Abstract
Background:
An effective interview can strengthen the clinician-patient relationship and improve treatment outcomes. We aimed to assess the effect of communication skills training using the Calgary-Cambridge model on interviewing skills among midwifery students.
Materials and Methods:
In this randomized controlled trial, 30 midwifery students of Golestan University of Medical Sciences were selected using the convenience sampling method and randomly assigned through minimization into the intervention (n = 15) and control (n = 15) groups in 2018. The routine interventions were administered for the control group, and four sessions of communication skills training based on the Calgary-Cambridge model was performed in small groups for the intervention group. Evan and colleague's History-taking Rating Scale was used before and four weeks after the intervention. Data were analyzed using paired and independent-sample t and Mann-Whitney U tests at the significance level of less than 0.05.
Results:
The mean (SD) scores of interviewing skill before and after the intervention was 33.71 (7.34) and 54.50 (8.16), respectively, in the intervention group (t13= 9.26, p < 0.001) and 33.64 (6.02) and 33.93 (5.39) in the control group, respectively (p = 0.85). The difference between the two groups was significant (t26= 7.86, p < 0.001).
Conclusions:
Communication skills training based on the Calgary-Cambridge model can be used as an effective method to improve interviewing skills among midwifery students.
Keywords: Communication, health occupations, medical history taking, students
Introduction
The patient interview is one of the most common professional activities of clinicians. Each clinician performs 100–200 thousand interviews during his/her professional life.[1] The main goal of the patient interview is health promotion. Therefore, an effective interview is not limited to asking several simple questions[2]; rather, it includes extensive knowledge and skills about communication, physical examination, and problem-solving[3] and requires careful attention to patients' feelings and non-verbal behaviors.
An effective interview can improve treatment outcomes,[4] while ineffective interviews may prevent clinicians from collecting necessary data about patient conditions. Therefore, an ineffective interview may lead to dissatisfaction with treatments, increased patient anxiety, and suffering, coping problems related to health conditions in patients, and treatment failure.[5] Yet, some studies showed that medical staff has poor to moderate interviewing skills. A study reported that midwives in healthcare centers in Mashhad, Iran, had moderate history-taking and interpersonal communication skills and poor clinical examination, counseling, and patient education skills.[6] Another study reported that medical students had problems in starting, continuing, and terminating patient interviews.[7] Two other studies also found that physicians had moderate communication and interviewing skills.[4,8]
Communication skills are significant factors behind performing effective patient interviews.[3] Effective communication helps clinicians develop the patients' confidence and respect, gather reliable data about their medical history, and create a supportive and comfortable environment for them.[9] Developing patients' confidence helps them openly express their feelings, concerns, and thoughts and avoid withholding information about their medical history.[10] Therefore, the clinicians' interviewing skills can be improved by improving their communication skills.
A well-known strategy to improve clinicians' communication and interviewing skills is communication skills training programs. These programs can improve communication skills such as initial rapport, explanation of the interview aims, body language, proper position during interview, eye contact, active listening, verbal and non-verbal feedback, silence, psychological assessment, empathy and warmth, selecting appropriate interview questions, and avoiding the use of jargons and making conclusions.[11] Previous studies reported that communication skills training programs for clinicians were effective in significantly improving their clinical skills such as interpersonal communication,[12,13] data gathering, and patient education skills,[8] enabling them to promote patient recovery,[4] enhancing patient satisfaction, treatment adherence, and effectiveness,[14] and promoting public health.[15]
The Calgary-Cambridge model is one of the common approaches to communication skills training, developed as a framework for planning communication skills training.[16] It combines traditional clinical teaching methods and effective communication skills.[17] A study reported that communication skills training based on this model significantly improved clinical skills among medical students.[18] However, another study reported that communication skills training based on this model was not effective in improving interviewing skills among the instructors of a dentistry faculty in Iran.[19] These contradictory results highlight the need for further studies on the effectiveness of this model. Therefore, we evaluated the effect of communication skills training through the Calgary-Cambridge model on interviewing skills among midwifery students.
Materials and Methods
This randomized controlled trial (IRCT20180516039692N1) was conducted on two groups of undergraduate midwifery students and in two stages (pre-t and post-test) in Golestan University of Medical Sciences, Gorgan, Iran, between March and May 2018.
The sample size was calculated based on the results of a previous study reporting a communication mean (SD) score of 21.56 (11.31).[8] Accordingly, with a confidence level of 95%, a power of 80%, a hypothetical increase of 50% (or 11 points) in the interviewing skill mean score, and a hypothetical decrease of 20% (or 2.26 points) in its standard deviation, the sample size of this study was determined to be 28 (14 in the control and 14 in the intervention group). We included students in the 6th or 8th semester who were willing to participate and gave their informed consent. The exclusion criteria were unwillingness to continue participating in the study or being absent in two communication skills training sessions. Initially, Sampling was done using the convenience sampling method, and then the students were allocated to control or intervention groups through minimization based on their semester, academic achievement, and the Persian version of Evan and colleague's History-taking Rating Scale scores before intervention. One student in each pair was labeled 1 (control group), and the next was labeled 2 (intervention group).
Data collection tools were a demographic form used at the beginning and Evan and colleagues' History-taking Rating Scale used at the beginning and four weeks after intervention. This scale includes 22 items in three main areas, namely initiating the interview (six items), interview implementation (eleven items), and interview termination (five items). The items of the scale are scored either 1 (”Poor”), 2 (”Moderate”), or 3 (”Good”). Higher scores stand for a higher interviewing skill.[20] The reliability (Cronbach's alpha of 0.928) and content validity of the Persian version of this scale were confirmed by Bani Davoodi and colleagues.[8] To prevent between-group information leakage, first, the participants in the control group were assessed. Accordingly, an observer used the History-taking Rating Scale to assess the interviewing skills of the participants while they were taking a medical history from a simulated patient at baseline and 4 weeks after the intervention. After that, an intervention was started for the intervention group. Initially, the same observer evaluated the interviewing skill of the participants in the intervention group in the same manner as explained for participants in the control group. The observer was blind to the intervention and control groups.
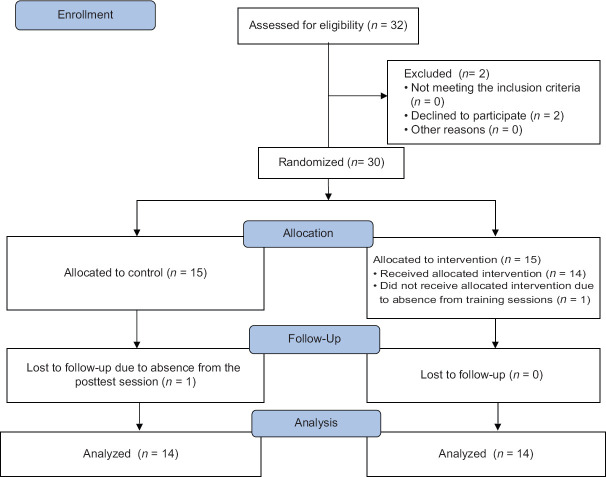
Then, four sessions of communication skills training based on the Calgary-Cambridge model [Table 1] was performed for the intervention group in small groups (7–8 individuals) on Monday and Wednesday afternoon for four hours with two 15-minute break times. The Calgary-Cambridge communication skills model includes five steps (initiating the session, gathering information, building relationships, explanation, and planning, and closing the session). The control group did not receive any specific intervention. The content of intervention sessions concluded introduction and importance of communication skills, clinician-patient communication, different models to establish communication, effective communication establishment, interview structure (starting an interview, data gathering; and developing an interview, and interview termination), and the elements of an interview (empathy, warmth, and adequate explanation). Educational materials were provided through lecture, role-playing, group discussion, brainstorming, video presentation, and Question and Answer teaching methods.[21] Four weeks after the intervention, the same observer re-evaluated the interviewing skills of the participants in the intervention group. Both observer and experimenter were master's students of consultation on midwifery who had passed communication skills units (128 hours) and then validated by midwifery and psychological counseling instructors. The simulated patient was a single 25-year-old master's student in polymer engineering who had no scientific knowledge about midwifery and was hypothetically in the fourteen weeks of her first pregnancy, had no history of abortion, and complained of dysuria and urinary frequency. Therefore, 30 students were primarily recruited and allocated to two equal groups. One participant was excluded from the control group because she did not refer for post-test. One participant was also excluded from the intervention group because she did not attend the training sessions. Therefore, the study was completed with 14 students in each group [Figure 1].
Table 1.
The educational material of communication skills training based on the Calgary-Cambridge model
| Session | Content |
|---|---|
| First | Introduction of communication skills and their importance; Clinician-patient communication; Different models to establish communication |
| Second | Effective communication establishment; Starting an interview; Data gathering; and Developing interview structure |
| Third | Empathy; Warmth; Adequate explanation; and Interview termination |
| Fourth | Teamwork; Watching an educational video; Group discussion about all components of the model |
Figure 1.
The flowchart of the study's inclusion, allocation and follow-up phases
SPSS software, version 18 (SPSS Inc., Chicago, IL, USA, SPSS), was used to analyze the data. Within and between-group comparisons were made using the paired and independent-sample t, Chi-square, and Mann-Whitney U tests at the significance level of less than 0.05.
Ethical Considerations
This study was approved by the Ethics Committee of Golestan University of Medical Sciences, Gorgan, Iran (code: IR.GOUMS.REC.1396.315). The objectives of the study were explained to the participants, and they were ensured that their data would be handled confidentially and they would have the freedom to stay in or withdraw from the study. Before the intervention, all participants signed the written informed consent. After performing the post-test, the study intervention was also offered to participants in the control group. However, none of them were willing to receive the intervention. Therefore, written educational materials were provided for all of them, and they were asked to refer to the authors in case of any question.
Results
The mean (SD) score age of the students in the control and intervention groups were 22.07 (1.07) and 21.64 (1.08), respectively (p = 0.301). All the students were women and most of them were single in both groups (control group: 78.57%, intervention group: 57.14%). Moreover, most participants in the control group had a history of participating in communication skills workshops (57.14%), while most participants in the intervention group did not have such a history (64.28%). The groups did not differ significantly from each other with respect to their demographic characteristics [Table 2].
Table 2.
Demographic characteristics of midwifery students in the two study groups
| Variable | Control n (%) | Intervention n (%) | Total n (%) | p | |
|---|---|---|---|---|---|
| Marital status | Single | 11 (78.57) | 8 (57.14) | 19 (67.85) | 0.225* |
| Married | 3 (21.42) | 6 (42.85) | 9 (32.14) | ||
| Place of residence | Urban areas | 10 (71.42) | 10 (71.42) | 20 (71.42) | 0.99* |
| Rural areas | 4 (28.57) | 4 (28.57) | 8 (28.57) | ||
| Grade point average | <15 | 0 (0) | 2 (14.28) | 2 (7.14) | 0.316* |
| 15-16 | 6 (42.85) | 3 (21.42) | 9 (32.14) | ||
| 16-17 | 5 (35.71) | 7 (50) | 12 (42.85) | ||
| 17-18 | 3 (21.42) | 2 (14.28) | 5 (17.85) | ||
| History of participating in communication skills workshops | Yes | 8 (57.14) | 5 (35.71) | 13 (46.43) | 0.256* |
| No | 6 (42.85) | 9 (64.28) | 15 (53.57) | ||
| Academic semester | 8 | 8 (57.14) | 7 (50) | 15 (53.57) | 0.705* |
| 6 | 6 (42.85) | 7 (50) | 13 (46.43) | ||
*Chi-square test
The pre-test mean (SD) interviewing skill scores in the control and intervention groups were 33.64 (6.02) and 33.71 (7.34), respectively (p = 0.978), but this difference was not significant according to the independent t-test with respect to the three interviewing skill domains (p > 0.05, Table 3). Four weeks after the intervention, the mean (SD) interviewing total skill scores in the control and intervention groups were 33.93 (5.39) and 54.50 (8.16), respectively (p < 0.001, Table 3).
Table 3.
Comparing the mean scores of interviewing skills and its three domains in the two groups before and after the intervention
| Interviewing skill | Mean (SD) |
Z or t | p | ||
|---|---|---|---|---|---|
| Control | Intervention | ||||
| Interview beginning | Before | 10.07 (1.73) | 9.64 (1.86) | -0.87 | 0.401** |
| After | 10.36 (1.49) | 14.29 (2.70) | -4.75 | <0.001* | |
| Interview implementation | Before | 17.36 (4.16) | 17.86 (5.48) | -0.27 | 0.788* |
| After | 17.36 (3.45) | 27.71 (3.97) | -4.24 | <0.001** | |
| Interview termination | Before | 6.21 (1.36) | 6.21 (1.57) | -0.19 | 0.874** |
| After | 6.21 (1.42) | 12.50 (2.95) | -4.20 | <0.001** | |
| Total | Before | 33.64 (6.02) | 33.71 (7.34) | -0.02 | 0.978* |
| After | 33.93 (5.39) | 54.50 (8.16) | -7.86 | <0.001* | |
*Independent-sample t-test. **Mann-Whitney U
Paired t-test results showed that within-group comparisons of the mean interviewing skills scores and all its three main domains did not significantly change in the control group (p > 0.05), while all these mean scores significantly increased in the intervention group (p < 0.001, Table 4).
Table 4.
Comparing the mean score of interviewing skills and its three domains in each group before and after the intervention
| Interviewing skill | Mean (SD) |
t | p | ||
|---|---|---|---|---|---|
| Before | After | ||||
| Interview beginning | Control | 10.07 (1.73) | 10.36 (1.49) | -0.69 | 0.50* |
| Intervention | 9.64 (1.86) | 14.29 (2.70) | -4.87 | <0.001* | |
| Interview implementation | Control | 17.36 (4.16) | 17.36 (3.45) | 0.00 | 0.99* |
| Intervention | 17.86 (5.48) | 27.71 (3.97) | -7.41 | <0.001* | |
| Interview termination | Control | 6.21 (1.36) | 6.21 (1.42) | 0.00 | 0.99* |
| Intervention | 6.21 (1.57) | 12.50 (2.95) | -8.61 | <0.001* | |
| Total | Control | 33.64 (6.02) | 33.93 (5.39) | -0.18 | 0.85* |
| Intervention | 33.71 (7.34) | 54.50 (8.16) | -9.26 | <0.001* | |
*Paired-sample t test
Discussion
We aimed to evaluate the effects of communication skills training using the Calgary-Cambridge model on interviewing skills among midwifery students. The results of the present study showed that communication skills training through the Calgary-Cambridge model significantly improved interviewing skills and all its three main domains among midwifery students. Despite the importance of patient interviews, studies showed that patients' highest dissatisfaction was with clinicians' poor communication skills such as listening.[22,23,24]
At the beginning of the study, participants in both groups had poor interviewing skills. The lowest interviewing skill domain score at baseline was related to the interview termination domain, while the highest domain score was related to the interview beginning domain. An earlier study also reported the same findings.[7] Compared with clinical examination and laboratory studies, a precise and comprehensive clinical interview can provide more detailed data about patients' conditions for accurate diagnosis and treatment.[25] In contrast, an incomprehensive interview in which a clinician does not address illness experience and psychological aspects of illness may result in adverse treatment outcomes.[11] A study showed that communication skills such as using open-ended questions, giving feedback, legitimization of the underlying condition, and respect had positive correlations with patients' verbalization of their anxiety while using focused and surveying questions was negatively correlated with verbalization of their anxiety.[26] Significant improvement in our participants' interviewing skills in the interview beginning domain may be related to the positive effects of the study intervention on their awareness and knowledge about the importance of asking patient's name, explaining interview aims, and enhancing patient's confidence at the beginning of the interview. Moreover, participants' improved interviewing skills in the domain of interview implementation can be attributed to improvements in their knowledge and skills about the appropriate use of open-ended and focused questions, empathy, use of simple and understandable words, active listening, respecting patient's beliefs, and encouraging patients to share more information. Finally, significant improvement in participants' interview termination skills in the intervention group could be related to the effectiveness of the intervention in significantly improving their ability to make conclusions and evaluate the patient's perception of the interview. In line with our findings, several earlier studies reported the positive effects of communication skills training through the Calgary-Cambridge model on interviewing skills among medical students,[27] physicians,[28] and infectious disease and internal medicine residents.[29] However, a study reported the ineffectiveness of communication skills training through this model on interviewing skills among dentistry faculty members in a leading university in Tehran, Iran.[19] This inconsistency may be attributed to the fact that communication skills training in that study consisted of a single four-hour session, in which some aspects of communication skills were directly trained through lectures, and the remaining aspects were indirectly addressed through pamphlets.
However, in the present study, all materials related to communication skills were directly provided to participants in four four-hour sessions. Moreover, our participants were students, while participants in that study were faculty members who might have a limited amount of time for reading pamphlets and practicing the learned skills. Communication skills training courses can be integrated into the academic curricula of all healthcare-related disciplines.[30] Thus, midwifery authorities can use this model to improve midwifery students' interviewing skills.
Among the study limitations were the limited number of eligible students and the limited amount of time for conducting the study. It is suggested that more studies be done over a longer period of time to examine the long-term effects of this training.
Conclusion
This study shows that communication skills training through Calgary-Cambridge model are effective in significantly improving interviewing skills among midwifery students. Thus, midwifery authorities can use this model to improve midwifery students' interviewing skills.
Financial Support and Sponsorship
Golestan University of Medical Sciences, Gorgan, Iran
Conflicts of interest
Nothing to declare.
Acknowledgements
This study was financially supported by the Department of Research and technology Affairs of Golestan University of Medical Sciences, Gorgan, Iran (Grant no 961222311). Hereby, the authors would like to thank the Department of Department of Research and technology Affairs of the University, the authorities of Booyeh Nursing and Midwifery Faculty, Gorgan, Iran, and all midwifery students who participated in the study.
References
- 1.Biglu M-H, Nateq F, Ghojazadeh M, Asgharzadeh A. Communication skills of physicians and patients' satisfaction. Mater Sociomed. 2017;29:192–5. doi: 10.5455/msm.2017.29.192-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bickley L, Szilagyi PG. Bates' Guide to Physical Examination and History-Taking. Philadelphia: Lippincott Williams and Wilkins; 2012. [Google Scholar]
- 3.Silverman J, Kurtz S, Draper J. Skills for Communicating with Patients. Florida: CRC Press; 2016. [Google Scholar]
- 4.Bahraminia S, Amini M. Evaluating final-year medical students' communication skills using an observational rating scale in Shiraz medical school? Biomed Res. 2018;29:2992–6. doi: 10.4066/biomedicalresearch. 29-17-3449. [Google Scholar]
- 5.Ryle G, Salathé M, Bonhoeffer S, Schwitzer G, Silberg W, Lundberg G, et al. 86 Medical Interviewing. Cambridge Handbook of Psychology, Health and Medicine. 2019;5:387. [Google Scholar]
- 6.Mirzaee K, Oladi Ghadikolaee S, SHakeri M, Mousavi Bazzaz M. Evaluation of the quality of postpartum care based on bruce model in medical health centers of Mashhad City in 2013-2014. Iran J Obstet Gynecol Infertil. 2015;18:1–10. [Google Scholar]
- 7.Rahman A. Initial assessment of communication skills of intern doctors in history-taking. Med Teach. 2000;22:184–8. [Google Scholar]
- 8.Banidavoodi S, Hoseinzade M, Maraghi E. Assessment of physicians' communication with patients in Ahvaz hospitals from patient and observer 'Perspectives. J Ahvaz Jundishapur Univ Med Sci. 2013;4:65–71. [Google Scholar]
- 9.Nair BT. Role play-An effective tool to teach communication skills in pediatrics to medical undergraduates. J Educ Health Promot. 2019;8:18. doi: 10.4103/jehp.jehp_162_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burkman RT. Berek & Novak's gynecology. JAMA. 2020;308:516–7. [Google Scholar]
- 11.Awinda D, Syakurah R, Fadilah M. Assessment of doctor-patient communication among residents in internal medicine polyclinic at RSUP Dr. Mohammad Hoesin Palembang 2014 using simplified checklist of Calgary Cambridge guide. Medicinus. 2020;7:184–94. [Google Scholar]
- 12.Gibson S, Davidson Z. An observational study investigating the impact of simulated patients in teaching communication skills in preclinical dietetic students. J Hum Nutr Diet. 2016;29:529–36. doi: 10.1111/jhn.12352. [DOI] [PubMed] [Google Scholar]
- 13.Moore PM, Rivera S, Bravo-Soto GA, Olivares C, Lawrie TA. Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database Syst Rev. 2013;2013:CD003751. doi: 10.1002/14651858.CD003751.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsimtsiou Z, Stavropoulou C, Papastefanou N, Lionis C. Enhancing clinical communication in dermatologists: A personalized educational intervention. J Dermatolog Treat. 2017;28:647–51. doi: 10.1080/09546634.2017.1309348. [DOI] [PubMed] [Google Scholar]
- 15.Schneider M-J. Introduction to Public Health. Jones and Bartlett Learning. 2020 [Google Scholar]
- 16.Kurtz SM, Silverman JD. The Calgary-Cambridge referenced observation guides: An aid to defining the curriculum and organizing the teaching in communication training programmes. Med Educ. 1996;30:83–9. doi: 10.1111/j.1365-2923.1996.tb00724.x. [DOI] [PubMed] [Google Scholar]
- 17.Kurtz S, Silverman J, Benson J, Draper J. Marrying content and process in clinical method teaching: Enhancing the Calgary-Cambridge guides. Acad Med. 2003;78:802–9. doi: 10.1097/00001888-200308000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Gupta A, Gupta B, Verma A, Sharma C, Thakur S, Soni A. Assessment of labor room communication skills among postgraduate students of obstetrics and gynecology. Int J Reprod Contracept Obstet Gynecol. 2020;9:2281–7. [Google Scholar]
- 19.Rezvani M, Hosseini M, Ebn Ahmadi A, Sabur S. Effect of Communication Skills course on academic staff of dental school on their competency in establishing an effective communication with patient in 2011-2012, according to Calgary-Cambridge. tehran: Shahid Beheshti University of Medical Sciences. 2014 [Google Scholar]
- 20.Evans BJ, Stanley RO, Coman GJ, Sinnott V. Measuring medical students' communication skills: Development and evaluation of an interview rating scale. Psychol Health. 1992;6:213–25. [Google Scholar]
- 21.Choudhary A, Gupta V. Teaching communications skills to medical students: Introducing the fine art of medical practice. Int J Appl Basic Med Res. 2015;5(Suppl 1):S41–4. doi: 10.4103/2229-516X.162273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kee JW, Khoo HS, Lim I, Koh MY. Communication skills in patient-doctor interactions: Learning from patient complaints. Health Prof Educ. 2018;4:97–106. [Google Scholar]
- 23.Zawisza K, Galas A, Tobiasz-Adamczyk B. Factors associated with patient satisfaction with health care among Polish older people: Results from the polish part of the COURAGE in Europe. Public Health. 2020;179:169–77. doi: 10.1016/j.puhe.2019.10.012. [DOI] [PubMed] [Google Scholar]
- 24.Ganasegeran K, Perianayagam W, Abdul Manaf R, Ali Jadoo SA, Al-Dubai SA. Patient satisfaction in Malaysia's busiest outpatient medical care. ScientificWorldJournal. 2015;2015:714754. doi: 10.1155/2015/714754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schultz MA, Doty M. Why the history and physical examination still matter. JAAPA. 2016;29:41–5. doi: 10.1097/01.JAA.0000480568.62755.72. [DOI] [PubMed] [Google Scholar]
- 26.Goto M, Takemura YC. Which medical interview skills are associated with patients' verbal indications of undisclosed feelings of anxiety and depressive feelings? Asia Pac Fam Med. 2016;15:2. doi: 10.1186/s12930-016-0027-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Managheb S, Zamani A, Shams B, Farajzadegan Z. The effect of communication skills training by video feedback method on clinical skills of interns of Isfahan University of medical sciences compared to didactic methods. Health Educ J. 2012;71:546–52. [Google Scholar]
- 28.Zamani A, Shams B, Moazzam E. Communication skills training for physicians as a strategy for enhancing patients' satisfaction: A model for continuing education. Iran J Med Sci. 2004;4:15–22. [Google Scholar]
- 29.Zamani AR, Shams B, Siadat Z, Adibi P, Salehi H, Saneii H. The effect of communication skill training on clinical skill of internal medicine and infectious disease residents of Isfahan University of medical sciences. J Med Sci. 2006;8:97–102. [Google Scholar]
- 30.Tavakol M, Murphy R, Torabi S. A needs assessment for a communication skills curriculum in Iran. Teach Learn Med. 2005;17:36–41. doi: 10.1207/s15328015tlm1701_7. [DOI] [PubMed] [Google Scholar]