-triangle analysis, we introduced angles AXK (the angle formed among points A, X, and K. The angle is positive when point A locates anterior to line X–K and negative when point A locates posterior to line X–K) and BXK (the angle formed among points B, X, and K. The angle is positive when point B locates anterior to line X–K and negative when point B locates posterior to line X–K). For each enlisted cephalometric film, angles AXK and BXK as well as angles SNA (the angle formed among sella turcia, nasion, and point A) and SNB (the angle formed among sella turcia, nasion, and point B) were measured and recorded using custom-programmed computer software. The procedure was performed again by the same operator after 2 weeks to ensure intraexaminer reliability, which was acceptable according to the pilot experiment. The means of each measurement were then calculated and entered into Excel software (Microsoft, Redmond, WA).
Data Process
On the basis of the cut points from literature,16 the data were divided into the following 6 groups:
-
1.
Maxillary retrognathism (SNA < 80.23° in females and SNA < 80.48° in males),
-
2.
Normal maxilla (80.23° < SNA < 86.05° in females and 80.48° < SNA < 85.44° in males),
-
3.
Maxillary prognathism (SNA > 86.05° in females and SNA > 85.44° in males),
-
4.
Mandibular retrognathism (SNB < 77.55° in females and SNB < 77.97° in males),
-
5.
Normal mandible (77.55° < SNB < 83.31° in females and 77.97° < SNB < 82.53° in males), and
-
6.
Mandibular prognathism (SNB > 83.31° in females and SNB > 82.53° in males).
Statistical Analysis
Data were then summarized by determining the means and standard deviations. Independent Student t tests were performed to check for statistical differences between mean values within the female and male groups. One-way analysis of variance was used, followed by Newman–Keuls post hoc testing, to determine the presence of a statistically significant difference between the mean values of the 6 groups. The Pearson correlation coefficient was calculated between SNA with AXK and SNB with BXK for the different gender groups and whole samples. P <0.05 was considered statistically significant for all tests. Receiver-operating characteristic curves were plotted to estimate the diagnostic performance of AXK and BXK for the maxilla and mandible positions, respectively. With these curves, cut points were established to calculate the sensitivity and specificity of each measurement for each malocclusion. All statistics were performed in SPSS 19.0 (SPSS, Chicago, IL).
RESULTS
A total of 240 subjects were enrolled, of whom 120 were female and 120 were male. The mean age of the female group was 22.61 ± 4.13 years, whereas the mean age of the male group was 22.40 ± 3.46 years. There was no statistically significant difference in age (P =0.672) between the 2 groups.
Supplemental Digital Content, Table 2 listed the mean values and standard deviation values of SNA and SNB between the female and male cohorts of the 6 groups. There was no statistically significant difference in the mean values of the SNA and SNB of the sexes within most of the groups, except for the group with maxillary prognathism (P = 0.006) and the normal mandible group (P = 0.013). Thus, in the following analysis, we calculated cephalometric measurements in the female and male groups separately.
The results of the Student–Newman–Keuls post hoc test indicated that the groups were significantly different (Supplemental Digital Content, Tables 3, 4, 5, and 6). There was no statistically significant difference in the mean values of AXK and BXK of the sexes within the groups, except for the group with maxillary prognathism (Supplemental Digital Content, Table 7). When assessing the entire samples, a statistically significant positive correlation and an intraclass correlation coefficient were found between SNA and AXK (r = 0.991) and SNB and BXK (r = 0.992) (Supplemental Digital Content, Table 8).
The cut points of AXK and BXK for the different groups between genders are shown in Supplemental Digital Content, Table 9. Those values coincide with the mean value of AXK and BXK in the normal group. Therefore, it can be predicted with a high degree of certainty that a female patient with an AXK angle between −2.255° and 2.860° truly has a normal maxilla position and a male patient with an AXK angle between −2.615° and 2.120° truly has a normal maxilla position. Meanwhile, a female patient with a BXK angle between −2.61° and 2.93° truly has a normal mandible position, and a male patient with a BXK angle between −2.275° and 0.610° truly has a normal mandible position.
DISCUSSION
For evaluation of the actual sagittal position of the maxilla and mandible, the anterior cranial base is used inevitably as a reference in most of the cephalometric analysis. However, the structure of the anterior cranial base varies significantly, causing unreliable results in these cephalometric analyses. Despite several investigations over several decades, no cephalometric analysis has been found to reveal the precise sagittal position of the maxilla and mandible and predictably identify their ideal sagittal position.17 However, Andrews18 offered an alternative approach to evaluate the sagittal position of the maxilla using “element II” of “The Six Elements of Orofacial Harmony,” which characterizes the maxillary position in relation to the forehead. In Andrew's method, the facial surface of the maxillary incisor touches the goal anterior limit line when the maxilla is in its ideal sagittal position. The use of forehead position and angulation to predict the ideal sagittal position of the maxilla, although a little difficult in clinical application, is a promising technique that could become an important addition for the orthodontist and orthognathic surgeons. In our study, we proposed a novel sagittal cephalometric analysis, the sagittal G-triangle analysis, which is a combination of traditional cephalometric analyses and forehead position evaluation.
The key foundation of G-triangle analysis is the equilateral triangle constructed by Bolton point (Bo) and point X as its vertex. Bo was located in the posterior cranial base, which presents the middle point of the foramen magnum in the sagittal plane. The Bolton plane (the Bolton–nasion line) is widely used as a reliable cranial base reference for craniofacial growth evaluation. Point X is a virtual landmark that is constructed by a specific geometric relationship of 5 anatomic landmarks (Ba, Bo, Po, Or, and G). We believe that craniofacial landmarks are not randomly scattered on the cephalometric films but follow some internal relationship rules. Point X reveals one of the possible relationships between the cranial facial landmarks. The 5 landmarks of the G-triangle interact with each other, so a small inaccuracy in identification or position deviation in one landmark will have a minimum effect on the final result. Once the Bolton point and point X are located, the frame of G-triangle is determined, and its 3 sides (Bo–X, X–K, and K–Bo) and 3 altitudes could be used as reference planes. In this study, we primarily discuss the role of the X–K line in the sagittal evaluation of the maxilla and mandible.
The sagittal G-triangle analysis is composed of 2 measurements: angle AXK for the maxilla and angle BXK for the mandible. To determine the diagnostic ability of this analysis, the most widely applied SNA and SNB angles were set as the targets for comparison in our study. Because the SNA and SNB angles are sometimes affected by the inclined SN plane and shifted point nasion, we limited the samples with SN-FH to 6° to 8° and normal-sized frontal sinus to minimize their bias. We hypothesized that the correlation of angles AXK and SNA as well as angles BXK and SNB would match well. The statistical analysis confirmed a statistically significant positive high correlation between angles SNA and AXK (r = 0.991) and angles SNB and BXK (r = 0.992), suggesting that angles AXK and BXK could be used in sagittal cephalometric analysis as an alternate analysis. Meanwhile, according to the normal value of angles SNA and SNB, we calculated the normal value of angles AXK and BXK, which are all near the value 0. Based on these results, the ideal location of the maxilla and mandible can be very easily determined according to the X–K line. With the help of the X–K line, orthodontists and surgeons could easily determine whether the patient needs one-jaw (Fig. 2) or two-jaw surgery (Fig. 3) and whether the patient needs direct or compensate surgery (Fig. 4). With the combination of the bilateral sagittal split osteotomy (Fig. 5), Lefort I osteotomy (Fig. 6), and genoplasty (Fig. 7) surgery, the goal of the surgery plan is much easier to reach.
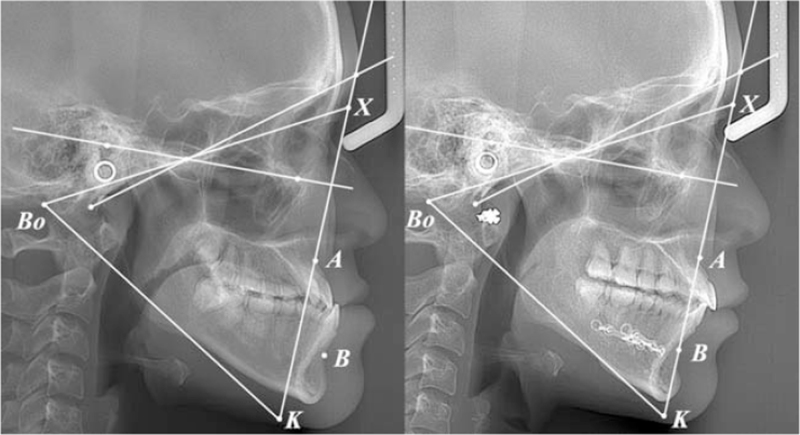
FIGURE 2.
Bilateral sagittal split osteotomy for a skeletal Class III patient. Point A was on the X–K line, whereas Point B was anterior to the X–K line before surgery. After surgery, Point B was on the X–K line. (Left) Before surgery; (Right) after surgery.
FIGURE 3.
Bilateral sagittal split osteotomy + LeFort I maxillary advancement surgery for a skeletal Class III patient. Point A was posterior to the X–K line, whereas Point B was anterior to the X–K line before surgery. After surgery, both Points A and B were on the X–K line. (Left) Before surgery; (Right) after surgery.
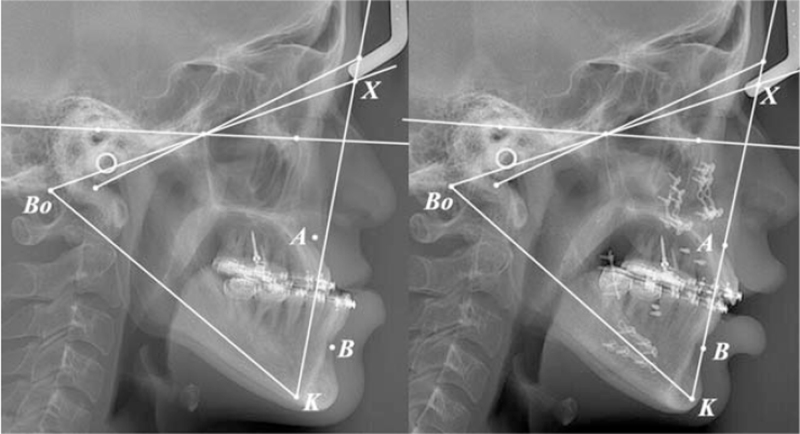
FIGURE 4.
LeFort I maxillary retrogression surgery + genoplasty surgery for a skeletal Class II patient. Point A was anterior to the X–K line, whereas Point B was too much posterior to the X–K line, which was beyond the limit for bilateral sagittal split osteotomy before surgery. After surgery, Point A was on the X–K line. Compensate genoplasty surgery was performed for a better facial profile. (Left) Before surgery; (Right) after surgery.
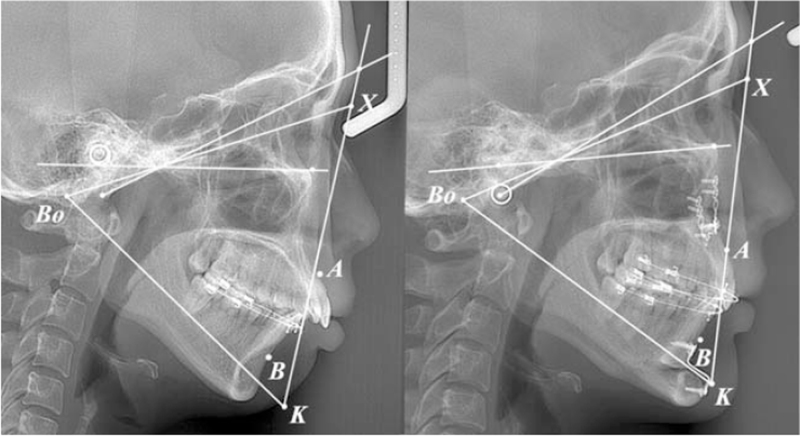
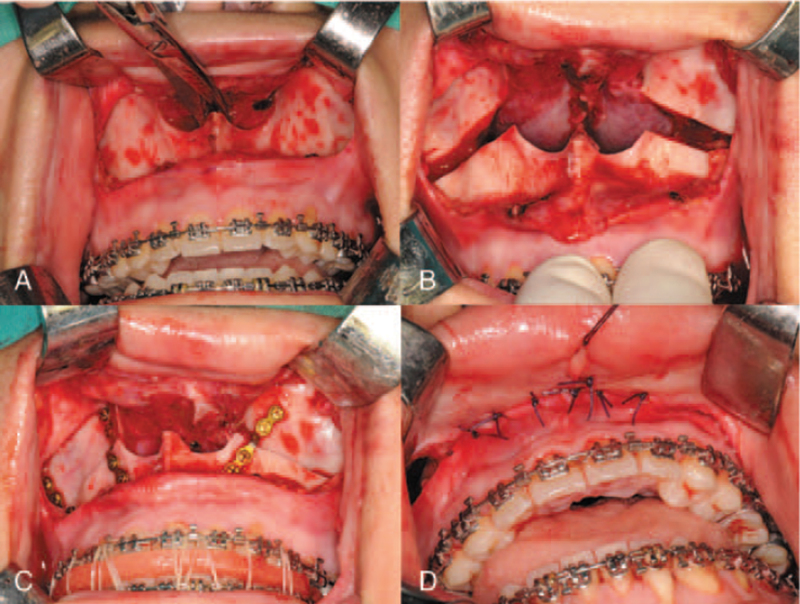
FIGURE 5.
LeFort I osteotomy. A: incision. B: separate maxilla. C: rigid fixation. D: suture.
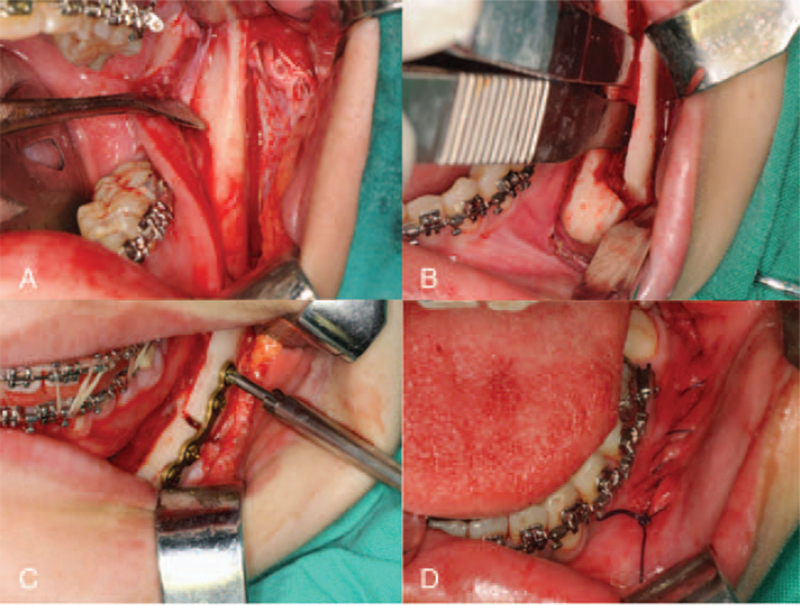
FIGURE 6.
Bilateral sagittal split osteotomy. A: incision. B: sagittal split the ramus. C: rigid fixation. D: suture.
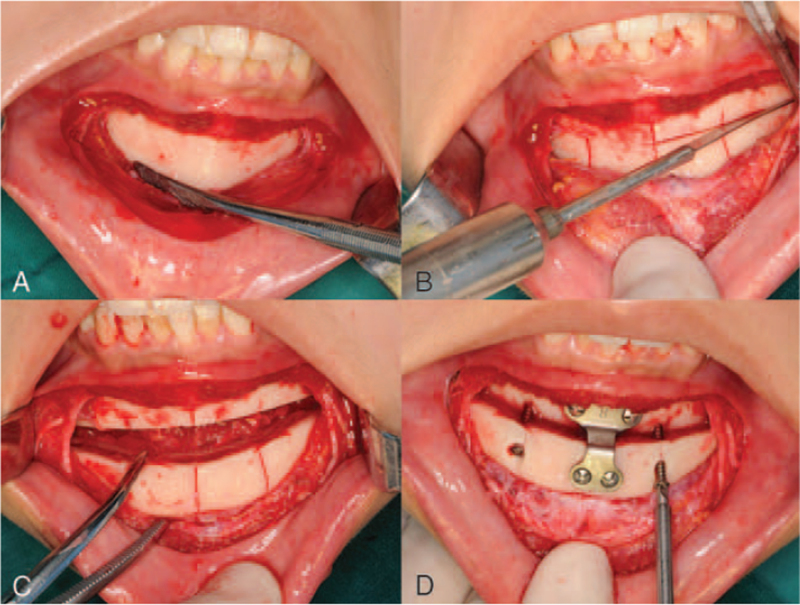
FIGURE 7.
Genoplasty surgery. A: incision. B: separate the mental bone. C: reposition the mental bone. D: rigid fixation.
The first highlight of the sagittal G-triangle analysis is that it bypasses the landmarks in the varying anterior cranial base and provides an alternate method to evaluate the sagittal position of the maxilla and mandible based on the cranial landmarks. The G-triangle analysis views the entire craniofacial skeleton as a whole rather than as separated regions. Through the internal geometric relationship of the cranial structure, a virtual X point is constructed. Together with point Bo, the Bo–X line serves as the basic reference of the G-triangle analysis. Both points Bo and X are less affected by the varying cranial base; hence, the Bo–X line could be considered as a relatively stable reference plane.
The second highlight of sagittal G-triangle analysis is that based on the Bo–X line, an equilateral triangle framework is constructed. In this framework, its 3 sides (Bo–X, X–K, and K–Bo) and 3 altitudes are of equal importance in reference as the Bo–X line. For example, in the sagittal G-triangle analysis, angle AXK has an equal role as angle AXBo in determining the maxilla position, but angle AXK has a much smaller absolute value. With this equilateral triangle framework as reference, any target line in the cephalometric film could find its nearest neighboring reference line among the 6 lines in the G-triangle framework (3 sides and 3 altitudes). All the measuring results in the G-triangle analysis are between −15° and 15°, a number range much easier for measuring and memory.
The third highlight of the sagittal G-triangle analysis is that the X–K side of the G-triangle could be used as a guided goal line for the sagittal evaluation. Based on the statistical analysis, our study revealed that both angles AXK and BXK have a normal range of approximately 0°. In an ideal case, as point B in the mandible is a bit posterior to point A in the maxilla in the sagittal direction, the conventional cephalometric measurements of points A and B have little difference. For example, in Steiner's analysis,3 the normal value of SNA is 82° and that of SNB is 80°. However, in the sagittal G-triangle analysis, the reference X–K line is sloping at a certain angle, so angles AXK and BXK have almost the same normal range. According to the position of points A and B to the X–K line, an easy sagittal evaluation could be deduced. The intermaxillary relationship of the maxilla and mandible could also be evaluated. Because sagittal G-triangle analysis provides a more precise reliable parameter for the assessment of the sagittal jaw relationship according to the harmonious facial profile, it can be a valuable tool when planning maxillofacial surgery for patients with sagittal skeletal deformities.
Because our study had a limited number samples, it has some inevitable limitations. First, only young adults were included. Age-related changes should have been considered as one of the most contributory factors. The cranium develops earlier and faster than the facial skeleton during the early years of infancy and childhood. Thus, sagittal evaluation is different between preadult subjects and adult subjects. Second, only southern Chinese patients were included in this study. Future studies should include patients of diverse racial and ethnic backgrounds to include different craniofacial skeleton structures and facial profile features. Third, the rotation of the jaws was not considered in the sagittal evaluation. There is more than one approach in which a combination could provide the most accurate picture of the relationship of the jaws. No single parameter in the cephalometric analysis should be relied entirely upon and interpreted as the absolute value. Despite these limitations, this study presents an alternative method for sagittal evaluation. With the assistance of the G-triangle frame, improved diagnosis and treatment planning for patients can be obtained even when nasion is not reliable.
In conclusion, the G-triangle frame could be used as an alternative reference in cephalometric analysis. The Sagittal G-triangle analysis, composed of angle AXK and angle BXK, was developed as a diagnostic aid to more consistently evaluate the sagittal jaw relationship. Chinese female patients with an AXK angle between −2.255° and 2.860° truly have a normal maxilla position, and male patients with an AXK angle between −2.615° and 2.120° truly have a normal maxilla position. Chinese female patients with a BXK angle between −2.61° and 2.93° truly have a normal mandible position, and male patients with a BXK angle between −2.275° and 0.610° truly have a normal mandible position.
Supplementary Material
Footnotes
The authors report no conflicts of interest.
Supplemental digital contents are available for this article.
REFERENCES
- 1.Abhinav S, Shao HS, Han NA, et al. Three-dimensional cephalometric analysis: the changes in condylar position pre- and post-orthognathic surgery with skeletal class III malocclusion. J Craniofac Surg 2021; 32:546–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davis GS, Jr, Cannon JL, Messersmith ML. Determining the sagittal relationship between the maxilla and the mandible: a cephalometric analysis to clear up the confusion. J Tenn Dent Assoc 2013; 93:22–28. [PubMed] [Google Scholar]
- 3.Steiner C. The use of cephalometrics as an aid to planning and assessing orthodontic treatment. Am J Orthod 1960; 48:721–735. [Google Scholar]
- 4.McNamara JA, Jr. A method of cephalometric evaluation. Am J Orthod 1984; 86:449–469. [DOI] [PubMed] [Google Scholar]
- 5.Harvold EP. The Activator in Interceptive Orthodontics. St. Louis, MO: The C.V. Mosby Company; 1974. [Google Scholar]
- 6.Jacobson A. Jacobson A. Ricketts analysis. Radiographic Cephalometry: From Basics to Video Imaging. Chicago: Quintessence Publishing; 1995. 85–87. [Google Scholar]
- 7.Jacobson A. The “Wits” appraisal of jaw disharmony. Am J Orthod 1975; 67:125–138. [DOI] [PubMed] [Google Scholar]
- 8.Kim YH, Vietas JJ. Anteroposterior dysplasia mediator: an adjunct to cephalometric differential diagnosis. Am J Orthod 1978; 73:619–633. [DOI] [PubMed] [Google Scholar]
- 9.Tanaka JL, Ono E, Filho Medici E, et al. Influence of the facial pattern on ANB, AF-BF, and Wits appraisal. World J Orthod 2006; 7:369–375. [PubMed] [Google Scholar]
- 10.Moore AW. Observations on facial growth and its clinical significance. Am J Orthod 1959; 45:399–423. [Google Scholar]
- 11.Enlow DH. A morphogenetic analysis of facial growth. Am J Orthod 1966; 52:283–299. [DOI] [PubMed] [Google Scholar]
- 12.Tehranchi A, Motamedian SR, Saedi S, et al. Correlation between frontal sinus dimensions and cephalometric indices: a cross-sectional study. Eur J Dent 2017; 11:64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Özer CM, Atalar K, Öz II, et al. Sphenoid sinus in relation to age, gender, and cephalometric indices. J Craniofac Surg 2018; 29:2319–2326. [DOI] [PubMed] [Google Scholar]
- 14.Yu XN, Bai D, Feng X, et al. Correlation between cephalometric measures and end-of-treatment facial attractiveness. J Craniofac Surg 2016; 27:405–409. [DOI] [PubMed] [Google Scholar]
- 15.Lin G, Kim PJ, Baek SH, et al. Early prediction of the need for orthognathic surgery in patients with repaired unilateral cleft lip and palate using machine learning and longitudinal lateral cephalometric analysis data. J Craniofac Surg 2021; 32:616–620. [DOI] [PubMed] [Google Scholar]
- 16.Li YY, Zhao BJ, Lan TC, et al. Cephalometric analysis of Chinese young adults with normal occlusions. J Clin Stomatol 2016; 32:211–213. [Google Scholar]
- 17.Cory MR, Carly EC, Anthea SR. Maxillary sagittal position in relation to the forehead: a target for orthognathic surgery. J Craniofacial Surg 2018; 29:688–691. [DOI] [PubMed] [Google Scholar]
- 18.Andrews WA. AP relationship of the maxillary central incisors to the forehead in adult white females. Angle Orthod 2008; 78:662–669. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.